Abstract
INTRODUCTION
Ankle proprioception training has been found to improve balance-related gait disorders; yet, the relationship between ankle proprioception and specific gait patterns in older adults with and without impaired balance has not been systematically examined.
METHODS
This study characterizes gait patterns of 230 older adults aged 60 – 95 evaluated in the Baltimore Longitudinal Study of Aging (BLSA) gait laboratory with (n=82) and without impaired balance (inability to successfully complete a narrow walk) and examines ankle proprioception performance.
RESULTS
Participants with impaired balance had a higher angle threshold for perceiving ankle movement than those without impaired balance even after controlling for the substantial age difference between groups (p = 0.017). Gait speed, stride length, hip and ankle range of motion and mechanical work expenditure from the knee and ankle were associated with ankle proprioception performance (p < 0.050 for all) in the full sample, but in stratified analysis these associations were evident only in participants with impaired balance.
CONCLUSION
Ankle proprioception in older persons with balance impairment may play a role in balance related gait disorders and should be targeted for intervention.
Keywords: ankle proprioception, mechanical work expenditure, BLSA gait lab, impaired balance in gait
Introduction
Evaluating gait performance is an important component of monitoring the health of older adults. Analysis of gait performance not only provides insight into health status in older individuals, but also helps detect physiologically abnormal patterns which may lead to unstable locomotion and falls (6, 17). Impaired balance and instability during walking commonly occur in older adults (7, 12) and may directly contribute to falls as well as activity restriction and mobility limitation (8, 19, 22). Overall, age-related gait patterns of older adults are often less efficient for forward locomotion as reflected in constrained kinematic performance including slower speed, shorter stride length, and smaller range of motion of lower extremity joints.
Balance problems are likely to be associated with defects in gait performance that often emerge with aging (9). Balance problems that occur during walking can be easily and quickly assessed using a tandem walk over a defined distance on which poorer performance (low speed and inability to maintain the tandem) has been associated with falling (4, 5). Evaluating the association between performance on this relatively simple balance test and gait parameters assessed in a gait laboratory may help improve understanding of mechanisms that support stability during walking and also identify targets for interventions aimed at improving mobility in older adults. Ankle proprioception, the perception of position and motion of the ankle joint during movement, is essential for precise locomotor control (2, 14). Considering the primary role of ankle proprioception in both sensing and controlling movement of the feet and ankles, ankle proprioception can be crucial for balance and gait (20, 21). Ankle proprioception training has been found to improve balance-related gait disorders (20); yet, the relationship between ankle proprioception and specific gait patterns in older adults with and without impaired balance has not been examined systematically.
The present study examines the relationship between ankle proprioception performance and impaired balance in older adults and explores the hypothesis that poor ankle proprioception is associated with impaired balance during walking. We also examined whether ankle proprioception is associated with gait characteristics indicative of impaired balance.
Methods
Participants
Data were collected on 230 men (53%) and women aged 60 to 92 years evaluated in the Baltimore Longitudinal Study of Aging (BLSA) gait laboratory who had a clinic visit between January 2008 and April 2013. Participants were classified as having impaired balance (N=82) who could not attempt or failed narrow walking (unable to stay within the marked path on any trial) or not (N=148) based on the ability to successfully complete a narrow walk, described below. The BLSA is a continuous enrollment cohort study initiated in 1958 to study normative aging and is currently supported by the Intramural Research Program of the National Institute on Aging, National Institutes of Health. Participants with no hip or knee joint replacements, no report of severe knee osteoarthritis or history of stroke or Parkinson's disease, able to follow instructions and safely walk without using aids were eligible for gait laboratory testing and included in the study. The BLSA protocol was approved by the Institutional Review Board of record at the time of data collection (MedStar Health Research Institute, Baltimore, MD or National Institute of Environmental Health Sciences, NC). Participants were given a detailed description of the study and consented to participate.
Gait laboratory measurements
The procedure for the gait analysis performed in the BLSA gait laboratory has been described previously (11). Briefly, participants were instrumented with 20 reflective markers placed at anatomical landmarks: anterior and posterior superior iliac spines, medial and lateral knees, medial and lateral ankles, toe (second metatarsal head), heel, and lateral wands over the mid-femur and mid-tibia. To avoid errors in hip joint calculation due to excessive adipose tissue of over-weight and obese participants, a tie band was used in the pelvic area, and the distance between left and right anterior superior iliac spines (ASIS) was measured manually. A Vicon 3D motion capture system with 10 digital cameras (Vicon 612 system, Oxford Metrics Ltd., Oxford, U.K.) measured the 3D locations of all markers on the landmarks of lower extremity segments (60 Hz sampling frequency). After all markers were positioned on the skin and non-reflective, form-fitting spandex pants, participants were asked to walk across a 10m long gait laboratory walkway at their self-selected usual speed (“like walking in the street”). Trials were performed until at least 3 complete gait cycles starting from both the left and right sides, with the entire foot landing on the force platform, were obtained (11). Gait parameters were averaged over the successful trials. For the narrow base walk test, participants were asked to walk within a narrow path outlined by tape on the walking surface. The width of narrow path was standardized to 50% of the distance between the subject's ASIS (Anterior Superior Iliac Spines) (18). The raw coordinate data of marker positions were digitally filtered with fourth-order zero-lag Butterworth filter with a cutoff at 6 Hz. For the present study, fundamental gait parameters included gait speed, stride length, step width, and lower extremity joint (hip, knee, and ankle) kinematics (range of motion; ROM) and kinetics (weight normalized mechanical work expenditure for one gait cycle; MWE) in the sagittal plane. MWEs were calculated by numerical integration of joint power for the duration of one gait cycle (11)
Ankle proprioception test
The procedure for the ankle proprioception test in the BLSA has been described previously (10). This test was developed to assess proprioception in the ankle joint by measuring ability to sense movement and control static and dynamic position. Participants included in ankle proprioception test did not report severe pain in their lower limbs during ankle rotations of plantarflexion and dorsiflexion. The current study focuses on the two most reliable performance components of the ankle proprioception test (1, 10). The threshold test assesses the minimal angular displacement (degrees) required for perception of passive movement in the proper direction (plantar flexion or dorsiflexion). The tracking test evaluates the ability to track continuous passive ankle angular rotations in plantar flexion and dorsiflexion produced by the machine on the right ankle by rotating the free pedal of the left ankle. Tracking performance is measured by calculating the normalized cross-correlation at zero lag of the ankle rotation curves of left and right sides, thus higher scores indicate better performance. Averages of two repeated tests were used for both measurement of threshold and tracking.
Statistical analysis
Characteristics of the study population and ankle proprioception scores were compared using general linear regression analysis and were reported as mean values and standard errors separately for persons with and without balance impairment (Table 1). Next, the associations between ankle proprioception and balance impairment were examined before and after covariate adjustment. Lastly, the relationship between ankle proprioception performance and kinematic and kinetic gait parameters were examined in adjusted models with consideration of balance impairment and the interaction of balance impairment (Table 2). All models were adjusted for age, sex, weight and height. Statistical significance was defined using a p value less than 0.05. Statistical analyses were performed with SAS 9.2 Statistical Package (SAS Institute, Inc., Cary, North Carolina, USA).
Table 1.
Characteristics and ankle proprioception performance of participants by balance impairment group
| With Impaired balance (N=82) | Without impaired balance (N=148) | p-value | |
|---|---|---|---|
| mean (SE) | mean (SE) | ||
| Characteristics | |||
| Age, yr | 80 (0.731) | 70 (0.545) | < 0.001 |
| Sex, female (%) | 43 (NA) | 50 (NA) | 0.289 |
| Height, cm | 167.1 (1.0) | 168.5 (0.8) | 0.266 |
| Mass, kg | 76.1 (1.7) | 78.3 (1.3) | 0.316 |
| Ankle proprioception (Without age-adjustment) | |||
| threshold, degree | 1.427 (0.075) | 0.926 (0.056) | < 0.001 |
| Tracking, score | 0.878 (0.006) | 0.905 (0.004) | < 0.001 |
| Ankle proprioception (With age-adjustment) | |||
| threshold, degree | 1.286 (0.087) | 1.005 (0.060) | 0.017 |
| Tracking, score | 0.885 (0.007) | 0.901 (0.005) | 0.100 |
Table 2.
Gait and ankle proprioception (threshold) associations for the participants with impaired and without impaired balance
| Gait parameters | Associations with ankle proprioception (Threshold)a | Group Comparisons | |||||
|---|---|---|---|---|---|---|---|
| whole sample | stratified analysis | Between with impaired and without impaired balance | |||||
| Slope β | p-value | Balance impairment | Slope β | p-value | Mean (SE) | p-value | |
| Spatiotemporal gait parameters | |||||||
| Gait speed, meter/sec. | −0.043 | 0.012 | yes | −0.045 | 0.041 | 1.020 (0.023) | < 0.001 |
| no | −0.016 | 0.530 | 1.150 (0.016) | ||||
| Stride length, meter | −0.046 | < 0.001 | yes | −0.064 | < 0.001 | 1.119 (0.016) | < 0.001 |
| no | −0.003 | 0.843 | 1.221 (0.011) | ||||
| Step width, meter | 0.004 | 0.090 | yes | 0.005 | 0.153 | 0.108 (0.003) | 0.066 |
| no | 0.002 | 0.579 | 0.100 (0.002) | ||||
| Range of motion, degree | |||||||
| Hip | −1.193 | 0.004 | yes | −1.453 | 0.007 | 36.531 (0.558) | 0.029 |
| no | −0.573 | 0.355 | 38.182 (0.387) | ||||
| Knee | −0.292 | 0.516 | yes | −0.441 | 0.446 | 51.424 (0.589) | < 0.001 |
| no | 0.512 | 0.441 | 54.393 (0.409) | ||||
| Ankle | −0.745 | 0.032 | yes | −1.058 | 0.021 | 24.000 (0.472) | 0.164 |
| no | −0.188 | 0.721 | 24.884 (0.328) | ||||
| Mechanical work expenditure, J/kg | |||||||
| Hip Concentric | −0.008 | 0.150 | yes | −0.007 | 0.290 | 0.173 (0.007) | 0.046 |
| no | −0.004 | 0.587 | 0.192 (0.005) | ||||
| Hip Eccentric | −0.005 | 0.705 | yes | −0.011 | 0.501 | 0.427 (0.016) | 0.266 |
| no | −0.002 | 0.925 | 0.402 (0.011) | ||||
| Knee Concentric | −0.004 | 0.289 | yes | −0.001 | 0.855 | 0.082 (0.005) | 0.395 |
| no | −0.007 | 0.217 | 0.088 (0.004) | ||||
| Knee Eccentric | −0.014 | 0.037 | yes | −0.011 | 0.197 | 0.237 (0.009) | < 0.001 |
| no | −0.009 | 0.385 | 0.284 (0.006) | ||||
| Ankle Concentric | −0.016 | 0.007 | yes | −0.020 | 0.011 | 0.271 (0.008) | 0.009 |
| no | −0.006 | 0.504 | 0.298 (0.005) | ||||
| Ankle Eccentric | 0.004 | 0.231 | yes | 0.001 | 0.943 | 0.127 (0.005) | 0.478 |
| no | 0.004 | 0.429 | 0.122 (0.003) | ||||
in threshold, - sign mean positive association with gait parameters because lower threshold score means higher performance
All models are controlled for age, height, weight, and sex
Results
Participants with impaired balance were older (p < 0.001) and had poorer ankle proprioception performance in threshold and tracking (for both; p < 0.001) than those without impaired balance (Table 1). After adjusting for age, ankle proprioception, assessed as movement threshold was still higher in those with impaired balance compared to those without impaired balance (p = 0.017). Participants with impaired balance had slower gait speed (p < 0.001), shorter stride length (p < 0.001), smaller hip and knee ROM (p = 0.029, and p < 0.001, respectively), and lower MWEs in hip (p = 0.046), knee (p < 0.001), and ankle (p = 0.009), compared to the participants without impaired balance (Table 2). In the whole sample, poor ankle proprioception was associated with slower gait speed (β = −0.043; p = 0.012), shorter stride length (β = −0.046; p < 0.001), and smaller ROM from the hip and ankle joints (β = −1.193; p = 0.004, and β = −0.745; p = 0.032, respectively). Poor ankle proprioception was also associated with lower knee eccentric MWE (β = −0.014; p = 0.037) and lower ankle concentric MWE (β = −0.016; p = 0.007). No significant associations between gait parameters and ankle proprioception performance were found in participants without impaired balance. Ankle proprioception indicated by tracking test showed significant association only with stride length (β = 0.557, p = 0.009; for the participants with impaired balance; Table 3).
Table 3.
Gait and ankle proprioception (tracking) associations for the participants with impaired and without impaired balance
| Gait parameters | Associations with ankle proprioception (Tracking)a | Group Comparisons | |||||
|---|---|---|---|---|---|---|---|
| whole sample | stratified analysis | Between with impaired and without impaired balance | |||||
| Slope β | p-value | Balance impairment | Slope β | p-value | Mean (SE) | p-value | |
| Spatiotemporal gait parameters | |||||||
| Gait speed, meter/sec. | 0.144 | 0.499 | yes | 0.053 | 0.862 | 1.020 (0.023) | < 0.001 |
| no | 0.015 | 0.958 | 1.150 (0.016) | ||||
| Stride length, meter | 0.302 | 0.045 | yes | 0.557 | 0.009 | 1.119 (0.016) | < 0.001 |
| no | −0.060 | 0.755 | 1.221 (0.011) | ||||
| Step width, meter | 0.002 | 0.952 | yes | 0.043 | 0.351 | 0.108 (0.003) | 0.066 |
| no | −0.018 | 0.663 | 0.100 (0.002) | ||||
| Range of motion, degree | |||||||
| Hip | 6.213 | 0.224 | yes | 8.164 | 0.281 | 36.531 (0.558) | 0.029 |
| no | 2.181 | 0.750 | 38.182 (0.387) | ||||
| Knee | 1.559 | 0.778 | yes | 10.218 | 0.198 | 51.424 (0.589) | < 0.001 |
| no | −10.163 | 0.157 | 54.393 (0.409) | ||||
| Ankle | 3.208 | 0.456 | yes | 11.223 | 0.078 | 24.000 (0.472) | 0.164 |
| no | −4.624 | 0.422 | 24.884 (0.328) | ||||
| Mechanical work expenditure, J/kg | |||||||
| Hip Concentric | −0.025 | 0.699 | yes | −0.138 | 0.153 | 0.173 (0.007) | 0.046 |
| no | 0.035 | 0.687 | 0.192 (0.005) | ||||
| Hip Eccentric | −0.153 | 0.299 | yes | −0.230 | 0.294 | 0.427 (0.016) | 0.266 |
| no | −0.133 | 0.501 | 0.402 (0.011) | ||||
| Knee Concentric | 0.033 | 0.493 | yes | 0.025 | 0.725 | 0.082 (0.005) | 0.395 |
| no | 0.031 | 0.638 | 0.088 (0.004) | ||||
| Knee Eccentric | −0.009 | 0.912 | yes | 0.145 | 0.222 | 0.237 (0.009) | < 0.001 |
| no | −0.061 | 0.570 | 0.284 (0.006) | ||||
| Ankle Concentric | 0.089 | 0.218 | yes | 0.057 | 0.595 | 0.271 (0.008) | 0.009 |
| no | 0.074 | 0.443 | 0.298 (0.005) | ||||
| Ankle Eccentric | 0.011 | 0.812 | yes | −0.007 | 0.908 | 0.127 (0.005) | 0.478 |
| no | 0.014 | 0.802 | 0.122 (0.003) | ||||
in thracking, - higher tracking score means highs performance
All models are controlled for age, height, weight, and sex
Discussion
Independent of age, ankle proprioception threshold was higher in older adults with impaired balance compared to those without impaired balance as indicated by the inability to maintain a narrow walking path without stepping out. Poorer ankle proprioception performance (higher threshold to discern movement) was also associated with less favorable gait characteristics – specifically slower gait speed, shorter stride length, smaller hip and ankle ROM, higher knee energy absorption and lower ankle energy generation – all of which were also associated with impaired balance. It is important to note, however, that associations of between ankle proprioception with gait characteristics detected in the whole population were driven by the participants with impaired balance. These associations were not evident in participants with intact balance; that is, those who successfully performed the narrow walking test.
Slower gait speed, shorter stride length, and smaller hip ROM in participants with impaired balance, all of which can either reflect deficits in stability or compensatory strategies to reduce forward momentum during locomotion, were associated with poorer ankle proprioception. This finding suggests that poor or diminished awareness of foot rotation in older adults may impact specific gait characteristics associated with balance problems. These results confirm previous studies on the importance of ankle proprioception for precision in motor control (2, 14) and support the relationship between ankle proprioception and balance problems (15).
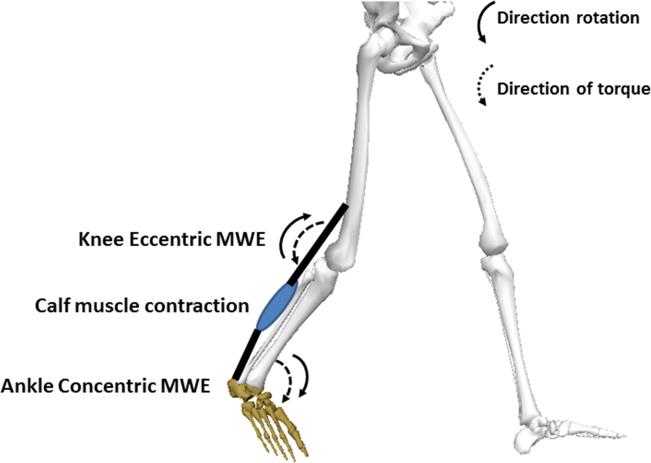
Smaller knee ROM and lower hip concentric MWE were observed in participants with balance impairment, but these measurements of knee kinematics and hip kinetics, were not associated with ankle proprioception. It is interesting to note that these measures of knee kinematics and hip kinetics are controlled by the knee flexors and hip extensors, respectively, and these two gait parameters are commonly governed by the hamstrings. Thus, instead of direct affect from ankle proprioception, these balance related gait pattern differences may be due mainly to weakness in the leg muscles of the thigh. In contrast, poorer ankle proprioception performance was associated with lower knee eccentric and ankle concentric MWE both of which are mainly generated during late stance for knee flexion and ankle plantar flexion, respectively as a function of calf muscle (gastrocnemius) contraction (3) (Figure 1). The observed relationship between ankle proprioception and ankle MWE supports previous observations of the contribution of ankle plantar flexion power to gait characteristics (13, 16). Lower mechanical energy (or work) generation during late stance from ankle and knee joints may explain lower propulsion generation, which limits forward momentum through the swing phase resulting in slower gait speed, shorter stride and smaller ROM, which may result in impaired balance during walking.
Figure 1.
Knee eccentric MWE and ankle concentric MWE during late stance for knee flexion and ankle plantar flexion, respectively.
This study has some limitations. Other factors or impairments such as fear of falling, past fall experience, muscle weakness or plantar cutaneous sensation, which can be related to balance problems in narrow walking were not evaluated in this study. Thus, some portions of associations between ankle proprioception and gait parameters with different narrow walk performance may be partially explained by factors not included in this study. Future studies should consider these and other factors associated with balance problems.
Results suggest that assessing ankle proprioception performance in older adults, especially those with impaired balance may provide important insights for better targeting interventions to improve balance related gait disorders. Deteriorated gait stability in older adults can be better understood by evaluating whether it stems from muscle weakness or is due to a combination of diminished distal awareness of movement and related muscle activations. If the results of present study can be confirmed through longitudinal study, then the use of a simple balance test combined with ankle proprioception evaluation may prove to be a robust pair of assessments for detecting subtle, but important gait deterioration in older adults and may facilitate early intervention for optimal gait performance.
Acknowledgments
This paper was supported by the Intramural Research Program of the NIH, National Institute on Aging and Chonnam National University. Data for these analyses were obtained from the Baltimore Longitudinal Study of Aging, a study performed by the National Institute on Aging. The results of the present study do not constitute endorsement by ACSM.
Footnotes
Conflict of interest:
All the authors declare that no financial or personal relationships were conducted with other people or organizations that could inappropriately influence or bias this work.
References
- 1.Deshpande N, Connelly DM, Culham EG, Costigan PA. Reliability and validity of ankle proprioceptive measures. Arch Phys Med Rehabil. 2003;84(6):883–9. doi: 10.1016/s0003-9993(03)00016-9. [DOI] [PubMed] [Google Scholar]
- 2.Diener HC, Dichgans J. On the role of vestibular, visual and somatosensory information for dynamic postural control in humans. Prog Brain Res. 1988;76:253–62. doi: 10.1016/s0079-6123(08)64512-4. [DOI] [PubMed] [Google Scholar]
- 3.Francis CA, Lenz AL, Lenhart RL, Thelen DG. The modulation of forward propulsion, vertical support, and center of pressure by the plantarflexors during human walking. Gait Posture. 2013;38(4):993–7. doi: 10.1016/j.gaitpost.2013.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gunter KB, White KN, Hayes WC, Snow CM. Functional mobility discriminates nonfallers from one-time and frequent fallers. J Gerontol A Biol Sci Med Sci. 2000;55(11):M672–6. doi: 10.1093/gerona/55.11.m672. [DOI] [PubMed] [Google Scholar]
- 5.Hiura M, Nemoto H, Nishisaka K, Higashi K, Katoh T. The association between walking ability and falls in elderly Japanese living in the community using a path analysis. Journal of community health. 2012;37(5):957–62. doi: 10.1007/s10900-011-9531-y. [DOI] [PubMed] [Google Scholar]
- 6.Jin B, Thu TH, Baek E, et al. Walking-age analyzer for healthcare applications. IEEE journal of biomedical and health informatics. 2014;18(3):1034–42. doi: 10.1109/JBHI.2013.2296873. [DOI] [PubMed] [Google Scholar]
- 7.Kelly VE, Schrager MA, Price R, Ferrucci L, Shumway-Cook A. Age-associated effects of a concurrent cognitive task on gait speed and stability during narrow-base walking. J Gerontol A Biol Sci Med Sci. 2008;63(12):1329–34. doi: 10.1093/gerona/63.12.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ko SU, Gunter KB, Costello M, et al. Stride width discriminates gait of side-fallers compared to other-directed fallers during overground walking. J Aging Health. 2007;19(2):200–12. doi: 10.1177/0898264307299308. [DOI] [PubMed] [Google Scholar]
- 9.Ko SU, Hausdorff JM, Ferrucci L. Age-associated differences in the gait pattern changes of older adults during fast-speed and fatigue conditions: results from the Baltimore longitudinal study of ageing. Age Ageing. 2010;39(6):688–94. doi: 10.1093/ageing/afq113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ko SU, Simonsick E, Deshpande N, Ferrucci L. Sex-specific age associations of ankle proprioception test performance in older adults: results from the Baltimore Longitudinal Study of Aging. Age Ageing. 2015;44(3):485–90. doi: 10.1093/ageing/afv005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ko SU, Stenholm S, Chia CW, Simonsick EM, Ferrucci L. Gait pattern alterations in older adults associated with type 2 diabetes in the absence of peripheral neuropathy--results from the Baltimore Longitudinal Study of Aging. Gait & posture. 2011;34(4):548–52. doi: 10.1016/j.gaitpost.2011.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krasovsky T, Banina MC, Hacmon R, Feldman AG, Lamontagne A, Levin MF. Stability of gait and interlimb coordination in older adults. J Neurophysiol. 2012;107(9):2560–9. doi: 10.1152/jn.00950.2011. [DOI] [PubMed] [Google Scholar]
- 13.Kulmala JP, Korhonen MT, Kuitunen S, et al. Which muscles compromise human locomotor performance with age? Journal of the Royal Society. Interface / the Royal Society. 2014;11(100):20140858. doi: 10.1098/rsif.2014.0858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lephart SM, Pincivero DM, Rozzi SL. Proprioception of the ankle and knee. Sports Med. 1998;25(3):149–55. doi: 10.2165/00007256-199825030-00002. [DOI] [PubMed] [Google Scholar]
- 15.Park YH, Kim YM, Lee BH. An ankle proprioceptive control program improves balance, gait ability of chronic stroke patients. Journal of physical therapy science. 2013;25(10):1321–4. doi: 10.1589/jpts.25.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rijken NH, van Engelen BG, de Rooy JW, Weerdesteyn V, Geurts AC. Gait propulsion in patients with facioscapulohumeral muscular dystrophy and ankle plantarflexor weakness. Gait Posture. 2015;41(2):476–81. doi: 10.1016/j.gaitpost.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 17.Sawers A, Ting LH. Beam walking can detect differences in walking balance proficiency across a range of sensorimotor abilities. Gait Posture. 2015;41(2):619–23. doi: 10.1016/j.gaitpost.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 18.Schrager MA, Kelly VE, Price R, Ferrucci L, Shumway-Cook A. The effects of age on medio-lateral stability during normal and narrow base walking. Gait Posture. 2008;28(3):466–71. doi: 10.1016/j.gaitpost.2008.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Soto-Varela A, Faraldo-Garcia A, Rossi-Izquierdo M, et al. Can we predict the risk of falls in elderly patients with instability? Auris, nasus, larynx. 2015;42(1):8–14. doi: 10.1016/j.anl.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 20.Sterling DA, O'Connor JA, Bonadies J. Geriatric falls: Injury severity is high and disproportionate to mechanism. J Trauma. 2001;50(1):116–9. doi: 10.1097/00005373-200101000-00021. [DOI] [PubMed] [Google Scholar]
- 21.Tromp AM, Pluijm SM, Smit JH, Deeg DJ, Bouter LM, Lips P. Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. Journal of clinical epidemiology. 2001;54(8):837–44. doi: 10.1016/s0895-4356(01)00349-3. [DOI] [PubMed] [Google Scholar]
- 22.Wright RL, Peters DM, Robinson PD, Watt TN, Hollands MA. Older adults who have previously fallen due to a trip walk differently than those who have fallen due to a slip. Gait Posture. 2015;41(1):164–9. doi: 10.1016/j.gaitpost.2014.09.025. [DOI] [PubMed] [Google Scholar]