Abstract
Avian influenza A H5N1 remains unusual in its virulence for humans. While infection of humans remains inefficient, many of those with H5N1 disease have a rapidly progressing viral pneumonia leading to acute respiratory distress syndrome and death but its pathogenesis remains an enigma. Comparisons in the virology and pathogenesis of human seasonal influenza viruses (H3N2 and H1N1) and H5N1 in patients, animal models and in relevant primary human cell cultures remains instructive. While the direct effects of viral replication and differences in the tropism of the virus for cells in the lower respiratory tract clearly contribute to the pathogenesis, we focus here on the possible contribution of the host innate immune response in the pathogenesis of this disease.
Keywords: influenza, H5N1, pandemic, innate immune response, cytokine, macrophage
Type A and B influenza viruses cause regular seasonal influenza e pidemics but only type A influenza viruses are associated with influenza pandemics. The virus haemagglutinin (HA) and neuraminidase (NA) are the major surface proteins of the virus which induce protective host antibody responses and they are classified into 16 HA and 9 NA subtypes by antigenic analysis. Influenza virus is a single stranded RNA virus with an 8-segmented genome. As with other RNA viruses, mutations generate genetic and antigenic diversity (“genetic drift”). The segmented RNA genome allows the virus an additional mechanism for generating diversity through genetic reassortment. The pandemics of 1957 and 1968 arose by the prevailing human H1N1 influenza virus acquiring a novel HA and the polymerase basic 1 (PB1) gene (and in 1957 also the NA) from an avian source to generate a virus with a novel subtype; H2N2 in 1957 and H3N2 in 19681. The origin of the H1N1 virus in 1918 remains controversial, with some arguing that it arose from an avian virus directly (i.e. all 8 gene segments) adapting to efficient transmission in humans2 while others contend that it is also derived by reassortment3.
Avian influenza H5N1 continues to zoonotically transmit to humans causing severe disease and poses a pandemic threat4. However, this virus has so far not adapted to efficient human-to-human transmission. In early 2009, a novel H1N1 variant (H1N1v) virus of swine origin emerged and has now become pandemic5. This confounded the previously held dogma that an influenza pandemic is associated with the emergence of a virus with a novel HA subtype. The novel H1N1 virus is antigenically distant from the prevailing human H1N1 virus and there is little prior cross-reacting humoral immunity in the population with the exception of those inviduals older than 60 years or so6. Thus we now have a pandemic virus of an influenza subtype (H1N1) that is already endemic in the human population. It remains to be seen whether the novel pandemic H1N1 2009 virus will replace or co-circulate with the previously endemic H1N1 and H3N2 viruses. Although the infection appears to be comparatively mild, some patients have developed fatal pneumonia with acute respiratory distress syndrome (ARDS)7 but information on the pathogenesis of pandemic H1N1 is still emerging8. In this review we will focus on innate immune responses in the pathogenesis of lung disease caused by influenza, with a particular emphasis on human H5N1 disease.
Seasonal and pandemic influenza
Influenza is typically a self limiting upper respiratory disease but may range from an asymptomatic illness to (rarely) a severe illness with potentially fatal complications, especially in those with a pre-existing underlying disease. Complications of influenza include pneumonia, exacerbation of asthma or chronic obstructive pulmonary disease (COPD)9. Influenza is also associated with febrile seizures in children, encephalopathy which is particularly notable in Japan, and also with increased risk of myocardial infarction and strokes10–12. Since there is little evidence of systemic spread of the seasonal influenza virus, the systemic manifestations (e.g. myalgia) as well as some of these complications of seasonal influenza have been attributed to cytokines and other inflammatory mediators10,13.
The pneumonia following influenza is generally a rare complication and may be a primary viral pneumonia, or more commonly, secondary to bacterial infection. In contrast, a primary viral pneumonia is a major manifestation of human H5N1 disease14,15. Primary viral pneumonia was seen in the severe pandemic of 1918. A similar diffuse alveolar pattern of disease was also seen in a minority of young patients dying in the 1957 pandemic. Virus antigen has been detected in alveolar epithelial cells and alveolar macrophages. There continues to be controversy over whether the lung pathology of primary influenza viral pneumonia is solely due to a direct viral cytopathic effect or whether it is contributed to by innate immune responses16–18. Primary viral pneumonia is also now being reported in those with severe pandemic H1N1v disease8.
Human H5N1 disease
Virology
The current lineage of highly pathogenic avian influenza (HPAI) H5N1 virus derives from a group of H5N1 viruses first recognised in geese in Guangdong province, China in 199619,20. These viruses have undergone a series of genetic reassortments with other avian influenza viruses to give rise to a number of different virus “genotypes” (constellation of 8 genes). The virus HA has also undergone genetic mutation over the last 14 years to give rise to a number of recognised virus clades and sub-clades which are antigenically and genetically diverse21. However only limited numbers of the H5N1 genotypes and clades are known to have caused human disease15.
A number of viral mutations are recognised as potential virulence factors for humans. The non-structural 1(NS1) gene segment is an interferon (IFN) antagonist and plays a key role in evading host innate immune responses22. NS1 binds double stranded RNA thereby preventing the activation of 2’5’oligo(A) synthetase and the downstream consequences of its activation. NS1 interacts with RIG-1 RNA helicase and suppresses its normal function as a cytosolic innate immune sensor of viral infection23. The four carboxy-terminal amino acids of NS1 form a PDZ ligand domain motif which is relevant in mouse virulence24. The PB1 gene segment of most human and avian influenza viruses encode a second open-reading frame, PB1-F2. Via its interaction with mitochondrial proteins, PB1-F2 is believed to induce apoptosis25, enhance inflammation in mice and synergistically enhance the severity of secondary bacterial infections26. In addition, influenza virus infection blocks many features of dendritic cell (DC) maturation (e.g. co-stimulatory molecules CD80, CD86) that are key to T-cell stimulation27.
While the basic amino acids at the HA cleavage site is clearly an important virulence factor for chicken and turkeys and also for mice, its contribution to virulence in humans is less clear. The PB2 Lys627 is associated with virulence in mice28 and contributes to replication competence in mammalian cells at lower temperatures29. However, humans infected with clade 2.2 H5N1 viruses that consistently carry PB2 Lys627 do not manifest more severe disease; in fact the reverse may be true (see below)30. Other known viral determinants of pathogenicity include PB2 Asp701Asn, PB1-F2 Asn66Ser, NS1 Asp92Glu (reviewed elsewhere31,32).
Clinical features and epidemiology
Avian influenza H5N1 is inefficiently and rarely transmitted to humans in spite of repeated and substantial exposure to the virus33,34. Underlying immunocompromising factors or other diseases associated with increased risk for seasonal influenza are not commonly observed in patients with H5N1 disease. Thus, exposure to virus is necessary but is not a sufficient explanation for the observed epidemiology – other factors such as host genetic or immunological susceptibility or unusual routes of exposure are likely to play a role. Interestingly, H5N1 disease is less common in those over 40 years of age, an observation not explainable by the population age-structure or risk behaviour of affected populations35,36. It is possible that cumulative hetero-subtypic immunity through repeated exposure to seasonal influenza may contribute to this age distribution. There is increasing evidence of antigenic epitopes that can mediate such cross-subtype immunity37.
The overall mortality of patients with virologically confirmed H5N1 disease is over 60%15. While this observation may be skewed by the selective investigation and diagnosis of patients who are more severely ill, there is no doubt that H5N1 disease in humans is overall associated with a markedly worse clinical outcome. A proportion of patients appear to have a milder disease presentation and these have been most notably reported in Hong Kong in 1997 (clade 0 virus) and more recently in Egypt (clade 2.2 virus) although even then, overall case mortality was >30%. In these two instances, young children had a milder disease presentation than adults30,38. Whether this reflects increased case detection of milder cases in Hong Kong and Egypt or is a reflection of differences of virulence of different virus clades remains unclear. Patients with severe H5N1 disease have a rapidly progressive primary viral pneumonia associated with leukopenia (a finding also documented in the 1918 outbreak), gastro-intestinal symptoms and mild liver and renal dysfunction15,38. The key autopsy findings are diffuse alveolar damage with hyaline membrane formation, i.e. the pathology of ARDS. Patchy interstitial infiltrates and pulmonary congestion is seen with varying degrees of haemorrhage (Figure 1A). The cellular infiltrate predominantly comprises of macrophages, neutrophils and activated lymphocytes (Figure 1B). Apoptosis of alveolar epithelial cells is noted. Lymphocyte depletion is seen in the spleen and lymph nodes39–44.
Figure 1.
(A) Lung histology of fatal human H5N1 disease stained with Haematoxylin & Eosin showing increased cellular inflammation within the alveoli compared to normal lung. (B) Immunohistochemistry for the macrophage marker CD68 (brown) shows increased numbers of macrophages infiltrating the lung tissue. (C) The histological appearance and alveolar macrophages shown by CD68 immunohistochemistry in a control lung is shown for comparison. Magnification × 200.
Pathogenesis
The severe disease associated with H5N1 disease in humans may possibly arise through different mechanisms (or combinations thereof). These include a) dissemination of virus beyond the respiratory tract (in contrast with seasonal flu), b) higher and prolonged viral replication leading to direct viral cytolytic damage, c) differences in the tissue tropism of the avian H5N1 virus (in contrast to the human seasonal influenza viruses) and d) differences in host responses induced by H5N1 virus (Figure 2). While H5N1 virus appears to have the ability to spread beyond the respiratory tract, i.e. the virus can be isolated from the faeces45, serum46,47 and very rarely from the central nervous system46, the lung pathology (ARDS) remains the major cause of mortality in human H5N1 disease. However, at the time of death, immune-histochemistry rarely shows overwhelming viral infection of the lungs and often very few if any virus infected cells are demonstrable39,41,43,44. Since the limited autopsy data arises from patients who have died after prolonged periods of illness and assisted ventilation, the paucity of virus at autopsy does not of course preclude a major role for virus in initiating the lung injury.
Figure 2.
Mechanisms that may contribute to the pathogenesis of H5N1 disease. Arrows indicate the factors contributing to outcome. Higher levels of viral replication, the binding of the H5N1 virus to receptors in alveolar epithelial cells, and the spread of the virus beyond the respiratory tract could all contribute to the severity of human H5N1 disease. In this review, we argue that the H5N1 virus differentially activates host responses in macrophages and primary lung alveolar epithelia and such differences in host responses contribute to disease pathogenesis. This figure is modified from reference 3.
The mechanism for ARDS is not fully defined, but cytokine-induced inflammatory responses are believed to play a significant role (reviewed in48,49). Scientific approaches to address the pathogenesis of ARDS in human H5N1 disease includes clinical studies, investigations in relevant animal models and in vitro investigations. While each has advantages and limitations, a synthesis of knowledge from all three approaches would be informative.
H5N1 virus load in the respiratory tract remains elevated for much longer than is usually seen with seasonal influenza50. This is not surprising because, in contrast to seasonal influenza which infects most of us repeatedly, leading to development of cross-reacting immune responses, most humans (perhaps with the exception of older individuals, see discussion above) are unlikely to have prior immunity against H5N1. The H5N1 polymerase complex is associated with its virulence in ferrets51. The Glu627Lys in the viral gene PB2 determines virulence in mice as well as efficiency of viral replication in mouse cells52.
It has been proposed that the avian H5N1, which binds sialic acids (SA) with α 2–3 linkages (typically found in avian cells) preferentially infects cells of the human lower respiratory tract. The alveolar epithelial cells express α 2–3 SA-Gal-GlcNAc while the upper respiratory tract has a paucity of these receptors. In contrast the human upper respiratory tract (nasopharynx, trachea) has an abundance of α 2–6 SA which preferentially binds the human seasonal influenza viruses H3N2 and H1N1. They also have O-linked α 2–3 SA which bind both avian and human influenza viruses53–57. Furthermore, within the lung, H5N1 viruses preferentially attach to type 2 pneumocytes and macrophages. These findings led to the hypothesis that the lung pathology of H5N1 is caused by differential targeting of the virus to the lower respiratory tract. Furthermore, if the H5N1 virus is unable to replicate efficiently in the upper respiratory tract, it would explain why the virus is not readily transmitted to humans. However, there are some key observations that do not fit in with such a hypothesis. H5N1 viruses readily infect ex vivo cultures of upper respiratory tissues e.g. nasopharyngeal and tonsillar tissue54 and immunohistochemistry for viral antigen and virus receptors in tracheal tissue of a patient with fatal H5N1 disease demonstrated that the virus can be found infecting tracheal epithelium58. Conversely, some seasonal influenza viruses H1N1 can readily infect the ex vivo cultures of lung (lower respiratory tissues)53,54 but they are not commonly associated with severe lung pathology. There are also patients with H5N 1 disease who had mild self-limited upper respiratory illness without lower respiratory involvement. As part of rapid diagnostic procedures, influenza antigen was detected in nasopharyngeal epithelial cells from nasopharyngeal aspirates of these patients suggesting that H5N1 virus can in fact infect the upper respiratory tract38. While tissue tropism may well play a role, we contend that other mechanisms also contribute to the unusual severity of human H5N1 disease (discussed below).
Host responses to H5N1 influenza
Host responses to influenza are clearly complex and involve humoral and cell mediated immune responses as well as innate immune responses. While specific antibodies are the best established correlate of protection against infection, cell mediated immune responses play a key role in recovery from disease59. Adoptive transfer experiments have shown that CD8+ T memory cells can crossprotect across different subtypes60. Furthermore, memory T cells induced in response to seasonal human influenza can cross-react even with avian influenza H5N161. There is however, limited data on cell mediated immune responses in H5N1 disease. For the purpose of this review, we will therefore focus on innate immune responses, while remaining fully cognizant of the importance of the contribution of adaptive immune responses in the clinical outcome of H5N1 disease.
Clinical data
When compared with seasonal influenza, patients with H5N1 disease have higher serum levels of macrophage and neutrophil chemoattractant chemokines (CXCL10, CXCL2, IL-8) and both pro- and anti-inflammatory cytokines (e.g. IL-6, IL-10, IFN-γ)50,62. Patients who died had higher serum levels of these mediators than those who survived. However, the levels of these mediators also correlated with viral load in the nasopharynx and may simply be a reflection of increased virus replication and increased pathology50.
Animal models
Ferrets, mice, macaques and other mammals have been used as experimental models for influenza pathogenesis, each with their own advantages and limitations63,64. The most appropriate animal model for use depends on the purpose, i.e. vaccine evaluation, antiviral testing, transmission or pathogenesis. The most challenging of these is the choice of an animal model to study transmission and pathogenesis. While guinea-pigs are being used to study virus transmission, influenza causes minimal pathology or disease in this animal model65. Relevant features of available animal models for the study of pathogenesis of HPAI H5N1 and human seasonal influenza are summarised in the table. Ferrets most closely mimic humans in the distribution of putative SA receptors in the respiratory tract while mice and macaques do not57. For instance, ferrets can be infected with human influenza viruses without prior adaptation while mice typically cannot. There is however a paucity of immunological reagents and genomic data on ferrets, an issue that currently imposes major limitations on the detailed immunological study of this animal model. While mice have been widely used for studies on influenza virulence and pathogenesis, particularly because of the availability of reagents, inbred mouse strains and mice with defined gene defects still have a number of caveats. Firstly, there is sometimes poor correlation between lethality of viruses for mice and for ferrets63. For instance, some H5N1 viruses are highly neurotropic in mice and fatality is therefore more likely related to virus dissemination to the brain rather than related to the lung pathology. Many investigators use H5N1 viruses with rapid lethality for mice because they provide a clear end-point, although such lethality may in fact reflect neurotropism rather than the ARDS-like lung pathology which is the cause of death in humans.
Table.
Animal models used for the study of pathogenesis of highly pathogenic avian influenza (HPAI) H5N1 and seasonal human influenza (based on data and reviews in64,63,57)
| Human | Mice | Ferret | Macaque | Cat | Pig | |
|---|---|---|---|---|---|---|
| H5N1 virus | ||||||
|
Binding of H5N1 virus. Anatomical site and cell type57 |
Alveoli>>Trachea Type II pneumocyte |
Trachea>Alveoli Type II pneumocyte |
Alveoli>>Trachea Type II pneumocyte |
Alveoli>>Trachea Type I pneumocyte |
Alveoli>>Trachea Type II pneumocyte |
Alveoli>>Trachea Type II pneumocyte |
|
Disease readily caused by H5N1 virus without prior virus adaptation |
Yes ARDS Hyaline membranes |
Yes ARDS with some strains, e.g. A/Ck/Hebei/108/02 |
Yes | Yes ARDS with a few strains A/HK/156/97 |
Yes ARDS-like Hyaline membranes |
Poor |
|
Dissemination beyond respiratory tract |
Limited extent | May be widespread. Depends on virus strain |
May be widespread. Depends on virus strain. Dissemination may not correlate with strains that disseminate in mice |
No | Yes | No |
| H1N1 or H3N2 virus | ||||||
|
Binding of human seasonal H1N1 or H3N2 virus. Anatomical site and cell type57 |
Trachea>>Alveoli Type 1 pneumocyte |
+/−alveoli | Trachea>>Alveoli Type 1 pneumocyte |
Poor binding | Poor binding | Poor binding Type I pneumocyte |
|
Disease following human H1N1 or H3N2 virus without prior virus adaptation |
Yes | Very mild and does not recapitulate human disease. Mice-adapted viruses may lead to severe disease. |
Yes Mimics human disease. |
Mild illness | No | Mild illness. Tracheal inoculation may lead to more severe pneumonia |
| Other comments | Availability of genetic sequence data, microarrays and immunological reagents |
Availability of genetic sequence data, microarrays, knock-out mouse lines and immunological reagents |
Paucity of genetic information and immunological reagents |
Availability of some genetic sequence data and immunological reagents |
Paucity of genetic information and immunological reagents |
Paucity of genetic information and immunological reagents |
In general, in comparison with seasonal influenza viruses, HPAI H5N1 viruses show increased virulence in mice, ferrets and macaques with evidence of increased viral replication and dysregulated host responses. Mice infected with H5N1 had cytokine and chemokine responses including the IL-1β, IFN-γ, TNF-α, MIP-1α, IL-6 and MIP-2, MCP-1, KC (equivalent to human IL-8), IL-1 α, at day 3–5 post-infection66–68. This was associated with recruitment of macrophages and neutrophils into the lungs causing acute lung inflammation68. Ferrets infected with H5N1 viruses had markedly stronger induction of the chemokine CXCL10 and IFN response genes in the lungs in comparison with H3N2 subtype seasonal influenza. On the contrary, CD45, GRB2, phosphonositide-3-kinase gene and the mitogen-activated protein kinase (MAPK) genes associated with B and T-cell signaling were all downregulated69. Blocking of CXCR3, the cognate receptor of CXCL10, with the drug AMG487 in H5N1-infected ferrets resulted in a reduction of symptom severity and delayed mortality compared to vehicle treatment69. Macaques infected with H5N1 virus had more intense and more protracted expression of type I IFN responses, IFN-induced genes IL-1 and 6, TNF-α and CXCL10 than was seen in H1N1 infected macaques. Similarly, H5N1 virus infection was associated with higher and more prolonged viral replication in the lung, more severe lung pathology as well as a dramatic depletion of CD4+ and CD8+ T cells and premature apoptosis of DCs70. Surprisingly, although the H5N1 virus induced a more potent IFN response, virus replication remained poorly controlled.
The aberrant host responses induced by H5N1 virus in mice and macaques is reminiscent of those induced by the 1918 H1N1 virus in these animals. In mice, the 1918 virus differentially activated apoptosis pathways, IL-6, type I IFN and Toll-like receptor (TLR) response genes and these findings were associated with severe pulmonary pathology71. Similarly further studies found higher viral titres in the lung and increased lung macrophage and neutrophil infiltration, MIP-1α, IL-1, IL-6 and IFN in association with the 1918 virus68. In macaques, the 1918 virus led to dysregulated immune responses with higher IL-6 and lower type 1 IFN titres72. A recombinant seasonal influenza H1N1 virus with the 1918 HA and NA with or without the NS gene segment were studied for their pathogenicity in macaques70. While these recombinant viruses did not have the virulence associated with the full 1918 H1N1 virus reported by Kobasa and colleagues72, the 1918 HA and NA appeared to increase the virulence of the seasonal influenza H1 N1 virus and was also associated with changes in gene expression profile.
Studies with gene defective mice and the effect of experimental immunomodulator treatment
When challenged with H5N1 viruses, mice deficient in IL-6 or MIP-1α had comparable morbidity and mortality in comparison to wild type controls although this is not surprising since most cytokines and chemokines have some redundancy in their effector pathways. Mice with defects in genes for the IL-1 receptor, the type I interferons IFN-α or IFN-β had a worse outcome following H5N1 infection suggesting that these pathways are protective67,73. Interestingly, tumor necrosis factor (TNF) receptor 1 deficient mice as well as mice treated with anti-TNF antibody had less weight loss following infection when compared with controls although survival was no different67. This may reflect a role for TNF receptor signalling in the pathogenesis of influenza-induced lung disease although mortality (which in these mice was associated with neuro-invasion) was unaffected. In a study where a number of immunomodulators currently in clinical use were investigated together with an antiviral agent (zanamivir) in a mouse model of H5N1 disease, zanamivir in combination with a COX2 inhibitor (Celecoxib) and mesalazine led to improved survival when compared to the antiviral alone74. The hyper-induction of chemokines by H5N1 virus led to the accumulation of a particular subset of DC described as TNF-α/inducible nitric oxide synthase (iNOS) producing DCs (tipDCs) in the lung airways. These tipDCs are important for proliferation of influenza specific CD8+ T-cells in the lung. CCR2 defective mice who lack this chemokine attraction have markedly reduced accumulation of tipDCs in the lung leading to delayed virus clearance. However, modulation of the tipDC trafficking by treatment with the peroxisome proliferator-activated receptor-γ (PPAR-γ) agonist pioglitazone moderated the deleterious effects of tipDC recruitment without losing its beneficial effects of cytotoxic T cell recruitment75.
Studies with seasonal influenza viruses have suggested that defects in TLR-3 or COX2 are beneficial to mice challenged with seasonal H3N2 virus76,77 suggesting that innate immune responses may sometimes be deleterious. On the other hand, ferrets infected with a higher virulence influenza virus induced weaker type I and II IFNs and IL-8 mRNA but more IL-6 mRNA in the nasal fluid washes compared to animals infected with a lower virulence virus. The authors of this study speculated that the lack of an IFN response allowed the virus to spread to the lung leading to the increase in virus virulence. However, the lung cytokine levels were not measured78. These findings would support the therapeutic use of IFN to correct this weaker induction of IFN by the more virulent seasonal influenza virus.
It has been found that mice with inactivating mutations in TLR-4 or TRIF (but not MyD88) were protected from acute lung injury by chemicals as well as inactivated H5N1 virus administered intra-tracheally79. IL-6 deficient mice were also protected from lung pathology in this model. Inactivated H5N1 virus was shown to induce oxidized phopholipids which triggered an inflammatory response leading to acute lung injury (ALI) via TLR-4 and the TRIF / TRAF6 signalling pathway. Deletion of the Ncf1 gene, which controls reactive oxygen species production, reduced the severity of H5N1-mediated ALI. Collectively this suggests that oxidative stress and innate immunity are key lung injury pathways that control the severity of ALI. It remains to be seen if these pathways are relevant to infection with the live H5N1 virus.
Protease-activated receptors (PAR) are activated by extracellular proteases that are abundantly found in the lung. PAR2 was shown to be induced by seasonal influenza virus infection and appears to inhibit virus replication via an IFN-γ dependent pathway. PAR2 agonists increase survival of A/PR/8/34 (H1N1) virus infected mice. The increased survival was associated with reduced viral titres in the lung, reduced neutrophil infiltrates, reduced RANTES and increased IFN-γ secretion80.
Studies in primary human cells in vitro and ex vivo cultures
The studies in humans with H5N1 disease as well those from animals experimentally infected with H5N1 and seasonal influenza viruses demonstrate that the increased pathology of the H5N1 virus is associated with increased viral replication and enhanced host responses. As these observations reflect the outcome of multiple cycles of virus replication and associated tissue damage in the human or animal, it is not possible to differentiate whether the aberrant host responses are merely secondary to the enhanced pathology caused by H5N1 virus, whether they reflect increased cumulative viral load, or whether there are intrinsic differences between viruses in their ability to induce these host responses. This question can only be addressed by experiments carried out on physiologically relevant well defined cell-populations with a defined virus inoculum, a synchronous virus infection and sampling of the host response parameters at defined times. Since alveolar pneumocytes and macrophages are the two key cells infected by H5N1 viruses in vivo (see above), we and others have compared the host responses induced in primary human macrophages and type 1 epithelial cells by H5N1 or seasonal influenza (H1N1, H3N2) viruses. Compared with human H1N1 or H3N2 viruses, equivalent infecting doses (approx 2 infectious virus particles per cell) of H5N1 virus more strongly induces a range of cytokines and chemokines including TNF-α, IFN-α and -β, IL-1 β, CCL2, CCL3, CCL4, CCl5 and CCXL10 from primary human macrophages68,81. Similarly, H5N1 viruses differentially upregulated CXCL10, IL-6, IL-8, CCL2, CCL5, and IFN-β from alveolar epithelial cells82. Thus, many of the cytokines and chemokines found to be differentially elevated in the sera of patients with H5N1 disease (compared to seasonal influenza) were also more strongly induced in vitro using comparable challenge doses of the virus (Figure 3). This differential gene expression occurred within the first few hours of virus infection and was dependent on infection with live virus. Furthermore, increasing the infecting dose of H1N1 (low cytokine phenotype) virus to 10 times that of H5N1 virus could still not result in a comparable host response.
Figure 3.
Cytokine and chemokine induction in macrophages infected with H5N1 virus. Virus infection activates interferon regulatory factor 3 (IRF-3) and the p38-MAPK signaling pathways as well as others. Activation of these pathways leads to the expression of primary mediators such as tumor necrosis factor- α (TNF-α), the type I interferons (IFN)-α and -β which in turn trigger release of other cytokines and chemokines through autocrine and paracrine effects. Cyclooxygenase-2 (COX-2) is involved in regulating cytokine expression within the infected cell, as well as those activated by secreted mediators in adjacent uninfected cells.
Cytokine responses are induced directly by the stimulus but are also amplified by autocrine and paracrine mediator cascades. The primary mediators directly and differentially induced by H5N1 virus are TNF-α, IFN-β and IFN-λ1, the other mediators being the result of autocrine and paracrine responses83 (Figure 3). The induction of the primary mediators occurred, at least in part, by the virus differentially activating interferon regulatory factor (IRF)-3 and p38MAPK pathways83,84. In an intact organ, there are interactions between different cell types and we have tried to mimic such interactions between virus infected macrophages and alveolar epithelial cells in vitro85. The virus-free supernatants of H5N1-infected macrophages induce mediator cascades in alveolar epithelial cells and these lead to amplification and broadening of the host responses. For example, TNF-α is not induced directly by the H5N1 virus infection of alveolar epithelial cells but virus-free supernatants from H5N1 infected macrophages do. COX-2 was found to be a key controller of this amplifying cytokine cascade and COX2 inhibitors could dampen these amplifying mediator cascades85 (summarised in Figures 3 and 4). Some of these cytokines (e.g. IFNs) are expected to have an antiviral effect (see above), but the overall effects of these cytokine cascades may well contribute to pathogenesis. While we had reported that H5N1 more strongly induced type 1 IFNs from alveolar epithelial cells82, others reported that H5N1 induced a weaker type 1 IFN response from differentiated bronchial epithelium than seasonal influenza H3N286.
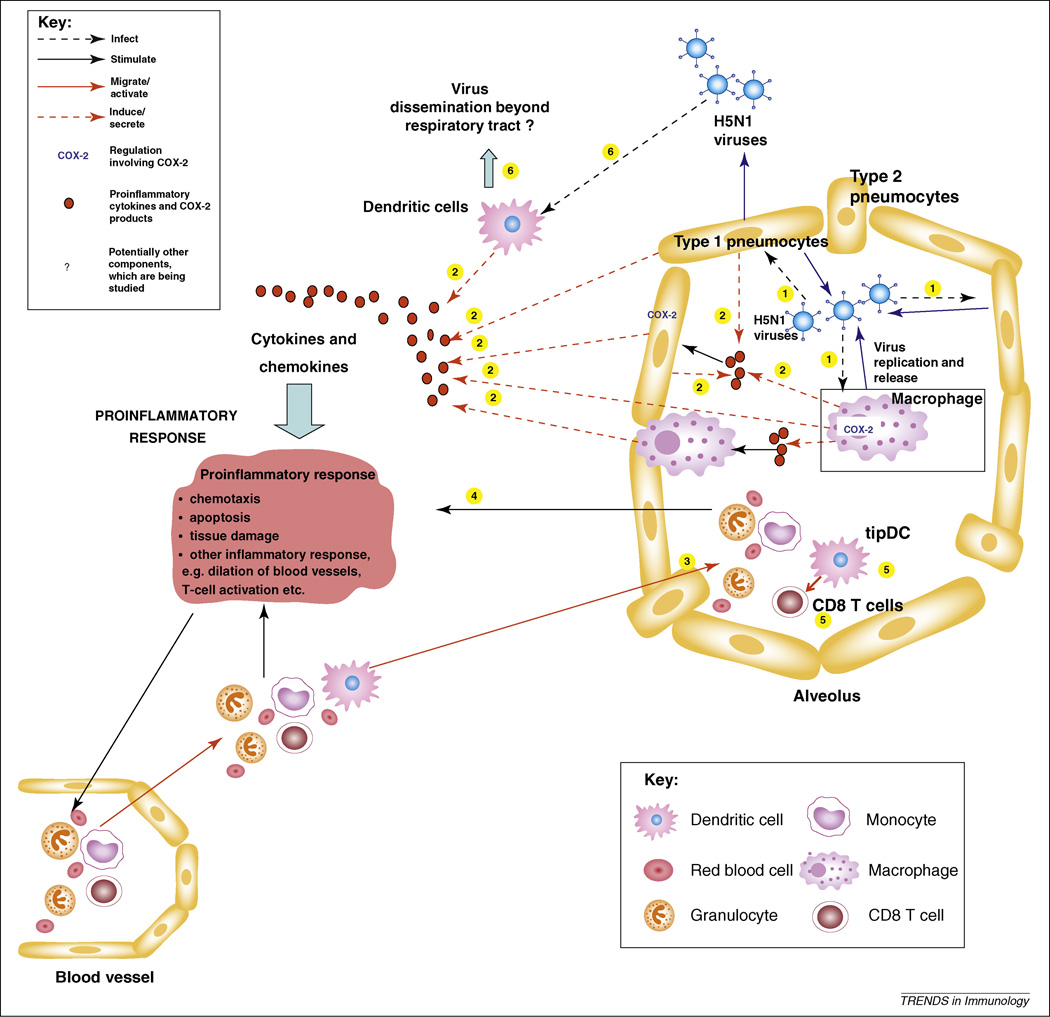
Figure 4.
Proinflammatory cascades in the pathogenesis o f lung damage in H5N1 disease. (1) Virus infection of macrophages and alveolar epithelium leads to virus replication as well as release of cytokines and chemokines (2), which trigger autocrine and paracrine proinflammatory cascades involving both cell types and infected as well as uninfected cells. These host responses are more potently induced by H5N1 virus compared to seasonal influenza viruses. Some of these cytokines (e.g. interferons) are expected to have an antiviral effect, but the overall effects of these cytokine cascades may well contribute to pathogenesis. The amplification cascade involving adjacent uninfected cells leads to a faster and broader inflammatory response than that induced by direct virus infection. (3) Chemokines lead to the infiltration of inflammatory cells (lymphocytes, monocytes/macrophages, neutrophils, and dendritic cells) into the alveolar spaces thereby further amplifying these proinflammatory cascades (4). Infiltration of tipDCs (TNF-α/inducible nitric oxide synthase [iNOS] producing DCs) into the alveolar space leads to proliferation of influenza-specific CD8+ cytotoxic T-cells in the lung (5). These CD8+ cells are important for the control of the virus infection, but in excessive numbers, may also contribute to tissue damage. (6) Virus may also infect and replicate in myeloid DCs and this may possibly allow virus to be disseminated by these cells to other organs and tissues.
Taken together these findings support the contention that the differences in host responses seen in animal models and in humans with H5N1 infection at least in part reflect intrinsic differences in the virus-induced host response. Interestingly, in contrast with H5N1 viruses, the 1918 H1N1 and seasonal influenza H1N1 viruses induced comparable levels of cytokines in macrophages infected in vitro68. Thus the differential host responses seen in animals with 1918 H1N1 infection (see above) might not reflect differential host response at the individual cell level, although further work needs to be done on other cell types (e.g. alveolar epithelium).
It is important to understand the virus genetic factors that determine the high-cytokine phenotype of H5N1 viruses. Using virus reverse genetics, we have established that the H5N1 virus HA and NA are not essential to the high cytokine phenotype. Rather, the constellation of internal genes, in particular the polymerase genes and NS gene segments play key roles in this87. Interestingly not all H5N1 virus genotypes manifest the high cytokine phenotype but those that are associated with human disease appear to do so87,88.
Cytokine induction is not the only host response pathway that is differentially modulated by H5N1 viruses. Seasonal influenza virus H1N1 induces apoptosis pathways faster than H5N1 viruses89. Induction of early apoptosis is potentially a host defense mechanism to limit viral replication and these differences may therefore have pathogenic relevance. On the other hand, H5N1 viruses appear to enhance expression of TNF-related apoptosis-inducing ligand (TRAIL) and lead to more potent bystander apoptosis of T cells90. This may contribute to the lymphopenia seen in H5N1 disease.
H5N1 virus infects other cells of the innate immune system with potentially pathogenic consequences. In vitro infection of human myeloid DCs leads to productive virus replication, production of IFN-α and TNF-α and leads to cell death within 24 hours. DCs are present below the respiratory epithelial layer and migrate to draining lymph nodes upon activation. Thus productive infection of these DCs might contribute to dissemination of the virus, however depletion of these cells might lead to an impaired immune response to the virus infection. Pre-treatment of DCs with IFN-α abolishes virus infection and plasmacytoid DCs (pDCs), which are naturally high type I interferon producers, are refractory to virus infection and produce large amounts of IFN-α after co-culture with H5N1 virus68,91. H5N1 virus can also infect and replicate in primary human NK cells leading to apoptosis. Targeting NK cells might help the virus evade NK cell innate immune defences92. Finally, recent in vitro studies have demonstrated that γδ T cells (which are chiefly associated with mucosal surfaces) can be activated and expanded to have potent cytotoxic activity against cells infected with a wide range of influenza subtypes including H5N1 viruses93.
Conclusion
The world is currently in the throes of a pandemic caused by a novel H1N1v virus. The disease remains relatively mild although a small minority of patients appear to manifest with a primary viral pneumonia which may progress to an ALI or ARDS-like clinical presentation. Most of these patients have been healthy young adults and some of them had no underlying illnesses that would predispose to severe influenza disease. While the clinical presentation in these patients with severe respiratory disease is reminiscent of human H5N1 disease7, the underlying disease pathogenesis remains to be explored.
Notwithstanding the current H1N1v pandemic, H5N1 remains endemic in poultry in Asia and parts of Africa and continues to pose a major threat to public health. Its morbidity and mortality in humans not contained very effectively by antiviral therapy alone. For example, in Indonesia, while earlier commencement of oseltamivir treatment is associated with improved survival, even treatment within the first 4 days of disease is not a guarantee of survival and is still associated with a 42% mortality94. Alternative therapeutic strategies are urgently needed. The first step towards this is to understand the pathogenic mechanisms underlying the lung pathology associated with human H5N1 disease and how it differs from seasonal influenza. Here, we have reviewed data that suggests that the innate immune response may be both friend and foe. This points to possibilities of novel therapeutic interventions that deserve further investigation. Preliminary data suggests that the differences in host responses induced by H5N1 appear to be similar to those of seasonal H1N1, albeit of greater intensity83 but more systematic studies using gene expression profiling and proteomic studies to address this question are warranted. It is relevant to also investigate whether biomarkers that provide early indication of a poor prognosis can be identified to guide such immunomodulatory interventions. It is particularly interesting that targeting some signalling pathways that are associated with inflammation (e.g. the RAF-MEK-ERK kinase cascade, NF-κB activation) can also block viral replication95. Thus, such therapeutic interventions may potentially combine antiviral effects with beneficial immunomodulatory effects.
As the pandemic H1N1 virus arose from swine, its spread globally may possibly be associated with a panzootic of this novel H1N1 virus in swine. This enhances the opportunity for reassortments between the pandemic virus and other viruses including with H5N1 virus which has been reported in pigs96. The internal gene “cassette” of these swine viruses from which the H1N1 pandemic viruses arises appears to have unusual propensity for reassortment. Given the unprecedented severity of H5N1 disease and its continued threat to human health, it is important that we better understand the biological basis of its virulence and pathogenesis. This would also provide an improved understanding of the pathogenesis of ALI and ARDS caused by influenza as well as other causes. ALI and ADRS arising from many diverse causes continues to be a major cause of morbidity and mortality97.
Acknowledgments
We acknowledge research funding from the National Institutes of Health (NIAID Contract HHSN26620070005C), the Area of Excellence Scheme of the University Grants Committee (Grant AoE/M-12/06) and the Central Allocation Grant HKU1/05C from the Research Grants Council of the Hong Kong Special Administrative Region.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Webster RG, et al. Evolution and Ecology of Influenza-a Viruses. Microbiological Reviews. 1992;56(1):152–179. doi: 10.1128/mr.56.1.152-179.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taubenberger JK, et al. Characterization of the 1918 influenza virus polymerase genes. Nature. 2005;437(7060):889–893. doi: 10.1038/nature04230. [DOI] [PubMed] [Google Scholar]
- 3.Smith GJ, et al. Dating the emergence of pandemic influenza viruses. Proc Natl Acad Sci U S A. 2009;106(28):11709–11712. doi: 10.1073/pnas.0904991106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peiris JSM, et al. Avian influenza virus (H5N1): a threat to human health. Clinical Microbiology Reviews. 2007;20(2):243-+. doi: 10.1128/CMR.00037-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dawood FS, et al. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;360(25):2605–2615. doi: 10.1056/NEJMoa0903810. [DOI] [PubMed] [Google Scholar]
- 6.Centers-for-Disease-Control-and-Prevention-(CDC) Serum cross-reactive antibody response to a novel influenza A (H1N1) virus after vaccination with seasonal influenza vaccine. MMWR Morb Mortal Wkly Rep. 2009;58(19):521–524. [PubMed] [Google Scholar]
- 7.Perez-Padilla R, et al. Pneumonia and Respiratory Failure from Swine-Origin Influenza A (H1N1) in Mexico. N Engl J Med. 2009 doi: 10.1056/NEJMoa0904252. [DOI] [PubMed] [Google Scholar]
- 8.Peiris JS, et al. Emergence of a novel swine-origin influenza A virus (S-OIV) H1N1 virus in humans. J Clin Virol. 2009;45(3):169–173. doi: 10.1016/j.jcv.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nicholson KG. Human Influenza. In: Nicholson KG, et al., editors. Textbook of Influenza. Blackwell Science; 1998. pp. 219–264. [Google Scholar]
- 10.Ichiyama T, et al. Cerebrospinal fluid and serum levels of cytokines and soluble tumor necrosis factor receptor in influenza virus-associated encephalopathy. Scandinavian journal of infectious diseases. 2003;35(1):59–61. doi: 10.1080/0036554021000026986. [DOI] [PubMed] [Google Scholar]
- 11.Chiu SS, et al. Influenza A infection is an important cause of febrile seizures. Pediatrics. 2001;108(4) doi: 10.1542/peds.108.4.e63. [DOI] [PubMed] [Google Scholar]
- 12.Wong CM, et al. Influenza-associated mortality in Hong Kong. Clinical Infectious Diseases. 2004;39(11):1611–1617. doi: 10.1086/425315. [DOI] [PubMed] [Google Scholar]
- 13.Hayden FG, et al. Local and systemic cytokine responses during experimental human influenza A virus infection. Relation to symptom formation and host defense. The Journal of clinical investigation. 1998;101(3):643–649. doi: 10.1172/JCI1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yuen KY, et al. Clinical significance of alimentary tract microbes in bone marrow transplant recipients. Diagn Micr Infec Dis. 1998;30(2):75–81. doi: 10.1016/s0732-8893(97)00213-7. [DOI] [PubMed] [Google Scholar]
- 15.Abdel-Ghafar AN, et al. Update on avian influenza A (H5N1) virus infection in humans. N Engl J Med. 2008;358(3):261–273. doi: 10.1056/NEJMra0707279. [DOI] [PubMed] [Google Scholar]
- 16.Hers JF, et al. Enzyme histochemistry of bronchial epithelium and alveolar cells in the early stages of influenza-virus pneumonia of mice. Nature. 1962;193:348–349. doi: 10.1038/193348a0. [DOI] [PubMed] [Google Scholar]
- 17.Kuiken T, Taubenberger JK. Pathology of human influenza revisited. Vaccine. 2008;26(Suppl 4):D59–D66. doi: 10.1016/j.vaccine.2008.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taubenberger JK, Morens DM. The pathology of influenza virus infections. Annual review of pathology. 2008;3:499–522. doi: 10.1146/annurev.pathmechdis.3.121806.154316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu X, et al. Genetic characterization of the pathogenic influenza A/Goose/Guangdong/1/96 (H5N1) virus: similarity of its hemagglutinin gene to those of H5N1 viruses from the 1997 outbreaks in Hong Kong. Virology. 1999;261(1):15–19. doi: 10.1006/viro.1999.9820. [DOI] [PubMed] [Google Scholar]
- 20.Duan L, et al. The development and genetic diversity of H5N1 influenza virus in China, 1996–2006. Virology. 2008;380(2):243–254. doi: 10.1016/j.virol.2008.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WHO/OIE/FAO-H5N1-evolution-working-group. Continuing progress towards a unified nomenclature for the highly pathogenic H5N1 avian influenza viruses: divergence of clade 2.2 viruses. Influenza and other respiratory viruses. 2009;3(2):59–62. doi: 10.1111/j.1750-2659.2009.00078.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garcia-Sastre A. Inhibition of interferon-mediated antiviral responses by influenza A viruses and other negative-strand RNA viruses. Virology. 2001;279(2):375–384. doi: 10.1006/viro.2000.0756. [DOI] [PubMed] [Google Scholar]
- 23.Mibayashi M, et al. Inhibition of retinoic acid-inducible gene I-mediated induction of beta interferon by the NS1 protein of influenza A virus. J Virol. 2007;81(2):514–524. doi: 10.1128/JVI.01265-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jackson D, et al. A new influenza virus virulence determinant: the NS1 protein four C-terminal residues modulate pathogenicity. Proc Natl Acad Sci U S A. 2008;105(11):4381–4386. doi: 10.1073/pnas.0800482105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zamarin D, et al. Influenza virus PB1-F2 protein induces cell death through mitochondrial ANT3 and VDAC1. PLoS Pathog. 2005;1(1):e4. doi: 10.1371/journal.ppat.0010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McAuley JL, et al. Expression of the 1918 influenza A virus PB1-F2 enhances the pathogenesis of viral and secondary bacterial pneumonia. Cell host & microbe. 2007;2(4):240–249. doi: 10.1016/j.chom.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lopez CB, et al. Type I interferon induction pathway, but not released interferon, participates in the maturation of dendritic cells induced by negative-strand RNA viruses. J Infect Dis. 2003;187(7):1126–1136. doi: 10.1086/368381. [DOI] [PubMed] [Google Scholar]
- 28.Hatta M, et al. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science. 2001;293(5536):1840–1842. doi: 10.1126/science.1062882. [DOI] [PubMed] [Google Scholar]
- 29.Hatta M, et al. Growth of H5N1 Influenza A Viruses in the Upper Respiratory Tracts of Mice. PLoS Pathog. 2007;3(10):e133. doi: 10.1371/journal.ppat.0030133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dudley JP. Age-specific infection and death rates for human A(H5N1) avian influenza in Egypt. Euro Surveill. 2009;14(18) doi: 10.2807/ese.14.18.19198-en. [DOI] [PubMed] [Google Scholar]
- 31.Neumann G, et al. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nature. 2009;459(7249):931–939. doi: 10.1038/nature08157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.de Wit E, et al. Pathogenicity of highly pathogenic avian influenza virus in mammals. Vaccine. 2008;26(Suppl 4):D54–D58. doi: 10.1016/j.vaccine.2008.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Santhia K, et al. Avian influenza A H5N1 infections in Bali Province, Indonesia: a behavioral, virological and seroepidemiological study. Influenza and other respiratory viruses. 2009;3(3):81–89. doi: 10.1111/j.1750-2659.2009.00069.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vong S, et al. Risk factors associated with subclinical human infection with avian influenza A (H5N1) virus--Cambodia, 2006. J Infect Dis. 2009;199(12):1744–1752. doi: 10.1086/599208. [DOI] [PubMed] [Google Scholar]
- 35.Smallman-Raynor M, Cliff AD. Avian influenza A (H5N1) age distribution in humans. Emerg Infect Dis. 2007;13(3):510–512. doi: 10.3201/eid1303.060849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ly S, et al. Interaction between humans and poultry, rural Cambodia. Emerg Infect Dis. 2007;13(1):130–132. doi: 10.3201/eid1301.061014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Throsby M, et al. Heterosubtypic neutralizing monoclonal antibodies cross-protective against H5N1 and H1N1 recovered from human IgM+ memory B cells. PLoS ONE. 2008;3(12):e3942. doi: 10.1371/journal.pone.0003942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yuen KY, et al. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet. 1998;351(9101):467–471. doi: 10.1016/s0140-6736(98)01182-9. [DOI] [PubMed] [Google Scholar]
- 39.To KF, et al. Pathology of fatal human infection associated with avian influenza A H5N1 virus. J Med Virol. 2001;63(3):242–246. doi: 10.1002/1096-9071(200103)63:3<242::aid-jmv1007>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 40.Uiprasertkul M, et al. Influenza A H5N1 replication sites in humans. Emerg Infect Dis. 2005;11(7):1036–1041. doi: 10.3201/eid1107.041313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peiris JS, et al. Re-emergence of fatal human influenza A subtype H5N1 disease. Lancet. 2004;363(9409):617–619. doi: 10.1016/S0140-6736(04)15595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gu J, et al. H5N1 infection of the respiratory tract and beyond: a molecular pathology study. Lancet. 2007;370(9593):1137–1145. doi: 10.1016/S0140-6736(07)61515-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ng WF, To KF. Pathology of human H5N1 infection: new findings. Lancet. 2007;370(9593):1106–1108. doi: 10.1016/S0140-6736(07)61490-1. [DOI] [PubMed] [Google Scholar]
- 44.Ng WF, et al. The comparative pathology of severe acute respiratory syndrome and avian influenza A subtype H5N1--a review. Human pathology. 2006;37(4):381–390. doi: 10.1016/j.humpath.2006.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Buchy P, et al. Influenza A/H5N1 virus infection in humans in Cambodia. Journal of Clinical Virology. 2007;39(3):164–168. doi: 10.1016/j.jcv.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 46.de Jong MD, et al. Fatal avian influenza A (H5N1) in a child presenting with diarrhea followed by coma. N Engl J Med. 2005;352(7):686–691. doi: 10.1056/NEJMoa044307. [DOI] [PubMed] [Google Scholar]
- 47.Chutinimitkul S, et al. H5N1 influenza A virus and infected human plasma. Emerg Infect Dis. 2006;12(6):1041–1043. doi: 10.3201/eid1206.060227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cohen J. The immunopathogenesis of sepsis. Nature. 2002;420(6917):885–891. doi: 10.1038/nature01326. [DOI] [PubMed] [Google Scholar]
- 49.Bhatia M, Moochhala S. Role of inflammatory mediators in the pathophysiology of acute respiratory distress syndrome. The Journal of pathology. 2004;202(2):145–156. doi: 10.1002/path.1491. [DOI] [PubMed] [Google Scholar]
- 50.de Jong MD, et al. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nature Medicine. 2006;12(10):1203–1207. doi: 10.1038/nm1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Salomon R, et al. The polymerase complex genes contribute to the high virulence of the human H5N1 influenza virus isolate A/Vietnam/1203/04. Journal of Experimental Medicine. 2006;203(3):689–697. doi: 10.1084/jem.20051938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shinya K, et al. PB2 amino acid at position 627 affects replicative efficiency, but not cell tropism, of Hong Kong H5N1 influenza A viruses in mice. Virology. 2004;320(2):258–266. doi: 10.1016/j.virol.2003.11.030. [DOI] [PubMed] [Google Scholar]
- 53.Shinya K, et al. Avian flu: influenza virus receptors in the human airway. Nature. 2006;440(7083):435–436. doi: 10.1038/440435a. [DOI] [PubMed] [Google Scholar]
- 54.Nicholls JM, et al. Tropism of avian influenza A (H5N1) in the upper and lower respiratory tract. Nature Medicine. 2007;13(2):147–149. doi: 10.1038/nm1529. [DOI] [PubMed] [Google Scholar]
- 55.Nicholls JM, et al. Sialic acid receptor detection in the human respiratory tract: evidence for widespread distribution of potential binding sites for human and avian influenza viruses. Respir Res. 2007;8:73. doi: 10.1186/1465-9921-8-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.van Riel D, et al. H5N1 Virus Attachment to Lower Respiratory Tract. Science. 2006;312(5772):399. doi: 10.1126/science.1125548. [DOI] [PubMed] [Google Scholar]
- 57.van Riel D, et al. Human and avian influenza viruses target different cells in the lower respiratory tract of humans and other mammals. Am J Pathol. 2007;171(4):1215–1223. doi: 10.2353/ajpath.2007.070248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yao L, et al. Avian influenza receptor expression in H5N1-infected and noninfected human tissues. Faseb J. 2008;22(3):733–740. doi: 10.1096/fj.06-7880com. [DOI] [PubMed] [Google Scholar]
- 59.Doherty PC, Kelso A. Toward a broadly protective influenza vaccine. The Journal of clinical investigation. 2008;118(10):3273–3275. doi: 10.1172/JCI37232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thomas PG, et al. Cell-mediated protection in influenza infection. Emerg Infect Dis. 2006;12(1):48–54. doi: 10.3201/eid1201.051237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lee LY, et al. Memory T cells established by seasonal human influenza A infection cross-react with avian influenza A (H5N1) in healthy individuals. The Journal of clinical investigation. 2008;118(10):3478–3490. doi: 10.1172/JCI32460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Peiris JSM, et al. Re-emergence of fatal human influenza A subtype H5N1 disease. Lancet. 2004;363(9409):617–619. doi: 10.1016/S0140-6736(04)15595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Maines TR, et al. Pathogenesis of emerging avian influenza viruses in mammals and the host innate immune response. Immunological reviews. 2008;225(1):68–84. doi: 10.1111/j.1600-065X.2008.00690.x. [DOI] [PubMed] [Google Scholar]
- 64.Barnard DL. Animal models for the study of influenza pathogenesis and therapy. Antiviral Res. 2009;82(2):A110–A122. doi: 10.1016/j.antiviral.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mubareka S, et al. Transmission of influenza virus via aerosols and fomites in the guinea pig model. J Infect Dis. 2009;199(6):858–865. doi: 10.1086/597073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tumpey TM, et al. Depletion of lymphocytes and diminished cytokine production in mice infected with a highly virulent influenza A (H5N1) virus isolated from humans. J Virol. 2000;74(13):6105–6116. doi: 10.1128/jvi.74.13.6105-6116.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Szretter KJ, et al. Role of host cytokine responses in the apthogenesis of avian H5N1 influenza viruses in mice. J Virol. 2007;81(6):2736–2744. doi: 10.1128/JVI.02336-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Perrone LA, et al. H5N1 and 1918 pandemic influenza virus infection results in early and excessive infiltration of macrophages and neutrophils in the lungs of mice. PLoS Pathog. 2008;4(8):e1000115. doi: 10.1371/journal.ppat.1000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cameron CM, et al. Gene expression analysis of host innate immune responses during Lethal H5N1 infection in ferrets. J Virol. 2008;82(22):11308–11317. doi: 10.1128/JVI.00691-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Baskin CR, et al. Early and sustained innate immune response defines pathology and death in nonhuman primates infected by highly pathogenic influenza virus. Proc Natl Acad Sci U S A. 2009;106(9):3455–3460. doi: 10.1073/pnas.0813234106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kash JC, et al. Genomic analysis of increased host immune and cell death responses induced by 1918 influenza virus. Nature. 2006;443(7111):578–581. doi: 10.1038/nature05181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kobasa D, et al. Aberrant innate immune response in lethal infection of macaques with the 1918 influenza virus. Nature. 2007;445(7125):319–323. doi: 10.1038/nature05495. [DOI] [PubMed] [Google Scholar]
- 73.Szretter KJ, et al. Early control of H5N1 influenza virus replication by the type I interferon response in mice. J Virol. 2009;83(11):5825–5834. doi: 10.1128/JVI.02144-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zheng BJ, et al. Delayed antiviral plus immunomodulator treatment still reduces mortality in mice infected by high inoculum of influenza A/H5N1 virus. Proc Natl Acad Sci U S A. 2008;105(23):8091–8096. doi: 10.1073/pnas.0711942105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Aldridge JR, Jr, et al. TNF/iNOS-producing dendritic cells are the necessary evil of lethal influenza virus infection. Proc Natl Acad Sci U S A. 2009;106(13):5306–5311. doi: 10.1073/pnas.0900655106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Carey MA, et al. Contrasting effects of cyclooxygenase-1 (COX-1) and COX-2 deficiency on the host response to influenza A viral infection. J Immunol. 2005;175(10):6878–6884. doi: 10.4049/jimmunol.175.10.6878. [DOI] [PubMed] [Google Scholar]
- 77.Le Goffic R, et al. Detrimental contribution of the Toll-like receptor (TLR)3 to influenza A virus-induced acute pneumonia. PLoS Pathog. 2006;2(6):e53. doi: 10.1371/journal.ppat.0020053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Svitek N, et al. Severe seasonal influenza in ferrets correlates with reduced interferon and increased IL-6 induction. Virology. 2008;376(1):53–59. doi: 10.1016/j.virol.2008.02.035. [DOI] [PubMed] [Google Scholar]
- 79.Imai Y, et al. Identification of oxidative stress and Toll-like receptor 4 signaling as a key pathway of acute lung injury. Cell. 2008;133(2):235–249. doi: 10.1016/j.cell.2008.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Khoufache K, et al. Protective role for protease-activated receptor-2 against influenza virus pathogenesis via an IFN-gamma-dependent pathway. J Immunol. 2009;182(12):7795–7802. doi: 10.4049/jimmunol.0803743. [DOI] [PubMed] [Google Scholar]
- 81.Cheung CY, et al. Induction of proinflammatory cytokines in human macrophages by influenza A (H5N1) viruses: a mechanism for the unusual severity of human disease? Lancet. 2002;360(9348):1831–1837. doi: 10.1016/s0140-6736(02)11772-7. [DOI] [PubMed] [Google Scholar]
- 82.Chan MCW, et al. Proinflammatory cytokine responses induced by influenza A (H5N1) viruses in primary human alveolar and bronchial epithelial cells. Resp Res. 2005;6 doi: 10.1186/1465-9921-6-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hui KP, et al. Induction of proinflammatory cytokines in primary human macrophages by influenza A virus (H5N1) is selectively regulated by IFN regulatory factor 3 and p38 MAPK. J Immunol. 2009;182(2):1088–1098. doi: 10.4049/jimmunol.182.2.1088. [DOI] [PubMed] [Google Scholar]
- 84.Lee DCW, et al. p38 mitogen-activated protein kinase-dependent hyperinduction of tumor necrosis factor alpha expression in response to avian influenza virus H5N1. Journal of Virology. 2005;79(16):10147–10154. doi: 10.1128/JVI.79.16.10147-10154.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lee SM, et al. Hyperinduction of cyclooxygenase-2-mediated proinflammatory cascade: a mechanism for the pathogenesis of avian influenza H5N1 infection. J Infect Dis. 2008;198(4):525–535. doi: 10.1086/590499. [DOI] [PubMed] [Google Scholar]
- 86.Zeng H, et al. Highly pathogenic avian influenza H5N1 viruses elicit an attenuated type i interferon response in polarized human bronchial epithelial cells. J Virol. 2007;81(22):12439–12449. doi: 10.1128/JVI.01134-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mok CKP, et al. The Viral Genetic Determinants of H5N1 Influenza Viruses that Contribute To Cytokine Dysregulation. J Infect Dis. 2009 doi: 10.1086/605606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Guan Y, et al. H5N1 influenza: A protean pandemic threat. P Natl Acad Sci USA. 2004;101(21):8156–8161. doi: 10.1073/pnas.0402443101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mok CKP, et al. Differential onset of apoptosis in influenza A virus H5N1- and H1N1-infected human blood macrophages. Journal of General Virology. 2007;88:1275–1280. doi: 10.1099/vir.0.82423-0. [DOI] [PubMed] [Google Scholar]
- 90.Zhou JF, et al. Functional tumor necrosis factor-related apoptosis-inducing ligand production by avian influenza virus-infected macrophages. Journal of Infectious Diseases. 2006;193(7):945–953. doi: 10.1086/500954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Thitithanyanont A, et al. High susceptibility of human dendritic cells to avian influenza H5N1 virus infection and protection by IFN-alpha and TLR ligands. J Immunol. 2007;179(8):5220–5227. doi: 10.4049/jimmunol.179.8.5220. [DOI] [PubMed] [Google Scholar]
- 92.Mao H, et al. Influenza virus directly infects human natural killer cells and induces cell apoptosis. J Virol. 2009 doi: 10.1128/JVI.00805-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Qin G, et al. Phosphoantigen-Expanded Human gammadelta T Cells Display Potent Cytotoxicity against Monocyte-Derived Macrophages Infected with Human and Avian Influenza Viruses. J Infect Dis. 2009;200(6):858–865. doi: 10.1086/605413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kandun IN, et al. Factors associated with case fatality of human H5N1 virus infections in Indonesia: a case series. Lancet. 2008;372(9640):744–749. doi: 10.1016/S0140-6736(08)61125-3. [DOI] [PubMed] [Google Scholar]
- 95.Ludwig S. Targeting cell signalling pathways to fight the flu: towards a paradigm change in anti-influenza therapy. J Antimicrob Chemother. 2009;64(1):1–4. doi: 10.1093/jac/dkp161. [DOI] [PubMed] [Google Scholar]
- 96.Takano R, et al. A comparison of the pathogenicity of avian and swine H5N1 influenza viruses in Indonesia. Arch Virol. 2009;154(4):677–681. doi: 10.1007/s00705-009-0353-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Rubenfeld GD, et al. Incidence and outcomes of acute lung injury. N Engl J Med. 2005;353(16):1685–1693. doi: 10.1056/NEJMoa050333. [DOI] [PubMed] [Google Scholar]