Abstract
Somatostatin receptor imaging with 68Ga-DOTATATE PET/CT (DOTATATE) is increasingly used for managing patients with neuroendocrine tumors. The objective of this study was to determine referring physicians’ perspectives on the impact of DOTATATE on the management of neuroendocrine tumors.
Methods
A set of 2 questionnaires (pre-PET and post-PET) was sent to the referring physicians of 100 consecutive patients with known or suspected neuroendocrine tumors, who were evaluated with DOTATATE. Questionnaires on 88 patients were returned (response rate, 88%). Referring physicians categorized the DOTATATE findings on the basis of the written PET reports as negative, positive, or equivocal for disease. The likelihood for metastatic disease was scored as low, moderate, or high. The intended management before and changes as a consequence of the PET study were indicated.
Results
The indications for PET/CT were initial and subsequent treatment strategy assessments in 14% and 86% of patients, respectively. Referring physicians reported that DOTATATE led to a change in suspicion for metastatic disease in 21 patients (24%; increased and decreased suspicion in 9 [10%] and 12 [14%] patients, respectively). Intended management changes were reported in 53 of 88 (60%) patients. Twenty patients (23%) scheduled to undergo chemotherapy were switched to treatments without chemotherapy, and 6 (7%) were switched from watch-and-wait to other treatment strategies. Conversely, 5 patients (6%) were switched from their initial treatment strategy to watch-and-wait.
Conclusion
This survey of referring physicians demonstrates a substantial impact of DOTATATE on the intended management of patients with neuroendocrine tumors.
Keywords: NET, neuroendocrine tumors, somatostatin receptor, PET, DOTATATE
Imaging somatostatin receptor (SSTR) expression using 68Ga-labeled SSTR agonists represents the diagnostic arm of the 68Ga/90Y/177Lu theranostic pair used for managing neuroendocrine tumors (NETs). Epidemiologic data demonstrate that the prevalence and incidence of NETs is increasing (1973, 1.09/100,000; 2004, 5.25/100,000) (1). Because metastases at the time of diagnosis are present in around 20%–50% (2,3) and tumors recur in 40%–60% of patients (4,5), there is a clinical need for an imaging assay that allows for precise staging and restaging of the disease while at the same time serving as a predictive biomarker for treatment response.
Assessing the expression of SSTRs has been the domain of 111In-diethylene triamine pentaacetic acid-octreotide, which preferentially binds to SSTR 2 (6) and detects gastroenteropancreatic NETs with a median sensitivity of 84% (7). Hybrid SPECT/CT scanners have not improved the detection of lesions smaller than 1.5 cm (8). More recently, 68Ga-labeled SSTR agonists such as 68Ga-DOTATOC, 68Ga-DOTANOC, and 68Ga-DOTATATE were introduced for PET imaging (9,10) and have been shown to detect and phenotype NETs with a high accuracy (11).
However, high accuracy of a diagnostic test does not necessarily translate into an impact on patient management. We were recently granted an Investigational New Drug (IND) application by the Food and Drug Administration to prospectively determine whether and how 68Ga-DOTATATE imaging affects the management of patients with NETs.
MATERIALS AND METHODS
We obtained an IND from the Food and Drug Administration that allowed us to study 100 patients. From June 2013 to July 2014, we enrolled 100 patients (age 18 y or older) with suspected or histologically proven NETs referred to UCLA for a clinical 68Ga-DOTATATE PET/CT (DOTATATE) scan. The prospective questionnaire of referring physicians was approved by the University of California, Los Angeles Institutional Review Board (IRB). Because referring physicians were surveyed on the impact of this diagnostic test on patient management, the informed consent requirements were waived by the IRB.
Patient Preparation and Image Acquisition
Patients fasted for 4 h before the PET/CT study. Patients on SSTR blockade were scanned before the scheduled monthly dose of long-acting octreotide (12).
DOTATATE was synthesized using the fractionated method as described before (13). It was injected intravenously at a dose of 5.1 ± 188.7 ± 18.5 MBq (5.1 ± 0.5 mCi; range, 122.1–210.9 MBq [3.3–5.7 mCi]). A tracer uptake time of 60 min (mean, 63 ± 8 min) was allowed before imaging with a 64-detector PET/CT system commenced (Biograph True Point 64 or Biograph mCT; Siemens). No adverse events occurred during the tracer uptake period and the scanning procedure. Furthermore, no subsequent adverse events were brought to our attention by patients or referring physicians. Scanning time per bed position varied between 2 and 5 min depending on patient weight (14).
PET images were reconstructed with an iterative algorithm (ordered-subset expectation maximization; 2 iterations, 8 subsets). The CT acquisition parameters were 130 kV, 0.5-s tube rotation, 4-mm slice collimation, and a bed speed of 8 mm/s. The CT images were reconstructed using filtered backprojection at 3.4 mm axial intervals to match the slice separation of the PET data. A previously published CT-based algorithm was used for attenuation correction and lesion localization (15). Intravenous contrast was administered in 81 of 88 patients (92%) using 90–115 mL of Omnipaque 350 (GE Healthcare) with an injection speed of 2 mL/s.
Image Interpretation
DOTATATE studies were interpreted qualitatively during a clinical readout session. Scans were classified as positive if focally increased tracer uptake not attributable to normal physiologic uptake was seen and as negative if no increased tracer uptake was identified. Scans were interpreted as equivocal if focally increased tracer uptake was not clearly physiologic or pathologic. Pertinent clinical information such as patient history, biopsy results, and reports from previous imaging tests were available at the time of image interpretation. The written reports of the imaging studies were used by the referring physicians to classify PET interpretations as positive, negative, or equivocal.
Survey
Eighteen referring physicians participated in the survey. A set of 2 questionnaires per patient was mailed to the referring physicians as follows: the first was a pre-PET questionnaire inquiring about the indications for the study (initial vs. subsequent treatment strategy); tumor characteristics such as grade, primary location, and stage; the level of clinical suspicion for metastases; previous imaging and therapy; the planned treatment approach; and whether additional imaging was intended. The second questionnaire, post-PET, required referring physicians to categorize the DOTATATE findings on the basis of the written PET reports as negative, positive, or equivocal for disease. They were asked to score the likelihood for metastatic disease as low, moderate, or high. Furthermore, the survey inquired about any unexpected metastases and the need for additional biopsies. Finally, referring physicians were queried about intended management changes as a consequence of the PET study.
Statistical Analysis
The suspicion for metastatic disease based on written PET reports was scored by referring physicians as 0, low; 1, moderate; or 2, high on the pre- and post-PET questionnaires. Changes in the level of suspicion were classified as increasing, decreasing, or unchanged. The intended treatment plan was recorded before and after the scan, and changes in treatment were determined for each patient. The treatment options were watch-and-wait, radiation, chemotherapy, octreotide analogs, surgery, peptide receptor radiotherapy (PRRT), and other. Changes from one modality to another or the addition of a different modality were classified as change in treatment plan. Selection of the same modality before and after the scan was categorized as no change. To simplify the analysis, we focused on changes from/to watch-and-wait, from/to surgery, and from/to chemotherapy.
RESULTS
Referring Physicians and Questionnaires
One hundred patients were referred by 18 physicians. Referring physicians returned 88 of 100 complete sets of pre- and post-PET questionnaires (response rate, 88%). Pre- and post-PET questionnaires were completed within a median of 9.0 d (mean, 12.9 ± 14.9 d) and 13.5 d (mean, 30.8 ± 37.1 d) after the scan, respectively.
Patient Population and Treatment History
The patient population consisted of 38 men and 50 women, with a mean age of 59 ± 12 y (range, 27–84 y). Primary tumor location, tumor grades, and tumor stages are listed in Table 1. Twelve patients (13.6%) were referred for initial treatment strategy assessment, and the remaining 76 patients (86.4%) underwent subsequent treatment strategy assessments.
TABLE 1.
Patient Characteristics
| Characteristic | Primary staging (n = 12) |
Restaging (n = 76) |
|---|---|---|
| Primary tumor location | 12 (100.0%) | 76 (100.0%) |
| Chest | 3 (25.0%) | 10 (13.2%) |
| Pancreas | 4 (33.3%) | 18 (23.7%) |
| Small bowel | 1 (8.3%) | 30 (39.5%) |
| Colon | 1 (8.3%) | 4 (5.3%) |
| Other | 0 (0.0%) | 5 (6.6%) |
| Unknown | 3 (25.0%) | 9 (11.8%) |
| Tumor grade | ||
| Low | 6 (50.0%) | 34 (44.7%) |
| Intermediate | 2 (16.7%) | 26 (34.2%) |
| High | 0 (0.0%) | 7 (9.2%) |
| Unknown | 4 (33.3%) | 9 (11.8%) |
| Tumor stage | ||
| I | 0 (0.0%) | 8 (10.5%) |
| II | 1 (8.3%) | 2 (2.6%) |
| III | 1 (8.3%) | 12 (15.8%) |
| IV | 3 (25.0%) | 48 (63.2%) |
| Unknown | 7 (58.3%) | 6 (7.9%) |
Twelve of 88 patients (13.6%) had no prior treatment. Of the remaining 76 patients, 6 (7.9%) had only chemotherapy, 26 (34.2%) only surgery, 8 (10.5%) only octreotide, 5 (6.6%) chemotherapy and surgery, 2 (2.6%) chemotherapy and octreotide, and 1 (1.3%) chemotherapy and PRRT. Two patients (2.6%) had surgery and PRRT and 19 (25.0%) surgery and octreotide. The remaining 7 patients had prior surgery, octreotide, and either chemotherapy (n = 4; 5.3%), PRRT (n = 2; 2.6%), or both (n = 1; 1.3%).
Referring Physicians’ Interpretation of Clinical PET Reports
DOTATATE reports were interpreted by the referring physicians as negative in 28 (31.8%), positive in 55 (62.5%), and equivocal in 5 (5.7%) patients. In addition, metastases unknown by the referring physician before PET were found in 38 patients (43.2%) (Supplemental Table 1; supplemental materials are available at http://jnm.snmjournals.org).
Level of Suspicion for Metastatic Disease
Responding physicians reported that the pre-PET suspicion for metastatic disease was low in 24 patients (27.3%), intermediate in 13 patients (14.8%), and high in 51 patients (58.0%). After PET, the suspicion level remained unchanged in 67 patients (76.1%), decreased in 12 (13.6%), and increased in 9 (10.2%) patients (Figs. 1 and 2; Table 2; Supplemental Table 1). Thus, the level of suspicion for metastatic disease changed in 23.9% of the patients.
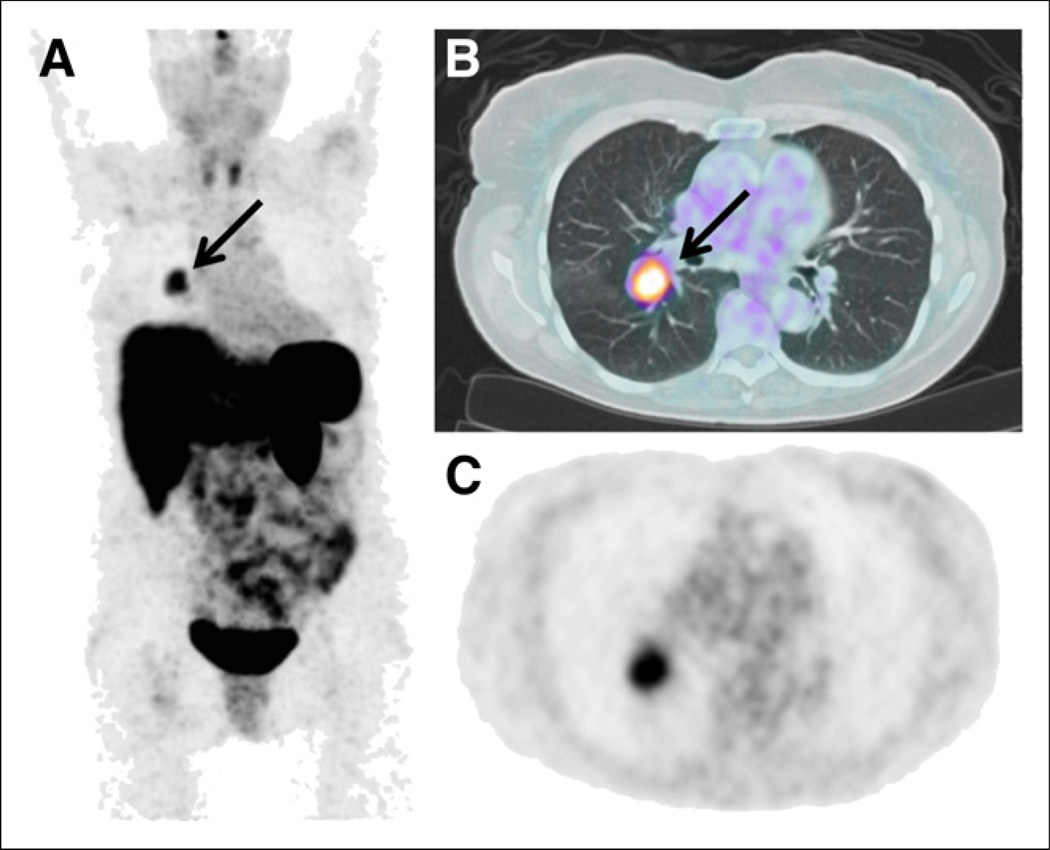
FIGURE 1.
A 75-y-old female patient with stage IIIB pulmonary carcinoid (arrow). (A) Maximum-intensity projection. (B and C) Axial images. The level of suspicion for metastasis decreased from moderate to low after the DOTATATE study. Because the previously biopsied tumor was positive for SSTR expression by imaging, intended management was switched from surgery to surgery + octreotide.
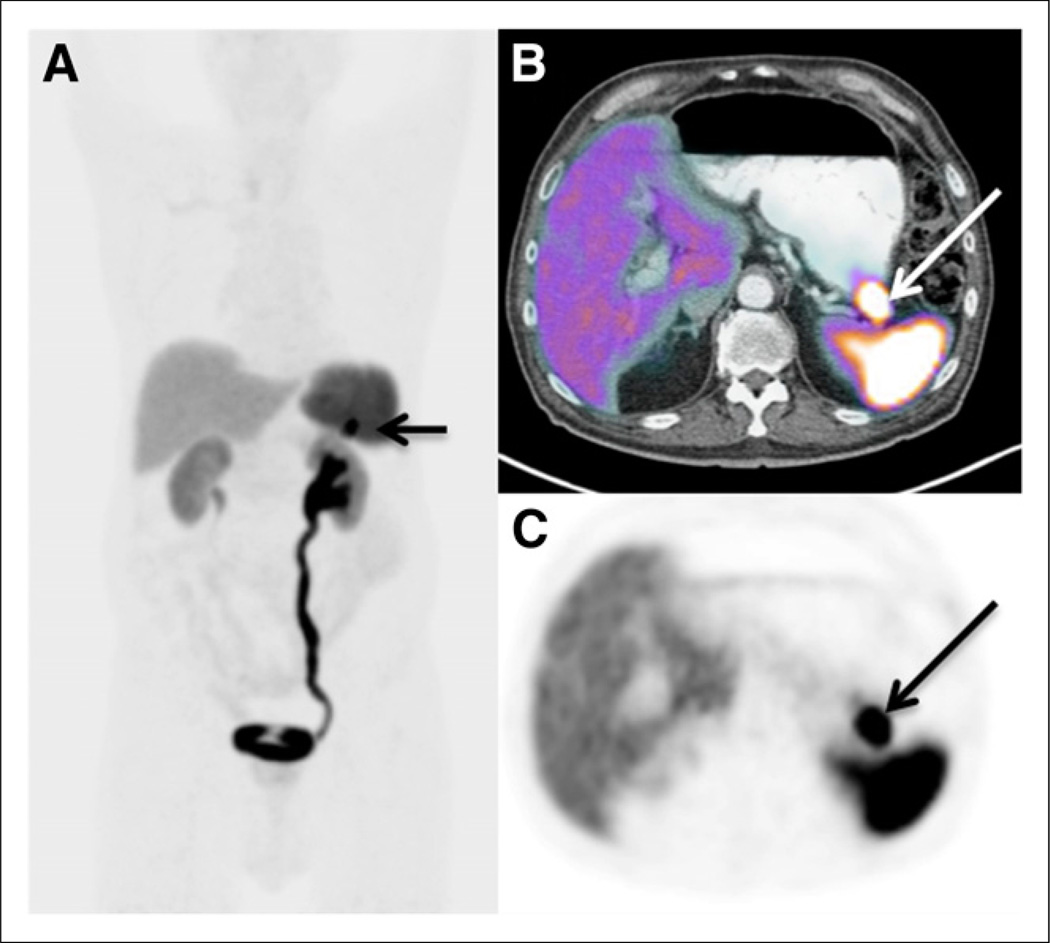
FIGURE 2.
A 78-y-old male patient whose pancreatic head NET had been resected. Other imaging tests, including recent CT, revealed no evidence for metastatic disease. An unexpected pancreatic tail lesion was identified by DOTATATE (arrow). (A) Maximum-intensity projection. (B and C) Axial images. On the basis of this finding, the level of suspicion for metastatic disease increased from low to high. Intended treatment was switched from watch-and-wait to somatostatin therapy and surgery.
TABLE 2.
Changes of M1 Suspicion
| Suspicion for M1 disease | n |
|---|---|
| Increased | 9 |
| Low to intermediate | 2 |
| Low to high | 6 |
| Intermediate to high | 1 |
| Decreased | 12 |
| Intermediate to low | 10 |
| High to low | 2 |
| High to intermediate | 0 |
Clinical Assessment After PET and Impact of DOTATATE on Patient Management
Referring physicians interpreted all available clinical information including PET and concluded that there was no evidence for disease in 25 patients (28.4%), evidence for primary tumor without regional or distant metastases in 6 patients (6.8%), lymph node involvement in 3 patients (3.4%), and distant metastases in 54 patients (61.4%) (Supplemental Table 1).
The intended treatment for each patient before PET/CT is listed in Supplemental Table 2. The most frequent intended treatment strategies before PET included watch-and-wait (20/88; 23%), octreotide (9/88; 10%), surgery (7/88; 8%), and chemotherapy + octreotide (11/88; 13%). DOTATATE imaging resulted in intended management changes in 53 of 88 (60.2%) patients (Fig. 3). All intended treatment changes as a consequence of PET are listed in Supplemental Table 3.
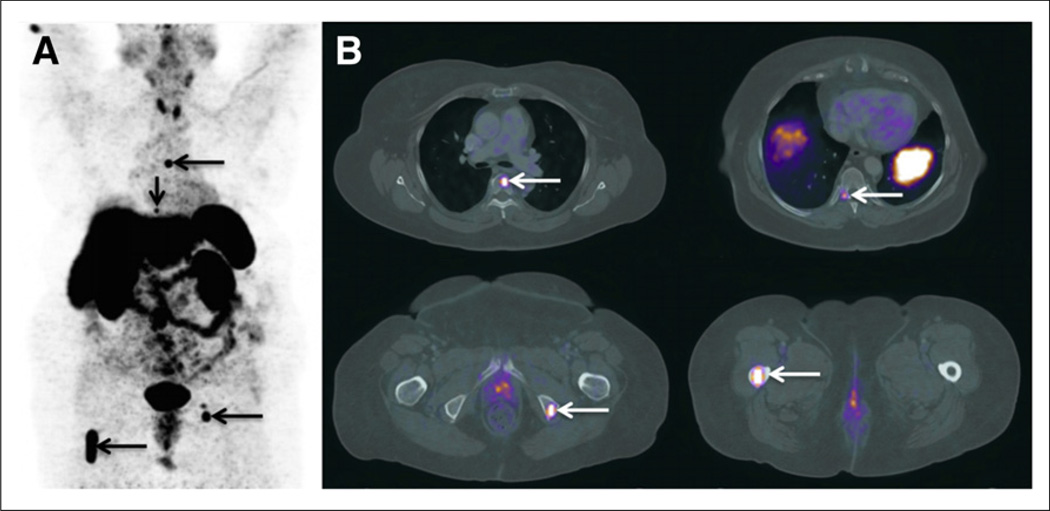
FIGURE 3.
A 70-y-old female patient with a history of midgut carcinoid with known soft-tissue and bone metastases based on outside 111In-octreotide study. Outside MR imaging reported a 6.5-cm lesion within the right proximal femur diaphysis with benign appearance and without gadolinium enhancement. Corresponding DOTATATE maximum-intensity projection (A) revealed multiple mesenteric and pelvic, as well as multiple unexpected osseous metastases (arrows), shown in more detail in axial images (B). The level of suspicion for metastases remained unchanged (high), but intended treatment was switched from surgery and octreotide to surgery, octreotide, and selective radiotherapy of bone metastases.
The most relevant intended management changes are depicted in Table 3: 20 patients (22.7%) scheduled to undergo chemotherapy were switched to treatments without chemotherapy (Fig. 4), whereas 3 patients were switched to a chemotherapy-including treatment plan. In 6 (6.8%) patients, watch-and-wait was changed to other treatment strategies. Conversely, in 5 patients (5.7%) the initial treatment strategy was replaced by watch-and-wait. Three patients initially planned to undergo surgery only were switched to surgery + octreotide (2/88) or watch-and-wait (1/88). In contrast, 1 (1/88) patient was switched from a multimodality approach to surgery alone.
TABLE 3.
Extract of Intended Treatment Changes after 68Ga-DOTATATE
| Treatment change | n | % |
|---|---|---|
| Switched from CTx to treatment without chemotherapy | ||
| CTx + octreotide → octreotide | 6 | 6.8 |
| CTx + octreotide → octreotide + surgery | 1 | 1.1 |
| CTx + octreotide → watch-and-wait | 1 | 1.1 |
| CTx + octreotide + other → octreotide | 2 | 2.3 |
| CTx + octreotide + PRRT → octreotide | 1 | 1.1 |
| CTx + octreotide + PRRT → octreotide + surgery | 1 | 1.1 |
| CTx + octreotide + PRRT + other → surgery | 1 | 1.1 |
| CTx + octreotide + PRRT + other → octreotide + surgery | 2 | 2.3 |
| CTx + octreotide + surgery → octreotide | 1 | 1.1 |
| CTx + octreotide + surgery → octreotide + surgery | 1 | 1.1 |
| CTx + octreotide + surgery + PRRT → octreotide + surgery + other | 1 | 1.1 |
| CTx + octreotide + surgery + PRRT + other → octreotide | 1 | 1.1 |
| CTx + RTx + surgery → PRRT | 1 | 1.1 |
| Total | 20 | 22.7 |
| Switched to a chemotherapy-including treatment plan | ||
| Octreotide → CTx + octreotide | 1 | 1.1 |
| Watch-and-wait → CTx + octreotide + surgery | 1 | 1.1 |
| Watch-and-wait → CTx + octreotide + surgery + other | 1 | 1.1 |
| Total | 3 | 3.4 |
| Watch-and-wait changed to other treatment strategies | ||
| Watch-and-wait → octreotide + surgery | 2 | 2.3 |
| Watch-and-Wait → CTx + octreotide + surgery | 1 | 1.1 |
| Watch-and-wait → CTx + octreotide + surgery + other | 1 | 1.1 |
| Watch-and-wait + octreotide → octreotide | 1 | 1.1 |
| Watch-and-wait + octreotide → octreotide + surgery | 1 | 1.1 |
| Total | 6 | 6.8 |
| Initial treatment strategy switched to watch-and-wait | ||
| Surgery → watch-and-wait | 1 | 1.1 |
| Octreotide → watch-and-wait | 2 | 2.3 |
| Octreotide + surgery + other → watch-and-wait | 1 | 1.1 |
| CTx + octreotide → watch-and-wait | 1 | 1.1 |
| Total | 5 | 5.7 |
| Surgery switched to surgery + octreotide or watch-and-wait | ||
| Surgery → octreotide + surgery | 2 | 2.3% |
| Surgery → watch-and-wait | 1 | 1.1% |
| Total | 3 | 3.4% |
| Switched from a multimodality approach to surgery alone | ||
| CTx + octreotide + PRRT + other → surgery | 1 | 1.1% |
| Total | 1 | 1.1% |
CTx = chemotherapy; RTx = radiotherapy.
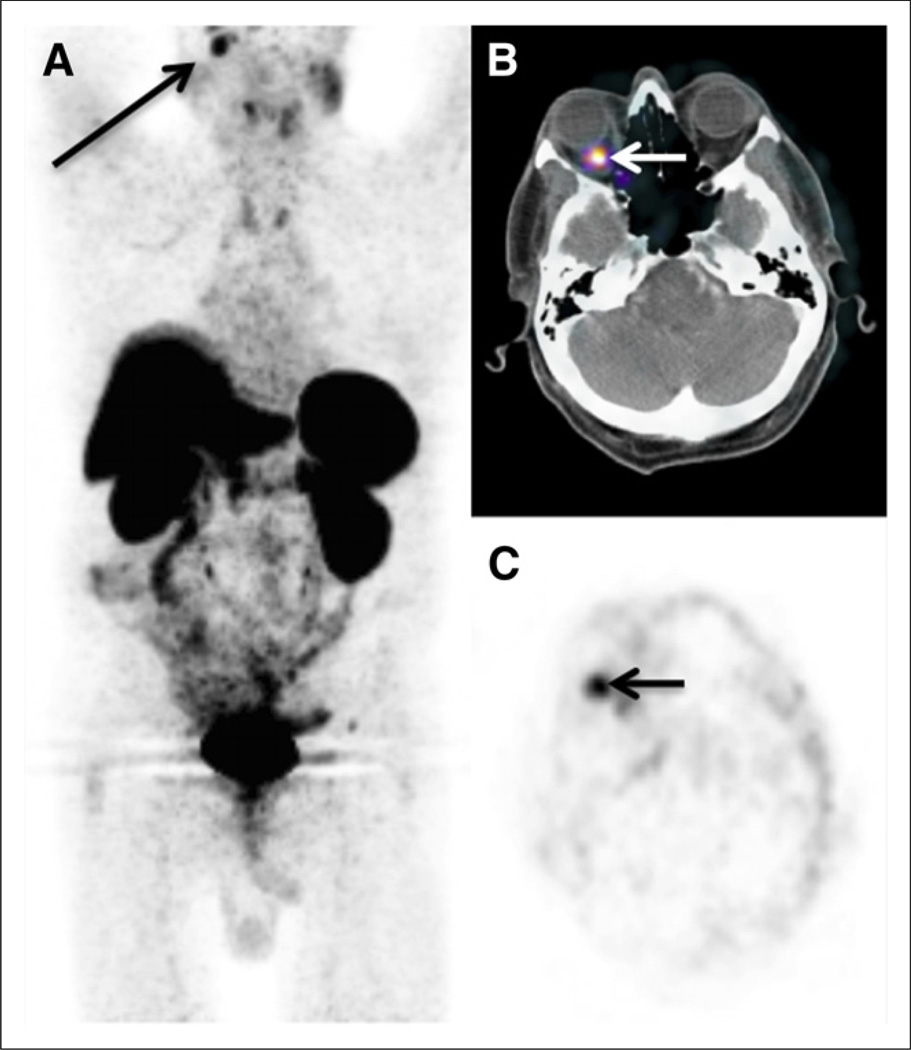
FIGURE 4.
A 74-y-old male patient with history of pancreatic NET found to have an orbital metastasis (maximum-intensity projection [A] and axial images [B and C] show a metastasis in the right retroorbital region [arrows]), which was histopathologically confirmed by biopsy. No other metastases were identified. Intended treatment was therefore switched from chemotherapy, octreotide, and surgery to octreotide and surgery.
In addition to patient management, patient safety was also observed for adverse reactions during administration of DOTATATE and for 1 h after its administration. At approximately 24 h after administration of DOTATATE, patients were questioned about any signs or symptoms of a drug reaction and any adverse reactions. The results indicated no discomfort or adverse events associated with DOTATATE.
DISCUSSION
This prospective survey of treating physician’s perspective demonstrates a substantial impact of DOTATATE on the intended management of patients with NETs. DOTATATE changed intended management in 60% of the patients. Importantly, the intent to treat with chemotherapy was changed to intended strategies without chemotherapy in more than 20% of the population.
Forty-three percent of PET reports were interpreted by referring physicians as showing evidence for unexpected metastases. However, the level of suspicion for metastatic disease changed only in 24% of the patients. This difference is explained by additional lesions detected by DOTATATE in patients with already known metastatic disease as illustrated in Figure 5. Previous retrospective studies in patients with NETs had reported a comparable impact of DOTATATE or DOTATOC on patient management (16,17). Another study (18) in 64 patients reported a switch to or from chemotherapy in 16% of the patients. Interestingly, this study also identified a need for contrast-enhanced PET/CT studies as 21% of the management changes were based on CT findings. This justifies performing the CT portion of the PET/CT as a diagnostic CT (including intravenous and oral contrast) rather than as a low-dose CT for attenuation correction only.
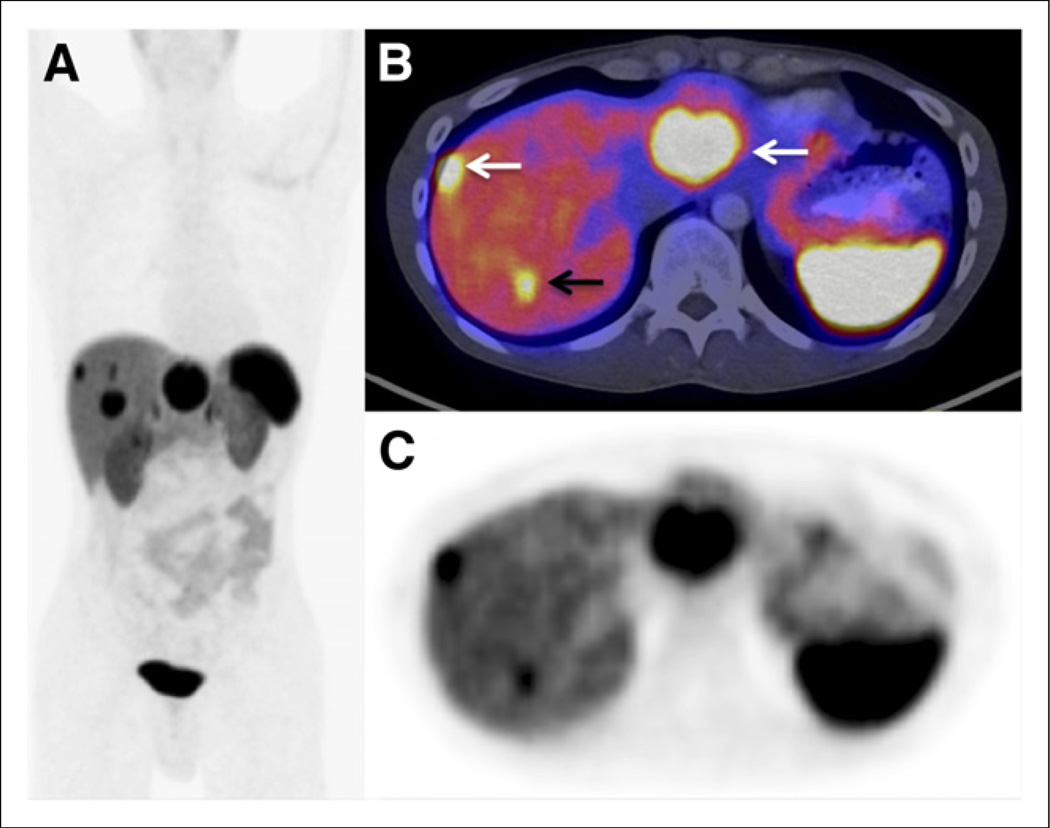
FIGURE 5.
A 36-y-old male with pancreatic NET and known liver metastases was referred for subsequent treatment strategy assessment. Multiple liver metastases are seen on the maximum-intensity-projection image (A). Axial views show the known (white arrows) and an unexpected additional liver metastasis (black arrow). Despite an additional metastasis discovered by DOTATATE, both the level of suspicion for metastatic disease (high) and the intended management (surgical removal of liver metastases) remained unchanged.
Thirty-two percent of DOTATATE reports were interpreted by referring physicians as negative for disease. However, their overall clinical assessment concluded that only 28% of the patients were disease-free. Thus, in 3 patients the DOTATATE scan was considered false-negative. Two of these patients had aggressive, dedifferentiated disease indicated by proliferation indices of 25% and 95%, likely associated with loss of SSTR expression (19). In both patients, the anatomically evident lesions were considered true-positive for metastatic disease. The third patient had sclerotic, DOTATATE-negative bone lesions and a prior history of prostate cancer. No biopsy was available, and the referring physician attributed the bone metastases to the NET rather than the prostate cancer. Intended management changes occurred much more frequently than changes in the level of suspicion for metastatic disease. One explanation is that confirmation of SSTR expression of metastatic lesions led to changes from chemotherapy to octreotide-based treatments (Table 3; Fig. 4). In other patients, DOTATATE ruled out or confirmed disease, leading to changes to/from watch-and-wait. Most likely DOTATATE increased the confidence of intended treatment plans or helped to decide among multiple available treatment modalities.
It is important to mention that the current study has some limitations. First, the surveyed physicians were all users of PET. The reported impact on management may therefore by study design favor PET. Second, this study evaluated only intended changes of treatment strategy. It was beyond the scope of this study to analyze implementation of intended management changes as well as the impact of PET on patient outcome. Third, we investigated a heterogeneous group of patients including staging and restaging, previously known metastases as well as patients with a low probability of metastatic disease. However, we believe that this heterogeneity represents a realistic clinical scenario for DOTATATE imaging.
DOTATATE and DOTATOC are the diagnostic standard of care in patients with NETs in most parts of the world. However, because DOTATATE is not approved in the United States, the current study required an IND granted by the Food and Drug Administration.
CONCLUSION
The major impact of DOTATATE or DOTATOC on the management of patients with NETs established retrospectively (16–18) and now prospectively emphasizes the need for professional organizations and patient advocacy groups to collaborate and petition the Food and Drug Administration for rapid approval of DOTATATE without the need for large-scale randomized trials. It appears ethically questionable to conduct trials between 2 diagnostic modalities when one of them has already been shown to provide higher diagnostic accuracy.
In summary, 68Ga-DOTATATE PET/CT affects the intended management of 60% of patients with SSTR-expressing NETs. Future studies will need to determine prospectively whether these management changes are implemented and if treatment changes have an impact on patient outcome.
Supplementary Material
Acknowledgments
We thank Dr. Ronald Walker at Vanderbilt University for providing us a letter of authorization to reference the Vanderbilt DOTATATE IND.
Footnotes
DISCLOSURE
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26:3063–3072. doi: 10.1200/JCO.2007.15.4377. [DOI] [PubMed] [Google Scholar]
- 2.Fischer L, Bergmann F, Schimmack S, et al. Outcome of surgery for pancreatic neuroendocrine neoplasms. Br J Surg. 2014;101:1405–1412. doi: 10.1002/bjs.9603. [DOI] [PubMed] [Google Scholar]
- 3.Sharma P, Arora S, Dhull VS, et al. Evaluation of Ga-DOTANOC PET/CT imaging in a large exclusive population of pancreatic neuroendocrine tumors. Abdom Imaging. 2014 Aug 19; doi: 10.1007/s00261-014-0219-5. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Boninsegna L, Panzuto F, Partelli S, et al. Malignant pancreatic neuroendocrine tumour: lymph node ratio and Ki67 are predictors of recurrence after curative resections. Eur J Cancer. 2012;48:1608–1615. doi: 10.1016/j.ejca.2011.10.030. [DOI] [PubMed] [Google Scholar]
- 5.Welin S, Stridsberg M, Cunningham J, et al. Elevated plasma chromogranin A is the first indication of recurrence in radically operated midgut carcinoid tumors. Neuroendocrinology. 2009;89:302–307. doi: 10.1159/000179900. [DOI] [PubMed] [Google Scholar]
- 6.de Herder WW, Hofland LJ, van der Lely AJ, Lamberts SW. Somatostatin receptors in gastroentero-pancreatic neuroendocrine tumours. Endocr Relat Cancer. 2003;10:451–458. doi: 10.1677/erc.0.0100451. [DOI] [PubMed] [Google Scholar]
- 7.Modlin IM, Kidd M, Latich I, Zikusoka MN, Shapiro MD. Current status of gastrointestinal carcinoids. Gastroenterology. 2005;128:1717–1751. doi: 10.1053/j.gastro.2005.03.038. [DOI] [PubMed] [Google Scholar]
- 8.Sundin A. Radiological and nuclear medicine imaging of gastroenteropancreatic neuroendocrine tumours. Best Pract Res Clin Gastroenterol. 2012;26:803–818. doi: 10.1016/j.bpg.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Maecke HR, Reubi JC. Somatostatin receptors as targets for nuclear medicine imaging and radionuclide treatment. J Nucl Med. 2011;52:841–844. doi: 10.2967/jnumed.110.084236. [DOI] [PubMed] [Google Scholar]
- 10.Werner RA, Bluemel C, Allen-Auerbach MS, Higuchi T, Herrmann K. Gallium- and yttrium-/lutetium: “theranostic twins” for diagnosis and treatment of NETs. Ann Nucl Med. 2014 Aug 20; doi: 10.1007/s12149-014-0898-6. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Srirajaskanthan R, Kayani I, Quigley AM, Soh J, Caplin ME, Bomanji J. The role of 68Ga-DOTATATE PET in patients with neuroendocrine tumors and negative or equivocal findings on 111In-DTPA-octreotide scintigraphy. J Nucl Med. 2010;51:875–882. doi: 10.2967/jnumed.109.066134. [DOI] [PubMed] [Google Scholar]
- 12.Haug AR, Rominger A, Mustafa M, et al. Treatment with octreotide does not reduce tumor uptake of 68Ga-DOTATATE as measured by PET/CT in patients with neuroendocrine tumors. J Nucl Med. 2011;52:1679–1683. doi: 10.2967/jnumed.111.089276. [DOI] [PubMed] [Google Scholar]
- 13.Breeman WA, de Jong M, de Blois E, Bernard BF, Konijnenberg M, Krenning EP. Radiolabelling DOTA-peptides with 68Ga. Eur J Nucl Med Mol Imaging. 2005;32:478–485. doi: 10.1007/s00259-004-1702-y. [DOI] [PubMed] [Google Scholar]
- 14.Halpern BS, Dahlbom M, Quon A, et al. Impact of patient weight and emission scan duration on PET/CT image quality and lesion detectability. J Nucl Med. 2004;45:797–801. [PubMed] [Google Scholar]
- 15.Kinahan PE, Townsend DW, Beyer T, Sashin D. Attenuation correction for a combined 3D PET/CT scanner. Med Phys. 1998;25:2046–2053. doi: 10.1118/1.598392. [DOI] [PubMed] [Google Scholar]
- 16.Frilling A, Sotiropoulos GC, Radtke A, et al. The impact of 68Ga-DOTATOC positron emission tomography/computed tomography on the multimodal management of patients with neuroendocrine tumors. Ann Surg. 2010;252:850–856. doi: 10.1097/SLA.0b013e3181fd37e8. [DOI] [PubMed] [Google Scholar]
- 17.Hofman MS, Kong G, Neels OC, Eu P, Hong E, Hicks RJ. High management impact of Ga-68 DOTATATE (GaTate) PET/CT for imaging neuroendocrine and other somatostatin expressing tumours. J Med Imaging Radiat Oncol. 2012;56:40–47. doi: 10.1111/j.1754-9485.2011.02327.x. [DOI] [PubMed] [Google Scholar]
- 18.Ruf J, Heuck F, Schiefer J, et al. Impact of multiphase 68Ga-DOTATOC-PET/CT on therapy management in patients with neuroendocrine tumors. Neuroendocrinology. 2010;91:101–109. doi: 10.1159/000265561. [DOI] [PubMed] [Google Scholar]
- 19.Binderup T, Knigge U, Loft A, et al. Functional imaging of neuroendocrine tumors: a head-to-head comparison of somatostatin receptor scintigraphy, 123I-MIBG scintigraphy, and 18F-FDG PET. J Nucl Med. 2010;51:704–712. doi: 10.2967/jnumed.109.069765. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.