Abstract
Objectives
To assess racial variation in depression risk factors and symptom trajectories among older women.
Design
Nurses’ Health Study participants aged ≥60 years, free of depression in 2000, were followed until 2012.
Setting
Prospective cohort.
Participants
29,483 non-Hispanic white and 288 black women.
Measurements
Data on race and risk factors, selected a priori, were obtained from biennial questionnaires. Incident depression was defined as depression diagnosis, antidepressant use, or presence of severe depressive symptoms. Group-based trajectories of depressive symptoms were determined using latent variable modeling approaches.
Results
Black participants had lower risk (hazard ratio=0.76, 95% confidence interval[CI]=0.57-0.99) of incident late-life depression compared to whites. Although blacks had higher prevalence than whites of some risk factors at study baseline, distributions of major contributors to late-life depression risk (low exercise, sleep difficulty, physical/functional limitation, pain) were comparable. There was evidence of effect modification by race for relations of region of birth (Southern birthplace), smoking and medical comorbidity to depression risk; however, there were wide CIs among blacks, due to smaller sample size. Four trajectories were identified: minimal symptoms-stable (58.3%); mild symptoms-worsening (31.4%); sub-threshold symptoms-worsening (4.8%); sub-threshold symptoms-improving (5.5%); probabilities of trajectory types were similar for blacks and whites.
Conclusion
While overall trajectories of late-life depressive symptoms were comparable by race, there was racial variation in depression risk estimates associated with less-studied factors, such as US region of birth. Future work may address unmeasured health and resilience determinants that may underlie observed findings and that could inform clinical assessment of late-life depression risk factors.
Keywords: race, geriatric, depression, mood, trajectory, longitudinal, epidemiology
INTRODUCTION
Depression is a common and life-impairing problem in older adults(1). Even with appropriate treatment, residual symptoms and dysfunction frequently occur(2). Although racial differences in late-life depression (LLD) prevalence have been reported(3-8), the important issue of whether there are race differences in the distributions and relative contributions of risk factors to LLD is less understood. Such work is pivotal to optimizing depression prevention strategies in diverse older populations.
Prior studies that investigated racial differences in the frequencies of LLD risk factors(3, 4, 7-13) showed that non-Hispanic blacks had more chronic conditions, functional limitations, unfavorable lifestyle behaviors (e.g., cigarette smoking and physical activity), and relative economic disadvantages compared to non-Hispanic whites. However, most studies were cross-sectional; all included both depressed and non-depressed individuals, which can influence frequency estimates. Furthermore, despite lower reported risk of depression in blacks compared to whites(4, 8, 14), there have been no studies, to our knowledge, that comprehensively examined potential race/ethnic differences in the impact of risk factors on incident late-life depression.
Additionally, emerging research has emphasized the importance of temporal variations of symptoms over time to identify underlying heterogeneity of depression(15, 16). Evaluation of long-term symptom trajectories in blacks and whites may help identify subpopulations with different symptomatology and risk factors. Three studies have examined racial variations in depressive symptoms trajectory longitudinally; however, these studies adjusted for a few risk factors (such as income, marital status, functional status and health(16-18)), and behavioral risk factors for LLD were not incorporated. Furthermore, results from these studies suggested that racial variation in trajectories may have been largely confounded or mediated by frequently observed disparities in socioeconomic status (SES) between blacks and whites in the U.S.(19).
In separate work, we observed that multiple social stressors, unfavorable lifestyle behaviors, and poor health conditions were significantly associated with higher depression incidence in older women. To address the above-mentioned gaps in the literature, we now: (1) extend this work to address potential race differences in prevalence of the risk factors at baseline and their contributions to development of LLD prospectively; (2) investigate potential race differences in 12-year trajectories of late-life depressive symptoms among a socioeconomically comparable group of black and white older women, and whether there are differential relations by race of the risk factors to symptom trajectories.
METHODS
Nurses’ Health Study
The Nurses’ Health Study (NHS) began in 1976 when 121,700 U.S. female nurses, aged 30-55 years, returned a mailed questionnaire regarding lifestyle and medical history. Participants have received questionnaires biennially since then. The institutional review board of Brigham and Women's Hospital approved the study.
Measures
Risk Factors
All potential risk factors examined in this study were collected from NHS questionnaires and selected a priori from either previous NHS findings or other literature(20-24):
(1) Demographic
Age (in years); education (RN associate vs. bachelor's or higher degree); living alone; census-tract median household income; birth region.
(2) Psychosocial
Social network, measured by the Simplified Berkman-Syme Social Network Index (quintiles)(25); subjective social standing (measured using a 10-point visual analog scale representing social standing in U.S. society)(26); hours of regular caregiving to children/grandchildren and/or to ill relatives.
(3) Lifestyle/behavioral
Current smoking status; physical activity (validated in NHS(27); measured as average hours/week in moderate/vigorous exercise); heavy or binge drinking (having ≥3 drinks in a single day during a typical month in the past year).
(4) Health/medical
Body mass index (in kg/m2); medical comorbidity burden (having ≥2 major chronic diseases)(28); difficulty falling/staying asleep (frequency categories: none to all of the time); daily hours of sleep; significant physical/functional limitation (having limitations in milder activities or having more than moderate limitations in demanding activities)(28); total bodily pain (severity categories: none to very severe).
Assessment and Measures of Depression
Depression assessments include symptoms, medications and diagnosis. Symptoms were first assessed using the 5-item Mental Health Index (MHI-5) subscale of the Short-Form 36 Health Status Survey on the 1992/1996/2000 questionnaires, and continued to be assessed in 2004 (using 10-item Center for Epidemiologic Studies Depression; CESD-10) and in 2008/2012 (using 15-item Geriatric Depression Scale; GDS-15). These measures have published cut-points for screening for clinical depression (MHI-5≤52; CESD-10≥10; GDS-15≥6)(29-31). Questions on regular antidepressant use and physician/clinician-diagnosed depression were respectively assessed biennially since 1996 and 2000. Because 2000 was the earliest year in which we could classify women as ever having physician/clinician-diagnosed depression, we designated this as the study baseline.
NHS questionnaires were administered every 2 years; participants reported on depressive symptoms, antidepressant use, or physician/clinician-diagnosed depression within these time windows. Because there is no information on the number or duration of discrete depressive episodes within 2-year windows, recurrent depression events cannot be unambiguously determined during follow-up. Therefore, we only examined incident, or new-onset, depression in this study. Incident depression is defined as the first occurrence of self-reported physician/clinician-diagnosed depression, regular antidepressant use, or presence of severe depressive symptoms by published cut-points. This “Boolean OR” definition was applied, as preliminary data from separate, ongoing validation work supported optimal sensitivity and specificity using this definition. Prior NHS publications have illustrated the ability to use this depression definition to predict health outcomes or to relate individual factors to depression risk(32, 33). For medication, we included selective serotonin reuptake inhibitors but excluded tricyclic antidepressants, which could be more likely to be prescribed for other indications(34).
As a complement to our analyses examining LLD incidence, we evaluated race differences in longitudinal trajectories of late-life depressive symptoms. Because the dimensional outcome of symptoms does not depend on binary clinical cut-points or on action of clinicians to diagnose/treat depression, this approach enables us to examine directly the race differences in long-term paths of mood during late-life. Furthermore, we can examine how the risk factors influence any observed race differences in the relative proportions of trajectory group membership. In the trajectory analysis, data on depressive symptoms were used; the symptom measures were the MHI-5, CES-D and GDS-15 (see Appendix).
Sample for analysis
Participants were excluded from this study if they: did not return the baseline questionnaire or died before baseline; had a missing MHI-5 score before/at baseline; had prior history of depression before/at baseline, determined by: (1) physician/clinician-diagnosed depression, (2) antidepressant use, and/or (3) MHI-5 score ≤52; stopped returning questionnaires after baseline; reported race/ethnicity other than non-Hispanic white or black; lacked data on risk factors (see Risk Factors); had no health examination anytime during follow-up (i.e., no opportunity for depression detection by a clinician); were aged<60 years at baseline. 29,483 non-Hispanic whites and 288 blacks were in the final analysis (Supplementary Figure 1).
Statistical Methods
Risk Factor Categorization
We dichotomized risk factors, accommodating the relatively small number of black participants. Cutoff determinations were driven by the distributions of response options, their plausible expected effects, and/or their conceptual degrees of intensity or severity. We calculated the percentages of each risk factor by race.
Estimating Depression Incidence
Among incident cases, we examined race differences in the case identification methods. Individuals contributed person-time from the baseline questionnaire return date to the date of LLD incidence, death, end of follow-up (5/31/2012), or the last returned questionnaire, whichever occurred first. Cox proportional hazards models were used to estimate age- and multivariate-adjusted hazard ratios (HRs), and their 95% confidence intervals (CIs), of developing LLD. The basic model included age (in years). The multivariate-adjusted model simultaneously adjusted for age and all risk factors listed under Risk Factors; covariates were updated in time-dependent fashion where possible. Effect modification of each risk factor association by race was assessed using a multiplicative interaction term, with main effects of the risk factor and race in the multivariate-adjusted model that included all other risk factors (17 separate models to test effect modification – one for each risk factor). For each factor, the group with expected lowest risk was considered as the reference group.
To scrutinize robustness of results, we conducted a sensitivity analysis excluding cases in the first 2 years of follow-up and adding a 2-year outcome lag to address possible reverse causation (e.g., incipient depression may lead to changes in sleep or physical activity).
Trajectory Models of Depressive Symptoms
We used group-based trajectory modeling to determine distinct trajectories of depressive symptoms as a function of age at each questionnaire cycle, through a polynomial relationship estimated via a latent variable, among participants without depression history at baseline. These models were implemented using the SAS TRAJ procedure(35).
Because depressive symptoms were assessed by different instruments during follow-up, they could not be directly combined to characterize trajectory. Therefore, we applied equipercentile equating(36) to determine comparable scores based on percentile equivalents for different forms of one underlying measurement to create CESD-10-converted and GDS-15-converted MHI-5 scores for each participant (see methods in Appendix). The original (in 2000) and inferred (in 2004/2008/2012) MHI-5 scores were then used to model trajectories.
We were then able to employ latent class growth-curve analyses to estimate mean trajectories for two or more unobserved classes, in combination with membership probability in each latent class for every individual. We first assessed the most appropriate number of groups and the shape of their trajectories, from two- to ten-group models. Consistent with other work in the field(15), we determined the final number of groups based on Bayesian Information Criteria (BIC), proportion of assigned trajectory groups, model parsimony, and clinical meaningfulness and interpretation; use of this approach was also in recognition of the fact that BIC is not the sole indicator of fitness and will tend to decrease as more groups are added, even though the additional groups may not enhance interpretability. The shapes of the trajectories were set to be quadratic for all groups initially; we dropped the parameters if statistically non-significant to reduce model complexity. We then examined race differences in symptom trajectories by including the race variable in the trajectory model. Participants were assigned to the group with the highest posterior probability of group membership. Goodness-of-fit of the final model was assessed by calculating average posterior probabilities of all groups. The final model was also run separately in blacks and whites to scrutinize robustness of results.
Because covariates can change over time, we additionally performed multivariate-adjusted trajectory analyses to estimate probabilities of latent class membership, incorporating baseline and time-varying risk factors that were statistically significant in bivariate analyses. Finally, to aid in comparing our findings with those from prior studies(15, 16), we also modeled the trajectories where prevalent depression cases at baseline were included. Statistical analyses were conducted using SAS v. 9.3 (SAS Institute Inc., Cary, NC). All nominal p-values were 2-sided (p < 0.05).
RESULTS
Race Differences in Distributions of Depression Risk Factors
As shown in Table 1, blacks had significantly higher baseline prevalence of some factors previously associated with higher risk of LLD: demographic factors (living alone; lower household income), psychosocial stressors (lower social network; lower subjective social status), and health/medical factors (obesity; medical comorbidity). However, they had significantly lower baseline prevalence of other LLD risk factors (lower education, heavy/binge drinking). The largest race difference in risk factor prevalence at study baseline was for place of birth: 41.2% of blacks were born in the South; 8.0% of whites were born in the South. No significant differences by race were observed in distributions of other factors, including those with strong reported relations to LLD risk (e.g., low exercise, sleep difficulty, physical/functional limitation, and pain).
Table 1.
Baseline prevalence of depression risk factors by race/ethnicity among older women in the Nurses’ Health Study (2000) a
| White (n=29,483) | Black (n=288) | Test statistic b | p-value | |
|---|---|---|---|---|
| Age, mean (st.d) | 68.9(5.5) | 68.4(5.4) | −1.55 | 0.122 |
| Demographic factors | ||||
| RN or associate degree, % | 70.9 | 45.0 | 82.58 | <0.001 |
| Living alone, % | 21.7 | 30.2 | 13.03 | <0.001 |
| Lower census-tract median household income (<40K per year), % | 11.5 | 26.8 | 58.43 | <0.001 |
| Born in South, % | 8.0 | 41.2 | 295.27 | <0.001 |
| Psycho-social factors | ||||
| Social network index at bottom 3 quintiles, % | 49.1 | 61.0 | 15.90 | <0.001 |
| Subjective social status at bottom 5 ladders, % | 8.5 | 16.9 | 24.36 | <0.001 |
| Caregiving to children (none), % | 67.3 | 69.1 | 0.24 | 0.621 |
| Caregiving to ill relatives (some to a lot), % | 21.9 | 24.1 | 0.91 | 0.340 |
| Lifestyle/behavioral factors | ||||
| Current smoking, % | 6.8 | 6.2 | 0.22 | 0.642 |
| Lack of regular physical activity (<1 hour/week), % | 58.6 | 63.5 | 3.14 | 0.077 |
| Heavy/binge drinking (largest number ≥ 3 drinks/day), % | 11.5 | 5.4 | 10.33 | 0.002 |
| Health/medical factors | ||||
| Obesity (body mass index ≥ 30 kg/m2), % | 19.4 | 31.1 | 25.14 | <0.001 |
| Medical comorbidity (≥2 chronic conditions), % | 6.9 | 10.0 | 4.56 | 0.033 |
| Difficulty falling or staying asleep (some to all of the time), % | 31.3 | 31.8 | 0.04 | 0.835 |
| Excessive sleep (≥9 hours/day), % | 7.0 | 6.0 | 0.44 | 0.507 |
| Significant physical/functional limitation, % | 58.8 | 63.5 | 3.05 | 0.081 |
| Bodily pain (moderate or worse), % | 22.5 | 22.0 | 0.02 | 0.902 |
Percentages are standardized to the age distribution of the study population.
All test statistics were Wald χ2 with 1 degree of freedom except for age which was t-test with 29769 degrees of freedom
Race Differences in Case Detection
The crude depression incidence was lower in blacks than in whites (16.0 vs. 20.1 per 1,000 person-years). The HR (95% CI) of developing LLD among blacks, compared to whites, was 0.78 (0.59-1.03) and 0.76 (0.57-0.99) in the age- and multivariate-adjusted models, respectively. Nearly half of the depression cases were identified by severe depressive symptoms, and there was no significant global difference in case detection method (; p=0.232). Health care utilization also appeared highly similar in blacks and whites (t(29768)=−0.66; p=0.508).
Racial Variations in Relations of Risk Factors to Incident Depression
Among whites, effect estimates in multivariate-adjusted models were generally consistent, but attenuated, compared with those in age-adjusted models. Many demographic (Southern birthplace), psychosocial (lower social network; lower subjective social status; no caregiving to children/grandchildren; any caregiving to ill relatives), lifestyle (current smoking; low physical activity; and heavy/binge drinking), and health/medical (medical comorbidity; sleep difficulty; excessive sleep; physical/functional limitation; pain) risk factors were significantly associated with increased LLD risk. However, living alone and lower census-tract median household income of $40,000 USD per year had modest but statistically significant relations to lower LLD risk among whites (Table 2). Only three interactions offered significant or suggestive statistical evidence that effects differed by race: (1) while being born in the South was significantly associated with 11% higher LLD risk in whites, it was significantly related to a 54% lower LLD risk in blacks (, p-for-interaction=0.056); (2) the association between current smoking and elevated LLD risk appeared non-significantly stronger in blacks (, p-for-interaction=0.062); and (3) medical comorbidity was significantly associated with a higher LLD risk among whites, but was related to a statistically non-significant lower LLD risk among blacks (, p-for-interaction=0.024) (Table 2). Notably, the findings could be affected by estimation instability in blacks due to small number of cases and multiple testing. Results were consistent in the lagged sensitivity analysis (data not shown).
Table 2.
Age- and multivariate-adjusted race/ethnicity-stratified hazard ratios of late-life depression incidence among 29,771 older women in the Nurses’ Health Study, 2000-2012
| Age-adjusted model a | Multivariate-adjusted model a, b | |||||
|---|---|---|---|---|---|---|
| White | Black | White | Black | Interaction | ||
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | p-value c | ||
| #cases/person-years | 6,807/338,807 | 52/3,253 | 6,807/338,807 | 52/3,253 | ||
| Crude incidence rate (per 1000 person-years) | 20.1 | 16.0 | 20.1 | 16.0 | ||
| Demographic Factors | ||||||
| RN or associate degree | 1.09 (1.03-1.15) | 1.19 (0.65-2.17) | 1.01 (0.96-1.07) | 1.22 (0.62-2.40) | 0.13 | 0.718 |
| Living alone | 0.94 (0.88-0.99) | 0.59 (0.29-1.19) | 0.90 (0.84-0.96) | 0.91 (0.39-2.11) | 1.71 | 0.191 |
| Lower census-tract household income (<40K per year) | 0.97 (0.90-1.05) | 0.94 (0.50-1.78) | 0.92 (0.85-0.99) | 0.87 (0.42-1.82) | 1.25 | 0.264 |
| Born in South | 1.13 (1.03-1.22) | 0.52 (0.27-0.98) | 1.11 (1.02-1.21) | 0.46 (0.23-0.92) | 3.66 | 0.056 |
| Psycho-social Factors | ||||||
| Social network index at bottom 3 quintiles | 1.10 (1.05-1.15) | 0.62 (0.34-1.14) | 1.10 (1.05-1.16) | 0.64 (0.32-1.30) | 1.50 | 0.222 |
| Subjective social status at bottom 5 ladders | 1.31 (1.21-1.41) | 1.25 (0.57-2.74) | 1.17 (1.08-1.26) | 1.17 (0.49-2.81) | 0.0003 | 0.961 |
| No caregiving to children or grandchildren | 1.03 (0.97-1.08) | 0.87 (0.47-1.62) | 1.07 (1.02-1.13) | 0.72 (0.36-1.47) | 0.74 | 0.391 |
| Any caregiving to ill relatives | 1.22 (1.15-1.28) | 1.22 (0.63-2.35) | 1.22 (1.15-1.29) | 1.10 (0.52-2.32) | 0.04 | 0.834 |
| Lifestyle/Behavioral Factors | ||||||
| Current smoking | 1.24 (1.12-1.36) | 3.30 (1.22-8.91) | 1.17 (1.06-1.29) | 2.38 (0.80-7.08) | 3.49 | 0.062 |
| Lack of regular physical activity (<1 hour/week) | 1.40 (1.33-1.47) | 1.84 (0.94-3.59) | 1.20 (1.14-1.27) | 1.49 (0.69-3.20) | 0.40 | 0.530 |
| Heavy/binge drinking (largest number ≥ 3 drinks/day) | 1.10 (1.02-1.18) | 0.39 (0.05-3.00) | 1.12 (1.04-1.21) | 0.39 (0.05-3.26) | 0.83 | 0.362 |
| Health/Medical Factors | ||||||
| Obesity (body mass index ≥ 30 kg/m2) | 1.19 (1.12-1.26) | 1.14 (0.62-2.12) | 0.97 (0.91-1.03) | 0.92 (0.43-1.96) | 0.09 | 0.763 |
| Medical comorbidity (≥2 chronic conditions) | 1.62 (1.51-1.73) | 0.30 (0.07-1.28) | 1.40 (1.30-1.50) | 0.26 (0.06-1.19) | 5.15 | 0.024 |
| Difficulty falling or staying asleep | 1.76 (1.68-1.85) | 2.11 (1.16-3.82) | 1.62 (1.54-1.70) | 1.71 (0.90-3.28) | 0.40 | 0.528 |
| Excessive sleep (≥9 hours/day) | 1.27 (1.17-1.37) | 0.44 (0.10-1.96) | 1.25 (1.15-1.36) | 0.38 (0.08-1.88) | 0.97 | 0.324 |
| Significant physical or functional limitation | 1.75 (1.66-1.85) | 2.79 (1.32-5.87) | 1.39 (1.31-1.48) | 1.93 (0.82-4.56) | 1.82 | 0.178 |
| Bodily pain (moderate or worse) | 1.77 (1.68-1.86) | 2.38 (1.30-4.38) | 1.42 (1.35-1.50) | 1.57 (0.77-3.19) | 2.27 | 0.132 |
The hazard ratios and 95% confidence intervals are stratum-specific by race. Individual with a risk factor are compared to individuals without that risk factor, within each race/ethnic group.
Multivariate-adjusted model adjusted for all covariates listed in the table simultaneously
p for interaction was calculated using a Wald χ2 test with 1 degree of freedom from the multivariate-adjusted model
In addition to examining the effect of Southern birthplace separately in whites and blacks (i.e., two different reference groups, one in each racial group), we examined joint associations of race and Southern birthplace. Compared to a single common reference group of whites not born in the South, blacks not born in the South showed no difference in LLD risk (HR=0.91, 95% CI=0.65-1.26); however, Southern-born whites had a HR of 1.11 (95% CI=1.02-1.21) whereas Southern-born blacks had a HR of 0.56 (95% CI=0.34-0.92) in the multivariate-adjusted model.
Racial Variations in Trajectories of Late-life Depressive Symptoms
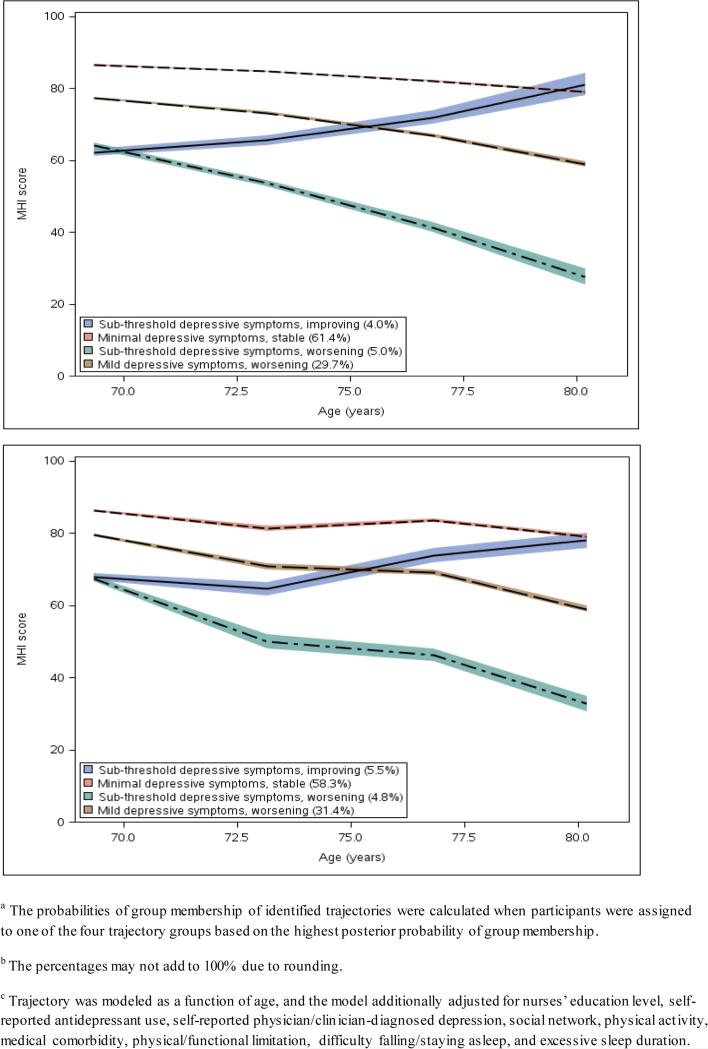
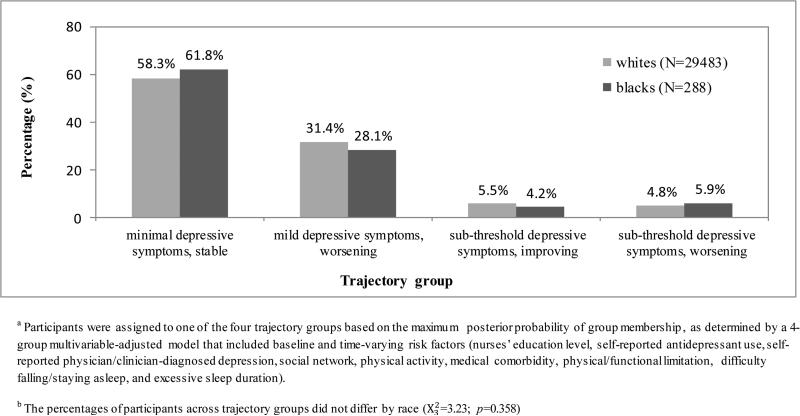
Four distinct 12-year trajectories were identified (Figure 1a): minimal symptoms-stable (61.4%); mild symptoms-worsening (29.7%); sub-threshold symptoms-worsening (5.0%); and sub-threshold symptoms-improving (4.0%) (percentages do not add to 100% due to rounding). Average posterior probabilities were good (>0.70) in all groups. We did not observe significant race differences in likelihood of belonging to any trajectory type: e.g., compared to the sub-threshold symptoms-improving group, blacks did not have statistically different probabilities of being classified in any of the three remaining trajectories compared to whites (t-test statistic=0.17-0.32 with 29769 degrees of freedom (df), p=0.747-0.863). Symptom trajectory patterns also appeared similar when modeled separately in blacks and whites, despite wide confidence bounds among blacks (Supplemental Figure 2). Observed trajectories adjusting for significant baseline and time-varying risk factors were similar to those observed without such adjustments (Figure 1b); average posterior probabilities were also >0.70 in all groups. In the multivariate-adjusted trajectory model, race was not significantly associated with probabilities of belonging to any identified trajectories (t=−0.21−0.71 with 29769 df, p=0.477−0.838). Figure 2 illustrates that the frequencies of trajectory groups – where each participant was assigned to the group of maximum posterior probability – were comparable among blacks and whites (; p=0.358).
Figure 1.
12-year mean trajectories of depressive symptoms by increasing age among older women in the Nurses’ Health Study (N=29,771)
a. Trajectory model as a function of age a,b
b. Multivariate-adjusted trajectory model as a function of age, additionally adjusting for significant baseline and time-varying risk factors a,b,c
Figure 2.
Trajectory groups by race/ethnicity among older women without history of depression at study baseline (2000) in the Nurses’ Health Study (N=29,771) a,b
In additional analyses that included those with lifetime depression history at baseline, six trajectory groups were identified (Supplemental Figure 3). Four were the same as above, with two additional groups observed: clinical range depressive symptoms-persistent and worsening (2.1%), and clinical range depressive symptoms-improving (1.8%). Thus, in this validity check, we observed the broader range of symptom patterns expected, when including prevalent cases. There were no race differences in probabilities of group membership when including baseline prevalent cases (t=−0.24−0.01 with 37284 df, p=0.809−0.991).
DISCUSSION
To our knowledge, this is the first study that longitudinally investigated racial differences in relations of a comprehensive array of risk factors to development of incident LLD, and also addressed racial variations in longitudinal late-life depressive symptoms trajectories among individuals without depression history at baseline. Consistent with prior U.S. national surveys(8, 14), we observed that blacks had lower LLD incidence compared to non-Hispanic whites in the Nurses’ Health Study. Although blacks had higher prevalence of several risk factors, the distributions of the factors with the strongest contributions to LLD risk – low exercise, sleep difficulty, physical/functional limitation and pain – were comparable in blacks and whites. Estimates for the relations of risk factors to LLD incidence were also generally similar by race. Notably, the largest discrepancy in risk factor prevalence at baseline and effect estimate was for Southern birthplace; we observed a birthplace-by-race interaction on LLD risk: being born in the U.S. South was associated with significantly lower depression risk in blacks but higher risk in whites. Finally, we identified four distinct long-term trajectory patterns of depressive symptoms among older women without depression history at baseline, but there were no significant differences by race in the type or proportion of trajectories of depressive symptoms.
While reasons for the contrast in associations of U.S. birthplace with LLD risk by race cannot be fully determined in these data, there are several speculative possibilities. NHS participants were born in 1921-1946; many were born during the Great Depression, which had greater adverse economic impact among blacks. It is possible that some Southern-born blacks living under combined hardships of segregation, discrimination and economic depression as young persons may have developed unmeasured resilience or social cohesion attributes – which in turn may be protective against depression later in life. Southern-born blacks who went on to become nurses in this study may represent a resilient group. If true, one could expect that Southern-born blacks would also have lower lifetime prevalence of depression at baseline. Indeed, in our data, blacks and whites who were not born in the South had similar lifetime depression prevalence at baseline (19-20%); by contrast, Southern-born whites had higher (23.8%) and Southern-born blacks had lower (13.9%) lifetime depression prevalence (; p<0.0001). Furthermore, blacks – especially those who were Southern-born – reported higher life optimism scores (measured on the 2004 and 2008 questionnaires by the Life Orientation Test-revised)(37) (; p=0.012). These findings support that resilience factors may contribute to the observed lower LLD risk. Birthplace also serves as a proxy for numerous unmeasured factors, such as childhood environment or sunlight/vitamin D exposure; additional investigation of this complex topic is needed. Living alone and lower census-tract median household income were significantly associated with slightly lower LLD risk among whites, but these modest observed effect estimates may be due to chance or unmeasured confounding and require future study.
Our examination of depressive symptoms trajectories specifically among those non-depressed at baseline complements the extant literature, as prior investigations included both depressed and non-depressed persons at baseline(15, 16). When prevalent cases were included, we identified six distinct trajectories. Although the number of groups is higher than that in some prior work(15, 38), it is consistent with results from a comparable study by Liang et al(16) with 17,196 adults aged 50+ years, followed for 11 years. Our finding that adjustment for risk factors did not meaningfully alter the trajectories was also consistent with Liang et al(16). However, with respect to race differences, we observed similar distributions of all trajectories by race, while Liang et al(16) observed higher likelihood of being in the increasing depressive symptoms trajectory groups among blacks compared to whites. Population composition may explain the different findings. In the Liang et al study(16), there was a higher percentage of women among blacks compared to whites; older women have nearly twice the depression incidence of older men(39). Also, blacks had lower education and yearly household income (blacks: 30.6K/whites: 54.9K) in that study; by contrast, all NHS participants are female nurses, and blacks on average had higher education than whites in the NHS. Although we observed lower household income in blacks, the disparity was not as large in the NHS (blacks: 55.7K/whites: 63.4K).
Additionally, the apparent discrepancy between observing lower overall risk of LLD among blacks, yet finding no racial differences in 12-year symptom trajectories, deserves discussion. In the depression incidence analyses, the outcome is defined by first occurrence of diagnosis, medication, and/or symptoms above clinical cut-points. Once a participant became a case, she was no longer at risk and her subsequent depressive symptoms did not contribute further information. On the other hand, the trajectory models incorporate depressive symptoms throughout follow-up, regardless of whether or when a participant becomes a case; instead, these models provide information on the long-term course of mood and may help identify heterogeneous subpopulations.
Strengths of this study include prospective data collection, large sample size, lengthy follow-up, and repeated measures of a wide array of risk factors. Potential limitations should also be addressed. First, we used self-reported indicators to define incident depression; thus, some outcome misclassification is inevitable. However, LLD incidence in our study is consistent with reports from prior studies that featured clinical evaluations to define depression(39) – suggesting that either our observed incidence is close to true incidence or that any underestimation of depression in this study is not appreciably greater than that occurring elsewhere. As we have done in prior work(22), to interrogate the outcome misclassification issue, we also applied alternate depression definitions that were more strict (i.e., depression was defined as having: 1) both physician/clinician-diagnosed depression and antidepressant use, 2) either diagnosis or antidepressant use, but not incorporating symptoms); however, findings from these models were unchanged (data not shown). Nevertheless, potential outcome misclassification remains a limitation. Second, although the number of blacks in this study (N=288) was larger than in several prior studies (N range=47-181)(5, 6, 13, 40), the relatively small sample size limited the precision of estimates, and results should be interpreted cautiously. Third, despite the comprehensive and repeated measures of a wide array of variables, information on some potentially relevant confounders is not available in the NHS (e.g., early-life adversities or personality traits); therefore, unmeasured confounding is a potential concern. Fourth, all NHS participants are well-educated; thus, participant characteristics and the study results may not be generalizable to the rest of U.S. population. It is possible that NHS black nurses were a selected group of individuals who overcame adversity to attain high education. On the other hand, this selection may also render blacks and whites in this sample more comparable in SES and access to health care; this may have provided a unique opportunity to examine risk differences due to other factors besides SES and health care knowledge/access and also reduced residual confounding due to these factors. Finally, for the trajectory models, depressive symptom scores measured by different instruments were converted to a common scale using equipercentile transformation, which assumed an equivalent percentile distribution of the score on different instruments. Therefore, some misclassification of this harmonized score is unavoidable. However, correlations between raw and inferred MHI-5 scores among a NHS subset within an ongoing validation study were strong, suggesting that recalibration errors in symptom scores were likely not substantial. In addition, depressive symptoms were assessed every 4 years in the NHS. Therefore, the extent of variation of depressive symptoms within 4-year intervals was unknown and misclassification of symptom trajectory is possible; however, on average, the between-person variability is expected to be greater than within-person variability.
In conclusion, we observed a lower depression incidence in older non-Hispanic blacks compared to non-Hispanic whites in this prospective cohort of U.S women. In general, significant evidence of racial variation was not observed in the estimates of association between a comprehensive set of risk factors and incidence of late-life depression. Late-life trajectories of depressive symptoms were also comparable by race. However, potential racial variations in depression risk associations for less-studied factors – most notably, U.S. Southern birthplace - require further investigation. For example, additional inquiry is needed to examine whether specific factor(s) related to birthplace are protective among blacks with regard to developing LLD. Future studies that include larger samples of black participants are also needed to examine potential differences by race in the relations of cigarette smoking and medical comorbidity to LLD risk. Finally, unmeasured health, resilience, and genetic determinants may underlie some of the observed findings, and improved understanding of these determinants through future work can help to inform optimal clinical assessment of depression risk factors in diverse older adults.
Supplementary Material
ACKNOWLEDGEMENT
The authors thank the participants and staff of the Nurses’ Health Study for their valuable contributions.
This study was supported by National Institutes of Health research grants UM1 CA186107, R01 MH091448 and R01 MH096776. Dr. Okereke also received funding support from the Harvard Medical School Office for Diversity Inclusion and Community Partnership Faculty Fellowship. Dr. Chang is also supported by a NARSAD Young Investigator Award from the Brain & Behavior Research Foundation. The funders of this study had no role in its design or conduct; in the collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript.
Sponsor's Role: The sponsor had no role in this manuscript.
Appendix
Equipercentile equating method
Three different instruments have been used to assess depressive symptoms within the Nurses’ Health Study, since 1992. The MHI-5 was administered in 1992, 1996 and 2000; the CESD-10 was administered in 2004; and the GDS-15 was utilized on the 2008 and 2012 questionnaires. Because the instruments were administered among NHS participants sequentially, as opposed to simultaneously, they cannot be directly linked to each other at a single time point. Furthermore, key participant factors – most notably, age – as well as the distributions of other important characteristics of relevance to depression are changing as time progresses. Thus, simplistic linking of the scales in all NHS participants is undesirable.
Thus, the first step in the linking process was to create matched sub-sets of NHS participants across the nearest adjacent questionnaires in which the three instruments were used: 2000, 2004 and 2008. Seven matching factors (age, pack-years of cigarette smoking, physical activity, alcohol consumption, self-report of receiving a diagnosis of depression from a physician/clinician, regular antidepressant use, and medical comorbidities) were used in the matching procedure to select comparable sub-cohorts between 2000 and 2004. The same approach was repeated to create comparable sub-cohorts between 2000 and 2008. Within each pair of matching sub-cohorts, equipercentile equating method estimates the nonlinear linking relationship using the percentile rank distributions of the three instruments (MHI-5, CESD-10, and GDS-15) assuming that a score could have an equivalent percentile distribution on different instruments. A conversion table was then produced to convert between the three measures.
We then examined the performance of the euqipercentile equating method in an ongoing validation study of a small subset of NHS women (N=158) who have answered MHI-5, CESD-10, and GSD-15 along with the diagnostic instrument at the same time. The Pearson correlation between CESD10-converted MHI-5 and actual MHI-5 score was 0.85, and the GSD15-converted MHI-5 and actual MHI-5 score was 0.77 in the validation sample.
Footnotes
The authors have no disclosures to report.
Conflicts of Interest: There are no conflicts of interest to report on behalf of the study authors.
REFERENCES
- 1.Katon WJ, Lin E, Russo J, et al. Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psychiatry. 2003;60:897–903. doi: 10.1001/archpsyc.60.9.897. [DOI] [PubMed] [Google Scholar]
- 2.Beekman AT, Geerlings SW, Deeg DJ, et al. The natural history of late-life depression: a 6-year prospective study in the community. Arch Gen Psychiatry. 2002;59:605–611. doi: 10.1001/archpsyc.59.7.605. [DOI] [PubMed] [Google Scholar]
- 3.Cohen CI, Magai C, Yaffee R, et al. Racial differences in syndromal and subsyndromal depression in an older urban population. Psychiatr Serv. 2005;56:1556–1563. doi: 10.1176/appi.ps.56.12.1556. [DOI] [PubMed] [Google Scholar]
- 4.Dunlop DD, Song J, Lyons JS, et al. Racial/ethnic differences in rates of depression among preretirement adults. Am J Public Health. 2003;93:1945–1952. doi: 10.2105/ajph.93.11.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Azar AR, Murrell SA, Mast BT. Race and vascular depression risk in community-dwelling older adults. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2005;13:329–332. doi: 10.1176/appi.ajgp.13.4.329. [DOI] [PubMed] [Google Scholar]
- 6.Cohen CI, Goh KH, Yaffee RA. Depression outcome among a biracial sample of depressed urban elders. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2009;17:943–952. doi: 10.1097/JGP.0b013e3181b970c7. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez HM, Croghan T, West B, et al. Antidepressant use in black and white populations in the United States. Psychiatr Serv. 2008;59:1131–1138. doi: 10.1176/appi.ps.59.10.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Breslau J, Aguilar-Gaxiola S, Kendler KS, et al. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychol Med. 2006;36:57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barry LC, Thorpe RJ, Jr., Penninx BW, et al. Race-related differences in depression onset and recovery in older persons over time: the health, aging, and body composition study. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2014;22:682–691. doi: 10.1016/j.jagp.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Husaini BA. Predictors of depression among the elderly: racial differences over time. Am J Orthopsychiatry. 1997;67:48–58. doi: 10.1037/h0080210. [DOI] [PubMed] [Google Scholar]
- 11.Pickett YR, Weissman J, Bruce ML. Racial differences in antidepressant use among older home health care patients. Psychiatr Serv. 2012;63:827–829. doi: 10.1176/appi.ps.201100233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reynolds CF, 3rd, Thomas SB, Morse JQ, et al. Early intervention to preempt major depression among older black and white adults. Psychiatr Serv. 2014;65:765–773. doi: 10.1176/appi.ps.201300216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sriwattanakomen R, McPherron J, Chatman J, et al. A comparison of the frequencies of risk factors for depression in older black and white participants in a study of indicated prevention. Int Psychogeriatr. 2010;22:1240–1247. doi: 10.1017/S1041610210001523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasin DS, Goodwin RD, Stinson FS, et al. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 15.Byers AL, Vittinghoff E, Lui LY, et al. Twenty-year depressive trajectories among older women. Arch Gen Psychiatry. 2012;69:1073–1079. doi: 10.1001/archgenpsychiatry.2012.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liang J, Xu X, Quinones AR, et al. Multiple trajectories of depressive symptoms in middle and late life: racial/ethnic variations. Psychol Aging. 2011;26:761–777. doi: 10.1037/a0023945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiao X, Liang J, Bennett JM, et al. Ethnic differences in the dynamics of depressive symptoms in middle-aged and older Americans. J Aging Health. 2010;22:631–652. doi: 10.1177/0898264310370851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spence NJ, Adkins DE, Dupre ME. Racial differences in depression trajectories among older women: socioeconomic, family, and health influences. J Health Soc Behav. 2011;52:444–459. doi: 10.1177/0022146511410432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prevention CfDCa: CDC Health Disparities and Inequalities Report — United States, 2013. MMWR Suppl 2013. 62:1–187. [PubMed] [Google Scholar]
- 20.Schoevers RA, Smit F, Deeg DJ, et al. Prevention of late-life depression in primary care: do we know where to begin? Am J Psychiatry. 2006;163:1611–1621. doi: 10.1176/ajp.2006.163.9.1611. [DOI] [PubMed] [Google Scholar]
- 21.Lyness JM, Yu Q, Tang W, et al. Risks for depression onset in primary care elderly patients: potential targets for preventive interventions. Am J Psychiatry. 2009;166:1375–1383. doi: 10.1176/appi.ajp.2009.08101489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lucas M, Mekary R, Pan A, et al. Relation between clinical depression risk and physical activity and time spent watching television in older women: a 10-year prospective follow-up study. Am J Epidemiol. 2011;174:1017–1027. doi: 10.1093/aje/kwr218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pulkki-Raback L, Kivimaki M, Ahola K, et al. Living alone and antidepressant medication use: a prospective study in a working-age population. BMC Public Health. 2012;12:236. doi: 10.1186/1471-2458-12-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lorant V, Croux C, Weich S, et al. Depression and socio-economic risk factors: 7-year longitudinal population study. Br J Psychiatry. 2007;190:293–298. doi: 10.1192/bjp.bp.105.020040. [DOI] [PubMed] [Google Scholar]
- 25.Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 26.Adler NE, Epel ES, Castellazzo G, et al. Relationship of subjective and objective social status with psychological and physiological functioning: preliminary data in healthy white women. Health Psychol. 2000;19:586–592. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- 27.Wolf AM, Hunter DJ, Colditz GA, et al. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol. 1994;23:991–999. doi: 10.1093/ije/23.5.991. [DOI] [PubMed] [Google Scholar]
- 28.Sun Q, Townsend MK, Okereke OI, et al. Alcohol consumption at midlife and successful ageing in women: a prospective cohort analysis in the nurses' health study. PLoS Med. 2011;8:e1001090. doi: 10.1371/journal.pmed.1001090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yamazaki S, Fukuhara S, Green J. Usefulness of five-item and three-item Mental Health Inventories to screen for depressive symptoms in the general population of Japan. Health and quality of life outcomes. 2005;3:48. doi: 10.1186/1477-7525-3-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Andresen EM, Malmgren JA, Carter WB, et al. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 31.Friedman B, Heisel MJ, Delavan RL. Psychometric properties of the 15-item geriatric depression scale in functionally impaired, cognitively intact, community-dwelling elderly primary care patients. J Am Geriatr Soc. 2005;53:1570–1576. doi: 10.1111/j.1532-5415.2005.53461.x. [DOI] [PubMed] [Google Scholar]
- 32.Mekary RA, Lucas M, Pan A, et al. Isotemporal substitution analysis for physical activity, television watching, and risk of depression. American journal of epidemiology. 2013;178:474–483. doi: 10.1093/aje/kws590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pan A, Sun Q, Czernichow S, et al. Bidirectional association between depression and obesity in middle-aged and older women. International journal of obesity. 2012;36:595–602. doi: 10.1038/ijo.2011.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Okereke OI, Cook NR, Albert CM, et al. Effect of long-term supplementation with folic acid and B-vitamins on risk of depression in older women. Br J Psychiatry. 2015;206:324–331. doi: 10.1192/bjp.bp.114.148361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones BL, Nagin D, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods Research. 2001;29:374–393. [Google Scholar]
- 36.Kolen MJ, Brennan RL. Test Equating Methods and Practice. Springer; New York: 2005. [Google Scholar]
- 37.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 38.Kuo SY, Lin KM, Chen CY, et al. Depression trajectories and obesity among the elderly in Taiwan. Psychol Med. 2011;41:1665–1676. doi: 10.1017/S0033291710002473. [DOI] [PubMed] [Google Scholar]
- 39.Luijendijk HJ, van den Berg JF, Dekker MJ, et al. Incidence and recurrence of late-life depression. Arch Gen Psychiatry. 2008;65:1394–1401. doi: 10.1001/archpsyc.65.12.1394. [DOI] [PubMed] [Google Scholar]
- 40.Harralson TL, White TM, Regenberg AC, et al. Similarities and differences in depression among black and white nursing home residents. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2002;10:175–184. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.