Abstract
Purpose
Tension band wiring is commonly used for fixation of simple transverse fractures. The popular configuration is parallel Kirschner wires (K-wires) and a stainless steel wire loop placed in a vertically oriented figure-of-8.
Methods
We used a wooden model of a patella with a midway transverse fracture and compared four different types of fixation. The first construct had a vertical figure-of-8 with one twist of wire. The second contained a vertical figure-of-8 with two twists of wire. The third was a vertical figure-of-8 with two twists of wire placed at adjacent corners while the last one had a horizontal figure-of-8 with two twists of wire placed at adjacent corners. Interfragmentary compression at the point of wire breakage was measured for each construct as well as permanent displacement on cyclic loading.
Results
Placement of the figure-of-eight in a horizontal orientation with two wire twists at the corner improved interfragmentary compression by 63% (p < 0.05, Tukey post hoc test). On cyclic loading, all the constructs with vertical figure-of-eight but none with a horizontal construct failed (p = 0.01; Fisher's exact test). Permanent fracture displacement after cyclic loading was 67% lower with horizontal figure-of-eight constructs (p < 0.05; t test).
Conclusion
Placing wire twists at the corner and a horizontal placement of figure-of-8 improves stability of the construct.
Keywords: Patella transverse fractures, Tension band wiring, Biomechanical analysis
Introduction
Patella fractures comprise 1% of all fractures encountered in the emergency department, and about 30% of them require surgical intervention.1 Tension band wiring (TBW) of patella is one of the most common and popular methods of fixation, specially for simple mid-pole patella fractures.2 Fixation of patellar fractures is very crucial as it allows early mobilisation of the knee without detrimental displacement at the fracture site.3 Displacement of more than 2 mm in 22% of the fractures after early mobilisation using TBW technique popularised by the Arbeitsgemeinschaft für Osteosynthesefragen (AO group) has been reported.4 Some studies reported re-operation rates between 20% and 56% following the use of Kirschner wires (K-wires).5, 6, 7, 8, 9 Errors in technique and failure by patients to act in accordance with postoperative mobilisation protocol were reported to be the reasons for these failures. It would be understandable to most surgeons that, in order to reduce the risk of displacement or failure, a construct that produces the greatest interfragmentary compression and has the maximum stiffness to resist cyclic loads should be used. This in turn would allow early mobilisation of the knee after fracture fixation.
TBW technique popularised by the AO group involves the use of two K-wires (1.6 mm) placed parallel to each other and an anterior tension band of stainless steel wire in a vertically oriented figure-of-8 pattern (Fig. 1A and B).10 This configuration resulted in the smallest displacement at the fracture site, when compared with other fixation constructs.11
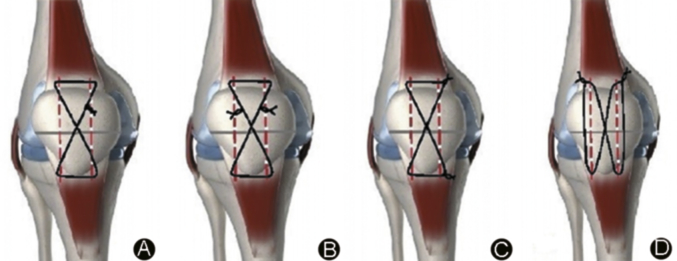
Fig. 1.
Configurations of stainless steel wire loops.
It has been noticed that the site of placement of the wire twists by the surgeon to tighten the loop is done in an arbitrary manner. There is also a view prevailing that using two twists of wires reduces the strength of fixation.12 These observations prompted us to investigate the effects of: increasing the loops of SS wire, increasing the diameter of SS wire, using a transversely oriented loop of wire, placing the twists at corners of the wire loop and using an additional strand of wire on interfragmentary compression and resistance to cyclic loading.
Hypothesis
-
1)
Compared to one loop of wire, two loops of wire should produce greater interfragmentary compression and resistance to cyclic loading.
-
2)
Compared to a wire loop of smaller diameter, a wire loop of larger diameter should produce greater interfragmentary compression and resistance to cyclic loading.
-
3)
Compared to two arbitrarily placed twists, placing two twists of wires at the corners of the figure-of-8 construct increases interfragmentary compression.
-
4)
Compared to a vertically oriented figure-of-8 configuration, placing the figure-of-8 horizontally increases interfragmentary compression and resistance to cyclic loading.
Materials and methods
A wooden model of patella with a midway transverse fracture was used. Two-mm drill holes were made for placement of 1.6 mm K-wires. These holes were large enough to allow easy gliding of the K-wires and ensured identical placement of the K-wires for each experiment. A 25.4 mm diameter × 3.8 mm thick load transducer (ELW-D1, Entran Ltd, Watford, UK) was placed between the fragments in a slot to ensure that its position would be identical at each experiment. Data from the load cell were read into a personal computer. Stainless steel wire (Aesculap, Tuttlingen, Germany) was used to compress the fracture site. The four configurations tested are represented in Fig. 1.6
-
1)
Vertical figure-of-8 with 1 twist of wire (Fig. 1A).
-
2)
Vertical figure-of-8 with 2 twists of wire (Fig. 1B).
-
3)
Vertical figure-of-8 with 2 twists of wire placed at adjacent corners (Fig. 1C).
-
4)
Horizontal figure-of-8 with 2 twists of wire placed at adjacent corners (Fig. 1D). Stainless steel wire of different diameters (0.70 mm, 1.00 mm, 1.20 mm) with either one or two loops were used to compress the fracture site and check for displacement on cyclic loading, using the configuration in Fig. 1D.
Interfragmentary compression
For each of the investigation, K-wires were placed in the pre-drilled holes and appropriate lengths of stainless steel wire were bent around them and twisted, while measuring interfragmentary compression. When two twists were used, they were twisted in an alternating manner to ensure that each wire length was tensioned uniformly and equally. Measurements were stopped at wire failure. For each configuration five samples were tested. Using configuration in Fig. 1D, five samples each were tested for wire diameters of 0.70 mm, 1.00 mm and 1.20 mm respectively. The same was done using 2 strands of 0.70 mm SS wire.
Cyclic loading
Configurations 3 and 4 (vertical figure-of-8 and transverse figure-of-8, both with two twists placed at adjacent corners) were each subjected to a cyclic loading test. For the cyclic loading test, all the four samples were prepared in the above manner. Wires were twisted until the interfragmentary compression force was half the average maximum interfragmentary compression force of the configuration. The configuration in Fig 1D was then used to prepare samples using the different diameters of SS wire (0.70 mm, 1.00 mm and 1.20 mm). Samples using 2 strands of wires were prepared similarly. The samples were then placed in a material testing machine (ESH Testing Ltd, Brierley Hill, UK) and loaded using a 3-point bending test. Twenty-five cycles were applied of 150 N, 300 N and 450 N (corresponding to bending moments of 7.7 Nm, 15.4 Nm and 23.1 Nm), while measuring applied force and resulting displacement using the testing machine's built-in transducers.
Statistical analysis
For interfragmentary compression, forces were compared between the four configurations using One-Way ANOVA followed by the Tukey post-hoc test. For the cyclic loading test, permanent displacement after 25 cycles at each load level was compared using Student's t-test. In all the cases, a p value of 0.05 was assumed to denote statistical significance. All statistical analyses were performed using SYSTAT Version 11 (Systat Software Inc, Point Richmond, USA).
Results
Interfragmentary compression
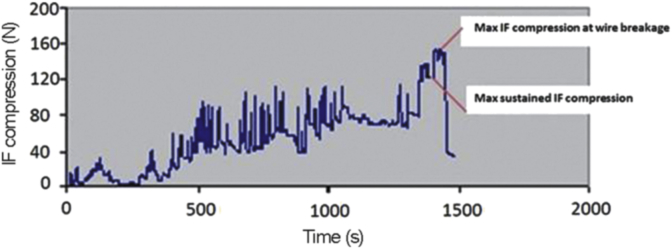
The pattern of interfragmentary compression (Fig. 2) revealed that the maximum compression achieved for every twist of wire was not maintained; it settled into a lower value (sustained compression) which was higher than the level after the previous twist. The sustained values after each twist are more representative of values achievable in clinical practice.6 The values of maximum and the sustained interfragmentary compression were used to compare the various groups.
-
1.
Number of twists: When two twists of wire were used instead of one, the compression increased by nearly 12%. It is important to point out that the second twist was placed at an arbitrary point along the figure-of-8 (Table 1).
-
2.
Site of wire twists: There was an additional advantage in placing the two twists at adjacent corners, which increased the compression by a further 18% (Table 1).
-
3.
Orientation of figure-of-8: The investigations revealed an improvement in interfragmentary compression when the figure-of-8 was placed horizontally as opposed to vertically (traditional configuration). The placement of the figure-of-8 in a horizontal configuration increased compression by 67%, implying that this configuration (Fig. 1D) was significantly stronger than all other configurations (p < 0.05).
-
4.
Diameter of stainless steel wire loop: Increasing the diameter of the figure-of-8 loop improved values for both the maximum and sustained interfragmentary compression. The improvement was statistically significant (p = 0.002, Table 2). Although increasing the diameter of the figure-of-8 loop from 1.0 mm to 1.20 mm resulted in an improvement in interfragmentary compression, this did not reach statistical significance (p > 0.05).
-
5.
Two strands of wire in the figure-of-8 loop: On adding an extra strand of 0.7 mm wire loop, the maximum interfragmentary compression achieved improve significantly (p = 0.005).
Fig. 2.
Pattern of interfragmentary compression. Note: IF compression = interfragmentary compression.
Table 1.
Sustained interfragmentary compression for each group tested. Differences between groups were significant (p = 0.005, One-Way ANOVA), with the horizontal configuration producing greater compression than all other configurations (p < 0.05, Tukey post-hoc test).
| Groups | Compression | SD |
|---|---|---|
| Vertical 1 twist | 79.5 | 22.5 |
| Vertical 2 twists | 88.8 | 39 |
| Vertical 2 twists corner | 104.8 | 27.2 |
| Horizontal 2 twists corner | 171.1 | 33.3 |
Table 2.
Maximum and sustained interfragmentary compression produced with wire loops of different diameters and 2 wire strands in the figure-of-8 loop.
| Diameter (mm) | Max IF compression (N) | SD | Sustained IF compression (N) | SD |
|---|---|---|---|---|
| SS Wire 1.20 | 351.6998 | 33.62372 | 234.9342 | 19.91627 |
| SS Wire 1.00 | 290.4077 | 35.88125 | 222.9845 | 23.67119 |
| SS Wire 0.70 | 205.9122 | 20.40038 | 164.313 | 33.32085 |
| SS 0.70 (2 strands) | 260.1403 | 24.48924 | 192.5469 | 28.43786 |
Displacement on cyclic loading
-
1.
Orientation of Figure-of-8: The cyclic loading tests revealed a difference between the two groups tested, as all the vertical figure-of-8 loop (traditional configuration) specimens failed at 15.4 Nm, while all specimens fixed using the horizontal configuration (Fig. 1D) survived up to 23.1 Nm (Table 3). The average fracture displacement of the samples fixed with the vertical configuration was 64.5% more than that of the samples fixed with the horizontal configuration, a significant difference (p < 0.05).
-
2.
Diameter of stainless steel wire loop: Increasing the diameter of the SS wire used to make the figure-of-8 loop decreased the final permanent displacement after cyclic loading at 2.31 Nm significantly (p = 0.002). The difference in displacement between 1.20 mm wire group and 1.00 mm group was marginal (p = 0.06). It was interesting to note that the SD in the 1.20 mm group was larger than the 1.00 mm group, suggesting that the tension through thicker wire loop was not uniform between samples (Table 4).
-
3.
Two strands of wire in the figure-of-8 loop: On using a second strand of 0.7 mm SS wire, the permanent displacement at cyclic loads of 2.31 Nm decreased significantly compared to figure-of-8 loop with a single strand (p = 0.02). The 0.7 mm wire loop was used in preference to the thicker wire strands for its ease of handling when the second strand was added.
Table 3.
Displacement on cyclic loading tests.
| Load level (Nm) | Sample |
Average | SD | ||||
|---|---|---|---|---|---|---|---|
| No.1 | No.2 | No.3 | No.4 | No.5 | |||
| Vertical configuration | |||||||
| 7.7 | 5.1 | 4 | 6.4 | 4.6 | 5.4 | 5.1 | 1.23 |
| 15.4 | Failed | Failed | Failed | Failed | Failed | ||
| Horizontal configuration | |||||||
| 7.7 | 3.9 | 2.1 | 2.7 | 3.2 | 3.5 | 3.1 | 0.79 |
| 15.4 | 6.1 | 2.2 | 4.4 | 5 | 5.3 | 4.6 | 1.61 |
| 23.1 | 16.7 | 12.2 | 6.8 | 15.9 | 12.4 | 12.8 | 4.46 |
Table 4.
Final displacement on cyclic loading of 2.31 Nm with different diameters of SS wire and 2 strands.
| Diameter (mm) | Count | Average displacement (mm) | SD |
|---|---|---|---|
| SS Wire 1.20 | 5 | 6.3084 | 0.69547 |
| SS Wire 1.00 | 5 | 7.0652 | 0.305219 |
| SS Wire 0.70 | 5 | 13.9405 | 4.750136 |
| SS 0.70 (2 strands) | 5 | 5.6666 | 1.010377 |
Discussion
The patella is susceptible to injury from a direct blow as a result of its anterior location and thin overlying soft tissue covering. Fractures of the patella may result from direct, indirect, or combined injury patterns.13 In reality, patellar fractures could signify a mixture of both direct and indirect forces: the culmination of a direct blow, quadriceps muscle contraction, and secondary joint collapse. The preponderance of patellar fractures has a transverse fracture pattern as a consequence of the disproportionate tensile forces through the extensor mechanism.3
The transverse fractures of patella after fixation are subject to forces that act at the fracture site either in distraction due to the action of the quadriceps in extension or three-point bending that takes place on flexion of the knee. Tension band principles are successfully applied only if three-point bending is achieved by flexing the knee.
This study showed that the interfragmentary compression and permanent displacement at the fracture site on cyclic loading can be improved significantly by making variations in the traditional wiring construct. We have also quantified the improvements that can be achieved by each individual variation in isolation.
Although greater interfragmentary compression is accepted to help improve bone healing at fracture site, it is also a measure of the resistance to displacement at fracture site that may be caused by distraction forces generated by the quadriceps contraction in extension.
The increase in interfragmentary compression achieved by placing two points of twists on the loop of stainless steel wire (double twist technique) has been reported previously.14 Although it is widely accepted that double twist technique helps the surgeon achieve better control of both lengths of wire, previous investigations have showed a loss of strength of nearly 25%.12 Our investigation did not reveal a statistically significant improvement with the double twist technique, but certainly did not show deterioration in fixation strength. The improvement achieved by placing the twists at the corners and placing the figure-of-8 loop horizontally was reported by the authors in a previous paper.15
Increasing the diameter of the figure-of-8 wire loop in order to increase the interfragmentary compression is intuitive and is a practice resorted to by many surgeons. The authors have noticed a variation in preference between surgeons in the use of 1.20 mm SS wire or 1.00 mm SS wire. Any wire diameter larger than the 1.2 mm (16 gauge) is perceived to be difficult to handle. The interfragmentary compression and resistance to cyclic loading improved significantly with the increasing diameter of the figure-of-8 loop (0.70 mm, 1.00 mm and 1.20 mm). Interestingly the differences between the 1.00 mm group and 1.2 mm group were not statistically significant both for interfragmentary compression and displacement on cyclic loading at 23.1 Nm. Moreover the final displacements after cyclic loading showed a greater variation for the 1.20 mm group (SD 0.70) as compared to the 1.00 mm group (SD 0.31). This reinforced our experience that it is harder to achieve uniform tension when using the thicker wire prior to cyclic loading. The 1.00 mm wire appears to achieve a similar interfragmentary compression and displacement on cyclic loading as the 1.20 mm wire loop without the problems of non-uniform tension or laxity more reliably.
Increasing the number of strands to increase the interfragmentary compression is intuitive. The potential problem is that achieving uniform and nearly equal tension in both strands is difficult to replicate. The use of 0.70 mm SS wire offset this problem at least for the purposes of this investigation. The interfragmentary compression achieved at wire breakage and the displacement on cyclic loading was significantly improved by the addition of the second strand. The double stranded loop of 0.70 mm wire did not achieve the same level of interfragmentary compression or resistance to cyclic loading when compared to 1.00 mm wire. The use of a double stranded loop of 1.00 mm wire is an attractive proposition at the time of surgery.
It was noticed that during the investigation the stainless steel wire used elongates prior to failure. This elongation has been reported to be approximately 50% prior to fracture. Fatigue failure of stainless steel wire is one aspect that was not investigated. It is well established that notching of wires during handling with instruments harder than 316 L stainless steel decreases the fatigue life. It has been shown by previous investigators that a notch of 1% of diameter can reduce fatigue life by 63%.16 In this investigation we used the same instruments used at the time of surgery and did not have failures for the specific number of cycles tested, which can be attributed to fatigue failure.
Although in this study we used stainless steel wire, the improvements in principle may be used, even when nonmetallic sutures are used. Nonmetallic sutures are in vogue with some surgeons for their obvious advantages of preventing metallic implant-related problems like skin irritation which might necessitate implant removal.14, 17 Increasing the diameter of the material, the number of strands and orientation of the figure-of-8 loop is likely to improve the interfragmentary compression and resistance to cyclic loading regardless of the material used in the fixation construct.
Most reports in the literature, except a previous report by the authors15 have used cadaveric patellae. The confounding influences that may arise from the variation in the trabecular architecture of the cadaveric patellae18 can be considerable and probably explain why previous investigations of patellar fixation on cadaveric patellae have reported wide variations to the extent of drawing opposite conclusions.19, 20, 21 The advantages of the wooden model of a patella used in this investigation were highlighted in our previous report.15 It did not deform around the load transducer and allowed accurate measurement of the interfragmentary compression, both of which would have been difficult with cadaveric patellae.
In conclusion, the TBW construct for transverse fractures of the patellae may be improved by
-
1)
Placing two twists at corners rather than in an arbitrary fashion.
-
2)
Placing the figure-of-8 loop in transverse orientation.
-
3)
Increasing the diameter of the wire used to make the figure-of-8 loop. Our investigation revealed 1.00 mm SS wire to be ideal as it achieves comparable compression and resistance to cyclic loading as the 1.2 mm wire, without suffering from the problems of nonuniform tension.
-
4)
Increasing the number of strands in the figure-of-8 loop. Additional strand significantly increased the compression and resistance to cyclic loads.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Scilaris T.A., Grantham J.L., Prayson M.J. Biomechanical comparison of fixation methods in transverse patella fractures. J Orthop Trauma. 1998;12:356–359. doi: 10.1097/00005131-199806000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Egol K., Howard D., Monroy A. Patella fracture fixation with suture and wire: you reap what you sew. Iowa Orthop J. 2014;34:63–67. [PMC free article] [PubMed] [Google Scholar]
- 3.Lotke P.A., Ecker M.L. Transverse fractures of the patella. Clin Orthop Relat Res. 1981;158:180–184. [PubMed] [Google Scholar]
- 4.Smith S.T., Cramer K.E., Karges D.E. Early complications in the operative treatment of patella fractures. J Orthop Trauma. 1997;11:183–187. doi: 10.1097/00005131-199704000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Gosal H.S., Singh P., Field R.E. Clinical experience of patellar fracture fixation using metal wire or non-absorbable polyester–a study of 37 cases. Injury. 2001;32:129–135. doi: 10.1016/s0020-1383(00)00170-4. [DOI] [PubMed] [Google Scholar]
- 6.Tian Y., Zhou F., Ji H. Cannulated screw and cable are superior to modified tension band in the treatment of transverse patella fractures. Clin Orthop Relat Res. 2011;469:3429–3435. doi: 10.1007/s11999-011-1913-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hung L.K., Lee S.Y., Leung K.S. Partial patellectomy for patellar fracture: tension band wiring and early mobilization. J Orthop Trauma. 1993;7:252–260. doi: 10.1097/00005131-199306000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Hung L.K., Chan K.M., Chow Y.N. Fractured patella: operative treatment using the tension band principle. Injury. 1985;16:343–347. doi: 10.1016/0020-1383(85)90144-5. [DOI] [PubMed] [Google Scholar]
- 9.LeBrun C.T., Langford J.R., Sagi H.C. Functional outcomes after operatively treated patella fractures. J Orthop Trauma. 2012;26:422–426. doi: 10.1097/BOT.0b013e318228c1a1. [DOI] [PubMed] [Google Scholar]
- 10.Muller M.E., Algöwer M., Schneider R. 3rd ed. Springer-Verlag; Berlin: 1990. Manual of Internal Fixation. [Google Scholar]
- 11.Weber M.J., Janecki C.J., Mcleod P. Efficacy of various forms of fixation of transverse fractures of the patella. J Bone Jt Surg Am. 1980;62:215–220. [PubMed] [Google Scholar]
- 12.Guadagni J.R., Drummond D.S. Strength of surgical wire fixation. A laboratory study. Clin Orthop Relat Res. 1986;209:176–181. [PubMed] [Google Scholar]
- 13.Melvin J.S., Karunakar M.A. Patella fractures and extensor mechanism injuries. AAOS Annu Meet. 2015;54:2–3. [Google Scholar]
- 14.Patel V.R., Parks B.G., Wang Y. Fixation of patella fractures with braided polyester suture: a biomechanical study. Injury. 2000;31:1–6. doi: 10.1016/s0020-1383(99)00190-4. [DOI] [PubMed] [Google Scholar]
- 15.John J., Wagner W.W., Kuiper J.H. Tension-band wiring of patella. The effect of site of wire twists and orientation of stainless steel wire loop: a biomechanical investigation. Int Orthop. 2007;31:703–707. doi: 10.1007/s00264-006-0238-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oh I., Sander T.W., Treharne R.W. The fatigue resistance of orthopaedic wire. Clin Orthop Relat Res. 1985;192:228–236. [PubMed] [Google Scholar]
- 17.Chen A., Hou C., Bao J. Comparison of biodegradable and metallic tension-band fixation for patella fractures. 38 patients followed for 2 years. Acta Orthop Scand. 1998;69:39–42. doi: 10.3109/17453679809002354. [DOI] [PubMed] [Google Scholar]
- 18.Toumi H., Higashiyama I., Suzuki D. Regional variations in human patellar trabecular architecture and the structure of the proximal patellar tendon enthesis. J Anat. 2006;208:47–57. doi: 10.1111/j.1469-7580.2006.00501.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Benjamin J., Bried J., Dohm M. Biomechanical evaluation of various forms of fixation of patella. J Orthop Trauma. 1987;1:219–222. doi: 10.1097/00005131-198701030-00004. [DOI] [PubMed] [Google Scholar]
- 20.Carpenter J.E., Kasman R.A., Patel N. Biomechanical evaluation of current patella fracture fixation techniques. J Orthop Trauma. 1997;11:351–356. doi: 10.1097/00005131-199707000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Weber M.J., Janecki C.J., McLeod P. Efficacy of various forms of fixation of transverse fractures of the patella. J Bone Jt Surg Am. 1980;62:215–220. [PubMed] [Google Scholar]