Abstract
Stanford Type A aortic dissection is a rapidly progressing disease process that is often fatal without emergent surgical repair. A small proportion of Type A dissections go undiagnosed in the acute phase and are found upon delayed presentation of symptoms or incidentally. These chronic lesions may have a distinct natural history that may have a better prognosis and could potentially be managed differently then those presenting acutely. The method of repair depends on location and extent of the false lumen, as well as involvement of critical structures and branch arteries. Surgical repair techniques similar to those employed for acute dissection management are currently first-line therapy for chronic cases that involve the aortic valve, sinuses of Valsalva, coronary arteries, and supra-aortic branch arteries. In patients with high-risk for surgery, endovascular repairs have been successful, and active development of delivery systems and grafts will continue to enhance outcomes. We present two cases of chronic Type A aortic dissection and review the current literature.
Keywords: Chronic aortic dissection, Stanford Type A dissection, Thoracic endovascular aortic repair
Introduction
Stanford Type A aortic dissections are life-threatening emergencies in the acute phase that require immediate surgical repair, in contradistinction to dissections limited to the descending aorta, which can be managed medically in most cases. The emergency of acute Type A dissections (ATAD) is defined by the high propensity to quickly develop severe complications including aortic rupture, severe aortic regurgitation, pericardial tamponade, and cerebral and coronary malperfusion. Mortality estimates suggest 40% are fatal prior to reaching a hospital, 1% die per hour upon arrival, and perioperative mortality of repair is 5–20% [1]. These statistics do not account for cases that are incorrectly diagnosed, due to prehospital mortality or failure to recognize dissection as the cause of a complication.
Chronic Type A dissections (CTAD) of the native aorta represent a subset of patients who were not diagnosed at the time of onset due to absent or atypical symptoms and remained stable, in contrast to the majority of symptomatic ATAD. Chronic aortic dissections are traditionally defined as those older than 14 days. A designation of subacute has also been proposed for dissections at 14–90 days, placing chronic at more than 90 days, though these definitions are less commonly utilized [2]. Few Type A dissections advance to the chronic phase, and thus the natural progression of CTAD is not well understood. The current standard management of CTAD is also open surgical aortic repair; however, a range of disease characteristics and associated pathologies may have implications for prognosis and repair. Moreover, new successes with endovascular techniques are providing credence for alternative repair approaches.
Case Presentation
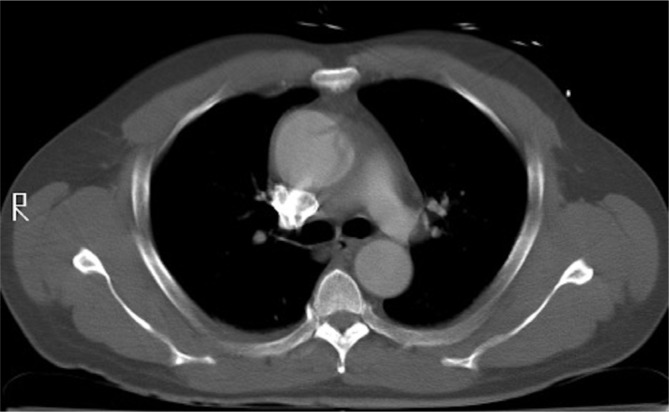
The first case is that of a 57-year-old male with a history of hypertension and alcohol abuse who presented with dizziness and chest pain and reported having similar though milder bouts of chest pain over the preceding 2 years. Transesophageal echocardiogram (TEE) showed moderate aortic insufficiency (AI) and aortic root dilatation. Contrast-enhanced computed tomography (CECT) revealed a dissection of the ascending aorta and 5.5 cm fusiform dilatation limited to the ascending aorta (Figure 1). The patient was taken to the operating room for open repair. Intraoperatively the intimal tear was identified 2 cm distal to the sinotubular junction on the anterolateral aspect of the aorta, and exhibited evidence of chronicity based on thickening of the septum and fibrotic changes. The false lumen was confined to the ascending aorta; however, it extended into the right coronary sinus. The patient, therefore, underwent a repair of the ascending aorta with Dacron interposition graft and resuspension of the aortic valve. TEE at the end of the procedure showed trace AI. His postoperative course was uncomplicated. He survived without recurrence of symptoms or AI until 8 years later when he died of complications of pancreatic cancer.
Figure 1.
Stanford Type A dissection confined to the ascending aorta with associated aneurysm.
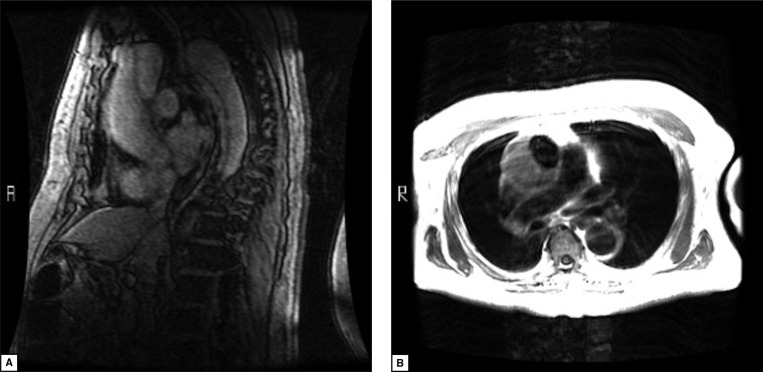
The second case is a 76-year-old male with a history of hypertension and a known abdominal aortic dissection previously diagnosed incidentally. He had delayed follow up imaging of the thoracic aorta for several months, but ultimately presented with complaints of recurrent chest pain. CECT found a dissection extending from ascending aorta down to infrarenal abdominal aorta (Figure 2). The ascending aorta and root were dilated to 5.5 cm and contained thrombus in the false lumen, which extended into the left coronary sinus as well as the innominate artery. Magnetic resonance imaging revealed signals consistent with chronic thrombus of the false lumen (Figure 3). The patient underwent aortic repair with composite mechanical valve graft and hemiarch replacement. Cannulations of the left femoral artery and right atrium were made for cardiopulmonary bypass. Hypothermic circulatory arrest at 18°C was instituted for distal anastomosis of the hemiarch repair. This was complicated by postoperative complete heart block managed by placement of a permanent transvenous pacemaker. He had no further aortic disease complications and died 2.5 years later of cardiac arrest during an admission for non-obstructive bowel ileus.
Figure 2.
Stanford Type A dissection extending from the ascending aorta into the descending aorta with a chronic thrombus of the false lumen in the ascending aorta.
Figure 3.
Magnetic resonance imaging showing chronic thrombus of the Type A false lumen confined to the ascending aorta. Panel A. Saggital-left image in proof. Panel B. Axial-right image.
Discussion
Natural History
Given that ATAD is often rapidly fatal without surgical management, patients with CTAD likely have pathologic or physiologic differences that allow for stabilization of the disease process. A recent review of 696 Type A dissection (TAD) repairs found that CTADs were significantly more likely to have bicuspid aortic valve morphology and less likely to extend beyond the arch, compared with ATAD [3]. Somewhat intuitively, a greater proportion of CTAD had undergone previous cardiac surgery; however, postoperative dissections are likely a separate disease process from spontaneous CTAD. Chronic cases were reported as asymptomatic 69% of the time, with a median of 10 weeks until symptom onset in patients who became symptomatic. Following open repair, the same study found in-hospital mortality for CTAD to be 1/3 of the rate for ATAD (4.5% vs. 13.2%), corroborating previous reports [4], and survival to be longer (80% vs. 68%) at 5 years and at 10 years (64% vs. 49%).
The relative stability of CTAD provides logical support for medical management of uncomplicated asymptomatic lesions. Furthermore, histologic evaluations suggest a remodeling process that may stabilize the false lumen through development of a new endothelial lining and thickening of the media by production of new smooth muscle cells [5]. However, there is no significant body of data to adequately define the outcomes of nonoperative management for this subset of patients. In fact, many cases reportedly have been associated with sudden onset of delayed symptoms, false lumen expansion, and progressive aneurysmal dilatation.
Classification
The type of intimal lesion may influence disease progression in CTAD though, in general, Type A lesions tend to be more progressive and do not mirror the natural history of Type B lesions [6]. Intimal tears of the aorta are stratified into five classes based on imaging characteristics according to the European Society of Cardiology [7]. Class I tears have the standard pairing of true and false lumina, involving variable length of aorta that determine associated symptoms and type of necessary repair. Class II, also known as intramural hematomas (IMH), do not have an intimal tear visible on imaging, though a majority have a tear seen at the time of surgery or autopsy [1]. Stable IMH of the ascending aorta is believed to portend slightly better outcomes than Class I tears, and have been reported to resorb in some cases. However, 1-year mortality with medical management of these lesions is approximately 60%, whereas open ascending aortic repair decreases 1-year mortality to 5–26% depending on patient characteristics and center experience [8]. Class III tears do not have separation of the medial layers, and thus create an eccentric mural bulge that undermines a small area of intima and are difficult to detect on imaging. Class IV, commonly referred to as penetrating atheromatous ulcerations (PAU), are tears down to the adventitia that form adjacent to atheromatous plaques. Although rarely found in the ascending aorta, PAU in this region are associated with increased rate of aneurysmal dilatation, and therefore should be repaired upon diagnosis [2]. Class V lesions are iatrogenic tears associated with endovascular procedures or previous aortic surgery [1].
Surgical Technique
Though surgical guidelines for the management of CTAD are limited by the paucity of data, generally accepted indications for aortic repair include onset of severe AI, enlarging ascending aortic diameter or onset of symptoms. Management of uncomplicated asymptomatic CTAD must be individualized considering patient comorbidities, and those patients unfit for open surgical repair may be candidates for emerging hybrid and endovascular therapies.
Depending on the extent of dissection, open repair may include simple tube graft replacement of the ascending aorta, aortic valve replacement when one or more leaflets is damaged, valve repair or resuspension when the valve is salvageable, and hemiarch or total arch replacement techniques. Perioperative mortality of ascending aorta or arch repairs ranges from 1–15% [8].
Endovascular Repair
Chronic lesions restricted to the ascending aorta that do not involve the arch, aortic valve or coronary arteries, have been successfully managed with endovascular stent grafts, as a variation on thoracic endovascular aortic repair (TEVAR). Experience is limited to cases performed in patients at prohibitive risk for open aortic repair and patients refusing surgery. Current challenges include the lack of endovascular delivery systems and stents designed for the ascending aorta [9] at most centers, though new devices have been developed and utilized in cases approved on compassionate grounds [10]. The curvature of the aorta also makes measurement of graft size difficult to estimate, which may be associated with early graft migration at or near the time of deployment [11]. In addition, lack of vascular suitability can preclude Type A TEVAR (aTEVAR); imaging studies estimate that a minority of patients undergoing open repair of Type A dissections meet criteria for endovascular repair of the ascending aorta [12, 13]. In this regard, suitability criteria have largely been extrapolated from success with Type B TEVAR. Proposed tenets of aTEVAR include 2 cm distance from sinotubular junction to the intimal tear, 0.5 cm from tear to brachiocephalic artery, absence of pericardial tamponade or severe aortic regurgitation, absence of ischemia of aortic branches, and no prior coronary revascularization from ascending aorta [13]. Patients with connective tissue diseases are not regularly considered for aTEVAR due to likelihood of requiring further surgery [11].
Long-term outcome data for aTEVAR are lacking due to small number of cases. Reported periprocedural complications with aTEVAR include endoleaks, stent buckling [14], stent migration [15], delivery device retention [9], and stroke. Further, the optimal degree of oversizing has not been delineated, although excess oversizing has been associated with aortic insufficiency. Broader experience and improvement of endovascular device design to conform to the ascending aortic environment will address many of these issues.
Conclusions
The small number of cases continues to limit our understanding of CTAD. Open surgical repair remains the first-line management when any complications or symptoms are present. The current body of evidence suggests most chronic Type A lesions should also be considered progressive, despite poor understanding of factors affecting prognosis. Endovascular repair of Type A dissections have met some success; and despite significant challenges, hold potential for improvement with further device innovations.
Conflict of Interest
The authors have no conflicts of interest relevant to this publication.
EDITOR'S QUESTIONS
-
What do you feel would be the outlook for your two chronic ascending aortic dissection patients without an operation? Why do you think so?
The lack of a strong body of evidence in the current literature defining the natural history of chronic Type A dissections creates uncertainty in predicting the outcomes of these patients. However, given that dissections of this type have been found to become rapidly progressive, in combination with onset of symptoms in these patients, we believe both cases were high risk for becoming rapidly fatal.
-
Is there any literature evidence that chronic ascending dissections rupture?
Chronic Type A dissections have been reported to quickly develop expansion of the false lumen, as well as be associated with progressive aortic dilatation. The relationship between chronic dissections and rupture has not been clearly established; however, the risk of rupture exists in cases of sudden progression or cases with extensive dilatation. Whether this risk is attenuated by chronic fibrosis surrounding the dissection is unknown.
-
Is not the key to development of chronic ascending dissections that early rupture has not occurred in these cases?
Correct. Unlike cases of rapidly fatal acute Type A dissections, chronic dissections have somehow been able to stabilize and are associated with a reactive fibrotic process at the site of intimal tear. This suggests therapy of these lesions could be aimed at supporting the stabilizing process rather than replacing the tissue. Cases of prohibitive operative risk give us a limited ability to evaluate this pathway.
-
Are you not concerned about the cardiac arrest at 2.5 years follow-up in patient # 2? Do you think this was aortic related? Valve related (anticoagluation held)? Coronary related? Pacemaker related? Is there any autopsy data or first hand hospital data?
Unfortunately, we do not have complete data surrounding this patient’s death, which did not occur at our institution. We are indeed suspicious that this mortality could have been related to the mechanical valve, coronary arteries or aortic repair. The 2.5-year survival is positive, given the initial presentation of symptomatic progression of Type A dissection; however, the cardiac arrest raises serious concerns.
References
- 1.Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr., et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. J Am Coll Cardiol. 2010;15:e27–129. DOI: 10.1016/j.jacc.2010.02.015 [DOI] [PubMed] [Google Scholar]
- 2.Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases. Eur Heart J. 2014;35:2873–2926. DOI: 10.1093/eurheartj/ehu281 [DOI] [PubMed] [Google Scholar]
- 3.Rylski B, Milewski RK, Bavaria JE, Branchetti E, Vallabhajosyula P, Szeto WY, et al. Outcomes of surgery for chronic type A aortic dissection. Ann Thorac Surg. 2015;99:88–94. DOI: 10.1016/j.athoracsur.2014.07.032 [DOI] [PubMed] [Google Scholar]
- 4.Pompilio G, Spirito R, Alamanni F, Agrifoglio M, Polvani G, Porqueddu M, et al. Determinants of early and late outcome after surgery for type A aortic dissection. World J Surg. 2001;25:1500–1506. DOI: 10.1007/s00268-001-0160-y [DOI] [PubMed] [Google Scholar]
- 5.Carnevale D, Lembo G, Frati G. Chronic type A aortic dissection: Could surgical intervention be guided by molecular markers? J Cell Mol Med. 2011;15:1615–1619. DOI: 10.1111/j.1582-4934.2011.01314.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eggebrecht H, Plicht B, Kahlert P, Erbel R. Intramural hematoma and penetrating ulcers: Indications to endovascular treatment. Eur J Endovasc Surg. 2009;38:659–665. DOI: 10.1016/j.ejvs.2009.09.001 [DOI] [PubMed] [Google Scholar]
- 7.Erbel R, Alfonso F, Boileau C, Dirsch O, Eber B, Haverich A, et al. Diagnosis and management of aortic dissection. Eur Heart J. 2001;22:1641–1681. DOI: 10.1053/euhj.2001.2782 [DOI] [PubMed] [Google Scholar]
- 8.Svensson LG, Adams DH, Bonow RO, Kouchoukos NT, Miller DC, O’Gara PT, et al. Aortic valve and ascending aorta guidelines for management and quality measures. Ann Thorac Surg. 2013;95:1491–1505. DOI: 10.1016/j.athoracsur.2012.12.027 [DOI] [PubMed] [Google Scholar]
- 9.Roselli EE, Idrees J, Greenberg RK, Johnston DR, Lytle BW. Endovascular stent grafting for ascending aorta repair in high-risk patients. J Thorac Cardiovasc Surg. 2015;149:144–154. DOI: 10.1016/j.jtcvs.2014.07.109 [DOI] [PubMed] [Google Scholar]
- 10.Metcalfe MJ, Karthikesalingam A, Black SA, Loftus IM, Morgan R, Thompson MM. The first endovascular repair of an acute type A dissection using an endograft designed for the ascending aorta. J Vasc Surg. 2012;55:220–222. DOI: 10.1016/j.jvs.2011.06.116 [DOI] [PubMed] [Google Scholar]
- 11.Kolvenbach RR, Karmeli R, Pinter LS, Zhu Y, Lin F, Wassilijew S, et al. Endovascular management of ascending aortic pathology. J Vasc Surg. 2011;53:1431–1438. DOI: 10.1016/j.jvs.2010.10.133 [DOI] [PubMed] [Google Scholar]
- 12.Nordon IM, Hinchliffe RJ, Morgan R, Loftus IM, Jahangiri M, Thompson MM. Progress in endovascular management of type A dissection. Eur J Vasc Endovasc Surg. 2012;44:406–410. DOI: 10.1016/j.ejvs.2012.07.018 [DOI] [PubMed] [Google Scholar]
- 13.Ronchey S, Serrao E, Alberti V, Fazzini S, Trimarchi S, Tolenaar JL, et al. Endovascular stenting of the ascending aorta for type A aortic dissections in patients at high risk for open surgery. Eur J Vasc Endovasc Surg. 2013;45:475–480. DOI: 10.1016/j.ejvs.2013.01.033 [DOI] [PubMed] [Google Scholar]
- 14.Brechtel K, Kalender G, Stock UA, Wildhirt SM. Hybrid debranching and TEVAR of the aortic arch off-pump, in re-do patients with complicated chronic type-A aortic dissections: A critical report. J Cardiothorac Surg. 2013;8:188 DOI: 10.1186/1749-8090-8-188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palma JH, Gaia DF, Guilhen JS, Buffolo E. Endovascular treatment of chronic type A dissection. Interact Cardiovasc Thorac Surg. 2008;7:164–166. DOI: 10.1510/icvts.2007.165027 [DOI] [PubMed] [Google Scholar]