Abstract
Hearing rehabilitation tends to focus on the influence of intraindividual factors and concepts such as readiness for change and health beliefs. In contrast, less is known about the role of social context and the potential role of significant others on hearing aid adoption. This explorative retrospective study investigated whether hearing aid adoption is associated with significant other attendance at audiology appointments. The study sample consisted of 33,933 and 27,031 individuals who attended appointments either alone or with a significant other, respectively (n = 60,964). It was found that hearing aid adoption was significantly greater when patients attended audiology appointments with a significant other (63.8%) than when attending appointments alone (50.6%). The association between hearing aid adoption and attendance by a significant other was hearing dependent, with 96% higher hearing aid adoption for patients with mild hearing losses when patients attended appointments with a significant other than when attending appointments alone. Hearing aid return rates were comparable when patients attended appointments alone (27%) or with a significant other (24%). Several potential explanations for the observed association are discussed. The pattern of results is consistent with the view that greater adherence is observed when audiologic care is provided from a patient-centered care perspective. Future research should establish whether there is a causal relationship between attendance at appointments by significant others and hearing aid adoption and should attempt to better understand the mechanisms underpinning the relationship between these variables.
Keywords: social context, hearing aids, social support, help seeking, decision making
Introduction
For hundreds of millions of people globally, disabling hearing loss compromises the ability to fully participate in society. Left untreated, hearing loss is associated with negative consequences in economic, physical, cognitive, psychosocial, emotional, and behavioral domains of one’s life (Dalton et al., 2003; Lin, 2011). Hearing aids are often an essential component of hearing loss rehabilitation. Use of hearing aids has been found to improve quality of life and decrease psychological and socio-emotional effects of hearing loss (Chisolm et al., 2007). Importantly, the uptake of hearing aids remains low with only about one in three individuals who could potentially benefit from hearing aids actually reporting current use of hearing aids (Abrams & Kihm, 2015; Bainbridge & Ramachandran, 2014).
Hearing Aid Adoption
Research investigating hearing rehabilitation has identified several factors associated with hearing aid adoption. Factors positively correlated with hearing aid uptake include (a) degree of hearing impairment (Popelka et al., 1998); (b) awareness of communication difficulties (Carson, 2005; Palmer, Solodar, Hurley, Byrne, & Williams, 2009); (c) self-reported hearing disability (Garstecki & Erler; 1998; Helvik, Wennberg, Jacobsen, & Hallberg, 2008; van den Brink, Wit, Kempen, & van Heuvelen, 1996); (d) finger dexterity and visual acuity (Humes, Wilson, & Humes, 2003; Kochkin, 2007); (e) not feeling stigmatized by hearing impairment (van den Brink et al., 1996; Wallhagen, 2010); (f) willingness to use information communication technologies (Gonsalves & Pichora-Fuller, 2008); (g) dispositions and personality traits such as higher openness to new experiences, less neuroticism, having an internal locus of control (i.e., a belief that one controls events affecting the self), and having fewer coping strategies (e.g., less able to cope without additional hearing rehabilitation; Cox, Alexander, & Gray, 2005); and (h) positive expectations and attitudes of family, significant others (SO), and health-care professionals toward hearing aid cost and ownership (Duijvestijn et al., 2003; Garstecki & Erler, 1998; Kochkin, 2007; Meister, Walger, Brehmer, von Wedel, & von Wedel, 2008; van den Brink et al., 1996). For a review, see Knudsen, Oberg, Nielsen, Naylor, and Kramer (2010) and Meyer and Hickson (2012).
Social Support and Audiologic Outcomes
In general, investigations of hearing aid adoption in the context of hearing rehabilitation have identified mostly intraindividual factors associated with hearing aid uptake. In contrast, less is known about the influence of social context on hearing rehabilitation, although there are some exceptions. For example, recent studies have found noteworthy correlations that link positive audiologic outcomes with interindividual factors such as social support. Hickson, Meyer, Lovelock, Lampert, and Khan (2014) identified factors that differentiate successful from unsuccessful users of hearing aids. They found that reported availability of social support was the factor that best distinguished successful from unsuccessful users of hearing aids. Furthermore, in two studies, the availability of social support was found to be the best predictor of hearing aid satisfaction, outperforming other known predictors of hearing aid satisfaction such as reported benefit from hearing aids, personality, and style of hearing aid (Singh, Lau, & Pichora-Fuller, 2015). Other research has observed that SOs can potentially foster a greater understanding of the communication and psychosocial consequences of the hearing loss, encourage and motivate hard-of-hearing individuals to seek help, help patients adjust to the psychological distress (e.g., depression, anxiety, and paranoia) associated with hearing loss, promote treatment adherence, facilitate communication by reiterating topics of conversation, assist with the care and operation of hearing aids, and improve outcomes of audiologic rehabilitation classes (Carson, 2005; Duijvestijn et al., 2003; Frankel & Turner, 1983; Lockey, Jennings, & Shaw, 2010; Mahoney, Stephens, & Cadge, 1996; Manchaiah, Stephens, & Lunner, 2013; Meyer, Hickson, Lovelock, Lampert, & Kahn, 2014; Preminger, 2003; van den Brink et al., 1996).
Previous research has examined the role of SOs in audiologic rehabilitation (e.g., third-party disability and social support); however, very little research has focused on hearing aid adoption and the role of SOs in the decision to pursue treatment. Critically, SOs are often in the appointment room when treatment options are discussed with patients and SOs. When making a decision to pursue or not to pursue amplification, individuals often experience uncertainty because of incomplete information. Uncertainty can arise from several sources, such as not knowing whether hearing aids are a suitable rehabilitation option that will address the needs of the individual or concerns as to whether the hearing aids will perform as hoped or expected (Urbany, Dickson, & Wilkie, 1989). Previous research suggests that SOs can potentially minimize perceptions of risk and uncertainty that consumers associate with purchase decisions (Kiecker & Hartman, 1994). Significant others can act as interpersonal sources of information, support decision-making processes, and increase confidence that wise decision making takes place (Furse, Punj, & Stewart, 1984; Kiecker & Hartman, 1993; 1994).
The Current Research
The primary goal of the current research is to determine whether there is an association between attendance by SOs at audiology appointments and hearing aid adoption. It is hypothesized that greater hearing aid adoption will be observed when patients attend audiology appointments with an SO than by themselves. The second goal of the research is to determine whether a potential relationship between SO attendance and hearing aid adoption is dependent on the degree of hearing loss. It is hypothesized that hearing aid adoption will be less influenced by the presence of an SO for hearing-impaired individuals with more hearing loss than less hearing loss because individuals with more severe hearing losses may already have sufficient motivation to pursue hearing aids (Popelka et al., 1998). In other words, it could be that individuals with less severe hearing losses may be more hesitant to pursue amplification and that SOs may reduce uncertainty regarding hearing aid adoption. The third goal of the study is to explore whether return rates (i.e., the decision to return the hearing aid before the conclusion of a trial period) are associated with attendance by SOs at audiology appointments. It is hypothesized that return rates will be lower when patients attend audiology appointments with an SO because SOs assist the patient to overcome perceived barriers associated with the successful use of hearing aids (e.g., Hickson et al., 2014).
Exploring the role of SOs in hearing aid adoption is relevant for clinical practice insofar as such knowledge could enable clinicians to assess the extent to which they should encourage SOs to participate in the audiologic rehabilitation process. The study would be the first to provide quantitative evidence in a large-scale data set linking attendance at appointments by SOs, hearing aid adoption, and the decision to return hearing aids. This explorative study was conducted by analyzing existing data from a network of audiology clinics in which patients are encouraged to bring SOs along to appointments.
Methods
Procedures
The study consists of a retrospective examination of 60,964 patient records obtained from a private chain of audiology clinics in the United Kingdom. The participants were first-time patients of the clinics and all received a hearing assessment. Patients of the hearing clinics were encouraged by clinic staff to attend appointments with an SO if possible, and it was recorded whether the patient attended the initial hearing assessment alone (“Alone” condition) or with an SO (“SO” condition). A recommendation for at least one hearing aid was provided to all patients, but it was not recorded whether the recommendation was for one or two hearing aids. Decisions to proceed with a hearing aid were almost always made at the conclusion of the hearing assessment. No information was available that describes the nature of the relationship between the SO and the patient. Informally, it was reported that the person attending the appointment with the patient was typically a spouse, adult child, or parent. None of the participants had previously worn hearing aids.
Outcome Measures
The decisions to purchase and possibly return the hearing aids were measured as follows. Hearing aid adoption is defined as the proportion of patients who made the decision to include amplification as a component of their rehabilitation. Return rate is defined as the proportion of hearing aids that were evaluated by patients but ultimately returned before the conclusion of the trial period.
Sample Characteristics
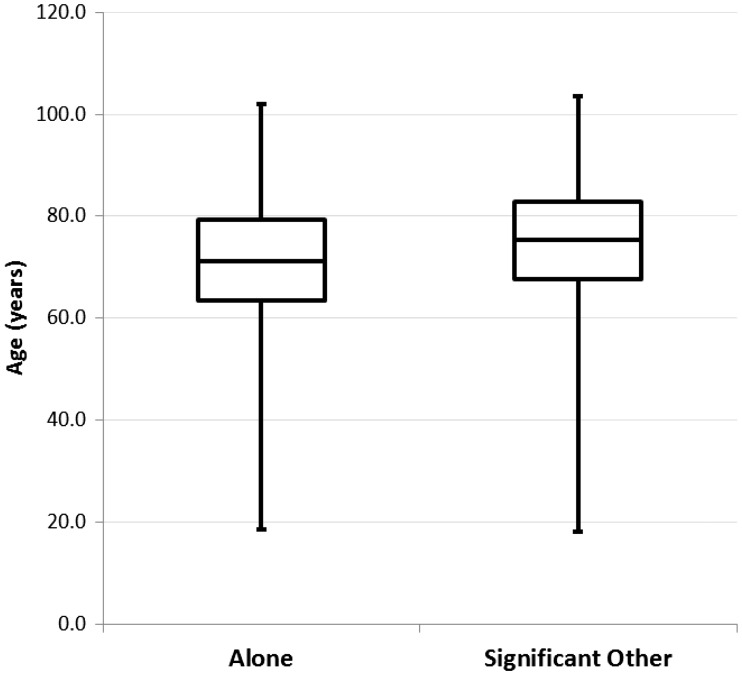
Demographic information regarding the final sample of 60,964 individuals is provided in Table 1. Overall, 44.3% of the sample attended an audiology appointment with an SO. Independent samples t tests revealed that individuals in the SO condition were significantly older and more likely to be male. Details regarding the distribution, dispersion, and skewness of the age of the participants can be found in Figure 1. Audiometric information was only available on a subset of the sample (n = 718), and these details and sample sizes can be found in Table 2. Mild, moderate, and greater than moderate hearing loss was defined using the mean binaural pure-tone audiometric thresholds at 500, 1000, 2000, and 4000 Hz (B4PTA). For the subsample for whom audiometric information was available, independent samples t tests with Sidak–Bonferroni corrections (Šidák, 1967) were calculated (significance level is p level < .009) in order to determine if there are differences in hearing thresholds between the SO and Alone condition. No significant differences in B4PTA were observed for any of the subgroups (see Table 2).
Table 1.
Sample Characteristics (Full Sample).
| Alone | SO | t | df | p | |
|---|---|---|---|---|---|
| Sample size | 33,933 | 27,031 | – | – | – |
| % Female | 56.5 | 54.4 | 5.3 | 60,962 | .000 |
| Mean age (years; SD) | 70.4 (12.4) | 74.5 (11.6) | 48.3 | 60,962 | .000 |
| Adopter mean age (years; SD) | 72.4 (12.0) | 75.8 (11.3) | 27.2 | 34,430 | .000 |
| Non-adopter mean age (years; SD) | 68.3 (12.4) | 72.0 (11.9) | 23.8 | 26,530 | .000 |
| Mean age (years): Returned HA(s) | 72.2 (12.8) | 75.6 (11.9) | 13.0 | 8,854 | .000 |
| Mean age (years): Did not return HA(s) | 72.5 (11.7) | 75.9 (11.1) | 23.8 | 25,574 | .000 |
Note. SD = standard deviation; SO = significant other; HA = hearing aid.
Figure 1.
Box plot (minimum, quartile 1, median, quartile 3, and maximum) describing the age (years) of patients in the Alone and Significant Other conditions.
Table 2.
Mean B4PTA dB HL (SD) [Sample Sizes] for Adopters and Nonadopters in the Alone and SO Conditions.
| Degree of HL | Alone | SO | t | df | P | |
|---|---|---|---|---|---|---|
| Adopters | Mild | 33.2 (5.5) [n = 68] | 33.8 (4.9) [n = 75] | 0.60 | 141 | .550 |
| Moderate | 47.0 (4.0) [n = 122] | 48.2 (4.0) [n = 88] | 2.10 | 208 | .037 | |
| >Moderate | 65.6 (10.5) [n = 65] | 65.0 (7.7) [n = 58] | 0.37 | 121 | .715 | |
| Nonadopters | Mild | 31.8 (5.4) [n = 120] | 33.8 (5.1) [n = 31] | 1.85 | 149 | .066 |
| Moderate | 46.8 (4.2) [n = 48] | 45.8 (4.4) [n = 18] | 0.90 | 64 | .372 | |
| >Moderate | 63.4 (9.1) [n = 14] | 67.6 (8.0) [n = 11] | 1.20 | 23 | .243 |
Note. SD = standard deviation; HL = hearing loss; SO = significant other; Significance level for multiple comparisons with Sidak–Bonferroni corrections is p-level < .009.
Statistical Analyses
To determine which factors were associated with hearing aid adoption and the decision to return hearing aids before the conclusion of a trial period, hierarchical binary logistic regressions were conducted using IBM® SPSS® Statistics software (version 24; Field, 2013). Hierarchical binary logistic regressions were conducted in order to statistically control for the possibly confounding influence of age and degree of hearing loss on hearing aid adoption. To assess overall hearing aid adoption for the full sample, participant age was entered in Block 1, and sex (female or male) and SO attendance status (Alone or SO) were entered as predictor variables. Hearing aid adoption decision (Yes or No) was entered as the dependent variable.
To determine whether SO attendance status is associated with hearing aid adoption rate above and beyond the predictive capacity of age and audiometric hearing loss, a second hierarchical binary logistic regression was conducted for the subsample for whom audiometric information was available. For this analysis, participant age and B4PTA were entered in Block 1, and SO attendance status (Alone or SO) was entered in Block 2 as predictor variables. To assess whether there is a differential impact of SO attendance on hearing aid adoption for different degrees of audiometric hearing loss, the B4PTA by SO attendance status interaction term was also entered in Block 2 as a predictor variable. Hearing aid adoption decision (Yes or No) was entered as the dependent variable. Post hoc analyses were conducted using Pearson chi-square testing.
To assess overall return rate, age, sex (female or male), and SO status (Alone or SO) were entered as predictor variables and the decision to return the hearing aid (Yes or No) was entered as the dependent variable. To assess return rate for the subsample for whom audiometric information was available, B4PTA and the B4PTA by SO attendance status interaction term were entered as predictor variables. Return rate was entered as the dependent variable.
For all regression analyses, variables needed to have a p value < .05 to remain in the model. There was no evidence of multicollinearity as all predictor variables in the study exhibited variation inflation factors < 2.0. Furthermore, there was no evidence of strong correlations between the predictor variables (all r’s < .30). To measure goodness-of-fit for each of the significant regression models, the Hosmer–Lemeshow goodness-of-fit statistic was calculated.
Results
The primary goal of the study was to determine whether there is an association between SO attendance at audiology appointments where decisions regarding hearing aid adoption are made. A significant association was observed (−2 log likelihood = 80796.43, χ2 = 2691.02, Nagelkerke R2 = .06, p < .001). Goodness-of-fit was deemed appropriate as the Hosmer–Lemeshow statistic was nonsignificant (p > .05). Overall, greater hearing aid adoption was observed when participants attend audiology appointments with an SO (Mean = 63.8%) than when attending audiology appointments alone (Mean = 50.6%; odds ratio (OR) = 1.56; 95% confidence interval (CI) = [1.51, 1.61]; p < .001). It was also observed that older individuals were significantly more likely to pursue amplification than younger individuals (OR = 1.03; 95% CI = [1.03, 1.03]; p < .001). Gender did not predict hearing aid adoption (p > .05).
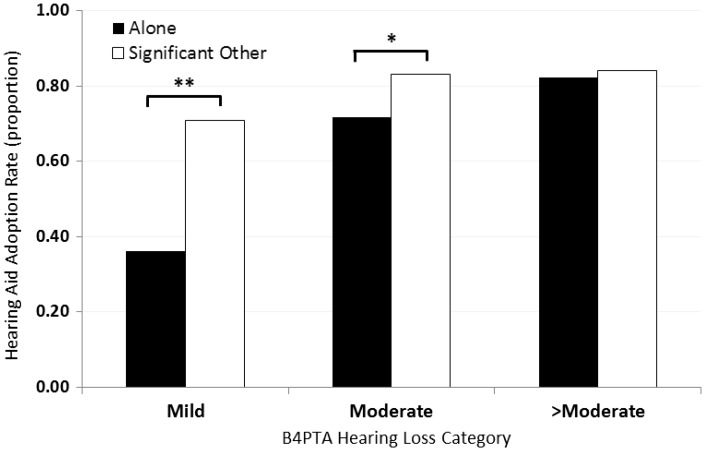
The second goal of the study was to determine whether the relationship between SO attendance at audiology appointments and hearing aid adoption is influenced by degree of audiometric hearing loss while also accounting for the influence of age on hearing aid adoption. A significant model was observed (−2 log likelihood = 808.30, χ2 = 109.38, Nagelkerke R2 = .20, p < .001). Goodness-of-fit was deemed appropriate as the Hosmer–Lemeshow statistic was nonsignificant (p > .05). Significant other attendance status (OR = 16.94; 95% CI = [4.45, 64.52]; p < .001), B4PTA (OR = 1.07; 95% CI = [1.05, 1.09]; p < .001), and age (OR = 1.02; 95% CI = [1.00, 1.03]; p < .05) were all significantly associated with hearing aid adoption whereby patients attending appointments with an SO compared to alone, individuals with worse compared with better audiometric hearing loss, and older relative to younger adults were more likely to pursue amplification. Of main interest, B4PTA by SO attendance status was significantly associated with greater hearing aid adoption (OR = 1.05; 95% CI = [1.02, 1.08]; p < .01). Post hoc testing revealed that although there was no association between SO attendance and hearing aid adoption for individuals with greater than moderate hearing losses, χ2(1, N = 148) = 0.08, p > .05, hearing aid adoption was significantly higher (15%) when individuals with moderate hearing losses attended appointments with an SO than when attending appointments alone, χ2(1, N = 276) = 4.55, p < .05. The association between SO attendance and hearing aid adoption was even more robust for individuals with mild hearing losses, with 96% greater hearing aid adoption observed when patients attended appointments with an SO than when attending appointments alone, χ2(1, N = 294) = 32.45, p < .001; see Figure 2).
Figure 2.
Hearing aid adoption rate for the Alone (black bars) and Significant Other (white bars) conditions depicted by B4PTA hearing loss category. *p < .05. **p < .001.
The third goal of the study was to determine whether there is a significant association between return rates and SO attendance at audiology appointments. Although a significant model was observed (−2 log likelihood = 39173.33, χ2 = 86.77, Nagelkerke R2 = .004, p < .001), the Hosmer–Lemeshow statistic was significant (p < .001), thus suggesting that overall goodness-of-fit of the model was not stable. Furthermore, it should be noted that the total variance accounted for by all three of the predictor variables combined (age, sex, and SO attendance status) in the final model accounted for less than half of 1% (pseudo r2 = .004). Hence, the analysis found little support for the hypothesis that return rates are influenced by attendance by SOs at audiology appointments. Finally, an analysis was conducted in order to assess whether the relationship between SO attendance and return rates is influenced by degree of audiometric hearing loss. A significant effect was not observed (p > .05).
Discussion
The objectives of the study were explorative in nature and designed to motivate additional research. The current study provides quantitative evidence of a significant relationship between attendance by SOs at audiology appointments and greater hearing aid adoption. For the sample as a whole, hearing aid adoption was 13 percentage points higher when individuals attended audiology appointments with an SO than alone. Notably, the association between SO attendance at audiology appointments and hearing aid uptake was very strongly hearing loss dependent. For individuals with mild hearing losses, hearing aid adoption increased by a remarkable 96% when patients attended the audiology appointment with an SO than alone. For individuals with moderate hearing losses, hearing aid adoption increased by 15 percentage points when individuals attended appointments with an SO than alone (see Figure 2). Not surprising, other factors associated with higher hearing aid adoption were age of the participant (older compared with younger adults were more likely to pursue amplification) and degree of hearing loss (individuals with worse compared with better hearing were more likely to pursue amplification). Importantly, the associations observed between SO attendance at audiology appointments and hearing aid adoption were established hierarchically after statistically controlling for the contributions of age, sex, and degree of audiometric hearing loss to hearing aid adoption.
Previous research has observed positive linkages between social support and audiologic outcomes (e.g., Hickson et al., 2014; Singh et al., 2015). Hence, it was hypothesized that SO attendance at audiology appointments, a measure possibly positively correlated with actual social support, would be negatively associated with the rate at which patients return their hearing aids before the conclusion of a hearing aid trial period. The study found little support for this hypothesis. Overall, there was less than a 3.1 percentage point difference in return rates when individuals attended audiology appointments with SOs than by themselves. Thus, while previous research has found good evidence to warrant the involvement of SOs in the audiologic rehabilitation process, and the current study found that SO involvement is positively associated with hearing aid adoption (particularly for individuals with mild hearing losses), the benefits of SO involvement at audiology appointments may not influence rejection of hearing aids during a trial period.
The associations observed in the study were established retrospectively using a nonexperimental study methodology. To establish a causal link between SO attendance at audiology appointments and hearing aid adoption, it would be necessary to conduct an experimental study whereby patients are randomly assigned to attend audiology appointments either with an SO or by themselves. The intent of the current research is to draw attention to the relationship between SOs and hearing aid adoption, particularly the previously unknown and robust association between SO attendance at audiology appointments and hearing aid adoption for individuals with mild hearing losses, a group historically identified as exhibiting low hearing aid adoption (Kochkin, 2012). Indeed, the current study observed that when patients with mild hearing losses attend audiology appointments without an SO, only 36% of the group decided to pursue hearing instruments as part of their rehabilitation plan.
Patient-centered care is defined by the U.S Institute of Medicine as the provision of care that is “respectful of and responsive to individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decision” (p. 6) and its implementation in health care represents a means by which to improve health outcomes (Institute of Medicine, 2001). A core component of patient-centered care is the invitation by health-care practitioners to include SOs in the care process (Gilligan & Weinstein, 2014; Grenness, Hickson, Laplante-Lévesque, & Davidson, 2014; Institute of Medicine, 2001). As such, it is noteworthy to consider the rate of SO attendance in a large population of patients attending audiology appointments. Overall, it was observed that in the current sample of 60,964 individuals in the study, 44.3% attended an appointment with an SO.
Possible Explanations: Association Between SO Attendance and Hearing Aid Adoption
In light of the observed correlations between SO involvement at audiology appointments and hearing aid adoption, it would be informative to consider how these two variables may be related. It should be noted that the following section should be considered speculative in nature.
Preexisting Differences Hypotheses
The first possibility is that there may be preexisting differences between patients who tend to bring SOs to audiology appointments and those who do not. For example, it could be that hearing-impaired individuals who are more motivated to pursue amplification may be more likely to also bring an SO to a hearing assessment. In other words, it could be that patients who bring SOs to appointments exhibit tendencies such as increased readiness for change or have health beliefs more associated with hearing aid adoption (Saunders, Frederick, Silverman, Nielsen, & Laplante-Lévesques, 2016) than those who do not bring SOs to appointments. Alternatively, there could be systematic differences in the personality profiles of those who bring SOs to appointments. Specifically, it could be that those who tend to adhere to the recommendations of clinicians (i.e., following advice to attend an audiology appointment with an SO and pursue hearing aids) have personality characteristics that differ from those individuals who tend to adhere less to the recommendations of clinicians. Cox et al. (2005) found that hearing-aid seekers possess personality traits that differ from nonseekers such as increased agreeableness. However, if there was more readiness for change or personalities consistent with hearing aid adoption in the group of patients in the SO than Alone condition, then it is reasonable to expect that one should also observe lower return rates in the SO than Alone group because of higher preappointment baseline motivations and predispositions to pursue amplification. In light of the similar rate of return between the SO and Alone condition, there is some evidence to suggest that explanations based on preexisting differences such as readiness for change, health beliefs, and personality may not fully account for the observed difference in hearing aid adoption between the SO and Alone condition.
Coercion Hypothesis
A second possible relationship between attendance at appointments by SOs and hearing aid adoption is that there is a causal link between the two variables such that attendance at appointments by SOs leads to increased hearing aid adoption. There are several potential mechanisms that could account for such a relationship. Rather than providing social support, it could be that SOs attempt to influence in-clinic decision making by exerting unwanted social pressure to pursue hearing rehabilitation (Duijvestijn et al., 2003; Preminger & Montano, 2014). From this perspective, coercion may account for the increased hearing aid uptake observed in the SO than Alone condition.
Preadoption Decision Uncertainty Hypothesis
A third possibility is that the presence of SOs at audiology appointments moderates in-clinic decision uncertainty that arises before the purchase of hearing aids. To minimize unease associated with the purchase, individuals consult with others before making a rehabilitation decision. Such uncertainty may arise for several reasons. For example, hearing aids are significant financial investments and the patient may be unsure whether the potential benefits of the devices justify the cost. From this perspective, the SO provides the patient with momentary reassurance that the value of the hearing aids outweigh the financial cost and that they are worth the investment. Even when cost is not a concern, it could be that SOs increase hearing aid adoption by reinforcing motivation (Ridgway, Hickson, & Lind, 2015) and by addressing any lingering doubts held by the patient (e.g., concerns regarding the color or appearance of the devices).
As individuals weigh the relative costs and benefits of hearing aid ownership, there is likely greater uncertainty regarding hearing aid adoption for those with milder than more severe audiometric losses. If attendance by SOs at audiology appointments moderates decision uncertainty associated with hearing aid adoption, one might expect that the association between SO attendance and hearing aid adoption would be weakest for those with the most severe audiometric losses and most robust for those with mild hearing losses. Such a pattern was observed in the current study (see Figure 2).
It should be noted that the aforementioned hypotheses describing the relationship between SO attendance and hearing aid adoption are not mutually exclusive. In such a large data set, it is very possible that one of the hypotheses better describes some of the subject pairs, while other subject pairs are better described by a different hypothesis. The mechanistic underpinnings of hearing aid adoption are likely multifactorial.
Study Limitations, Strengths, and Future Directions
There are several notable limitations to the study and with retrospective designs more generally. Foremost among them, individuals were not randomly assigned to the SO and Alone conditions. Instead, patients self-selected whether to attend the appointment alone or with an SO or may not have had an SO who could attend the appointment. As described earlier, there are several potential explanations for the association between SO attendance and hearing aid adoption. One potential future direction for work in this area would be to recruit patients willing to bring an SO to their audiology appointments and to randomly assign participants to attend appointments either alone or with an SO. A second limitation is that the nature of the relationship between the patient and the SO was not recorded. It may be informative to know whether hearing aid adoption is influenced by this relationship (i.e., romantic partners, parent–child, etc.). Another limitation is that the study did not assess the degree of participation by the SO during appointments. Singh et al. (2016) note that active participation, rather than passive attendance, by SOs at appointments may be necessary to promote positive audiologic outcomes.
One of the strengths of the study design is the size of the sample under investigation. All other things being equal, as sample size increases, there are two important benefits. First, there is more power to detect relationships, particularly those with weak effect sizes, among variables. Second, larger sample sizes yield more accurate sample estimates thus providing more reliable data.
Consequences for Rehabilitation
Future research should attempt to better understand if and how pre-adoption decision uncertainty, inclusion of SOs in the audiologic care process, readiness for change, personality, coercion, and other factors contribute to hearing aid adoption. Importantly, the consequences for rehabilitation are markedly different depending on which mechanism or mechanisms account for the relationship between attendance at appointments by SOs and hearing aid uptake. Interventions intended to improve hearing aid adoption rates will likely be easier to design and more amenable to implementation if SOs increase hearing aid adoption by minimizing preadoption decision uncertainty. In contrast, it is probably more challenging to improve hearing aid adoption rates based on interventions targeting readiness for change or personality, as such factors are more resistant to change.
The findings of the study support the broader consensus that more positive audiologic outcomes are achieved when SOs are actively involved during the audiologic care process (Singh et al., 2016). However, it should be mentioned that while it may be tempting to insist that patients always attend audiology appointments with SOs, for some individuals, attendance by SOs at audiology appointments may be inappropriate or impossible. It should also be noted that hearing aids are not always an appropriate component of a rehabilitation plan for individuals with hearing loss. Accordingly, clinicians should be attuned and responsive to the individual needs of the patient and suggest rehabilitation options that respect their preferences.
Conclusion
This study attempted to analyze data collected in daily clinical practice from thousands of patients as a means to better understand factors affecting help seeking and adoption of hearing instruments. This retrospective study provides quantitative evidence in a large-scale sample that hearing aid adoption is positively associated with the presence of SOs at appointments where patients make decisions about whether to pursue hearing aids. Furthermore, the association between SO attendance and hearing aid adoption was particularly robust for those with mild losses, with 96% greater hearing aid adoption observed in the SO than Alone condition. It was also observed that the study did not find a reliable association between the presence of SOs at hearing assessments and hearing aid return rates. In light of the lack of random assignment to condition in the study, future research should establish whether there is a causal relationship between attendance at appointments by SOs and hearing aid adoption and should attempt to better understand mechanisms that contribute to hearing aid adoption. Several possible mechanisms describing the association between SO attendance and hearing aid adoption were provided. Given the magnitude of the relationship between hearing aid uptake and attendance of SOs at audiology appointments, in those instances where hearing aids are recommended as part of the treatment to address hearing impairment, clinicians should consider the appropriateness of encouraging SOs to participate in the audiologic rehabilitation process.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- Abrams H. B., Kihm J. (2015) An introduction to MarkeTrak IX: A new baseline for the hearing aid market. Hearing Review 22: 16. [Google Scholar]
- Bainbridge K. E., Ramachandran V. (2014) Hearing aid use among older U.S. adults; the national health and nutrition examination survey, 2005–2006 and 2009–2010. Ear and Hearing 35: 289–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson A. J. (2005) “What brings you here today?” The role of self-assessment in help-seeking for age-related hearing loss. Journal of Aging Studies 19: 185–200. [Google Scholar]
- Chisolm T. H., Johnson C. E., Danhauer J. L., Portz L. J., Abrams H. B., Lesner S., Newman C. W. (2007) A systematic review of health-related quality of life and hearing aids: Final report of the American academy of audiology task force on the health-related quality of life benefits of amplification in adults. Journal of the American Academy of Audiology 18: 151–183. [DOI] [PubMed] [Google Scholar]
- Cox R., Alexander G., Gray G. (2005) Who wants a hearing aid? Personality profiles of hearing aid seekers. Ear and Hearing 26: 12–26. [DOI] [PubMed] [Google Scholar]
- Dalton D. S., Cruickshanks K. J., Klein B. E., Klein R., Wiley T. L., Nondahl D. M. (2003) The impact of hearing loss on quality of life in older adults. Gerontologist 43: 661–668. [DOI] [PubMed] [Google Scholar]
- Duijvestijn J., Anteunis L., Hoek C., Van Den Brink R. H., Chenault M. N., Manni J. J. (2003) Help-seeking behavior of hearing-impaired persons aged ≥ 55 years: Effect of complaints, significant others and hearing aid image. Acta Oto-laryngologica 123: 846–850. [DOI] [PubMed] [Google Scholar]
- Field A. P. (2013) Discovering statistics using IBM SPSS Statistics, 4th ed London, England: Sage. [Google Scholar]
- Frankel B., Turner R. (1983) Psychological adjustment in chronic disability: The role of social support in the case of the hearing impaired. Canadian Journal of Sociology 8: 273–291. [Google Scholar]
- Furse D. H., Punj G. N., Stewart D. W. (1984) A typology of individual search strategies among purchasers of new automobiles. Journal of Consumer Research 10: 417–431. [Google Scholar]
- Garstecki D. C., Erler S. F. (1998) Hearing loss, control, and demographic factors influencing hearing aid use among older adults. Journal of Speech, Language, and Hearing Research: JSLHR 41: 527–537. [DOI] [PubMed] [Google Scholar]
- Gilligan J., Weinstein B. E. (2014) Health literacy and patient-centered care in audiology—Implications for adult aural rehabilitation. Journal of Communication Disorders, Deaf Studies & Hearing Aids 2: 110. [Google Scholar]
- Gonsalves C., Pichora-Fuller M. K. (2008) The effect of hearing loss and hearing aids on the use of information and communication technologies by community-living older adults. Canadian Journal on Aging 27: 145–157. [DOI] [PubMed] [Google Scholar]
- Grenness C., Hickson L., Laplante-Lévesque A., Davidson B. (2014) Patient-centred care: A review for rehabilitative audiologists. International Journal of Audiology 53(Suppl. 1): S60–S67. [DOI] [PubMed] [Google Scholar]
- Helvik A.-S., Wennberg S., Jacobsen G., Hallberg L. (2008) Why do some individuals with objectively verified hearing loss reject hearing aids? Audiological Medicine 6: 141–148. [Google Scholar]
- Hickson L., Meyer C., Lovelock K., Lampert M., Khan A. (2014) Factors associated with success with hearing aids in older adults. International Journal of Audiology 53: S18–S27. [DOI] [PubMed] [Google Scholar]
- Humes L. E., Wilson D. L., Humes A. C. (2003) Examination of differences between successful and unsuccessful elderly hearing aid candidates matched for age, hearing loss and gender. International Journal of Audiology 42(7): 432–441. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (U.S.) Committee on Quality of Health Care in America (2001) Crossing the quality chasm: A new health system for the 21st century, Washington, DC: National Academy Press. [Google Scholar]
- Kiecker P., Hartman C. L. (1993) Purchase pal use: Why buyers choose to shop with others. In: Varadarajan R., Bernard Jaworski B. (eds) Proceedings of the AMA Winter Educators’ Conference, Chicago, IL: American Marketing Association, pp. 378–384. [Google Scholar]
- Kiecker P., Hartman C. L. (1994) Predicting buyers’ selection of interpersonal sources: The role of strong tie and weak ties. In: Allen C. T., John D. R. (eds) Advances in consumer research vol. 21, Provo, UT: Association for Consumer Research, pp. 464–469. [Google Scholar]
- Kochkin S. (2007) MarkeTrak VII: Obstacles to adult non-user adoption of hearing aids. The Hearing Journal 60: 27–43. [Google Scholar]
- Kochkin S. (2012) MarkeTrak VIII: The key influencing factors in hearing aid purchase intent. Hearing Review 19(3): 12–25. [Google Scholar]
- Knudsen L. V., Oberg M., Nielsen C., Naylor G., Kramer S. E. (2010) Factors influencing help seeking, hearing aid uptake, hearing aid use and satisfaction with hearing aids: A review of the literature. Trends in Amplification 14(3): 127–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin F. R. (2011) Hearing loss and cognition among older adults in the United States. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 66: 1131–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockey K., Jennings M., Shaw L. (2010) Exploring hearing aid use in older women through narratives. International Journal of Audiology 49: 542–549. [DOI] [PubMed] [Google Scholar]
- Mahoney C., Stephens S., Cadge B. (1996) Who prompts patients to consult about hearing loss? British Journal of Audiology 30: 153–158. [DOI] [PubMed] [Google Scholar]
- Manchaiah, V. K. C., Stephens, D., & Lunner, T. (2013). Communication partners' journey through their partner's hearing impairment. International Journal of Otolaryngology 11. Article ID 707910. [DOI] [PMC free article] [PubMed]
- Meister H., Walger M., Brehmer D., von Wedel U. C., von Wedel H. (2008) The relationship between pre-fitting expectations and willingness to use hearing aids. International Journal of Audiology 47: 153–159. [DOI] [PubMed] [Google Scholar]
- Meyer C., Hickson L. (2012) What factors influence help-seeking for hearing impairment and hearing aid adoption in older adults? International Journal of Audiology 51: 66–74. [DOI] [PubMed] [Google Scholar]
- Meyer C., Hickson L., Lovelock K., Lampert M., Kahn A. (2014) An investigation of the factors that influence help-seeking for hearing impairment in older adults. International Journal of Audiology 53(S1): S3–S17. [DOI] [PubMed] [Google Scholar]
- Palmer C. V., Solodar H. S., Hurley W. R., Byrne D. C., Williams K. O. (2009) Self-perception of hearing ability as a strong predictor of hearing aid purchase. Journal of the American Academy of Audiology 20: 341–347. [DOI] [PubMed] [Google Scholar]
- Popelka M. M., Cruickshanks K. J., Wiley T. L., Tweed T. S., Klein B. E., Klein R. (1998) Low prevalence of hearing aid use among older adults with hearing loss: The epidemiology of hearing loss study. Journal of the American Geriatrics Society 46: 1075–1078. [DOI] [PubMed] [Google Scholar]
- Preminger J. E. (2003) Should significant others be encouraged to join adult group audiologic rehabilitation classes? Journal of the American Academy of Audiology 14: 545–555. [DOI] [PubMed] [Google Scholar]
- Preminger J. E., Montano J. J. (2014) Incorporating communication partners into the AR process. In: Montano J., Spitzer J. (eds) Adult audiologic rehabilitation, 2nd ed San Diego, CA: Plural Publishing, pp. 329–348. [Google Scholar]
- Ridgway J., Hickson L., Lind C. (2015) Autonomous motivation is associated with hearing aid adoption. International Journal of Audiology 54: 476–484. [DOI] [PubMed] [Google Scholar]
- Saunders G. H., Frederick M. T., Silverman S. C., Nielsen C., Laplante-Lévesques A. (2016) Description of adults seeking hearing help for the first time according to two health behavior change approaches: Transtheoretical mode (stages of change) and health belief model. Ear and Hearing 37: 324–333. [DOI] [PubMed] [Google Scholar]
- Šidák Z. K. (1967) Rectangular confidence regions for the means of multivariate normal distributions. Journal of the American Statistical Association 62: 626–633. [Google Scholar]
- Singh G., Hickson L., English K., Scherpiet S., Lemke U., Timmer B., Launer S. (2016) Family-centered adult audiologic care: A Phonak position statement. Hearing Review 23(4): 16. [Google Scholar]
- Singh G., Lau S.-T., Pichora-Fuller M. K. (2015) Social support and hearing aid satisfaction. Ear and Hearing 36: 664–676. [DOI] [PubMed] [Google Scholar]
- Urbany J. E., Dickson P. R., Wilkie W. L. (1989) Buyer uncertainty and information search. Journal of Consumer Research 16: 208–215. [Google Scholar]
- van den Brink R. H., Wit H. P., Kempen G. I., van Heuvelen M. J. (1996) Attitude and help-seeking for hearing impairment. British Journal of Audiology 30: 313–324. [DOI] [PubMed] [Google Scholar]
- Wallhagen M. I. (2010) The stigma of hearing loss. The Gerontologist 50: 66–75. [DOI] [PMC free article] [PubMed] [Google Scholar]