Review on how complex mixtures of bioactive lipids and cholesterol may influence the pulmonary immune response during infection.
Keywords: respiratory infections, immunity, oxidized phospholipids, n-3 PUFAs
Abstract
Bacterial and viral respiratory tract infections result in millions of deaths worldwide and are currently the leading cause of death from infection. Acute inflammation is an essential element of host defense against infection, but can be damaging to the host when left unchecked. Effective host defense requires multiple lipid mediators, which collectively have proinflammatory and/or proresolving effects on the lung. During pulmonary infections, phospholipid acyl chains and cholesterol can be chemically and enzymatically oxidized, as well as truncated and modified, producing complex mixtures of bioactive lipids. We review recent evidence that phospholipids and cholesterol and their derivatives regulate pulmonary innate and adaptive immunity during infection. We first highlight data that oxidized phospholipids generated in the lung during infection stimulate pattern recognition receptors, such as TLRs and scavenger receptors, thereby amplifying the pulmonary inflammatory response. Next, we discuss evidence that oxidation of endogenous pools of cholesterol during pulmonary infections produces oxysterols that also modify the function of both innate and adaptive immune cells. Last, we conclude with data that n-3 polyunsaturated fatty acids, both in the form of phospholipid acyl chains and through enzymatic processing into endogenous proresolving lipid mediators, aid in the resolution of lung inflammation through distinct mechanisms. Unraveling the complex mechanisms of induction and function of distinct classes of bioactive lipids, both native and modified, may hold promise for developing new therapeutic strategies for improving pulmonary outcomes in response to infection.
Introduction
Respiratory infections, both bacterial and viral, contribute to more than 3 million deaths worldwide annually [1, 2]. Currently, pneumonia is the leading cause of death by infection [3]. Therapeutics available to treat respiratory infections are limited in scope and can have multiple adverse side effects and low efficacy [4–6]. Respiratory infections initiate both innate and adaptive immune responses in the lung. Although these immune responses are critical for clearing respiratory pathogens, they must be tightly regulated to effectively kill invading microorganisms while minimizing bystander tissue injury and maintaining pulmonary function. In the present review, we discuss evidence that 2 classes of lipid mediators—oxPLs and oxysterols—are generated during infection and then mediate the pulmonary immune response. We also explain how pools of exogenous lipids (n-3 PUFAs) incorporated into host phospholipids can mitigate and improve the immunopathology associated with bacterial and viral pneumonia. Improved insight into these lipid mediators may ultimately provide novel therapeutic targets for the clinical management of pulmonary infection.
A BRIEF OVERVIEW OF THE PULMONARY INNATE IMMUNE RESPONSE TO INFECTION
The respiratory tract is constantly exposed to the outside environment and is challenged by insults both infectious and inflammatory [7]. The first line of defense that the lungs have against invading pathogens is the resident cells of the lung, both structural (i.e., respiratory epithelial cells) and hematopoietic (i.e., AMs) [8]. These cells, and the communications between them, are pivotal in orchestrating the pulmonary immune response to microorganisms. The epithelial cells of the respiratory tract create barriers mediated by their production of both secretory mediators and intercellular junctional proteins [9]. The secretory products of the upper and lower airways include mucin and pulmonary surfactant. During infection, mucin production is upregulated, in part through metaplasia of goblet cells, and serves to prevent microbes from binding to and infecting epithelial cells [10, 11]. Pulmonary surfactant, a complex mixture of ∼90% lipid and 10% protein, serves both to decrease surface tension in the alveolus and to protect the respiratory tract from pathogens [12]. The hydrophobic SP-A and SP-D, are collectins, a protein family that recognizes a wide range of PAMPs, including those found on respiratory viruses, bacterial and fungal pathogens, and associated toxins [13–15]. Once the SPs bind to pathogens, they promote opsonization and subsequent killing of the pathogens by phagocytic cells in the respiratory tract, such as AMs.
In addition to providing protection against infection through mucociliary clearance and surfactant, respiratory epithelial cells also express PRRs, including TLRs, SRs, NOD-like receptors, and retinoic acid-inducible gene 1-like receptors, that recognize PAMPs and DAMPs [16, 17]. Once PRRs on respiratory epithelial cells are stimulated by PAMPs and DAMPs, cytokine production is initiated by downstream signaling adapters, such as MyD88 and TRIF, that in turn activate key transcription factors, such as NF-κB and interferon regulatory factor-3 [9, 16]. The release of cytokines and chemokines recruits innate and adaptive immune cells to the lung from the periphery [9, 16]. During pulmonary infections, MyD88-dependent downstream signaling leads to the production of proinflammatory cytokines, such as TNF-α and IL-6, that act in concert with chemoattractants, such as CXCL1 and -2, to recruit PMNs to the lungs that kill pathogens [9, 16, 18]. The TRIF-mediated pathway in the respiratory epithelium induces type I IFN production (i.e., IFN-α and -β) [19] . Type I IFN signaling is critical to host defense, as revealed by mice lacking the receptor to type I IFN that succumb to infection by influenza virus [20]. Activation of type I IFNs produces several specific antiviral factors, such as IFN-induced GTP-binding protein MX dynamin-like GTPase 1, as well as various cellular responses that are important in T cell recruitment and polarization [20, 21].
The lung has resident populations of hematopoietic cells—in particular, AMs and DCs—that patrol the airspace, detecting PAMPs and contributing to the local milieu of cytokines and chemokines [22]. Upon recognizing PAMPs or DAMPs, these 2 cell populations upregulate costimulatory molecules essential for initiation of adaptive immune responses. Stimulus-matured DCs in particular present Ag after migration to the local lymph nodes [23, 24]. In addition, cytokine and chemokine production by AMs and DCs can recruit innate immune cells, such as PMNs, monocytes/macrophages, and NK cells to facilitate killing of infected cells and pathogens [25, 26]. Additional innate immune cells serve important roles in respiratory infections, such as mast cells, NK T cells, and innate lymphoid cells; however, in this review, we focus primarily on immune cell types with a defined response to lipid mediators.
Recruited innate immune cells provide the first line of defense during pulmonary infections. PMNs, NK cells, and monocytes in particular infiltrate the lung and commence pathogen clearance. PMNs respond to the various chemokines produced by AMs and epithelial cells, including CXCL1 and the MIPs CCL3, CCL4, and CXCL2, and serve a predominant function in intracellular and extracellular killing of microbes [18, 27]. PMN-mediated killing is an essential aspect of host defense in a variety of pulmonary infections, including those caused by Aspergillus fumigatus [28], Bordetella pertussis [29], Pseudomonas aeruginosa [30], Streptococcus pneumoniae [31], and Klebsiella pneumoniae [32]. PMNs express numerous PRRs and mediate microbial killing through production of ROS and secretion of azurophilic granule contents, lysozymes [33], and via the formation of neutrophil extracellular traps [34].
NK cells are innate lymphocytes that also contribute to the first line of defense against infection. NK cells are widely distributed in lymphoid and nonlymphoid tissues [35–37]. However, in the respiratory tract, NK cells make up a higher percentage of lymphocytes than in other tissues and are able to respond quickly to infection and thus are critical for maintaining pulmonary homeostasis [38]. The function of NK cells is regulated by a range of activating and inhibitory receptors. Genetic deficiencies that result in loss of NK cell function have been associated with recurrent viral and bacterial infections, including those of the upper and lower respiratory tract.
Macrophages and DCs provide a key bridge between innate and adaptive immunity. Macrophages and DCs are professional APCs that, in response to infection and insult, infiltrate tissues and initiate an inflammatory response. Macrophages are not only key players in the initiation of inflammation, but also orchestrate its resolution [25]. Macrophages can be broadly categorized into 2 subsets [39]. Classically activated or M1 macrophages are induced by the bacterial cell wall component LPS or a combination of the Th1 cytokines IFN-γ and TNF-α [39]. Alternatively activated or M2 macrophages are induced by Th2 cytokines such as IL-4 and -13 [5]. M1 macrophages are characterized by the production of ROS, reactive nitrogen intermediates, IL-1, IL-12, and TNF-α [39, 40]. In addition, M1 macrophages drive Th1 responses, have roles in antitumor immunity, and kill intracellular foreign pathogens [41]. M2 macrophages express arginase-1, scavenger and mannose receptors, and IL-10. This macrophage subset regulates wound healing, restores tissue homeostasis, and also antagonizes proinflammatory M1 macrophage responses. Recent studies have shown that M1 phenotype is not static and that these macrophages can acquire anti-inflammatory features with an M2 wound-healing phenotype depending on the cytokine milieu to which they are exposed [42]. There is also evidence for subpopulations of M2 macrophages (M2a, M2b, and M2c) that are also characterized by differential expression of surface receptors and transcription factor expression as well as functional differences [43].
A BRIEF OVERVIEW OF THE PULMONARY ADAPTIVE IMMUNE RESPONSE TO INFECTIONS
After the innate immune response is initiated in the lung, the adaptive immune response is called in to perform definitive pathogen clearance and to protect against reinfection. The 2 main adaptive immune cell types required after pulmonary infection are T and B cells. T cell migration into the lung is thought to be driven by chemokine gradients produced by innate and adaptive immune cells [44]. Both CD4+ and CD8+ T cells program antibody production by B cells and are required for reduction of pathogen burden [45]. In murine models of influenza infection, viral clearance is not dependent upon CD4+ or CD8+ T cells individually; however, genetic deletion of both cell types completely abolishes viral clearance [46, 47]. Thus, these 2 T cell subsets work in concert to eliminate pathogens from the lungs.
CD4+ Th cells assist B cells to mount antibody secretion, provide feedback to DCs via costimulatory molecules and the elaboration of cytokines, as well as enhance and maintain responses of CD8+ (cytotoxic) T cells [44]. Moreover, CD4+ T cells have direct effector actions, including performing cytotoxic functions, mediating macrophage activation, and inducing genes in mucosal tissues that contribute to host defense [48]. Polarization of naïve CD4+ T cells into effector T cells is determined by the cytokine milieu, the strength of signal associated with Ag presentation, and the Ag itself [49]. Effector Th-cell subsets include Th1 (characterized by IFN-γ secretion and T-box transcription factor expression), Th2 (characterized by IL-4 secretion and GATA3 expression), Th17 (characterized by IL-17 secretion and RORγt expression), T-regulatory (Treg; characterized by forkhead box P3 expression), and T follicular helper (characterized by CXCR5 expression, B-cell lymphoma-6, and enhanced IL-21 secretion) [48]. Each Th subtype has a unique and essential role in the pulmonary immune response during respiratory infections, but if inappropriately stimulated, can also lead to detrimental effects on the host.
Much like CD4+ Th cells, CD8+ T cells are heterogeneous after activation [50, 51]. However, in the context of pulmonary infections, CTLs are perhaps the best characterized. CD8+ CTLs play a vital role in eliminating influenza-infected cells in the lung by Ag-specific cytotoxicity and cytokine and chemokine production. When CTLs recognize an infected cell through foreign peptides in the context of host MHC molecules, CTL-mediated killing is induced by secretion of pore-forming proteins (perforin) and cytotoxic granules that initiate apoptosis [52]. This mechanism is very effective in controlling infection in the lung but can also lead to significant inflammation and release of DAMPs that can increase tissue injury.
After CD4+ and CD8+ T cells develop an effector phenotype as a result of Ag stimulation, they possess the ability to proliferate or survive for long-term maintenance of adaptive immunity [22, 27, 29–34, 53, 54]. In addition, a fraction of these T cells retain a memory phenotype, which is important in the recall response during infection. Memory T cells share epitope specificity and T cell receptor sequences with the effector T cell subsets and have stem cell-like characteristics [55, 56].
B cells are key effector cells of the immune response to infection and are composed of both innate (i.e., B1) and adaptive (i.e., B2) subsets [57, 58]. The role of B cells during infection has been mostly studied in conjunction with diverse antibody production (IgG, IgA, and IgM). However, B cells are also important sources of cytokines and Ag presentation during respiratory infections [59]. After infection with respiratory viruses such as influenza, B cells are primed with viral Ag in the secondary lymphoid organs. After priming, B cells proliferate into short- and long-lived plasma cells and memory B cells that either travel back to the lung and form induced bronchus-associated lymphoid tissue or stay in the lymph nodes [60]. This provides not only a source of neutralizing antibody for the primary infection but also source of protection against reinfection.
CHANGES IN PULMONARY PHOSPHOLIPID COMPOSITION DURING INFECTION AND INFLAMMATION
The primary source of phospholipids (PLs) in the lung is pulmonary surfactant, synthesized and released by alveolar epithelial type II cells. As discussed above, surfactant contains approximately 80–90% PLs, with fatty acid chains that can be oxidized during different challenges in the lung [61, 62]. In addition, PLs are major constituents of cellular membranes and can be released during cell death and injury [63]. Oxidation of these PLs in the lung can occur during normal physiologic and metabolic processes but also in the setting of the increased oxidative stress of infection and inflammation [64]. Upon oxidation, PLs can be oxidized into a variety of species, including 1-palmitoyl-2-(5,6) epoxyisoprostane E2-sn-glycero-3-phosphocholine (PEIPC), 1-palmitoyl-2-(5-oxovaleroyl)-sn-glycero-3-phosphocholine (POVPC), and smaller chemical fragments [65]. OxPLs are generated through either enzymatic or nonenzymatic reactions induced by ROS production, air pollution, cigarette smoke, and UV radiation [65–68]. OxPLs are thought to serve as DAMPs, insofar as they can stimulate multiple innate immune receptors, leading to prolonged inflammation and downstream signaling [64]. Once generated, oxPLs can be cleared by multiple biologic mechanisms, including enzymatic inactivation by epoxide hydrolases and aldehyde dehydrogenases, formation of adducts, or uptake through SRs or through neutralization by natural antibodies, C-reactive protein, and complement factor H [69–72]. The immune effects of oxPLs during infectious diseases are inevitably dictated by the balance among activation, degradation, and scavenging.
The increase in oxPL levels has been well characterized in diseases associated with chronic inflammation, such as atherosclerotic cardiovascular disease and diabetes. It has been shown that oxPLs are generated in the lung during several pulmonary infections, including influenza [73, 74] and avian influenza (H5N1), SARS coronavirus, Bacillus anthracis, Yersinia pestis, and monkey pox. It is unclear what the primary source of increased oxPLs is during pulmonary infections; however, one could speculate that an increase in cellular apoptosis, an increase in ROS by phagocytic cells, and changes in surfactant from pulmonary inflammation are major contributors. In a pivotal paper Imai et al. [75] noted that oxPL levels are increased during H5N1 infection and that blocking oxPLs decreases the pulmonary inflammation associated with infection. They found oxPL-mediated inflammation during infection to be a result of TLR4 activation of the TRIF pathway, indicating that oxPLs can serve as DAMPs that amplify the innate immune response during infection (Fig. 1).
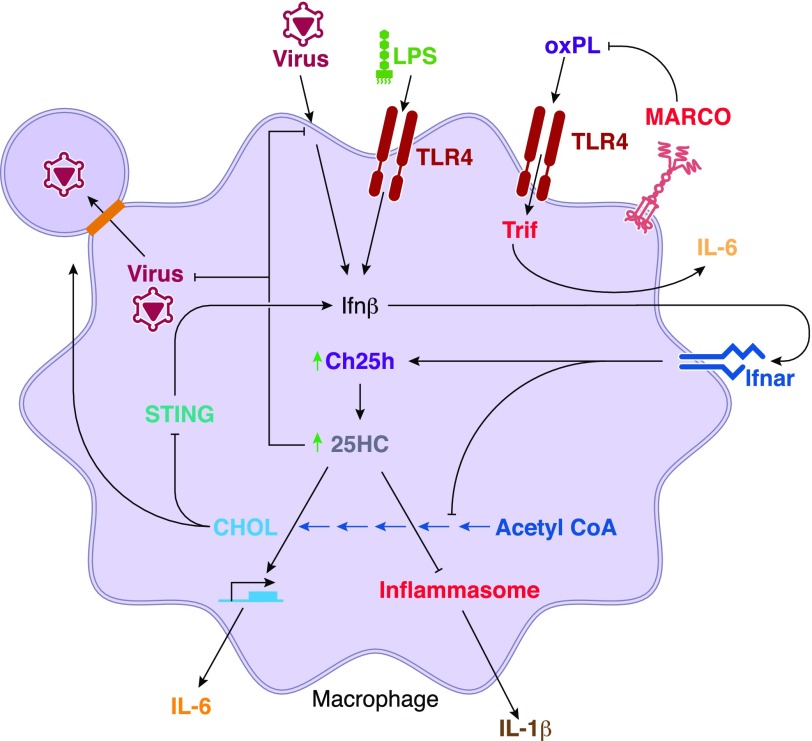
Figure 1. Integration of lipid homeostasis into the macrophage host defense response.
Selected roles for cholesterol, oxysterols, and oxPLs in the macrophage innate immune response are depicted. IFN-β induced by virus or LPS feeds back through autocrine/paracrine signaling, upregulating Ch25h and also inhibiting the cholesterol (CHOL) synthesis pathway. 25HC, the product of Ch25h, exerts several effects, inhibiting viral fusion and proliferation, inhibiting inflammasome-dependent IL-1β production, but also augmenting induction of select proinflammatory genes, such as IL-6. IFN-β-dependent inhibition of cholesterol biosynthesis augments antiviral defense by enhancing stimulator of Ifn genes–dependent IFN-β induction and also possibly by depleting lipid rafts, through which several viruses bud from host cells. OxPL induced in the inflamed lung and not cleared by scavenger receptors such as macrophage receptor with collagenous structure may induce TLR4-dependent proinflammatory cytokines via the adaptor protein TIR-domain–containing adaptor-inducing IFN-β (Trif), aggravating lung injury. Ifnar, Ifnα/β receptor.
IMMUNE CONSEQUENCES OF OXIDIZED PHOSPHOLIPID GENERATION DURING RESPIRATORY INFECTIONS
OxPLs have been shown to elicit multiple immune-mediated effects during infection and inflammation. As DAMPs, oxPLs are recognized by multiple PRRs, including macrophage receptor with collagenous structure (MARCO), SR-A, CD36, SR-BI, platelet activating factor receptor, prostaglandin receptors, and TLRs [69–72]. All of these receptors are expressed on resident or infiltrating cells of the lung. Therefore, excess production of oxPLs can alter multiple cellular functions that are important in the pulmonary immune response during respiratory infections. For the purpose of this review, we focus on the mechanisms by which oxPLs alter cytokine secretion, production of ROS by phagocytic cells, phagocytosis, and the adaptive immune response.
OxPLs may have stimulatory or inhibitory effects on PRRs, depending on the context of signaling. Mice deficient in TLR4, MyD88, or TRIF have decreased oxPAPC-induced lung inflammation; moreover, blocking TLR4 signaling during oxPAPC exposure leads to decreased IL-8 production [76]. In addition, TLR2-deficient bone marrow-derived macrophages have decreased cytokine production after oxPAPC stimulation [77]. However, oxPLs have also been reported to have dampening effects on PAMP-induced cytokine production. OxPAPC inhibits macrophage production of TNF-α after stimulation with LPS, 5′-C-phosphate-G-3′DNA, and Pam3CSK4 [77–79]. In the context of LPS signaling, oxPAPC has been reported to inhibit LPS binding to the TLR4 accessory proteins CD14 [77] and myeloid differentiation factor 2 [80]. In the context of influenza infection, oxPL-induced inflammation is mediated by TLR4 and TRIF, driving an increase in IL-6 production by AMs ([75], Fig. 1). However, in the context of an innate immune challenge in a model of LPS-induced pneumonitis wherein rats were pretreated intravenously with oxPLs, reductions in airspace PMNs, microvascular injury, and proinflammatory cytokines were noted [81]. The differences in pulmonary responses noted in these 2 studies could be the result of differences in the timing and route of oxPL delivery or in the technical features of the models tested. Taken together, the findings in these studies demonstrate that oxPLs can exert pro- and anti-inflammatory effects during the innate immune response.
OxPLs also alter phagocytosis and ROS production in addition to cytokine secretion [82, 83]. Some studies have shown that oxPAPC can inhibit PKA-mediated bacterial phagocytosis in peritoneal macrophages [82], as well as in the setting of bacterial pneumonia [84]. This effect could be a result of oxPLs altering the assembly of Rho, Rac, and Cdc42, as well as actin cytoskeleton remodeling, which has been reported in vitro in macrophages [65, 85]. Phagocytosis of pathogens is typically coupled to ROS production, which plays a central role in the killing of internalized microbes. Of note, oxPAPC has been shown to impair ROS production by PMNs [86]. It is intriguing to consider that oxPL-dependent defects in phagocytosis and ROS generation may lead to increased susceptibility to respiratory infections.
Recent findings suggest that oxPLs also modify adaptive immunity, at least in part through their effects on innate immune cells. DCs treated with oxPAPC display reduced upregulation of the costimulatory molecules CD40, CD80, CD86, MHCII, and CCR7 induced by LPS and the TLR3 PAMP poly(I:C) [87], suggesting probable downstream effects on Th cell programming. OxPAPC treatment of DCs also resulted in reduced IL-12 production and altered naïve T cell polarization [88]. Oxidized LDL has also been shown to inhibit TLR induction of proinflammatory cytokines in CD8aneg DCs, thus skewing T cells away from a Th1 phenotype [89]. In addition, flipping of phosphatidylserine from the inner to the outer plasma membrane leaflet during apoptosis of infected cells has been shown to suppress adaptive immune responses such as dendritic cell function and T cell activation [2, 3, 5, 6]. Although most of the effects of oxPLs have been documented in in vitro models, this area of oxPL-mediated immunity could ultimately prove highly relevant to the in vivo efficacy of vaccines designed to combat pulmonary pathogens.
EMERGING ROLES FOR CHOLESTEROL AND OXYSTEROLS IN PULMONARY INFLAMMATION AND HOST DEFENSE
Cholesterol is the major neutral lipid in pulmonary surfactant, in which it is thought to promote the spreading, mobility, and adsorption of surfactant films [90]. Most of the cholesterol in the lung derives from uptake of circulating plasma lipoproteins [91], rendering the lung and its extracellular surfactant reservoir sensitive to diet and systemic metabolic states [92]. Cholesterol overload in the lung and, in particular, in pulmonary macrophages, is avoided through reverse cholesterol transport from tissue to plasma which, as in other tissues, involves interactions between cellular lipid efflux transporters (e.g., ATP binding cassette transporter G1 [93]) and plasma lipid acceptors (e.g., HDL). Intriguingly, increased numbers of lipid-laden macrophage foam cells have been described in a wide range of chronic inflammatory lung diseases [94], suggesting that phagocyte cholesterol dysregulation may be a common, and potentially, a causal event in lung disorders. As a determinant of cell signaling and a molecular target of both chemical and enzymatic oxidation, cholesterol serves as a pivotal regulator of inflammation and host defense. The lung-specific implications of this emerging role for cholesterol in inflammation and immunity, however, have only recently begun to be defined [95].
Cholesterol levels in macrophages and other cells are determined as a balance between biosynthesis (by the mevalonic acid pathway) and receptor-mediated uptake on the one hand and regulated efflux on the other [96]. Cholesterol potentiates host defense signaling in part through promoting signaling interactions in so-called cholesterol-enriched lipid raft membrane microdomains where multiple receptors, including TLRs, the T cell receptor, the B-cell receptor, and MHCII are assembled and activated [97]. Raft cholesterol is also critical to the viral life cycle in host cells, as several viruses, including influenza A, respiratory syncytial virus, and HIV are thought to bud from lipid raft microdomains (Fig. 1) [98]. Raft cholesterol also regulates the invasion of multiple bacterial pathogens into host cells. Further suggesting intrinsic and perhaps evolutionary connections between virus and cholesterol trafficking, the HDL receptor SR-BI serves as a host cell receptor for HCV [99], and Niemann-Pick C1, an endosomal cholesterol transporter, was recently identified as the cellular receptor for Ebola virus [100, 101].
Recent reports have shown that IFN-dependent downregulation of the mevalonic acid synthesis pathway is an intrinsic feature of the antiviral host defense response (Fig. 1) [102, 103]. Viral infection induces downregulation of most of the enzymes in the mevalonic acid pathway in macrophages through an autocrine type I IFN loop, and this metabolic response is essential for successful host defense. Reports differ on whether host cell protection derives from shutdown of new cholesterol synthesis [103] or from depletion of cellular isoprenoids [102], an alternate lipid product of the mevalonic acid synthesis pathway. Depletion of newly synthesized cholesterol in the endoplasmic reticulum may potentiate activation of, and IFN induction by, the antiviral receptor stimulator of IFN genes, potentiating an antiviral feedforward loop (Fig. 1) [103]. Both statin treatment of wild-type mice [102] and gene-targeting of the mevalonic acid synthesis pathway in mutant mice [103] enhanced host defense against virus in vivo, including lung infections. Further suggesting an evolutionary role for cholesterol in antiviral host defense, the antiviral effector IFN-inducible transmembrane protein-3 is reported to inhibit viral entry into host cells via disruption of intracellular cholesterol trafficking [104].
Cholesterol is susceptible to oxidation. Analogous to the case for the double bonds of unsaturated acyl chains in surfactant PLs, direct oxidation of the carbon 5-6 double bond of the B ring of cholesterol by ROS is likely a common event for pulmonary surfactant cholesterol in the setting of inhaled oxidants such as ozone [105]. Ring oxidation yields cytotoxic oxysterols, such as β-epoxide [105], the clearance of which is regulated by SRs [106]. On the other hand, several enzymes are known to add hydroxyl groups to the side chain carbons of cholesterol (i.e., carbons 20–27), yielding side chain oxysterols (e.g., 25HC) that have pleiotropic bioactivity [107]. Several such oxysterol-synthetic enzymes appear to have particular relevance to phagocyte biology in the lung. For example, CYP27A1 is highly expressed in AMs of the human lung, and its product, cholestenoic acid, is thought to play a key role in cholesterol homeostasis in the human lung [108]. Ch25h, an enzyme that produces 25HC from cholesterol, is also most highly expressed in the lung in mice [107], likely because of its very high expression in AMs (www.immgen.org).
25HC has recently been shown to have highly complex effects on inflammation and host defense (Fig. 1). Proinflammatory actions include potentiation of activator protein-1 binding to the promoter of proinflammatory genes [109] and chemoattraction of leukocytes via CXCR2 [110], whereas potential anti-inflammatory actions include suppression of the inflammasome [111], repression of NF-κB via activation of the nuclear receptor liver X receptor [112], and suppression of B cell proliferation and IgA class switching [113]. A recent landmark discovery was the recognition that Ch25h is an IFN-stimulated gene that is robustly induced by both TLR agonists and virus [113–115] and that its product 25HC is a potent antiviral molecule that suppresses virus through inhibiting host cell fusion [114] or postfusion events [115]. As 25HC is reportedly increased in the sputum of patients with COPD [116] and also induced in vivo in the plasma of humans after systemic LPS challenge [117], its complex effects in host defense and inflammation are likely highly relevant to human disease and clearly warrant further study.
Additional oxysterols have recently been shown to have key roles in immunity. 7α,25-OHC, a further oxidation product of the effect of cytochrome P450 (family 7 subfamily b, polypeptide 1) on 25HC, was recently shown to be a chemoattractant to multiple leukocyte subtypes via ligation of the GPCR, Epstein-Barr virus-induced gene 2 (Ebi2). Because of deficient 7α,25-OHC gradients in the spleen or responsiveness to them, both Ch25h-null and Ebi2-null mice fail to position splenic B cells in the outer follicle and mount a reduced plasma cell response after immune challenge [118, 119]. 7α,25-OHC also plays a key role in Ebi2-dependent positioning of CD4+ DCs to marginal zone bridging channels in the spleen, facilitating capture, presentation, and antibody responses to bloodborne Ags [120, 121]. Several other oxysterols including 7β,27-dihydroxycholesterol have also been reported to be agonists for ROR-γt, the hallmark transcription factor for Th17 differentiation; thus, mice deficient in CYP27A1, an enzyme that contributes to synthesis of these RORγt-active oxysterols, have Th17 cell deficiency comparable to that of RORγt-knockout mice [122].
While in most cases direct roles for cholesterol and the various oxysterols in pulmonary inflammation and immunity have yet to be demonstrated, the very high expression of CYP27A1 and related oxysterol-synthetic enzymes in the lung suggest that cholesterol metabolism and the dynamic fluxes in it in response to environmental challenge are likely highly relevant to lung disease. Further directed study is thus clearly warranted for sterols in this disease context.
n-3 PUFAs POTENTIALLY REGULATE LUNG INFLAMMATION
Innate and adaptive immune responses are influenced not only by oxPLs and cholesterol, but also by the fatty acid profile of tissues in response to pharmacological agents and diet [123]. In particular, long-chain n-3 PUFAs have emerged as potential regulators of inflammation. Long chain n-3 PUFAs are essential fatty acids obtained from marine sources. These fatty acids can also be generated upon elongation and desaturation from short chain n-3 PUFAs [124], albeit the latter may not be an efficient process in many tissues. The 2 major long chain n-3 PUFAs that are discussed with respect to immunity are EPA (20:5) and DHA (22:6).
It is important to note that EPA and DHA (in addition to other PUFAs), by serving as substrates for select enzymes such as the 5- and 12/15-lipoxygenases, generate specialized proresolving lipid mediators (SPMs) [125]. SPMs, which include protectins, resolvins, lipoxins, and maresins, are potent molecules that stereospecifically target GPCRs to orchestrate the resolution phase of inflammation. A recent review elegantly highlights studies on how SPMs aid in the resolution of pulmonary inflammation [126]. Therefore, we are focusing in this review on key studies that demonstrate a role for EPA and DHA as dietary or pharmacologic agents in influencing lung inflammation and pulmonary outcomes in infection. We first review preclinical and clinical studies in which EPA and DHA were used to elucidate their role in lung homeostasis. We then discuss potential molecular mechanisms of EPA and DHA in the context of infection and inflammation.
n-3 PUFAs improve pulmonary outcomes associated with lung infection and inflammation in preclinical models
Several laboratories have examined in rodent models how n-3 PUFA uptake into the lung tissue influences outcomes associated with infection. For instance, n-3 PUFAs in a murine model promoted the resolution of inflammation, which was associated with enhanced bacterial clearance and survival of P. aeruginosa infection [127]. The researchers also measured lung permeability and found no effects of n-3 PUFAs on this endpoint. In another study, n-3 PUFAs reduced the frequency of PMNs and lowered IL-6 levels in male cystic fibrosis transmembrane conductance regulator (Cftr)-null mice in response to P. aeruginosa infection [128]. The same study also reported some gender differences by demonstrating that infected female Cftr-null mice had improved mortality, lung permeability, and IL-6 levels [128]. With S. pneumoniae infection in mice, n-3 PUFAs improved both inflammatory markers in lung homogenates and bacterial loads in the lungs [129–131]. Therefore, these studies suggest a potential beneficial role of long-chain n-3 PUFAs in inflammation associated with infection.
The potential beneficial effects of n-3 PUFAs in pulmonary immunity are not just limited to infection models. DHA specifically improved dust-induced airway inflammation by reducing alveolar PMN infiltration and inflammatory cytokine and chemokine levels relative to those of matching controls [132]. In a mouse model of bleomycin-induced pulmonary inflammation and fibrosis, DHA improved cellular inflammation in BAL, lowered select arachidonic acid-derived mediators, and increased IL-10 secretion [133]. There is even some suggestion that administration of n-3 PUFAs to the pregnant dam may have benefits for offspring. As an example, maternal DHA supplementation improved pulmonary function in newborn murine models of perinatal inflammation [134, 135].
Although some of the aforementioned studies demonstrated that exogenous n-3 PUFA administration has beneficial effects through pleiotropic mechanisms (discussed below), there are some studies that showed negative consequences of select n-3 PUFAs on pulmonary outcomes. For instance, DHA administration to mice in an aerosol ovalbumin model of asthma led to increased levels of eosinophils and IL-6 in BAL fluid, accompanied by high airway resistance [136]. The effects were specific for DHA, given that EPA did not show the same negative effects. In another study, mice consuming high levels of fish oil enriched in n-3 PUFAs had lower lung pathology scores, increased lung viral titers, and decreased survival of influenza A/PuertoRico/8/34 virus infection [137]. The implications of these findings are not clear, given that a more recent study has shown that the SPM 17-HDHA synthesized from DHA improves mouse survival upon live influenza infection by enhancing antibody production by CD138+ plasma cells [138]. Similarly, the SPM protectin D1 synthesized from DHA inhibited lung viral replication with H5N1 infection [139]. Perhaps there is an optimal amount of tissue n-3 PUFA concentration that is necessary for improving pulmonary outcomes and excess levels of n-3 PUFAs or perhaps even deficiencies lead to deleterious effects. Moreover, it is possible that excessive oxidation of n-3 PUFA acyl chains of PLs render cellular damage that contributes to excessive inflammation.
The efficacy of n-3 PUFAs at the clinical level is under investigation. In a randomized controlled trial, Hecker et al. [140] showed that BAL fluid from individuals that inhaled LPS and were given n-3 PUFAs showed decreased proinflammatory cytokines from PMNs and monocytes compared to controls. In another study, n-3 PUFA supplementation improved fractional exhaled NO, a marker of airway inflammation, in healthy men [141]. A review of observational studies between n-3 PUFAs and COPD revealed no strong relationship for improved prevalence and severity of outcomes in COPD [142]. On the other hand, there are data to suggest a correlation between serum inflammatory markers in COPD and short-chain n-3 PUFA levels [143]. Clinical trials of parenteral administration of n-3 PUFA-containing fish oil emulsions in acute lung injury have also been largely negative [144–146].
Cellular and molecular mechanisms by which n-3 PUFAs improve lung homeostasis
Mechanisms of n-3 PUFAs in the context of pulmonary infection and inflammation at the clinical and basic science levels have not been extensively investigated. Thus, we review what is known about the general cellular and molecular mechanisms of n-3 PUFAs and their potential involvement in modulating lung pathology (Fig. 2). At the cellular level, innate responses such as DC activation are generally suppressed by n-3 PUFAs. A series of studies in cell culture and mouse models have demonstrated that EPA and DHA diminish LPS-induced upregulation of surface molecules such as CD80, CD86, and MHCII. As a consequence, DC cytokine secretion and activation of naïve CD4+ T cells is suppressed by n-3 PUFAs [147–149]. Macrophage activation, in the context of obesity, has also been shown to be suppressed by DHA [150]. Less is known about PMN responses, with a recent study suggesting that high levels of n-3 PUFAs promote PMN activation [151]. Thus, the steady-state frequency and function of innate cells involved in pulmonary responses may be influenced by n-3 PUFAs. In one study, n-3 PUFA administration suppressed PMN infiltration in lung tissue of mice with polymicrobial sepsis [152].
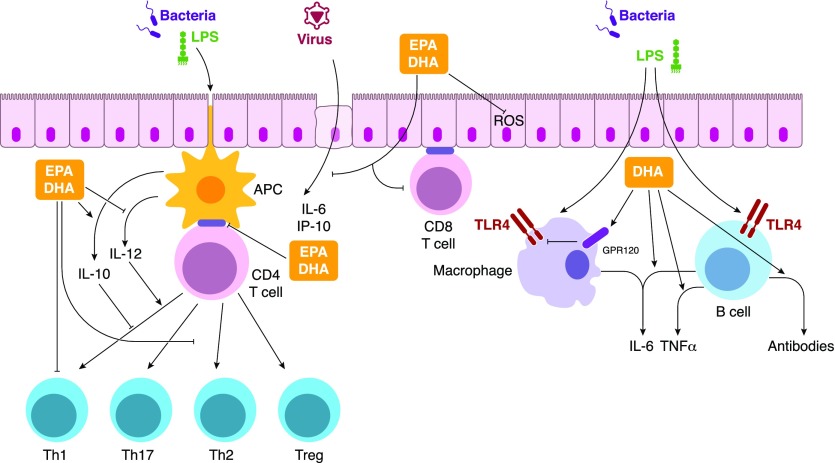
Figure 2. Potential mechanisms by which the long-chain n-3 PUFAs EPA and DHA target innate and adaptive immunity in pulmonary inflammation.
EPA and DHA target receptors such as GPR120 and TLR4, potentially through modification of lipid raft architecture, to influence key immune responses. These responses range from inhibition of APC–T cell synapse formation and suppression of inflammatory cytokines to the initiation of antibody production. Key roles for EPA and DHA remain elusive—particularly the relationship between generation of specialized proresolving lipid mediators (not depicted for simplicity) in response to exogenous EPA and DHA levels, to aid in the resolution of inflammation.
Adaptive immunity is also modulated by n-3 PUFAs (Fig. 2). n-3 PUFAs boost B-cell activation and antibody production in response to ex vivo or in vivo stimulation [153]. They generally suppress Th1/Th17 activation through direct effects on CD4+ T cells or indirectly through dampening of Ag presentation by APCs through MHCII [154–157]. The improved inflammatory outcome in the lung after n-3 PUFA intervention was reported to be accompanied by a lower percentage of Th1/Th17 cells in circulation and a higher Th1:Th2 ratio in circulation in a model of sepsis [152].
The effect of n-3 PUFA intervention on Th2 cytokines remains unclear and may be of key importance, as it relates to lung inflammation. Some studies have shown that Th2 cytokines are elevated by n-3 PUFAs, whereas others show the opposite [158]. IL-5 secretion has been shown to be elevated by n-3 PUFAs in 2 different mouse strains [159]. In another study, n-3 PUFAs increased IL-5 and -13 while lowering oxidative stress, as measured by the levels of F-isoprostanes in mice stimulated with ovalbumin to promote lung inflammation [160]. Still, others have shown that Th2 cytokines are dampened by n-3 PUFAs in the ovalbumin model, improving lung inflammation [161]. The differences between studies are likely attributable to the variable sources of n-3 PUFAs, doses, and timing of intervention. More studies are needed to establish how specific levels of n-3 PUFAs in lung tissue influence Th2 cytokines.
At a molecular level, n-3 PUFAs target innate and adaptive immunity through multiple overlapping mechanisms (Fig. 2). A key target is the plasma membrane, and several studies have highlighted how incorporation of n-3 PUFAs into membrane PLs can lead to immunomodulatory effects. To exemplify, DHA acyl chains of plasma membrane PLs restrict the appropriate geometry of key molecules within the immunologic synapse such as MHCII, the T cell receptor, and cytoskeletal components to inhibit downstream gene expression and proliferation of Th1 cells [157, 162–164]. The effects at the level of the membrane are not just driven by changes in lipid raft architecture but also by direct targeting of receptors. For instance, DHA suppresses macrophage activation through targeting GPR-120, which suppresses the downstream signaling pathways through JNK and NF-κB [150]. Overall, little is known about the role of biophysical plasma membrane lipid–protein distribution and GPR-120 in lung inflammation.
Downstream of the plasma membrane, n-3 PUFAs target cellular signaling pathways that converge on multiple targets, thereby influencing gene expression and cell fate. A few studies have begun to demonstrate the relevance of n-3 PUFA-regulated signaling to lung pathology. For example, DHA dampens apoptosis in the lungs associated with chronic inflammation [165]. EPA is reported to improve lung inflammation by inhibiting ROS signaling. In human bronchial epithelial cells, EPA lowered NADPH oxidase activity and ROS [166]. n-3 PUFAs can also directly target the expression of surface molecules, which is most likely driven by effects at the level of gene expression. For example, docosapentaenoic acid (22:5, n-3), the elongation production of EPA, decreases matrix metalloproteinase-2 and -9 and VEGF expression levels in lung tissue homogenates in experimental pulmonary rat hypertension [167]. These effects were driven by a decrease in p38 MAPK activation and NF-κB translocation.
One mechanism of n-3 PUFAs that has received scant attention in research is PUFA–gene interactions. The effects of n-3 PUFAs are likely to vary between individuals because of differences in genetic variations of key enzymes involved in PUFA biosynthesis and metabolism [168]. For instance, genetic variants in the fatty acid desaturase cluster (a key enzymatic step in PUFA metabolism) may be responsible for differences in n-3 PUFA levels between individuals of African and European descent [169]. Therefore, extensive studies on PUFA–gene interactions are needed in the context of lung pathology, to effectively translate n-3 PUFAs to clinical trials.
A final mechanism of high relevance is the generation of SPMs from n-3 PUFAs. As discussed earlier, SPMs are potent molecules that aid in the resolution of inflammation. Several studies have demonstrated the impact of SPMs in pulmonary inflammation. For instance, resolvin D1, synthesized from DHA, lowers lung inflammation in a model of cigarette smoking [170]. However, it remains unclear whether pharmacologic intake of EPA or DHA, respectively, leads to increased levels of E- and D-series SPMs in vivo. Some studies have shown that n-3 PUFAs given to humans can lead to increased levels of SPMs, although other studies have questioned this assumption [171, 172]. Given this discrepancy, the degree to which n-3 PUFAs affect inflammation and immunity in vivo through SPM generation vs. through SPM-independent mechanisms remains unclear. Taken together, the link between intake of n-3 PUFAs and SPMs requires more attention, especially in the context of lung tissues.
CONCLUDING REMARKS
Lipids are a broad class of molecules that have a range of roles in regulating lung inflammation in response to injury. PL homeostasis, cholesterol homeostasis, and n-3 PUFA metabolism are central examples of how lipids and their dynamic interaction with environmental factors in the lung influence the myriad of responses in innate and adaptive immunity. Connecting the mechanisms by which these lipid classes crosstalk to influence the targeting of receptors and downstream signaling in the lung will be centrally important in the development of new therapeutics for pulmonary disease. With the incidence of lung diseases on the rise, it is essential to understand how these mediators, singly and in combination, modify the pulmonary immune response and whether there are therapeutic opportunities for manipulating the levels of bioactive lipids in the lung during respiratory infection.
AUTHORSHIP
S.R.S. contributed expertise, drafted the n-3 PUFA section, and helped edit and proof the manuscript; M.B.F. contributed expertise, drafted the cholesterol section, helped edit and proof the manuscript, and provided both figures; and K.M.G. contributed expertise, drafted the introduction and the oxPL section, and helped organize, edit, and proof the manuscript.
ACKNOWLEDGMENTS
This work was supported in part by the U.S. National Institutes of Health (NIH), National Institute of Environmental Health Sciences (NIH/NIEHS) Grant Z01 ES102005 (to MBF), and NIH, National Institute of Complementary and Integrative Health Grant R01AT008375 (to SRS), and a Health Effects Institute Walter Rosenblith Award (to KMG). The authors thank Dr. William Guesdon (ECU) for help with literature searches and Lois Wyrick (NIH/NIEHS) for assistance with drafting the figures.
Glossary
- 7α,25-OHC
7α,25-dihydroxycholesterol
- 25HC
25-hydroxycholesterol
- AM
alveolar macrophage
- BAL
bronchoalveolar lavage
- CD
cluster of differentiation
- Cdc
cell division control protein
- Ch25h
cholesterol-25-hydroxylase
- COPD
chronic obstructive pulmonary disease
- CTL
cytotoxic T
- CXCL
C-X-C motif ligand, CYP27A1, cytochrome P450, family 27, subfamily A, polypeptide 1
- DAMP
danger-associated molecular pattern
- DC
dendritic cell
- DHA
docosahexaenoic acid
- Ebi2
Epstein-Barr virus–induced gene 2
- EPA
eicosapentaenoic acid, matrix metalloproteinase
- MyD88
myeloid differentiation primary response gene 88
- oxPAPC
oxidized 1-palmitoyl-2-arachidonyl-sn-glycero-3-phosphorylcholine
- oxPL
oxidized phospholipids
- PAMP
pathogen-associated molecular patterns
- PL
phospholipid
- PMN
polymorphonuclear leukocytes
- PRRs
pattern-recognition receptors
- PUFAs
n-3 polyunsaturated fatty acids
- ROR
retinoic acid receptor-related orphan nuclear receptor
- ROS
reactive oxygen species
- SP
surfactant protein
- SPM
specialized pro-resolving lipid mediators
- SR
scavenger receptor
- TRIF
Toll/IL-1R (TIR)-domain–containing adapter-inducing IFN-β
DISCLOSURES
The authors declare no conflicts of interest.
REFERENCES
- 1.Vos T., Flaxman A. D., Naghavi M., Lozano R., Michaud C., Ezzati M., Shibuya K., Salomon J. A., Abdalla S., Aboyans V., Abraham J., Ackerman I., Aggarwal R., Ahn S. Y., Ali M. K., Alvarado M., Anderson H. R., Anderson L. M., Andrews K. G., Atkinson C., Baddour L. M., Bahalim A. N., Barker-Collo S., Barrero L. H., Bartels D. H., Basáñez M. G., Baxter A., Bell M. L., Benjamin E. J., Bennett D., Bernabé E., Bhalla K., Bhandari B., Bikbov B., Bin Abdulhak A., Birbeck G., Black J. A., Blencowe H., Blore J. D., Blyth F., Bolliger I., Bonaventure A., Boufous S., Bourne R., Boussinesq M., Braithwaite T., Brayne C., Bridgett L., Brooker S., Brooks P., Brugha T. S., Bryan-Hancock C., Bucello C., Buchbinder R., Buckle G., Budke C. M., Burch M., Burney P., Burstein R., Calabria B., Campbell B., Canter C. E., Carabin H., Carapetis J., Carmona L., Cella C., Charlson F., Chen H., Cheng A. T., Chou D., Chugh S. S., Coffeng L. E., Colan S. D., Colquhoun S., Colson K. E., Condon J., Connor M. D., Cooper L. T., Corriere M., Cortinovis M., de Vaccaro K. C., Couser W., Cowie B. C., Criqui M. H., Cross M., Dabhadkar K. C., Dahiya M., Dahodwala N., Damsere-Derry J., Danaei G., Davis A., De Leo D., Degenhardt L., Dellavalle R., Delossantos A., Denenberg J., Derrett S., Des Jarlais D. C., Dharmaratne S. D., Dherani M., Diaz-Torne C., Dolk H., Dorsey E. R., Driscoll T., Duber H., Ebel B., Edmond K., Elbaz A., Ali S. E., Erskine H., Erwin P. J., Espindola P., Ewoigbokhan S. E., Farzadfar F., Feigin V., Felson D. T., Ferrari A., Ferri C. P., Fèvre E. M., Finucane M. M., Flaxman S., Flood L., Foreman K., Forouzanfar M. H., Fowkes F. G., Franklin R., Fransen M., Freeman M. K., Gabbe B. J., Gabriel S. E., Gakidou E., Ganatra H. A., Garcia B., Gaspari F., Gillum R. F., Gmel G., Gosselin R., Grainger R., Groeger J., Guillemin F., Gunnell D., Gupta R., Haagsma J., Hagan H., Halasa Y. A., Hall W., Haring D., Haro J. M., Harrison J. E., Havmoeller R., Hay R. J., Higashi H., Hill C., Hoen B., Hoffman H., Hotez P. J., Hoy D., Huang J. J., Ibeanusi S. E., Jacobsen K. H., James S. L., Jarvis D., Jasrasaria R., Jayaraman S., Johns N., Jonas J. B., Karthikeyan G., Kassebaum N., Kawakami N., Keren A., Khoo J. P., King C. H., Knowlton L. M., Kobusingye O., Koranteng A., Krishnamurthi R., Lalloo R., Laslett L. L., Lathlean T., Leasher J. L., Lee Y. Y., Leigh J., Lim S. S., Limb E., Lin J. K., Lipnick M., Lipshultz S. E., Liu W., Loane M., Ohno S. L., Lyons R., Ma J., Mabweijano J., MacIntyre M. F., Malekzadeh R., Mallinger L., Manivannan S., Marcenes W., March L., Margolis D. J., Marks G. B., Marks R., Matsumori A., Matzopoulos R., Mayosi B. M., McAnulty J. H., McDermott M. M., McGill N., McGrath J., Medina-Mora M. E., Meltzer M., Mensah G. A., Merriman T. R., Meyer A. C., Miglioli V., Miller M., Miller T. R., Mitchell P. B., Mocumbi A. O., Moffitt T. E., Mokdad A. A., Monasta L., Montico M., Moradi-Lakeh M., Moran A., Morawska L., Mori R., Murdoch M. E., Mwaniki M. K., Naidoo K., Nair M. N., Naldi L., Narayan K. M., Nelson P. K., Nelson R. G., Nevitt M. C., Newton C. R., Nolte S., Norman P., Norman R., O’Donnell M., O’Hanlon S., Olives C., Omer S. B., Ortblad K., Osborne R., Ozgediz D., Page A., Pahari B., Pandian J. D., Rivero A. P., Patten S. B., Pearce N., Padilla R. P., Perez-Ruiz F., Perico N., Pesudovs K., Phillips D., Phillips M. R., Pierce K., Pion S., Polanczyk G. V., Polinder S., Pope C. A. III, Popova S., Porrini E., Pourmalek F., Prince M., Pullan R. L., Ramaiah K. D., Ranganathan D., Razavi H., Regan M., Rehm J. T., Rein D. B., Remuzzi G., Richardson K., Rivara F. P., Roberts T., Robinson C., De Leòn F. R., Ronfani L., Room R., Rosenfeld L. C., Rushton L., Sacco R. L., Saha S., Sampson U., Sanchez-Riera L., Sanman E., Schwebel D. C., Scott J. G., Segui-Gomez M., Shahraz S., Shepard D. S., Shin H., Shivakoti R., Singh D., Singh G. M., Singh J. A., Singleton J., Sleet D. A., Sliwa K., Smith E., Smith J. L., Stapelberg N. J., Steer A., Steiner T., Stolk W. A., Stovner L. J., Sudfeld C., Syed S., Tamburlini G., Tavakkoli M., Taylor H. R., Taylor J. A., Taylor W. J., Thomas B., Thomson W. M., Thurston G. D., Tleyjeh I. M., Tonelli M., Towbin J. A., Truelsen T., Tsilimbaris M. K., Ubeda C., Undurraga E. A., van der Werf M. J., van Os J., Vavilala M. S., Venketasubramanian N., Wang M., Wang W., Watt K., Weatherall D. J., Weinstock M. A., Weintraub R., Weisskopf M. G., Weissman M. M., White R. A., Whiteford H., Wiersma S. T., Wilkinson J. D., Williams H. C., Williams S. R., Witt E., Wolfe F., Woolf A. D., Wulf S., Yeh P. H., Zaidi A. K., Zheng Z. J., Zonies D., Lopez A. D., Murray C. J., AlMazroa M. A., Memish Z. A. (2012) Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2163–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Child Health Epidemiology Reference Group of WHO and UNICEF (2012) Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 379, 2151–2161. [DOI] [PubMed] [Google Scholar]
- 3.Mizgerd J. P. (2012) Respiratory infection and the impact of pulmonary immunity on lung health and disease. Am. J. Respir. Crit. Care Med. 186, 824–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.European Study Group (1993) Monotherapy in serious hospital-acquired infections: a clinical trial of ceftazidime versus imipenem/cilastatin. J. Antimicrob. Chemother. 31, 927–937. [DOI] [PubMed] [Google Scholar]
- 5.Jaccard C., Troillet N., Harbarth S., Zanetti G., Aymon D., Schneider R., Chiolero R., Ricou B., Romand J., Huber O., Ambrosetti P., Praz G., Lew D., Bille J., Glauser M. P., Cometta A. (1998) Prospective randomized comparison of imipenem-cilastatin and piperacillin-tazobactam in nosocomial pneumonia or peritonitis. Antimicrob. Agents Chemother. 42, 2966–2972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Severe Pneumonia Study Group (1994) Treatment of severe pneumonia in hospitalized patients: results of a multicenter, randomized, double-blind trial comparing intravenous ciprofloxacin with imipenem-cilastatin. Antimicrob. Agents Chemother. 38, 547–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Woodland D. L., Randall T. D. (2004) Anatomical features of anti-viral immunity in the respiratory tract. Semin. Immunol. 16, 163–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martin T. R., Frevert C. W. (2005) Innate immunity in the lungs. Proc. Am. Thorac. Soc. 2, 403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whitsett J. A., Alenghat T. (2015) Respiratory epithelial cells orchestrate pulmonary innate immunity. Nat. Immunol. 16, 27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kreda S. M., Davis C. W., Rose M. C. (2012) CFTR, mucins, and mucus obstruction in cystic fibrosis. Cold Spring Harb. Perspect. Med. 2, a009589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Voynow J. A., Rubin B. K. (2009) Mucins, mucus, and sputum. Chest 135, 505–512. [DOI] [PubMed] [Google Scholar]
- 12.Whitsett J. A., Wert S. E., Weaver T. E. (2010) Alveolar surfactant homeostasis and the pathogenesis of pulmonary disease. Annu. Rev. Med. 61, 105–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hartshorn K. L. (2010) Role of surfactant protein A and D (SP-A and SP-D) in human antiviral host defense. Front. Biosci. (Schol. Ed.) 2, 527–546. [DOI] [PubMed] [Google Scholar]
- 14.Ariki S., Nishitani C., Kuroki Y. (2012) Diverse functions of pulmonary collectins in host defense of the lung. J. Biomed. Biotechnol. 2012, 532071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Numata M., Chu H. W., Dakhama A., Voelker D. R. (2010) Pulmonary surfactant phosphatidylglycerol inhibits respiratory syncytial virus-induced inflammation and infection. Proc. Natl. Acad. Sci. USA 107, 320–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lambrecht B. N., Hammad H. (2012) The airway epithelium in asthma. Nat. Med. 18, 684–692. [DOI] [PubMed] [Google Scholar]
- 17.Werner J. L., Steele C. (2014) Innate receptors and cellular defense against pulmonary infections. J. Immunol. 193, 3842–3850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rijneveld A. W., Florquin S., Branger J., Speelman P., Van Deventer S. J., van der Poll T. (2001) TNF-alpha compensates for the impaired host defense of IL-1 type I receptor-deficient mice during pneumococcal pneumonia. J. Immunol. 167, 5240–5246. [DOI] [PubMed] [Google Scholar]
- 19.Parker D., Prince A. (2011) Innate immunity in the respiratory epithelium. Am. J. Respir. Cell Mol. Biol. 45, 189–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vareille M., Kieninger E., Edwards M. R., Regamey N. (2011) The airway epithelium: soldier in the fight against respiratory viruses. Clin. Microbiol. Rev. 24, 210–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ivashkiv L. B., Donlin L. T. (2014) Regulation of type I interferon responses. Nat. Rev. Immunol. 14, 36–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guilliams M., Lambrecht B. N., Hammad H. (2013) Division of labor between lung dendritic cells and macrophages in the defense against pulmonary infections. Mucosal Immunol. 6, 464–473. [DOI] [PubMed] [Google Scholar]
- 23.Legge K. L., Braciale T. J. (2003) Accelerated migration of respiratory dendritic cells to the regional lymph nodes is limited to the early phase of pulmonary infection. Immunity 18, 265–277. [DOI] [PubMed] [Google Scholar]
- 24.Legge K. L., Braciale T. J. (2005) Lymph node dendritic cells control CD8+ T cell responses through regulated FasL expression. Immunity 23, 649–659. [DOI] [PubMed] [Google Scholar]
- 25.Hussell T., Bell T. J. (2014) Alveolar macrophages: plasticity in a tissue-specific context. Nat. Rev. Immunol. 14, 81–93. [DOI] [PubMed] [Google Scholar]
- 26.Lambrecht B. N., Hammad H. (2012) Lung dendritic cells in respiratory viral infection and asthma: from protection to immunopathology. Annu. Rev. Immunol. 30, 243–270. [DOI] [PubMed] [Google Scholar]
- 27.O’Brien D. P., Briles D. E., Szalai A. J., Tu A. H., Sanz I., Nahm M. H. (1999) Tumor necrosis factor alpha receptor I is important for survival from Streptococcus pneumoniae infections. Infect. Immun. 67, 595–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mircescu M. M., Lipuma L., van Rooijen N., Pamer E. G., Hohl T. M. (2009) Essential role for neutrophils but not alveolar macrophages at early time points following Aspergillus fumigatus infection. J. Infect. Dis. 200, 647–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moreno G., Errea A., Van Maele L., Roberts R., Léger H., Sirard J. C., Benecke A., Rumbo M., Hozbor D. (2013) Toll-like receptor 4 orchestrates neutrophil recruitment into airways during the first hours of Bordetella pertussis infection. Microbes Infect. 15, 708–718. [DOI] [PubMed] [Google Scholar]
- 30.Young R. L., Malcolm K. C., Kret J. E., Caceres S. M., Poch K. R., Nichols D. P., Taylor-Cousar J. L., Saavedra M. T., Randell S. H., Vasil M. L., Burns J. L., Moskowitz S. M., Nick J. A. (2011) Neutrophil extracellular trap (NET)-mediated killing of Pseudomonas aeruginosa: evidence of acquired resistance within the CF airway, independent of CFTR. PLoS One 6, e23637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hahn I., Klaus A., Janze A. K., Steinwede K., Ding N., Bohling J., Brumshagen C., Serrano H., Gauthier F., Paton J. C., Welte T., Maus U. A. (2011) Cathepsin G and neutrophil elastase play critical and nonredundant roles in lung-protective immunity against Streptococcus pneumoniae in mice. Infect. Immun. 79, 4893–4901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cai S., Batra S., Lira S. A., Kolls J. K., Jeyaseelan S. (2010) CXCL1 regulates pulmonary host defense to Klebsiella infection via CXCL2, CXCL5, NF-kappaB, and MAPKs. J. Immunol. 185, 6214–6225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cowburn A. S., Condliffe A. M., Farahi N., Summers C., Chilvers E. R. (2008) Advances in neutrophil biology: clinical implications. Chest 134, 606–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hahn S., Giaglis S., Chowdhury C. S., Hösli I., Hasler P. (2013) Modulation of neutrophil NETosis: interplay between infectious agents and underlying host physiology. Semin. Immunopathol. 35, 439–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grégoire C., Chasson L., Luci C., Tomasello E., Geissmann F., Vivier E., Walzer T. (2007) The trafficking of natural killer cells. Immunol. Rev. 220, 169–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stein-Streilein J., Bennett M., Mann D., Kumar V. (1983) Natural killer cells in mouse lung: surface phenotype, target preference, and response to local influenza virus infection. J. Immunol. 131, 2699–2704. [PubMed] [Google Scholar]
- 37.Reynolds C. W., Timonen T., Herberman R. B. (1981) Natural killer (NK) cell activity in the rat. I. Isolation and characterization of the effector cells. J. Immunol. 127, 282–287. [PubMed] [Google Scholar]
- 38.Culley F. J. (2009) Natural killer cells in infection and inflammation of the lung. Immunology 128, 151–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sica A., Mantovani A. (2012) Macrophage plasticity and polarization: in vivo veritas. J. Clin. Invest. 122, 787–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mantovani A., Biswas S. K., Galdiero M. R., Sica A., Locati M. (2013) Macrophage plasticity and polarization in tissue repair and remodelling. J. Pathol. 229, 176–185. [DOI] [PubMed] [Google Scholar]
- 41.Murray P. J., Wynn T. A. (2011) Protective and pathogenic functions of macrophage subsets. Nat. Rev. Immunol. 11, 723–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Murray P. J., Allen J. E., Biswas S. K., Fisher E. A., Gilroy D. W., Goerdt S., Gordon S., Hamilton J. A., Ivashkiv L. B., Lawrence T., Locati M., Mantovani A., Martinez F. O., Mege J. L., Mosser D. M., Natoli G., Saeij J. P., Schultze J. L., Shirey K. A., Sica A., Suttles J., Udalova I., van Ginderachter J. A., Vogel S. N., Wynn T. A. (2014) Macrophage activation and polarization: nomenclature and experimental guidelines. [Published correction in Immunity (2014) 41, 339–340.] Immunity 41, 14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martinez F. O., Gordon S. (2014) The M1 and M2 paradigm of macrophage activation: time for reassessment. F1000Prime Rep. 6, 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Braciale T. J., Sun J., Kim T. S. (2012) Regulating the adaptive immune response to respiratory virus infection. Nat. Rev. Immunol. 12, 295–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Doherty P. C., Topham D. J., Tripp R. A., Cardin R. D., Brooks J. W., Stevenson P. G. (1997) Effector CD4+ and CD8+ T-cell mechanisms in the control of respiratory virus infections. Immunol. Rev. 159, 105–117. [DOI] [PubMed] [Google Scholar]
- 46.Wells M. A., Albrecht P., Ennis F. A. (1981) Recovery from a viral respiratory infection. I. Influenza pneumonia in normal and T-deficient mice. J. Immunol. 126, 1036–1041. [PubMed] [Google Scholar]
- 47.Topham D. J., Tripp R. A., Doherty P. C. (1997) CD8+ T cells clear influenza virus by perforin or Fas-dependent processes. J. Immunol. 159, 5197–5200. [PubMed] [Google Scholar]
- 48.Chen K., Kolls J. K. (2013) T cell-mediated host immune defenses in the lung. Annu. Rev. Immunol. 31, 605–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Van Panhuys N., Klauschen F., Germain R. N. (2014) T-cell-receptor-dependent signal intensity dominantly controls CD4(+) T cell polarization In Vivo. Immunity 41, 63–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Berard M., Tough D. F. (2002) Qualitative differences between naïve and memory T cells. Immunology 106, 127–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cerwenka A., Morgan T. M., Dutton R. W. (1999) Naive, effector, and memory CD8 T cells in protection against pulmonary influenza virus infection: homing properties rather than initial frequencies are crucial. J. Immunol. 163, 5535–5543. [PubMed] [Google Scholar]
- 52.Hufford M. M., Kim T. S., Sun J., Braciale T. J. (2015) The effector T cell response to influenza infection. Curr. Top. Microbiol. Immunol. 386, 423–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ouyang Q., Wagner W. M., Voehringer D., Wikby A., Klatt T., Walter S., Müller C. A., Pircher H., Pawelec G. (2003) Age-associated accumulation of CMV-specific CD8+ T cells expressing the inhibitory killer cell lectin-like receptor G1 (KLRG1). Exp. Gerontol. 38, 911–920. [DOI] [PubMed] [Google Scholar]
- 54.Snyder C. M., Cho K. S., Bonnett E. L., van Dommelen S., Shellam G. R., Hill A. B. (2008) Memory inflation during chronic viral infection is maintained by continuous production of short-lived, functional T cells. Immunity 29, 650–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gattinoni L., Lugli E., Ji Y., Pos Z., Paulos C. M., Quigley M. F., Almeida J. R., Gostick E., Yu Z., Carpenito C., Wang E., Douek D. C., Price D. A., June C. H., Marincola F. M., Roederer M., Restifo N. P. (2011) A human memory T cell subset with stem cell-like properties. Nat. Med. 17, 1290–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Masopust D., Picker L. J. (2012) Hidden memories: frontline memory T cells and early pathogen interception. J. Immunol. 188, 5811–5817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Baumgarth N. (2011) The double life of a B-1 cell: self-reactivity selects for protective effector functions. Nat. Rev. Immunol. 11, 34–46. [DOI] [PubMed] [Google Scholar]
- 58.Choi Y. S., Dieter J. A., Rothaeusler K., Luo Z., Baumgarth N. (2012) B-1 cells in the bone marrow are a significant source of natural IgM. Eur. J. Immunol. 42, 120–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Notarangelo L. D. (2010) Primary immunodeficiencies. J. Allergy Clin. Immunol. 125(Suppl 2)S182–S194. [DOI] [PubMed] [Google Scholar]
- 60.Chiu C., Openshaw P. J. (2015) Antiviral B cell and T cell immunity in the lungs. Nat. Immunol. 16, 18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rodriguez Capote K., McCormack F. X., Possmayer F. (2003) Pulmonary surfactant protein-A (SP-A) restores the surface properties of surfactant after oxidation by a mechanism that requires the Cys6 interchain disulfide bond and the phospholipid binding domain. J. Biol. Chem. 278, 20461–20474. [DOI] [PubMed] [Google Scholar]
- 62.Veldhuizen R., Nag K., Orgeig S., Possmayer F. (1998) The role of lipids in pulmonary surfactant. Biochim. Biophys. Acta 1408, 90–108. [DOI] [PubMed] [Google Scholar]
- 63.Miller Y. I., Choi S. H., Wiesner P., Fang L., Harkewicz R., Hartvigsen K., Boullier A., Gonen A., Diehl C. J., Que X., Montano E., Shaw P. X., Tsimikas S., Binder C. J., Witztum J. L. (2011) Oxidation-specific epitopes are danger-associated molecular patterns recognized by pattern recognition receptors of innate immunity. Circ. Res. 108, 235–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Weismann D., Binder C. J. (2012) The innate immune response to products of phospholipid peroxidation. Biochim. Biophys. Acta 1818, 2465–2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bochkov V. N., Oskolkova O. V., Birukov K. G., Levonen A. L., Binder C. J., Stöckl J. (2010) Generation and biological activities of oxidized phospholipids. Antioxid. Redox Signal. 12, 1009–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hampton M. B., Kettle A. J., Winterbourn C. C. (1998) Inside the neutrophil phagosome: oxidants, myeloperoxidase, and bacterial killing. Blood 92, 3007–3017. [PubMed] [Google Scholar]
- 67.Babior B. M. (2000) Phagocytes and oxidative stress. Am. J. Med. 109, 33–44. [DOI] [PubMed] [Google Scholar]
- 68.Zhang R., Shen Z., Nauseef W. M., Hazen S. L. (2002) Defects in leukocyte-mediated initiation of lipid peroxidation in plasma as studied in myeloperoxidase-deficient subjects: systematic identification of multiple endogenous diffusible substrates for myeloperoxidase in plasma. Blood 99, 1802–1810. [PubMed] [Google Scholar]
- 69.Gillotte-Taylor K., Boullier A., Witztum J. L., Steinberg D., Quehenberger O. (2001) Scavenger receptor class B type I as a receptor for oxidized low density lipoprotein. J. Lipid Res. 42, 1474–1482. [PubMed] [Google Scholar]
- 70.Boullier A., Friedman P., Harkewicz R., Hartvigsen K., Green S. R., Almazan F., Dennis E. A., Steinberg D., Witztum J. L., Quehenberger O. (2005) Phosphocholine as a pattern recognition ligand for CD36. J. Lipid Res. 46, 969–976. [DOI] [PubMed] [Google Scholar]
- 71.Miller Y. I., Viriyakosol S., Worrall D. S., Boullier A., Butler S., Witztum J. L. (2005) Toll-like receptor 4-dependent and -independent cytokine secretion induced by minimally oxidized low-density lipoprotein in macrophages. Arterioscler. Thromb. Vasc. Biol. 25, 1213–1219. [DOI] [PubMed] [Google Scholar]
- 72.Li R., Mouillesseaux K. P., Montoya D., Cruz D., Gharavi N., Dun M., Koroniak L., Berliner J. A. (2006) Identification of prostaglandin E2 receptor subtype 2 as a receptor activated by OxPAPC. Circ. Res. 98, 642–650. [DOI] [PubMed] [Google Scholar]
- 73.Shirey K. A., Lai W., Scott A. J., Lipsky M., Mistry P., Pletneva L. M., Karp C. L., McAlees J., Gioannini T. L., Weiss J., Chen W. H., Ernst R. K., Rossignol D. P., Gusovsky F., Blanco J. C., Vogel S. N. (2013) The TLR4 antagonist Eritoran protects mice from lethal influenza infection. Nature 497, 498–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Van Lenten B. J., Wagner A. C., Navab M., Anantharamaiah G. M., Hui E. K., Nayak D. P., Fogelman A. M. (2004) D-4F, an apolipoprotein A-I mimetic peptide, inhibits the inflammatory response induced by influenza A infection of human type II pneumocytes. Circulation 110, 3252–3258. [DOI] [PubMed] [Google Scholar]
- 75.Imai Y., Kuba K., Neely G. G., Yaghubian-Malhami R., Perkmann T., van Loo G., Ermolaeva M., Veldhuizen R., Leung Y. H., Wang H., Liu H., Sun Y., Pasparakis M., Kopf M., Mech C., Bavari S., Peiris J. S., Slutsky A. S., Akira S., Hultqvist M., Holmdahl R., Nicholls J., Jiang C., Binder C. J., Penninger J. M. (2008) Identification of oxidative stress and Toll-like receptor 4 signaling as a key pathway of acute lung injury. Cell 133, 235–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Walton K. A., Hsieh X., Gharavi N., Wang S., Wang G., Yeh M., Cole A. L., Berliner J. A. (2003) Receptors involved in the oxidized 1-palmitoyl-2-arachidonoyl-sn-glycero-3-phosphorylcholine-mediated synthesis of interleukin-8: a role for Toll-like receptor 4 and a glycosylphosphatidylinositol-anchored protein. J. Biol. Chem. 278, 29661–29666. [DOI] [PubMed] [Google Scholar]
- 77.Erridge C., Kennedy S., Spickett C. M., Webb D. J. (2008) Oxidized phospholipid inhibition of toll-like receptor (TLR) signaling is restricted to TLR2 and TLR4: roles for CD14, LPS-binding protein, and MD2 as targets for specificity of inhibition. J. Biol. Chem. 283, 24748–24759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bochkov V. N., Kadl A., Huber J., Gruber F., Binder B. R., Leitinger N. (2002) Protective role of phospholipid oxidation products in endotoxin-induced tissue damage. Nature 419, 77–81. [DOI] [PubMed] [Google Scholar]
- 79.Ma Z., Li J., Yang L., Mu Y., Xie W., Pitt B., Li S. (2004) Inhibition of LPS- and CpG DNA-induced TNF-alpha response by oxidized phospholipids. Am. J. Physiol. Lung Cell. Mol. Physiol. 286, L808–L816. [DOI] [PubMed] [Google Scholar]
- 80.Kim M. J., Choi N. Y., Koo J. E., Kim S. Y., Joung S. M., Jeong E., Lee J. Y. (2013) Suppression of Toll-like receptor 4 activation by endogenous oxidized phosphatidylcholine, KOdiA-PC by inhibiting LPS binding to MD2. Inflamm. Res. 62, 571–580. [DOI] [PubMed] [Google Scholar]
- 81.Nonas S., Miller I., Kawkitinarong K., Chatchavalvanich S., Gorshkova I., Bochkov V. N., Leitinger N., Natarajan V., Garcia J. G., Birukov K. G. (2006) Oxidized phospholipids reduce vascular leak and inflammation in rat model of acute lung injury. Am. J. Respir. Crit. Care Med. 173, 1130–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Matt U., Sharif O., Martins R., Furtner T., Langeberg L., Gawish R., Elbau I., Zivkovic A., Lakovits K., Oskolkova O., Doninger B., Vychytil A., Perkmann T., Schabbauer G., Binder C. J., Bochkov V. N., Scott J. D., Knapp S. (2013) WAVE1 mediates suppression of phagocytosis by phospholipid-derived DAMPs. J. Clin. Invest. 123, 3014–3024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Blüml S., Rosc B., Lorincz A., Seyerl M., Kirchberger S., Oskolkova O., Bochkov V. N., Majdic O., Ligeti E., Stöckl J. (2008) The oxidation state of phospholipids controls the oxidative burst in neutrophil granulocytes. J. Immunol. 181, 4347–4353. [DOI] [PubMed] [Google Scholar]
- 84.Thimmulappa R. K., Gang X., Kim J. H., Sussan T. E., Witztum J. L., Biswal S. (2012) Oxidized phospholipids impair pulmonary antibacterial defenses: evidence in mice exposed to cigarette smoke. Biochem. Biophys. Res. Commun. 426, 253–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hall A. (2005) Rho GTPases and the control of cell behaviour. Biochem. Soc. Trans. 33, 891–895. [DOI] [PubMed] [Google Scholar]
- 86.Knapp S., Matt U., Leitinger N., van der Poll T. (2007) Oxidized phospholipids inhibit phagocytosis and impair outcome in gram-negative sepsis in vivo. J. Immunol. 178, 993–1001. [DOI] [PubMed] [Google Scholar]
- 87.Blüml S., Kirchberger S., Bochkov V. N., Krönke G., Stuhlmeier K., Majdic O., Zlabinger G. J., Knapp W., Binder B. R., Stöckl J., Leitinger N. (2005) Oxidized phospholipids negatively regulate dendritic cell maturation induced by TLRs and CD40. J. Immunol. 175, 501–508. [DOI] [PubMed] [Google Scholar]
- 88.Blüml S., Zupkovitz G., Kirchberger S., Seyerl M., Bochkov V. N., Stuhlmeier K., Majdic O., Zlabinger G. J., Seiser C., Stöckl J. (2009) Epigenetic regulation of dendritic cell differentiation and function by oxidized phospholipids. Blood 114, 5481–5489. [DOI] [PubMed] [Google Scholar]
- 89.Shamshiev A. T., Ampenberger F., Ernst B., Rohrer L., Marsland B. J., Kopf M. (2007) Dyslipidemia inhibits Toll-like receptor-induced activation of CD8alpha-negative dendritic cells and protective Th1 type immunity. J. Exp. Med. 204, 441–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fessler M. B., Summer R. S. (2016) Surfactant lipids at the host-environment interface: metabolic sensors, suppressors, and effectors of inflammatory lung disease. Am. J. Respir. Cell Mol. Biol. 54, 624–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Turley S. D., Andersen J. M., Dietschy J. M. (1981) Rates of sterol synthesis and uptake in the major organs of the rat in vivo. J. Lipid Res. 22, 551–569. [PubMed] [Google Scholar]
- 92.Baritussio A., Enzi G., Inelmen E. M., Schiavon M., de Biasi F., Allegra L., Ursini F., Baldo G. (1980) Altered surfactant synthesis and function in rats with diet-induced hyperlipidemia. Metabolism 29, 503–510. [DOI] [PubMed] [Google Scholar]
- 93.Draper D. W., Madenspacher J. H., Dixon D., King D. H., Remaley A. T., Fessler M. B. (2010) ATP-binding cassette transporter G1 deficiency dysregulates host defense in the lung. Am. J. Respir. Crit. Care Med. 182, 404–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Basset-Léobon C., Lacoste-Collin L., Aziza J., Bes J. C., Jozan S., Courtade-Saïdi M. (2010) Cut-off values and significance of Oil Red O-positive cells in bronchoalveolar lavage fluid. Cytopathology 21, 245–250. [DOI] [PubMed] [Google Scholar]
- 95.Gowdy K. M., Fessler M. B. (2013) Emerging roles for cholesterol and lipoproteins in lung disease. Pulm. Pharmacol. Ther. 26, 430–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fessler M. B. (2015) Regulation of adaptive immunity in health and disease by cholesterol metabolism. Curr. Allergy Asthma Rep. 15, 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Fessler M. B., Parks J. S. (2011) Intracellular lipid flux and membrane microdomains as organizing principles in inflammatory cell signaling. J. Immunol. 187, 1529–1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gabor K. A., Fessler M. B. (2016) Roles of the mevalonate pathway and cholesterol trafficking in pulmonary host defense. Curr. Mol. Pharmacol. doi: 10.2174/1874467209666160112123603 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Voisset C., Callens N., Blanchard E., Op De Beeck A., Dubuisson J., Vu-Dac N. (2005) High density lipoproteins facilitate hepatitis C virus entry through the scavenger receptor class B type I. J. Biol. Chem. 280, 7793–7799. [DOI] [PubMed] [Google Scholar]
- 100.Côté M., Misasi J., Ren T., Bruchez A., Lee K., Filone C. M., Hensley L., Li Q., Ory D., Chandran K., Cunningham J. (2011) Small molecule inhibitors reveal Niemann-Pick C1 is essential for Ebola virus infection. Nature 477, 344–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Carette J. E., Raaben M., Wong A. C., Herbert A. S., Obernosterer G., Mulherkar N., Kuehne A. I., Kranzusch P. J., Griffin A. M., Ruthel G., Dal Cin P., Dye J. M., Whelan S. P., Chandran K., Brummelkamp T. R. (2011) Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature 477, 340–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Blanc M., Hsieh W. Y., Robertson K. A., Watterson S., Shui G., Lacaze P., Khondoker M., Dickinson P., Sing G., Rodríguez-Martín S., Phelan P., Forster T., Strobl B., Müller M., Riemersma R., Osborne T., Wenk M. R., Angulo A., Ghazal P. (2011) Host defense against viral infection involves interferon mediated down-regulation of sterol biosynthesis. PLoS Biol. 9, e1000598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.York A. G., Williams K. J., Argus J. P., Zhou Q. D., Brar G., Vergnes L., Gray E. E., Zhen A., Wu N. C., Yamada D. H., Cunningham C. R., Tarling E. J., Wilks M. Q., Casero D., Gray D. H., Yu A. K., Wang E. S., Brooks D. G., Sun R., Kitchen S. G., Wu T. T., Reue K., Stetson D. B., Bensinger S. J. (2015) Limiting cholesterol biosynthetic flux spontaneously engages type I IFN signaling. Cell 163, 1716–1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Amini-Bavil-Olyaee S., Choi Y. J., Lee J. H., Shi M., Huang I. C., Farzan M., Jung J. U. (2013) The antiviral effector IFITM3 disrupts intracellular cholesterol homeostasis to block viral entry. [Published correction in Cell Host Microbe (2013), 14, 600–601.] Cell Host Microbe 13, 452–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Pulfer M. K., Murphy R. C. (2004) Formation of biologically active oxysterols during ozonolysis of cholesterol present in lung surfactant. J. Biol. Chem. 279, 26331–26338. [DOI] [PubMed] [Google Scholar]
- 106.Dahl M., Bauer A. K., Arredouani M., Soininen R., Tryggvason K., Kleeberger S. R., Kobzik L. (2007) Protection against inhaled oxidants through scavenging of oxidized lipids by macrophage receptors MARCO and SR-AI/II. J. Clin. Invest. 117, 757–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lund E. G., Kerr T. A., Sakai J., Li W. P., Russell D. W. (1998) cDNA cloning of mouse and human cholesterol 25-hydroxylases, polytopic membrane proteins that synthesize a potent oxysterol regulator of lipid metabolism. J. Biol. Chem. 273, 34316–34327. [DOI] [PubMed] [Google Scholar]
- 108.Babiker A., Andersson O., Lindblom D., van der Linden J., Wiklund B., Lütjohann D., Diczfalusy U., Björkhem I. (1999) Elimination of cholesterol as cholestenoic acid in human lung by sterol 27-hydroxylase: evidence that most of this steroid in the circulation is of pulmonary origin. J. Lipid Res. 40, 1417–1425. [PubMed] [Google Scholar]
- 109.Gold E. S., Diercks A. H., Podolsky I., Podyminogin R. L., Askovich P. S., Treuting P. M., Aderem A. (2014) 25-Hydroxycholesterol acts as an amplifier of inflammatory signaling. Proc. Natl. Acad. Sci. USA 111, 10666–10671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Raccosta L., Fontana R., Maggioni D., Lanterna C., Villablanca E. J., Paniccia A., Musumeci A., Chiricozzi E., Trincavelli M. L., Daniele S., Martini C., Gustafsson J. A., Doglioni C., Feo S. G., Leiva A., Ciampa M. G., Mauri L., Sensi C., Prinetti A., Eberini I., Mora J. R., Bordignon C., Steffensen K. R., Sonnino S., Sozzani S., Traversari C., Russo V. (2013) The oxysterol-CXCR2 axis plays a key role in the recruitment of tumor-promoting neutrophils. J. Exp. Med. 210, 1711–1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Reboldi A., Dang E. V., McDonald J. G., Liang G., Russell D. W., Cyster J. G. (2014) Inflammation. 25-Hydroxycholesterol suppresses interleukin-1-driven inflammation downstream of type I interferon. Science 345, 679–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zelcer N., Tontonoz P. (2006) Liver X receptors as integrators of metabolic and inflammatory signaling. J. Clin. Invest. 116, 607–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bauman D. R., Bitmansour A. D., McDonald J. G., Thompson B. M., Liang G., Russell D. W. (2009) 25-Hydroxycholesterol secreted by macrophages in response to Toll-like receptor activation suppresses immunoglobulin A production. Proc. Natl. Acad. Sci. USA 106, 16764–16769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Liu S. Y., Aliyari R., Chikere K., Li G., Marsden M. D., Smith J. K., Pernet O., Guo H., Nusbaum R., Zack J. A., Freiberg A. N., Su L., Lee B., Cheng G. (2013) Interferon-inducible cholesterol-25-hydroxylase broadly inhibits viral entry by production of 25-hydroxycholesterol. Immunity 38, 92–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Blanc M., Hsieh W. Y., Robertson K. A., Kropp K. A., Forster T., Shui G., Lacaze P., Watterson S., Griffiths S. J., Spann N. J., Meljon A., Talbot S., Krishnan K., Covey D. F., Wenk M. R., Craigon M., Ruzsics Z., Haas J., Angulo A., Griffiths W. J., Glass C. K., Wang Y., Ghazal P. (2013) The transcription factor STAT-1 couples macrophage synthesis of 25-hydroxycholesterol to the interferon antiviral response. Immunity 38, 106–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sugiura H., Koarai A., Ichikawa T., Minakata Y., Matsunaga K., Hirano T., Akamatsu K., Yanagisawa S., Furusawa M., Uno Y., Yamasaki M., Satomi Y., Ichinose M. (2012) Increased 25-hydroxycholesterol concentrations in the lungs of patients with chronic obstructive pulmonary disease. Respirology 17, 533–540. [DOI] [PubMed] [Google Scholar]
- 117.Diczfalusy U., Olofsson K. E., Carlsson A. M., Gong M., Golenbock D. T., Rooyackers O., Fläring U., Björkbacka H. (2009) Marked upregulation of cholesterol 25-hydroxylase expression by lipopolysaccharide. J. Lipid Res. 50, 2258–2264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hannedouche S., Zhang J., Yi T., Shen W., Nguyen D., Pereira J. P., Guerini D., Baumgarten B. U., Roggo S., Wen B., Knochenmuss R., Noël S., Gessier F., Kelly L. M., Vanek M., Laurent S., Preuss I., Miault C., Christen I., Karuna R., Li W., Koo D. I., Suply T., Schmedt C., Peters E. C., Falchetto R., Katopodis A., Spanka C., Roy M. O., Detheux M., Chen Y. A., Schultz P. G., Cho C. Y., Seuwen K., Cyster J. G., Sailer A. W. (2011) Oxysterols direct immune cell migration via EBI2. Nature 475, 524–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Liu C., Yang X. V., Wu J., Kuei C., Mani N. S., Zhang L., Yu J., Sutton S. W., Qin N., Banie H., Karlsson L., Sun S., Lovenberg T. W. (2011) Oxysterols direct B-cell migration through EBI2. Nature 475, 519–523. [DOI] [PubMed] [Google Scholar]
- 120.Yi T., Cyster J. G. (2013) EBI2-mediated bridging channel positioning supports splenic dendritic cell homeostasis and particulate antigen capture. eLife 2, e00757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Gatto D., Wood K., Caminschi I., Murphy-Durland D., Schofield P., Christ D., Karupiah G., Brink R. (2013) The chemotactic receptor EBI2 regulates the homeostasis, localization and immunological function of splenic dendritic cells. Nat. Immunol. 14, 446–453. [DOI] [PubMed] [Google Scholar]
- 122.Soroosh P., Wu J., Xue X., Song J., Sutton S. W., Sablad M., Yu J., Nelen M. I., Liu X., Castro G., Luna R., Crawford S., Banie H., Dandridge R. A., Deng X., Bittner A., Kuei C., Tootoonchi M., Rozenkrants N., Herman K., Gao J., Yang X. V., Sachen K., Ngo K., Fung-Leung W. P., Nguyen S., de Leon-Tabaldo A., Blevitt J., Zhang Y., Cummings M. D., Rao T., Mani N. S., Liu C., McKinnon M., Milla M. E., Fourie A. M., Sun S. (2014) Oxysterols are agonist ligands of RORγt and drive Th17 cell differentiation. Proc. Natl. Acad. Sci. USA 111, 12163–12168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Minihane A. M., Vinoy S., Russell W. R., Baka A., Roche H. M., Tuohy K. M., Teeling J. L., Blaak E. E., Fenech M., Vauzour D., McArdle H. J., Kremer B. H., Sterkman L., Vafeiadou K., Benedetti M. M., Williams C. M., Calder P. C. (2015) Low-grade inflammation, diet composition and health: current research evidence and its translation. Br. J. Nutr. 114, 999–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wood K. E., Mantzioris E., Gibson R. A., Ramsden C. E., Muhlhausler B. S. (2015) The effect of modifying dietary LA and ALA intakes on omega-3 long chain polyunsaturated fatty acid (n-3 LCPUFA) status in human adults: a systematic review and commentary. Prostaglandins Leukot. Essent. Fatty Acids 95, 47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Serhan C. N. (2014) Pro-resolving lipid mediators are leads for resolution physiology. Nature 510, 92–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Basil M. C., Levy B. D. (2016) Specialized pro-resolving mediators: endogenous regulators of infection and inflammation. Nat. Rev. Immunol. 16, 51–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Caron E., Desseyn J. L., Sergent L., Bartke N., Husson M. O., Duhamel A., Gottrand F. (2015) Impact of fish oils on the outcomes of a mouse model of acute Pseudomonas aeruginosa pulmonary infection. Br. J. Nutr. 113, 191–199. [DOI] [PubMed] [Google Scholar]
- 128.Tiesset H., Bernard H., Bartke N., Beermann C., Flachaire E., Desseyn J. L., Gottrand F., Husson M. O. (2011) (n-3) long-chain PUFA differentially affect resistance to Pseudomonas aeruginosa infection of male and female cftr−/− mice. J. Nutr. 141, 1101–1107. [DOI] [PubMed] [Google Scholar]
- 129.Saini A., Harjai K., Chhibber S. (2011) Sea-cod oil supplementation alters the course of Streptococcus pneumoniae infection in BALB/c mice. Eur. J. Clin. Microbiol. Infect. Dis. 30, 393–400. [DOI] [PubMed] [Google Scholar]
- 130.Saini A., Harjai K., Mohan H., Punia R. P., Chhibber S. (2010) Long-term flaxseed oil supplementation diet protects BALB/c mice against Streptococcus pneumoniae infection. Med. Microbiol. Immunol. (Berl.) 199, 27–34. [DOI] [PubMed] [Google Scholar]
- 131.Pierre M., Husson M. O., Le Berre R., Desseyn J. L., Galabert C., Béghin L., Beermann C., Dagenais A., Berthiaume Y., Cardinaud B., Barbry P., Gottrand F., Guery B. P. (2007) Omega-3 polyunsaturated fatty acids improve host response in chronic Pseudomonas aeruginosa lung infection in mice. Am. J. Physiol. Lung Cell. Mol. Physiol. 292, L1422–L1431. [DOI] [PubMed] [Google Scholar]
- 132.Nordgren T. M., Friemel T. D., Heires A. J., Poole J. A., Wyatt T. A., Romberger D. J. (2014) The omega-3 fatty acid docosahexaenoic acid attenuates organic dust-induced airway inflammation. Nutrients 6, 5434–5452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zhao H., Chan-Li Y., Collins S. L., Zhang Y., Hallowell R. W., Mitzner W., Horton M. R. (2014) Pulmonary delivery of docosahexaenoic acid mitigates bleomycin-induced pulmonary fibrosis. BMC Pulm. Med. 14, 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Velten M., Britt R. D. Jr., Heyob K. M., Tipple T. E., Rogers L. K. (2014) Maternal dietary docosahexaenoic acid supplementation attenuates fetal growth restriction and enhances pulmonary function in a newborn mouse model of perinatal inflammation. J. Nutr. 144, 258–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Rogers L. K., Valentine C. J., Pennell M., Velten M., Britt R. D., Dingess K., Zhao X., Welty S. E., Tipple T. E. (2011) Maternal docosahexaenoic acid supplementation decreases lung inflammation in hyperoxia-exposed newborn mice. J. Nutr. 141, 214–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Schuster G. U., Bratt J. M., Jiang X., Pedersen T. L., Grapov D., Adkins Y., Kelley D. S., Newman J. W., Kenyon N. J., Stephensen C. B. (2014) Dietary long-chain omega-3 fatty acids do not diminish eosinophilic pulmonary inflammation in mice. Am. J. Respir. Cell Mol. Biol. 50, 626–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Schwerbrock N. M., Karlsson E. A., Shi Q., Sheridan P. A., Beck M. A. (2009) Fish oil-fed mice have impaired resistance to influenza infection. J. Nutr. 139, 1588–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ramon S., Baker S. F., Sahler J. M., Kim N., Feldsott E. A., Serhan C. N., Martínez-Sobrido L., Topham D. J., Phipps R. P. (2014) The specialized proresolving mediator 17-HDHA enhances the antibody-mediated immune response against influenza virus: a new class of adjuvant? J. Immunol. 193, 6031–6040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Morita M., Kuba K., Ichikawa A., Nakayama M., Katahira J., Iwamoto R., Watanebe T., Sakabe S., Daidoji T., Nakamura S., Kadowaki A., Ohto T., Nakanishi H., Taguchi R., Nakaya T., Murakami M., Yoneda Y., Arai H., Kawaoka Y., Penninger J. M., Arita M., Imai Y. (2013) The lipid mediator protectin D1 inhibits influenza virus replication and improves severe influenza. Cell 153, 112–125. [DOI] [PubMed] [Google Scholar]
- 140.Hecker M., Linder T., Ott J., Walmrath H. D., Lohmeyer J., Vadász I., Marsh L. M., Herold S., Reichert M., Buchbinder A., Morty R. E., Bausch B., Fischer T., Schulz R., Grimminger F., Witzenrath M., Barnes M., Seeger W., Mayer K. (2015) Immunomodulation by lipid emulsions in pulmonary inflammation: a randomized controlled trial. Crit. Care 19, 226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ade C. J., Rosenkranz S. K., Harms C. A. (2014) The effects of short-term fish oil supplementation on pulmonary function and airway inflammation following a high-fat meal. Eur. J. Appl. Physiol. 114, 675–682. [DOI] [PubMed] [Google Scholar]
- 142.Fulton A. S., Hill A. M., Williams M. T., Howe P. R., Coates A. M. (2015) Paucity of evidence for a relationship between long-chain omega-3 fatty acid intake and chronic obstructive pulmonary disease: a systematic review. Nutr. Rev. 73, 612–623. [DOI] [PubMed] [Google Scholar]
- 143.PAC-COPD Study Group (2012) Association between Ω3 and Ω6 fatty acid intakes and serum inflammatory markers in COPD. J. Nutr. Biochem. 23, 817–821. [DOI] [PubMed] [Google Scholar]
- 144.Zhu D., Zhang Y., Li S., Gan L., Feng H., Nie W. (2014) Enteral omega-3 fatty acid supplementation in adult patients with acute respiratory distress syndrome: a systematic review of randomized controlled trials with meta-analysis and trial sequential analysis. Intensive Care Med. 40, 504–512. [DOI] [PubMed] [Google Scholar]
- 145.Manzanares W., Dhaliwal R., Jurewitsch B., Stapleton R. D., Jeejeebhoy K. N., Heyland D. K. (2014) Parenteral fish oil lipid emulsions in the critically ill: a systematic review and meta-analysis. JPEN J. Parenter. Enteral Nutr. 38, 20–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Stapleton R. D., Martin T. R., Weiss N. S., Crowley J. J., Gundel S. J., Nathens A. B., Akhtar S. R., Ruzinski J. T., Caldwell E., Curtis J. R., Heyland D. K., Watkins T. R., Parsons P. E., Martin J. M., Wurfel M. M., Hallstrand T. S., Sims K. A., Neff M. J. (2011) A phase II randomized placebo-controlled trial of omega-3 fatty acids for the treatment of acute lung injury. Crit. Care Med. 39, 1655–1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Teague H., Rockett B. D., Harris M., Brown D. A., Shaikh S. R. (2013) Dendritic cell activation, phagocytosis and CD69 expression on cognate T cells are suppressed by n-3 long-chain polyunsaturated fatty acids. Immunology 139, 386–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Draper E., Reynolds C. M., Canavan M., Mills K. H., Loscher C. E., Roche H. M. (2011) Omega-3 fatty acids attenuate dendritic cell function via NF-κB independent of PPARγ. J. Nutr. Biochem. 22, 784–790. [DOI] [PubMed] [Google Scholar]
- 149.Zeyda M., Säemann M. D., Stuhlmeier K. M., Mascher D. G., Nowotny P. N., Zlabinger G. J., Waldhäusl W., Stulnig T. M. (2005) Polyunsaturated fatty acids block dendritic cell activation and function independently of NF-kappaB activation. J. Biol. Chem. 280, 14293–14301. [DOI] [PubMed] [Google Scholar]
- 150.Oh D. Y., Talukdar S., Bae E. J., Imamura T., Morinaga H., Fan W., Li P., Lu W. J., Watkins S. M., Olefsky J. M. (2010) GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell 142, 687–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Duriancik D. M., Comstock S. S., Langohr I. M., Fenton J. I. (2015) High levels of fish oil enhance neutrophil development and activation and influence colon mucus barrier function in a genetically susceptible mouse model. J. Nutr. Biochem. 26, 1261–1272. [DOI] [PubMed] [Google Scholar]
- 152.Chang Y. F., Hou Y. C., Pai M. H., Yeh S. L., Liu J. J. (2015) Effects of ω-3 polyunsaturated fatty acids on the homeostasis of CD4+ T cells and lung injury in mice with polymicrobial sepsis. JPEN J. Parenter. Enteral Nutr. 0148607115597670. [DOI] [PubMed] [Google Scholar]
- 153.Teague H., Harris M., Fenton J., Lallemand P., Shewchuk B. M., Shaikh S. R. (2014) Eicosapentaenoic and docosahexaenoic acid ethyl esters differentially enhance B-cell activity in murine obesity. J. Lipid Res. 55, 1420–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Monk J. M., Hou T. Y., Turk H. F., McMurray D. N., Chapkin R. S. (2013) n3 PUFAs reduce mouse CD4+ T-cell ex vivo polarization into Th17 cells. J. Nutr. 143, 1501–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Rockett B. D., Melton M., Harris M., Bridges L. C., Shaikh S. R. (2013) Fish oil disrupts MHC class II lateral organization on the B-cell side of the immunological synapse independent of B-T cell adhesion. J. Nutr. Biochem. 24, 1810–1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Monk J. M., Hou T. Y., Turk H. F., Weeks B., Wu C., McMurray D. N., Chapkin R. S. (2012) Dietary n-3 polyunsaturated fatty acids (PUFA) decrease obesity-associated Th17 cell-mediated inflammation during colitis. PLoS One 7, e49739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Yog R., Barhoumi R., McMurray D. N., Chapkin R. S. (2010) n-3 polyunsaturated fatty acids suppress mitochondrial translocation to the immunologic synapse and modulate calcium signaling in T cells. J. Immunol. 184, 5865–5873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Petursdottir D. H., Hardardottir I. (2009) Dietary fish oil decreases secretion of T helper (Th) 1-type cytokines by a direct effect on murine splenic T cells but enhances secretion of a Th2-type cytokine by an effect on accessory cells. Br. J. Nutr. 101, 1040–1046. [DOI] [PubMed] [Google Scholar]
- 159.Gurzell E. A., Teague H., Harris M., Clinthorne J., Shaikh S. R., Fenton J. I. (2013) DHA-enriched fish oil targets B cell lipid microdomains and enhances ex vivo and in vivo B cell function. J. Leukoc. Biol. 93, 463–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Yin H., Liu W., Goleniewska K., Porter N. A., Morrow J. D., Peebles R. S. Jr (2009) Dietary supplementation of omega-3 fatty acid-containing fish oil suppresses F2-isoprostanes but enhances inflammatory cytokine response in a mouse model of ovalbumin-induced allergic lung inflammation. Free Radic. Biol. Med. 47, 622–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Jang H. Y., Lim K., Lee S. M., Park B. H. (2014) Effects of n-3 PUFA on the CD4⁺ type 2 helper T-cell-mediated immune responses in Fat-1 mice. Mol. Nutr. Food Res. 58, 365–375. [DOI] [PubMed] [Google Scholar]
- 162.Rockett B. D., Teague H., Harris M., Melton M., Williams J., Wassall S. R., Shaikh S. R. (2012) Fish oil increases raft size and membrane order of B cells accompanied by differential effects on function. J. Lipid Res. 53, 674–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Hou T. Y., Monk J. M., Fan Y. Y., Barhoumi R., Chen Y. Q., Rivera G. M., McMurray D. N., Chapkin R. S. (2012) n-3 polyunsaturated fatty acids suppress phosphatidylinositol 4,5-bisphosphate-dependent actin remodelling during CD4+ T-cell activation. Biochem. J. 443, 27–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Kim W., Fan Y. Y., Barhoumi R., Smith R., McMurray D. N., Chapkin R. S. (2008) n-3 polyunsaturated fatty acids suppress the localization and activation of signaling proteins at the immunological synapse in murine CD4+ T cells by affecting lipid raft formation. J. Immunol. 181, 6236–6243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ali M., Heyob K. M., Velten M., Tipple T. E., Rogers L. K. (2015) DHA suppresses chronic apoptosis in the lung caused by perinatal inflammation. Am. J. Physiol. Lung Cell. Mol. Physiol. 309, L441–L448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Liu M. H., Lin A. H., Lu S. H., Peng R. Y., Lee T. S., Kou Y. R. (2014) Eicosapentaenoic acid attenuates cigarette smoke-induced lung inflammation by inhibiting ROS-sensitive inflammatory signaling. Front. Physiol. 5, 440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Morin C., Hiram R., Rousseau E., Blier P. U., Fortin S. (2014) Docosapentaenoic acid monoacylglyceride reduces inflammation and vascular remodeling in experimental pulmonary hypertension. Am. J. Physiol. Heart Circ. Physiol. 307, H574–H586. [DOI] [PubMed] [Google Scholar]
- 168.Mathias R. A., Pani V., Chilton F. H. (2014) Genetic variants in the FADS gene: implications for dietary recommendations for fatty acid intake. Curr. Nutr. Rep. 3, 139–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Sergeant S., Hugenschmidt C. E., Rudock M. E., Ziegler J. T., Ivester P., Ainsworth H. C., Vaidya D., Case L. D., Langefeld C. D., Freedman B. I., Bowden D. W., Mathias R. A., Chilton F. H. (2012) Differences in arachidonic acid levels and fatty acid desaturase (FADS) gene variants in African Americans and European Americans with diabetes or the metabolic syndrome. Br. J. Nutr. 107, 547–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Hsiao H. M., Sapinoro R. E., Thatcher T. H., Croasdell A., Levy E. P., Fulton R. A., Olsen K. C., Pollock S. J., Serhan C. N., Phipps R. P., Sime P. J. (2013) A novel anti-inflammatory and pro-resolving role for resolvin D1 in acute cigarette smoke-induced lung inflammation. PLoS One 8, e58258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Skarke C., Alamuddin N., Lawson J. A., Li X., Ferguson J. F., Reilly M. P., FitzGerald G. A. (2015) Bioactive products formed in humans from fish oils. J. Lipid Res. 56, 1808–1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Barden A., Mas E., Croft K. D., Phillips M., Mori T. A. (2014) Short-term n-3 fatty acid supplementation but not aspirin increases plasma proresolving mediators of inflammation. J. Lipid Res. 55, 2401–2407. [DOI] [PMC free article] [PubMed] [Google Scholar]