Abstract
Background
Reducing added sugars intake is one of the Healthy People 2020 objectives. High added sugars intake may be associated with adverse health consequences.
Objective
This cross-sectional study identified sociodemographic and behavioral characteristics associated with added sugars intake among US adults (18 years and older) using the 2010 National Health Interview Survey data (n=24,967).
Methods
The outcome variable was added sugars intake from foods and beverages using scoring algorithms to convert dietary screener frequency responses on nine items to estimates of individual dietary intake of added sugars in teaspoons per day. Added sugars intake was categorized into tertiles (lowest, middle, highest) stratified by sex. The explanatory variables were sociodemographic and behavioral characteristics. Multinomial logistic regression was used to estimate the adjusted odds ratios for the highest and middle tertile added sugars intake groups as compared with the lowest tertile group.
Results
Estimated median added sugars intake was 17.6 tsp/d for men and 11.7 tsp/d for women. For men and women, those who had significantly greater odds for being in the highest tertile of added sugars intake (men: ≥22.0 tsp/d; women: ≥14.6 tsp/d) were younger, less educated, had lower income, were less physically active, were current smokers, and were former or current infrequent/light drinkers, whereas non-Hispanic other/multiracial and those living in the West had significantly lower odds for being in the highest tertile of added sugars intake. Different patterns were found by sex. Non-Hispanic black men had lower odds for being in the highest tertile of added sugars intake, whereas non-Hispanic black women had greater odds for being in the highest tertile.
Conclusions
One in three men consumed ≥22.0 tsp added sugars and one in three women consumed ≥14.6 tsp added sugars daily. Higher added sugars intake was associated with various sociodemographic and behavioral characteristics; this information can inform efforts to design programs and policies specific to high-intake populations.
Keywords: Added sugars, Sugar-sweetened beverages, Sweet food, Sociodemographic characteristics, Behaviors
The 2015–2020 dietary guidelines for americans defines added sugars as “syrups and other caloric sweeteners used as a sweetener in other food products. Specific examples of added sugars that can be listed as an ingredient include brown sugar, corn sweetener, corn syrup, dextrose, fructose, glucose, high-fructose corn syrup, honey, invert sugar, lactose, malt syrup, maltose, molasses, raw sugar, sucrose, trehalose, and turbinado sugar.”1 Naturally occurring sugars, such as fructose in fruits and lactose in milk and dairy products, are not considered added sugars.1 During food processing or preparation, added sugars are incorporated into foods and beverages to improve palatability and to extend the shelf life of products.1
The upper limits of calories from added sugars intake recommended by the American Heart Association are <150 kcal/d (approximately 9 tsp) for most American men and <100 kcal/d (approximately 6 tsp) for most American women.2 The 2015–2020 Dietary Guidelines for Americans recommends that Americans should limit their consumption of added sugars and that they consume <10% of total calories from added sugars per day.1 In the 2005–2010 National Health and Nutrition Examination Surveys (NHANES), the mean percentage of total calories from added sugars was 12.7% (335 kcal/d) for men and 13.2% (239 kcal/d) for women.3 Non-Hispanic blacks and adults with lower incomes consumed a larger percentage of total calories from added sugars compared with other adults in the population.3 In addition, 67% of calories from added sugars came from foods and 33% came from beverages among US adults.3 Many studies have shown that high consumption of added sugars (eg, >10% of total daily calories from added sugars) is associated with adverse health outcomes in adults, including obesity/weight gain,4,5 type 2 diabetes,6 cardiovascular disease,7,8 and periodontal disease.9
Although a few studies have investigated the associations between added sugars and sociodemographic characteristics among US adults, these studies did not examine behavioral factors related to added sugars intake.3,10 Certain unhealthy nondietary behaviors might be associated with unhealthy dietary behaviors.11,12 Identifying behavioral characteristics that coexist with high added sugars intake is important because this information can be used to inform intervention efforts to reach high-risk groups. The objective of this cross-sectional analysis was to examine the relationship between sociodemographic and behavioral factors and total added sugars intake for men and women using a nationally representative sample of civilian noninstitutionalized US adults. In addition, the relative contributions of foods and beverages to total added sugars intake are described for subgroups defined by demographic and behavioral variables.
METHODS
Study Sample and Survey Administration
Since 1957, the Centers for Disease Control and Prevention’s National Center for Health Statistics has conducted annually the National Health Interview Survey (NHIS). The NHIS uses a multistage sampling design to survey a representative sample of civilian noninstitutionalized US households. This cross-sectional analysis used data from the 2010 NHIS.13 Information on health and other characteristics of individual family members within the household was gathered using in-person interviews, and supplementary data were obtained from one randomly selected child (“Sample Child”) or one randomly selected adult (“Sample Adult”) from the household. The Sample Adult Module collected information on sociodemographic characteristics, occupations, certain medical conditions, illness, health status, functional limitations, health behaviors, and health care access and utilization. The Cancer Control Supplement, funded by the National Cancer Institute (NCI) and Centers for Disease Control and Prevention, collects additional behavioral information on sample adults (aged 18 years and older) and is administered every 5 years. The 2010 Cancer Control Supplement included a 26-item Dietary Screener Questionnaire, which was administered via computer-assisted personal interviewing. Adults reported the number of times per day, per week, or per month during the past month that they consumed selected foods and beverages.13,14 The 2010 NHIS was approved by the Research Ethics Review Board at the National Center for Health Statistics. The advance letter that is sent to potential respondents of NHIS before the interview is the consent statement. Each year, the Division of Health Interview Statistics, which conducts the NHIS, requests and is granted a waiver of documentation of signed informed consent for the NHIS.
Outcome Variables
Total calorie intake was not assessed in the NHIS and so the outcome variable was total added sugars intake estimated from reported frequency of foods and beverages during the past month by using NCI’s scoring algorithms. These algorithms convert dietary screener frequency responses on nine items (ie, regular soda, coffee/tea drinks, sport and energy drink, sweetened fruit drinks, chocolate/candy, doughnuts/sweet rolls/Danish/muffins/toaster pastries, cookies/cake/pie/brownies, ice cream/frozen desserts, and hot/cold cereals) to estimates of individual dietary intake of added sugars in teaspoons per day.10,13,15 A separate variable for sugar-sweetened beverages (SSB) was created from the four beverage intake items. For the development of the scoring algorithms, NCI used 24-hour dietary recall data from the 2003–2006 NHANES. More information on the scoring algorithms can be found at the NCI website.15 Because estimated total added sugars intake was not normally distributed, median intake values for total added sugars, added sugars from foods, and added sugars from SSBs are presented. As a categorical variable, three groups were created based on tertile distributions of total added sugars intake separately for men and women, because previous studies suggested a dose–response of added sugars intake on health outcomes, such as cardiovascular disease mortality7 and poor oral health.9
Explanatory Variables
The explanatory variables were sociodemographic and behavioral characteristics. Mutually exclusive response categories for each explanatory variable were created. Sociodemographic variables included age (18 to 24, 25 to 39, 40 to 59, or 60 years and older), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, or non-Hispanic other/multiracial), marital status (currently married/domestic partnership or not married), education (less than high school graduate, high school graduate or recipient of a general education development certificate, some college, or college graduate), annual family income (<$35,000, $35,000 to $74,999, $75,000 to $99,999, or ≥$100,000), and census region (Northeast, Midwest, South, and West).
Behavioral variables included reported participation in leisure-time physical activity for at least 10 minutes (0, >0 to <3, 3 to 5, or >5 times/wk), smoking status (never smokers, former smokers, or current smokers), and alcohol consumption (lifetime abstainer, former drinker, current infrequent/light drinker, or current moderate/heavier drinker).16 Lifetime abstainers were defined as <12 drinks in lifetime; former drinkers were defined as ≥12 drinks in lifetime but none in past year; current infrequent/light drinkers were defined as ≥12 drinks in lifetime and ≤3 drinks/wk in past year; and current moderate/heavier drinkers were defined as ≥12 drinks in lifetime and >3 drinks/wk in past year. Using self-reported weight and height data, weight status was categorized as underweight/normal weight (body mass index [BMI; calculated as kg/m2] <25), overweight (BMI 25 to <30), or obese (BMI ≥30).17
Statistical Analysis
In the 2010 NHIS, 27,157 adults aged 18 years and older completed the Sample Adult Module and the Cancer Control Supplement (response rate for the Sample Adult Module: 60.8%). Of these, a total of 2,190 (8%) were excluded from the study because of missing data on any of the nine foods used to estimate added sugars intake (n=2,073) or having extreme added sugars intake values (defined as >75th percentile value+2 times the interquartile range using the cube-root transformed variable) (n=117).10 Adults with missing responses on covariates were excluded from analyses when that variable was used in the analysis. The final analytic sample consisted of 24,967 adults (10,962 men and 14,005 women). When comparing the analytic sample and the sample of respondents who were excluded, there were no differences in age. However, the analytic sample contained a slightly higher proportion of females and non-Hispanic whites (χ2 test, P<0.05) than the excluded sample.
All analyses were stratified by sex. χ2 tests were used to examine the bivariate associations of sociodemographic and behavioral characteristics with total added sugars intake and P<0.05 to evaluate statistical significance. Multinomial logistic regression analysis was used to calculate adjusted odds ratio (aOR) and 95% CI for variables associated with the highest and middle tertiles of added sugars intake groups as compared with the lowest tertile of added sugars intake group. The multinomial logistic regression models included all explanatory variables in one model. Added sugars intake from foods was calculated by subtracting added sugars from SSB from total added sugars. SAS software (version 9.3, 2011, SAS Institute Inc) was used to perform all statistical analyses and account for the complex sampling design.
RESULTS
The study population distributions by sociodemographic and behavioral characteristics are shown in Table 1. Overall, 56% were women, 38% were aged 18 to 39 years, and 68% were non-Hispanic whites. The majority of men and women were in a married/domestic partnership, and about 60% of men and women had at least some college education. Based on χ2 tests, all sociodemographic and behavioral characteristics analyzed were significantly associated with the tertile distribution of estimated added sugars intake for both men and women (P≤0.01, Table 1).
Table 1.
Tertile distribution of estimated total added sugars intake from the dietary screener by sociodemographic and behavioral characteristics among US men and women aged 18 years and older—National Health Interview Survey, 2010
| Characteristic | Tertile Distribution of Total Added Sugars Intake During the Past Month by Men and Womena
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Men
|
Women
|
|||||||
| n (%)b | Tertile 1 (<13.5 tsp/d) | Tertile 2 (13.5 to <22.0 tsp/d) | Tertile 3 (≥22.0 tsp/d) | n (%)b | Tertile 1 (<9.2 tsp/d) | Tertile 2 (9.2 to <14.6 tsp/d) | Tertile 3 (≥14.6 tsp/d) | |
| ←%±standard error→ | ←%±standard error→ | |||||||
| All respondents | 10,962 | 33.0±0.6 | 33.1±0.5 | 33.9±0.6 | 14,005 | 32.7±0.5 | 33.2±0.5 | 34.2±0.5 |
| Age, y | 10,962 | 14,005 | ||||||
| 18 to 24 | 1,189 (13.3) | 14.0±1.3 | 28.5±1.6 | 57.5±1.9 | 1,387 (12.4) | 15.8±1.3 | 32.1±1.7 | 52.1±1.9 |
| 25 to 39 | 3,082 (27.2) | 21.0±0.8 | 34.7±1.0 | 44.3±1.0 | 3,725 (25.6) | 22.2±0.8 | 31.5±0.9 | 46.3±1.0 |
| 40 to 59 | 3,898 (36.8) | 35.7±0.9 | 33.6±0.8 | 30.7±0.9 | 4,775 (36.0) | 34.9±0.8 | 34.4±0.8 | 30.7±0.8 |
| 60 and older | 2,793 (22.7) | 54.0±1.2 | 33.2±1.1 | 12.8±0.8 | 4,118 (26.0) | 47.8±0.9 | 33.7±0.8 | 18.5±0.7 |
| Race/ethnicity | 10,962 | 14,005 | ||||||
| White, non-Hispanic | 6,354 (68.4) | 33.8±0.7 | 34.0±0.6 | 32.2±0.7 | 7,895 (68.1) | 33.6±0.6 | 34.4±0.6 | 32.0±0.7 |
| Black, non-Hispanic | 1,597 (10.6) | 31.8±1.5 | 31.4±1.3 | 36.8±1.4 | 2,356 (12.2) | 28.5±1.1 | 28.2±1.2 | 43.4±1.2 |
| Hispanic | 2,117 (15.1) | 26.3±1.2 | 30.8±1.2 | 42.2±2.1 | 2,627 (13.1) | 28.7±1.1 | 31.5±1.0 | 39.8±1.2 |
| Other/multiracial, non-Hispanic | 894 (5.9) | 42.2±2.1 | 32.1±2.0 | 25.6±1.9 | 1,127 (6.7) | 38.4±1.8 | 33.3±1.7 | 28.2±1.6 |
| Marital status | 10,949 | 13,980 | ||||||
| Married/domestic partnership | 6,032 (64.1) | 35.5±0.7 | 33.8±0.7 | 30.7±0.7 | 6,595 (59.2) | 33.1±0.7 | 33.8±0.6 | 33.1±0.7 |
| Not married | 4,917 (35.9) | 28.3±0.8 | 31.9±0.8 | 39.8±1.0 | 7,385 (40.8) | 32.0±0.7 | 32.2±0.7 | 35.8±0.8 |
| Education level | 10,917 | 13,958 | ||||||
| Less than high school | 1,871 (14.8) | 30.3±1.2 | 28.0±1.3 | 41.7±1.4 | 2,345 (13.6) | 30.6±1.2 | 26.8±1.0 | 42.6±1.3 |
| High school/GEDc | 2,901 (26.9) | 28.0±1.0 | 31.9±1.0 | 40.1±1.1 | 3,615 (26.1) | 31.2±0.9 | 30.9±1.1 | 37.9±1.1 |
| Some college | 3,075 (28.9) | 31.1±1.0 | 32.2±1.0 | 36.7±1.1 | 4,402 (32.4) | 31.0±0.9 | 33.6±0.9 | 35.5±0.9 |
| College graduate and beyond | 3,070 (29.4) | 40.5±1.0 | 37.9±1.0 | 21.7±0.9 | 3,596 (27.9) | 37.0±1.0 | 38.0±0.9 | 25.1±0.8 |
| Annual family income | 10,481 | 13,314 | ||||||
| <$35,000 | 4,192 (31.6) | 30.7±0.9 | 30.2±0.8 | 39.1±1.0 | 6,253 (35.9) | 30.2±0.7 | 29.4±0.7 | 40.4±0.8 |
| $35,000 to $74,999 | 3,413 (33.2) | 30.8±0.9 | 34.0±1.0 | 35.2±1.0 | 3,994 (32.3) | 31.6±0.9 | 33.3±0.8 | 35.1±1.0 |
| $75,000 to $99,999 | 1,106 (12.7) | 32.3±1.7 | 32.1±1.6 | 35.6±1.8 | 1,227 (11.8) | 32.6±1.5 | 36.1±1.5 | 31.3±1.6 |
| ≥$100,000 | 1,770 (22.4) | 38.4±1.3 | 36.6±1.3 | 25.0±1.4 | 1,840 (19.9) | 36.4±1.2 | 37.9±1.3 | 25.7±1.1 |
| Census region | 10,962 | 14,005 | ||||||
| Northeast | 1,730 (17.7) | 32.3±1.1 | 35.3±1.1 | 32.3±1.4 | 2,241 (17.4) | 32.0±1.2 | 35.5±1.3 | 32.5±1.2 |
| Midwest | 2,401 (23.0) | 32.6±1.2 | 32.4±1.1 | 35.1±1.2 | 3,100 (23.3) | 33.6±1.1 | 31.8±1.0 | 34.5±1.2 |
| South | 3,975 (35.2) | 32.2±1.0 | 30.9±0.8 | 36.9±1.1 | 5,169 (35.7) | 30.2±0.8 | 30.8±0.8 | 39.0±1.0 |
| West | 2,856 (24.1) | 34.8±1.1 | 35.5±1.2 | 29.7±1.2 | 3,495 (23.6) | 35.9±1.0 | 36.3±0.9 | 27.7±0.9 |
| Any leisure-time physical activity for at least 10 min | 10,811 | 13,840 | ||||||
| 0 times/wk | 3,392 (29.0) | 33.2±1.0 | 31.1±1.0 | 35.7±0.9 | 5,310 (35.2) | 31.0±0.8 | 29.0±0.8 | 40.0±0.9 |
| >0 to 3 times/wk | 2,448 (23.1) | 32.0±1.2 | 32.4±1.1 | 35.5±1.2 | 2,961 (22.2) | 30.2±1.0 | 36.9±1.2 | 32.9±1.0 |
| >3 to 5 times/wk | 1,332 (13.1) | 34.2±1.5 | 37.5±1.5 | 28.4±1.5 | 1,543 (11.5) | 36.8±1.5 | 36.0±1.4 | 27.2±1.4 |
| >5 times/wk | 3,639 (34.8) | 33.0±0.9 | 33.6±0.9 | 33.4±1.0 | 4,026 (31.1) | 34.7±1.0 | 34.4±0.9 | 30.8±0.9 |
| Smoking status | 10,946 | 13,993 | ||||||
| Never smoked | 5,757 (53.2) | 32.6±0.7 | 34.6±0.7 | 32.8±0.8 | 9,129 (64.6) | 34.1±0.6 | 34.6±0.6 | 31.4±0.6 |
| Former smoker | 2,822 (25.7) | 43.0±1.1 | 32.3±1.0 | 24.6±0.9 | 2,510 (18.2) | 38.1±1.3 | 35.6±1.2 | 26.4±1.0 |
| Current smoker | 2,367 (21.1) | 21.3±1.0 | 30.4±1.1 | 48.3±1.2 | 2,354 (17.2) | 21.7±1.0 | 25.3±1.1 | 53.1±1.2 |
| Alcohol intake | 10,829 | 13,923 | ||||||
| Lifetime abstainer | 1,589 (14.8) | 34.4±1.5 | 30.5±1.4 | 35.1±1.6 | 3,901 (25.8) | 36.3±1.0 | 30.2±0.9 | 33.5±1.1 |
| Former drinker | 1,706 (14.7) | 36.2±1.4 | 32.8±1.3 | 31.0±1.3 | 2,075 (14.0) | 35.5±1.3 | 31.2±1.3 | 33.3±1.3 |
| Current infrequent/light drinker | 4,479 (42.2) | 32.0±0.8 | 32.9±0.8 | 35.1±0.9 | 6,223 (46.6) | 29.7±0.7 | 34.9±0.7 | 35.4±0.7 |
| Current moderate/heavy drinker | 3,055 (28.3) | 31.9±1.0 | 35.2±1.0 | 32.9±1.1 | 1,724 (13.7) | 32.6±1.4 | 35.0±1.3 | 32.5±1.3 |
| Weight statusd | 10,883 | 13,476 | ||||||
| Underweight/normal weight | 3,354 (30.3) | 29.3±0.9 | 31.6±1.0 | 39.1±1.1 | 5,605 (43.8) | 31.1±0.8 | 34.8±0.8 | 34.2±0.8 |
| Overweight | 4,541 (41.4) | 33.7±0.9 | 34.6±0.9 | 31.7±0.9 | 3,918 (28.2) | 34.1±0.9 | 32.6±0.9 | 33.3±1.0 |
| Obese | 2,988 (28.3) | 35.8±1.1 | 32.6±1.0 | 31.6±1.0 | 3,953 (28.0) | 32.7±0.9 | 31.2±1.0 | 36.1±1.0 |
Based on χ2 tests across categories. All variables had P values ≤0.01 for both men and women.
Unweighted sample size and weighted percent are presented. Weighted percent may not add up 100% due to rounding.
GED=general education development certificate.
Based on body mass index (BMI; calculated as kg/m2). BMI <25 for underweight/normal weight, BMI 25 to <30 for overweight, and BMI ≥30 for obese.
For both men and women, those who had significantly greater odds for being in the highest tertile of added sugars intake (men: ≥22.0 tsp/d; women: ≥14.6 tsp/d) were younger (aOR range=2.52 to 18.52 for 18 to 59 years vs 60 years and older), less educated (aOR range=1.36 to 2.06 for less than high school, high school, or some college vs college graduate or beyond), had lower family income (aOR range=1.22 to 1.33; $35,000 to $74,999 for men and <$75,000 for women vs ≥$100,000), reported no physical activity (aOR=1.22 for men, aOR=1.64 for women vs >5 times/wk), were current smokers (aOR=1.96 for men, aOR=2.29 for women vs nonsmokers), and were former or current infrequent/light drinkers (aOR range=1.24 to 1.61 vs lifetime abstainers) (Table 2).
Table 2.
Adjusted odds ratios and 95% CI for estimated total added sugars intake from the dietary screener associated with sociodemographic and behavioral characteristics among US men and women aged 18 years and older—National Health Interview Survey, 2010
| Characteristic | Total Added Sugars Intake
|
|||
|---|---|---|---|---|
| Men (n=10,122)
|
Women (n=12,564)
|
|||
| Tertile 2 (13.5 to <22.0 tsp/d) | Tertile 3 (≥22.0 tsp/d) | Tertile 2 (9.2 to <14.6 tsp/d) | Tertile 3 (≥14.6 tsp/d) | |
| ←adjusted odds ratio (95% CI)a→ | ||||
| Age, y | ||||
| 18 to 24 | 3.38 (2.52–4.54)b | 18.52 (13.41–25.58)b | 2.92 (2.26–3.75)b | 9.91 (7.54–13.01)b |
| 25 to 39 | 2.82 (2.38–3.35)b | 10.46 (8.42–12.99)b | 2.01 (1.75–2.32)b | 6.48 (5.47–7.67)b |
| 40 to 59 | 1.51 (1.30–1.75)b | 3.84 (3.16–4.67)b | 1.38 (1.21–1.56)b | 2.52 (2.17–2.93)b |
| 60 and older | Reference | Reference | Reference | Reference |
| Race/ethnicity | ||||
| White, non-Hispanic | Reference | Reference | Reference | Reference |
| Black, non-Hispanic | 0.90 (0.74–1.08) | 0.80 (0.66–0.97)b | 0.99 (0.83–1.17) | 1.22 (1.03–1.45)b |
| Hispanic | 0.97 (0.80–1.18) | 1.11 (0.91–1.35) | 0.99 (0.85–1.16) | 1.03 (0.86–1.23) |
| Other/multiracial, non-Hispanic | 0.64 (0.51–0.81)b | 0.55 (0.43–0.71)b | 0.85 (0.69–1.03) | 0.78 (0.63–0.96)b |
| Marital status | ||||
| Married/domestic partnership | Reference | Reference | Reference | Reference |
| Not married | 0.93 (0.81–1.07) | 0.89 (0.78–1.03) | 0.94 (0.84–1.05) | 0.89 (0.79–1.01) |
| Education level | ||||
| Less than high school | 1.06 (0.86–1.31) | 2.06 (1.63–2.59)b | 1.01 (0.83–1.23) | 1.82 (1.47–2.26)b |
| High school/GEDc | 1.22 (1.02–1.45)b | 2.03 (1.68–2.46)b | 1.08 (0.91–1.27) | 1.63 (1.37–1.95)b |
| Some college | 1.02 (0.87–1.19) | 1.53 (1.27–1.84)b | 1.06 (0.92–1.22) | 1.36 (1.16–1.59)b |
| College graduate or beyond | Reference | Reference | Reference | Reference |
| Annual family income | ||||
| <$35,000 | 0.98 (0.81–1.20) | 1.23 (0.97–1.55) | 1.04 (0.87–1.25) | 1.33 (1.09–1.62)b |
| $35,000 to $74,999 | 1.11 (0.93–1.33) | 1.29 (1.06–1.58)b | 1.08 (0.92–1.27) | 1.22 (1.02–1.46)b |
| $75,000 to $99,999 | 0.96 (0.77–1.20) | 1.30 (1.00–1.69) | 1.09 (0.89–1.34) | 1.15 (0.92–1.44) |
| ≥$100,000 | Reference | Reference | Reference | Reference |
| Census region | ||||
| Northeast | 1.17 (1.01–1.36)b | 1.00 (0.85–1.18) | 1.10 (0.94–1.27) | 0.90 (0.76–1.05) |
| Midwest | 0.99 (0.85–1.16) | 0.89 (0.74–1.07) | 0.87 (0.76–1.00) | 0.77 (0.65–0.90)b |
| South | Reference | Reference | Reference | Reference |
| West | 1.03 (0.88–1.21) | 0.66 (0.55–0.79)b | 0.98 (0.85–1.12) | 0.64 (0.55–0.75)b |
| Any leisure-time physical activity for at least 10 min | ||||
| 0 times/wk | 1.06 (0.90–1.24) | 1.22 (1.04–1.44)b | 1.14 (0.99–1.32) | 1.64 (1.42–1.89)b |
| >0 to 3 times/wk | 0.98 (0.84–1.14) | 1.13 (0.95–1.34) | 1.36 (1.16–1.59)b | 1.36 (1.17–1.57)b |
| >3 to 5 times/wk | 1.03 (0.85–1.24) | 0.80 (0.65–1.00) | 0.96 (0.79–1.16) | 0.80 (0.66–0.98)b |
| >5 times/wk | Reference | Reference | Reference | Reference |
| Smoking status | ||||
| Never smoked | Reference | Reference | Reference | Reference |
| Former smoker | 0.87 (0.75–1.00) | 0.93 (0.80–1.08) | 0.99 (0.86–1.14) | 1.04 (0.89–1.22) |
| Current smoker | 1.29 (1.09–1.52)b | 1.96 (1.66–2.30)b | 1.06 (0.90–1.25) | 2.29 (1.98–2.65)b |
| Alcohol intake | ||||
| Lifetime abstainer | Reference | Reference | Reference | Reference |
| Former drinker | 1.36 (1.09–1.70)b | 1.61 (1.25–2.07)b | 1.23 (1.03–1.47)b | 1.24 (1.03–1.49)b |
| Current infrequent/light drinker | 1.23 (1.03–1.47)b | 1.39 (1.13–1.70)b | 1.41 (1.24–1.61)b | 1.37 (1.18–1.59)b |
| Current moderate/heavy drinker | 1.28 (1.06–1.56)b | 1.19 (0.96–1.48) | 1.26 (1.06–1.49)b | 1.07 (0.87–1.32) |
| Weight statusd | ||||
| Underweight/normal weight | Reference | Reference | Reference | Reference |
| Overweight | 1.04 (0.91–1.20) | 0.94 (0.81–1.10) | 0.90 (0.79–1.03) | 0.95 (0.82–1.10) |
| Obese | 0.91 (0.78–1.07) | 0.76 (0.64–0.91)b | 0.88 (0.77–1.01) | 0.97 (0.84–1.11) |
Multivariate logistic regression models included all variables in one model separately by sex. The comparison group for multivariate logistic regression analysis was tertile 1 category for men (<13.5 tsp/d) and women (<9.2 tsp/d).
Considered statistically significant based on the 95% CI.
GED=general education development certificate.
Based on body mass index (BMI; calculated as kg/m2). BMI <25 for underweight/normal weight, BMI 25 to <30 for overweight, and BMI ≥30 for obese.
For both men and women, lower odds for being in the highest tertile of added sugars intake was significantly associated with being non-Hispanic other/multiracial (aOR=0.55 for men and aOR=0.78 for women vs non-Hispanic white) and living in the West (aOR=0.66 for men and aOR=0.64 for women vs South). For men, lower odds for being in the highest tertile of added sugars intake (≥22.0 tsp/d) was also associated with being non-Hispanic black (aOR=0.80 vs non-Hispanic white) and obese (aOR=0.76, BMI ≥30 vs BMI <25). For women, being non-Hispanic black (aOR=1.22 vs non-Hispanic white) had significantly greater odds for being in the highest tertile of added sugars intake (≥14.6 tsp/d), but those living in the Midwest (aOR=0.77 vs South) had lower odds for being in the highest tertile of added sugars intake. For both men and women, the odds for being in the highest tertile of added sugars intake did not differ between Hispanics and non-Hispanic whites and between current moderate/heavy drinkers and lifetime abstainers of alcohol (Table 2). When only sociodemographic variables were included in the multinomial logistic regression model without behavioral variables, the findings remained the same for both men and women (data not shown). Although findings for the middle tertile of added sugars intake (tertile 2) were somewhat similar to those findings for the highest tertile of added sugars (tertile 3), the magnitude of association was attenuated for tertile 2 (Table 2).
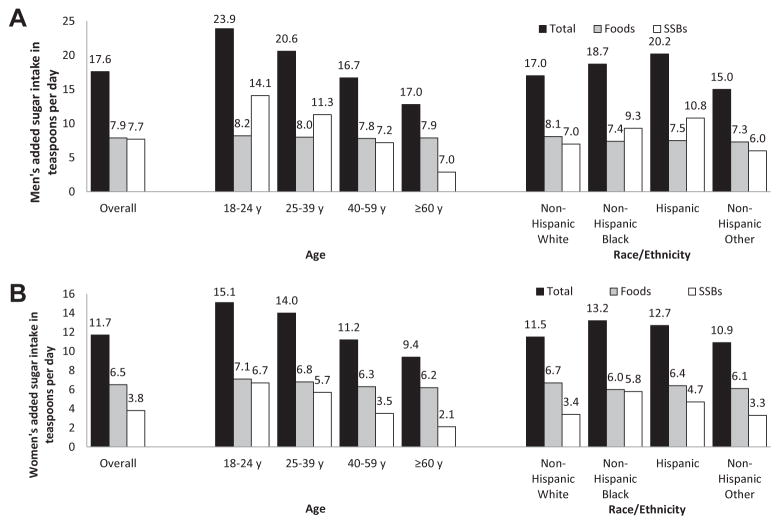
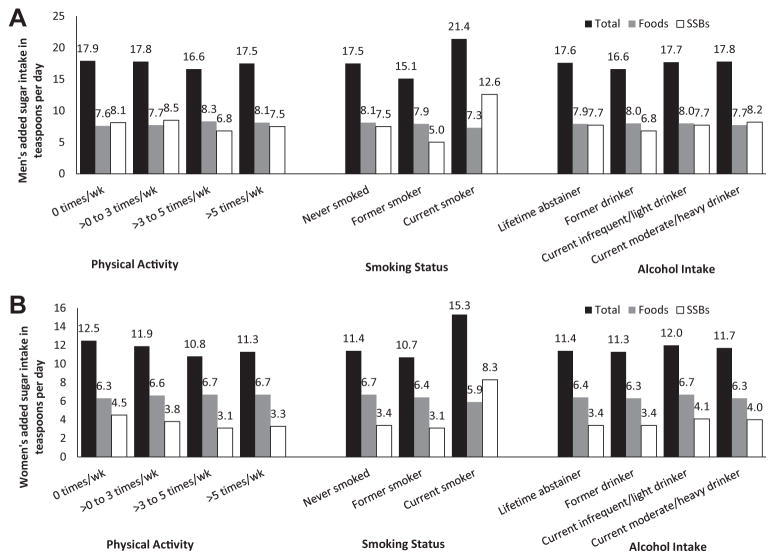
For descriptive statistics, the contribution of foods and SSBs to added sugars for men and women, as well as by age and race/ethnicity, are shown in Figure 1. Estimated median intake of added sugars was 17.6 tsp/d for men (Figure 1A) and 11.7 tsp/d for women (Figure 1B). For men, the overall median intake of added sugars from foods was similar to that for SSBs (7.9 and 7.7 tsp/d, respectively). However, the relative contributions of added sugars from foods and SSBs to total added sugars varied by the age and race/ethnicity of the men. For example, the median intake of added sugars from SSBs was higher than those from foods among younger men and Hispanic men. For women, overall median intake of added sugars from foods was higher than that for SSBs (6.5 and 3.8 tsp/d, respectively), and the same pattern was observed in older women and in non-Hispanic white and non-Hispanic other/multiracial women. For descriptive statistics, the contributions of foods and SSBs to total added sugars by behavioral characteristics are shown in Figure 2. This relative contribution varied by smoking status for men (Figure 2A) and women (Figure 2B); median intake of added sugars from SSBs was higher than those from foods among current smokers in both men and women. Patterns seen across subgroups defined by physical activity and alcohol consumption were similar.
Figure 1.
Estimated median intake of total added sugars from the dietary screener and the contribution of foods and sugar-sweetened beverages to total added sugars for men (A) and women (B) aged 18 years and older by age and race/ethnicity—National Health Interview Survey, 2010.
Figure 2.
Estimated median intake of total added sugars from the dietary screener and the contribution of foods and sugar-sweetened beverages to total added sugars for men (A) and women (B) aged 18 years and older by any leisure-time physical activity for at least 10 minutes, smoking status, and alcohol intake—National Health Interview Survey, 2010.
DISCUSSION
The NHIS offers a valuable resource for examining associations among a wide array of both demographic and behavioral variables of interest in public health policy and practice. Although NHIS lacks the 24-hour recall data collected in NHANES, the NHIS has particular advantages. It surveys a larger sample than NHANES and allows us to stratify by sex and still consider a wide range of sociodemographic and behavioral variables. The current study focused on the particular dietary factor of added sugars, a variable that has been related to a variety of conditions and diseases. In this analysis of NHIS data, 1 in 3 men consumed at least 22.0 tsp (358 kcal) of added sugars and 1 in 3 women consumed at least 14.6 tsp (237 kcal) of added sugars daily, based on the tertile distribution cutoffs. In addition, high consumption of added sugars was associated with a number of sociodemographic and behavioral characteristics among US men and women.
In the 2010 NHIS, added sugars was assessed by nine questions on a screener rather than by a more accurate and thorough diet assessment tool, such as the 24-hour recall.15 Despite this, for adults, the screener estimates of median added sugars intake in the 2010 NHIS were comparable to 24-hour recall estimates in the 2007–2010 NHANES: 17.6 tsp/d vs 17.1 tsp/d among men and 11.7 tsp/d vs 12.7 tsp/d among women.18 In addition, the present study found that relationships between added sugars and demographic variables in the NHIS mirrored results from NHANES: added sugars intake was higher among younger, less educated, and adults with lower incomes than their counterparts.3,10,18 Consistent with earlier analyses by Park and colleagues,19 the South was the region with the highest intakes. Although there is limited information on the regional variation of total added sugars intake among the US adult population, previous studies reported that SSB intake varied by states and geographical regions.12,19–22 Potential reasons for this geographical variation may be differences in the food environment, such as the availability/access of foods and beverages, advertising, culture, and regulations.23–26
These analyses add to existing knowledge by examining important behavioral variables associated with added sugars consumption controlling for demographics. For example, the present study found that physically inactive men and women had 22% and 64%, respectively, higher odds for being in the highest tertile of added sugars intake compared to men and women who were physically active. Consistent with findings in the present study, a previous study12 reported that daily SSB intake was associated with physical inactivity among US adults. The inverse association of physical activity with higher added sugars intake is also consistent with studies that have found that physically inactive adults have poorer diet quality in other dimensions than physically active adults.27,28
Regardless of sociodemographic factors, smokers consumed the highest amounts of added sugars in the present study. This is consistent with other studies that have found smokers have other less healthy dietary7,11,12 and health behaviors.11 The clustering may reflect overall attitudes about health and engaging in healthy behaviors. The finding might also reflect differences in taste perception caused by smoking. Previous studies showed that smokers had decreased sensitivity (or increased thresholds) to sucrose,29,30 indicating smokers might be less likely to perceive a food as sweet and thus eat more. In addition, some research indicates that addictions and addictive-like behaviors can be shared across domains, for example, smoking and food, in this case, added sugars.31–33
In the present analyses, added sugars consumption varied by the pattern of alcohol consumption; added sugars intake was higher among former alcohol drinkers or current infrequent/light alcohol drinkers than lifetime abstainers of alcohol, but there was no difference in added sugars intake between current moderate/heavy drinker and lifetime abstainers of alcohol after controlling for other factors. A previous study reported that alcohol drinkers had lower odds of consuming SSB at least once per day than non–alcohol drinkers among US adults.12 The reason for this finding in the present study is not clear. Unlike the findings from research on smokers, evidence that those who drink alcohol have a differential preference for sweets is inconsistent.34–36 Potentially, those who drink lightly are more likely to mix their alcohol with SSBs. Research that tests this and other hypotheses could improve the design of interventions to address excessive added sugars intake.
In addition, the present study found that obese men had 24% lower odds for consuming ≥22.0 tsp/d of total added sugars than underweight/normal-weight men, and weight status was not associated with added sugars intake among women after controlling for other factors. It is possible that obese men might decrease their added sugars intake as a strategy for weight control.
While the present study analyzed data from a large, nationally representative sample of US adults and included various behavioral characteristics, there are at least two limitations. First, the outcome variable (ie, total added sugars) was estimated from questions about usual intake of nine items on a screener rather than from a less-biased instrument that collects complete information on daily food and beverage intake, such as a 24-hour recall.15 However, the fact that the relationships found among important demographic variables are consistent with the findings based on NHANES data using 24-hour recall is reassuring. Second, food environmental variables (eg, access to supermarkets and food outlets) were not included in the study because the 2010 NHIS did not collect such information.
CONCLUSIONS
Based on the tertile distribution cutoff points, 1 in 3 men consumed at least 22.0 tsp of added sugars and 1 in 3 women consumed at least 14.6 tsp of added sugars daily. Findings in the present study showed that higher added sugars intake was associated independently with various sociodemographic and behavioral characteristics, such as younger age, lower education, lower income, physical inactivity, current smoking status, and alcohol intake. This information may inform intervention efforts by characterizing high-intake populations and aiding efforts to reduce their added sugars intake.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
STATEMENT OF POTENTIAL CONFLICT OF INTEREST
No potential conflict of interest was reported by the authors.
FUNDING/SUPPORT
There is no funding to disclose.
References
- 1.US Department of Agriculture, US Department of Health and Human Services. Dietary Guidelines for Americans, 2015–2020. 8. Washington, DC: US Government Printing Office; 2015. [Accessed March 8, 2016]. http://health.gov/dietaryguidelines/2015/guidelines/?linkId=20169028. [Google Scholar]
- 2.Johnson RK, Appel LJ, Brands M, et al. Dietary sugars intake and cardiovascular health: A scientific statement from the American Heart Association. Circulation. 2009;120(11):1011–1020. doi: 10.1161/CIRCULATIONAHA.109.192627. [DOI] [PubMed] [Google Scholar]
- 3.Ervin RB, Ogden CL. Consumption of added sugars among US adults, 2005–2010. NCHS Data Brief. 2013;(122):1–8. [PubMed] [Google Scholar]
- 4.Te Morenga L, Mallard S, Mann J. Dietary sugars and body weight: Systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ. 2013;346:e7492. doi: 10.1136/bmj.e7492. [DOI] [PubMed] [Google Scholar]
- 5.Bray GA, Nielsen SJ, Popkin BM. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am J Clin Nutr. 2004;79(4):537–543. doi: 10.1093/ajcn/79.4.537. [DOI] [PubMed] [Google Scholar]
- 6.Sonestedt E, Overby NC, Laaksonen DE, Birgisdottir BE. Does high sugar consumption exacerbate cardiometabolic risk factors and increase the risk of type 2 diabetes and cardiovascular disease? Food Nutr Res. 2012:56. doi: 10.3402/fnr.v56i0.19104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang Q, Zhang Z, Gregg EW, Flanders WD, Merritt R, Hu FB. Added sugar intake and cardiovascular diseases mortality among US adults. JAMA Intern Med. 2014;174(4):516–524. doi: 10.1001/jamainternmed.2013.13563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DiNicolantonio JJ, Lucan SC. The wrong white crystals: Not salt but sugar as aetiological in hypertension and cardiometabolic disease. Open Heart. 2014;1(1):e000167. doi: 10.1136/openhrt-2014-000167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lula EC, Ribeiro CC, Hugo FN, Alves CM, Silva AA. Added sugars and periodontal disease in young adults: An analysis of NHANES III data. Am J Clin Nutr. 2014;100(4):1182–1187. doi: 10.3945/ajcn.114.089656. [DOI] [PubMed] [Google Scholar]
- 10.Thompson FE, McNeel TS, Dowling EC, Midthune D, Morrissette M, Zeruto CA. Interrelationships of added sugars intake, socioeconomic status, and race/ethnicity in adults in the United States: National Health Interview Survey, 2005. J Am Diet Assoc. 2009;109(8):1376–1383. doi: 10.1016/j.jada.2009.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee CG, Seo DC, Middlestadt SE, Lin HC. Does the relationship between cigarette smoking and other key health behaviors vary by geographic area among US young adults? A multilevel analysis. Int J Behav Med. 2015;22(4):481–488. doi: 10.1007/s12529-014-9452-0. [DOI] [PubMed] [Google Scholar]
- 12.Park S, Pan L, Sherry B, Blanck HM. Consumption of sugar-sweetened beverages among US adults in 6 states: Behavioral Risk Factor Surveillance System, 2011. Prev Chronic Dis. 2014;11:E65. doi: 10.5888/pcd11.130304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. NHIS Survey Description. Hyattsville, MD: National Center for Health Statistics; 2011. [Accessed March 8, 2016]. 2010 National Health Interview Survey (NHIS) Public Use Data Release. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2010/srvydesc.pdf. [Google Scholar]
- 14.National Cancer Institute. [Accessed March 8, 2016];Dietary Screener Questionnaire in the National Health Interview Survey Cancer Control Supplement 2010: Overview. http://epi.grants.cancer.gov/nhis/2010-screener/. Revised November 2, 2015.
- 15.National Cancer Institute. [Accessed March 8, 2016];Dietary Screener Questionnaire (DSQ) in the NHANES 2009–10: Data Processing & Scoring Procedures. http://epi.grants.cancer.gov/nhanes/dietscreen/scoring/. Revised October 15, 2015.
- 16.Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for US adults: National Health Interview Survey, 2010. Vital Health Stat. 2012;10(252):1–207. [PubMed] [Google Scholar]
- 17.National Heart, Lung, and Blood Institute. The evidence report. Bethesda, MD: National Institutes of Health; 1998. [Accessed March 8, 2016]. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. NIH Publication No. 98–4083. http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf. [Google Scholar]
- 18.National Cancer Institute. Usual intake of added sugars. Table A40. [Accessed March 8, 2016];Added sugars: Means, percentiles and standard errors of usual intake, 2007–2010. http://appliedresearch.cancer.gov/diet/usualintakes/pop/2007-10/table_a40.html. Revised June 2, 2015.
- 19.Park S, Onufrak S, Sherry B, Blanck HM. The relationship between health-related knowledge and sugar-sweetened beverage intake among US adults. J Acad Nutr Diet. 2014;114(7):1059–1066. doi: 10.1016/j.jand.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kumar GS, Pan L, Park S, Lee-Kwan SH, Onufrak S, Blanck HM. Sugar-sweetened beverage consumption among adults—18 states, 2012. MMWR Morb Mortal Wkly Rep. 2014;63(32):686–690. [PMC free article] [PubMed] [Google Scholar]
- 21.Park S, McGuire LC, Galuska DA. Regional differences in sugar-sweetened beverage intake among US adults. J Acad Nutr Diet. 2015;115(12):1996–2002. doi: 10.1016/j.jand.2015.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park S, Xu F, Town M, Blanck HM. Prevalence of sugar-sweetened beverage intake among adults—23 states and the District of Columbia, 2013. MMWR Morb Mortal Wkly Rep. 2016;65(7):169–174. doi: 10.15585/mmwr.mm6507a1. [DOI] [PubMed] [Google Scholar]
- 23.Martin-Biggers J, Yorkin M, Aljallad C, et al. What foods are US supermarkets promoting? A content analysis of supermarket sales circulars. Appetite. 2013;62:160–165. doi: 10.1016/j.appet.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 24.Tucker KL, Maras J, Champagne C, et al. A regional food-frequency questionnaire for the US Mississippi Delta. Public Health Nutr. 2005;8(1):87–96. [PubMed] [Google Scholar]
- 25.Pomeranz JL. Advanced policy options to regulate sugar-sweetened beverages to support public health. J Public Health Policy. 2012;33(1):75–88. doi: 10.1057/jphp.2011.46. [DOI] [PubMed] [Google Scholar]
- 26.Studdert DM, Flanders J, Mello MM. Searching for public health law’s sweet spot: The regulation of sugar-sweetened beverages. PLoS Med. 2015;12(7):e1001848. doi: 10.1371/journal.pmed.1001848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Erinosho TO, Thompson OM, Moser RP, Yaroch AL. Fruit and vegetable intake of US adults: Comparing intake by mode of survey administration. J Am Diet Assoc. 2011;111(3):408–413. doi: 10.1016/j.jada.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 28.Wang Y, Chen X. Between-group differences in nutrition- and health-related psychosocial factors among US adults and their associations with diet, exercise, and weight status. J Acad Nutr Diet. 2012;112(4):486–498. e483. doi: 10.1016/j.jand.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pepino MY, Mennella JA. Effects of cigarette smoking and family history of alcoholism on sweet taste perception and food cravings in women. Alcohol Clin Exp Res. 2007;31(11):1891–1899. doi: 10.1111/j.1530-0277.2007.00519.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sato K, Endo S, Tomita H. Sensitivity of three loci on the tongue and soft palate to four basic tastes in smokers and non-smokers. Acta Otolaryngol Suppl. 2002;546:74–82. doi: 10.1080/00016480260046445. [DOI] [PubMed] [Google Scholar]
- 31.Mahler SV, de Wit H. Cue-reactors: Individual differences in cue-induced craving after food or smoking abstinence. PLoS One. 2010;5(11):e15475. doi: 10.1371/journal.pone.0015475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thorgeirsson TE, Gudbjartsson DF, Sulem P, et al. A common biological basis of obesity and nicotine addiction. Transl Psychiatry. 2013;3:e308. doi: 10.1038/tp.2013.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fortuna JL. Sweet preference, sugar addiction and the familial history of alcohol dependence: Shared neural pathways and genes. J Psychoactive Drugs. 2010;42(2):147–151. doi: 10.1080/02791072.2010.10400687. [DOI] [PubMed] [Google Scholar]
- 34.Tremblay KA, Bona JM, Kranzler HR. Effects of a diagnosis or family history of alcoholism on the taste intensity and hedonic value of sucrose. Am J Addict. 2009;18(6):494–499. doi: 10.3109/10550490903206023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kampov-Polevoy AB, Garbutt JC, Khalitov E. Family history of alcoholism and response to sweets. Alcohol Clin Exp Res. 2003;27(11):1743–1749. doi: 10.1097/01.ALC.0000093739.05809.DD. [DOI] [PubMed] [Google Scholar]
- 36.Fischer ME, Cruickshanks KJ, Schubert CR, et al. Taste intensity in the Beaver Dam Offspring Study. Laryngoscope. 2013;123(6):1399–1404. doi: 10.1002/lary.23894. [DOI] [PMC free article] [PubMed] [Google Scholar]