Abstract
Purpose
Tibial pilon fractures remain challenging for an orthopaedic surgeon to repair. External fixation (ExFix) and open reduction and internal fixation (ORIF) are two widely used methods for repairing tibial pilon fractures. However, conclusions of comparative studies regarding which method is superior are controversial. Our aim is to compare ORIF and ExFix and clarify which method is better in terms of reduction and union results and major complications.
Methods
A computerized research of MEDLINE, EMBASE, Springer, and Cochrane Library (before December 2014) for studies of any design comparing ORIF and ExFix was conducted. Weighted mean difference (WMD), risk ratio (RR) and corresponding 95% confidence intervals (CI) were used for estimating the effects of the two methods. Statistical analyses were done using Review Manager Version 5.2.
Results
Ten cohort studies and one randomized clinical trial were included in our ultimate analysis. And the analysis found no significant difference between the two methods in deep infection (p = 0.13), reduction (p = 0.11), clinical evaluation (p = 0.82), post-traumatic arthrosis (p = 0.87), and union time (p = 0.35). Besides, ExFix group was found to have a higher rate of superficial infection (p = 0.001), malunion (p = 0.01) and nonunion (p = 0.02), but have a lower risk of unplanned hardware removal (p = 0.0002).
Conclusions
We suggest that ORIF has a relatively lower incidence rate of superficial infection, malunion and nonunion, but a higher rate of unplanned hardware removal. No difference was found in deep infection, reduction, clinical evaluation, post-traumatic arthrosis and union time.
Keywords: Fractures, bone; Fracture fixation, internal; External fixation; Meta-analysis
Introduction
The incidence of tibial pilon fractures is increasing following the rise of the incidence of road traffic accidents.1, 2 Repairing pilon fractures remain challenging for orthopedic surgeons. Over the past years, a wide variety of treatment strategies for these fractures emerged and developed, which include nonoperative management, open reduction and internal fixation (ORIF), external fixation (ExFix), and minimally invasive treatments.3, 4 ORIF and ExFix are two methods frequently reported in the literature. ORIF can restore the anatomic structure of the bone, but it cannot avoid dissecting soft tissues which associate with recovery.5 On the other hand, ExFix allows indirect reduction but causes less soft tissues damage. However, a few studies conclude that ExFix is associated with high rates of malunion and nonunion.6, 7 Different authors have compared ORIF and ExFix from different aspects, but the clinical outcomes are still controversial. We searched for all the nonrandomized prospective or retrospective studies or randomized clinical trials comparing the clinical outcomes between ORIF and ExFix for tibial pilon fractures. The aim of this systematic review and meta-analysis is to compare ORIF and ExFix and clarify which method is better in terms of reduction score and major complications, including infection, malunion, nonunion and arthrosis.
Materials and methods
Search strategy
We searched MEDLINE, EMBASE, Springer, Cochrane Library to retrieve related studies published before December 2013 with combinations of keywords “tibia pylon/plafond”, “fracture?”, “ExFix”, “internal fixation”, “ORIF” and “comparative study”. The language was restricted to English. We also scanned the citation lists of the identified articles for additional relevant studies.
Eligibility
Studies were included if they met the following criteria: (1) randomized, quasi-randomized, prospective and retrospective cohort and case-control studies; (2) patients with tibial pilon fractures of type 43A, 43B, 43C according to the AO/OTA classification; (3) patients aged 18 years or older; (4) comparison of ORIF and ExFix for treatment; (5) outcomes of interest adequately reported for meta-analysis.
Data extraction and study quality assessment
Full texts were read and relevant data were extracted from each included study by the two authors independently using a data extraction form. The information extracted from each study included the first author, year, country, research type, patients' number. Outcomes of interest we extracted included the incidence of complications, the union time and unplanned hardware removal. After the first extraction, the data were rechecked by the two authors.
The quality of the included studies was assessed by the two independent observers, using the Downs and Black checklist for both randomized and nonrandomized studies.8 For the Downs and Black checklist, 27 questions were raised to assess reporting, external validity, internal validity-bias, internal validity-confounding, and power. This checklist is considered a reliable and valid tool to assess the methodological quality of studies, which has a total score of 31. Scores above 20 were considered high methodological quality; 11–20 moderate quality; and below 11 poor quality.
Statistical analysis
Statistical analyses were done using Review Manager Version 5.2 (Cochrane Collaboration, Software Update, Oxford). We analyzed the risk ratio (RR) with 95% confidence intervals (CI) for dichotomous variables and the weighted mean difference (WMD) with the 95% CI for continuous variables. I-squared (I2) statistic was used to assess statistical heterogeneity among studies and I2 > 50% reflects high heterogeneity.9 Both fixed-effects and random-effects models were used to pool the data. The random-effects model was used only when heterogeneity was significant. p-values less than 0.05 are considered statistically significant.
Results
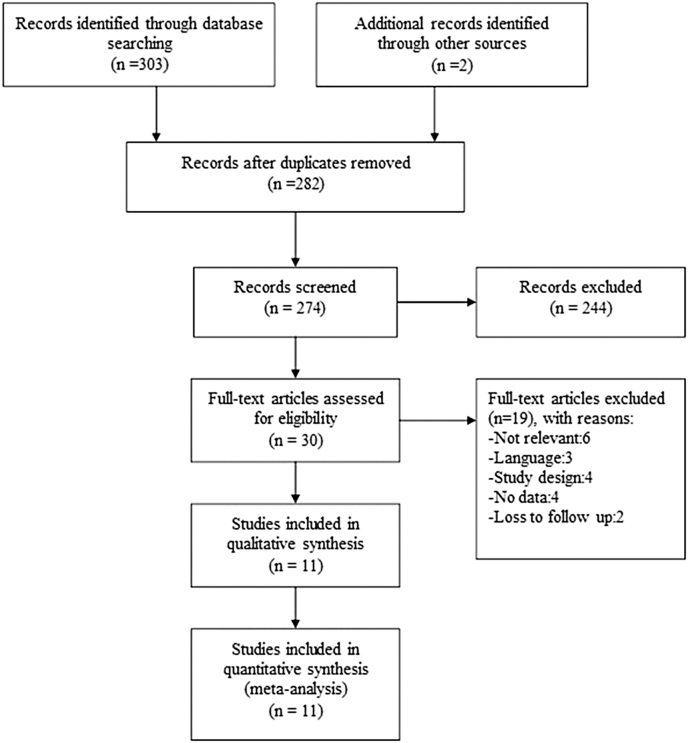
A total of eleven studies,7, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19 compared ORIF and ExFix for tibial pilon fractures and published between 1993 and 2013, fulfilled our inclusion criteria. Fig. 1 provides a flow diagram of the search results. These studies included 502 participants, of which 238 (47.4%) underwent ExFix and 264 (52.6%) underwent ORIF. The study consisted of ten retrospective or prospective nonrandomized studies and one randomized clinical trial. Results of quality assessment with the Downs and Black checklist are shown in Table 1. Total scores were on average 16.3 points. Ten of eleven studies were of moderate methodological quality, while one of poor quality. All eleven studies were of low power due to small intervention group sizes. A summary of meta-analysis results is shown in Table 2.
Fig. 1.
Flow chart of screening studies comparing ORIF and ExFix.
Table 1.
Methodological quality assessment of included studies based on the Downs and Black checklist.
| First author, year | Reporting 0–10 |
External validity 0–3 |
Bias 0–7 |
Confounding 0–6 |
Power 0–5 |
Total 0–31 |
|---|---|---|---|---|---|---|
| Bonar,10 1993 | 5 | 1 | 2 | 2 | 0 | 10 |
| Crutchfield,11 1995 | 7 | 2 | 4 | 3 | 0 | 16 |
| Wyrsch,12 1996 | 8 | 1 | 5 | 4 | 0 | 18 |
| Anglen,13 1999 | 9 | 1 | 4 | 2 | 0 | 16 |
| Pugh,14 1999 | 7 | 2 | 4 | 2 | 0 | 15 |
| Bocchi,19 2000 | 7 | 1 | 5 | 3 | 0 | 16 |
| Watson,15 2000 | 9 | 1 | 4 | 3 | 0 | 17 |
| Harris,7 2006 | 9 | 2 | 4 | 2 | 0 | 17 |
| Koulouvaris,16 2007 | 9 | 2 | 5 | 3 | 0 | 19 |
| Bacon,17 2008 | 8 | 1 | 4 | 3 | 0 | 16 |
| Richards,18 2012 | 10 | 2 | 4 | 3 | 0 | 19 |
| Mean (SD) | 8 (1.4) | 1.5 (0.5) | 4.1 (0.8) | 2.7 (0.6) | 0.0 (0.0) | 16.3 (2.5) |
Table 2.
Summary of meta-analysis of ORIF versus ExFix.
| Items | Test for heterogeneity |
Analysis model | Test for overall effect |
RR or WMD 95% CI | ||
|---|---|---|---|---|---|---|
| I2 | p | Z | p | |||
| Superficial infection | 0% | 0.46 | Fixed | 3.23 | 0.001 | 2.71 (1.48,4.97) |
| Deep infection | 31% | 0.16 | Fixed | 1.51 | 0.13 | 0.65 (0.37,1.14) |
| Reduction | 0% | 0.50 | Fixed | 1.60 | 0.11 | 0.89 (0.76,1.03) |
| Arthrosis | 13% | 0.33 | Fixed | 0.16 | 0.87 | 0.98 (0.79,1.23) |
| Malunion | 0% | 0.93 | Fixed | 2.44 | 0.01 | 2.85(1.23,6.60) |
| Nonunion | 33% | 0.19 | Fixed | 2.24 | 0.02 | 2.09 (1.10,3.98) |
| Hardware removal | 0% | 0.73 | Fixed | 3.71 | 0.0002 | 0.12 (0.04,0.37) |
| Union time | 70% | 0.04 | Random | 0.93 | 0.35 | 4.35 (−4.80,13.50) |
| Clinical evaluation | 36% | 0.21 | Fixed | 0.23 | 0.82 | 1.03 (0.82,1.28) |
Abbreviations: ExFix, external fixation; ORIF, open reduction and internal fixation; RR, risk ratio; WMD, weighted mean difference; CI, confidence interval.
Postoperative complications
Infection
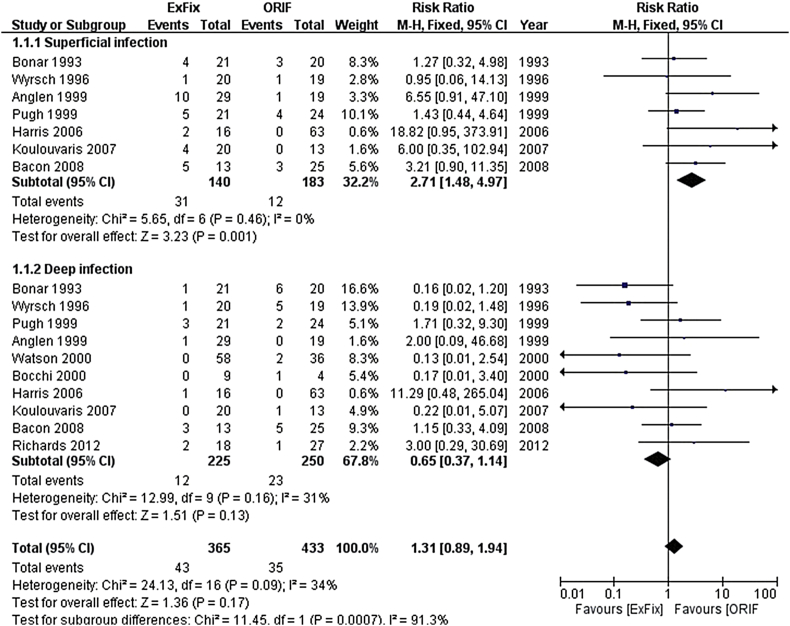
Eleven studies7, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19 reported the incidence of wound infections, with only two of them individually showing a statistically significant difference between the ExFix group and the ORIF group. One study did not give the detailed data and was excluded from analysis. Rate of total infection was 43 of 225 in the ExFix group and 35 of 250 in the ORIF group. Subgroup analysis showed a higher risk of incidence of superficial infection in the ExFix group (RR = 2.71, 95% CI = 1.48 to 4.97, Chi2 = 5.65, p = 0.001) with no significant heterogeneity (I2 = 0%), while for deep infection there was no difference between the two groups (RR = 0.65, 95% CI = 0.37 to 1.14, Chi2 = 12.99, p = 0.13) with an acceptable heterogeneity (I2 = 31%). The forest plot is presented in Fig. 2.
Fig. 2.
Meta-analysis of postoperative infection between ExFix and ORIF. Diamonds represent pooled estimates and width of the diamonds represents 95% CI.
Post-traumatic arthrosis
Arthrosis was a major complication reported by seven studies.10, 12, 15, 16, 17, 18, 19 Rate of arthrosis was higher in the ORIF group (57 of 144) than that of the ExFix group (55 of 159). Meta-analysis showed no significant difference in the incidence of arthrosis between the ExFix group and the ORIF group. The result was RR = 0.98, 95% CI = 0.79 to 1.23, Chi2 = 6.88, I2 = 13%, p = 0.87.
Malunion
Malunion was defined as >5° of angulation in the coronal plane, >10° in the sagittal plane, or >2 mm of articular step-off as seen on postoperative radiographs. Six studies7, 14, 15, 16, 17, 19 reported the incidence of malunion, none of which individually showed a statistically significant difference between the ExFix group and the ORIF group. The meta-analysis of these studies showed a significantly reduced incidence of malunion with ORIF as compared with ExFix (RR = 2.85, 95% CI = 1.23 to 6.60, Chi2 = 1.32, p = 0.01) with no significant heterogeneity (I2 = 33%).
Nonunion
Nonunion was defined as a fracture that did not heal in six months. A total of six studies7, 13, 14, 15, 17, 18 reported the incidence of nonunion. Meta-analysis showed a significantly higher risk of nonunion in ExFix groups with a moderate heterogeneity (RR = 2.09, 95% CI = 1.10 to 3.98, Chi2 = 7.49, I2 = 33%, p = 0.02).
Unplanned hardware removal
Postoperative infection or osteomyelitis was usually treated by additional secondary procedures including unplanned hardware removal. The rate of unplanned hardware removal was reported by five studies.12, 14, 15, 17, 19 Meta-analysis detected an increased risk of unplanned hardware removal in the ORIF group with no significant heterogeneity among the studies (RR = 0.12, 95% CI = 0.04 to 0.37, Chi2 = 2.01, I2 = 0%, p = 0.0002).
Union time
Union time was compared in four studies,13, 14, 16, 17 and one of them13 was excluded because of not mentioning the standard deviation. Meta-analysis of the other three studies revealed no significant difference regarding union time (RR = 4.35, 95%CI = −4.80 to 13.50, Chi2 = 6.69, p = 0.35) and the heterogeneity was significant (I2 = 70%).
Radiography results
Assessment of reduction was based on postoperative radiographs. Reduction was designated as excellent or anatomic if there was less than 2 mm of gap or step-off, less than 1 mm of mortise asymmetry, and normal alignment; poor if there was more than 4 mm of gap or step-off, more than 2 mm of asymmetry.13, 20 We studied the number of patients who were graded as excellent or anatomic in both groups. A total of six studies10, 12, 13, 15, 18, 19 measured and compared the reduction score. The meta-analysis did not reveal any difference between groups (RR = 0.89, 95%CI = 0.76 to 1.03, Chi2 = 4.32, I2 = 0%, p = 0.11).
Clinical evaluation
A total of seven studies7, 11, 12, 13, 15, 18, 19 described the clinical evaluation results of both groups, but only two of them15, 19 used the same scoring system which was modified by Teeny and Wiss.21 Meta-analysis of these two studies did not show a significant difference in clinical evaluation between the two groups (RR = 1.03, 95% CI = 0.82 to 1.28, Chi2 = 1.56, I2 = 36%, p = 0.82).
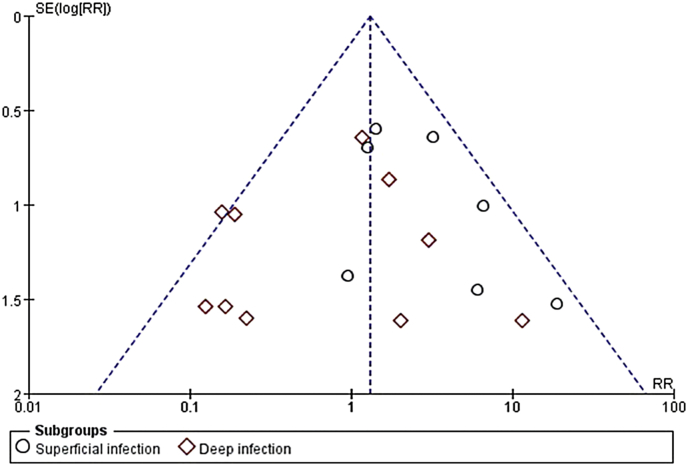
Publication bias
Funnel plots of standard error (SE) versus RR for outcome which included more than nine studies were made. For infection, visual inspection of the funnel plots did not show any remarkable asymmetry, which indicated no significant publication bias. The funnel plot is presented in Fig. 3.
Fig. 3.
Funnel plot for the meta-analysis on postoperative infection.
Discussion
Tibial pilon fracture is a severe injury with many different complications. Treatments of the injury have evolved for a long time but there is still not a gold standard for surgeons to follow. ORIF, the most reliable means to obtain excellent reduction of the articular surface, has been advocated since the mid-60s, but the strict steps of meticulous reduction and rigid fixation have gradually made the surgeon reluctant to use this method. The application of ExFix provided indirect ways of reduction and protection for the soft tissue. Few comparative studies between ORIF and ExFix concluded that ExFix was involved in fewer complications, while some other studies had opposite results. According to our knowledge, no meta-analysis compared the difference between ExFix and ORIF.
Our systematic review and meta-analysis included eleven studies, one prospective randomized and ten retrospective cohort comparing ORIF versus ExFix for tibial pilon fractures. The results of this meta-analysis of all eleven studies suggest that there is no statistically significant difference of the total postoperative infection between the ORIF and the ExFix group. Subgroup analysis of deep infection did not find a significant difference between the two groups, but when only superficial infection was considered, the incidence increased in the ExFix group. Only one study13 reported the operation time and blood loss and both outcomes showed no significant difference between two groups. Union time was compared by four studies. One of them reported that ORIF group took less time to union (p < 0.05) and did not describe the standard deviation. Meta-analysis of other three studies revealed no significant difference between the two treatment groups, but with a significant heterogeneity (I2 = 70%), which limited the reliability of the result. The source of heterogeneity is probably due to using an external Ilizarov ring fixator, which may result in a reduced union time in ExFix groups.17 Arthrosis is also a major complication, which could lead to amputation and other additional operations. Our analysis showed no significant difference in the incidence of post-traumatic arthrosis between both groups (p = 0.87). There is a significant reduction of incidence of malunion in ORIF groups (4.3%) versus ExFix groups (12%). Nonunion is a multifactorial complication caused by ignoring contraindications, unfavorable biomechanical and vascular conditions.22 The incidence rate of nonunion was compared by six studies and meta-analysis showed a significantly higher risk of nonunion in ExFix groups with an acceptable heterogeneity (p = 0.02). It was reported that smoking was a risk factor for nonunion of femoral neck fractures.23 Bacon et al17 stratified the complications according to the risk factor of smokers versus non-smokers and found no statistically significant association between a positive cigarette history and nonunion (p = 0.44). Additional secondary procedures such as unplanned hardware removal were also considerable factors for surgeons to select the operation. Many reasons lead to unplanned hardware removal, including deep infection and osteomyelitis. Meta-analysis showed a significantly reduced unplanned hardware removal rate in ExFix groups (RR = 0.12, 95%CI = 0.04 to 0.37, Chi2 = 2.01, I2 = 0%, p = 0.0002). More hardware was fixed in legs in ORIF groups, which tended to cause more infections, so it is easy to understand why ORIF groups have a higher rate of unplanned hardware removal. Regarding the reduction assessment, meta-analysis of six included studies showed no significant difference between the two groups and this result was similar to that found by Richards18 and Wyrsch.12 Ankle functions were evaluated by seven authors but only two of them used the same criteria. The meta-analysis result revealed no difference between the ExFix group and the ORIF group. Crutchfield11 used a 10-point grading scale including pain, stiffness, swelling and stability and found that patients who had undergone ORIF had higher scores. Wyrsch et al12 used a clinical scoring system based on patient pain, function and range of motion and found no difference between the two surgical methods. Harris7 used Foot function index and found that more ankle motion limitation was detected in patients with ExFix compared with patients after ORIF. Koulouvaris et al16 measured the range of ankle motion by comparing the injured ankle with the contralateral one and defined limitation as range of ankle motion <25%. In their study, no difference existed between two groups. Richards et al18 used Iowa ankle score and Short Form-36 (SF-36) physical function score to evaluate patient ankle function at 3-, 6-, 12-month follow-up. They observed that patients undergoing ORIF were significantly better in the 6-month ankle function score, the 6-month SF-36 physical function score, and the 12-month ankle function score.
This study has investigated the difference between ORIF and ExFix in terms of postoperative infection, nonunion, malunion, reduction, clinical evaluation and unplanned hardware removal. However, it has some limitations. First, the same outcome may be measured with different criteria by different authors. For instance, malunion was defined obscurely in few studies, while wound infection had an almost homogenous definition throughout all studies. In our analysis, we tried our utmost to select outcomes measured with the same criteria to reduce heterogeneity. Second, it seems impossible for an orthopedic surgeon to conduct randomized controlled trials on patients because of ethical reasons. Studies we selected are all cohort or case-control studies, whose design lacks a blinded or random allocation of treatment to different groups. Third, publication bias cannot be ignored because published studies which our analysis based on tend to report positive results rather than negative ones. Fourth, we could not exclude all confounding factors that may have effects on outcomes we measured. Studies we selected are all from the US except one, so the result may not apply to other districts.
In conclusion, we suggest that ORIF has a relatively lower incidence rate of superficial infection, malunion and nonunion, but a higher rate of hardware removal. In the future, more high quality randomized trials are needed to confirm our findings and to compare more factors that can alter the outcome.
Acknowledgments
We would like to thank the authors of the original studies included in this meta-analysis.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.De Vries J.S., Wijgman A.J., Sierevelt I.N. Long-term results of ankle fractures with a posterior malleolar fragment. J Foot Ankle Surg. 2005;44:211–217. doi: 10.1053/j.jfas.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Liporace F.A., Yoon R.S. Decisions and staging leading to definitive open management of pilon fractures: where have we come from and where are we now? J Orthop Trauma. 2012;26:488–498. doi: 10.1097/BOT.0b013e31822fbdbe. [DOI] [PubMed] [Google Scholar]
- 3.Poyanli O., Esenkaya I., Ozkut A.T. Minimally invasive reduction technique in split depression type tibial pilon fractures. J Foot Ankle Surg. 2012;51:254–257. doi: 10.1053/j.jfas.2011.10.034. [DOI] [PubMed] [Google Scholar]
- 4.Blauth M., Bastian L., Krettek C. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma. 2001;15:153–160. doi: 10.1097/00005131-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Xu Y.Q., Li Q., Shen T.G. An efficacy analysis of surgical timing and procedures for high-energy complex tibial plateau fractures. Orthop Surg. 2013;5:188–195. doi: 10.1111/os.12057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pollak A.N., McCarthy M.L., Bess R.S. Outcomes after treatment of high-energy tibial plafond fractures. J Bone Jt Surg Am. 2003;85:1893–1900. doi: 10.2106/00004623-200310000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Harris A.M., Patterson B.M., Sontich J.K. Results and outcomes after operative treatment of high-energy tibial plafond fractures. Foot Ankle Int. 2006;27:256–265. doi: 10.1177/107110070602700406. [DOI] [PubMed] [Google Scholar]
- 8.Downs S.H., Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higgins J.P., Thompson S.G., Deeks J.J. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonar S., Marsh J.L., Andre M. Unilateral external fixation vs. open reduction and internal fixation of severe tibial plafond fractures. J Orthop Trauma. 1993;7:169. [Google Scholar]
- 11.Crutchfield E.H., Seligson D., Henry S.L. Tibial pilon fractures: a comparative clinical study of management techniques and results. Orthopedics. 1995;18:613–617. doi: 10.3928/0147-7447-19950701-06. [DOI] [PubMed] [Google Scholar]
- 12.Wyrsch B., McFerran M.A., McAndrew M. Operative treatment of fractures of the tibial plafond. A randomized, prospective study. J Bone Jt Surg Am. 1996;78:1646–1657. doi: 10.2106/00004623-199611000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Anglen J.O. Early outcome of hybrid external fixation for fracture of the distal tibia. J Orthop Trauma. 1999;13:92–97. doi: 10.1097/00005131-199902000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Pugh K.J., Wolinsky P.R., McAndrew M.P. Tibial pilon fractures: a comparison of treatment methods. J Trauma. 1999;47:937–941. doi: 10.1097/00005373-199911000-00022. [DOI] [PubMed] [Google Scholar]
- 15.Watson J.T., Moed B.R., Karges D.E. Pilon fractures. Treatment protocol based on severity of soft tissue injury. Clin Orthop Relat Res. 2000;(375):78–90. [PubMed] [Google Scholar]
- 16.Koulouvaris P., Stafylas K., Mitsionis G. Long-term results of various therapy concepts in severe pilon fractures. Arch Orthop Trauma Surg. 2007;127:313–320. doi: 10.1007/s00402-007-0306-y. [DOI] [PubMed] [Google Scholar]
- 17.Bacon S., Smith W.R., Morgan S.J. A retrospective analysis of comminuted intra-articular fractures of the tibial plafond: open reduction and internal fixation versus external Ilizarov fixation. Injury. 2008;39:196–202. doi: 10.1016/j.injury.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 18.Richards J.E., Magill M., Tressler M.A. External fixation versus ORIF for distal intra-articular tibia fractures. Orthopedics. 2012;35:e862–867. doi: 10.3928/01477447-20120525-25. [DOI] [PubMed] [Google Scholar]
- 19.Bocchi L., Maniscalco P., Bertone C. Fractures of the tibial plafond: a comparison of treatment methods. J Orthop Traumatol. 2000;1:51–56. [Google Scholar]
- 20.Marsh J.L., Weigel D.P., Dirschl D.R. Tibial plafond fractures. How do these ankles function over time? J Bone Jt Surg Am. 2003;85:287–295. [PubMed] [Google Scholar]
- 21.Teeny S.M., Wiss D.A. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res. 1993;(292):108–117. [PubMed] [Google Scholar]
- 22.Upadhyay A., Jain P., Mishra P. Delayed internal fixation of fractures of the neck of the femur in young adults. A prospective, randomised study comparing closed and open reduction. J Bone Jt Surg Br. 2004;86:1035–1040. doi: 10.1302/0301-620x.86b7.15047. [DOI] [PubMed] [Google Scholar]
- 23.Huang H.K., Su Y.P., Chen C.M. Displaced femoral neck fractures in young adults treated with closed reduction and internal fixation. Orthopedics. 2010;33:873. doi: 10.3928/01477447-20101021-15. [DOI] [PubMed] [Google Scholar]