Abstract
Objective
To observe the clinical results of proximal femoral nail anti-rotation (PFNA) combined with zoledronic acid injection in the treatment of osteoporotic intertrochanteric fractures in the elderly.
Methods
60 elderly patients with osteoporotic intertrochanteric fractures were diagnosed using a dual energy X-ray bone density instrument. Patients were randomly divided into treatment or control groups (30 cases in each group). Patients in both groups were treated by closed/open reduction and internal fixation using PFNA. In the treatment group, patients received one zoledronic phosphonic acid injection of 5 mg/100 ml via intravenous drip, in addition to 600 mg of Caltrate D (qd) and 0.25 μg of alpha ossification alcohol (qd). The control group received 600 mg of Caltrate D (qd) and 0.25 μg of alpha ossification alcohol (qd). The oral drugs were administered for 12 months. Bone pain relief was observed, and changes in the bone mineral density (BMD) of the lumbar and health-side hip were recorded. Clinical results were evaluated using the Visual Analogue Scale (VAS), Harris joint function score, and Osteoporosis Quality of Life Scale (OQOLS).
Results
Compared with the control group, bone pain symptoms were significantly alleviated (p < 0.05) in the treatment group. In the treatment and control groups, both between-group and within-group differences in BMD were significantly increased in L1–4, femoral neck and trochanter (p < 0.05). No significant differences were found between the two groups in regard to the involved hip or the total rate of improvement at the end of the follow-up period, although cases in the treatment group had higher OQOLS scores than those of the controls (p = 0.04). Cases in the treatment group healed more quickly than those in the control group [(13 ± 3.2) weeks vs (15 ± 4.6) weeks, p = 0.02]. During the follow-up period, cases in the treatment group had no new fractures, whereas 2 new cases of hip fracture and 2 cases of distal radial fractures were observed among the controls.
Conclusion
Zoledronic acid injection combined with PFNA is a favorable treatment option for the elderly patients with osteoporotic intertrochanteric fracture. It can effectively relieve bone pain, increase bone density, improve quality of life, reduce the occurrence of new fractures and promote fracture healing.
Keywords: Hip fractures, Osteoporosis, Internal fixators, Aged
Introduction
Given the accelerated aging of the Chinese population, osteoporosis, being an age-related disease, has shown a corresponding yearly growth in the incidence among the elderly.1 The characteristics of osteoporosis include decreased bone mass and microstructure damage to bone tissue, which leads to a decrease in bone strength and accompanying increase in bone fragility, along with an increased risk of fracture. Osteoporotic fracture often occurs at the hip, the distal radius or the spinal column. The most serious fracture is an osteoporotic hip fracture, especially an intertrochanteric fracture, which features in high morbidity, mortality, and disability rates. At present, surgical intervention is the primary treatment for intertrochanteric fractures; however, more and more studies have shown that anti-osteoporosis therapy for patients in the perioperative period may be better for postoperative rehabilitation and long-term survival.2 The purpose of the present study was to observe the clinical results of the treatment of senile osteoporotic intertrochanteric fractures using a combination of zoledronic acid injection and proximal femoral nail antirotation (PFNA).
Patients and methods
Patients
This study was undertaken at the Department of Orthopedic Surgery of West China Hospital, Sichuan University, from January 2011 to December 2011. The research administration department and the ethical committee of West China Hospital approved the study protocol and procedures.
Study inclusion criteria included: (1) a diagnosis of osteoporosis (Chinese Diagnosis Standards of Osteoporosis3); (2) the presence of a hip fracture caused by low energy trauma; and (3) age ≥65 years. Exclusion criteria included: (1) a history of treatment for osteoporosis prior to hip fracture; (2) a history of administration of calcium, heparin, glucocorticoid or other medicines affecting bone metabolism within 6 months prior to hip injury; (3) a history of gastrointestinal surgery; (4) a history of illness related to the liver, kidney, thyroid or parathyroid glands; and (5) a history of organic psychosis or negative habits such as smoking. Based on the different treatment methods, the included patients were divided into a treatment group and a control group, each containing 30 cases. The bone mineral density (BMD) of all cases was determined using dual energy X-ray absorption (DEXA), and the BMD values reached the diagnostic criteria of osteoporosis according to the WHO standard. The Evans-Jensen system was used in the classification of fractures.4
Surgical treatment
Each patient underwent an internal fixation operation performed by the same surgical team using PFNA within three days of hospitalization. Under general or epidural anesthesia, the patient laid on his/her back on the traction table, with the uninjured extremity fixed on the bracket as far as possible to allow for C-arm fluoroscopic imaging during the operation. To expose the greater trochanter and the femoral medullary cavity, a 15-degree angle should be maintained between the affected extremity and trunk of the body. The operation should proceed with the C-arm fluoroscopy on. After traction and fracture reduction, a minor longitudinal incision of 4–6 cm in length was made approximately 5–10 cm proximal from the tip of the greater trochanter. Make a parallel incision of the fascia of the gluteus medius and split the gluteus medius in line with the fibers. In the AP view, the PFNA entry point was usually on the tip or slightly lateral to the tip of the greater trochanter in the 5° curved extension of the medullary cavity, as the medial-lateral angle of the PFNA was 5°. The tip, or slightly lateral to the tip, of the greater trochanter is a good option as the entry point for PFNA nailing. The guide pin was then burrowed into the distal medullary cavity under the monitoring of the C-arm. After proximal reaming, the PFNA is manually inserted with care as far as possible into the femoral opening. A slight twisting of the hand would facilitate insertion. If the PFNA cannot be inserted, select a PFNA with a smaller diameter or ream the medullary cavity to a diameter that is at least 1 mm larger than that of the selected nail. If necessary, light blows with the hammer on the protection shield of the insertion handle can support PFNA insertion. Fix the screw at the distal end after fixing the helical-faced blades at the proximal end. Use fluoroscopy again after fixing the PFNA to decide its position. An open reduction should be performed if the close reduction was difficult.
The patient should engage in joint motion and muscle strength exercise in bed on the first day after surgery. One day later, walking-assistance should be recommended. Weight-bearing exercise depends on the fracture type and the stability after reduction. In our study, all rehabilitation in the hospital was performed by the same therapist. Clinical healing of the fracture was standardized as follows: no pain in the affected extremity during weight-bearing walking; no percussion pain at the fracture area; no longitudinal percussion pain at the affected extremity; a fuzzy facture line observed on X-ray; and trabecular bone growth observed in the fractured zone.
Zoledronic acid injection
Given a creatinine clearance ≥35 ml/min and normal blood calcium levels, the patients in the treatment group were injected with zoledronic acid on postoperative day 3. The patients took one Tylenol tablet (q6h) continuing into the next day after the infusion. A 1000 mL balanced salt solution was given before the zoledronic acid injection (5 mg/100 mL, infusion time ≥15 min); next, a 500 mL balanced salt injection was also given. Patients in both groups continuously took 600 mg of Caltrate D and 0.25 μg of Calcitriol (qd) for 12 months after surgery.
Observation index
Bone pain evaluation: Hip pain was measured by the four-grade bone pain score: 0, no pain; 1, obvious pain while not affecting daily life; 2, bearable pain or partially affecting daily life and work; and 3, unbearable pain or unable to work. General pain was measured using the Visual Analogue Scale/Score (VAS), with scores ranging from 0 (no pain) to 10 (greatest pain).
Hip joint function score: The Harris joint function score was used to measure the function at the hip joint. Standard scores of ≥90, 80–90, 70–79, and ≤70 were indicative of excellent, good, acceptable, and poor function, respectively.
Quality of life score: The life quality was evaluated using the Osteoporosis Quality of Life Scale (OQOLS).5
Bone density examination: The American lunar prodigy dual-energy X-ray absorptiometry (DEXA) was used to examine the pretreatment and posttreatment bone density of the lumbar (L1–4) and hip (femoral neck, Ward's triangle area, and greater trochanter) of the uninjured side.
Safety evaluation: Influenza-like symptoms, such as fever, myalgia, and arthralgia were observed and recorded, in addition to the occurrence of any new fractures.
Statistical methods
SPSS version 17.0 statistical software was used. Data are represented as the mean ± standard deviation, and Student's t-test was used to conduct between-group comparisons. The Chi-square test was used to examine differences between categorical variables. Any result with a p-value below 0.05 was deemed statistically significant.
Results
Comparison of the pretreatment baseline and relative operation data are shown in Table 1.
Table 1.
Comparison of pretreatment baseline and relative operation data.
| Item | Treatment group (n = 30) | Control group (n = 30) | p value |
|---|---|---|---|
| Age (year) | 74.99 ± 4.81 | 73.96 ± 5.80 | 0.131 |
| Gender (male/female) | 11/19 | 13/17 | 0.598 |
| BMI (kg/cm2) | 25.37 ± 2.84 | 25.20 ± 2.61 | 0.708 |
| Serum calcium (mmol/L) | 2.3 ± 0.23 | 2.34 ± 0.28 | 0.572 |
| Serum creatinine (μmol/L) | 64.06 ± 0.29 | 63.43 ± 0.23 | 0.603 |
| BMD of L1–4 (g/cm2) | 0.79 ± 0.14 | 0.82 ± 0.12 | 0.524 |
| BMD of femoral neck (g/cm2) | 0.65 ± 0.13 | 0.69 ± 0.11 | 0.784 |
| BMD of greater trochanter (g/cm2) | 0.54 ± 0.10 | 0.55 ± 0.12 | 0.846 |
| Fracture classification | |||
| Evans-Jensen type 1 | 12 | 10 | 0.896 |
| Evans-Jensen type 2 | 11 | 12 | |
| Evans-Jensen type 3 | 7 | 8 | |
| Reduction (closed/open) | 29/1 | 27/3 | 0.612 |
| Average operating time (min) | 45 ± 17 | 43 ± 10 | 0.656 |
| Hospital stay (d) | 12 ± 3 | 12 ± 5 | 0.868 |
In general, patients were followed up two weeks after surgery and every four to six weeks thereafter. All the patients in the two groups received a 12-month follow-up.
The bone pain symptoms of the two groups was greatly alleviated after 12 months of treatment (p = 0.000, Table 2). There were no significant differences between the two groups in terms of VAS scores prior to surgery (Table 3). After 12 months of treatment, no significant difference was found between the two groups in the Harris scores of the affected hip (81.12 ± 7.9 vs 81.62 ± 5.4, p = 0.219). Likewise, in terms of the hip joint function, there was no significant between-group difference (p = 0.792, Table 4).
Table 2.
Comparison of the bone pain symptom scores of the two groups before and after treatment.
| Group | Time | Grade of pain |
p value | |||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |||
| Study (n = 30) | Pretreatment | 0 | 6 | 8 | 16 | 0.000a |
| Posttreatment | 10 | 12 | 7 | 1 | ||
| Control (n = 30) | Pretreatment | 0 | 7 | 10 | 13 | 0.000b |
| Posttreatment | 12 | 10 | 6 | 2 | ||
Pretreatment vs posttreatment in study group.
Pretreatment vs posttreatment in control group.
Table 3.
Comparison of VAS scores between the two groups before and 12 months after treatment.
| Group | Score of VAS |
p value | |
|---|---|---|---|
| Pretreatment | 12 months after treatment | ||
| Study (n = 30) | 8.2 ± 3.5 | 3.0 ± 2.8 | <0.001 |
| Control (n = 30) | 7.8 ± 3.8 | 4.3 ± 3.2 | <0.001 |
| p value | 0.845 | 0.030 | |
Table 4.
Between-group comparison of the Harris score at the affected hip and the hip joint function after treatment.
| Group | Harris score | Hip joint function |
|||
|---|---|---|---|---|---|
| Excellent | Good | Acceptable | Poor | ||
| Study (n = 30) | 81.12 ± 7.9 | 2 | 15 | 11 | 2 |
| Control (n = 30) | 81.62 ± 5.4 | 1 | 18 | 10 | 1 |
In both groups, patients had much higher post treatment OQOLS scores compared with baseline scores. After 12 months of treatment, the treatment group showed a higher OQOLS score than that of the control group (83.30 ± 9.4 vs 78.26 ± 9.8, p = 0.04, Table 5).
Table 5.
Comparison of the OQOLS scores before and 12 months after treatment between the two groups.
| Group | OQOLS score |
p value | |
|---|---|---|---|
| Before treatment | 12 months after treatment | ||
| Study (n = 30) | 45.65 ± 8.9 | 83.30 ± 9.4 | <0.001 |
| Control (n = 30) | 48.44 ± 10.8 | 78.26 ± 9.8 | <0.001 |
| p value | 0.762 | 0.040 | |
There was no significant difference in baseline BMDs of the lumbar and hip between the two groups before treatment. However, significant differences in the BMDs of the L1–4, the femoral neck and the greater trochanter were observed between the two groups after 12-month treatment, as well as a difference between the pre- and post-treatment BMDs in the treatment group (Table 6).
Table 6.
Comparison of the pretreatment and posttreatment BMDs between the two groups.
| Group | L1–4 |
Femoral neck |
Greater trochanter |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Before treatment | 12 months after treatment | p value | Before treatment | 12 months after treatment | p value | Before treatment | 12 months after treatment | p value | |
| Study (n = 30) | 0.79 ± 0.14 | 0.88 ± 0.16 | <0.001 | 0.65 ± 0.13 | 0.76 ± 0.14 | <0.001 | 0.54 ± 0.10 | 0.60 ± 0.14 | <0.001 |
| Control (n = 30) | 0.82 ± 0.12 | 0.84 ± 0.12 | 0.012 | 0.69 ± 0.11 | 0.70 ± 0.10 | =0.024 | 0.55 ± 0.12 | 0.57 ± 0.09 | 0.013 |
| p value | 0.524 | <0.001 | 0.784 | <0.001 | 0.846 | 0.001 | |||
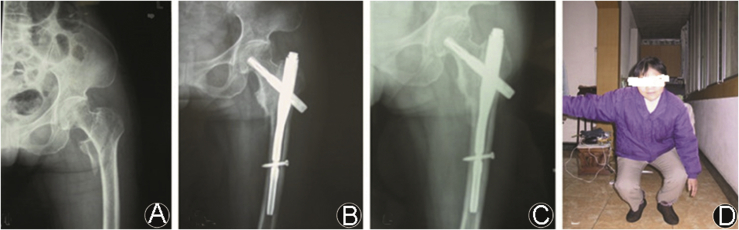
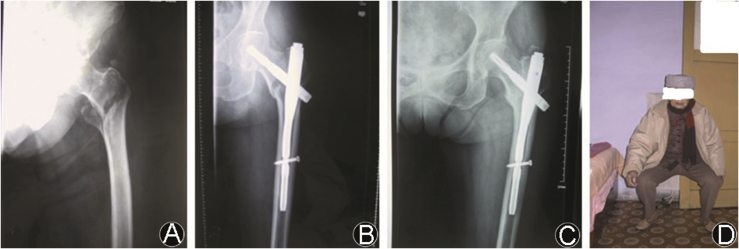
In both groups, there was no significant change in liver and kidney function after treatment. Among the 30 cases in the treatment group, four patients experienced fever, influenza, and headache symptoms. Emesis occurred in two patients and ceased after the patients took 5 mg of Metoclopramide intramuscularly and 10 mg of Metoclopramide (tid), orally for one day. After three-to-five months, the fractures healed for all the patients. The average healing time for the treatment group was (13 ± 3.2) weeks and for the control group was (15 ± 4.6) weeks (p = 0.02). No femoral head necrosis or coxavara was found during the follow-up period (Fig. 1, Fig. 2). During the 12-month follow-up, no new fractures were observed in the treatment group, whereas in the control group, four patients experienced a new fracture, including hip fracture in two cases, and distal radius fracture in two.
Fig. 1.
Pre- and post-treatment radiographs of the study group (A: pre-treatment; B: post-treatment; C: 12 months after treatment; and D: function recovery condition at 12 months after treatment).
Fig. 2.
Pre- and post-treatment radiographs of the control group (A: pre-treatment; B: post-treatment; C: 12 months after treatment; and D: function recovery condition at 12 months after treatment).
Discussion
Osteoporosis or osteoporotic fracture is one of the most common chronic diseases that jeopardize the health of elderly people.6 Among them, hormone levels reduce and exercise and nutrition intake decrease, which would give rise to the decrease in bone mass and to the deterioration of bone microarchitecture. As a result, these changes will result in diminished bone strength. The decrease in bone mass can be characterized by the corresponding decrease in osteogenesis and the relative surge of osteoclasts, leading to bone resorption more than bone formation. The deterioration of bone microstructure manifests in thinner, lighter, and sparser bone trabecula and microfracture.7 As a result of the poor mechanical character of bone ultrastructure, the mechanical strength of bone decreases and osteopsathyrosis increases, leading to poor load-bearing capacity, such that even a slight force can cause osteoporotic fractures.8 The most common osteoporotic fractures are hip fractures or distal radius fractures. Death related to osteoporotic hip fracture is high on the survey list of mortality rates among the elderly, second only to cardiovascular and cerebrovascular diseases and far beyond the mortality rate of cumulative malignancies.
Because of the high mortality and disability rates pertaining to hip fractures among the aged, in recent years treatment for osteoporotic hip fracture has intensified from more conservative treatment in the past to surgical intervention as early as possible. Such intervention can stabilize the fracture and enable patients to exercise as soon as possible, and hence reduce various complications that can greatly afflict long-term bedridden patients.9 Compared with conventional extramedullary fixation instruments, PFNA has been widely regarded as an ideal internal fixator for treating osteoporotic hip fracture of the aged. PFNA possesses a number of advantages, such as less trauma, firmer fixation, and being more amenable to counter-rotation and resistant to breakage. In this study, PFNA was used as the internal fixator in both groups, and at the end of the follow-up period, bone union was achieved in all patients with no internal fixation failure. This result is similar to the reports by other researchers.10 No significant differences in the Harris scores of the affected hip were found between the two groups during this study period, which may be attributed to the following reasons: (1) the same surgical team conducted the surgical intervention for all patients, and all patients received the same internal fixator; (2) all patients' rehabilitation program and rehabilitation exercises were performed and supervised by the same rehabilitation team. These outcomes have reminded us that the achievement of better hip joint function after surgery in patients with osteoporotic hip fracture is more related to the surgical method employed, the type of internal fixator used and the rehabilitation after surgery than to the type of anti-osteoporosis therapy.
Due to bone pain, elderly patients with osteoporosis usually experience limited functional activity, diminished physical function, and decreased ability of self-care. These factors often cause anxiety of the patients and bring a burden on their family. This study showed that quality of life significantly improved after conducting surgical intervention at an early stage, in which the study group exhibited more obvious improvements.
Bisphosphonates have been considered to be the most promising medicine for osteoporosis. They exhibited a much stronger ability to extinguish synthetase of farnesyl pyrophosphate because the heterocycle structure can make zoledronic acid bind with the hydroxyapatite more easily on the bone surface.11 This study found that patients with osteoporosis treated with zoledronic acid achieved greater improvement in BMD and more reduction in bone pain compared to the controls. For patients taking zoledronic acid, the incidences of new fractures of the hip and vertebra as well as non-vertebra fractures were 1.44%, 0.53%, and 7.97%, respectively, whereas for the placebo group the rates were 2.49%, 2.59% and 10.71%, respectively. So, the risks of relative fracture in the study group decreased by 41%, 71%, and 25%, respectively.12 Likewise, Black et al13 found that the risks of vertebra fracture and hip fracture decreased by 70% and 41%, respectively in women with osteoporosis who received zoledronic acid treatment for 3 years. In this study, no new fractures were found in the study group, whereas four were observed in the control group. This result is consistent with those of other researchers, which suggests that zoledronic acid can suppress bone resorption, increase bone formation, facilitate bone trabecula reconstruction and improve the mechanical property of bone ultrastructure, ultimately increase bone strength and decrease the incidence of new fractures.
Despite many advantages of zoledronic acid, we should also note the following problems: (1) Before injection, we need to assure that the patients' creatinine clearance and serum calcium reach the treatment standard and take care of kidney damage and hypocalcemia. (2) Before and after using zoledronic acid, large amounts of normal saline and analgesic-antipyretic should be given, which can diminish the incidence of influenza-like symptoms such as fever, headache, sore muscles, and vomiting.
Zoledronic acid can inhibit bone absorption and facilitate bone formation and, when combined with PFNA internal fixation, can more effectively relieve bone pain in the elderly with osteoporosis intertrochanteric fracture. It also can increase BMD, improve quality of life, reduce the occurrence of new fractures and facilitate fracture healing.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Gorai I., Hattori S., Tanaka Y. Alfacalcidol-supplemented raloxifene therapy has greater bone-sparing effect than raloxifene-alone therapy in postmenopausal Japanese women with osteoporosis or osteopenia. J Bone Min Meta. 2012;20:349–358. doi: 10.1007/s00774-011-0325-1. [DOI] [PubMed] [Google Scholar]
- 2.Lian C.G., Li W.Q., He J. The current situation about osteoporosis hip fracture. Chin J Osteoporos. 2008;14:217–219. [Google Scholar]
- 3.Osteoporosis Diagnostic Criteria Group of Osteoporosis Committee of the Gerontological Society of China Criteria for the diagnosis of primary osteoporosis in China. Chin J Osteoporos. 1999;5:2–3. [Google Scholar]
- 4.Jensen J.S., Michaelsen M. Trochanteric femoral fractures treated with McLaughlin osteosynthesis. Acta Orthop Scand. 1975;46:795–803. doi: 10.3109/17453677508989266. [DOI] [PubMed] [Google Scholar]
- 5.Cai T.S., Liu J., Wu P.L. Development of osteoporosis quality of life scale and item selection. Chin J Behav Med Sci. 2004;13:221–222. [Google Scholar]
- 6.Wu H.W., Meng X.W. We should pay more attention on the study of osteoporosis. Natl Med J China. 1992;72:959. [Google Scholar]
- 7.ShengZhong M., Dongjin W., Shiqing W. Modification of percutaneous vertebroplasty for painful old osteoporotic vertebral compression fracture in the elderly: preliminary report. Injury. 2012;43:486–489. doi: 10.1016/j.injury.2011.12.021. [DOI] [PubMed] [Google Scholar]
- 8.Ringe J.D. Questions on the superiority of alfacalcidol over plain vitamin D in the treatment of glucocorticoid-induced osteoporosis. Rheumatol Int. 2004;24:370. doi: 10.1007/s00296-004-0523-4. [DOI] [PubMed] [Google Scholar]
- 9.Han F., Wang J., Kuang J. Risk analysis of severe diabetic senile patients with hip fracture. Chin J Bone Tumor & Bone Dis. 2009;8:223–225. [Google Scholar]
- 10.Takiqami I., Matsumoto K., Ohara A. Treatment of trochanteric fractures with the PFNA (proximal femoral nail antirotation) nail system-report of early results. Bull NYU Hosp Jt Dis. 2008;66:276–279. [PubMed] [Google Scholar]
- 11.Nancollas G.H., Tang R., Phipps R.J. Novel insights into actions of bisphosphonates on bone: differences in interactions with hydroxyapatite. Bone. 2006;38:617–627. doi: 10.1016/j.bone.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 12.Dunford J.E., Thompson K., Coxon F.P. Structure-activity relationships for inhibition of farnesyl diphosphate synthase in vitro and inhibition of bone resorption in vivo by nitrogen-containing bisphosphonates. J Pharmacol Exp Ther. 2001;96:235–242. [PubMed] [Google Scholar]
- 13.Black D.M., Delmas P.D., Eastell R. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356:1809–1822. doi: 10.1056/NEJMoa067312. [DOI] [PubMed] [Google Scholar]