Abstract
Background
Timely initiation of breastfeeding within one hour after birth and exclusive breastfeeding is recommended for the first six months of infant life along with continuation of breastfeeding up to two years. Timely initiation of breastfeeding has the potential to prevent 22 % of neonatal deaths. The objective of this study was to assess timely initiation of breastfeeding and associated factors among mothers who have infants less than six months of age in Motta town, East Gojjam, Amhara Regional State, Ethiopia.
Method
Community based quantitative cross-sectional study was conducted from April 7, 2015 to May 7, 2015. Simple random sampling technique was applied after taking all registered mothers who have infants less than 6 months old from local health extension workers of each kebele. A total of 423 mothers with infant less than six month old were included in this study. The data was collected from all four Kebeles using interviewer administered questionnaire. Descriptive and inferential statistics were used to present the data. Both bivariate and multivariate logistic regression analyses were used to identify factors associated with timely initiation breastfeeding.
Result
Prevalence of timely initiation of breastfeeding was78.8 % [95 % CL: 74.88 %, 82.72 %]. Mothers who gave birth to their infant in a health institution [AOR = 3.486(1.253, 9.700)], birthed vaginally [AOR = 5.722(3.134, 11.246)] and didn’t give prelacteal food [AOR = 4.627(2.095, 10.220)] were more likely to initiate breastfeeding early than their counterparts.
Conclusion
Prevalence of timely initiation of breastfeeding in the study area was 78.8 %. Place of delivery, mode of delivery and prelactal feeding were the independent predictors of timely initiation of breastfeeding. Recommendations to increase timely initiation of breastfeeding were: encouraging mothers to deliver their child in a health institution, minimizing caesarean delivery as much as possible and educating mothers and community as a whole to avoid traditional prelactal feeding practice.
Keywords: Timely initiation of breastfeeding, Prevalence, Associated factors, Motta, Ethiopia
Background
It is estimated that every day, as many as 4,000 infants and young children die worldwide because they are not breastfed [1]. World Health Organization recommends initiation of breastfeeding within one hour after birth, exclusive breastfeeding for the first six months of infant life and continuation of breastfeeding up to two years [2]. Timely initiation of breastfeeding has the potential to prevent 22 % of neonatal deaths if all infants were breastfed within an hour after birth [3].
Early breastfeeding provides numerous benefits to infants, women, and society. It creates a special bond between mother and infant, enhances dental development, reduces risk for allergies, aids in cognitive development, and decreases the risk for obesity in later life. It also helps the uterus return to pre-pregnancy size faster: reduces risk of breast, ovarian, and uterine cancers: decreases the risk for osteoporosis; enhances emotional health, and saves money [4, 5].
Many factors have found to affect timely initiation of breastfeeding such as; societal beliefs favoring to start with other feeding, lack of adequate support in health facilities and in the community, aggressive promotion of infant formula through medias, and lack of knowledge on the dangers artificial feeding among women, their partners, and families [6].
The Ethiopian Demographic and Health Survey estimated approximately 51.5 % of newborns were initiated to breastfeeding within one hour of birth [7]. Ethiopian HSDP IV planned to increase in the proportion of timely initiation of breastfeeding to 92 % by the end of 2015 [8].
Breastfeeding and good nutrition for children are recognized as essential for achieving the Millennium Development Goals (MDG), particularly the goals relating to child survival, such as reducing child mortality by 2/3 between 1990 and 2015 [9].
Therefore, this study was conducted in Motta town to assess early initiation of breastfeeding and associated factors among mothers of children aged less than 6 months.
Methods
Study setting and participants
Community based quantitative cross-sectional study was conducted from April 7 to May 7, 2015. The study was conducted in Motta town which is located in Amhara National Regional State, East Gojjam Zone, Ethiopia. It is bordered in all dimensions by Hulet Ejju Enesse woreda. It is 371 km away from Addis Ababa. Motta town was founded in 1754. The town has a total of 4 kebeles. The population of the town is 33,500. The town has a total of 17 governmental and nongovernmental health care institutions. There is a hospital, health center, five clinics, a pharmacy and nine drug stores.
The sample size was calculated using single population proportion formula by considering the following assumptions; P (proportion of timely initiated mothers) = 50 % to get maximum sample size to represent the community, 95 % level of confidence 95 %, level of significance = 5 %, margin of error (d) = 5 and 10 % non- response rate. Using simple random sampling technique 423 mothers participated in the study. To select study participants from each kebele first the sample size was propertionally allocated to size and then a lottery method was used.
Measurement
A structured interviewer administered questionnaire was used to collect data from participants or mothers of a child. The questionnaire was constructed by adopting from Ethiopia Demographic and Health Survey (EDHS) 2011 and from previous research done on similar topic and modified accordingly.
A one day infant diet recall method was used for assessing exclusive breastfeeding. Four diploma nurses were recruited as data collectors and two Bachelor of Science nurses were recruited as supervisors. All data collectors and supervisors were oriented and trained on how to interview and record the data one day before the survey.
Operational definitions
Timely initiation of breastfeeding
If an infant within one hour of birth is put on mother’s breast to feed.
Pre-lacteal feeding
If an infant within the first three days of life was fed something other than breast milk.
Adequate knowledge about breast feeding
If a mother answered half or more questions correctly, from questions which were asked to measure breastfeeding knowledge, then adequate knowledge was determined.
Statistical analysis
The collected data was checked manually for completeness and consistencies, and then it was coded and entered in EPI Info version 3.5.3 and exported to SPSS version 16 for analysis. Descriptive statistics was used to summarize the socio-demographic characteristics’ of the study participants and the prevalence of timely initiation of breast feeding. To identify factors associated with timely initiation breastfeeding practice, binary logistic regression analysis carried out at two levels, first bivariate logistic regression was performed to each independent variable with the outcome variable and those variables with a p value < 0.05 was included in the final model (multivariate analysis). Strength of association was measured using odds ratio, and 95 % confidence intervals. Statistical significance was declared at P value < 0.05.
Ethical clearance was obtained from Addis Ababa University, department of nursing and midwifery research committee. Each study participant was adequately informed about the objective of the study and anticipated benefit and risk of the study by their data collector. Verbal consent was obtained from study participants for protecting autonomy and ensuring confidentiality. Respondents were also told of their right not to respond to the questions if they did not want to respond or if they wished to terminate the interview at any time.
Results
Socio-demographic characteristics
Out of 423 eligible mothers, 405 agreed to participate in this study, which made a response rate of 95.7 %. Age of mothers ranges from 18 to 47 years, with median age of 27 year. Around one third 127 (31.4 %) of mothers were between 25 and 29 years. More than half 229 (56.5 %) of mothers were Orthodox Christian followers. With regard to educational status, 162(40.2 %) mothers received no education. The majority 323 (79.6 %) of study participants were unemployed mothers. From all, 328(80 %) mothers live in a nuclear family. The average household income of the respondents was 76.22 USD month (SD ± 62.98), and 198(48.9 %) respondents earn less than 50 USD per month (Table 1).
Table 1.
Socio-demographic characteristics mothers (respondents) who have infants less than six months old, in Motta town, East Gojjam Zone, Ethiopia, 2015
| Variable | Category(n = 405) | Frequency | Percent (%) |
|---|---|---|---|
| Age of mother(in years) | 15–19 | 5 | 1.2 |
| 20–24 | 106 | 26.2 | |
| 25–29 | 127 | 31.4 | |
| 30–34 | 94 | 23.2 | |
| 35 and above | 73 | 18.0 | |
| Religion | Orthodox | 229 | 56.5 |
| Muslim | 158 | 39 | |
| Othersa | 18 | 4.4 | |
| Ethnicity | Amhara | 388 | 95.8 |
| Othersb | 17 | 4.2 | |
| Level of education of mother | No education | 163 | 40.2 |
| Primary level (1–8 grade) | 120 | 30.0 | |
| High school and above | 122 | 29.8 | |
| Occupational status of mother | Employed | 82 | 20.3 |
| Unemployed | 323 | 79.6 | |
| Current marital status | Married | 347 | 85.7 |
| Unmarriedc | 58 | 14.3 | |
| Husband educational level | No education | 79 | 22.4 |
| Primary level (1–8 grade) | 131 | 37.1 | |
| High school and above | 143 | 40.5 | |
| Husband occupation | Employed | 111 | 31.5 |
| Unemployed | 294 | 68.5 | |
| Type of family | Nuclear family | 328 | 80 |
| Extended family | 77 | 20 | |
| Household income/month/ | <50 USDd | 198 | 48.9 |
| 50–100 USD | 107 | 26.4 | |
| >100 USD | 100 | 24.7 |
aProtestant and Catholic bOromo, Tigrie and Gurage csingle, widowed and separeted dunited states dollar
Infant and maternal health service utilization characteristics
Almost half 211 (52.1 %) of mothers have 2–3 children. One hundred ten (27.2 %) infants were first in birth order. Majority 349 (86.2 %) of mothers received antenatal care (ANC) during period of pregnancy out of them only 206 (59.0 %) were counseled concerning to optimal breast feeding practice. With regarding to place of delivery, most 338 (83.5 %) mothers delivered in a health institution. From total respondents, around half 197 (48.6 %) of mothers received postnatal care (Table 2).
Table 2.
Infant and maternal health service utilization characteristics of study participants in Motta town, East Gojjam zone, Ethiopia, 2015
| Variable | Response (n = 423) | Frequency | Percent (%) |
|---|---|---|---|
| Number of children | One | 111 | 27.4 |
| Two to three | 211 | 52.1 | |
| Four and above | 83 | 20.5 | |
| Sex of child | Male | 180 | 44.4 |
| Female | 225 | 55.6 | |
| Age of child | 0–1 month | 55 | 13.6 |
| 2–3 month | 119 | 29.4 | |
| 4–5 month | 231 | 57.0 | |
| Birth order | First | 110 | 27.2 |
| Second | 125 | 30.9 | |
| Third and above | 169 | 41.9 | |
| Birth interval | Up to three years | 236 | 58.3 |
| Three years and above | 169 | 41.7 | |
| ANC follow up | Yes | 349 | 86.2 |
| No | 56 | 13.8 | |
| Number of ANC follow up (n = 349) | Less than or equal to three | 86 | 14.6 |
| Four times | 263 | 75.4 | |
| Counseling related breast feeding during ANC(n = 349) | Yes | 206 | 59.0 |
| No | 143 | 41.0 | |
| Place of birth | Health facility | 338 | 83.5 |
| Home | 67 | 16.5 | |
| Mode of delivery | Vaginal /normal | 367 | 90.6 |
| Caesarean section | 38 | 9.4 | |
| PNC | Yes | 197 | 48.6 |
| No | 208 | 51.4 | |
| Counseling regarding to breastfeeding during PNC(n = 197) | Yes | 186 | 94.4 |
| no | 11 | 5.6 |
Breastfeeding and related practices
From total, 320 (78.8 %) mothers initiated breast milk to infant immediately within one hour of birth. Most mothers 323 (79.8 %) fed colostrum/first milk to the newborn. Majority 323 (79.8 %) of mothers didn’t give prelactal food other than breast milk within three days of an infant life. Prevalence of timely initiation of breastfeeding in this study was 78.8 %. Among mothers who didn’t initiate breastfeeding timely to the newborn, the main reasons mentioned were; caesarean section 28 (32.9 %), baby was sick 12 (14.1 %), mother was sick 15 (17.6 %) and delayed milk secretion 30 (35.3 %) (Table 3).
Table 3.
Breastfeeding related practices of mothers who have infants less than six months old in Motta town, East Gojjam zone, Ethiopia, 2015
| Variables | Responses (n = 405) | Frequency | Percent (%) |
|---|---|---|---|
| Breastfeeding experience of current infant | Yes | 405 | 100 |
| No | 0 | 0.0 | |
| Timely initiation of breastfed | Immediately with in 1 h | 319 | 79.0 |
| 1 h to 1 day | 78 | 19.3 | |
| After one day | 8 | 2 | |
| Reasons for not initiating within one hour | Caesarean section | 28 | 32.9 |
| Baby was sick | 12 | 14.1 | |
| Mother was sick | 15 | 17.6 | |
| Delayed milk secretion | 30 | 35.3 | |
| Colostrum feeding | Yes | 323 | 79.8 |
| No | 82 | 20.2 | |
| Prelacteal feeding | No | 323 | 79.8 |
| Yes | 82 | 20.2 |
Knowledge and informational status of mothers regarding to breastfeeding
Almost two thirds, 283 (69.9 %), of mothers know that breastmilk is initiation within one hour of birth of infant is recommended and 310 (76.5 %) mothers had adequate knowledge regarding to breastfeeding. Regarding to information about exclusive breastfeeding 362(89.4 %) mothers were informed about EBF from different sources (Fig. 1).
Fig. 1.
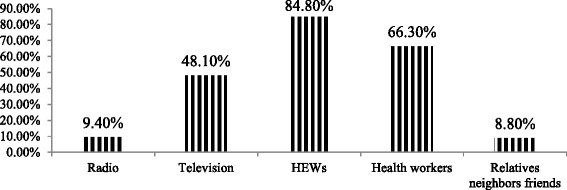
Sources of information for mothers about breastfeeding who have infant less than six months old in Motta town, East Gojjam zone, Ethiopia, 2015
Factors associated with timely initiation of breastfeeding
From total participants of this study, 79 % of mothers initiated breastfeeding to thier newborn within one hour of birth. The independet predictors for timely initiation of breastfeeding were; marital status, number of children, antenatal care, counseling about breastfeeding during antenatal care, place of birth, mode of delivery and husband support.
The final predictors for timely initiation of breastfeeding were counseling during ANC, place of birth and mode of delivery.
Breastfeeding counseling during pregnancy facilitates mothers to initiate breastfeeding immediately after birth of newborn. Mothers who were counseled regarding breastfeeding during ANC were almost 6 times more likely to initiate breastmilk immediately after birth of infant than mothers who were not counseled [AOR = 6.684(3.557, 12.58)].
Whereas mothers who gave birth in a health facility were almost three times more likely to initiate breastfeeding than those mothers who birthed their child at home [AOR = 2.831(1.134,7.066].
Mode of delivery was also significantly associated with timely initiation of breastfeeding. Mothers who experienced a normal vaginal dilevery were almost 4 times more likely to initiate breastfeeding immediately when compared to mothers who delivered by caesarean section [AOR = 3.722(1.484, 9.334)] (Table 4).
Table 4.
Factors that affect timely initiation breastfeeding among mothers of infants age less than 6 months using bivariate and multivariate logistic regression analysis model, East Gojjam, Ethiopia, 2015
| Variables | Timely initiation of breastfeeding | |||||
|---|---|---|---|---|---|---|
| Yes (N & %) |
No (N & %) |
COR (95 % CL) | AOR(95 % CL) | p- value | ||
| Marital status | Married | 280(80.7) | 67(19.3) | 2.036(1.107, 3.746) | ||
| Unmarried | 38(67.2) | 19(32.8) | 1 | |||
| Number of children | 1 | 90(81.1) | 21(18.9) | 1.955(1.006,3.797) | ||
| 1–3 | 172(81.5) | 39(18.5) | 2.012(1.127,3.592) | |||
| 4+ | 57(68.7) | 26(31.5) | 1 | |||
| ANC | Yes | 282(80.8) | 67(19.02) | 2.161(1.171,3.994) | ||
| No | 37(66.1) | 19(33.9) | 1 | |||
| Breastfeeding counseling during ANC | Yes | 177(85.9) | 75(14.1) | 2.209(1.287, 3.791) | ||
| No | 105(73.4) | 29(26.6) | 1 | 1 | ||
| Place of birth | Health facility | 278(82.2) | 60(17.8) | 2.938(1.670, 5.171) | 3.486(1.253,9.700)* | 0.007 |
| Home | 41(61.2) | 26(38.8) | 1 | 1 | ||
| Mode of delivery | Normal/vaginal | 313(85.3) | 54(14.7) | 6.442(3.124, 12.36) | 5.722(3.134,11.246)* | 0.0001 |
| C/S | 16(42.1) | 22(57.9) | 1 | 1 | ||
| Colostrum feeding | Yes | 270(83.6) | 53(16.4) | 3.431(2.018,5.832) | ||
| No | 49(59.8) | 33(60.2) | 1 | |||
| Prelactal feeding | No | 276(85.7) | 46(14.3) | 5.714(3.351,9.745) | 4.627(2.095, 10.220)* | 0.0001 |
| Yes | 42(51.2) | 40(48.8) | 1 | |||
N number, % percent
1 = reference
Discussion
In spite of what is known about timely initiation of breastfeeding; the practice is not satisfactory in the study area. Only 78.8 % [95 % CL: 74.88 %, 82.72 %] of mothers reported early initiation of breastfeeding, which is lower than Ethiopian HSDP IV target level; i.e. to increase the proportion of timely initiation breastfeeding mother from 51.5 to 92 % by the end of 2015 [8].
This result is higher when compared to the 2011 Ethiopian DHS report 51.5 % [7] and from studies done in; Saudi Arabia 22 % [10], Raya Kobo Northwest Ethiopia 71.7 % [11], Goba district Southeast Ethiopia 52.4 % [12], Arba Minch zuria southern Ethiopia 57.6 % [13], India 36.4 % [14], 34 % among those who deliver their child through vagina in Harcourt teaching hospital [15], Nepal 66.4 % [16], in a study using 2011 EDHS 52 % [17], Tanzania 51 % [18], Timor Liste 46.1 % [19], in Lebanon 55.9 % [20], in hospital delivered infants India 36.4 % [21], in baby friendly hospitals in Turkey 35.2 % [22].
Such variations may due to methodological variations between studies, dissimilarities in infant and maternal socio-demographic characteristics and other differences in sociocultural, economical, health and health service utilization characteristics between respondents of the referenced areas and the study place.
Among mothers who didn’t initiate timely breastfeeding, the main reasons mentioned were; caesarean section (32.9 %), baby was sick (14.1 %), mother was sick (17.6 %) and delayed milk secretion (35.3 %).
Place of delivery were significantly associated with timely initiation of breastfeeding. Mothers who deliver their child in health institution were almost 3.5 times more likely to practice timely initiation of breastfeeding than others. This finding is consistent with studies done in; Goba district Ethiopia [12], Nepal [16] and Tanzania [18]. This may be due to large number of home deliveries in the country and the cultural or traditional activities in the community that promote prelactal feeding to the infant before starting breast milk.
Mode of delivery was also significantly associated with timely initiation of breastfeeding in the study area. Mothers who gave birth vaginally were almost six times more likely to initiate breastfeeding than mothers who deliver through caesaraan section. This result is in line with studies done in Saudi Arabia [10], a systematic review done of Medline LILACS Scopus and Web of Science electronic databases [23], Harcourt teaching hospital [15], a study using 2011 EDHS [17], Tanzania [18], Lebanon [20] and Turkey [22]. This may be due to the effects of anesthesia delaying the onset of lactation. Appropriate guidelines for caesarean deliveries are needed to minimize delays in initiation of breastfeeding. Prospective mothers and health workers should be informed about the negative association between pre labor caesarean delivery decisions, and breastfeeding and the implications for infant wellbeing.
Whereas mothers who did not give prelacteal feeds were almost 4.6 times more likely to initiate breastfeeding within one hour than mothers who introduce other fluids, which is similar with findings in;- Raya kobo Ethiopia [11], western Nepal [24], Saudi Arabia [10] and India [21]. The introduction of prelacteal feeds may decrease infants suckling activity which in turn can affect or decrease maternal milk production due to decreased breast stimulation. The use of prelacteal feeding appears to be a constriant in the promotion of EBF. Explanations this study provided were delayed milk secretion; due to breast problems, illness of mother and culture/ traditional practices such as the belief that giving liquid will clean the baby’s throat. This habit harms the newborn and exposes him/her to various morbidities and therefore; the practice needs to be discouraged.
A limitation of this study is that only the quantitative aspects of timely initiation of breastfeeding were assessed. Also results may under estimate the prevalence of timely initiation of breastfeeding in the study area due to recall bais.
Conclusion
The prevalence of timely initiation of breastfeeding in the study area was 78.8 %, which was lower than the country recommended level. Among different socio-demographic, health service, maternal, and infant related factors studied; the place of delivery, mode of delivery and not giving prelactal feeding were the determinant factors for higher chance of timely initiation of breastfeeding.
Recommendations for improving EBF include; behavior change communication to avoid traditional activities, minimizing indications of caesarean delivery by health professionals, training of health professionals regarding to infant feeding practices, community based breastfeeding education and counseling to pregnant women and encouraging all mothers to give birth in health facilities.
Acknowledgement
This study received financial support from Addis Ababa University College of Health Sciences School of Allied Health Sciences. I would like to thank librarian staffs the school for their cooperation during the study. The study participants are duly acknowledged for voluntary participation and responding to the questionnaire. I would like to acknowlege data collectors and supervisors for their cooperation during the field work.
Availability of data and materials
The date of this study can’t be shared publically due to presence of sensitive (confidential) participants’ information.
Author’s contribution
TT contributed to the design of this study. TT conceived and designed study, collected, analyzed and interpreted data; drafted the manuscript for important intellectual content. The author reviewed and revised the draft further and approved the final version for submission.
Competing interests
The author declared that there is no any competing interest.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Ethical clearance was obtained from AAU, department of nursing and midwifery research committee. Each study participant was adequately informed about the objective of the study and anticipated benefit and risk of the study by their data collector. Respondents were also told of their right not to respond to the questions if they did not want to respond or if they wished to terminate the interview at any time. Verbal consent was obtained from study participants for protecting autonomy and ensuring confidentiality.
Abbreviations
- AAU
Addis Ababa University
- ANC
Antenatal care
- AOR
Adjusted odds ratio
- CL
Confidence level
- EDHS
Ethiopian Demographic Health Survey
- MDG
Millenium Development Goals
- PNC
Postnatal care
- SD
Standard deviation
- USD
United States Dollar
- WHO
World Health Organization
References
- 1.WHO . Indicators for assessing infant and young child feeding practice measurement. Conclusions of a consensus meeting held in Washington D.C., USA. 2010. p. 2. [Google Scholar]
- 2.WHO . Exclusive breastfeeding for Six months best for babies. Geneva: WHO; 2011. [Google Scholar]
- 3.Edmond KM, et al. Delayed breastfeeding initiation increases risk of neonatal mortality. Pediatrics. 2006;117(3):e380–e386. doi: 10.1542/peds.2005-1496. [DOI] [PubMed] [Google Scholar]
- 4.Iowa women, infant and child Program . Breastfeeding promotion and support guidelines for healthy full term infants. Iowa: Department of Public Health; 2001. [Google Scholar]
- 5.Victora CG, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475–490. doi: 10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- 6.WHO . Global strategy for infant and young child feeding. Geneva: WHO; 2003. [PubMed] [Google Scholar]
- 7.Central Statistical Agency . Ethiopia Demographic and Health Survey 2011 A.A, Ethiopia. Calverton: ICF International; 2012. [Google Scholar]
- 8.Federal Ministry of Health of Ethiopia . Health Sector Development Program IV (2010/11- 2014/15) 2010. [Google Scholar]
- 9.USAID . MCH program description, overall MCH and health sector situation of Ethiopia. Ethiopia: USAID; 2008. [Google Scholar]
- 10.Dorgham LS, et al. Assessment of initiation of breastfeeding, prevalence of exclusive breast feeding and their predictors in Taif, KSA. Life Science Journal. 2014;11(1):1–9. [Google Scholar]
- 11.Liben ML. Determinants of early initiation of breastfeeding among mothers: the case of Raya Kobo District, Northeast Ethiopia: a cross-sectional study. Int J Nutr Food Sci. 2015;4(3):289–294. doi: 10.11648/j.ijnfs.20150403.16. [DOI] [Google Scholar]
- 12.Setegn T, Gerbaba M, Belachew T. Determinants of timely initiation of breastfeeding among mothers in Goba Woreda, South East Ethiopia: A cross sectional study. BMC Public Health. 2011;11(1):217. doi: 10.1186/1471-2458-11-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adugna DT. Women’s perception and risk factors for delayed initiation of breastfeeding in Arba Minch Zuria, Southern Ethiopia. Int Breastfeed J. 2014;9(1):8. doi: 10.1186/1746-4358-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Athavale A, et al. Initiation of breast-feeding by urban women. Health Popul Perspect Issues. 2004;27(2):117–125. [Google Scholar]
- 15.Awi D, Alikor E. Barriers to timely initiation of breastfeeding among mothers of healthy full-term babies who deliver at the University of Port Harcourt Teaching Hospital. Niger J Clin Pract. 2007;9(1):57–64. [PubMed] [Google Scholar]
- 16.Adhikari M, et al. Factors associated with early initiation of breastfeeding among Nepalese mothers: further analysis of Nepal Demographic and Health Survey, 2011. Int Breastfeed J. 2014;9(1):21. doi: 10.1186/s13006-014-0021-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lakew Y, Tabar L, Haile D. Socio-medical determinants of timely breastfeeding initiation in Ethiopia: Evidence from the 2011 nation wide Demographic and Health Survey. Int Breastfeed J. 2015;10(1):1. doi: 10.1186/s13006-015-0050-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Exavery A, et al. Determinants of early initiation of breastfeeding in rural Tanzania. Int Breastfeed J. 2015;10(1):1. doi: 10.1186/s13006-015-0052-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Senarath U, Dibley M, Agho K. Breastfeeding practices and associated factors among children under 24 months of age in Timor-Leste. Eur J Clin Nutr. 2007;61(3):387–397. doi: 10.1038/sj.ejcn.1602536. [DOI] [PubMed] [Google Scholar]
- 20.Batal M, et al. Breast-feeding and feeding practices of infants in a developing country: a national survey in Lebanon. Public Health Nutr. 2006;9(03):313–319. doi: 10.1079/PHN2006860. [DOI] [PubMed] [Google Scholar]
- 21.Patel A, Banerjee A, Kaletwad A. Timely initiation of breastfeeding and pre-lacteal feeding rates in hospital delivered babies in India and associated factors. Pediatr Res. 2011;70:52. doi: 10.1038/pr.2011.277. [DOI] [Google Scholar]
- 22.Orun E, et al. Factors associated with breastfeeding initiation time in a baby-friendly hospital. Turk J Pediatr. 2010;52(1):10–6. [PubMed] [Google Scholar]
- 23.Esteves TMB, et al. Factors associated to breastfeeding in the first hour of life: systematic review. Rev Saude Publica. 2014;48(4):697–708. doi: 10.1590/S0034-8910.2014048005278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khanal V, et al. Factors associated with the introduction of prelacteal feeds in Nepal: findings from the Nepal demographic and health survey 2011. Int Breastfeed J. 2013;8(1):9. doi: 10.1186/1746-4358-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The date of this study can’t be shared publically due to presence of sensitive (confidential) participants’ information.


