Abstract
Background: It is uncertain how changes in the U.S. Preventive Services Task Force breast cancer screening recommendations (from annual to biennial mammography screening in women aged 50–74 and grading the evidence as insufficient for screening in women aged 75 and older) have affected mammography use among Medicare beneficiaries.
Materials and Methods: Cohort study of 12 million Medicare fee-for-service women aged 65–74 and 75 and older to measure changes in 3-year screening use, 2007–2009 (before) and 2010–2012 (after), defined by two measures—proportion screened and frequency of screening by age, race/ethnicity, and hospital referral region.
Results: Fewer women were screened, but with similar frequency after 2009 for both age groups (after vs. before: age 65–74: 60.1% vs. 60.8% screened, 2.1 vs. 2.1 mammograms per screened woman; age 75 and older: 31.7% vs. 33.6% screened, 1.9 vs. 1.9 mammograms per screened woman; all p < 0.05). Black women were the only subgroup with an increase in screening use, and for both age groups (after vs. before: age 65–74: 55.4% vs. 54.0% screened and 2.0 vs. 1.9 mammograms per screened woman; age 75 and older: 28.5% vs. 27.9% screened and 1.8 vs. 1.8 mammograms per screened woman; all p < 0.05). Regional change patterns in screening were more similar between age groups (Pearson correlation r = 0.781 for proportion screened; r = 0.840 for frequency of screening) than between black versus nonblack women (Pearson correlation r = 0.221 for proportion screened; r = 0.212 for frequency of screening).
Conclusions: Changes in screening mammography use for Medicare women are not fully aligned with the 2009 recommendations.
Keywords: : change in screening, mammography, older women, USPSTF recommendations, regional variation, race/ethnicity difference
Introduction
In November 2009, the U.S. Preventive Services Task Force (USPSTF) released an update to its 2002 guidelines for breast cancer screening that altered both the recommended screening interval and ending age.1 Current guidelines recommend screening for most women every 2 years (biennially, instead of annual) starting at age 50 (or at age 40 if women and providers find this more suitable) and ending at age 74, instead of no upper age limit. For women 75 years and older, USPSTF no longer provides recommendation for or against screening because of insufficient evidence to assess the benefits and harms of screening for this group. The 2009 USPSTF recommendations generated intense debate about the questionable benefits and potential harms of screening mammography for women.1–10 Recently, the USPSTF released a draft statement concerning screening mammography, but it did not change its 2009 recommendations.11
Since the 2009 release, many studies have examined the impact of the recommendation changes on breast cancer screening. Research to date has focused on younger women (age 40–49), ethnically diverse women, cancer patients, and providers' responses to the change in guidelines; many of the previous studies were based on self-reported survey data looking retrospectively for screening information.12–20 Sharpe et al. used Medicare Physician/Supplier Procedure Summary files for 2005–2010 to show that the use of screening mammography decreased in 2010, but they did not examine any differences by age or by regions.21 The decline in the use of screening mammography found in the Sharpe study could be the result of less frequent screening for younger Medicare beneficiaries or discontinuing screening for women 75 years and older. There is no nationwide evaluation of the impact of the 2009 USPSTF recommendations on screening patterns among cancer-free women aged 65 and older, nor specifically for those 75 years and older who are left without clear guidance. In addition, it is unknown whether any change in screening patterns are affected by population demographics or geographic regions.22,23
Using 5% sample of Medicare fee-for-service claims, Jiang et al. measured the number of women undergoing screening mammography by month between 2005–2012 and found declines in screening mammography use among women aged 75 and older in 2012, but not for women aged 65–74.24 It is unknown whether all regions experienced the similar change patterns in screening use. Another study done by Jiang et al. focused on the impact of the 2009 recommendations on subsequent screenings for 2004- and 2009-screened cohorts.25 The 2009-screened cohort in Jiang's study cannot detect any potential decline in screening use among women aged 75 and older after the 2009 recommendations were issued.
Medicare started to cover screening mammography without an upper age limit in 1991, waived Part B deductible in 1998, and waived copay in 2011.26 This provides a window of opportunity to examine the impact of the 2009 USPSTF recommendations on older women. We hypothesized that after 2009, for women aged 65–74, there would be no change in the proportion of women screened, but fewer mammograms performed (a lower frequency of screening among screened women resulting from shifting from annual to biennial frequency). On the other hand, for women 75 years and older, we hypothesized that both the proportion screened and the frequency of screening among screened women would decrease (forgone screenings resulting from no recommendation for this group). We expected the change patterns to be similar across different racial/ethnic groups. In addition, we also examined change patterns by hospital referral region (HRR) to evaluate regional variation in change in screening mammography use. Because we expected there would be changes in screening patterns, we also conducted exploratory regression analyses to examine the association between regional change patterns and regional characteristics that are known to be related to health and healthcare systems.27
Materials and Methods
Data sources
We used 2007–2012 100% Medicare fee-for-service claims data for our study. We obtained HRR level characteristics (total adjusted reimbursement, percent rural, poverty rate, composite quality score of Medicare effective care use) from the Dartmouth Atlas of Healthcare for the exploratory analysis.27
Study design
From Medicare data, we created two cohorts, 2007 (before) and 2010 (after), of women aged 65 and older and their subsequent 3-year screening use (before: 2007–2009; after: 2010–2012).
Cohort populations
From the 2007 to 2010 Medicare denominator files, we first identified women who were aged 65 and older on January 1. We then limited our cohort beneficiaries to those who resided in the U.S., were not enrolled in Medicare Advantage, and had full coverage in Medicare Parts A (inpatient care) and B (physician and outpatient services) during the study period. Each woman was assigned to a HRR based on her resident ZIP Code in 2007 or 2010.
Outcome measures
We examined two measures of screening mammography use: (1) the proportion of women with at least 1 screening mammogram (proportion screened) and (2) the number of screening mammograms per screened woman (frequency of screening).
Since Medicare covers annual mammography (at least 11 months after the last covered screening mammography)28 and the 2009 USPSTF recommends biennial mammography, we measured screening use in a 3-year period for each cohort (2007–2009 for the 2007 cohort, 2010–2012 for the 2010 cohort) to allow enough time to capture any changes in screening patterns.
We identified any claims indicating screening mammography (diagnosis V76.11, V76.12 and CPT 77052, 77057, G0202)29 among the study population from physician claims in the Physician/Supplier Part B files for 3 years. We counted 1 screening claim per day without any restriction on the interval between screenings.
The focus of our study was early detection among cancer-free women during the study period. Women with any code indicating mastectomy or breast cancer diagnosis during the 3-year measurement period were excluded (CPT 19160, 19162, 19180, 19182, 19200, 19220, 19240, 19242, 19301-19307 or ICD-9 174.xx, 233.0, 611.72 or 85.33-85.36, 85.4, 85.41-85.48 or DRG 257-260 or MS-DRG 582-585 from inpatient or physician claims).30,31
Independent variables
To evaluate alignment with the 2009 recommendations, we categorized each cohort of women into two age groups—65–74 and 75 years and older. Because screening rates vary by race and ethnicity,32 we also categorized women into four racial/ethnic groups: white, black, Hispanic, or other. To test whether changes in screening use were evenly across various regions, we examined differences in screening use between two cohorts by HRRs.
Statistical analysis
We calculated the proportion of women who were screened and the number of mammograms per screened woman over 3 years for each cohort. We then examined screening use by patient characteristics and by region for each cohort. We calculated age–race adjusted HRR-level proportion screened and frequency of screening for each cohort using indirect adjustment methods.22 Finally, we examined the differences in 3-year use of screening mammography between the two cohorts at both the individual and HRR levels. We tested differences in changes in 3-year use at the patient level by t-test or chi-square tests as appropriate. We used Pearson correlation coefficients to examine change patterns between age and racial/ethnic groups at the HRR level. We examined geographic variation in the change patterns by dividing the HRRs into equal-population quintiles based on the 2007 overall proportion of women screened to identify the regions in which the greatest changes occurred.
We also conducted exploratory regression analysis to determine the association between regional characteristics and regional change in mammography use. In this multivariable linear regression analysis, the outcomes of interests were HRR-level percent change of adjusted proportion screened and percent change of adjusted frequency of screening for each age group and for each race/ethnicity group within age groups. The HRR-level explanatory variables included price-adjusted per-beneficiary Medicare spending (a measure of healthcare use intensity), the percent of HRR residents living in a rural area (a measure of accessibility of healthcare), the percent of residents below 150% of the federal poverty limit (a measure of socioeconomic status), and a composite quality score of Medicare effective care use (a composite score of the standardized rates of the following measures: beneficiaries filling at least one prescription for beta-blockers within 6 months of a heart attack; the percent of diabetics who received appropriate hemoglobin monitoring; and the percent of diabetics who received appropriate eye exams).27 The sign and statistically significant level of coefficients of explanatory variables from each model would indicate how the regional characteristics associate with age- and age-race/ethnicity-specific changes in screening mammography use.
All analyses were conducted using SAS V9.2 (SAS Institute, Inc., Cary, NC). The Dartmouth College institutional review board approved this study.
Results
Patient level
There were over 12 million women aged 65 and older enrolled in the Medicare fee-for-service program in each cohort (Table 1). In both cohorts, the majority women were 75 years and older (mean age 76.8 in 2007 and 76.7 in 2010).
Table 1.
Screening Mammography Use Among Medicare Female Beneficiaries Before and After 2009
| % Screened | Frequency of usea | % Screened | Frequency of usea | % Screened | Frequency of usea | |
|---|---|---|---|---|---|---|
| Age 65–74 | Screening use 2007–2009 | Screening use 2010–2012 | Test of difference | |||
| No. of women | 5,400,259 | 5,674,176 | ||||
| Total | 60.8 | 2.1 | 60.1 | 2.1 | <0.001 | 0.002 |
| Race | ||||||
| White | 62.6 | 2.1 | 61.8 | 2.1 | <0.001 | <0.001 |
| Black | 54.0 | 1.9 | 55.4 | 2.0 | <0.001 | <0.001 |
| Hispanic | 50.6 | 1.8 | 50.5 | 1.8 | 0.191 | 0.017 |
| Other | 50.0 | 1.9 | 49.6 | 1.9 | 0.021 | 0.008 |
| Mortalityb | Screened | Not screened | Screened | Not screened | ||
| 2.1 | 12.9 | 2.0 | 12.0 | |||
| Age ≥75 | Screening use 2007–2009 | Screening use 2010–2012 | Test of difference | |||
| No. of women | 6,891,206 | 6,732,053 | ||||
| Total | 33.6 | 1.9 | 31.7 | 1.9 | <0.001 | <0.001 |
| Race | ||||||
| White | 34.6 | 1.9 | 32.5 | 1.9 | <0.001 | 0.084 |
| Black | 27.9 | 1.8 | 28.5 | 1.8 | <0.001 | <0.001 |
| Hispanic | 26.8 | 1.7 | 25.4 | 1.7 | <0.001 | <0.001 |
| Other | 26.9 | 1.8 | 24.3 | 1.8 | <0.001 | 0.627 |
| Mortalityb | Screened | Not screened | Screened | Not screened | ||
| 5.9 | 33.0 | 5.7 | 32.4 | |||
Per screened woman.
Three-year mortality.
Compared with screening use before 2009, slightly fewer women had a screening mammogram over 3 years for both age groups after 2009 (after vs. before: age 65–74: 60.1% vs. 60.8%; age 75 and older: 31.7% vs. 33.6%, all p < 0.05), but their frequency of screening did not change meaningfully even though it was statistically significant due to large sample size (age 65–74: 2.1 vs. 2.1 mammograms per screened woman; age 75 and older: 1.9 vs. 1.9 mammograms per screened woman, all p < 0.05).
Declines in screening use were also observed for each racial/ethnic group with the exception of black women. Although 3-year use of screening among black women was higher compared with Hispanic or other race women before the 2009 recommendations, there was an increase in the use of screening mammography for black women for both age groups after 2009 (after vs. before: age 65–74: proportion screened 55.4% vs. 54.0%; frequency of screening: 2.0 vs. 1.9 mammograms per screened woman; age 75 and older: proportion screened: 28.5% vs. 27.9%; frequency of screening: 1.8 vs. 1.8 mammograms per screened woman, all p < 0.05).
HRR level
Although most regions had fewer women screened after 2009 in both age groups, not all regions had an equivalent decline in proportion screened (age 65–74: median percentage change −1.5%, interquartile range −3.3% to −0.1%; age 75 and older: median percentage change −5.8%, interquartile range −8.2% to −4.1%). The top three regions with the biggest decline in proportion screened were the same for both age groups (after vs. before: Sioux City IA 42.4% vs. 53.0% for age 65–74, 23.4% vs. 31.6% for age 75 and older; Lebanon NH 58.0% vs. 66.7% for age 65–74, 32.1% vs. 39.9% for age 75 and older; Yakima WA 57.1% vs. 65.6% for age 65–74, 33.4% vs. 40.5% for age 75 and older). Interestingly, there were 76 regions out of 306 HRRs where more, not fewer, women aged 65–74 received screening mammograms after 2009 (the top three regions, after vs. before: Spartanburg SC 64.5% vs. 56.3%; Aurora IL 62.4% vs. 54.8%; Marquette MI 64.0% vs. 59.5%). Similarly, there were 11 regions where more women 75 years and older received screening mammograms after 2009 (the top three regions, after vs. before: Aurora IL 32.0% vs. 28.4%; Spartanburg SC 35.2% vs. 31.9%; Honolulu HI 49.9% vs. 47.2%). Much smaller change patterns were observed in frequency of screening (age 65–74: median percentage change −0.05%, interquartile range −1.4% to 1.0%; age 75 and older: median percentage change 0.2%, interquartile range −1.2% to 1.6%). Regional patterns of changes in screening between age groups were highly correlated (Pearson correlation r = 0.781 for change in proportion screened and r = 0.840 for change in frequency of screening, both p < 0.0001).
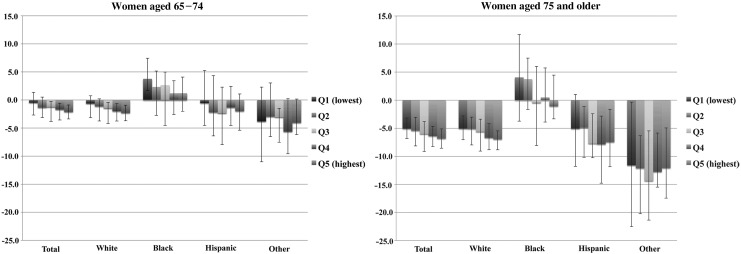
Because the overall magnitude of change is small, yet we observed some regions with relatively large increases in use, we further examined the patterns of regional change. We divided 306 HRRs into population-weighted quintiles of proportion screened before 2009 (Table 2). The greatest declines in proportion screened were in the regions with the highest proportion screened before 2009 for both age groups. Interestingly, the pattern of change among black women was the opposite of other racial/ethnic women (Fig. 1). For age 65–74, after 2009, fewer women of all other racial/ethnic groups were screened in all quintiles, with the highest quintile decreasing the most. In contrast, more black women were screened after 2009 in all quintiles, with the highest quintile increasing the least. For women 75 years and older, in the lowest two quintiles, more black women were actually screened. There was only a small decrease in proportion screened for black women in HRRs in the highest quintile compared to other racial/ethnic groups. The correlations of change in screening use between blacks and non-blacks were weak (Pearson correlation coefficient for change in proportion screened: r = 0.221, p = 0.0001; for change in frequency of screening: r = 0.212, p = 0.0002).
Table 2.
Proportion Screened (Median) Before and After 2009 at HRRs
| Quintilesaof % screened 2007–2009 | No. of HRRs | Overall % screened 2007–2009 | % Screened 2007–2009 | % Screened 2010–2012 | % Change |
|---|---|---|---|---|---|
| Age 65–74 | |||||
| Q1 (Lowest) | 61 | 43.6 | 56.3 | 56.0 | −0.5 |
| Q2 | 53 | 46.8 | 59.9 | 58.5 | −1.3 |
| Q3 | 54 | 49.2 | 62.6 | 61.6 | −1.2 |
| Q4 | 70 | 52.2 | 65.4 | 64.3 | −1.7 |
| Q5 (Highest) | 68 | 56.5 | 70.0 | 68.6 | −2.1 |
| Age ≥75 | |||||
| Q1 (Lowest) | 61 | 43.6 | 32.5 | 30.7 | −5.1 |
| Q2 | 53 | 46.8 | 35.5 | 33.5 | −5.4 |
| Q3 | 54 | 49.2 | 37.7 | 35.6 | −6.0 |
| Q4 | 70 | 52.2 | 40.7 | 38.2 | −6.4 |
| Q5 (Highest) | 68 | 56.5 | 44.5 | 41.5 | −6.8 |
Adjusted for population size so that each quintile has 20% of study women.
HRR, hospital referral region.
FIG. 1.
Median percentage change in proportion screened at HRRs before and after 2009 by quintiles of proportion screened before 2009. Colors for quintiles, lines for 25th and 75th percentile among HRRs within each quintile. Women aged 65–74, Women aged 75 and older.
Regional changes in screening use, even though the magnitudes were small, were associated with healthcare and health system characteristics (Tables 3 and 4 show coefficients from multivariate liner regression analyses; the sign of coefficient indicated the direction of association and statistical significance level indicated the strength of the association). For women aged 65–74, for whom biennial mammography screening is recommended, changes in screening were positively associated with the total price-adjusted per capita Medicare spending, but only for white and Hispanic women (Coefficient [95% CI]: white: proportion screened 0.56 [0.29–0.83] and frequency of screening 0.33 [0.13–0.54]; Hispanic: proportion screened 1.25 [0.83–1.67] and frequency of screening 0.65 [0.37–0.93], all p < 0.05). Moreover, only changes in proportion screened among white women were positively associated with a composite quality score (Coefficient [95% CI]: proportion screened 0.71 [0.21–1.21], p < 0.05). For women 75 years and older, changes in proportion screened were positively associated with Medicare spending for all race/ethnicity groups except for black women (Coefficient [95% CI]: white: 1.05 [0.68–1.41]; Hispanic: 1.35 [0.76–1.94]; other: 1.86 [0.92–2.80], all p < 0.05; vs. black: 0.17 [−0.68–1.01], p > 0.05). The changes in screening use among women 75 years and older were not associated with the composite quality score.
Table 3.
Association Between Regional Characteristics and Change in Proportion Screened
| Coefficient (95% CI) | ||
|---|---|---|
| Characteristics | Age 65–74 | Age ≥75 |
| All | ||
| Adjusted reimbursements | 0.62 (0.36, 0.88)a | 1.00 (0.66, 1.33)a |
| Percent rural | −0.03 (−0.05, −0.01)b | −0.02 (−0.04, 0.01) |
| Poverty rate | 0.05 (−0.02, 0.11) | 0.004 (−0.08, 0.09) |
| Quality score | 0.74 (0.25, 1.22)b | 0.46 (−0.16, 1.07) |
| White | ||
| Adjusted reimbursements | 0.56 (0.29, 0.83)a | 1.05 (0.68, 1.41)a |
| Percent rural | −0.02 (−0.05, 0.002)c | 0.02 (0.004, 0.05) |
| Poverty rate | 0.02 (−0.05, 0.09) | 0.03 (−0.07, 0.12) |
| Quality score | 0.71 (0.21, 1.21)b | 0.29 (−0.38, 0.95) |
| Black | ||
| Adjusted reimbursements | 0.54 (−0.03, 1.10) | 0.17 (−0.68, 1.01) |
| Percent rural | −0.06 (−0.10, −0.03)a | −0.02 (−0.08, 0.03) |
| Poverty rate | 0.17 (0.06, 0.28)b | 0.16 (−0.01, 0.33) |
| Quality score | 0.58 (−0.45, 1.60) | −0.13 (−1.67, 1.40) |
| Hispanic | ||
| Adjusted reimbursements | 1.25 (0.83, 1.67)a | 1.35 (0.76, 1.94)a |
| Percent rural | 0.02 (−0.04, 0.07) | 0.05 (−0.03, 0.14) |
| Poverty rate | 0.08 (−0.01, 0.17) | 0.14 (0.01, 0.26)c |
| Quality score | 0.71 (−0.30, 1.72) | 1.02 (−0.51, 2.54) |
| Other | ||
| Adjusted reimbursements | 0.32 (−0.39, 1.04) | 1.86 (0.92, 2.80)a |
| Percent rural | −0.18 (−0.25, −0.11)a | −0.19 (−0.29, −0.09)a |
| Poverty rate | 0.21 (0.02, 0.40)c | −0.06 (−0.31, 0.20) |
| Quality score | −0.03 (−1.45, 1.40) | 0.53 (−1.40, 2.45) |
Characteristics source:
Choosing Wisely: Prevalence and Correlates of Low-Value Healthcare Services in the United States Cola, et al. JIM 2014.
p < 0.001.
p < 0.01.
p < 0.05.
Table 4.
Association Between Regional Characteristics and Change in Frequency of Screening
| Coefficient (95% CI) | ||
|---|---|---|
| Characteristics | Age 65–74 | Age ≥75 |
| All | ||
| Adjusted reimbursements | 0.30 (0.11, 0.49)b | 0.12 (−0.10, 0.33) |
| Percent rural | −0.01 (−0.02, 0.01) | 0.003 (−0.01, 0.02) |
| Poverty rate | 0.02 (−0.03, 0.06) | 0.0002 (−0.05, 0.05) |
| Quality score | 0.18 (−0.19, 0.54) | −0.30 (−0.70, 0.10) |
| White | ||
| Adjusted reimbursements | 0.33 (0.13, 0.54)b | 0.15 (−0.08, 0.37) |
| Percent rural | 0.0003 (−0.02, 0.02) | 0.01 (−0.01, 0.02) |
| Poverty rate | −0.01 (−0.06, 0.05) | 0.001 (−0.06, 0.06) |
| Quality score | 0.19 (−0.19, 0.56) | −0.25 (−0.66, 0.17) |
| Black | ||
| Adjusted reimbursements | −0.04 (−0.37, 0.30) | −0.30 (−0.75, 0.16) |
| Percent rural | −0.05 (−0.07, −0.03)a | −0.03 (−0.06, 0.003)c |
| Poverty rate | 0.16 (0.09, 0.23)a | 0.12 (0.04, 0.21)b |
| Quality score | 0.25 (−0.36, 0.86) | −0.53 (−1.35, 0.30) |
| Hispanic | ||
| Adjusted reimbursements | 0.65 (0.37, 0.93)a | 0.30 (−0.07, 0.68) |
| Percent rural | 0.002 (−0.04, 0.04) | 0.06 (0.01, 0.12)c |
| Poverty rate | 0.01 (−0.05, 0.07) | −0.02 (−0.10, 0.06) |
| Quality score | −0.76 (−1.43, −0.09)c | −1.09 (−2.06, −0.13)c |
| Other | ||
| Adjusted reimbursements | −0.12 (−0.46, 0.22) | −0.06 (−0.53, 0.41) |
| Percent rural | −0.01 (−0.04, 0.03) | 0.001 (−0.05, 0.05) |
| Poverty rate | 0.06 (−0.03, 0.15) | −0.01 (−0.14, 0.11) |
| Quality score | 0.37 (−0.31, 1.06) | 0.60 (−0.36, 1.56) |
Characteristics source:
Choosing Wisely: Prevalence and Correlates of Low-Value Healthcare Services in the United States Cola, et al. JIM 2014.
p < 0.001.
p < 0.01.
p < 0.05.
Discussion
Using Medicare claims, we examined the 3-year use of screening mammography among Medicare women aged 65 and older before and after the 2009 USPSTF recommendations were published. Except for women of black race, we found a slight decrease in the number of women screened for breast cancer during a 3-year look-forward period for both under and over age 75 after 2009. There was, however, little change in the frequency of screening after 2009.
Our findings of a decrease in screening use among Medicare women were consistent with that of the previous Medicare study by Sharpe study.21 However, studies based on self-reported screening in the past year did not find a significant decline in mammography rates.14,17 Our 3-year observation period provides sufficient time to capture screenings from any interval changes (from annual to biennial) or a delay in schedule to obtain one within 2 years.
One possible explanation for our finding could be the result of conflicting recommendations from clinicians.12,13,18,20 Another possible explanation could be that the frequency changes to every other year from every year, which could make it harder for older women to remember the last screening date. On the other hand, the fact that more than 2 million women aged 65–74 (40%) did not have a screening mammogram claim in 3 years is a potential concern. Because these women had higher mortality in 3 years (Table 1), they might have other health problems and competing risks that prevent them from receiving screening or rendered the screening irrelevant. However, much of this cohort was still alive at the end of the follow-up period, indicating potential underuse of this service. Previous research has identified several factors related to not getting screened such as not recommended, wasn't needed, or having no primary care provider based on data before 2009.26,33,34 Beginning January 1, 2011, there is no cost to Medicare beneficiaries for annual screening mammograms because the Affordable Care Act enhanced benefits for clinical preventive service under Medicare and eliminated patient cost-sharing for recommended preventive services.35 Our results indicated that payment incentive to beneficiaries has a limited impact on screening mammography. Further research is needed to understand why this group of women did not have a screening.
On the other hand, we did not find a large decline in the use of screening among women 75 years and older. It is conceivable that this group of women would believe that there is a benefit from frequent screening mammograms if they have done so for many years.2,4,36 They may continue to be screened even when there is no evidence to support that belief; especially since Medicare continues to cover screening mammography as a preventive care service.
Schonberg et al. evaluated the effect of a decision aid on screening mammography among women 75 years and older.37 Exposure to the decision aid did not impact screening intentions among women with a longer (>9 years) life expectancy. Half of women with a shorter life expectancy still intended to get a mammogram. After participating in the study, 60% of all women were still screened within 15 months. Because there is no consensus about how long women should continue to be screened for breast cancer, while the decision aids may improve women's knowledge of the evidence regarding screening, they may not lead to a change in the habit of being screened. The notion of preventive care does not comprise the consequences of emotional harm due to false-positive results,3,8 increasing the risk of overdiagnosis and needless treatment.4–6,38 This can be a concern, especially for women with less than a 10-year life expectancy.4
Recently the American Cancer Society (ACS) released its breast cancer screening guideline for women at average risk for breast cancer.39 This is the first time, since 2003, ACS recommends that women aged 55 years and older should transition to biennial screening, a recommendation that is much aligned with the USPSTF biennial frequency guideline for women 50 years and older. However, ACS does not provide an upper age limit for screening, rather, it leaves to older women and their physicians to decide if their overall health is good and if they have a life expectancy of 10 years or longer. With this change in frequency of screening from ASC, there would be a measurable decline in coming years. Further research is needed to examine how this new change in guideline from ACS impacts screening mammography.
Another unexpected finding was the change in screening use among black women. Because black women have higher breast cancer death rates and more advanced stage at breast tumor diagnoses compared to other racial/ethnic groups, many have advocated for increasing screening among black women.16,32,40 Our findings of increased screening among black women aged 65–74 were encouraging. However, an unintended consequence could be that more black women 75 years and older also were screened without clear guidance from the USPSTF. This indicates that more research is needed to better address the use of screening resources.41,42
The observed geographic variation in screening mammography at the HRR level likely reflects variation in both clinician practice and patient choice. Because women can receive a screening mammogram without a physician's referral, the decision to undergo a screening mammogram or not, and how frequently to be screened, may not always reflect a fully informed choice.
Since screened women had much lower mortality, it suggests that screenings were performed among relatively healthy women. Yet, without a benchmark, it is difficult to know how the practice may be over-, under-, or misused. It appears, however, that the changes in screening mammography use among older women were not fully aligned with the USPSTF recommendations.
Limitations
We used Medicare fee-for-service claims to examine a 3-year use of screening mammography before and after 2009. We do not know if any shifts in use patterns we observed were directly attributed to the USPSTF guideline changes. We did not have any information about the test results or how the decision to screen or not was made. Although we excluded women with mastectomy or breast cancer diagnosis during the study years, we did not have information before study period or before their enrollment in Medicare. Our sensitivity analysis, including women with mastectomy or breast cancer diagnosis, did not alter the results. We were also unable to ascertain whether women resided in nursing homes or had diseases that would prevent them from receiving screening. We also did not know how many were called back for a second screening mammogram because of concerns resulting from the first one. We examined the geographic variation in screening mammography for older women in fee-for-service Medicare; the variation observed in this study may not be applicable to younger women or Medicare Advantage enrollees.
Conclusions
We examined the changes in screening mammography use among women aged 65 and older following the 2009 USPSTF recommendations. We found that older women were slightly less likely to have a screening mammogram after 2009, except for black women. Among women who received screening mammography, there was negligible change in their frequency of screening. Our findings indicate that attention is warranted from policy makers, clinicians (both primary care providers and radiologists), and Medicare, with the goal of working together for policy changes that will result in evidence-based breast cancer screening among older women.
Acknowledgments
The authors would like to thank Kristen Bronner for assistance with article preparation. Funders: This work was supported, in part, by grants from the National Cancer Institute (P01 CA154292, U54 CA163307, P30 CA023108), the National Institute on Aging (P01 AG019783), The Dartmouth Clinical and Translational Science Institute, and under award number UL1TR001086 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author Disclosure Statement
The authors declare no competing financial interests.
References
- 1.U. S. Preventive Services Task Force. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2009;151:716–726, W-236 [DOI] [PubMed] [Google Scholar]
- 2.Biller-Andorno N, Juni P. Abolishing mammography screening programs? A view from the Swiss medical board. N Engl J Med 2014;370:1965–1967 [DOI] [PubMed] [Google Scholar]
- 3.Tosteson AN, Fryback DG, Hammond CS, et al. Consequences of false-positive screening mammograms. JAMA Intern Med 2014;174:954–961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walter LC, Schonberg MA. Screening mammography in older women: A review. JAMA 2014;311:1336–1347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Welch HG, Passow HJ. Quantifying the benefits and harms of screening mammography. JAMA Inter Med 2014;174:448–454 [DOI] [PubMed] [Google Scholar]
- 6.Miller AB, Wall C, Baines CJ, Sun P, To T, Narod SA. Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: Randomised screening trial. BMJ 2014;348:g366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marmot MG. Sorting through the arguments on breast screening. JAMA 2013;309:2553–2554 [DOI] [PubMed] [Google Scholar]
- 8.Kachalia A, Mello MM. Breast cancer screening: Conflicting guidelines and medicolegal risk. JAMA 2013;309:2555–2556 [DOI] [PubMed] [Google Scholar]
- 9.Smith RA, Kerlikowske K, Miglioretti DL, Kalager M. Clinical decisions. Mammography screening for breast cancer. N Engl J Med 2012;367:e31. [DOI] [PubMed] [Google Scholar]
- 10.Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med 2012;367:1998–2005 [DOI] [PubMed] [Google Scholar]
- 11.U.S. Preventive Services Task Force. Draft recommendation statement breast cancer screening. April 2015; Available at: www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementDraft/breast-cancer-screening1 Accessed April22, 2015
- 12.Wang AT, Fan J, Van Houten HK, et al. Impact of the 2009 US Preventive Services Task Force guidelines on screening mammography rates on women in their 40s. PLoS One 2014;9:e91399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Allen JD, Bluethmann SM, Sheets M, et al. Women's responses to changes in U.S. Preventive Task Force's mammography screening guidelines: Results of focus groups with ethnically diverse women. BMC Public Health 2013;13:1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pace LE, He Y, Keating NL. Trends in mammography screening rates after publication of the 2009 US Preventive Services Task Force recommendations. Cancer 2013;119:2518–2523 [DOI] [PubMed] [Google Scholar]
- 15.Friedman EB, Chun J, Schnabel F, et al. Screening prior to breast cancer diagnosis: The more things change, the more they stay the same. Int J Breast Cancer 2013;2013:327567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin N, Wingfield J. USPSTF screening recommendations for breast cancer: The potential impact on the African American community. J Health Care Poor Underserved 2012;23(2 Suppl):91–97 [DOI] [PubMed] [Google Scholar]
- 17.Howard DH, Adams EK. Mammography rates after the 2009 US Preventive Services Task Force breast cancer screening recommendation. Prev Med 2012;55:485–487 [DOI] [PubMed] [Google Scholar]
- 18.Anderson BL, Pearlman M, Griffin J, Schulkin J. Conflicting and changing breast cancer screening recommendations: Survey study of a national sample of ob-gyns after the release of the 2009 USPSTF guidelines. J Healthc Qual 2013;35:25–35 [DOI] [PubMed] [Google Scholar]
- 19.Aragon R, Morgan J, Wong JH, Lum S. Potential impact of USPSTF recommendations on early diagnosis of breast cancer. Ann Surg Oncol 2011;18:3137–3142 [DOI] [PubMed] [Google Scholar]
- 20.Bryant H, Mai V. Impact of age-specific recommendation changes on organized breast screening programs. Prev Med 2011;53:141–143 [DOI] [PubMed] [Google Scholar]
- 21.Sharpe RE, Jr., Levin DC, Parker L, Rao VM. The effect of the controversial US Preventive Services Task Force recommendations on the use of screening mammography. J Am Coll Radiol 2013;10:21–24 [DOI] [PubMed] [Google Scholar]
- 22.Wennberg JE, Cooper MM. The quality of medical care in the United States: A report on the medicare program. The Dartmouth Atlas of Health Care. Chicago, Ill: American Hospital Publishing, 1996 [PubMed] [Google Scholar]
- 23.Elmore JG, Etzioni R. Effect of screening mammography on cancer incidence and mortality. JAMA Inter Med. 2015;175:1490–149 [DOI] [PubMed] [Google Scholar]
- 24.Jiang M, Hughes DR, Duszak R., Jr. Screening mammography rates in the medicare population before and after the 2009 U.S. Preventive Services Task Force guideline change: An interrupted time series analysis. Womens Health Issues 2015;25:239–245 [DOI] [PubMed] [Google Scholar]
- 25.Jiang M, Hughes DR, Appleton CM, McGinty G, Duszak R., Jr. Recent trends in adherence to continuous screening for breast cancer among Medicare beneficiaries. Prev Med 2015;73:47–52 [DOI] [PubMed] [Google Scholar]
- 26.Salloum RG, Kohler RE, Jensen GA, Sheridan SL, Carpenter WR, Biddle AK. U.S. Preventive Services Task Force recommendations and cancer screening among female medicare beneficiaries. J Womens Health. 2014;23:211–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Colla CH, Morden NE, Sequist TD, Schpero WL, Rosenthal MB. Choosing wisely: Prevalence and correlates of low-value health care services in the United States. J Gen Intern Med 2015;30:221–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centers of Medicare & Medicaid Services. Your medicare coverage. Available at: www.medicare.gov/coverage/mammograms.html Accessed July23, 2015
- 29.Centers for Medicare & Medicaid Services. Quick reference information: Preventive services: Medicare Learning Network. ICN 006559
- 30.Tan A, Kuo YF, Goodwin JS. Potential overuse of screening mammography and its association with access to primary care. Med Care 2014;52:490–495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nattinger AB, Laud PW, Bajorunaite R, Sparapani RA, Freeman JL. An algorithm for the use of medicare claims data to identify women with incident breast cancer. Health Serv Res 2004;39(6 Pt 1):1733–1749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Center for Disease Control and Prevention. Breast cancer statistics. 2014; Available at: www.cdc.gov/cancer/breast/statistics/ Accessed May14, 2015
- 33.Meissner HI, Breen N, Taubman ML, Vernon SW, Graubard BI. Which women aren't getting mammograms and why? (United States). Cancer Causes Control 2007;18:61–70 [DOI] [PubMed] [Google Scholar]
- 34.Schueler KM, Chu PW, Smith-Bindman R. Factors associated with mammography utilization: A systematic quantitative review of the literature. J Womens Health 2008;17:1477–1498 [DOI] [PubMed] [Google Scholar]
- 35.Jensen GA, Salloum RG, Hu J, Ferdows NB, Tarraf W. A slow start: Use of preventive services among seniors following the affordable care act's enhancement of medicare benefits in the U.S. Prev Med 2015;76:37–42 [DOI] [PubMed] [Google Scholar]
- 36.Torke AM, Schwartz PH, Holtz LR, Montz K, Sachs GA. Older adults and forgoing cancer screening: “I think it would be strange”. JAMA Intern Med 2013;173:526–531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schonberg MA, Hamel MB, Davis RB, et al. Development and evaluation of a decision aid on mammography screening for women 75 years and older. JAMA Intern Med 2014;174:417–424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pace LE, Keating NL. A systematic assessment of benefits and risks to guide breast cancer screening decisions. JAMA 2014;311:1327–1335 [DOI] [PubMed] [Google Scholar]
- 39.Oeffinger KC, Fontham ETH, Etzioni R, et al. Breast cancer screening for women at average risk: 2015 guideline update from the American Cencer Society. JAMA 2015;314:1599–1614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.American Cancer Society. Breast Cancer Facts & Figures. 2013; Available at: www.cancer.org/research/cancerfactsstatistics/breast-cancer-facts-figures Accessed May15, 2015
- 41.O'Donoghue C, Eklund M, Ozanne EM, Esserman LJ. Aggregate cost of mammography screening in the United States: Comparison of current practice and advocated guidelines. Ann Intern Med 2014;160:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Elmore JG, Gross CP. The cost of breast cancer screening in the United States: A picture is worth … a billion dollars? Ann Intern Med 2014;160:203. [DOI] [PubMed] [Google Scholar]