Summary
Understanding the cost of burn treatment is very important for patients, their families, governmental authorities and insurance companies. It alleviates patient and familial stress, provides a framework for better use of resources, and facilitates better performance between burn centers. Hospital burn costs can provide a basis for authorities to budget for acute burn treatment, for further management of chronic complications, and for planning prevention and public educational programs in Iran. To identify costs we used data from our burn registry program. Over the two-year assessment period, we treated roughly 28,700 burn patients, 1,721 of whom were admitted, with a mortality rate of 5.9%. The male to female ratio was 1.7:1 (63% male; 37% female). Flame burns were most frequent (49.8%) followed by scalds (35.7%). Mean hospital stay was 14.41 days (range 0-64 days). Mean TBSA was 17.39%. Skin grafts were carried out in 65.4% of the patients, with a mean of 5.2 surgeries per patient. The total cost of all patient admissions over the two years was US$ 4,835,000. The maximum treatment cost for one patient was US$ 91,000. The mean cost per patient was US$ 2,810 (29,500,000 Rials). The mean cost for each percent of burn was US$ 162. The mean cost for a one-day stay in hospital was US$ 195. The mean cost of each operation was US$ 540. Patients who contracted infections endured longer hospital stays, meaning increased costs of US$ 195 per day. With comparable outcome and results, the cost of burn treatment in Iran is cheaper than in the US and Europe
Keywords: burns, registry, financial burden, economic, hospital costs
Abstract
Connaître le coût du traitement d’un brûlé est très important pour les patients, leur famille, les autorités gouvernementales et les compagnies d’assurance. Ces informations peuvent rassurer les familles, donner des bases pour adapter les subsides gouvernementaux (pour la prise en charge initiale et celle des séquelles) et promouvoir une meilleure utilisation des ressources dans les services concernés. Afin de modéliser le coût de la prise en charge d’un patient brûlé, nous avons examiné les données de notre service. Au cours de deux ans d’évaluation, nous avons traité environ 28 700 patients brûlés, parmi lesquels 1 721 ont été hospitalisés, avec une mortalité de 5.9%. Le rapport hommes-femmes était de 1,7:1 (63% d’hommes; 37% de femmes). Le coût total global était 4 835 000$ (maximum pour un patient 91.000$), soit un coût moyen de 2 810$ (29,5 millions de rials). Le coût moyen par « pour cent brûlé » était de 162$, de 195$ par journée d’hospitalisation et de 540$ par intervention chirurgicale, ce qui se révèle inférieur aux coûts observés aux États-Unis et en Europe
Introduction
Burns are one of the most common forms of injury in our country. In a list of the greatest causes of burden from disease or injury, burns rank seventh place.1 We have more than 100,000 burn cases across the country and about 8,000-9,000 patients are admitted annually. Our center is the largest burn hospital in Iran and acts as the main referral center for the entire country. We have about 900 admissions each year. Since 2009, we have established a burn registry program for collating data on all burn patients within Iran.2
The present study focuses on the economic and financial burden of burns. About 1% of the population suffers burn injuries each year,3 with burn victims making up roughly 1-1.5% of all emergency department patients.4 Approximately 1% of all hospital admissions are due to burn injury.5 These would induce a heavy financial burden on any medical system around the world, let alone our country. 3 Eighty-five percent of burns occur in low and middle income countries but still the reports about the cost of burn treatment in these countries are rare.6 It is important for the patients, their families, the government, society, and the insurance companies to be aware of the costs of burn treatment. Burn care in specialized burn units requires trained doctors and staff, specialist equipment, facilities, special tissue banks and specific dressings, and is thus very expensive.6
In 2010, Patil stated that the mean daily intensive care unit cost of burn patients is similar to regular ICU care cost.7 However, a 2013 report suggests that the cost of treating burns in an intensive care unit is about US$ 6,000 (4,600 Euros) for every percent of burn.9 Others have found the cost of burn treatment to be much higher, since burn severity and institutional care differences can significantly vary the cost of treatment, as seems to be the issue in our country.9,16 Burn care in Iran is not as expensive as in other countries but nonetheless proves to be a high financial burden for patients, their families and the wider society. The huge incidence of burns in the developing world has been shown before. Likewise, there is a high incidence in our country.
In this report we comprehensively calculate almost all the direct costs of managing in-hospital acute burns. We also compare the results of treatment with other reports. In this way, burn costs are compared according to the results of treatment. Whereas other reports did not calculate the mean cost per operation for burn patients, this aspect will be covered in our study. This report can provide a baseline against which future improvements in burn care can be measured. The governmental and burn hospital authorities can have a better estimation of the direct costs of a burn center and the total budget that may be required for the whole country to cover the annual costs of treating burn patients.
Material & methods
Over the two-year study period, we treated 28,700 burn patients, 1,721 of whom required hospital admission. All patients admitted with acute burns in the study period were included in this investigation. We prospectively reviewed the epidemiological data and outcome of our patients in this period with a follow-up period of 3 +/- 0.5 years. We used a specifically designed questionnaire to gather all patient demographic factors. These factors included: age, sex, inhalation injury, the length of time from injury to care, accompanying traumas, previous medical history and illnesses, place of burn, anatomic distribution of burn, seasonal variation, total surface area of burns, cause of burn (including explosions and ignition of clothing), mode of extinguishing the fire, extent of 3rd and 4th degree burns, marital status, insurance coverage, level of education, type of transportation to hospital, mode of burn (intentional or accidental), previous clinical condition, any treatment for burn at home (pre-hospital treatment), medical staff pre-hospital care, ICU admission and mortality, length of hospital stay, mode of therapy and operative intervention, infection, SIRS, sepsis, multiple organ failure, culture of burn wounds, antibiotics used, result of treatment, lab tests, number of blood transfusions, mortality rate and cause of death, total expenditure during the study period, total TBSA involvement for all patients, total length of stay of all patients, mean % TBSA burns, mean cost of treatment per patient, maximum treatment cost, minimum treatment cost, mean length of hospitalization, average cost of treatment per patient per day, and the average cost of treatment per patient per TBSA%.
Inhalation injury was defined on the basis of exposure to smoke, burn in a closed space, presence of carbonaceous putum, signs of airway obstruction, deterioration of Po2 in serial arterial blood gas tests and/or positive findings in bronchoscopy. Sepsis was defined as systemic inflammation response to infection and positive blood culture. Wound cultures with more than 100,000 bacteria in each gram of tissue were considered positive. SIRS was defined as body temperature >38 or <36oC, heart rate >90/minute, respiratory rate >20/minute and white blood cell count >12,000 or <4,000.
We kept financial files on the patients to calculate the cost of burn care, including the cost of all medications and medical consumables, dressing material, hospital fees, investigations, lab tests, OT costs, blood products, dietary costs, hospital administrative costs and so on, as well as the type of insurance and whether or not they were insured. (For reference, blood donation and transfusion is completely free of charge in our country.)
The government and ministry of health fund the costs of establishing the hospital, the equipment, salaries of doctors, residents, nurses and staff, and therefore these were not included in the calculation of patient charges. Afterward, staff salaries were calculated, and then the total cost of treatment with salaries was calculated. The maintenance and utility costs of electricity, water, piped propane gas, sewerage, air conditioning, laundry, etc. were included in the hospital fees and were not calculated separately again
Burn unit details and treatment policies
During the study period, our burn hospital staff consisted of four plastic surgery consultants, five general surgeons, two internal medicine specialists, two infectious disease specialists, one pediatrician, one orthopedic surgeon, eleven residents, six physiotherapists (with some students), 18 medical students, 75 nurses, 17 operating theatre staff, four anaesthesiologists and more than 80 service staff. After admission, all patients were given intravenous fluid resuscitation, topical antibiotic therapy (Nitrofurazone ointment, mupirocin ointment, silver sulfadiazine and mafenid cream) with daily dressing changes, and occasional dressing with Amnion, Acticoat, Ag+, ADM, Alloderm and Xenoderm when indicated, routine blood investigations, bacteriological monitoring, intensive care when needed, burn wound excision and skin grafting, good nutrition, intensive physiotherapy and rehabilitation. Number of surgeries was gathered from the files. When indicated, early excision and grafting were also carried out. All information and data were collected via a questionnaire. Data and statistical analysis were performed with SPSS 16 software. P values less than 0.05% were considered significant.
Results
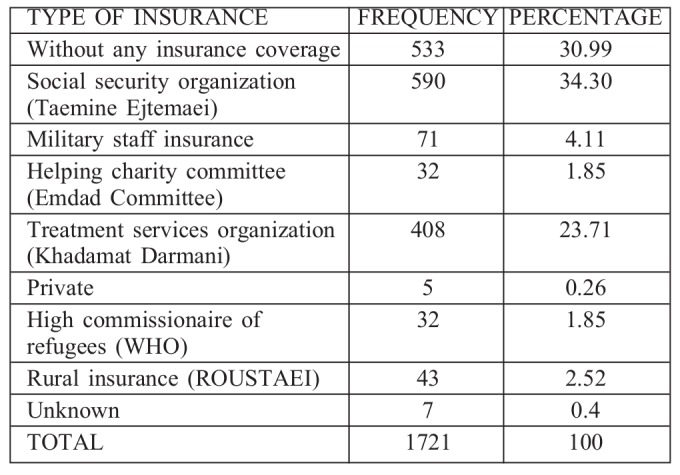
During the two years from March 2009 to March 2011, we treated a total of 28,700 cases, including 1,721 burn patients admitted for hospital stay. Sixty-three percent of our patients were male and 37% female. The male to female ratio was 1.7:1. Burns caused by open flame were the most frequent (49.8%) followed by scalds (35.7%), electrical burns (10.3%) and chemical burns (3.2%). Table I shows the cause of burns and Table II shows the age distribution of the patients. Table III shows the insurance coverage of the patients. Close to 31% of patients did not have any insurance cover.
Tableau I. Cause of burns.
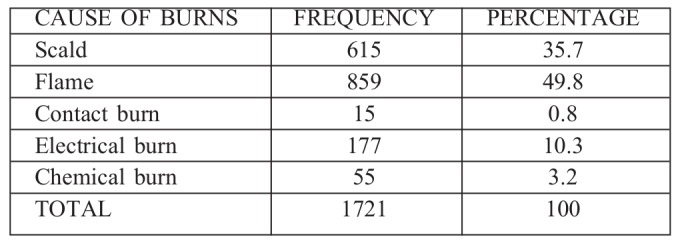
Tableau II. Age distribution of burn patients.
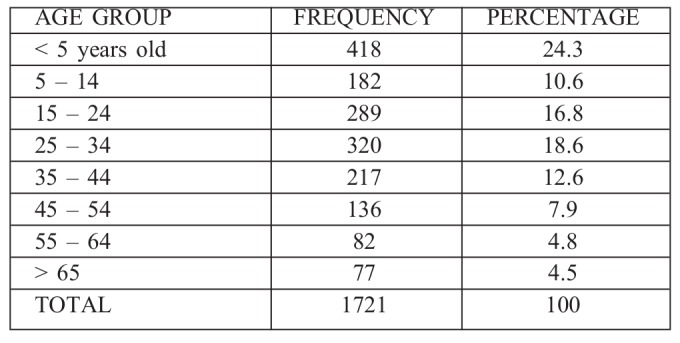
Tableau III. Insurance coverage of burn patients.
Mean hospital stay was 14.41 +/- 10.91 days (range 0-64 days). Complications requiring ICU admission were encountered in 9.6% of the patients. The mean +/- SD of ICU stay was 6.07+/- 3.58 days. The length of hospital stay was shown to increase in line with the increased size of the burn area (p<0.02). The mean TBSA of our patients was 17.39%. Skin graft surgery was carried out in 65.4% of the patients. The mean number of operations was 5.2 surgeries for each patient.
A total of 47.7% of our patients developed signs of burn wound infection and received burn wound biopsy and tissue culture. Of these patients, 58.6% had positive culture results. The most common bacteria found in burn wound cultures were: Coagulase-negative Staph. (66.8%), Pseudomonas aeroginosa (44.1%) and Coagulase-positive Staph. (33.6%). The most frequently prescribed antibiotics according to sensitivity tests were: Amikacin (91.9%), Ceftazidim (60.5%) and Meropenem (37.7%).
A patient mortality rate of 5.9% was identified, while 3.9% of patients were discharged at their own request (against the physician’s advice), 82.5% were discharged with partial recovery and 7.4% with complete recovery. During follow-up, we had only two mortalities, which were unrelated to the burn injury.
We examined the financial files of the patients. Total costs for the admission of our patients during the two-year period were US$ 4,835,000 (50,769,500,000 Rials). The mean total cost for one year was US$ 2,417,595 (25,384,750,000 Rials). The maximum treatment cost was US$ 91,000 (955,508,396 Rials). The minimum cost of treatment was US$ 46 (478,780 Rials). The total number of our patients was 1,721, giving a mean cost of burn treatment for every patient of US$ 2810 (29,500,000 Rials). The mean cost for every percent of TBSA was US$ 162 (1,696,377 Rials). The mean cost for a one-day stay in hospital was US$ 195 (2,047,190 Rials), while the mean cost for every operation was US$ 540. Those with infections had a longer stay in hospital and therefore their additional costs are expressed as more days in hospital, namely an extra US$ 195 per day. The total cost with salaries included was about US$ 6,435,000. Thus the mean cost of treatment for one patient was US$ 3,740, the mean for every TBSA percent was US$ 215, the mean per day was US$ 259 and the mean for each operation was US$ 719.
Patient marital status was not shown to have any effect on their outcome or hospital costs. The level of education of patients was considered as a possible indication of their socioeconomic status, but neither of these factors was found to have a major effect on the burn cost.
Discussion
Burn injury is one of the most devastating and disabling traumas for a human being. Burns are still very frequent in our country and result in a high mortality and morbidity rate. Usually, burns occur in low socioeconomic populations, meaning that the cost of burn treatment is very important for patients, their families, the government and insurance companies. Hospital charges and costs associated with further treatment post-discharge have a great impact on the psychosocial situation of the patients.9 Park, in 2008, reported that lack of family support and the economic burden of life expenses after a burn injury were the two most significant risk factors for psychosocial problems, especially among chronic burn patients.15
In another report from 2008, Sanchez stated that mean burn care costs were US$ 99,773 every year, which was only 19.6% of the total cost of further treatment.16 In 2009, Kai-Yang et al. reported that half of LOS and hospitalization costs were for young children under 3 years old, nearly 70% of the LOS and more than half of the hospitalization costs were for patients with less than 10% TBSA, and second-degree burns were responsible for more than 78% of hospitalization costs.17
In 1998, Evasovich reported that the average cost per day of treating burn-related child abuse was about US$ 1,200,18 whereas in our study the average cost per day for all burn types was less – about US$ 195. Allorto, in 2011, stated that the average cost of patient treatment for each percent of TBSA in South Africa was about US$ 703.19 Ours was US$ 162. In 2013, Mirastschijski reported a cost of US$ 6000 (4,600 Euros) for every percent of burn treated in intensive care units, and US$ 351,000 (270,000 Euros) per patient per annum for treatment of burns-related complications.8 Ahuja, also in 2013, reported the cost of providing inpatient burn care in a tertiary teaching hospital to be about US$ 1,060 for every patient in India, about one third of the cost in our center but with higher mortality.6
It thus appears that the costs of treating burns in Europe and South Africa are higher than in Iran, whereas they are lower in India. Comparisons of the mortality rates of the burn centers in these countries with our own treatment outcomes can tell us about the efficacy and quality of their procedures. It is reported that early excision and skin grafting reduces the length of hospital stay and burn costs of severe burn patients.3,19-23 Therefore the cost of early excision can be calculated by reduction in days of stay in hospital; the less LOS, the less burn cost, which sometimes can be onethird or one-fourth of the total cost. 5,17
Burn injuries usually occur among low and medium socio-economic populations. The average wage for basic workers in our country for the period under assessment was roughly US$ 200-600 per year. It is obvious, therefore, that the cost of burn treatment for even a single patient (mean = US$ 2810) is a huge financial burden on the family. Given this, if more than one member of the family is burned, the problem would be catastrophic.
Data from our burn registry program can help health authorities to develop measures to decrease the incidence and hospitalization costs of burn patients. Burn injuries are preventable, provided a community-specific prevention program is implemented with a strong educational component.
During this study we examined data on marital status because single or divorced patients may be more likely to suffer from loneliness or depression. Such patients may also be more likely to experience financial problems. However, this variable was not shown to have any effect on the outcome or hospital costs of the patients.
The patients’ level of education was also reviewed as a possible indication of their socioeconomic status. Again, this information was not found to have any significant effect on the costs associated with the burn injury. Therefore, socioeconomic status has no major bearing on the outcome of burn treatment, whereas the burns themselves have a great impact on the socioeconomic status of the patients and their families. It is worth noting here that, as blood donations and transfusions are free in Iran, these incur no charges for patients and thus do not add to the financial burden of burn patients.
Our review of the data on insurance coverage showed that roughly one third of the patients were unemployed and thus may have had financial problems. More than 31% of the patients had no coverage. This category of patients requires help from government or charity organizations. The financial burden of their treatment therefore has a great impact on the burn hospital’s budget. The cost of acute treatment is only about 20% of the total costs,16 meaning that health authorities should have a sophisticated program to help them, and should have strong financial support to treat their chronic complications as well.
In our country, insurance companies would cover 90-100% of the hospital costs, with patients only needing to pay 0-10% (depending on the type of insurance). Therefore treatment of acute burns does not have a big impact on patient finances, provided they are insured. However, it was shown that only just over 64% of our patients had governmental insurance coverage. For this reason, health authorities have to try to reduce the burn cost figures and cover the costs of any unemployed patients. Prevention programs and educational multimedia may also help to reduce the number of burn patients.
The data from our registry can help health authorities to forecast the economic costs of burns and budget accordingly. The information can also assist with the promotion of measures to reduce the cost of treatment through enabling cost comparisons over several years, and across various burn centers in Iran. This could lead to the spread of newer and better treatments that are cost-effective for burn patients.
Conclusions
The cost of burn treatment in Iran is lower than in the USA and Europe (developed world), with acceptable and comparable mortality rates. The mean burn cost per patient in our country is US$ 2,810. Insurance companies generally cover 90-100% of the costs and therefore play a significant role in decreasing the financial burden of burns (and thus some of the associated psychological problems) for the patients
Acknowledgments
Funding. This study was conducted with a grant from Iran University of Medical Sciences – Research, Vice President’s office.
Acknowledgements.The authors wish to thank Mrs. R. Amiri, Mrs. A. Kermanshahi and Mrs. Z. Karami for their support and cooperation during this study.
References
- 1.WHO Library Cataloguing-in-Publication Data, The Global Burden of Disease. ISBN 978 92 4 156371 0 (NLM classification: W 74); 2004. 1.Cost of illness. 2.World Health - statistics. 3.Mortality - trends. World Health Organization. [Google Scholar]
- 2.Karimi H, Momeni M, Motevalian A, Bahar MA et al. The burn registry program in Iran - first report. Ann Burns Fire Disasters. 2014;27:154–159. [PMC free article] [PubMed] [Google Scholar]
- 3.Perry ZH, Palivatkel M, Yanculewitch N, Koren L, Rosenberg N. Burns - risk factors and treatment. Harefuah. 2009;148:375–380. [PubMed] [Google Scholar]
- 4.Vercruysse GA, Ingram WL, Feliciano DV. The demographics of modern burn care: Should most burns be cared for by non-burn surgeons? Am J Surg. 2011;201:91–96. doi: 10.1016/j.amjsurg.2009.12.023. [DOI] [PubMed] [Google Scholar]
- 5.Mashreky SR, Rahman A, Chowdhury SM, Giashuddin S et al. Burn injury: Economic and social impact on a family. Public Health. 2008;122:1418–1424. doi: 10.1016/j.puhe.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 6.Ahuja RB, Goswami P. Cost of providing inpatient burn care in a tertiary teaching hospital of North India. Burns. 2013;39:558–564. doi: 10.1016/j.burns.2013.01.013. [DOI] [PubMed] [Google Scholar]
- 7.Patil V, Dulhunty JM, Udy A, Thomas P et al. Do burn patients cost more? The intensive care unit costs of burn patients compared with controls matched for length of stay and acuity. J Burn Care Res. 2010;31:598–602. doi: 10.1097/BCR.0b013e3181e4d6a4. [DOI] [PubMed] [Google Scholar]
- 8.Mirastschijski U, Sander JT, Weyand B, Rennekampff HO. Rehabilitation of burn patients: An underestimated socio-economic burden. Burns. 2013;39:262–268. doi: 10.1016/j.burns.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 9.Carey K, Kazis LE, Lee AF, Liang MH et al. Multi-center benchmarking study working group. Measuring the cost of care for children with acute burn injury. J Trauma Acute Care Surg. 2012;73:229–233. doi: 10.1097/TA.0b013e318265c88a. [DOI] [PubMed] [Google Scholar]
- 10.Ahn CS, Maitz PK. The true cost of burn. Burns. 2012;38:967–974. doi: 10.1016/j.burns.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 11.Sahin I, Ozturk S, Alhan D, Açikel C, Isik S. Cost analysis of acute burn patients treated in a burn centre: the Gulhane experience. Ann Burns Fire Disasters. 2011;24:9–13. [PMC free article] [PubMed] [Google Scholar]
- 12.Ali SN, Soueid A, Rao K, Moiemen N. Self-inflicted burns, outcome and cost. Burns. 2006;32:463–466. doi: 10.1016/j.burns.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 13.Cornish P, Mittmann N, Gomez M, Cartotto RC, Fish JS. Cost of medications in patients admitted to a burn center. Am J Clin Dermatol. 2003;4:861–867. doi: 10.2165/00128071-200304120-00005. [DOI] [PubMed] [Google Scholar]
- 14.Takayanagi K, Kawai S, Aoki R. The cost of burn care and implications for efficient care. Clin Perform Qual Health Care. 1999;7:70–73. [PubMed] [Google Scholar]
- 15.Park SY, Choi KA, Jang YC, Oh SJ. The risk factors of psychosocial problems for burn patients. Burns. 2008;34:24–31. doi: 10.1016/j.burns.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 16.Sanchez JL, Bastida JL, Martínez MM, Moreno JM, Chamorro JJ. Socio-economic cost and health-related quality of life of burn victims in Spain. Burns. 2008;34:975–981. doi: 10.1016/j.burns.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 17.Kai-Yang L, Shi-Hui Z, Hong-Tai T, Yi-Ta J et al. The direct hospitalisation costs of paediatric scalds: 2-year results of a prospective case series. Burns. 2009;35:738–745. doi: 10.1016/j.burns.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Evasovich M, Klein R, Muakkassa F, Weekley R. The economic effect of child abuse in the burn unit. Burns. 1998;24:642–645. doi: 10.1016/s0305-4179(98)00070-9. [DOI] [PubMed] [Google Scholar]
- 19.Allorto NL, Clarke DL, Thomson SR. management of burns at a regional hospital in South Africa. Burns. 2011;37:1033–1037. doi: 10.1016/j.burns.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 20.Karimi H, Motevalian A, Motabar AR, Safari R et al. Epidemiology of paediatric burns in Iran. Ann Burns Fire Disasters. 2012;25:115–120. [PMC free article] [PubMed] [Google Scholar]
- 21.Muller MJ, Herndon DN. The challenge of burns. Lancet. 1994;343:216–220. doi: 10.1016/s0140-6736(94)90995-4. [DOI] [PubMed] [Google Scholar]
- 22.Kilburn N. Socioeconomic impact of children’s burns - A pilot study. Burns. 2014;S0305:4179(14)–00105-3. doi: 10.1016/j.burns.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 23.Fauerbach JA, Lezotte D, Hills RA, Cromes GF et al. Burden of burn: A norm-based inquiry into the influence of burn size and distress on recovery of physical and psychosocial function. J Burn Care Rehabil. 2005;26:21–32. doi: 10.1097/01.bcr.0000150216.87940.ac. [DOI] [PubMed] [Google Scholar]


