Syncope is a common problem that many clinicians may encounter in various outpatient settings. Neurally mediated syncopal syndrome includes carotid sinus syndrome, situational syncope, and neurocardiogenic syncope (also known as vasovagal syncope), which is the most common cause of syncope in both children and adults, accounting for 50-66% of unexplained syncope.1,2 The distinction between neurocardiogenic syncope and other causes of fainting is essential, as the prognosis and treatment are different.
Sources and selection criteria
We selected articles from the PubMed database by using the search words “syncope” and “neurocardiogenic syncope.” Inclusion criteria were articles published in English, in peer reviewed journals, between 1980 and 2004. Exclusion criteria were articles not published in English, case reports, and articles not published in peer reviewed journals. We incorporated guidelines from the American College of Cardiology, European Society of Cardiology, and American Heart Association, along with a summary of clinical trials. We selected 31 references for this review.
Definition and incidence
Syncope is defined as a transient loss of consciousness, with loss of posture (that is, falling). Commonly described as “fainting,” “passing out,” or “blackout,” syncope accounts for 3% of visits to emergency departments and 6% of all admissions to hospital.1,3 It occurs relatively often in all age groups, ranging from 15% in children aged under 18 years to 23% in elderly patients aged over 70.4 The prevalence and incidence of syncope increase with advancing age,5 with a 30% recurrence rate.3
Neurocardiogenic syncope, with a mean prevalence of 22% in the general population,2 is defined as a syndrome in which “triggering of a neural reflex results in a usually self-limited episode of systemic hypotension characterized by both bradycardia (asystole or relative bradycardia) and peripheral vasodilation.”6
Causes of syncope
Syncope is a symptom, not a disease, and can be classified according to the underlying cause: neurological, metabolic, psychiatric, and cardiac7; cardiac syncope is the most common form. Cardiac syncope includes syncope due to mechanical or structural heart disease, cardiac arrhythmias, and neurocardiogenic syncope (box 1).7
Summary points
Syncope, commonly described as “fainting,” is a symptom, not a disease, and can be classified according to the cause, the most common of which is neurocardiogenic syncope
Neurocardiogenic syncope (also known as vasovagal syncope) is a benign condition characterised by a self limited episode of systemic hypotension
Stimulation of the cardiac C fibres results in vasodilation and increased vagal tone, with consequent reduction in cardiac filling and bradycardia, with ensuing syncope
Differential diagnoses include carotid sinus hypersensitivity (resulting from an extreme reflex response to carotid sinus stimulation) and orthostatic hypotension (failure of the autonomic reflex response)
The mainstay of management is education of the patient to avoid situations that predispose to syncope, with anxiety management, coping skills, and reassurance of the patient and others that this is a benign condition
Neurocardiogenic syncope is caused by an abnormal or exaggerated autonomic response to various stimuli, of which the most common are standing and emotion.8,9 The mechanism is poorly understood but involves reflex mediated changes in heart rate or vascular tone, caused by activation of cardiac C fibres.2
Pathophysiology of neurocardiogenic syncope
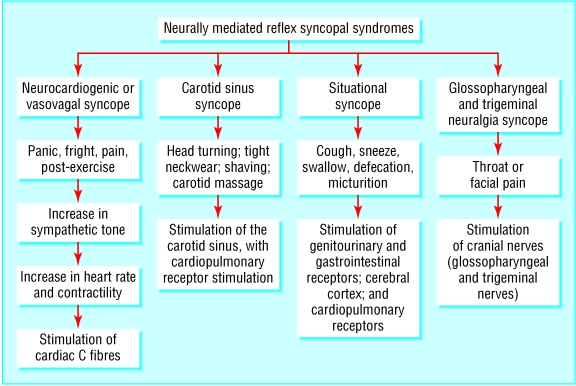
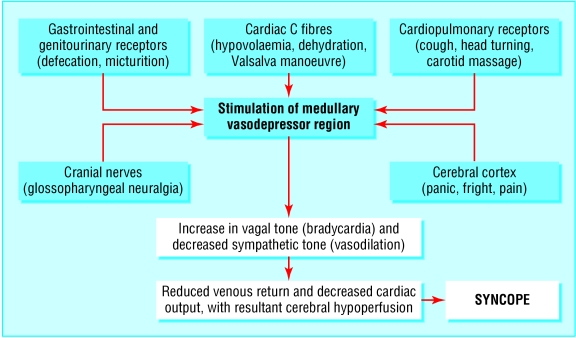
Stimulation of the cardiac C fibres is implicated in neurocardiogenic syncope.7 An abnormal autonomic response occurs, resulting in vasodilation and increased vagal tone, with subsequent reduction in cardiac filling and bradycardia, which ultimately leads to syncope (fig 1). Stimulation of the medullary vasodepressor region of the brain stem may occur owing to activation of various receptors, such as cardiac C fibres (mechanocardiac receptors), cardiopulmonary baroreceptors, cranial nerves, cerebral cortex, and gastrointestinal or genitourinary mechanoreceptors (fig 2).2,4,7
Fig 1.
Pathophysiology of neurally mediated reflex syncopal syndromes
Fig 2.
Activation of receptors in neurally mediated syncopal syndromes
In hypovolaemia and other conditions of reduced preload, sympathetic tone is increased, resulting in hypercontractility of the volume depleted ventricle (with increase in myocardial inotropy and chronotropy), with subsequent stimulation of the cardiac C fibres.3,7,10 This results in a combination of parasympathetic enhancement (bradycardia) and decreased sympathetic tone (hypotension), with ensuing syncope.3,10
Clinical signs and symptoms
Although presentation of neurocardiogenic syncope is similar to that of other types of syncope, loss of consciousness in patients with neurocardiogenic syncope may be preceded by prodromata such as nausea, diaphoresis, lightheadedness, blurred vision, headaches, palpitations, paraesthesia, and pallor,3,7,10,11 which usually occur in the upright position (with downward displacement of 300-800 ml of blood3) and resolve almost immediately when the patient assumes the supine position.7 In addition, after recovery, patients with neurocardiogenic syncope may complain of a “washed out” and tired feeling.4,7
Assessment of the symptoms and setting may yield clues as to the possible cause of the syncope. Syncope after cough, defecation, and micturition suggests situational syncope; syncope associated with throat or facial pain (glossopharyngeal or trigeminal neuralgia) is indicative of neurally mediated syncope with neuralgia; and syncope after pain, fear, or noxious stimuli suggests neurocardiogenic syncope.4 Carotid sinus syncope may occur with rotation or turning of the head or pressure on the carotid sinus (for example, carotid massage, shaving, tight collars or neckwear, or tumour compression).4
Cardiac causes
Structural cardiac or cardiopulmonary disease (aortic stenosis, mitral stenosis, pulmonary stenosis, left atrial myxoma, aortic dissection, acute myocardial infarction, cardiac tamponade, pulmonary embolism, obstructive cardiomyopathy)
Cardiac arrhythmias (tachyarrhythmias, bradyarrhythmias)
Neurally mediated syncopal syndrome (includes neurocardiogenic or vasovagal syncope, carotid sinus syncope, and situational syncope)
Orthostatic (or postural) hypotension
Metabolic causes
Hypoxia
Hypoglycaemia
Hyperventilation
Psychiatric causes
Somatisation disorders
Hysteria
Panic
Fright
Neurological causes
Seizure disorders
Transient ischaemic attacks
Subclavian steal syndrome
Normal pressure hydrocephalus
Diagnosis
A thorough assessment of associated symptoms, setting, drugs, and family history and a physical examination often provide important clues to the cause and help to guide baseline testing. However, the history and physical examination are non-diagnostic in more than 50% of patients with neurocardiogenic syncope.6 Structural cardiac disease and cardiac arrhythmias must be ruled out, especially in elderly people, who have a higher incidence of syncope. Differential diagnoses include carotid sinus hypersensitivity and orthostatic hypotension.
Neurocardiogenic syncope results from excessive autonomic reflex activity, which shows as abnormal vascular tone and heart rate. In contrast, orthostatic hypotension is a failure of the autonomic reflex response.12 Orthostatic hypotension affects 5% of the population and 7-17% of patients in acute care settings.13 It is more common in elderly people and is attributed to an age related decrease in physiological function (reduction in baroreceptor sensitivity) and polypharmacy (including various vasoactive drugs).13 Orthostatic hypotension is a drop in blood pressure on assuming an upright posture and is due to failure of the autonomic system to compensate for venous pooling in the lower extremities, which results in reduced venous return, decreased cardiac output, and cerebral hypoperfusion.13 Carotid sinus massage is done to rule out carotid sinus syndrome or hypersensitivity as the cause of syncope. This procedure should be avoided in patients with carotid bruits or a history of cerebrovascular events or transient ischaemic attacks, because of the risk of neurological complications.4 Carotid sinus hypersensitivity is defined as “syncope or presyncope resulting from an extreme reflex response to carotid sinus stimulation.”14 This reflex response has two components:
Box 2: Indications and contraindications for tilt table testing6
Indications
Recurrent syncope or single syncopal episode accompanied by physical injury or motor vehicle crash or occurring in a high risk setting (for example, pilot, surgeon, commercial vehicle driver) and no evidence of structural cardiovascular disease; or presence of structural cardiovascular disease but other causes of syncope ruled out by diagnostic testing
Syncope induced by or associated with exercise
Further evaluation of patients in whom an apparent specific cause of syncope has been established (for example, asystole, high atrioventricular block) but susceptibility to neurocardiogenic syncope may affect treatment plan
Contraindications
Syncope with severe left ventricular outflow obstruction (for example, aortic stenosis)
Syncope in presence of severe mitral stenosis
Syncope in setting of known critical proximal coronary artery disease
Syncope in setting of known critical cerebrovascular disease
A cardioinhibitory component, due to enhanced parasympathetic tone, manifested by slowing of the sinus rate or prolongation of the PR interval and advanced atrioventricular block, alone or in combination
A vasodepressor component, due to decreased sympathetic activity, resulting in loss of vascular tone and hypotension, independent of changes in heart rate.14
Carotid sinus hypersensitivity is diagnosed when a ≥ 50 mm Hg reduction in systolic blood pressure or a ventricular pause of ≥ 3 s occurs when a 5-10 s carotid sinus massage is done.4 Although the condition is rare before the age of 40, the prevalence increases with age and with comorbidities (cardiovascular, cerebrovascular, and neurodegenerative).4 The condition is recognised in up to 45% of elderly patients with syncope, falls, and dizziness.15
Tests
Once cardiac arrhythmias, structural heart disease, and non-cardiac causes of syncope have been ruled out, head up tilt testing is usually the first line of testing. Tilt testing is an orthostatic stress test, used when neurocardiogenic syncope is suspected. In people without neurocardiogenic syncope, tilting causes a reduction in venous return, with subsequent baroreceptor stimulation and increased α and β adrenergic tone, averting syncope. In patients with neurocardiogenic syncope, tilting causes decreased venous return, but sympathetic tone increases with stimulation of cardiac C fibres. This leads to stimulation of the medullary vasodepressor region of the brain stem, resulting in sudden reduction in sympathetic tone (vasodilation) and concomitant increase in vagal tone (bradycardia), with consequent syncope. Tilt testing is considered positive if the original symptoms are reproduced, along with an abrupt drop in blood pressure, heart rate, or both.4,10 Box 2 summarises indications and contraindications for tilt testing.6 See bmj.com for protocols for tilt testing, including pharmacological provocation.6
Box 3: Indications for permanent pacing in neurocardiogenic syncope and carotid sinus hypersensitivity14
Class I
• Recurrent syncope caused by carotid sinus stimulation; minimal carotid sinus pressure induces ventricular asystole of > 3 s duration in the absence of any drug that depresses the sinus node or atrioventricular conduction (Level of evidence C)
Class IIa
Recurrent syncope without clear, provocative events and with a hypersensitive cardioinhibitory response (Level of evidence C)
Syncope of unexplained origin when major abnormalities of sinus node function or atrioventricular conduction are discovered or provoked in electrophysiological studies (Level of evidence C)
Class IIb
• Neurally mediated syncope with significant bradycardia reproduced by a head up tilt with or without isoproterenol or other provocative manoeuvres (Level of evidence B)
Class III
A hyperactive cardioinhibitory response to carotid sinus stimulation in the absence of symptoms
A hyperactive cardioinhibitory response to carotid sinus stimulation in the presence of vague symptoms such as dizziness, lightheadedness, or both
Recurrent syncope, lightheadedness, or dizziness in the absence of a hyperactive cardioinhibitory response
Situational vasovagal syncope in which avoidance behaviour is effective
Strength of recommendation
Class I—Conditions for which evidence or general agreement exists that a given procedure or treatment is beneficial, useful, and effective
Class II—Conditions for which conflicting evidence or a divergence of opinion exists about the usefulness or efficacy of a procedure or treatment
Class IIa—Weight of evidence or opinion is in favour of usefulness or efficacy
Class IIb—Usefulness or efficacy is less well established by evidence or opinion
Class III—Conditions for which evidence or general agreement exists that a procedure or treatment is not useful or effective and in some cases may be harmful
Strength of evidence
Level A—Data from multiple randomised clinical trials or meta-analyses
Level B—Data from a single randomised trial or multiple non-randomised trials
Level C—Consensus opinion of experts
Box 4: Treatment protocol4
Education
Avoidance of triggering events
Recognition of presyncopal symptoms and subsequent use of self help manoeuvres to avert syncope
Class I recommendation; level of evidence C
Volume expanders
Increased intake of salt and fluids through salt tablets or “sports” beverages
Class II recommendation; level of evidence B
Moderate exercise training
• Class II recommendation; level of evidence B
Tilt training
Progressively prolonged periods of enforced upright posture
Class II recommendation; level of evidence B
Drug therapy
Overall class II-III recommendation; level of evidence A-B
β blockers (class III; level A)
Etilephrine (α1 agonist) (class III; level B)
Modification or discontinuation of hypotensive drugs for comorbidities (class I; level C)
Other agents—no recommendations due to lack of evidence of benefit of various drugs over placebo in several long term placebo-controlled, prospective trials
Pacemaker treatment
Overall class I-II recommendation; level of evidence B
Cardiac pacing in patients with cardioinhibitory or mixed carotid sinus syndrome (class I; level B)
-
Cardiac pacing in patients with cardioinhibitory vasovagal syncope with more than five episodes a year or severe physical injury and age > 40 years (class II; level B)
See box 3 for definition of strengths of recommendations and evidence
Other ways of evaluating syncope can be grouped into three main categories: electrocardiographic recordings (including event recorders); analysis of heart rate variability (to assess susceptibility to neurocardiogenic syncope); and other tests (including Valsalva manoeuvre) to assess the autonomic function. However, more research is needed to determine the diagnostic value of these methods.6
Treatment of neurocardiogenic syncope
Treatment consists of education, manoeuvres to avert syncope, drug treatment, and pacemakers. Education, the mainstay of treatment, includes avoidance of predisposing situations (for example, dehydration, stress, alcohol consumption, extremely warm environments, tight clothing),4,10 anxiety management and coping skills, and reassurance of the patient and others that this is a benign condition. Drug treatments include β blockers, α agonists, selective serotonin reuptake inhibitors, fludrocortisone, disopyramide, scopolamine, and anticholinergic agents.
Drug treatment
β blockers are preferred as initial treatment,10 as they are believed to reduce the degree of mechanoreceptor activation and block the effects of circulating catecholamines.4 However, randomised controlled trials fail to support the efficacy of these drugs, showing no difference from placebo.4,16,17 Furthermore, β blockers may worsen syncope through their negative chronotropic effects and atrioventricular node blocking effects.3
α agonists work by increasing peripheral vascular resistance and reducing vascular capacitance (to cause increased venous return).3,10 Midodrine, an α agonist, has been shown to be effective in several randomised controlled clinical trials.18-20
Selective serotonin reuptake inhibitors selectively block serotonin, which has been shown to induce vagally mediated bradycardia and blood pressure lowering.3,10 Selective serotonin reuptake inhibitors have been used to treat syncope, but their efficacy has been documented in only one randomised controlled trial of 68 patients to date.21 Side effects of these agents include nausea, insomnia, weight gain, and sexual dysfunction.3
Fludrocortisone, a mineralocorticoid that promotes renal reabsorption of sodium to cause increased blood volume,3,10 has been used in the treatment of vasodepressor syncope in both children and adults.22,23 Vascular volume and preload are maintained through the resultant sodium and water retention by fludrocortisone, thereby preventing activation of the cardiac mechanoreceptors.3 However, caution is needed in elderly patients because of the risk of hypertension, cardiac failure, and oedema.24
Disopyramide, a class Ia antiarrhythmic agent with anticholinergic and negative inotropic effects, is not considered first line treatment because of the risk of proarrhythmic and anticholinergic side effects (dry mouth, constipation, blurred vision, and urinary retention).3 Enhanced vagal activity in vasodepressor syncope is counteracted by using anticholinergic agents,10 which are useful when syncope is due solely to increased vagal tone and not to vasodilation.3 Scopolamine, an anticholinergic agent, has central nervous system depressant effects and has been used successfully in some patients with syncope.3
The table summarises clinical trials of various drugs. Most randomised, placebo-controlled clinical studies to date show no differences between the treatment and placebo groups. Other trials that have shown benefit from treatment were not randomised. Most clinical trials, whether randomised or not, had small sample sizes (ranging from 11 to 68 participants) and involved only short term treatment and follow up (most ranging from one week to six months).
Table 1.
Drug treatment in syncope: summary of clinical trials*
| Investigators | Drug | Study design | Sample | Results |
|---|---|---|---|---|
| Ventura et al (2002)w1 |
β blocker (metoprolol, propranolol, or no treatment) |
Prospective randomised controlled clinical trial |
n=56 (36 female, 20 male); mean (SD) age 44 (18) years |
β blocker group had fewer recurrent episodes of syncope v no treatment |
| Madrid et al (2002)16 |
β blocker (atenolol) |
Prospective randomised double blind placebo controlled clinical trial |
n=50 (26 on atenolol, 24 on placebo) |
Atenolol group had similar No of recurrent syncope episodes to placebo group, with no difference in time to first syncopal recurrence |
| Flevari et al (2002)17 |
β blocker (propranolol, nadolol, or placebo) |
Randomised crossover controlled clinical trial |
n=30 consecutive patients with vasovagal syncope and positive tilt test (all were serially and randomly assigned to propranolol, nadolol, or placebo for three months each, with crossover) |
After nine month follow up: no difference in recurrence of syncope or presyncope among the three groups; all three treatments were equally effective in treating vasovagal syncope |
| Mahanonda et al (1995)w2 |
β blocker (oral atenolol) v placebo for one month |
Randomised controlled clinical trial |
n=42 (21 on atenolol, 21 on placebo); all had at least one syncopal episode or two presyncopal episodes occurring one month before presentation and had positive isoproterenol tilt test |
After one month: 62% of atenolol group v 5% of placebo group had negative tilt test (P=0.0004), and 71% of atenolol group v 29% of placebo group reported symptomatic improvement (P=0.02) |
| Takata et al (2002)w2 |
Selective serotonin reuptake inhibitors (paroxetine/paxil) 20 mg/day v placebo for six weeks |
Randomised double blind controlled trial |
n=25 (19 completed the study: 9 on paroxetine, 10 on placebo) |
Paroxetine did not attenuate sympathoinhibition or vagotonia (did not prevent syncope) |
| DiGirolamo et al (1999)21 |
Selective serotonin reuptake inhibitors (paroxetine/paxil) 20 mg/day v placebo for one month |
Randomised controlled clinical trial |
n=68 (42 female, 26 male); mean (SD) age 44.7 (16.5) years |
61.8% of paroxetine group v 38.2% of placebo group had negative tilt test; 17.6% of paroxetine group v 52.9% of placebo group had spontaneous syncope (P<0.0001); paroxetine improved symptoms of vasovagal syncope |
| Kaufmann et al (2002)18 |
Selective α1 adrenergic agonist (midodrine) v placebo |
Randomised double blind crossover placebo controlled trial |
n=12 (with recurrent neurally mediated syncope) |
Midodrine significantly improved orthostatic tolerance during tilt test in patients with neurally mediated syncope (P<0.02) |
| Perez-Lugones et al (2001)19 |
Selective α1 adrenergic agonist (midodrine) v fluid and salt tablets for six months |
Prospective randomised controlled trial |
n=61 (31 on midodrine, 30 on fluid and salt tablet) |
81% of midodine v 13% of fluid and salt tablet group remained asymptomatic (P<0.001); midodrine was beneficial in treating neurally mediated syncope |
| Ward et al (1998)20 |
Selective α1 adrenergic agonist (midodrine) v placebo for one month |
Randomised double blind placebo controlled trial |
n=16 (11 female, 5 male); mean (SD) age 56 (18) years |
Midodrine group had more symptom-free days and fewer positive tilt tests v placebo group; midodrine reduced symptom frequency and symptoms during tilt test |
| Mitro et al (1999)w4 |
Selective α1 adrenergic agonist (midodrine) |
Prospective non-randomised clinical trial |
n=41 (23 female, 18 male); mean age 34 years; with recurrent syncope and positive tilt test |
95% had no inducible presyncope or syncope during repeat tilt test; the effective dose was 2.5 mg po bid in 25 patients, and 5 mg po bid in 16 patients; on mean (SD) follow up of 19 (9) months, 97% with negative repeat tilt test remained free of syncope recurrence |
| Yu and Sung (1997)w5 |
Anticholinergic (propantheline bromide), mean (SD) 64.3 (21) mg/day for seven days |
Prospective non-randomised clinical trial |
n=16 (5 female, 11 male); mean (SD) age 48.8 (15.1) years |
81% of patients had no inducible presyncope or syncope on repeat tilt test; on mean (SD) follow up of 15.2 (7.4) months in 12 patients, 33% had clinical recurrence of symptoms |
| Da Costa et al (1993)22 | Salt retaining mineralocorticoid (fludrocortisone) for two weeks | Prospective non-randomised clinical trial | n=11; mean (SD) age 83 (5) years; all patients had daily dizziness and had vasodepressor carotid sinus syndrome | Fludrocortisone effectively reduced vaspdepressor response and relieved symptoms of vasodepressor carotid sinus syndrome |
As noted in text, most randomised placebo controlled clinical studies to date show no differences between treatment and placebo groups. Other trials that have shown benefit from treatment were not randomised. Most clinical trials, whether randomised or not, consisted of small sample sizes (ranging from 11 to 68 participants) and involved only short term treatment and follow up (most ranged from one week to six months).
Pacemaker treatment
In most people with neurocardiogenic syncope, a fall in blood pressure precedes bradycardia, so pacing may be ineffective in most patients. However, dual chamber pacing may be effective in reducing symptoms if there is a large cardioinhibitory component.14,25 The cardioinhibitory component results from enhanced parasympathetic tone, manifested by slowing of the sinus rate or prolongation of the PR interval and advanced atrioventricular block, either alone or in combination.14 Box 3 lists indications for permanent pacemaker treatment.6 Box 4 outlines a treatment protocol, along with strength of supporting evidence and strength of recommendation.4
Conclusion
Syncope is associated with considerable morbidity (including injury due to falls or motor vehicle crashes) and poses a potential danger if episodes occur during critical activity (such as participation in sport, driving, operating heavy or critical machinery). Suspension of driving and piloting privileges after syncopal episodes varies according to different state and country laws. The mortality due to syncope varies according to the cause: cardiac causes (arrhythmias or cardiovascular disease) have a 20-30% mortality compared with 5-10% mortality for non-cardiac causes.3 Although frequent or recurrent episodes can negatively affect quality of life and employability, neurocardiogenic syncope is generally considered a benign condition as episodes are self limiting. Understanding of the pathophysiology of neurocardiogenic syncope is necessary to guide appropriate management. Finally, more randomised controlled clinical trials are needed to assess the efficacy of the various treatment strategies used.
Additional educational resources
Resources for healthcare professionals
Heart Rhythm Society (www.hrspatients.org/patients/signs_symptoms/fainting/non-cardiovascular_syncope.asp)—describes neurocardiogenic syncope and its causes, diagnosis, and treatment
Brignole M, Alboni P, Benditt D, Bergfeldt L, Blanc JJ, Bloch Thomsen PE, et al for the European Society of Cardiology. Guidelines on management (diagnosis and treatment) of syncope. Eur Heart J 2001;22: 1256-306
Brignole M, Alboni P, Benditt D, Bergfeldt L, Blanc JJ, Bloch Thomsen PE, et al. Task force on syncope, European Society of Cardiology: part 1—the initial evaluation of patients with syncope. Europace 2001;3: 253-6011678381
Brignole M, Alboni P, Benditt D, Bergfeldt L, Blanc JJ, Bloch Thomsen PE, et al. Task force on syncope, European Society of Cardiology: part 2—diagnostic tests and treatment: summary of recommendations. Europace 2001;3: 261-811678382
Kapoor WN. Syncope. N Engl J Med 2000;343: 1856-6211117979
Benditt DG, Ferguson DW, Grubb BP, Kapoor WN, Kugler J, Lerman BB, et al. Tilt table testing for assessing syncope. J Am Coll Cardiol 1996;28: 263-75
Four key ongoing research studies
Relationship of autonomic function to hypnotic susceptibility—a study to investigate the relation between susceptibility to hypnosis and regulation of the autonomic nervous system
Propranolol for syncope with sympathoadrenal imbalance—evaluating treatment with oral propranolol for a particular form of neurocardiogenic syncope characterised by a neuroendocrine pattern called sympathoadrenal imbalance
Clinical laboratory evaluation of chronic orthostatic intolerance—to identify and characterise distinct types of chronic orthostatic intolerance
Randomized study of midodrine, an adrenergic agonist, in patients with neurally mediated syncope—to determine the efficacy of midodrine, a selective α1 adrenergic agonist, in preventing neurally mediated syncope (For more detailed information, visit www.clinicaltrials.gov and enter “syncope” as search term)
Supplementary Material
 Additional references and protocols for tilt testing are on bmj.com
Additional references and protocols for tilt testing are on bmj.com
Contributors: CC-S had the idea for the article. Both CC-S and TMS did the literature search, contributed to the design of the review, and wrote the paper. CC-S is the guarantor.
Funding: None.
Competing interests: None declared.
References
- 1.American Heart Association. Syncope. www.americanheart.org/presenter.jhtml?identifier=4749 (accessed 30 Jan 2004).
- 2.Kapoor WN. Syncope. N Engl J Med 2000;343: 1856-62. [DOI] [PubMed] [Google Scholar]
- 3.White CM, Tsikouris JP. A review of pathophysiology and therapy of patients with vasovagal syncope. Pharmacotherapy 2000;20: 158-65. [DOI] [PubMed] [Google Scholar]
- 4.Brignole M, Alboni P, Benditt D, Bergfeldt L, Blanc JJ, Bloch Thomsen PE, et al for the Task Force on Syncope, European Society of Cardiology. Guidelines on management (diagnosis and treatment) of syncope. Eur Heart J 2001;22: 1256-306. [DOI] [PubMed] [Google Scholar]
- 5.Kenny RA. Neurally mediated syncope. Clin Geriatr Med 2002;18: 191-210. [DOI] [PubMed] [Google Scholar]
- 6.Benditt DG, Ferguson DW, Grubb BP, Kapoor WN, Kugler J, Lerman BB, et al. ACC expert consensus document: tilt table testing for assessing syncope. J Am Coll Cardiol 1996;28: 263-75. [DOI] [PubMed] [Google Scholar]
- 7.Fogoros RN. Practical cardiac diagnosis: electrophysiologic testing. 3 rd ed. Malden, MA: Blackwell Publishing, 1999.
- 8.Krediet CT, van Dijk N, Linzer M, van Lieshout JJ, Wieling W. Management of vasovagal syncope: controlling or aborting faints by leg crossing and muscle tensing. Circulation 2002;106: 1684-9. [DOI] [PubMed] [Google Scholar]
- 9.Lu CC, Diedrich A, Tung CS, Paranjape SY, Harris PA, Byrne DW, et al. Water ingestion as prophylaxis against syncope. Circulation 2003;108: 2660-5. [DOI] [PubMed] [Google Scholar]
- 10.Zaqqa M, Massumi A. Neurally mediated syncope. Tex Heart Institute J 2000;27: 268-72. [PMC free article] [PubMed] [Google Scholar]
- 11.Nair N, Padder FA, Kantharia BK. Pathophysiology and management of neurocardiogenic syncope. Am J Managed Care 2003;9: 327-34. [PubMed] [Google Scholar]
- 12.Sutton R, Petersen ME. The clinical spectrum of neurocardiogenic syncope. J Cardiovasc Electrophysiol 1995;6: 569-76. [DOI] [PubMed] [Google Scholar]
- 13.Frishman WH, Azer V, Sica D. Drug treatment of orthostatic hypotension and vasovagal syncope. Heart Dis 2003;5: 49-64. [DOI] [PubMed] [Google Scholar]
- 14.Gregoratos G, Cheitlin M, Conill A, Epstein AE, Fellows C, Ferguson TB Jr, et al. ACC/AHA guidelines for implantation of cardiac pacemakers and antiarrhythmia devices: executive summary—a report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee on pacemaker implantation). Circulation 1998;97: 1325-35. [DOI] [PubMed] [Google Scholar]
- 15.O'Mahony D. Pathophysiology of carotid sinus hypersensitivity in elderly patients. Lancet 1995;346: 950-2. [DOI] [PubMed] [Google Scholar]
- 16.Madrid AH, Ortega J, Rebollo JG, Manzano JG, Segovia JG, Sanchez A, et al. Lack of efficacy of atenolol for the prevention of neurally mediated syncope in a highly symptomatic population: a prospective, double-blind, randomized and placebo-controlled study. J Am Coll Cardiol 2001;37: 544-9. [DOI] [PubMed] [Google Scholar]
- 17.Flevari P, Livanis EG, Theodorakis GN, Zarvalis E, Mesiskli T, Kremastinos DT. Vasovagal syncope: a prospective, randomized, crossover evaluation of the effect of propranolol, nadolol and placebo on syncope recurrence and patients' well-being. J Am Coll Cardiol 2002;40: 499-504. [DOI] [PubMed] [Google Scholar]
- 18.Kaufmann H, Saadia D, Voustianiouk A. Midodrine in neurally mediated syncope: a double-blind, randomized, crossover study. Ann Neurol 2002;52: 342-5. [DOI] [PubMed] [Google Scholar]
- 19.Perez-Lugones A, Schweikert R, Parra S, Sra J, Akhtar M, Jaeger F, et al. Usefulness of midodrine in patients with severely symptomatic neurocardiogenic syncope: a randomized control study. J Cardiovasc Electrophysiol 2001;12: 935-8. [DOI] [PubMed] [Google Scholar]
- 20.Ward CR, Gray JC, Gilroy JJ, Kenny RA. Midodrine: a role in the management of neurocardiogenic syncope. Heart 1998;79: 45-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DiGirolamo E, Di Iorio C, Sabatini P, Leonzio L, Barbone C, Barsotti A. Effects of paroxetine hydrochloride, a selective serotonin reuptake inhibitor, on refractory vasovagal syncope: a randomized, double-blind, placebo-controlled study. J Am Coll Cardiol 1999;33: 1227-30. [DOI] [PubMed] [Google Scholar]
- 22.Da Costa D, McIntosh S, Kenny RA. Benefits of fludrocortisone in the treatment of symptomatic vasodepressor carotid sinus syndrome. Br Heart J 1993;69: 308-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scott WA, Pongiglione G, Bromberg BI, Schaffer MS, Deal BJ, Fish FA, et al. Randomized comparison of atenolol and fludrocortisone acetate in the treatment of pediatric neurally mediated syncope. Am J Cardiol 1995;76: 400-2. [DOI] [PubMed] [Google Scholar]
- 24.Hussain RM, McIntosh SJ, Lawson J, Kenny RA. Fludrocortisone in the treatment of hypotensive disorders in the elderly. Heart 1996;76: 507-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Connolly SJ, Sheldon R, Roberts RS, Gent M. The North American vasovagal pacemaker study (VPS): a randomized trial of permanent cardiac pacing for the prevention of vasovagal syncope. J Am Coll Cardiol 1999;33: 16-20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.