Abstract
Objective
To assess the correlation of psychosocial resiliency factors (mindfulness and coping) with symptoms of posttraumatic stress (PTS), anxiety, and depression in patients recently admitted to the Neuroscience Intensive Care Unit (Neuro-ICU) and their primary informal caregivers.
Design
A descriptive, cross-sectional correlational study.
Setting
Neuro-ICU in a major medical center.
Participants
78 dyads of patients (total N= 81) and their primary caregivers (total N= 92) from June to December 2015. Study enrollment occurred within the first 2 weeks of patient admission to the Neuro-ICU.
Intervention
None
Measurements and Main Results
Dyads completed self-report measures of mindfulness (CAMS-R), coping (MOCS-A), PTS (PCL-S), anxiety (HADS), and depression (HADS). Rates of clinically significant PTS, anxiety, and depressive symptoms were high and comparable between patient and caregiver samples. Own psychological resilience factors and psychiatric symptoms were strongly correlated for both patients and caregivers. Depressive symptoms were interdependent between patients and their caregivers, and one’s own mindfulness was independently related to one’s partner’s depressive symptoms.
Conclusions
Rates of clinically significant psychiatric symptoms were high, equally prevalent in patients and caregivers, and interdependent between patients and their caregivers. For both patients and caregivers, psychological resiliency factors were associated with both self and partner psychiatric symptoms. Findings suggest that attending to the psychiatric health of both patients and caregivers in the Neuro-ICU is a priority, and that patients and their caregivers must be considered together in a system to fully address either individual’s psychiatric symptoms.
Keywords: Neuroscience ICU, Posttraumatic stress, depression, actor-partner interdependence model, mindfulness, coping, informal caregiver
INTRODUCTION
Admission to the Neuroscience Intensive Care Unit (Neuro-ICU) is traumatic for patients and their families and close friends, often leading to chronic psychological morbidity. Among both patients and informal caregivers respectively, substantial rates of clinically significant posttraumatic stress disorder (PTSD; 30%; 20%) (1, 2), anxiety (20-27%; 18-25%) (3-6), and depression (30-50%; 34-52%) (5-9) have been documented. These psychiatric symptoms largely do not improve with time, with the majority of distressed patients and caregivers continuing to meet diagnostic criteria months or years later (10, 11). Psychiatric symptoms interfere with patients’ ability to adhere to treatment regimens (12), leading to poorer recovery (10, 12, 13) and higher all-cause mortality (10, 14). Caregivers’ psychiatric symptoms increase their own risk for disease (15-17) and mortality (18).
Emerging literature, primarily cross-sectional, demonstrates that patient and caregiver psychosocial factors influence each other and shape each person’s adjustment to illness, including outcomes of PTSD, anxiety, and depression (13, 19). Poor patient mental health and physical functioning translate into greater caregiving burden (5), which negatively impacts caregivers’ mental health (13, 20). In turn, caregivers’ poorer mental health increases risk for providing poor quality care to the patients (7, 21), which has been linked to greater depression among patients (22, 23). Given the evidence of interdependence between patient and caregiver psychiatric health, it is important to consider the context of the dyad to fully capture an individual’s level of mental health risk following the stress of Neuro-ICU hospitalization.
Resiliency, defined as the ability to bounce back from stressful and adverse situations, has been associated with positive health outcomes across a variety of populations (24-26). Mindfulness, the ability to remain attentive to the present moment without becoming overwhelmed, is one skill that enhances resilience to stressors including traumatic experiences. Mindfulness allows non-judgmental acceptance of all experiences even when these are painful, while fostering a sense of calm and the ability to respond intentionally (27). Resiliency also depends on the breadth and accessibility of one’s coping arsenal, or one’s bank of behavioral (e.g., use of social support, employment of relaxation techniques), cognitive (e.g., adaptive thinking), and emotional (e.g., ability to regulate emotions) strategies to manage stress (28). Both mindfulness (27, 29) and coping arsenal (30) have been consistently associated with mental and physical health benefits. Among patients with acute neurological injuries specifically, depression and anxiety have been associated with emotional avoidance and poor coping strategies (31, 32). Among their caregivers, greater psychological distress has been associated with lack of acceptance and poor coping behaviors (33, 34). Literature from other medical illnesses shows that psychological resilience following illness is significantly related between patients and their families (35, 36). The synergistic relations between patients’ and caregivers’ psychiatric symptoms and psychological resilience factors, however, have yet to be examined following admission to the Neuro-ICU.
This study aims to fill this gap in the literature and provide a more comprehensive picture of patients’ and their informal caregivers’ psychiatric risk following admission to the Neuro-ICU. The purposes of this cross-sectional study were to: 1) estimate rates of clinically significant psychiatric symptoms (i.e., PTSD, anxiety, and depression) in dyads of patients recently (within 2 weeks) admitted to the Neuro-ICU and their primary informal caregivers, and 2) examine relations of dyad members’ psychological resilience factors (i.e., mindfulness and coping) with their own and their partners’ psychiatric symptoms. We hypothesize that greater patient and caregiver mindfulness and coping will be associated with lower symptoms of PTSD, anxiety, and depression among dyads.
MATERIALS AND METHODS
Sample and Setting
The institutional review board approved this study, which took place in the Neuro-ICU at a major medical center in Boston, Massachusetts between June and December 2015. The study inclusion criteria for patients were: 1) being 18 years of age or older; 2) English fluency and literacy; and 3) admission to the Neuro-ICU within the past 2 weeks. All patients were first cleared for participation in the consent process by the medical team. Patients who, based on the clinical judgment of the medical team or unable to consent due to any medical (e.g., critical illness included anticipated death within the ICU), or cognitive factors (e.g., chronic aphasia) were not referred to the study. Patient with transient aphasia or delirium who were asymptomatic at the time of consent were allowed to participate. The decision to use clinical judgment of the medical team rather than the use of specific questionnaires or cognitive test was predicated on using a criterion that is feasible, efficient, does not add burden to study participants, and can be easily employed in a planned subsequent intervention study. The inclusion criteria for the informal caregiver were: 1) being 18 years of age or older; 2) English fluency and literacy; and 3) identification as an eligible patient’s primary caregiver (i.e., family member or close friend providing the majority of unpaid emotional or instrumental care for the patient).
Design
This study was a descriptive, cross-sectional study of rates of clinically significant PTS, anxiety, and depressive symptoms in Neuro-ICU patients and their caregivers and the correlations of these symptoms with mindfulness and coping. A research assistant (RA) rounded in the Neuro-ICU 2 days per week and identified dyads of patients and their caregivers. The RA approached eligible and medically cleared patients and their primary caregiver to discuss the study. Enrollment, inclusionary criteria review, and questionnaire completion occurred at the bedside (all Neuro-ICU rooms were single-patient rooms). When a patient met the eligibility criteria for the study but the caregiver was not present at the patient’s bedside, the RA explained the study to the caregiver at a different time, either in the patient’s room or another private location. If the patient was unable to complete the questionnaire at the time of enrollment, the RA followed the progress of the patient and re-approached the patient when appropriate. In some cases (N= 6), the patient was never able to complete the questionnaire, so only the caregiver provided data.
Patients and caregivers completed questionnaires within 2 weeks of the patients’ admission to the Neuro-ICU. Both patients and caregivers completed a demographic form and psychosocial questionnaires. We also collected data from electronic medical chart review on the reason for admission to the Neuro-ICU, discharge status, and whether the patient was intubated during their hospital admission.
Measurement
Demographic form
Patient and caregiver characteristics were assessed via self-report and included age, gender, race/ethnicity, education, and marital status.
Post-Traumatic Checklist–Specific Stressor (PCL-S)
Symptoms of post-traumatic stress (PTS) were measured with the PCL-S (37). The 17 items are scored using a 5-point Likert scale with responses ranging from 1 (“Not at all”) to 5 (“Extremely”). A total symptom severity score is computed by summing the items. Scores range from 17 to 85, with higher scores indicating higher symptom severity. Clinically significant PTS symptoms suggestive of PTSD are estimated based on an algorithm consistent with Diagnostic and Statistical Manual of Mental Disorders-IV TR (38) criteria.
Hospital Anxiety and Depression Scale (HADS)
Symptoms of anxiety and depression were measured with the HADS (39). The 14 items are scored using a 4-point Likert scale with responses ranging from 0 (“Not at all” or “Very rarely”) to 3 (“All of the time” or “Very often”). Separate scores for anxiety (7 items) and depression (7 items) are computed by summing the respective items. Scores range from 0 to 21 for each subscale, with higher scores indicating higher symptom severity. Scores of 8 or greater for a subscale are suggestive of clinically significant anxiety or depressive symptoms (40).
Cognitive and Affective Mindfulness Scale-Revised (CAMS-R)
Everyday mindfulness, or the degree to which participants experience their thoughts and feelings in the present moment, was measured with the CAMS-R (41). The 12 items are scored using a 4-point Likert scale with responses ranging from 1 (“Rarely/Not at all”) to 4 (“Almost always”). A total mindfulness score is computed by summing the items. Scores range from 12 to 48, with higher scores reflecting greater mindfulness.
Measure of Coping Status-A (MOCS-A)
Coping styles, including relaxation, awareness of stress, assertiveness, and disputing maladaptive thoughts, were measured using the MOCS-A (42). The 13 items are scored using a 5-point Likert scale with responses ranging from 0 (“I cannot do this at all”) to 4 (“I can do this extremely well”). The sum of all of the items composes an overall coping skill score. Scores range from 0 to 52, with higher scores indicating more effective coping skills.
Statistical Analyses
Participant characteristics were summarized by measures of central tendency (e.g., proportion, mean) as appropriate. Univariate relations between patient and caregiver variables were tested using Pearson’s r and paired sample t tests. Small, medium, and large effect sizes are distinguished by Pearson’s r values of 0.10, 0.30, and 0.50 and Cohen’s d values of 0.20, 0.50, and 0.80, respectively (43). Categorical variables were compared using chi square analyses. An alpha level of .05 and two-tailed tests were used to determine statistical significance in all analyses. These analyses were completed using SPSS version 20 (IBM Corp, 2011).
Dyadic modeling called actor-partner interdependence modeling (APIM) (44, 45) was used to determine the relations of patients’ and caregivers’ mindfulness and coping with their own and their partners’ symptoms of PTS, anxiety, and depression (see Figure 1). In the APIM for this study, the “actor effect” is the relation of a person’s psychological resiliency factors (i.e., mindfulness and coping) with his/her own symptoms of PTS, anxiety, and depression. The “partner effect” is the relation of a person’s psychological resiliency factors with his/her partner’s symptoms of PTS, anxiety, and depression. Variance in dyad members’ predictor variables and residual variance in their outcome variables is allowed to correlate to account for the interdependence of dyad members’ data. Effects were considered equal when chi square difference tests revealed no significant difference in model fit between models with and without effects constrained equal. Multivariate dyadic analyses were completed using MPlus version 7 (Muthén & Muthén, 1998-2012).
Figure 1. APIM for Psychiatric Symptom Outcomes.
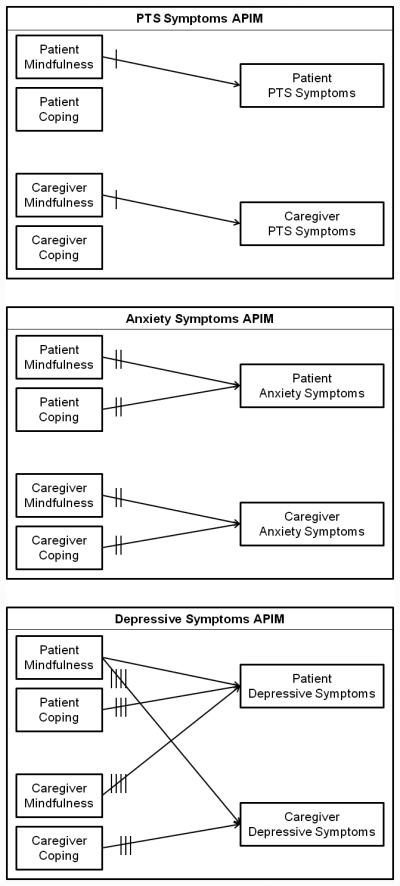
*Note: only significant paths shown. Hash marks within model indicate which paths are equivalent.
RESULTS
Characteristics of Patients and Caregivers
Of 121 eligible patients who were approached, 91 patients (75%) and 102 of their primary caregivers consented to participate (84%). Of those consented, 81 patients (89%) and 92 caregivers (90%) completed questionnaires. This represents 78 full patient-caregiver dyads, with 3 patients participating without caregivers and 14 caregivers participating without patients. Missing data exists where participants were unable to complete questionnaires, were lost to follow up after consent, or exercised their right to decline to answer questionnaires.
We summarize demographic and medical characteristics of the sample in Table 1. Patients and caregivers did not differ in terms of demographics. Overall, participants were middle aged, approximately evenly split between males and females, and a majority were non-Hispanic white, highly educated, and married. The most prevalent diagnoses causing patients to be hospitalized were stroke/hemorrhage (40%) and tumors (28%). Approximately two-thirds of the patients were discharged to home. Most patients (74%) were intubated during the course of their treatment. The majority of primary caregivers were their patients’ romantic partner (61%).
Table 1.
Demographic and Medical Characteristics of Neuro-ICU Patients (N= 81) and their Family Caregivers (N= 92)
| Patients |
Caregivers |
|||
|---|---|---|---|---|
| N (%) | N (%) | t or χ2 | df | |
| Age (M [SD]) | 51.82 (16.57) | 52.08 (14.42) | −0.73 | 75 |
| Gender (male) | 41 (51%) | 36 (40%) | 2.12 | 1 |
| Race/Ethnicity (non-Hispanic white) | 64 (79%) | 77 (84%) | 0.63 | 1 |
| Education (some college or more) | 60 (74%) | 73 (79%) | 0.67 | 1 |
| Marital status (married/cohabitating) | 56 (69%) | 73 (80%) | 2.81 | 1 |
| Diagnosis | ||||
| Cerebrovascular | ||||
| Stroke/Hemorrhage | 32 (40%) | – | – | – |
| Brain aneurysm | 3 (4%) | – | – | – |
| Structural | ||||
| Tumor | 23 (28%) | – | – | – |
| Lesion/Brain mass | 13 (16%) | – | – | – |
| Other | ||||
| Traumatic brain injury | 5 (6%) | – | – | – |
| Seizures | 3 (4%) | – | – | – |
| Other/More than 1 diagnosis | 2 (2%) | – | – | – |
| Discharge status | ||||
| Discharge to home | 55 (68%) | |||
| Discharge to rehabilitation facility | 26 (32%) | |||
| Intubated (yes) | 60 (74%) | – | – | – |
| Relationship to patient | ||||
| Spouse/partner | – | 56 (61%) | – | – |
| Parent | – | 17 (18%) | – | – |
| Child | – | 15 (16%) | – | – |
| Sibling | – | 4 (4%) | – | – |
Note. All p-values for t- and χ2 tests > .05
We summarize participants’ continuous levels of psychological resilience and psychiatric symptoms in Table 2. Patients and caregivers did not differ in terms of psychological resilience factors or level of psychiatric symptoms. The only exception was that patients reported significantly greater PTS symptoms than their caregivers. Psychiatric symptoms also did not differ by any demographic or medical characteristic (ps> .07), with the exception that unmarried participants reported greater PTS symptoms (M= 35.97) than married participants (M= 28.67, t(154)= 2.98, p= .003, Cohen’s d= 0.48). No significant differences in PTS model effects or fit were observed when controlling for marital status (data not shown); therefore, the PTS model is reported without controlling for marital status.
Table 2.
Clinical Characteristics of Neuro-ICU Patients and their Family Caregivers
| Patients |
Caregivers |
Comparison |
||||||
|---|---|---|---|---|---|---|---|---|
| Continuous Scores | M | SD | Range | M | SD | Range | t | df |
| Mindfulness | 33.93 | 5.49 | 19 – 45 | 33.89 | 5.16 | 20 – 43 | −0.05 | 63 |
| Coping | 32.75 | 9.27 | 11 – 52 | 32.77 | 9.03 | 14 – 51 | 0.23 | 64 |
| PTS Symptoms | 32.05 | 14.68 | 17 – 81 | 28.89 | 12.24 | 17 – 70 | 2.00* | 67 |
| Anxiety Symptoms | 7.20 | 4.26 | 0 – 21 | 7.21 | 4.17 | 0 – 16 | 0.56 | 68 |
| Depressive Symptoms | 5.24 | 3.72 | 0 – 18 | 5.57 | 2.86 | 1 – 15 | 0.31 | 69 |
|
| ||||||||
| % Meeting Clinical Cut-Off | N | % | – | N | % | – | χ2 | df |
|
| ||||||||
| PTS Symptoms | 15 | 21% | 14 | 17% | 0.39 | 1 | ||
| Anxiety Symptoms | 32 | 43% | 40 | 46% | 0.18 | 1 | ||
| Depressive Symptoms | 18 | 24% | 21 | 24% | 0 | 1 | ||
p < .05
Note. Mindfulness = CAMS-R; Coping = MOCS-A; Post-traumatic stress (PTS) symptoms = PCL-S; Anxiety symptoms = HADS-A; Depressive symptoms = HADS-D; Meeting clinical cut-off: symptomatic responses on 1 cluster B, 3 cluster C, and 2 cluster D items (PCL-S), ≥ 8 (HADS-A and HADS-D)
Clinically Significant Psychiatric Symptoms among Patients and Caregivers
We summarize proportions of participants reporting clinically significant psychiatric symptoms in Table 2. Rates of clinically significant PTS, anxiety, and depressive symptoms were high, comparable to prior literature, and did not differ between patient and caregiver samples.
Relations of Own Psychological Resilience Factors with Own Psychiatric Symptoms
Bivariate analyses
We summarize bivariate relations between own psychological resilience factors and psychiatric symptoms in Table 3. For both patients and caregivers, all psychological resilience factors and psychiatric symptoms were related within individuals, with medium to large effects.
Table 3.
Bivariate Correlations of Psychological Resilience and Psychiatric Symptoms for Neuro-ICU Patients and their Family Caregivers
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| 1. Patient Mindfulness | 1 | ||||||||
| 2. Patient Coping | .48*** | 1 | |||||||
| 3. Patient PTS Symptoms | −.54*** | −.34** | 1 | ||||||
| 4. Patient Anxiety Symptoms | −.55*** | −.32** | .68*** | 1 | |||||
| 5. Patient Depressive Symptoms | −.48*** | −.51*** | .52*** | .41*** | 1 | ||||
| 6. Caregiver Mindfulness | .06 | .15 | −.05 | −.07 | −.10 | 1 | |||
| 7. Caregiver Coping | .10 | .18 | −.07 | −.01 | −.11 | .73*** | 1 | ||
| 8. Caregiver PTS Symptoms | −.02 | −.04 | .18 | −.002 | .04 | −.54*** | −.52*** | 1 | |
| 9. Caregiver Anxiety Symptoms | −.21 | −.11 | .24 | .06 | .23 | −.47*** | −.58*** | .70*** | 1 |
| 10. Caregiver Depressive Symptoms | −.28* | −.08 | .16 | .10 | .30* | −.42*** | −.48*** | .48*** | .63*** |
p < .05
p < .01
p < .001
Note. Mindfulness = CAMS-R; Coping = MOCS-A; Post-traumatic stress (PTS) symptoms = PCL-S; Anxiety symptoms = HADS-A; Depressive symptoms = HADS-D.
Multivariate dyadic analyses: Actor effects
We summarize results from the three multivariate APIM (one model for each psychiatric symptom outcome) in Table 4 and Figure 1. All effects, unless otherwise noted, were equal for patients’ resilience factors to their own psychiatric symptoms and caregivers’ resilience to own psychiatric symptoms. For PTS symptoms, greater mindfulness was related to lower PTS symptoms, but coping was unrelated to PTS symptoms. For anxiety symptoms, both greater mindfulness and greater coping were related to lower anxiety symptoms. For depressive symptoms, for patients but not caregivers, greater mindfulness was related to lower depressive symptoms. However, greater coping was related to lower depressive symptoms (for both patients and caregivers).
Table 4.
Actor-Partner Interdependence Models Testing Effects of Own Psychological Resilience Factors on Own and Partner Psychiatric Symptoms
| Patients |
Caregivers |
|||||||
|---|---|---|---|---|---|---|---|---|
| Unstandardized |
Standardized |
Unstandardized |
Standardized |
|||||
| B | [95% CI] | p | β | B | [95% CI] | p | β | |
| PTS Symptoms | ||||||||
| Actor Effects | ||||||||
| Mindfulness | −1.05 | [−1.49, −0.61] | <.001 | −.41 | −1.05 | [−1.49, −0.67] | <.001 | −.48 |
| Coping | −0.22 | [−0.48, 0.05] | .11 | −.14 | −0.22 | [−0.48, 0.05] | .11 | −.17 |
| Partner Effects | ||||||||
| Mindfulness | 0.03 | [−0.11, 0.17] | .68 | .01 | 0.03 | [−0.11, 0.17] | .65 | .01 |
| Coping | 0.03 | [−0.11, 0.17] | .68 | .02 | 0.03 | [−0.11, 0.17] | .65 | .02 |
|
| ||||||||
| Anxiety Symptoms | ||||||||
| Actor Effects | ||||||||
| Mindfulness | −0.12 | [−0.16, −0.09] | <.001 | −.21 | −0.12 | [−0.16, −0.09] | <.001 | −.22 |
| Coping | −0.12 | [−0.16, −0.09] | <.001 | −.36 | −0.12 | [−0.16, −0.09] | <.001 | −.38 |
| Partner Effects | ||||||||
| Mindfulness | −0.01 | [−0.04, 0.03] | .76 | −.01 | −0.01 | [−0.04, 0.03] | .76 | −.01 |
| Coping | −0.01 | [−0.04, 0.03] | .76 | −.02 | −0.01 | [−0.04, 0.03] | .76 | −.02 |
|
| ||||||||
| Depressive Symptoms | ||||||||
| Actor Effects | ||||||||
| Mindfulness | −0.17 | [−0.27, −0.07] | .001 | −.38 | −0.07 | [−0.15, 0.02] | .11 | −.23 |
| Coping | −0.05 | [−0.09, −0.01] | .02 | −.19 | −0.05 | [−0.09, −0.01] | .02 | −.31 |
| Partner Effects | ||||||||
| Mindfulness | −0.08 | [−0.13, −0.02] | .01 | −.17 | −0.08 | [−0.13, −0.02] | .01 | −.27 |
| Coping | 0.03 | [−0.01, 0.06] | .14 | .10 | 0.03 | [−0.01, 0.06] | .14 | .16 |
Note. Bolding identifies significant (p< .05) paths depicted in figures; PTS model reported without covariate of marital status.
Relations of Own Psychological Resilience Factors with Partner Psychiatric Symptoms
Bivariate analyses
Only caregivers’ depressive symptoms were related to patient reports (see Table 3). Among caregivers reporting high depressive symptoms, their patients tended to report low mindfulness and high depressive symptoms, with small to medium effects.
Multivariate dyadic analyses: Partner effects
Only own greater mindfulness was related to one’s partner’s lower depressive symptoms. The strength of this effect for patients’ mindfulness and their caregivers’ depressive symptoms was equal to that for caregivers’ mindfulness and their patients’ depressive symptoms. No other partner effects were significant.
DISCUSSION
In this descriptive, cross-sectional data analysis of patients recently admitted to the Neuro-ICU and their primary caregivers, rates of clinically significant PTS, anxiety, and depressive symptoms were high and equally prevalent among patients and caregivers. Psychological resilience factors of mindfulness and coping were strongly inversely related to both patients’ and caregivers’ psychiatric symptoms. Findings provide the first evidence documenting the interdependence between patients’ and their caregivers’ mental health following hospitalization in the Neuro-ICU and suggest novel psychosocial intervention strategies to address their related psychiatric morbidity.
Findings reinforce that hospitalization in the Neuro-ICU is a traumatic event, leaving not only the patient, but also their family member, at risk for psychiatric morbidity (3, 6). Considering PTS, anxiety, and depression together, more than two in five patients and one in four caregivers met criteria for any psychiatric diagnosis. Consistent with literature from other medical conditions (8, 46, 47), patients’ and their informal caregivers’ depressive symptoms were interdependent. With one’s partner’s psychiatric adjustment to hospitalization in the Neuro-ICU representing an important risk factor for one’s own as well as one’s partner’s psychiatric morbidity, assessing and addressing distress in both patients and caregivers should be a priority during hospitalization (48, 49).
Given the interdependence noted among patients’ and their caregivers’ psychiatric adjustment to hospitalization, dyadic modeling was critical to our ability to capture the unique relation of patients’ own resilience with their own psychiatric symptoms teased apart from the effects of caregivers’ resilience and psychiatric distress on their patients’ symptoms (and similarly for caregivers’ own resilience to symptoms apart from patient effects). For both patients and caregivers, own greater mindfulness was independently related to own lower PTS and anxiety symptoms; own greater mindfulness was independently related to own lower depressive symptoms for patients only. Conversely, for both patients and caregivers, own greater coping skills were independently related to own lower anxiety and depressive symptoms, yet not PTS symptoms. Mindfulness may be particularly relevant to PTSD and anxiety, two disorders characterized by intrusive and unwanted thoughts, through increasing patients’ and caregivers’ ability to notice and disengage from these thoughts. Coping may be more pertinent to depressive symptoms through principles of behavioral activation, a key tenant of psychological therapies for depression.
Importantly, however, patients and caregivers who reported high use of mindfulness also tended to report a robust arsenal of coping skills, fitting with prior literature that these factors tend to be related (50). Indeed, mindfulness may be a key skill to know when and which coping strategy should be employed under stress (27). Further, psychiatric symptoms of PTS, anxiety, and depression were also highly interrelated within individuals. Findings suggest that psychosocial intervention to ameliorate distress among patients and caregivers in the Neuro-ICU may be most effective by enhancing psychological resilience factors broadly, rather than targeting any one psychiatric condition specifically. Techniques from evidence-based therapies may be particularly useful in enhancing patients’ and caregivers’ awareness of their stress triggers (e.g., uncertainty, fatigue, communication with family or doctors), knowledge of stress coping skills (e.g., problem solving, relaxation, observe-and-describe), and ability to effectively pair coping skills with stressors (e.g., action-oriented coping with controllable stressors, emotion-oriented coping with uncontrollable stressors). A broad, resiliency-based intervention may therefore be most applicable to reducing distress in the widest range of patients and caregivers in the Neuro-ICU.
Beyond capturing unique effects of own resilience on own psychiatric symptoms, the dyadic model also illuminates how one’s resilience may affect one’s partner’s psychiatric symptoms, beyond the effects of their partners’ own resilience. Such cross-over effect was revealed for depressive symptoms: beyond effects of own psychological resiliency factors, one’s own mindfulness was related to one’s partner’s depressive symptoms. This effect was independent of significant effects of one’s own resiliency factors and was equally strong for patients’ mindfulness to caregivers’ depression and vice versa from caregivers to patients. Findings fit within a broader literature showing that patients and caregivers adjust together to medical illness (36), encouraging the use of dyadic modeling when describing adjustment to medical illness. The ability to remain non-judgmental, accepting, and calm in the face of own or partner’s illness—facets of mindfulness—may assist in responding effectively to a partner’s distress and foster healthy interactions that may protect against development of depressive symptoms. Further investigation of this effect is warranted, yet suggests that targeting the patient-caregiver dyad as the unit of care holds promise to improve outcomes for both members of the dyad relative to current practice focusing on patients alone (48, 49).
Limitations and Future Directions
The current project is limited by use of self-report measures, which can be affected by bias. Future studies should seek to replicate results using objective markers of psychiatric distress through clinical interview, chart review, or psychoneuroimmuno/endocrinological markers, when possible. Further, the current analysis is cross-sectional. Future studies should seek to track the relations between patients’ and caregivers’ psychological resiliency and psychiatric symptoms across the recovery trajectory. Findings from other populations of medically ill patients and their caregivers suggests that dyads’ psychological distress aligns over time (47), suggesting patients’ and their caregivers’ psychiatric symptoms are likely to show stronger correlations as time since hospitalization progresses. Assessing these relationships prospectively over the long term is an important area for future research. Research is ongoing by our group to ascertain the extent to which early psychological resilience factors and psychiatric symptoms prospectively predict patients’ and their caregivers’ own and partners’ distress across the recovery trajectory following hospitalization in the Neuro-ICU.
Conclusions
Despite limitations, findings from the current study hold powerful clinical applications. Rates of clinically significant PTS, anxiety, and depression were high and equally prevalent among patients within 2 weeks of hospitalization in the Neuro-ICU and their primary informal caregiver. For patients and caregivers equally, high use of psychological resiliency factors of mindfulness and coping was associated with lower psychiatric symptoms. Moreover, patients’ and their caregivers’ depressive symptoms were intertwined, and the dyad members’ mindfulness mutually affected the others’ depression. Findings suggest that attending to the psychiatric health of both patients and caregivers in the Neuro-ICU is a priority, and that patients and their caregivers must be considered together in a system to fully address either individual’s psychiatric symptoms. Dyadic psychosocial interventions designed to enhance both patients’ and caregivers’ psychological resiliency through mindfulness and coping efficacy training may prove an effective and innovative way to ameliorate psychiatric morbidity and reduce suffering among vulnerable families presenting to the Neuro-ICU.
ACKNOWLEDGMENTS
We thank Tara Tehan, Mary Guanci, and the nursing staff within the Neuroscience ICU for their help with recruitment.
Ms. Shaffer received support for this project from the National Cancer Institute (NCI 1 F31 CA189431-01A1). Dr. Vranceanu received support from the Clinical Trials Methodology Course 5R25NS088248-02.
Copyright form disclosures: Ms. Shaffer received support for article research from the National Institutes of Health. Her institution received funding from the National Cancer Institute and the Clinical Trials Methodology Course.
Footnotes
This work was performed at the Massachusetts General Hospital, Boston, MA.
Disclosures: None.
The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Kiphuth IC, Utz KS, Noble AJ, Kohrmann M, Schenk T. Increased prevalence of posttraumatic stress disorder in patients after transient ischemic attack. Stroke. 2014;45(11):3360–3366. doi: 10.1161/STROKEAHA.113.004459. [DOI] [PubMed] [Google Scholar]
- 2.Carek V, Norman P, Barton J. Cognitive appraisals and posttraumatic stress disorder symptoms in informal caregivers of stroke survivors. Rehabil Psychol. 2010;55(1):91–96. doi: 10.1037/a0018417. [DOI] [PubMed] [Google Scholar]
- 3.Campbell Burton CA, Murray J, Holmes J, Astin F, Greenwood D, Knapp P. Frequency of anxiety after stroke: a systematic review and meta-analysis of observational studies. Int J Stroke. 2013;8(7):545–559. doi: 10.1111/j.1747-4949.2012.00906.x. [DOI] [PubMed] [Google Scholar]
- 4.Cumming TB, Blomstrand C, Skoog I, Linden T. The high prevalence of anxiety disorders after stroke. Am J Geriatr Psychiatry. 2015 doi: 10.1016/j.jagp.2015.06.003. pii:S1064-7481(15)00189-X. [DOI] [PubMed] [Google Scholar]
- 5.Denno MS, Gillard PJ, Graham GD, DiBonaventura MD, Goren A, Varon SF, et al. Anxiety and depression associated with caregiver burden in caregivers of stroke survivors with spasticity. Arch Phys Med Rehabil. 2013;94(9):1731–1736. doi: 10.1016/j.apmr.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 6.Hwang DY, Yagoda D, Perrey HM, Tehan TM, Guanci M, Ananian L, et al. Anxiety and depression symptoms among families of adult intensive care unit survivors immediately following brief length of stay. J Crit Care. 2014;29(2):278–282. doi: 10.1016/j.jcrc.2013.11.022. [DOI] [PubMed] [Google Scholar]
- 7.Turner-Stokes L, Hassan N. Depression after stroke: a review of the evidence base to inform the development of an integrated care pathway. Part 1: Diagnosis, frequency and impact. Clin Rehabil. 2002;16(3):231–247. doi: 10.1191/0269215502cr487oa. [DOI] [PubMed] [Google Scholar]
- 8.Cameron JI, Cheung AM, Streiner DL, Coyte PC, Stewart DE. Stroke survivors' behavioral and psychologic symptoms are associated with informal caregivers' experiences of depression. Arch Phys Med Rehabil. 2006;87(2):177–183. doi: 10.1016/j.apmr.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 9.Han B, Haley WE. Family caregiving for patients with stroke. Review and analysis. Stroke. 1999;30(7):1478–1485. doi: 10.1161/01.str.30.7.1478. [DOI] [PubMed] [Google Scholar]
- 10.Ayerbe L, Ayis S, Wolfe CD, Rudd AG. Natural history, predictors and outcomes of depression after stroke: systematic review and meta-analysis. Br J Psychiatry. 2013;202(1):14–21. doi: 10.1192/bjp.bp.111.107664. [DOI] [PubMed] [Google Scholar]
- 11.Gillen R, Tennen H, Affleck G, Steinpreis R. Distress, depressive symptoms, and depressive disorder among caregivers of patients with brain injury. J Head Trauma Rehabil. 1998;13(3):31–43. doi: 10.1097/00001199-199806000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Edmondson D, Richardson S, Fausett JK, Falzon L, Howard VJ, Kronish IM. Prevalence of PTSD in survivors of stroke and transient ischemic attack: a meta-analytic review. PLoS One. 2013;8(6):e66435. doi: 10.1371/journal.pone.0066435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carod-Artal FJ, Egido JA. Quality of life after stroke: the importance of a good recovery. Cerebrovasc Dis. 2009;27(Suppl. 1):204–214. doi: 10.1159/000200461. [DOI] [PubMed] [Google Scholar]
- 14.Bartoli F, Lillia N, Lax A, Crocamo C, Mantero V, Carrà G, et al. Depression after stroke and risk of mortality: a systematic review and meta-analysis. Stroke Res Treat. 2013;2013:862978. doi: 10.1155/2013/862978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee S, Colditz GA, Berkman LF, Kawachi I. Caregiving and risk of coronary heart disease in US women: a prospective study. Am J Prev Med. 2003;24(2):113–119. doi: 10.1016/s0749-3797(02)00582-2. [DOI] [PubMed] [Google Scholar]
- 16.Ji J, Zöller B, Sundquist K, Sundquist J. Increased risks of coronary heart disease and stroke among spousal caregivers of cancer patients. Circulation. 2012;125(14):1742–1747. doi: 10.1161/CIRCULATIONAHA.111.057018. [DOI] [PubMed] [Google Scholar]
- 17.Rohleder N, Marin TJ, Ma R, Miller GE. Biologic cost of caring for a cancer patient: dysregulation of pro-and anti-inflammatory signaling pathways. J Clin Oncol. 2009;27(18):2909–2915. doi: 10.1200/JCO.2008.18.7435. [DOI] [PubMed] [Google Scholar]
- 18.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282(23):2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 19.Godwin KM, Swank PR, Vaeth P, Ostwald SK. The longitudinal and dyadic effects of mutuality on perceived stress for stroke survivors and their spousal caregivers. Aging Ment Health. 2013;17(4):423–431. doi: 10.1080/13607863.2012.756457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bakas T, Burgener SC. Predictors of emotional distress, general health, and caregiving outcomes in family caregivers of stroke survivors. Top Stroke Rehabil. 2002;9(1):34–45. doi: 10.1310/GN0J-EXVX-KX0B-8X43. [DOI] [PubMed] [Google Scholar]
- 21.Beach SR, Schulz R, Williamson GM, Miller LS, Weiner MF, Lance CE. Risk factors for potentially harmful informal caregiver behavior. J Am Geriatr Soc. 2005;53(2):255–261. doi: 10.1111/j.1532-5415.2005.53111.x. [DOI] [PubMed] [Google Scholar]
- 22.Martire LM, Stephens MA, Druley JA, Wojno WC. Negative reactions to received spousal care: predictors and consequences of miscarried support. Health Psychol. 2002;21(2):167–176. [PubMed] [Google Scholar]
- 23.Palmer S, Glass TA. Family function and stroke recovery: A review. Rehabil Psychol. 2003;48(4):255–265. [Google Scholar]
- 24.Molina Y, Yi JC, Martinez-Gutierrez J, Reding KW, Yi-Frazier JP, Rosenberg AR. Resilience among patients across the cancer continuum: diverse perspectives. Clin J Oncol Nurs. 2014;18(1):93–101. doi: 10.1188/14.CJON.93-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Siriwardhana C, Ali SS, Roberts B, Stewart R. A systematic review of resilience and mental health outcomes of conflict-driven adult forced migrants. Confl Health. 2014;8:13. doi: 10.1186/1752-1505-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cal SF, Santiago MB. Resilience in systemic lupus erythematosus. Psychol Health Med. 2013;18(5):558–563. doi: 10.1080/13548506.2013.764457. [DOI] [PubMed] [Google Scholar]
- 27.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 28.Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. J Health Soc Behav. 1980;21(3):219–239. [PubMed] [Google Scholar]
- 29.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: a meta-analysis. J Psychosom Res. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 30.Penley JA, Tomaka J, Wiebe JS. The association of coping to physical and psychological health outcomes: A meta-analytic review. J Behav Med. 2002;25(6):551–603. doi: 10.1023/a:1020641400589. [DOI] [PubMed] [Google Scholar]
- 31.Hedlund M, Ronne-Engström E, Carlsson M, Ekselius L. Coping strategies, health-related quality of life and psychiatric history in patients with aneurysmal subarachnoid haemorrhage. Acta Neurochir (Wien) 2010;152(8):1375–1382. doi: 10.1007/s00701-010-0673-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Finset A, Andersson S. Coping strategies in patients with acquired brain injury: relationships between coping, apathy, depression and lesion location. Brain Inj. 2000;14:887–905. doi: 10.1080/026990500445718. [DOI] [PubMed] [Google Scholar]
- 33.Wartella JE, Auerbach SM, Ward KR. Emotional distress, coping and adjustment in family members of neuroscience intensive care unit patients. J Psychosom Res. 2009;66(6):503–509.. doi: 10.1016/j.jpsychores.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 34.Cruzado JA, Elvira de la Morena MJ. Coping and distress in caregivers of patients with disorders of consciousness. Brain Inj. 2013;27(7-8):793–798. doi: 10.3109/02699052.2013.793402. [DOI] [PubMed] [Google Scholar]
- 35.Ben-Zur H, Gilbar O, Lev S. Coping with breast cancer: patient, spouse, and dyad models. Psychosom Med. 2001;63(1):32–39. doi: 10.1097/00006842-200101000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychol Bull. 2007;133(6):920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- 37.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behav Res Ther. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 38.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th. American Psychiatric Association; Washington, DC: 2000. text rev. [Google Scholar]
- 39.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 40.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 41.Feldman G, Hates A, Kumar S, Greeson J, Laurenceau JP. Mindfulness and emotion regulation: The development and initial validation of the Cognitive and Affective Mindfulness Scale Revised (CAMS-R) J Psychopathol Behav Assess. 2007;29(3):177–190. [Google Scholar]
- 42.Carver CS. Measure of Current Status. 2006 http://www.psy.miami.edu/faculty/ccarver/sclMOCS.html.
- 43.Cohen J. A power primer. Psych Bull. 1992;112(1):155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 44.Kenny DA, Cook W. Partner effects in relationship research: Conceptual issues, analytic difficulties, and illustrations. Pers Relationships. 1999;6(4):433–448. [Google Scholar]
- 45.Kenny DA, Kashy DA, Cook WL. Dyadic Data Analysis. The Guilford Press; 2006. [Google Scholar]
- 46.Rosendahl J, Brunkhorst FM, Jaenichen D, Strauss B. Physical and mental health in patients and spouses after intensive care of severe sepsis: a dyadic perspective on long-term sequelae testing the Actor–Partner Interdependence Model. Crit Care Med. 2013;41(1):69–75. doi: 10.1097/CCM.0b013e31826766b0. [DOI] [PubMed] [Google Scholar]
- 47.Hodges L, Humphris G, MacFarlane G. A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their carers. Soc Sci Med. 2005;60(1):1–12. doi: 10.1016/j.socscimed.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 48.White CL, Lauzon S, Yaffe MJ, Wood-Dauphinee S. Toward a model of quality of life for family caregivers of stroke survivors. Qual Life Res. 2004;13(3):625–638. doi: 10.1023/B:QURE.0000021312.37592.4f. [DOI] [PubMed] [Google Scholar]
- 49.Martire LM, Lustig AP, Schulz R, Miller GE, Helgeson VS. Is it beneficial to involve a family member? A meta-analysis of psychosocial interventions for chronic illness. Health Psychol. 2004;23(6):599–611. doi: 10.1037/0278-6133.23.6.599. [DOI] [PubMed] [Google Scholar]
- 50.Weinstein N, Brown KW, Ryan RM. A multi-method examination of the effects of mindfulness on stress attribution, coping, and emotional well-being. J Res Pers. 2009;43(3):374–385. [Google Scholar]


