Abstract
Objectives
We aimed to assess the prevalence of opioid and benzodiazepine prescription drug misuse in older adults, the risk factors associated with misuse, and age-appropriate interventions.
Methods
Following PRISMA guidelines, we conducted a literature search for reports on misuse of prescription benzodiazepines and opioids in older adults. We searched PubMed, PsycINFO, and EMBASE for peer reviewed journal articles in English through April 2014 with updates through November 2015. We reviewed relevant publications that included participants ≥ 65 years of age. We also manually searched reference lists of key identified articles and geriatric journals through April 2016. Information on the study design, sample, intervention, comparators, outcome, time frame, and risk of bias were abstracted for each article.
Results
Of 4932 reviewed reports, 15 were included in this systematic review. Thirteen studies assessed the prevalence of prescription drug misuse and included studies related to opioid shopping behavior, assessment of morbidity and mortality associated with opioid and/or benzodiazepine use, frequency and characteristics of opioid prescribing, frequency of substance use disorders and non-prescription use of pain relievers, and the health conditions and experiences of long-term benzodiazepine users. One study identified risk factors for misuse and one study described the effects of provider education and an electronic support tool as an intervention.
Discussion
There is a dearth of high quality research on prescription drug misuse in older adults. Existing studies are heterogeneous, making it difficult to draw broad conclusions. We discuss the need for further research specific to prescription drug misuse among older adults.
Key Terms: aging, geriatrics, prescription drug abuse, primary care, substance abuse
Introduction
Substance use is a widely recognized medical and public health problem affecting patients across the lifespan.1 Substance use disorders as defined by the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) incorporate criteria associated with impaired control, social impairment, risky use, and pharmacological effects associated with substance use.2 Substance misuse, defined as intentional or unintentional use of a prescribed medication not in accordance with prescribed directions, is not necessarily associated with harm. Prescription drug misuse, particularly of benzodiazepines and opioids, however, is especially concerning because of the risk of fatal and nonfatal overdoses.1 Misuse can include adjusting doses without direction from a prescriber, unintentionally taking larger doses than prescribed, or taking medication for indications other than the intended use. Patients may take opioids, for example, for their mood altering effects.3
In 2008, 74% of prescription drug overdose deaths were related to use of opioid analgesics.4 An analysis of ambulatory data from 1995–2000 assessing trends in medical visits involving Schedule II opioids (e.g., morphine, methadone, fentanyl) noted that “older adults are at the greatest risk of nonmedical use of opioids prescribed directly from their physician” because they make more clinic visits and are more likely to be seen for pain than younger patients. Older adults are also among those most likely to receive a prescription for a benzodiazepine. Higher utilization of primary care services and opioid and benzodiazepine medications makes the potential misuse of these medications among older adults in the primary care setting an important public health concern.5–7
Older adults are also more likely to have memory and psychomotor abnormalities related to benzodiazepine and opioid use. Risk of falls and hip fractures as well as traffic accidents increase with prolonged use of these prescribed medications.8 Additionally, hepatic metabolism and changing proportions of body fat and water may alter effective dosing of these medications. Drug interactions also increase with age due to likelihood of higher number of pharmacologic agents being used and because of changes in metabolism associated with age.9,10 Furthermore, given the combination of more painful diagnoses with age and the social (e.g., loneliness, isolation, bereavement), psychological (e.g., depression, helplessness), and physical limitations common with aging, older adults may be a group particularly vulnerable to the negative consequences associated with opioids and benzodiazepines.11–14 While all of these complications may occur while adhering to medications as prescribed, misuse of medications may lead to increased risks of these complications and more difficulty for providers in identifying the cause of the issues. Complicating the identification of substance misuse problems in late-life is the fact that addiction or intoxication may present similarly to depression, delirium, or dementia.12,15
It is established that substance use disorders both exist and persist among older adults.16 Indeed, it is estimated that at least 5.7 million Americans age 50 years and older will need substance misuse treatment in the year 2020.17,18 Perhaps reflecting a cohort effect, older adults are increasingly presenting for first time substance use treatment.4 In recognition of the severity of the problem, several organizations, including the American College of Physicians,19 Substance Abuse and Mental Health Services Administration,20 and the American Psychiatric Association,21 have issued treatment guidelines and policy statements about physician prescribing, patient education, and the use of Prescription Drug Monitoring Programs to aid in the prevention and reduction of prescription misuse.
The aim of this systematic review was to survey the current state of the literature describing the prevalence, risk factors, and treatment studies of older adults with opioid and benzodiazepine misuse in primary care, and to highlight the need for further research into risk factors, interventions, and evidence-based treatments.
Methods
Following PRISMA guidelines,22 we conducted systematic literature searches in peer reviewed biomedical and behavioral journals for reports on prescription drug misuse in older adults in primary care. The focus was restricted to benzodiazepines and opioids. We searched PubMed, PsycINFO on OVID, and EMBASE through April 2014 with an updated search in November 2014 and November 2015. The initial literature search was tested and refined in PubMed. The final strategy was then translated into PsycINFO and EMBASE search languages.
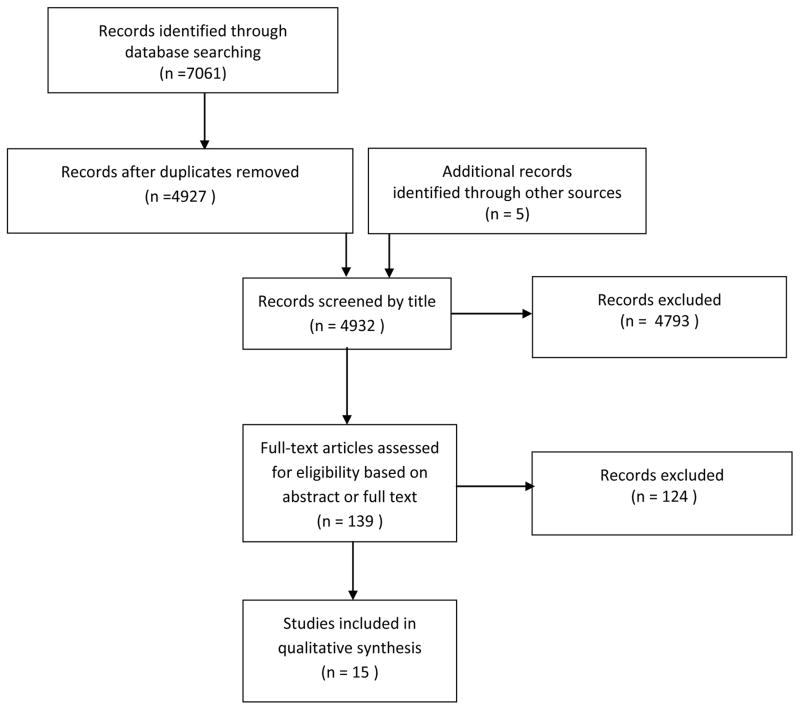
All searches were conducted using a combination of database-specific controlled vocabulary and free-text word and phrase searching, mainly in titles and keywords. We used Boolean operators “AND/OR” and database specific conventions such as broadening/narrowing of concepts, truncation, and available search fields and filters to customize the search strategy for implementation in each individual database. English language, age (middle aged–very elderly) and publication type (e.g., randomized controlled trial) filters were applied to all searches. The searches yielded a total of 4927 results across the three databases. Additionally, manual searches of literature databases, government publications, and references of other articles were conducted by the authors, resulting in 5 additional articles for consideration. Fifteen of the 4930 articles were included in this systematic review (Figure 1).
Figure 1.
Study Selection Flowchart
The challenge in searching the literature for this project was the near interchangeable use of the terminology denoting the concepts of drug misuse versus drug abuse in the literature. To focus the search on drug misuse, our search included as many variations of the terminology used for this concept as we could find in the database thesauri and the related literature. The prescription drug misuse terms were then coupled with the two aforementioned classes of prescription drugs.
The following information from the studies obtained from the search protocol was assessed: incidence/prevalence of and risk factors for prescription benzodiazepine and opioid misuse in the elderly; how to identify said misuse in the geriatric population in primary care settings; treatments/interventions implemented once the misuse was identified; outcomes of said treatments/interventions; and future clinical needs to address the burden of prescription drug misuse among older adults in primary care.
Eligible study designs included controlled clinical trials, open-label treatment studies, systematic reviews, cohort (both prospective and retrospective) studies, and cross-sectional assessments. Papers that only included case studies or case reports were excluded. However, case studies and reports that were presented in conjunction with a review of the literature were included. Studies that included a wide range of ages were included if they provided results specific to the geriatric subsample. Studies were excluded if they were not available in English or did not specifically address prescribed benzodiazepine or opioid misuse.
Identification of articles was done using the following procedure. A list of the citations pulled from each database and manual search was provided by the research librarian (ES), and two reviewers (RM and ZM) excluded articles based upon title. These two reviewers then evaluated this subset of citations by abstract. If, based upon an abstract alone, an article could not be excluded; the full text was evaluated to determine eligibility. Following PRISMA guidelines, the quality of each article was assessed by identifying potential biases based upon study design, sample population, and results. To minimize missing articles, in April 2016, we performed a manual search for papers about benzodiazepine and opioid use that were published within the previous 12 months in The American Journal of Geriatric Psychiatry, International Journal of Geriatric Psychiatry, International Psychogeriatrics, and Journal of the American Geriatrics Society.
Results
Of the fifteen articles included in this systematic review, thirteen were descriptive studies of prevalence (Table 1), one was a screening study (Table 2), and one was an intervention trial (Table 2). The descriptive studies (Table 1) included studies related to opioid shopping behavior (n=2), assessment of morbidity and mortality associated with opioid and/or benzodiazepine use (n=4), frequency and characteristics of opioid prescribing (n=2), prevalence of substance use disorders and frequency of non-prescription use of pain relievers (n=2), experiences of long-term benzodiazepine users (n=2), and assessment of health conditions of benzodiazepine users (n=1). The screening study (Table 2) sought to determine means and characteristics of detecting benzodiazepine misuse in older patients. The intervention study (Table 2) assessed whether an educational and electronic medical record intervention would affect prescriptions of opioids given in the emergency department. There were no additional articles found in the April 2016 manual search of journals that met criteria for inclusion.
Table 1.
Descriptive Studies
| Author/Year/Location | Sample Source, Design, Length of Follow-up | Sample Size | Objective | Measurement | Results | Author’s Conclusion | Relevance for Primary Care | Risk of Bias |
|---|---|---|---|---|---|---|---|---|
| Alvarenga et. al., 2009, Brazil24 | Cohort of The Bambui Health and Aging Study in Brazil, ≥60 years old with benzodiazepine use in the past 90 days; cross sectional study (Jan 1, 1997) | N = 1419 | Assess the health conditions and use of health services among older users of benzodiazepines. | Assessment of general and mental health, physical health, and use of health services and medications | Prevalence of use of benzodiazepines was 21% in those 70–79 years old and 27% in those ≥ 80years old. Users of benzodiazepines were more likely to be female, have bad self-reported health, have common mental disorders, diagnosis of myocardial infarction, 2 or greater doctor’s visits, and use 2 or more concomitant medications. |
Factors associated with benzodiazepine use in this population are similar to those associated with older people in higher income countries and further reinforces risk associated with benzodiazepine use in older adults. | Outpatient providers should assess for misuse among geriatric populations as the associated risks can lead to other physical conditions and leads to increase use of health care services. | The cross sectional nature of the study doesn’t allow for the assessment of health conditions and benzodiazepine use over time. It is difficult to compare this study to other cities in Brazil or to other populations abroad. |
| Blazer and Wu, 2009, United States32 | National Survey on Drug Use and Health (NSDUH) data, Cross sectional data analysis of a national community survey, two years (2005–2006) | N= 10,953 respondents 50+, 6,717 were 50–64 and 4,236 were ≥65 | Estimate the frequency, distribution and correlates of non-prescription use of pain relievers among middle-aged and older persons in the United States | Adjusted odds ratio (AOR) and confidence interval of past year non-prescription use of prescription pain relievers of those age 50–64 as compared to ≥65 | AOR = 2.39 (1.31–4.36) | There was much higher use among middle aged adults, suggesting that the problem may increase as the cohort ages. | As the population ages, misuse of prescription pain relievers will become an even greater issue. The number of older adults with past year misuse of prescription pain relievers is expected to rise. | This information is cross sectional and does not allow causation to be understood. The sample was taken from non-institutionalized persons, and as such is not a comprehensive representation of the US population within these age demographics. The data used does not have additional age breakdown for those ≥65, which may also provide more information. |
| Carriere et. al/2015/France30 | Mulit-site cohort study of community dwelling adults ≥65 years of age from the electoral rolls of three French cities between 1999 and 2001, Prospective Cohort Study, Evaluations were taken at baseline and with 2,4 and 7 year follow up | Cross sectional analysis = 6600 Restriction Incidence Analysis = 5766 Mobility Limitation Incidence Analysis = 3484 IADL Limitation Incidence Analysis = 5651 |
Examine cross sectional and longitudinal associations between benzodiazepine use and daily activity limitations considering drug indications and duration of action | Activity Limitations were assessed using two validated self report outcomes. Mobility was assessed using the Rosow and Breslau Scale. IADLs were assessed using the Lawton-Brody IADL scale For each outcome, any indication of inability to perform one activity was considered a limitation. Benzodiazepines were categorized as hypnotics, short and long acting. |
Cross Sectional Analysis: All three benzodiazepine categories were associated with odds of having mobility limitations. Long and short acting were IADL limitations. A significant difference between mobility and IADL limitations were found between benzodiazepine users and non users. Longitudinal: Probablities of having participation restriction, mobility limitations and IADL limitations increased over seven years at higher percentage for benzodiazepine users than non benzodiazepine users. |
Older adult benzodiazepine users have increased risk of activity limitations regardless of duration of action or indication. Chronic users of benzodiazepines should be avoided in order to delay disability | This information is important as further evidence of the potential morbidity associated with benzodiazepine use in older adults and should influence prescribing practices in this demographic. Additional training could be provided for physicians regarding avoiding chronic use and reducing and discontinuing benzodiazepine use. | Indication bias may be present, which occurs when persons are prescribed drugs for a condition associated with the outcome of interest. Channeling bias may have occurred when comparint duration of action of benzodiazepines. Dose-effect relationships were not assessed due to lack of needed information. Associations may have been underestimated as demented persons were excluded from this study. |
| Centers for Disease Control and Prevention, 2010; United States27 | SAMHSA Drug Abuse Warning Network (DAWN) that monitors drug related hospital Emergency Department (ED) visits, sampling technique to produce national estimates in metropolitan areas and the US, 5 years (2004–2008) | 231 hospitals from 12 metropolitan areas in the US. | Assess the morbidity associated with non-medical use of prescription drugs | Emergency Department Visits involving non-medical use of selected prescription drugs (i.e. taking higher than recommended dose, taking a drug prescribed for another person, drug facilitated assault, or documented misuse or abuse) | ED visits per 100,000 person years doubled for opioid misuse and showed increase for benzodiazepine misuse in those ≥ 65 years old from 2004–2008 (As can best be determined from graphical representation) | The increase in ED visits reflects the increase in prescribing of these classes of drugs. ED visits for opioid and benzodiazepine prescription misuse are as common as ED visits for illicit drugs. |
Misuse of opioids and benzodiazepines may place unnecessary burden on emergency departments. Stronger measures to reduce misuse of prescription drugs are warranted. Increases in rates are likely a reflection of increased prescribing of these medications. | These results are only for metropolitan areas and for the US. This leaves out rural areas that may have their own trends in ED use for non-medical use of selected prescription drugs. This population data also cannot necessarily be applied to patients on the individual level. |
| Centers for Disease Control, 2013, United States28 | Death rates based on National Vital Statistics System and SAMHSA Drug Abuse Warning Network (DAWN), sampling technique to produce national estimates in metropolitan areas and the US, 2 years for death rates (1999–2010) and 5 years for ED visits for drug misuse (2004–2008) | N = 15,323 total deaths among women due to drug overdose N = 943,365 ED visits by women for drug misuse or abuse |
Describe drug related deaths and ED visits among women. | 2010 Drug related deaths among women (Number, rate per 100,000 population) 2010 Drug misuse or abuse related ED visits among women (Number, rate per 100,000 population) |
Opioids: Total = 6631, 4.2; ≥ 65 yo = 284, 1.2 Benzodiazepines : Total = 2579, 1.6; ≥ 65 yo = 136, 0.6 Opioids: Total = 203,417, 129.6; ≥ 65 yo = 14,922, 65.1 Benzodiazepines : Total = 211,339, 134.6; ≥ 65 yo = 10,804, 47.2 The highest ED visit rates in 2010 included those for benzodiazepines (134.6 per 100,000 population and opioid pain relievers (129.6/100,000). |
Deaths from opioid pain relievers increased five-fold between 1999 and 2010 for women. ED visits related to misuse/abuse of opioid pain relievers among women more than doubled from 2004 to 2008. |
These data reinforce the need for responsible prescribing, screening for substance misuse and mental health problems and for prescription monitoring programs. Misuse of opioids and benzodiazepines place increased burden on emergency departments. | There is the potential that all drugs involved in the deaths or misuse were not reported. |
| Cepeda et. al. 2012; United States22 | 2008 IMS (corporate research company), LRx database (longitudinal patient level prescription database that covers 65% of retail prescriptions in the US, including mail and specialty pharmacy provider prescriptions), retrospective population based cohort study, 18 months | Total = 25,161,024 subjects ≥ 65 = 4,750,887 subjects | Define opioid shopping behavior by comparing overlapping prescriptions of Opioid, Benzodiazepines, and Diuretics | 1. at least 1 day of overlapping dispensing of prescriptions written by two or more different prescribers 2. frequency of shopping behavior defined as ≥ 2 overlapping prescriptions written by different prescribers and dispensed in ≥3 pharmacies |
Total = 13.1%, ≥ 65 = 15% with overlapping opioid Rx Total = 9.8% and ≥65 = 10% with overlapping benzodiazepine Rx Total = 0.18%, ≥65 = 0.07% for opioids; Total = 0.10% and ≥65 =0.03% for benzodiazepines |
Define opioid shopping behavior as having at least one day of overlapping prescriptions by different prescribers, filled at three or more pharmacies. The determining factor for qualification of shopping behavior is the number of pharmacies; Risk of Opioid abuse decreases with age | Identifying shopping behavior can reduce risk of misuse and diversion of prescription medications. The results of this study reinforce the use of Prescription Drug Monitoring Programs. | Only outpatient prescriptions were used. Only 65% of retail prescriptions were included and many of these were not from independent pharmacies. Shopping behaviors are likely underestimated by this study given these imitations. |
| Cepeda et. al. 2012, United States21 | 2008 IMS LRx database (covers 65% of retail prescriptions in the US, including mail and specialty pharmacy provider prescriptions), Retrospective Population Based cohort study, 18 months | Total = 25,161,024 ≥ 65 = 4,750,887 | How soon shopping behavior was observed after opioid exposure, number of events per shopper, preferred opioids, and method of payment. | 1. Risk of shopping behavior 2. Time to first shopping episode (Median number of days) 3. Number of Days to first shopping event 4. Number of shopping episodes (1st–99th percentile) |
Total 3/1000 and for ≥ 65 = 1.2/1000 persons exposed to opioids will abuse or divert them Total = 234 days and ≥ 65 = 233 days Total = 5–543 and ≥ 65 = 5–541 Total = 1–23 and ≥ 65 = 1–20 |
Risk per exposed subject is similar to risk of abuse from other studies. Shopping behavior is exhibited approximately eight months after exposure on average. Strong opioids are sought, combination products are avoided, prescriptions are often paid for in cash and obtained from a few providers | Identifying shopping behavior can reduce risk of misuse and diversion of prescription medications. The results of this study reinforce the use of Prescription Drug Monitoring Programs | Only outpatient prescriptions were used. Only 65% of retail prescriptions were included and many of these were not from independent pharmacies. Shopping behaviors are likely underestimated by this study given these limitations. |
| Jena et al, 2014, United States23 | Database of prescription drugs and medical claims in 20% random sample of Medicare beneficiaries, Retrospective cohort study, one year (2010) | N= 1,808,355 Medicare beneficiaries in 2010 | Estimate the frequency and characteristics of opioid prescribing by multiple providers in Medicare and the association with hospital admissions related to opioid use. | Beneficiaries ≥ 65yo (number and %): In the entire sample: With one prescription With >1 prescription and 1 provider With >1 prescription and 2 providers With >1 prescription and 3 providers With >1 prescription and ≥ 4 providers Adjusted Odds Ratio and 95% CI for filling an opioid prescription from more than one provider (≥85 is the comparison group) |
N = 1,310,539, 72.4% N = 494,567, 82.4% N = 350,970, 73.9% N = 264,763, 70.5% N = 105,645, 61.6% N = 61, 594, 45.1% 65–74 yo = 1.55 (1.53–1.57) 75–84 yo = 1.32 (1.31–1.34) |
Current opioid prescribing by multiple providers is common in Medicare patients and is associated with higher rates of hospital admission related to opioid use. | Multiple prescriptions may be a reflection of fragmented care or doctor shopping by patients. | This study provides an assessment of the geriatric population’s characteristics of opioid prescribing. However, it may be an underestimation of this demographic as some patients may have prescriptions not filled by using Medicare. |
| Landreat et. al., 2010, France26 | First five patients who met criteria for inclusion from partner pharmacies of the Faculty of Pharmacy of Nantes, cross sectional, 3 month period | N=176 patients ≥ 65 years old | Establish whether there is an addiction to benzodiazepine or equivalents in persons age 65 years or older who were taking benzodiazepines or equivalents on a chronic basis and to carry out a quantitative analysis of their profile. | DSM IV Questionnaire administered by a health professional with addiction defined as meeting three items according to DSM IV Principal Component Analysis assessing medico-surgical, psychiatric history, alcohol consumption and smoking history Logistic Regression models |
35.2% of subjects were addicted to BZD/equivalents. Addicted subjects differ from non-addicted subjects based on the following two dimensional factors: 1. Deprivation signs and Unsuccessful attempts to stop treatment and 2. Tolerance, taking higher doses than prescribed, concerned by treatment/treatment duration Defined addiction based on tolerance, taking higher doses, deprivation signs and unsuccessful attempts to stop treatment. |
A high prevalence of addiction was found that was not previously reported. A two factor concept of addiction can be used to conceptualize benzodiazepine addiction in this population. | Assessing older patients by the criteria noted is more effective in determining any abuse or dependence as other common factors associated with diagnosis as these factors (i.e. length of time, social/medical consequences) are not necessarily specific to diagnosing benzodiazepine dependence in this population. | The patients included were the first five who met criteria for study inclusion that happened to show up in the pharmacy that day. This is indicative of selection bias and was not a random sampling of customers picking up prescriptions. |
| Mura et. al, 2013, France29 | Mulit-site cohort study of community dwelling adults ≥ 65 years of age from the electoral rolls of three French cities between 1999 and 2001, Prospective Cohort Study, Evaluations were taken at baseline and with 2,4 and 7 year follow up | 4226 non benzodiazepine users 969 chronic benzodiazepine users |
Examine if long term use of benzodiazepines is associated with an accelerated decline of cognitive performances | Multivariate longitudinal bounded quantitative outcomes of Mini Mental Status Exam, Isaacs Set test, Benton Visual Retention Test, Trail Making Test (A&B) | Chronic benzodiazepine use was significantly associated with lower performance in each test except MMSE when assessing cross sectional effect. There were no longitudinal effects for each test regarding the link between chronic use and cognitive decline. | The results of the study emphasize predominant impairment of cognitive level in chronic benzodiazepine users regarding immediate visual memory and visuomotor processing speed but do not indicate that there is accelerated cognitive decline with chronic benzodiazepine use in the elderly. | This information is important as further evidence of the potential morbidity associated with benzodiazepine use in older adults and should influence prescribing practices in this demographic. Additional training could be provided for physicians regarding avoiding chronic use and reducing and discontinuing benzodiazepine use. | Some selection bias was present in selecting subjects for the study, which may impact outcomes. |
| Neutel et. al., 2013, Norway31 | Persons 70–89 years old who filled at least five opioid prescriptions from Norwegian Prescription Database, which registers all Rx filled at any pharmacy in Norway, Cross Sectional, in 2008 | Weak opioids, N= 19,675 (i.e. tramadol and combination drugs with codeine or dextropropoxyphene) Strong opioids, N= 4,268 (i.e., morphine, oxycodone, fentanyl, buprenorphine) | Assess multiple prescribers as an indicator of abuse by relating quantity of opioids obtained by older Norwegians to number of prescribers. | 1. Number of prescribers 2. Length of medication episode 3. Cancer/Palliative care subgroup |
1. More than 30% of weak and strong opioid users had three or more prescribers. Almost 5% of frequent strong opioid users and 6.6% of frequent weak opioid users received prescriptions from five or more prescribers. 2. Over 50% of strong and weak opioid users had at least 40 weeks of treatment. 3. The cancer/palliative care group showed the greatest increase in strong opioid use with number of prescribers. |
The increasing quantities of strong opioids with increasing number of prescribers are largely due to treatment of cancer/palliative care patients and should not be synonymous with ‘doctor shopping’ or abuse. | Consider the medical co-morbidities of patients in assessing the need for Opioid prescriptions. Primary care providers should also make efforts to know who other providers are and what they are prescribing to patients to avoid multiple prescriptions. | The study was conducted in Norway and the results cannot be extrapolated to similar age groups of other countries. The study results are also limited to a particular age demographic within the geriatric population and results are not necessarily able to be extrapolated. |
| Voyer et. al. 2004, Canada33 | Volunteer residents from two retirement residences for ambulatory seniors who were prescribed benzodiazepine medications in Quebec, Canada, cross sectional study | N=45 patients ≥ 65 years old | Understand how dependence was experienced by long-term benzodiazepine users | Directive interviews including questions about reason for duration of and effects of benzodiazepine drug use; withdrawal experiences; and attitudes and reactions from health professionals and relatives. | 36 participants were prescribed only benzodiazepines and 9 received benzodiazepines and antidepressants 75% of prescriptions were as needed (PRN). All participants met study definition of long-term use. Mean duration of use was nine years. Qualitative interviews showed that the indicators of dependence include: self-identifying as a dependent user, invoking multiple stressors to justify benzodiazepine use, using benzodiazepines to cope with anticipated stressors, trivializing the dangers of benzodiazepines, keeping a supply in reserve, having previously tried and failed to stop, and reducing the dosage. | There is a need to take a more elaborate, person-centered view of dependence. | Definitions of misuse/abuse/dependence may be different for geriatric population and may present differently. Awareness of this fact may allow for more opportunity of treatment and intervention. | This study was conducted outside the United States, and as such results are likely unable to be extrapolated to the US population. Additionally, the small sample size was comprised of volunteer residents in retirement communities. This represents a selection bias as there are likely several confounding factors. |
| Voyer et al., 2010, Canada25 | Random, proportional sample of adults age ≥ 65 who completed the large scale population based, Quebec Survey on the Health of Older Persons from Jan 2005 to Sept 2006 | N=2785 | Determine the prevalence rate of benzodiazepine dependence in older persons according to DSM-IV-TR and criteria. | 1. Asking respondents if they had taken one of several benzodiazepines in the past year. 2. Questions asked from DSM-IV-TR criteria for substance dependence 3. Seven atypical signs of benzodiazepine use were assessed |
1. 707 (25.4%) respondents endorsed using a benzodiazepine in the past year. 2. Of this subset, 67 (9.5%) met DSM-IV-TR criteria for dependence. Of those with benzodiazepine dependence, 60 (88.9%) endorsed ongoing resolution or fruitless efforts to reduce or cease medication. 34 (50%) reported tolerance and 37 (54.4%) reported withdrawal. 3. In dependent respondents, 47(69%) felt that it would be good to stop using benzodiazepines, 41 (60.5%) felt they were dependent, and 30 (45.1) believed the medication was addictive. |
Benzodiazepine use is prevalent in this sample and some of the users would classify themselves as dependent. | Almost 10% of those using a benzodiazepine met criteria for dependence. This further highlights the necessity of ongoing screening by prescribers and primary care providers. | This data is obtained from a specific province in Canada and cannot be generalized to other provinces/countries. It was based on self-reported data and there is potential for recall bias as patients were reporting their use. The data also excludes institutionalized persons and is therefore not a representation of the entire population. |
Table 2.
Screening and Intervention
| Author/Year/Study Location | Sample Source, Design, Length of Follow up | N | Objective | Measurement | Results | Author’s Conclusion | Relevance for Primary Care | Risk of Bias |
|---|---|---|---|---|---|---|---|---|
| Voyer, et. al 2010, Canada34 | Proportional sample of households based on corresponding administrative regions of Quebec who completed the Quebec Survey on the Health of Senior from Jan 2005–Sept 2006 | N= 2785 adults age ≥ 65 years old who agreed to be in the study | Determine a sample means of detecting benzodiazepine use in the elderly | Assessment based on 12 month period diagnosis according to DSM IV TR criteria for substance dependence Assessment of validity by pairing two criteria together (total of 45 pairs) and examining sensitivity and specificity |
25.4% (707) of the respondents used benzodiazepines and 9.5% of this subgroup met DSM IV criteria for dependence. Of the pairs, “Attempt to stop “ and “Tolerance” had the highest sensitivity and specificity (97.1% and 94.9% respectively) |
Using the two questions as a screening measure could help identify patients with possible benzodiazepine dependence. | This tool may be a good screening measure to use. Further assessment and validation would be required. | This is an international study and as such, the results cannot be generalized to other national populations. Additionally, there is risk of some selection bias as study participants are those who were agreeable to participating. Subjects may also not have given accurate report of use or inaccurately recalled use or attempts to stop. |
| Gugelmann et.al, 2013, United States35 | Patients in two urban EDs who are prescribed opioids from the ED assessed during a Pre-intervention (6–9 months) and Post-intervention (8–11 months) period at 2 tertiary care urban EDs (a primary and affiliate hospital) at different times, Prospective study (Primary Hospital January 2012–August 2012 and affiliate hospital September 2011–August 2012) | N= 40,554 pre-intervention and 30,958 post intervention at the primary hospital N = 18,000 pre-intervention and 27,143 post-intervention at the affiliate hospital At both hospitals, for persons age ≥65, N = 1360 pre-intervention and 852 post-intervention |
To determine if multidisciplinary educational intervention (lectures, journal clubs, case discussions, and EMR decision support tool) would decrease ED opioid packs (4 tablets of Oxycodone 5mg-Acetaminophen 325) dispensed at discharge. | 1. Pre-intervention and post-intervention change in opioid discharge packs dispensed to all patients treated and discharged through August 2012. 2. Analysis of change in opioid dispensing among patients with known risk factors (<65 yo, history of substance abuse, chronic pain or psychiatric disorder) for Rx opioid dependence |
1. Overall discharge packs decreased by 39.6% at primary hospital and 56.2% at the affiliate hospital. 2. For persons age ≥ 65 yo, 210/1360 (15.4%) were given an opioid pack at pre-intervention. 83/852 (9.7%) were given an opioid pack post-intervention. |
Gugelmann et.al, 2013, United States35 | Patients in two urban EDs who are prescribed opioids from the ED assessed during a Pre-intervention (6–9 months) and Post-intervention (8–11 months) period at 2 tertiary care urban EDs (a primary and affiliate hospital) at different times, Prospective study (Primary Hospital January 2012–August 2012 and affiliate hospital September 2011–August 2012) | N= 40,554 pre-intervention and 30,958 post intervention at the primary hospital N = 18,000 pre-intervention and 27,143 post-intervention at the affiliate hospital At both hospitals, for persons age ≥ 65, N = 1360 pre-intervention and 852 post-intervention |
Descriptive Studies
Doctor shopping is generally defined as obtaining multiple prescriptions for the same or similar medications from multiple providers.23 A study on the assessment of shopping behavior for opioid and benzodiazepine medications in those ≥65 years of age found that one significant criterion for determining this behavior was when prescriptions were filled at three or more pharmacies in addition to being written by different providers.24 Another study described that measurement of time to first shopping episode and number of shopping episodes for opioid medications were similar in persons ≥ 65 years old as to the general population, suggesting that this behavior may not be unique to older adults.23 A more specific study involving Medicare recipients observed that opioid prescribing by multiple providers was common among beneficiaries and was also associated with increased rates of hospital admissions.25
Prevalence studies also showed that there were similarities in various countries regarding the increased use of benzodiazepine medications among older adults.26 Assessments of self-perception about benzodiazepine use also have been studied and showed some personal awareness of the dependence and the need for decreased use among that study population.27,28 Increased morbidity was associated with benzodiazepine and opioid prescription misuse based on evidence that ED visits increased for those ≥65 years old using these substances without medical indication (taking higher than recommended dose, taking a drug prescribed for another person, drug facilitated assault, or documented misuse or abuse) and that opioid overdoses from prescription pain relievers also increased among females in this age demographic.29,30 Additionally, benzodiazepine use in older adults has been linked to cognitive impairment and activity limitations.31,32 It has been suggested that increased use of opioid medications in older adults is related to increased treatment of medical comorbidities, particularly cancer and other conditions associated with palliative care.33 However, even higher rates of prescription drug misuse are expected in the future as the current middle aged population (ages 50–64) has notably higher rates of substance misuse than those currently ≥ 65 years of age.34
Of note, many of these studies are valuable in the information they provide, but their findings are difficult to extrapolate to larger populations. The cross sectional nature of the data do not allow for assessment of variables over time and provide only a snapshot of issues related to benzodiazepine and opioid use among older adults.26,28,34 While the demographics of those sampled are often limited to non-institutionalized persons, which may provide more accurate data for understanding this issue in the primary care setting, it provides limited data in understanding prescription substance misuse among the general population of older adults. Additionally, some studies were isolated to various communities (i.e. international,26–28,31–33,35 rural vs. urban,29 particular age cohort among older adults 26,33), limiting their generalizability.
Selection biases are also present in studies based on methods of inclusion (i.e. willing participants35 and first five patients28). Death rates from a CDC study also may be biased as the authors note the potential for incomplete records related to which particular drugs may have been involved in deaths.30 Studies assessing prescriptions also present with biases as they include outpatient prescriptions, non-independent pharmacies, and Medicare prescriptions. These data sources are not comprehensively representative of all prescriptions filled and likely underestimate provided estimates of opioid shopping behavior.23–25 Prescriptions obtained from independent pharmacies and through non-Medicare providers may provide additional information and allow for more accurate estimates about opioid shopping behavior.
Screening and Intervention
The single study that met inclusion criteria for screening described an assessment of how to detect risk of benzodiazepine misuse in older adults. The study noted that when screening using Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM IV) dependence criteria, asking about 1) attempts to stop, and 2) tolerance of medications yielded the most sensitive and specific results.36 There is selection bias in this study as it was completed by survey and included those who were agreeable to participating. There may also have been instances of underreporting use or recall bias given the methodology of the survey.
The review of the single intervention study showed the positive effects of using an electronic medical record (EMR)-based support tool to aid emergency department (ED) prescribers’ decisions regarding dispensing opioids to patients based on known risk factors. Educational interventions for providers and the EMR tool were associated with a decrease in the number of opioid packs (4 tablets of Oxycodone 5mg-Acetaminophen 325mg) dispensed and in the number of packs ordered for all patients including those ≥65 years of age. This study showed that real-time efforts to manage prescribing practices in settings that are often front line for diagnosis and treatment can limit prescriptions for patients at high risk of misuse or diversion.37 While the results of this study show that there was a decrease in the number of opioid packs dispensed, efficacy of the intervention would be more evident if a control group had been used for comparison. Pain scores and chronic pain assessments were taken during triage and used in analysis of risk factors, but no results for efficacy in treatment of pain data was gathered for pre or post intervention.
Discussion and Conclusion
Overall, our main findings showed that the data on prescription substance misuse among older adults is sparse. During our search via methods outlined above and via manual investigations of medical and psychiatric geriatric journals, there was little consistent and generalizable evidence found regarding prescription opioid and benzodiazepine misuse among adults ≥65 years of age. Among the 15 articles that met our search criteria, the majority focused on the prevalence of benzodiazepine and opioid misuse in specific primary care settings. Our findings also show that there are limited studies examining screening for risks or characteristics of older adults with misuse in primary care settings and few studies assessing treatment or intervention strategies for opioid or benzodiazepine misuse in older adults.
Descriptive Studies
Based on the results from this review, it appears there have been several attempts to quantify the prevalence of opioid and benzodiazepine misuse among older adults in outpatient and primary care settings through different methods: attempting to define shopping behavior and time to shopping behavior after initial exposure through pharmacy claims databases; examining study data and interviews with patients; and through assessing drug-related ED deaths. While these studies provide a signal that there is increasing misuse of prescription medications in older adults, the prevalence of opioid and benzodiazepine misuse among older adults remains unquantified given the various study populations and methods used in these studies.
Further investigation into the reason behind some Medicare patients’ multiple prescriptions, possibly using qualitative research methods, may be warranted to avoid mislabeling and stigmatization of patients as prescription misusers. Another important note is that these multiple prescriptions may be indicators of fragmented care instead of opioid prescription seeking by patients.25
With multiple prescribers, patients have the potential to obtain multiple prescriptions for the same condition, which supports the need for nation-wide prescription drug monitoring programs. Developing and utilizing prescription monitoring systems has the potential to reduce multiple prescriptions, prescription shopping behavior, and ED visits due to misuse of prescribed medications. Prescription opioid monitoring systems are often used by pain specialists who provide opioid therapy. Such systems could also help primary care providers who are often first-line prescribers of opioids and benzodiazepines for patients with complaints of pain, anxiety, and insomnia. Primary barriers to implementing these systems are funding and an infrastructure for ongoing monitoring.38 Furthermore, the utilization and utility of these programs is sometimes questionable as studies have shown that not all physicians utilize the resource and that the type of medications and level of providers who have access to this information varies from state to state.39 Policy questions also arise surrounding the concern for patient privacy, stigmatization, and the potential for primary care physicians to limit the number and length of prescriptions for substances such as opioids and benzodiazepines to avoid being seen as an inappropriate prescriber, thus compromising patient care.40 Additional studies regarding other morbidity assessments including cognitive impairment and activity limitations with benzodiazepine and opioid medications could be helpful in determining more appropriate prescribing guidelines for these medications in older populations.31,32
Screening and Intervention
The data presented from the study of risk measurement are also important for primary care as it is often the gateway to recognizing drug misuse problems. Of note, we observed that asking about both attempts to stop and tolerance of benzodiazepine medications produced the highest sensitivity and specificity as screening tools among older adults with benzodiazepine misuse.36 Future research using larger datasets of a random sampling of adults age 65 and older in primary care settings is needed to provide more generalizable results.
Screening for substance misuse in primary care settings is important as many primary care providers are often the first to identify psychosocial stressors and psychiatric and substance misuse disorders. Determining cultural and age appropriate, yet efficient ways to identify prescription drug misuse in older adults, is critical to make implementing screenings and interventions a success in primary care. Of note, additional screening measures in a group of Philadelphia primary care clinics observed that those patients with lower frequency of use and less anxiety were more likely to be willing to engage in tapering or discontinuing their benzodiazepine use.41
There are screening tools available for benzodiazepine misuse, such as the Benzodiazepine Dependence Self-Report Questionnaire and the Severity of Dependence Scale.42,43 While the use of the benzodiazepine abuse scales may have benefit in primary care, they have not been specifically validated for use with older adults. Moreover, studies assessing opioid abuse in chronic pain patients may have applications in older adults as well.44 Most of the opioid abuse scales were developed for use of evaluating chronic pain patients and not for use in primary care settings. Development of specifically tailored instruments for older patients in primary care may result in a more accurate picture of the prevalence and facilitate referral to appropriate resources as needed for treatment and interventions addressing benzodiazepine and opioid misuse.
While our systematic review identified a single intervention study, there are several other treatment and intervention studies that did not meet inclusion criteria due to setting, age range cut-offs, or lack of age-specific data for older adults. For example, sending an intervention letter advising patients to gradually taper their benzodiazepine use, engaging patients in supervised withdrawal, assessing benzodiazepine craving in a treatment intervention aimed at long term benzodiazepine users, conducting brief interventions, and providing self-help booklets from primary care physicians are several other methods studied in the outpatient setting.45–49 Inpatient methods of intervention included assessing the effects of having clinical pharmacists on inpatient teams in an effort to reduce future ED visits and inpatient admissions for those 80 years and older by reducing inappropriate prescribing of opioid and benzodiazepine medications. 50 There were no studies found using our search criteria that addressed treatment or intervention for patients with identified misuse of prescribed opioid or benzodiazepine medications, which is an important area for future research.
Previous studies assessing alcohol misuse among older adults have shown that there are benefits to age-specific treatment interventions tailored to older adults and their needs, which may prove true for benzodiazepine and opioid misuse as well.51 The Florida Brief Intervention and Treatment for Elders (BRITE) project, a three year pilot program of screening and brief intervention for older adult substance misusers, showed that improvements in substance use could be made with a series of brief interventions focused on drug use and depression.52 To date, it is one of few studies in older adults that has utilized screening, intervention, and treatment methods to assess the impact of substance misuse in older adults.
Additional studies have shown the benefits of addressing substance use, particularly alcohol misuse in the primary care setting. The Primary Care Research in Substance Abuse and Mental Health for Elderly (PRISM-E) study compared effects of substance abuse and mental health services when integrated into primary care vs. using an enhanced referral to outside providers. While the study did not note any difference in clinical outcome between the two models of care, access to and participation in mental health and substance abuse services were noted to be significantly better in the integrated care model. Efforts from the BRITE and PRISM-E studies could potentially be used to impact benzodiazepine and opioid misuse among older adults in the primary care setting.53,54
The emergence of Federally Qualified Health Centers and Patient Centered Medical Homes also provide opportunities to offer integrated care and treatment for older adults with substance misuse in primary care settings as there are emerging incentives under the Affordable care Act (ACA) to provide coverage for mental health and addiction treatment, reducing the need for care in multiple settings.55 Coordinating care between various sites for patients has been a method often used to treat substance misuse in the primary care setting, but recent efforts at “co-locating” primary care and substance use services together have shown improved outcomes and may also be especially useful in older adult populations for logistical reasons.56
The research gaps identified in this paper are numerous. While there have been many attempts to quantify the prevalence of benzodiazepine and opioid misuse among older adults, these attempts have been done using different data sources, each of which present their own limitations in scope and generalizability of results. Furthermore, the lack of identifiable risk factors makes efforts at prevention and monitoring difficult. Additionally, further studies regarding potential interventions and treatment for older adults with benzodiazepine and opioid misuse are needed. Nonetheless, the results of this manuscript do reinforce the importance of the idea that primary care is an important location through which issues regarding misuse can be identified and treated.
Limitations
Our review has important limitations. Of note, there may be studies that were not included based upon search criteria utilized and because of the way prescription drug abuse may be described in the literature. There were several studies that provide important results and information that did not meet criteria for inclusion based upon lack of data specific for older adults. Furthermore, there are also studies that sought to include older adults, but did not meet the cut-off criteria or provide age specific criteria for persons ≥ 65 years of age. While these studies did not meet criteria for this review, they may provide ideas for formulating research and interventions related to older adults and prescription medication misuse.7,13,15,38,41–47,50,57–65
The articles in this systematic review are limited in their applicability to general populations. Many of them included small sample sizes or data specific to older adults within a particular demographic (i.e. urban or nursing home). International studies were also included in this review. They involved a wide range of topics including prescribing practices, prevalence rates, and access to services from countries in Europe and South America. While the results from these articles may not be applicable internationally, the methods used may be implemented in other systems of health care to collect more information about prescription drug misuse.
Conclusion and Call for Action
The misuse of prescription benzodiazepines and opioids among older adults in primary care is a problem of mounting importance in an aging society. There is limited published research on this topic, and continued efforts to better measure this public health problem and develop age-specific and culturally appropriate interventions are needed to ensure optimal health outcomes. Further research into the implications for primary care as the gateway to identifying misuse and the potential setting for intervention and treatment are warranted. The increasing incidence of prescription drug misuse also highlights the need for education among primary care providers regarding both prescription medication misuse and safe prescribing practices for opioid and benzodiazepine medications in the older adult population. Engaging stakeholders and policy-makers in prescription monitoring programs is an important consideration to improve patient safety. These issues, along with the aforementioned gaps in screening and evidence-based treatments, need to be addressed as physicians and health systems strive to provide the safest and most effective care for patients.
Table 3.
Treatment and Intervention Studies
| Author/Year/Study Location | Sample Source, Design, Length of Follow up | N | Objective | Measurement | Results | Author’s Conclusion | Relevance for Primary Care | Risk of Bias |
|---|---|---|---|---|---|---|---|---|
| Gugelmann et.al, 2013, United States35 | Patients in two urban EDs who are prescribed opioids from the ED assessed during a Pre-intervention (6–9 months) and Post-intervention (8–11 months) period at 2 tertiary care urban EDs (a primary and affiliate hospital) at different times, Prospective study (Primary Hospital January 2012–August 2012 and affiliate hospital September 2011–August 2012) | N= 40,554 pre-intervention and 30,958 post intervention at the primary hospital N = 18,000 pre-intervention and 27,143 post-intervention at the affiliate hospital At both hospitals, for persons age ≥ 65, N = 1360 pre-intervention and 852 post-intervention |
To determine if multidisciplinary educational intervention (lectures, journal clubs, case discussions, and EMR decision support tool) would decrease ED opioid packs (4 tablets of Oxycodone 5mg-Acetaminophen 325) dispensed at discharge. | 1. Pre-intervention and post-intervention change in opioid discharge packs dispensed to all patients treated and discharged through August 2012. 2. Analysis of change in opioid dispensing among patients with known risk factors (<65 yo, history of substance abuse, chronic pain or psychiatric disorder) for Rx opioid dependence |
1. Overall discharge packs decreased by 39.6% at primary hospital and 56.2% at the affiliate hospital. 2. For persons age ≥ 65 yo, 210/1360 (15.4%) were given an opioid pack at pre-intervention. 83/852 (9.7%) were given an opioid pack post-intervention. |
Interventions were associated with a decrease in the number of opioid packs dispensed and also in the number ordered for those with risk factors. | Providing education to prescribers can influence the trends in prescriptions and help prevent misuse and comorbidity. | It is difficult to assess the true efficacy of the intervention without a control group. |
Acknowledgments
Source of Funding: Funding was provided in part by AG033575 and MH101371 (Karp).
Footnotes
Conflicts of Interest: Dr. Marcum is a consultant for Purdue Pharma. Dr. Karp has received medication supplies for investigator initiated trials from Invidior and Pfizer.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Schulden J, Lopez M, Compton W. Clinical Implications of Drug Abuse Epidemiology. Psychiatr Clin North Am. 2012;35(2):411–423. doi: 10.1016/j.psc.2012.03.007.Clinical. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. 2013. [Google Scholar]
- 3.Gilson AM, Kreis PG. The burden of the nonmedical use of prescription opioid analgesics. Pain Med. 2009;10(S2):S89–S100. doi: 10.1111/j.1526-4637.2009.00668.x. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Vital Signs: Overdoses of Prescription Opioid Pain relievers -- United States, 1999–2008. Morb Mortal Wkly Rep. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- 5.Olfson M, Wang S, Iza M, Crystal S, Blanco C. National trends in the office-based prescription of schedule II opioids. J Clin Psychiatry. 2013;74(9):932–939. doi: 10.4088/JCP.13m08349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Becker W, Tobin D, Feillin D. Nonmedical Use of Opioid Analgesics Obtained Directly From Physicians: Prevalence and Correlates. Arch Intern Med. 2011;171(11):1034–1035. doi: 10.1001/archinternmed.2011.217. [DOI] [PubMed] [Google Scholar]
- 7.West NA, Severtson SG, Green JL, Dart RC. Trends in abuse and misuse of prescription opioids among older adults. Drug Alcohol Depend. 2015;149:117–121. doi: 10.1016/j.drugalcdep.2015.01.027. [DOI] [PubMed] [Google Scholar]
- 8.Campanelli CM. American Geriatrics SOciety Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults: The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. J Am Geriatr Soc. 2012;60(4):616–631. doi: 10.1111/j.1532-5415.2012.03923.x.American. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ries RK, Fiellin DA, Miller SC, Saitz R. American Society for Addiction Medicine Principles of Addiction Medicine. 5. Philadelphia, PA: Lippincott, Williams and Wilkins; 2014. [Google Scholar]
- 10.Mulsant BH, Pollock BG. Psychopharmacology. In: Thakur ME, Blazer DG, Steffens DC, editors. Clinical Manual of Geriatric Psychiatry. Vol. 1. Washington, D.C: American Psychiatric Publishing; 2014. pp. 17–82. [Google Scholar]
- 11.Gossop M, Moos R. Substance misuse among older adults: a neglected but treatable problem. Addiction. 2008;103(3):347–348. doi: 10.1111/j.1360-0443.2007.02096.x. [DOI] [PubMed] [Google Scholar]
- 12.Koechl B, Unger A, Fischer G. Age-Related aspects of addiction. Gerontology. 2012;58(6):540–544. doi: 10.1159/000339095.Age-related. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luijendijk HJ, Tiemeier H, Hofman A, Heeringa J, Stricker BHC. Determinants of chronic benzodiazepine use in the elderly: a longitudinal study. Br J Clin Pharmacol. 2007;65(4):593–599. doi: 10.1111/j.1365-2125.2007.03060.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petrovic M, Vandierendonck A, Mariman A, Van Maele G, Afschrift M, Pevernagie D. Personality traits and socio-epidemiological status of hospitalised elderly benzodiazepine users. Int J Geriatr Psychiatry. 2002;17(8):733–738. doi: 10.1002/gps.677. [DOI] [PubMed] [Google Scholar]
- 15.Mcinnes E, Powell J. Drug and alcohol referrals : are elderly substance abuse diagnoses and referrals being missed ? 1994;308(February):444–446. doi: 10.1136/bmj.308.6926.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reynolds K, Pietrzak RH, El-Gabalawy R, Mackenzie CS, Sareen J. Prevalence of psychiatric disorders in U. S. older adults: findings from a nationally representative survey. World Psychiatry. 2015;14(February):74–81. doi: 10.1002/wps.20193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Han B, Gfroerer J, Colliver J, Penne M. Substance use disorder among older adults in the United States in 2020. Addiction. 2009;104(1):88–96. doi: 10.1111/j.1360-0443.2008.02411.x. [DOI] [PubMed] [Google Scholar]
- 18.Gfroerer J, Penne M, Pemberton M, Folsom R. Substance abuse treatment need among older adults in 2020: The impact of the aging baby-boom cohort. Drug Alcohol Depend. 2003;69(2):127–135. doi: 10.1016/s0376-8716(02)00307-1. [DOI] [PubMed] [Google Scholar]
- 19.Kirschner N, Ginsburg J, Sulmasy LS, Policy P. Position Paper Annals of Internal Medicine Prescription Drug Abuse : Executive Summary of a Policy Position Paper From the American College of Physicians 2014. 2013 Dec; doi: 10.7326/M13-2209. [DOI] [PubMed] [Google Scholar]
- 20.Center for Substance Abuse Treatment. Substance Abuse Among Older Adults. Treatment Improvement Protocol (TIP) Series 26. Vol. 7. Rockville, MD: Substance Abuse and Mental Health Services Administration, US Dept of Health and Human Services; 1998. pp. 1–252. DHHS publication no. SMA 98-3179. [Google Scholar]
- 21.APA. Position Statement on Mental Health & Substance Abuse and Aging : Three Resolutions. 2004. [Google Scholar]
- 22.Moher D, Liberati A, Tetzlaff J, Altman DG. Academia and Clinic Annals of Internal Medicine Preferred Reporting Items for Systematic Reviews and Meta-Analyses. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 23.Cepeda MS, Fife D, Chow W, Mastrogiovanni G, Henderson SC. Opioid shopping behavior: how often, how soon, which drugs, and what payment method. J Clin Pharmacol. 2012;53(1):112–117. doi: 10.1177/0091270012436561. [DOI] [PubMed] [Google Scholar]
- 24.Cepeda MS, Fife D, Chow W, Mastrogiovanni G, Henderson SC. Assessing Opioid Shopping Behaviour. Drug Saf. 2012;35(4):325–334. doi: 10.2165/11596600-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 25.Jena AB, Goldman D, Weaver L, Karaca-Mandic P. Opioid prescribing by multiple providers in Medicare: retrospective observational study of insurance claims. BMJ. 2014;348(February):g1393. doi: 10.1136/bmj.g1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alvarenga J, de Layola Filho A, Firmo J, Maria L-C, Elizabeth U. A population based study on health conditions associated with the use of benzodiazepines among older adults (The Bambuí Health and Aging Study) Estudo de base populacional sobre condições de saúde associadas ao uso de benzodiazepínicos em idosos ( Proje. Cad saude Publica, rio Janiero. 2009;25(3):605–612. doi: 10.1590/s0102-311x2009000300015. [DOI] [PubMed] [Google Scholar]
- 27.Voyer P, Préville M, Cohen D, Berbiche D, Béland S. The Prevalence of Benzodiazepine Dependence among Community-Dwelling Older Adult Users in Quebec According to Typical and Atypical Criteria *. Can J Aging. 2010;29(2):205–213. doi: 10.1353/cja.0.0124. [DOI] [PubMed] [Google Scholar]
- 28.Landreat MG, Vigneau CV, Hardouin JB, et al. Can we say that seniors are addicted to benzodiazepines? Subst Use Misuse. 2010;45(12):1988–1999. doi: 10.3109/10826081003777568. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. Emergency Department Visits Involving Nonmedical Use of Selected Prescription Drugs—United States, 2004–2008. Morb Mortal Wkly Rep. 2010;59(23):705–709. [PubMed] [Google Scholar]
- 30.Prevention C for DC and. Vital Signs: Overdoses of Prescription Opioid Pain Relievers and Other Drugs Among Women -- United States, 1999–2010. Morb Mortal Wkly Rep. 2013;62(26):537–542. [PMC free article] [PubMed] [Google Scholar]
- 31.Mura T, Tzourio C, Chevassus H. Chronic use of benzodiazepines and latent cognitive decline in the elderly : Results from the Three-city study. Eur Neuropsychophyarmacology. 2013;23:212–223. doi: 10.1016/j.euroneuro.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 32.Carriere I, Mura T, Peres K, et al. Elderly Benzodiazepine Users at Increased Risk of Activity Limitations : Influence of Chronicity, Indications, and Duration of Action—The Three-City Cohort. Am J Geriatr Psychiatry. 2015;23(8):840–851. doi: 10.1016/j.jagp.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 33.Neutel CI, Skurtveit S, Berg C, Sakshaug S, Centre N. Multiple prescribers in older frequent opioid users–does it mean abuse? 2013;20(3):397–405. [PubMed] [Google Scholar]
- 34.Blazer D, Wu L-T. Non-Prescription Use of Pain Relievers Among Middle Aged and Elderly Community Adults: National Survey on Drug Use and Health. J Am Geriatr Soc. 2009;57(7):1252–1257. doi: 10.1111/j.1532-5415.2009.02306.x.Non-Prescription. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Voyer P, McCubbin M, Cohen D, Lauzon S, Collin J, Boivin C. Unconventional indicators of drug dependence among elderly long-term users of benzodiazepines. Issues Ment Health Nurs. 2004;25(6):603–628. doi: 10.1080/01612840490472138. [DOI] [PubMed] [Google Scholar]
- 36.Voyer P, Roussel ME, Berbiche D, Préville M. Effectively detect dependence on benzodiazepines among community-dwelling seniors by asking only two questions. J Psychiatr Ment Health Nurs. 2010;17(4):328–334. doi: 10.1111/j.1365-2850.2009.01529.x. [DOI] [PubMed] [Google Scholar]
- 37.Gugelmann H, Shofer FS, Meisel ZF, Perrone J. Multidisciplinary intervention decreases the use of opioid medication discharge packs from 2 urban EDs. Am J Emerg Med. 2013;31(9):1343–1348. doi: 10.1016/j.ajem.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 38.Wilsey BL, Fishman SM, Casamalhuapa C, Gupta A. Documenting and improving opioid treatment: the Prescription Opioid Documentation and Surveillance (PODS) System. Pain Med. 2009;10(5):866–877. doi: 10.1111/j.1526-4637.2009.00652.x. [DOI] [PubMed] [Google Scholar]
- 39.Rutkow L, Turner L, Lucas E, Hwang C, Alexander GC. Most primary care physicians are aware of prescription drug monitoring programs, but many find the data difficult to access. Health Aff (Millwood) 2015;34(3):484–492. doi: 10.1377/hlthaff.2014.1085. [DOI] [PubMed] [Google Scholar]
- 40.Islam M, McRae IS. An inevitable wave of prescription drug monitoring programs in the context of prescription opioids: pros, cons and tensions. BMC Pharmacol Toxicol. 2014;15(1):46. doi: 10.1186/2050-6511-15-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cook J, Biyanova T, Thompson R, Coyne J. Older Primary Care Patients’ Willingness to Consider Discontinuation of Chronic Benzodiazepines. Gen Hosp Psychiatry. 2007;29(5):396–401. doi: 10.1016/j.genhosppsych.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kan CC, Breteler MH, van der Ven a H, Zitman FG. Cross-validation of the benzodiazepine dependence self-report questionnaire in outpatient benzodiazepine users. Compr Psychiatry. 2001;42(5):433–439. doi: 10.1053/comp.2001.26275. [DOI] [PubMed] [Google Scholar]
- 43.Cuevas CDELAS, Sanz EJ, Fuente JADELA, Padilla J, Berenguer JC. The Severity of Dependence Scale ( SDS ) as screening test for benzodiazepine dependence : SDS validation study. Addiction. 2000;95(2000):245–250. doi: 10.1046/j.1360-0443.2000.95224511.x. [DOI] [PubMed] [Google Scholar]
- 44.Kalapatapu RK, Sullivan Ma. Prescription use disorders in older adults. Am J Addict. 2011;19(6):515–522. doi: 10.1111/j.1521-0391.2010.00080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gorgels WJMJ, Oude Voshaar RC, Mol a JJ, et al. Predictors of discontinuation of benzodiazepine prescription after sending a letter to long-term benzodiazepine users in family practice. Fam Pract. 2006;23(1):65–72. doi: 10.1093/fampra/cmi065. [DOI] [PubMed] [Google Scholar]
- 46.van de Steeg-van Gompel CHPa, Wensing M, De Smet PaGM. Implementation of a discontinuation letter to reduce long-term benzodiazepine use--a cluster randomized trial. Drug Alcohol Depend. 2009;99(1–3):105–114. doi: 10.1016/j.drugalcdep.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 47.Mol JJ, Oude Voshaar RC, Gorgels WJMJ, et al. The absence of benzodiazepine craving in a general practice benzodiazepine discontinuation trial. Addict Behav. 2006;31(2):211–222. doi: 10.1016/j.addbeh.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 48.Salonoja MA, Salminen MA, Aarnio PE, Vahlberg TERO, Kivelä SII. One-time counselling decreases the use of benzodiazepines and related drugs among community-dwelling older persons. Age Aging. 2010;39(January):313–319. doi: 10.1093/ageing/afp255. [DOI] [PubMed] [Google Scholar]
- 49.Gould RL, Coulson MC, Patel N, Highton-williamson E, Howard RJ. Interventions for reducing benzodiazepine use in older people : meta-analysis of randomised controlled trials. Br J Psychiatry. 2014;204:98–107. doi: 10.1192/bjp.bp.113.126003. [DOI] [PubMed] [Google Scholar]
- 50.Alassaad A, Bertilsson M, Gillespie U, Sundström J, Hammarlund-Udenaes M, Melhus H. The effects of pharmacist intervention on emergency department visits in patients 80 years and older: subgroup analyses by number of prescribed drugs and appropriate prescribing. PLoS One. 2014;9(11):e111797. doi: 10.1371/journal.pone.0111797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kuerbis A, Sacco P. A review of existing treatments for substance abuse among the elderly and recommendations for future directions. Subst Abuse. 2013;7:13–37. doi: 10.4137/SART.S7865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schonfeld L, King-Kallimanis BL, Duchene DM, et al. Screening and brief intervention for substance misuse among older adults: the Florida BRITE project. Am J Public Health. 2010;100(1):108–114. doi: 10.2105/AJPH.2008.149534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ayalon L, Jin C, Mcculloch CE, et al. Integrated specialty mental health care among older minorities improves access but not outcomes : results of the PRISMe study. Int J Geriatr Psychiatry. 2008;23(August):1086–1092. doi: 10.1002/gps. [DOI] [PubMed] [Google Scholar]
- 54.Eden J, Maslow K, Le M, Blazer D Services C. The Mental Health and Substance Use Workforce for Older Adults : In Whose Hands ? AND SUBSTANCE USE WORKFORCE FOR. 2012. [PubMed] [Google Scholar]
- 55.Buck Ja. The looming expansion and transformation of public substance abuse treatment under the Affordable Care Act. Health Aff (Millwood) 2011;30(8):1402–1410. doi: 10.1377/hlthaff.2011.0480. [DOI] [PubMed] [Google Scholar]
- 56.Pating DR, Miller MM, Goplerud E, Martin J, Ziedonis DM. New systems of care for substance use disorders: treatment, finance, and technology under health care reform. Psychiatr Clin North Am. 2012;35(2):327–356. doi: 10.1016/j.psc.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 57.Baldoni ADO, Ayres LR, Martinez EZ, Dewulf NDLS, Dos Santos V, Pereira LRL. Factors associated with potentially inappropriate medications use by the elderly according to Beers criteria 2003 and 2012. Int J Clin Pharm. 2014;36(2):316–324. doi: 10.1007/s11096-013-9880-y. [DOI] [PubMed] [Google Scholar]
- 58.Bashir K, King M, Ashworth M. Controlled evaluation of brief intervention by general practitioners to reduce chronic use of benzodiazepines. Br J Gen Pract. 1994;44(September 1994):408–412. [PMC free article] [PubMed] [Google Scholar]
- 59.Bradley MC, Fahey T, Cahir C, et al. Potentially inappropriate prescribing and cost outcomes for older people: a cross-sectional study using the Northern Ireland Enhanced Prescribing Database. Eur J Clin Pharmacol. 2012;68(10):1425–1433. doi: 10.1007/s00228-012-1249-y. [DOI] [PubMed] [Google Scholar]
- 60.Brown J, Setnik B, Lee K, et al. Assessment, stratification, and monitoring of the risk for prescription opioid misuse and abuse in the primary care setting. 2011 Dec; doi: 10.5055/jom.2011.0088. [DOI] [PubMed] [Google Scholar]
- 61.Cook JM, Biyanova T, Masci C, Coyne JC. Older patient perspectives on long-term anxiolytic benzodiazepine use and discontinuation: a qualitative study. J Gen Intern Med. 2007;22(8):1094–1100. doi: 10.1007/s11606-007-0205-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Huang AR, Mallet L. Prescribing opioids in older people. Maturitas. 2013;74(2):123–129. doi: 10.1016/j.maturitas.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 63.Kuerbis A, Sacco P, Blazer DG, Moore Aa. Substance abuse among older adults. Clin Geriatr Med. 2014;30(3):629–654. doi: 10.1016/j.cger.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lanier WA, Johnson EM, Rolfs RT, et al. Risk Factors for Prescription Opioid-Related Death, Utah, 2008–2009. 2012:1580–1589. doi: 10.1111/j.1526-4637.2012.01518.x. [DOI] [PubMed] [Google Scholar]
- 65.Beaudoin FL, Merchant RC, Clark MA. Prevalence and Detection of Prescription Opioid Misuse and Prescription Opioid Use Disorder among Emergency Department Patients 50 Years of Age and Older: Performance of the Prescription Drug Use Questionnaire, Patient Version. Am J Geriatr Psychiatry. 2016 doi: 10.1016/j.jagp.2016.03.010. In Press. [DOI] [PubMed] [Google Scholar]