Abstract
Purpose
Lower urinary tract symptoms (LUTS) are common in the United States leading to a significant economic, quality-of-life, and public health burden. This burden will increase as the population ages and risk factors for LUTS such as diabetes and obesity remain highly prevalent. Improving clinical management and establishing the knowledge base to prevent LUTS will require a comprehensive research approach that examines factors beyond the lower urinary tract (LUT). While the study of these “extra-LUT” factors has increased recently, current urologic research does not systematically account for the broad set of potential LUTS contributors that span biologic, behavioral, psychological/executive function, and sociocultural factors. A comprehensive assessment of potential contributors to LUTS risk, treatment response, and progression is necessary to reduce the burden of this condition within the United States.
Materials and Methods
We consider challenges to continuing the predominantly LUT dysfunctioncentric approach that has dominated previous LUTS research, and propose a new, comprehensive framework for future urology research that includes a broader set of potential LUTS contributors.
Results and Conclusions
This comprehensive approach should help reduce the medical and economic burden of LUTS in the U.S. population.
Keywords: Lower Urinary Tract Symptoms, Behavioral Medicine, Psychological Factors, Executive Function, Social Determinants of Health
Introduction
Lower Urinary Tract Symptoms (LUTS)—including urinary incontinence, urinary frequency, urgency, nocturia, bladder pain and voiding difficulties—are common, especially in older adults. It has been estimated that more than 30 million Americans experienced LUTS in 2000.1 By 2025, with aging of the U.S. population, the prevalence of LUTS is expected to increase to more than 42 million.1 The impact of LUTS is substantial. Individuals who experience LUTS report similarly low quality of life scores to diabetes, hypertension, cancer, and—in severe cases—heart attack and stroke.2 In addition to reducing quality of life, LUTS is associated with important public health outcomes, though further research is needed to determine causal relationships. Individuals who experience LUTS are less likely than individuals with normal bladder function to achieve recommended levels of physical activity,3 and women with LUTS have reported their symptoms as a barrier to physical activity and a contributor to weight gain.4 As a potential barrier to physical activity, LUTS may increase the risk for obesity and related conditions, which is consistent with the strong association between urinary incontinence and both obesity5-8 and diabetes9,10 in women. Among the elderly, nocturia and urgency may increase risk for falls and fractures.11,12 Additionally, LUTS may increase social isolation.13
The lower urinary tract (LUT)—defined anatomically as the bladder and urethra, or functionally, as the bladder, urethra, pelvic floor muscles, prostate gland and afferent/efferent nerve supply—stores and evacuates urine. Because past research has emphasized characterization of LUT dysfunction (e.g., storage, voiding and post-micturition symptoms) rather than normal function, our understanding of the latter is limited. LUTS may not result solely from LUT dysfunction but also may be affected by other factors, such as co-morbid conditions and behavior. As examples, prostate enlargement can interfere with voiding and nocturnal polyuria may result from renal or cardiac failure rather than abnormalities in bladder storage or emptying. Similarly, a rectum distended with stool following use of narcotics may precipitate significant voiding difficulties in the absence of obstruction of the bladder neck or urethra.
The urology research community has made significant advances in LUT dysfunction-centered research in recent decades. However, a broader framework for assessing LUTS risk beyond dysfunction of the LUT has yet to be developed and subsequently integrated into clinical practice or research. Such a framework will likely contribute to greater understanding of the contributors of LUTS and may eventually lead to approaches to prevent these conditions. We advocate that the urology research community must expand their foundation of LUT-centric research to a broader set of extra-LUT factors. Indeed, continuing the narrow focus on LUT dysfunction that has dominated LUTS research to date may hinder future understanding of LUTS risk and management. We consider challenges with continuing a predominantly LUT dysfunction-centric approach to urology research and establish a comprehensive framework for consideration of LUT and extra-LUT factors in future studies of LUTS.
Challenges with Current Treatment of LUTS
Major advances have been made over the past several decades in the management of men and women with LUTS who present for care. These treatments span the spectrum of modalities and include behavioral therapy, drugs, neuromodulation, surgery, and biologics, among others. Despite these improvements, there remains considerable opportunity to reduce the burden of LUTS. Persons who seek treatment represent only a small segment of the population who suffer from LUTS, leaving many individuals who may benefit from treatment undiagnosed and untreated.14-17 Importantly, individuals who do not seek treatment often adopt negative coping behaviors (e.g., fluid manipulation) that may compromise overall health.18 While some individuals choose not to seek treatment because of minimal bother,19 others avoid care because of shame,20 misperceptions about the inevitability of LUTS,19 and lack of information about available treatment.19 Among treated patients, drug side effects (e.g., dry mouth, constipation, reduced ejaculation), morbidity associated with surgery, co-morbid illnesses, cost and many other factors can negate the benefits of intervention across LUTS conditions. For urinary incontinence (UI), first-line treatments—including pelvic floor muscle training for stress UI (SUI) and behavioral therapy for urgency UI (UUI)—improve outcomes in many patients21 but depend in large part on the patient's ability to self-manage, which is affected by psychological, cognitive, and social factors. Many second and third-line treatments for SUI and UUI have inconsistent outcomes, uncertain durability, and high risk of complications.21,22 For LUTS associated with benign prostatic hyperplasia (BPH), randomized clinical trials (RCT) have demonstrated the efficacy of commonly used pharmacologic therapies in men, but the beneficial effects of treatment may not be generalizable, can be costly because of long-term use, and produce numerous, often intolerable side-effects, which reduces adherence.23 For interstitial cystitis/bladder pain syndrome (IC/BPS) and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), numerous medical interventions have been proposed; however, effective treatment remains elusive. Because IC/BPS and CP/CPPS commonly occur with non-urologic chronic pain conditions (e.g., fibromyalgia, irritable bowel syndrome, chronic fatigue syndrome)24 that likely complicate treatment approaches, a comprehensive approach to assess and treat patients with these syndromes may lead to better clinical management and possibly to development of more effective therapies.
Because therapies developed based on a narrow LUT-centric view of LUTS often achieve limited and inconsistent success, we suggest a broader approach to LUTS research may be warranted. Indeed, such comprehensive assessments may yield a better understanding of factors associated with increased risk and/or severity of LUTS. We propose such assessments must be undertaken if the burden of LUTS in the U.S. population is to be reduced in the coming years, including among persons who may benefit from but do not seek care.
Establishing a Comprehensive Framework to Understand LUTS
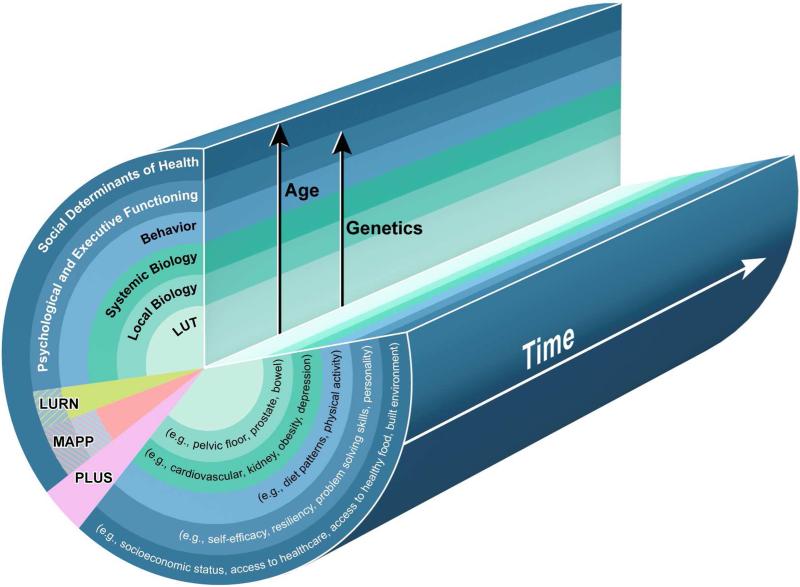
To expand our thinking for potential contributors to LUTS, we conceptualized a new multi-level framework (Figure 1). Beginning in the center and expanding outward, the framework shows a comprehensive view of potential contributors to LUTS from most to least studied. The LUT—where much of the prior research in LUTS has focused—comprises the center of the framework, followed by local (e.g., reproductive organs, pelvic floor myofascial support, rectum and vulvovaginal tissues) and systemic (e.g., cardiovascular, renal, neuropsychiatric, metabolic, musculoskeletal) biologic factors. The next level moves beyond biologic considerations to behavioral factors, such as diet, level of physical activity, and decisions about when to use the toilet. Less well studied than behavioral considerations are factors relating to psychology and executive functioning, including personality traits, self-efficacy, resiliency, and problem-solving ability. Finally, social determinants, defined as the “conditions in which people are born, grow, live, work and age”25 (e.g., socioeconomic status, access to healthcare, culture, availability of healthy food, environment), have received limited evaluation as potential contributors to LUTS. This framework aims to broaden research to consider a comprehensive set of potential LUTS contributors and to engage a broad range of researchers (from urologists and urogynecologists to primary care providers, internal medicine subspecialists, behavioral medicine experts, nurses, social workers, epidemiologists, and public health professionals) in the investigation of as many extra-LUT factors as possible in future research, with the ultimate goal of improving clinical care and prevention.
Figure 1. A Multi-level Framework for Considering Potential Causes and Contributors to LUTS.
This schematic shows a comprehensive view of potential contributors to LUTS from the well-studied lower urinary tract at the center, to those increasingly less studied in each successive ring emanating from the center. Prior studies that have considered factors outside of LUT dysfunction have mostly focused on biologic domains, including local and systemic biology. There has been limited research on behavioral factors, such as diet, level of physical activity, and decisions about when to use the toilet. Even less well-studied are factors relating to psychology and executive functioning—including personality traits, self-efficacy, resiliency, and problem-solving ability—and social determinants of health (e.g., socioeconomic status, access to healthcare, availability of healthy food, environment). The NIDDK has promoted a shift in emphasis so that the major research studies of LUTS it supports—MAPP, LURN, and PLUS—now include a more comprehensive assessment of factors. The factors included in these “rings” often interact with each other. Factors across all rings of the schematic are influenced by age of the person and the time or duration of exposure, and several (e.g., LUT and local biology, systemic biology, behavior, and psychological and executive functioning) may be influenced by genetics.
Many of the “rings” in this framework interact or overlap. For example, postponement of urination or defecation is a behavioral factor that may result from an environmental factor, such as toilet access or cleanliness. Additionally, factors such as genetics, time and age may influence multiple levels of this schematic.
The State of Research on Potential Extra-LUT Contributors to LUTS
There has been some recognition of the importance of extra-LUT factors to LUTS. For example, the “DIAPPERS” mnemonic (delirium, infection, atrophic urogenital tissues, pharmaceuticals, psychological disorders, endocrine disorders, restricted mobility, stool impaction), which reminds clinicians to consider systemic issues such as depression and restricted mobility in assessing LUTS in the elderly,26 was proposed 30 years ago. However, the mnemonic has seen limited application in research and its use in clinical care has been primarily limited to geriatric populations. Further, current consideration of extra-LUT factors remains primarily limited to biologic factors (such as immune system mediators and central pain processing), rather than cognitive, psychological, or social determinants. Interest in identifying lifestyle and co-morbid conditions (primarily obesity, diabetes and metabolic syndrome) that are associated with the risk of LUTS and/or its severity has emerged only recently. As an example, the Boston Area Community Health (BACH) Survey27 enrolled approximately 5,500 men and women over a relatively broad age range and studied urologic signs and symptoms (questionnaires focused on assessing symptoms of BPH/LUTS, CP/CPPS, IC, UI and erectile dysfunction) over a period of about 7 years. This investigation was unique in that it was population based and assessed a broad range of factors including socio-demographic characteristics, health care access/utilization, lifestyle/behavioral, psychosocial factors, health status, physical measures, and biochemical parameters. Subsequently, BACH investigators have reported on a broad array of factors associated with LUTS including beverages,28 vitamins and minerals,29 psychoactive medications,30 dietary macronutrients, cholesterol and sodium,29,31 physical activity, smoking and alcohol consumption32 and vitamin C.33 There is worldwide interest in lifestyle factors with individual studies conducted in England,34,35 Japan,36 Taiwan,37 Australia,38,39 Norway,40 China,41,42 and Korea,43 as well as across multiple countries.44
Most of our understanding of extra-LUT factors as potential contributors to LUTS is derived from observational epidemiological studies, many of which were cross-sectional, limiting inference of the findings. Importantly, RCTs have been conducted only infrequently to assess the benefits of lifestyle changes on LUTS. For example, the Ambulatory Treatments for Leakage Associated with Stress Incontinence trial showed that a pessary with or without pelvic floor muscle training could be used to treat SUI,45 and the Program To Reduce Incontinence by Diet and Exercise demonstrated that moderate weight loss among overweight and obese women reduced UI.46 The early, exploratory efforts—often underpowered, single site, single population studies—that comprise the majority of existing extra-LUT research support expanded focus in this area. However, aside from pelvic floor muscle training and weight loss in UI, increased evidence is required to justify the effort (potential side effects, cost, etc.) to intervene on the majority of non-LUT factors to reduce the impact of LUTS both at the patient and population level.
Over the past eight years, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) has promoted a shift in emphasis so that the major research studies of LUTS it supports now include a more comprehensive assessment of factors (Figure 1):
The Multidisciplinary Approach to the Study of Chronic Pelvic Pain (MAPP) Research Network (http://www.mappnetwork.org), established in 2008, is broadly assessing potential contributors to several urologic chronic pelvic pain syndrome clinical phenotypes. These include systemic biological factors; the interplay between co-occurring urologic and non-urologic conditions (e.g., fibromyalgia, irritable bowel syndrome, chronic fatigue syndrome); and psychosocial determinants such as depression and anxiety, among others. The phenotypes identified through the MAPP Research Network may improve targeting of existing treatment strategies and inform future research to evaluate novel treatment targets.
The Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN, https://nihlurn.org), begun in 2012, is considering behavioral (e.g., diet, fluid intake, tobacco use, physical activity) and psychological (e.g., psychological disorders, coping) factors as potential contributors to LUTS. Recently, LURN conducted a systematic literature review (personal communication, Dr. Catherine Bradley) to evaluate non-LUT factors as potential contributors to LUTS. Three major non-LUT factor groups were identified: a) lifestyle, food and beverage consumption, psychological and social factors, b) pelvic function, and c) health characteristics and medications. Under lifestyle, consumption, psychological and social factors, studies of 14 categories of factors were identified including: diet, fluid intake, alcohol intake, caffeine intake, tobacco use, work schedule, physical activity, mindfulness/meditation, sleep disorders, psychological disorders, physiological stress, history of trauma, coping, and social support. The review—which consisted of an initial screening followed with evidence grading by two independent experts—identified only 472 relevant studies of the 2,064 studies generated in initial search results. The extent of evidence varied substantially; weak for most of the categories, and moderate in some. However, despite the lack of governmental funding for this research, the extensive volume of existing data suggests that extra-LUT factors are important and provides an impetus for their further study.
The Prevention of Lower Urinary Tract Symptoms in Women (PLUS) Research Consortium (http://grants.nih.gov/grants/guide/rfa-files/RFA-DK-14-004.html)—launched in September 2015—will comprehensively address extra-LUT factors among women. The Consortium includes researchers with broad expertise in nursing, urology, urogynecology, pediatrics, adolescent health, obstetrics-gynecology, geriatrics, psychology, epidemiology, and public health. The goals of this Consortium are to define bladder health, identify risk factors for LUTS, and conduct future prevention research based on behavioral and psychosocial/executive function factors and social determinants of health.
Opportunities for Expanding LUTS Research
To significantly advance our understanding of LUTS, we suggest that urology researchers must take the lead in developing a body of evidence that encompasses a comprehensive set of potential extra-LUT contributors to LUTS. This can be accomplished through qualitative research to identify relevant patient-centered concerns, ongoing and future epidemiologic research, and RCTs for selected factors where strong associations and potential mechanisms of action have been identified. These studies must move beyond the exploratory nature of existing research to include investigations of sufficient size and ethnic/racial diversity. Subsequently, effective methods to disseminate and implement research findings into clinical care must be identified.
Developing this body of research represents a significant challenge; however, several opportunities exist that will facilitate a more comprehensive approach to LUTS research:
Adapting and testing interventions shown to be successful for other diseases/conditions
Urologic and urogynecologic investigators have an opportunity to learn from research in other chronic diseases. Fields outside of urology have embraced this comprehensive perspective, expanding research to consider the role of non-biologic factors in disease etiology and management. This research has yielded insights that have enhanced clinical practice and ultimately improved patient outcomes. In diabetes, behavioral factors are well integrated into research and clinical prevention interventions. The contribution of behavioral factors to diabetes risk and prevention has been well documented through the Diabetes Prevention Program (DPP), which showed that weight loss achieved through dietary modification and increased physical activity reduced the risk of diabetes onset among individuals at risk for the disease.47,48 Even before this landmark study, Medicare began providing reimbursement for diabetes self-management training provided by a qualified clinician—including non-physician providers such as diabetes educators.49 Obesity research has identified psychological and executive function factors such as mindfulness50 and negative affect51 as potential positive and negative contributors to loss of control eating in children—a precursor to adult binge-eating disorders. Leading health organizations—including the World Health Organization,25 the U.S. Department of Health and Human Services,52 and the Institute of Medicine (IOM)53—recognize the important role social determinants play in disease prevention and management. The role of social determinants of health is being explored through research in numerous disease areas, including diabetes,54 chronic kidney disease,55 and cardiovascular disease.56 Adapting findings from other diseases to study non-biologic factors for LUTS holds great promise.
Collaboration within and beyond the urologic and urogynecologic communities
Much of the past research on LUTS has been carried out by urologists and urogynecologists without broader cross-discipline collaboration. A more comprehensive approach to LUTS research will require trans-disciplinary efforts led by urologists or urogynecologists and incorporating expertise from a variety fields, including other medical specialties, behavioral science, psychology, and public health. For example, musculoskeletal strengthening interventions that reduce falls and fractures in the elderly and other high risk populations have the potential to improve LUTS by helping individuals with functional urinary incontinence to reach the bathroom in time. However, exploring a potential connection would require urology specialists to work with musculoskeletal experts to properly design studies. In turn, urology specialists must engage researchers from relevant fields outside of urology to incorporate LUTS into their ongoing research efforts. For example, cardiologists and nephrologists should partner with urology researchers to consider urinary incontinence as a barrier to adherence to diuretics among heart and kidney disease patients.
Focusing on factors that may be more readily incorporated into LUTS research and care
Some extra-LUT factors may require less effort to incorporate into research and clinical care than others and therefore may more readily be implemented into research and ultimately care. For example, the close relationship between rectal distention and bladder dysfunction in children is well known and interventions to improve rectal emptying are integral to treatment of bladder conditions by pediatricians;57,58 However, rectal distention has yet to be evaluated as a risk or promoting factor for LUTS in adults or as an impediment to successful treatment. Additionally, a questionnaire for assessment of the impact of dietary factors on LUTS in IC/BPS has been developed but not incorporated into research.59
Conclusion
Despite growing interest in the role of extra-LUT factors in LUTS, there remains a need to incorporate these factors in future research. To date, scientific advances for improving the treatment, management, mitigation and ultimately prevention of LUTS has likely been slowed by a narrow focus on LUT dysfunction. We encourage a comprehensive approach to the study of LUTS and have begun this process as evidenced by the research focus of three NIDDK supported urology research networks. This comprehensive approach includes local and systemic biology, as well as behavior, psychology and executive functioning, and social determinants of health. The approach will be facilitated by the LUT specialists taking the lead in incorporating other research perspectives into LUT research through 1) adaptation and testing of interventions shown to be effective in other diseases/conditions, 2) collaboration within and beyond the urologic and urogynecologic communities, and 3) early focus on factors that may be more readily incorporated into research and routine clinical care. We hope that investigators will consider this expanded perspective in all future research independent of funding source. This will require active outreach to other specialties and research disciplines. We anticipate that research findings from a comprehensive assessment of factors that potentially underlie LUTS risk and progression will likely take time; however, the long-term benefit will lead to improved clinical care and a reduction in the burden of these highly prevalent conditions in the U.S. population.
Acknowledgments
The authors have no relevant financial interests, activities, relationships, or affiliations to disclose.
Key of Definitions for Abbreviations
- BACH
Boston Area Community Health Survey
- BPH
benign prostatic hyperplasia
- CP/CPPS
chronic prostatitis/chronic pelvic pain syndrome
- DPP
Diabetes Prevention Program
- IC/BPS
interstitial cystitis/bladder pain syndrome
- IOM
Institute of Medicine
- LURN
the Symptoms of Lower Urinary Tract Dysfunction Research Network
- LUT
lower urinary tract
- LUTS
lower urinary tract symptoms
- MAPP
the Multidisciplinary Approach to the Study of Chronic Pelvic Pain Research Network
- NIDDK
National Institute of Diabetes and Digestive and Kidney Diseases
- PLUS
the Prevention of Lower Urinary Tract Symptoms in Women Research Consortium
- RCT
randomized clinical trials
- SUI
stress urinary incontinence
- UI
urinary incontinence
- UUI
urgency urinary incontinence
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Litman HJ, McKinlay JB. The future magnitude of urological symptoms in the USA: projections using the Boston Area Community Health survey. BJU international. 2007;100(4):820. doi: 10.1111/j.1464-410X.2007.07018.x. [DOI] [PubMed] [Google Scholar]
- 2.Robertson C, Link CL, Onel E, et al. The impact of lower urinary tract symptoms and comorbidities on quality of life: the BACH and UREPIK studies. BJU international. 2007;99(2):347. doi: 10.1111/j.1464-410X.2007.06609.x. [DOI] [PubMed] [Google Scholar]
- 3.Coyne KS, Sexton CC, Clemens JQ, et al. The impact of OAB on physical activity in the United States: results from OAB-POLL. Urology. 2013;82(4):799. doi: 10.1016/j.urology.2013.05.035. [DOI] [PubMed] [Google Scholar]
- 4.Dmochowski RR, Newman DK. Impact of overactive bladder on women in the United States: results of a national survey. Current medical research and opinion. 2007;23(1):65. doi: 10.1185/030079907X159533. [DOI] [PubMed] [Google Scholar]
- 5.Hall SA, Cinar A, Link CL, et al. Do urological symptoms cluster among women? Results from the Boston Area Community Health Survey. BJU international. 2008;101(10):1257. doi: 10.1111/j.1464-410X.2008.07557.x. [DOI] [PubMed] [Google Scholar]
- 6.Maserejian NN, Minassian VA, Chen S, et al. Treatment status and risk factors for incidence and persistence of urinary incontinence in women. International urogynecology journal. 2014;25(6):775. doi: 10.1007/s00192-013-2288-3. [DOI] [PubMed] [Google Scholar]
- 7.Tennstedt SL, Link CL, Steers WD, et al. Prevalence of and risk factors for urine leakage in a racially and ethnically diverse population of adults: the Boston Area Community Health (BACH) Survey. American journal of epidemiology. 2008;167(4):390. doi: 10.1093/aje/kwm356. [DOI] [PubMed] [Google Scholar]
- 8.Link CL, Steers WD, Kusek JW, et al. The association of adiposity and overactive bladder appears to differ by gender: results from the Boston Area Community Health survey. The Journal of urology. 2011;185(3):955. doi: 10.1016/j.juro.2010.10.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang R, Lefevre R, Hacker MR, et al. Diabetes, Glycemic Control, and Urinary Incontinence in Women. Female pelvic medicine & reconstructive surgery. 2015;21(5):293. doi: 10.1097/SPV.0000000000000193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weinberg AE, Leppert JT, Elliott CS. Biochemical Measures of Diabetes are Not Independent Predictors of Urinary Incontinence in Women. The Journal of urology. 2015 doi: 10.1016/j.juro.2015.06.074. [DOI] [PubMed] [Google Scholar]
- 11.Lee A, Lee KW, Khang P. Preventing falls in the geriatric population. The Permanente journal. 2013;17(4):37. doi: 10.7812/TPP/12-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hunter K, Voaklander D, Hsu Z, et al. Lower urinary tract symptoms and falls risk among older women receiving home support: a prospective cohort study. BMC Geriatrics. 2013;13(1):46. doi: 10.1186/1471-2318-13-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fonda D. Promoting continence as a health issue. European urology. 1997;32(Suppl 2):28. [PubMed] [Google Scholar]
- 14.Burgio KL, Ives DG, Locher JL, et al. Treatment seeking for urinary incontinence in older adults. Journal of the American Geriatrics Society. 1994;42(2):208. doi: 10.1111/j.1532-5415.1994.tb04954.x. [DOI] [PubMed] [Google Scholar]
- 15.Kinchen KS, Burgio K, Diokno AC, et al. Factors associated with women's decisions to seek treatment for urinary incontinence. Journal of women's health. 2002;12(7):687. doi: 10.1089/154099903322404339. 2003. [DOI] [PubMed] [Google Scholar]
- 16.Chong C, Fong L, Lai R, et al. The prevalence of lower urinary tract symptoms and treatment-seeking behaviour in males over 40 years in Singapore: a community-based study. Prostate cancer and prostatic diseases. 2012;15(3):273. doi: 10.1038/pcan.2011.69. [DOI] [PubMed] [Google Scholar]
- 17.Jimenez-Cidre M, Costa P, Ng-Mak D, et al. Assessment of treatment-seeking behavior and healthcare utilization in an international cohort of subjects with overactive bladder. Current medical research and opinion. 2014;30(8):1557. doi: 10.1185/03007995.2014.918028. [DOI] [PubMed] [Google Scholar]
- 18.Elstad EA, Maserejian NN, McKinlay JB, et al. Fluid manipulation among individuals with lower urinary tract symptoms: a mixed methods study. Journal of clinical nursing. 2011;20(1-2):156. doi: 10.1111/j.1365-2702.2010.03493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Welch LC, Taubenberger S, Tennstedt SL. Patients' experiences of seeking health care for lower urinary tract symptoms. Research in nursing & health. 2011;34(6):496. doi: 10.1002/nur.20457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nicolson P, Kopp Z, Chapple CR, et al. It's just the worry about not being able to control it! A qualitative study of living with overactive bladder. British journal of health psychology. 2008;13(Pt 2):343. doi: 10.1348/135910707X187786. [DOI] [PubMed] [Google Scholar]
- 21.MacLachlan LS, Rovner ES. New treatments for incontinence. Advances in chronic kidney disease. 2015;22(4):279. doi: 10.1053/j.ackd.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 22.Chohan N, Hilton P, Brown K, et al. Efficacy and duration of response to botulinum neurotoxin A (onabotulinumA) as a treatment for detrusor overactivity in women. International urogynecology journal. 2015 doi: 10.1007/s00192-015-2751-4. [DOI] [PubMed] [Google Scholar]
- 23.Gupta K, Yezdani M, Sotelo T, et al. A synopsis of drugs currently in preclinical and early clinical development for the treatment of benign prostatic hyperplasia. Expert opinion on investigational drugs. 2015;24(8):1059. doi: 10.1517/13543784.2015.1048333. [DOI] [PubMed] [Google Scholar]
- 24.Rodriguez MA, Afari N, Buchwald DS. Evidence for overlap between urological and nonurological unexplained clinical conditions. The Journal of urology. 2009;182(5):2123. doi: 10.1016/j.juro.2009.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization What are social determinants of health? Secondary World Health Organization. What are social determinants of health? 2015 http://www.who.int/social_determinants/sdh_definition/en/
- 26.Resnick NM. Urinary incontinence in the elderly. Hospital practice (Office ed) 1986;21(11):80C. [PubMed] [Google Scholar]
- 27.Piccolo RS, Araujo AB, Pearce N, et al. Cohort profile: the Boston Area Community Health (BACH) survey. International journal of epidemiology. 2014;43(1):42. doi: 10.1093/ije/dys198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maserejian NN, Wager CG, Giovannucci EL, et al. Intake of caffeinated, carbonated, or citrus beverage types and development of lower urinary tract symptoms in men and women. American journal of epidemiology. 2013;177(12):1399. doi: 10.1093/aje/kws411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maserejian NN, Giovannucci EL, McVary KT, et al. Intakes of vitamins and minerals in relation to urinary incontinence, voiding, and storage symptoms in women: a cross-sectional analysis from the Boston Area Community Health survey. European urology. 2011;59(6):1039. doi: 10.1016/j.eururo.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hall SA, Maserejian NN, Link CL, et al. Are commonly used psychoactive medications associated with lower urinary tract symptoms? European journal of clinical pharmacology. 2012;68(5):783. doi: 10.1007/s00228-011-1170-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maserejian NN, Giovannucci EL, McKinlay JB. Dietary macronutrients, cholesterol, and sodium and lower urinary tract symptoms in men. European urology. 2009;55(5):1179. doi: 10.1016/j.eururo.2008.07.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maserejian NN, Kupelian V, Miyasato G, et al. Are physical activity, smoking and alcohol consumption associated with lower urinary tract symptoms in men or women? Results from a population based observational study. The Journal of urology. 2012;188(2):490. doi: 10.1016/j.juro.2012.03.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Curto TM, Giovannucci EL, McKinlay JB, et al. Associations between supplemental or dietary intake of vitamin C and severity of lower urinary tract symptoms. BJU international. 2015;115(1):134. doi: 10.1111/bju.12653. [DOI] [PubMed] [Google Scholar]
- 34.McGrother CW, Donaldson MM, Thompson J, et al. Etiology of overactive bladder: a diet and lifestyle model for diabetes and obesity in older women. Neurourology and urodynamics. 2012;31(4):487. doi: 10.1002/nau.21200. [DOI] [PubMed] [Google Scholar]
- 35.Dallosso HM, Matthews RJ, McGrother CW, et al. The association of diet and other lifestyle factors with the onset of overactive bladder: a longitudinal study in men. Public health nutrition. 2004;7(7):885. doi: 10.1079/phn2004627. [DOI] [PubMed] [Google Scholar]
- 36.Masue T, Wada K, Nagata C, et al. Lifestyle and health factors associated with stress urinary incontinence in Japanese women. Maturitas. 2010;66(3):305. doi: 10.1016/j.maturitas.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 37.Yeh HC, Liu CC, Lee YC, et al. Associations of the lower urinary tract symptoms with the lifestyle, prostate volume, and metabolic syndrome in the elderly males. The aging male : the official journal of the International Society for the Study of the Aging Male. 2012;15(3):166. doi: 10.3109/13685538.2012.669437. [DOI] [PubMed] [Google Scholar]
- 38.Smith DP, Weber MF, Soga K, et al. Relationship between lifestyle and health factors and severe lower urinary tract symptoms (LUTS) in 106,435 middle-aged and older Australian men: population-based study. PloS one. 2014;9(10):e109278. doi: 10.1371/journal.pone.0109278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martin S, Vincent A, Taylor AW, et al. Lower Urinary Tract Symptoms, Depression, Anxiety and Systemic Inflammatory Factors in Men: A Population-Based Cohort Study. PloS one. 2015;10(10):e0137903. doi: 10.1371/journal.pone.0137903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hannestad YS, Rortveit G, Daltveit AK, et al. Are smoking and other lifestyle factors associated with female urinary incontinence? The Norwegian EPINCONT Study. BJOG : an international journal of obstetrics and gynaecology. 2003;110(3):247. [PubMed] [Google Scholar]
- 41.Wang Y, Hu H, Xu K, et al. Prevalence, risk factors and the bother of lower urinary tract symptoms in China: a population-based survey. International urogynecology journal. 2015;26(6):911. doi: 10.1007/s00192-015-2626-8. [DOI] [PubMed] [Google Scholar]
- 42.Zhang X, Zeng X, Liu Y, et al. Impact of metabolic syndrome on benign prostatic hyperplasia in elderly Chinese men. Urologia internationalis. 2014;93(2):214. doi: 10.1159/000357760. [DOI] [PubMed] [Google Scholar]
- 43.Oh MJ, Eom CS, Lee HJ, et al. Alcohol consumption shows a J-shaped association with lower urinary tract symptoms in the general screening population. The Journal of urology. 2012;187(4):1312. doi: 10.1016/j.juro.2011.11.085. [DOI] [PubMed] [Google Scholar]
- 44.Coyne KS, Kaplan SA, Chapple CR, et al. Risk factors and comorbid conditions associated with lower urinary tract symptoms: EpiLUTS. BJU international. 2009;103(Suppl 3):24. doi: 10.1111/j.1464-410X.2009.08438.x. [DOI] [PubMed] [Google Scholar]
- 45.Richter HE, Burgio KL, Goode PS, et al. Non-surgical management of stress urinary incontinence: ambulatory treatments for leakage associated with stress (ATLAS) trial. Clinical trials (London, England) 2007;4(1):92. doi: 10.1177/1740774506075237. [DOI] [PubMed] [Google Scholar]
- 46.Subak LL, Whitcomb E, Shen H, et al. Weight loss: a novel and effective treatment for urinary incontinence. The Journal of urology. 2005;174(1):190. doi: 10.1097/01.ju.0000162056.30326.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes care. 2002;25(12):2165. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England journal of medicine. 2002;346(6):393. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.The Balanced Budget Act of 1997. Title 31, 1997.
- 50.Pivarunas B, Kelly NR, Pickworth CK, et al. Mindfulness and eating behavior in adolescent girls at risk for type 2 diabetes. The International journal of eating disorders. 2015;48(6):563. doi: 10.1002/eat.22435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vannucci A, Nelson EE, Bongiorno DM, et al. Behavioral and neurodevelopmental precursors to binge-type eating disorders: support for the role of negative valence systems. Psychological medicine. 2015;1 doi: 10.1017/S003329171500104X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Department of Health and Human Services Social Determinants of Health. Secondary Department of Health and Human Services. Social Determinants of Health 2015. http://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health.
- 53.Capturing Social and Behavioral Domains in Electronic Health Records. National Academies Press; Washington, DC: 2014. Institute of Medicine Committee on the Recommended Social and Behavioral Domains and Measures for Electronic Health Records. [PubMed] [Google Scholar]
- 54.Clark ML, Utz SW. Social determinants of type 2 diabetes and health in the United States. World journal of diabetes. 2014;5(3):296. doi: 10.4239/wjd.v5.i3.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Crews DC, Pfaff T, Powe NR. Socioeconomic factors and racial disparities in kidney disease outcomes. Seminars in nephrology. 2013;33(5):468. doi: 10.1016/j.semnephrol.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 56.Havranek EP, Mujahid MS, Barr DA, et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015;132(9):873. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 57.Averbeck MA, Madersbacher H. Constipation and LUTS - how do they affect each other? International braz j urol : official journal of the Brazilian Society of Urology. 2011;37(1):16. doi: 10.1590/s1677-55382011000100003. [DOI] [PubMed] [Google Scholar]
- 58.Loening-Baucke V. Urinary incontinence and urinary tract infection and their resolution with treatment of chronic constipation of childhood. Pediatrics. 1997;100(2 Pt 1):228. doi: 10.1542/peds.100.2.228. [DOI] [PubMed] [Google Scholar]
- 59.Shorter B, Ackerman M, Varvara M, et al. Statistical validation of the shorter-moldwin food sensitivity questionnaire for patients with interstitial cystitis/bladder pain syndrome. The Journal of urology. 2014;191(6):1793. doi: 10.1016/j.juro.2013.11.055. [DOI] [PubMed] [Google Scholar]