Abstract
Background
Patients attending hospital emergency departments (ED) commonly cite the urgency and severity of their condition as the main reason for choosing the ED. However, the patients’ perception of urgency and severity may be different to the nurses’ perception of their urgency and severity, which is underpinned by their professional experience, knowledge, training and skills. This discordance may be a cause of patient dissatisfaction. The purpose of this study is to understand the extent of agreement/disagreement between the patient’s perceived priority and actual triage category and associated factors.
Methods
A cross-sectional survey of 417 patients attending eight public hospital EDs in Queensland, Australia between March and May 2011 was conducted. The survey included patient’s perceived priority and other health-related, socio-demographic and perceptual factors. Patients’ triage category data were retrieved from their ED records and linked back to their survey data. Descriptive and multinomial logistic regression analyses were used.
Results
Over 48 % of the respondents expected to be given higher priority than the actual triage category they were assigned; 31 % had their perceived priority matched with the triage category; and 20 % of the respondents expected a lower priority than the triage category they received (Kappa 0.07, p < 0.01). Patients who expected a higher priority tended to be more frequent users (≥3 times in the past six months), and to score higher on perceived seriousness, perceived urgency, and pain score compared to the patients whose perceived priority matched the triage category or anticipated a lower priority. In the multivariate analysis, only perceived urgency remained significantly associated with expected higher priority (OR = 1.27, 95 % CI: 1.14–1.43).
Discussion
Our findings clearly confirmed the discrepancy between patient perception of urgency and staff assessment of urgency. This can have important implications particularly for the patients who underrate the urgency of their condition. Improved and open communication and the incorporation of the ‘patient voice’ into the triage process require understanding the patient’s perspectives and their involvement in the decision making process.
Conclusions
Noted differences between patient and practitioner perception of clinical urgency were identifed in this study.
Keywords: Emergency department, Inter-rater agreement, Triage, Patient perception, Perceived priority
Background
While hospital emergency departments’ (EDs) primary role is to treat the acutely ill and injured, they also provide a safety net for people who do not have access or cannot afford private health services [1, 2]. This coincides with the rising demand for and use of EDs in many countries including Australia [3, 4]. Although many factors contribute to this increase, some literature point to “inappropriate” users [5–9] who are also referred to as “primary care” or “general practitioner (GP) type” patients. Advocates of this opinion use criteria such as low triage category and lack of the need for admission into the hospital wards to assert that these patients do not need to be in an ED in the first place and should visit a primary health care service instead [10, 11]. On the other hand, opponents of this view assert that the claims of inappropriateness based on post hoc diagnoses are themselves inappropriate as patients are neither equipped with medical knowledge and skills nor should they be expected to be able to self-diagnose and identify the type of medical care that suits them [10, 11].
An ED or emergency care centre is defined as a place where people who perceive a need for urgent health advice or treatment turn to [12, 13]. On arrival to an ED, patients should be seen and briefly assessed by a triage nurse who assigns them a triage category 1–5 based on the Australasian Triage Scale (ATS) indicating how urgently the patient is to be attended by the medical staff (ATS-1 = immediately; ATS-5 = within 2 h) [14]. With studies showing that patient satisfaction is positively related to better access to the health system [13], and good communication with the staff [15–17], a discrepancy between the patient’s and practitioner’s views at the point of triage can become an early source of dissatisfaction and complaints for a patient and their family. An Australian study undertaken 10 years ago found that while the participants did not have a clear understanding of how the triage system worked, they wanted to know their initial triage category and receive ongoing information about it [18]. In today’s patient-centred approach to health care delivery, further research is required in this area.
Patients attend EDs because they see their condition as urgent and requiring medical attention [19–23]. However, the triage nurse or doctor who examines the patient may not share the patient’s sense of urgency. Furthermore, doctors and nurses can disagree over a patient’s triage category [18, 24–26]. Thus, expecting the patient to share a similar view with the triage nurse or doctor and agree with their decision can prove difficult. This suggests that there may be a discrepancy between patient’s perception and nurse’s perception of acuity; however further work is required to more definitively understand this.
The aim of this study is to assess the degree of agreement between patients’ perceived priority and actual triage category in the ED. Factors that may explain any concordance or discordance will also be explored.
Methods
Detailed information about the study design, population, sampling, data collection, theoretical framework and measures have been previously published [23, 27, 28]. In summary, a cross-sectional survey of ED patients was conducted in eight public hospitals across Queensland, Australia. Four of the hospitals were located in major cities, two in inner regional areas, and two were in outer regional and remote areas. One ED was a children’s ED and all others treated both adults and children. The data collection was conducted by four members of the research team and a group of eight trained interviewers in March to May 2011 (corresponding to autumn season). Data collection took place between 8 am and 10 pm on at least two midweek and one weekend days in each ED to capture a variety of patients. Of the total of 1608 patients in all eight emergency departments the interviewers were able to approach 1361 patients (85 %) and seek their consent to participate in the study. In total, 911 valid surveys were collected for the study, out of which 417 consented for their medical records to be accessed for this analysis (response rate = 31 % of those approached). Figure 1 shows the data collection process.
Fig. 1.
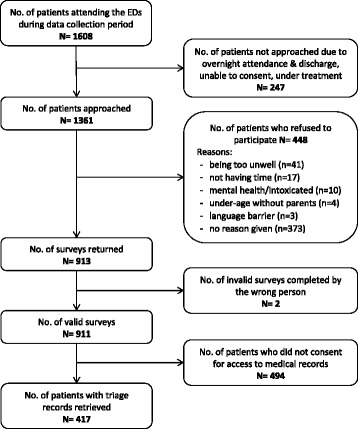
Flow chart of data collection process
As part of the self-assessment questions, the respondents were asked what priority they thought they should be given based on their perceived severity and urgency of their condition. The response options were aligned with the recommended Time-to-be-Seen by the Australasian Triage Scale, that is: (1) Immediately; (2) Within 10 min; (3) Within 30 min; (4) Within 60 min; and (5) Within 2 h [14].
To be able to compare patient responses with their actual triage category, participants were requested to provide consent for their medical records to be accessed by the research team. The triage category for the patients who consented was retrieved from the Emergency Department Information System (EDIS), and added to their survey responses.
All data were managed and analysed using IBM SPSS Statistics V21.0 (IBM Corp.). Univariate analysis, Crosstabs, Chi-squared and F tests were used to analyse the data and bivariate associations of the dependent variable (i.e. agreement between patient perceived priority and actual nurse assigned triage category) with independent factors. Kappa, Tau-b and Gamma statistics were used to assess the strength of the inter-rater agreement. All factors that had a statistically significant association with the dependent variable at p ≤0.05 were entered into a Multinomial Logistic Regression to estimate the relative strength of predictor variables, using the Main Effects model with Forward Entry, and Confidence Interval (CI) set at 95 %.
Results
A total of 911 valid surveys were collected, of whom 45.8 % (n = 417) consented for their triage category to be retrieved from their medical records. As Table 1 shows, the consented and non-consented respondents were not significantly different in terms of their general demographic and perceived health characteristics suggesting representativeness of the sample and the ability to generalise the findings to the broader patient population.
Table 1.
Respondents’ characteristics by consent group
| Characteristic | Consented | Non-consented | χ 2 (p) | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Respondent | |||||
| - Patient | 309 | 45.0 | 378 | 55.0 | 0.71 (0.22) |
| - Parent/Carer | 108 | 48.2 | 116 | 51.8 | |
| Age (year) | |||||
| - Mean | 42.2 | 43.9 | F test: 1.79 | ||
| - Standard Deviation | 18.3 | 18.4 | (0.18) | ||
| Gender | |||||
| - Male | 188 | 46.8 | 214 | 53.2 | 0.20 (0.35) |
| - Female | 224 | 48.3 | 240 | 51.7 | |
| Indigenous status | |||||
| - Indigenousa | 23 | 54.8 | 19 | 45.2 | 0.66 (0.26) |
| - Non-Indigenous | 389 | 48.3 | 416 | 51.7 | |
| Country of birth | |||||
| - Australia | 322 | 49.2 | 333 | 50.8 | 2.36 (0.07) |
| - Other | 90 | 43.1 | 119 | 56.9 | |
| Household weekly income | |||||
| - $1–249 | 23 | 54.8 | 19 | 45.2 | 2.46 (0.65) |
| - $250–599 | 87 | 51.5 | 82 | 48.5 | |
| - $600–999 | 104 | 52.0 | 96 | 48.0 | |
| - $1000–1599 | 84 | 45.7 | 100 | 54.3 | |
| - $1600,+ | 65 | 52.4 | 59 | 47.6 | |
| Highest education | |||||
| - None/Primary | 46 | 54.1 | 39 | 45.9 | 2.63 (0.27) |
| - High school/ Trade | 207 | 46.7 | 236 | 53.3 | |
| - Tertiary | 157 | 51.6 | 147 | 48.4 | |
| General health status | |||||
| - Poor | 22 | 45.8 | 26 | 54.2 | 1.25 (0.87) |
| - Fair | 55 | 50.9 | 53 | 49.1 | |
| - Good | 113 | 46.3 | 131 | 53.7 | |
| - Very good | 122 | 44.9 | 150 | 55.1 | |
| - Excellent | 100 | 45.2 | 121 | 54.8 | |
| Patient perceived priority | |||||
| 1 - Immediately | 54 | 49.5 | 55 | 50.5 | 3.80 (0.43) |
| 2 - Within 10 min | 63 | 42.9 | 84 | 57.1 | |
| 3 - Within 30 min | 128 | 44.1 | 162 | 55.9 | |
| 4 - Within 60 min | 100 | 50.3 | 99 | 49.7 | |
| 5 - Within 2 h | 61 | 50.8 | 59 | 49.2 | |
| ED use in past 6 months | |||||
| - None | 228 | 46.1 | 267 | 53.9 | 1.80 (0.41) |
| - 1–2 times | 132 | 48.9 | 138 | 51.1 | |
| - 3,+ times | 53 | 41.7 | 74 | 58.3 | |
| Totalb | 417 | 45.8 | 494 | 54.2 | |
aIncludes Aboriginals and Torres Strait Islanders
bWhere the sum of sub-categories does not equal the Total, indicates missing values
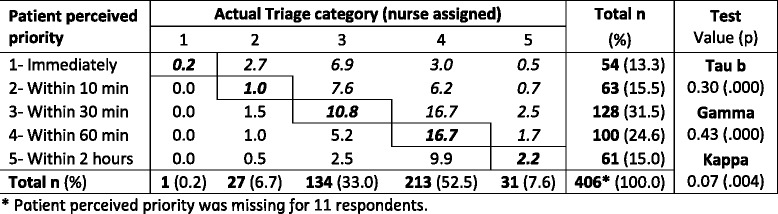
As Table 2 shows, in 30.9 % of the respondents’ who consented to medical record access, perceived priority matched the triage category (bold italic cells); 48.5 % of expected to be given higher priority (italic cells) than the actual triage category they were assigned; and 20.6 % of the respondents expected a lower priority than the actual triage category. Although there is a tendency for patients to over-rate their priority, the correlation between perceived priority and actual triage category is weak (based on Tau-b and Gamma), and the Kappa shows no statistically significant agreement between the two variables.
Table 2.
Agreement between perceived priority and triage category (% of Total)
Factors associated with Inter-rater agreement
The concordance between the two variables (i.e. Patient’s perceived priority and Actual triage category) was also considered in three categories for further analysis:
Expected higher priority, includes those who received a lower triage category than their perceived priority (n = 197);
Concordance, includes those whose triage category matched their perceived priority (n = 126);
Expected lower priority, includes those who received a higher triage category than their perceived priority (n = 83).
We tested the bivariate associations between inter-rater agreement and other variables including socio-demographic factors (age, gender, employment status, income, education, country of birth, Indigenous status, living arrangement, social support, self-efficacy), health related factors (perceived health status, urgency, seriousness and pain, previous ED attendance, arrival method) and reasons for attending ED. Table 3 shows the factors that were significantly associated with inter-rater agreement (only statistically significant associations with p ≤ 0.05 have been displayed).
Table 3.
Inter-rater agreement and associated factors
| Inter-rater agreement | ||||
|---|---|---|---|---|
| Factor | Expected higher priority | Concordance | Expected lower priority | Test (p) |
| ED use in past 6 months | % (95 % CI) | % (95 % CI) | % (95 % CI) | |
| - None | 42.2 (35.9–48.7) | 35.9 (29.9–42.4) | 22.0 (17.0–27.8) | χ2 = 11.63 |
| - 1–2 times | 53.4 (44.9–61.8) | 24.4 (17.9–32.4) | 22.1 (15.9–30.0) | (0.02) |
| - 3,+ times | 62.7 (49.0–74.7) | 27.5 (17.1–40.9) | 9.8 (4.3–21.0) | |
| Needed urgent care | ||||
| - Not considered | 34.0 (22.2–48.3) | 42.6 (29.5–56.7) | 23.4 (13.6–37.2) | χ2 = 16.51 |
| - Considered to some extent | 40.4 (32.7–48.7) | 32.6 (25.4–40.7) | 27.0 (20.3–34.8) | (0.002) |
| - Considered to a great extent | 58.0 (51.2–64.6) | 25.9 (20.3–32.2) | 16.1 (11.7–21.7) | |
| Perceived seriousness (1–10) | ||||
| - Mean (95 % CI) | 7.1 (6.8–7.4) | 6.0 (5.6–6.3) | 6.1 (5.7–6.5) | F = 14.23 |
| - Standard Deviation | 2.1 | 2.0 | 1.9 | (<0.001) |
| Perceived urgency (1–10) | ||||
| - Mean (95 % CI) | 7.4 (7.1–7.7) | 6.2 (5.8–6.6) | 6.0 (5.5–6.5) | F = 17.11 |
| - Standard Deviation | 2.2 | 2.2 | 2.3 | (<0.001) |
| Pain score (1–10) | ||||
| - Mean (95 % CI) | 6.5 (6.2–6.9) | 5.7 (5.2–6.2) | 5.3 (4.7–5.9) | F = 7.65 |
| - Standard Deviation | 2.6 | 2.8 | 2.6 | (<0.001) |
| Total (%) | 197 (48.5) | 126 (31.0) | 83 (20.4) | 406a (100.0) |
aPatient perceived priority was missing for 11 respondents
Expected higher priority was significantly associated with less frequent ED attendance in the past six months (χ2 = 11.6, p = 0.02) and stronger perceived need for urgent care (χ2 = 16.5, p = 0.002). Also, respondents who expected a higher priority than the assigned triage category were significantly more likely to perceive their condition as serious (mean score = 7.1 ± 2.1, p ≤ 0.01), urgent (mean = 7.4 ± 2.2, p ≤ 0.01), and painful (mean = 6.5 ± 2.6, p = <0.01) than the other two categories.
Expected lower priority was significantly associated with frequent ED attendance in the past six months (χ2 = 11.6, p = 0.02) and weaker perceived need for urgent care (χ2 = 16.5, p = 0.002). Also, respondents who expected a lower priority than the assigned triage category were significantly less likely to perceive their condition as serious (mean score = 6.1 ± 1.9, p ≤ 0.01), urgent (mean = 6.0 ± 2.3, p ≤ 0.01), and painful (mean = 5.3 ± 2.6, p ≤ 0.01) than the other two categories.
Multivariate analysis
A multinomial logistic regression analysis was conducted with the variables in Table 3. While these variables were statistically significant in the bivariate analysis, only two variables, Perceived Urgency and Pain Score, reached the final stage (Table 4). Using Nagelkerke test, these two variables explained nearly 12 % of the variance in the dependent variable. However, only Perceived Urgency was significantly associated with expected higher priority (OR: 1.27, 95 % CI: 1.14–1.43).
Table 4.
Results of multivariate analysis
| Factor | Adjusted OR | 95 % (CI) | Adjusted OR | 95 % (CI) |
|---|---|---|---|---|
| Expected higher prioritya | Expected lower prioritya | |||
| Perceived urgency | 1.273 | (1.136–1.426) | 0.999 | (0.880–1.133) |
| Pain score | 1.069 | (0.973–1.174) | 0.923 | (0.828–1.029) |
| Pseudo R2 | Nagelkerke = 0.116 | |||
aThe reference category is: Concordance. OR Odds Ratio, CI Confidence Interval
Discussion
Our study showed little agreement between patient perceived priority and actual nurse assigned triage category. There is a paucity of comparable studies in this area. Studies on inter-rater agreement have pre-dominantly focussed on the validation of the triage scales through the eyes of different health practitioners such as nurses, emergency physicians and general practitioners [26, 29–31].
Our findings are consistent with a recent study of concordance between patients’ and their doctors’ assessment of urgency levels in a Norwegian emergency outpatient clinic [32]. The study showed low agreement between doctors and patients (Kendall tau-b = 0.202, p < 0.001). However, while country of birth was not associated with inter-rater agreement in our study, the Norwegian study showed that doctors were significantly more likely to assess African patients with higher priority [32].
A study of 73 non-urgent self-referrals to an ED in Israel compared the patients’ evaluation of the urgency with the treating nurses’ evaluation [33]. The results found statistically significant differences between the two groups. Whilst over 77 % of the patients rated their condition as “urgent to most urgent”, only 21 % of the nurses rated the patients’ condition as urgent to most urgent [33]. The study, however, did not analyse the inter-rater agreement between the patients and nurses.
Earlier studies have shown similar results. A 1980 study in USA showed that 44.4 % of the patients thought they needed care immediately, 28.5 % urgently, and 15.6 % promptly. However, the emergency physicians’ prospective assessments were 12.6 %, 26.3 % and 28.1 %, respectively [34]. Another similar study in 1996 confirmed the discordance between patients’ and physicians’ assessment of the urgency of the needed care, although with different magnitudes [35]. In this latter study, 31.7 % of the patients thought they should be seen immediately, 33.6 % urgently, and 21.2 % promptly, whereas the physicians’ assessments were 14.8 %, 22.8 % and 28.2 %, respectively.
Notably, although the multivariate analysis (Table 4) did not yield statistical significance for most variables (except for Perceived Urgency), the findings and the directions of the associations can have important implications. Our findings clearly confirmed the discrepancy between patient perception of urgency and staff assessment of urgency. Respondents seemed to expect a higher priority if they had attended the ED more than once in the past six months, possibly indicating the presence of significant co-morbidities or experience with the system. They considered their condition to be serious and required urgent care.
Our findings also indicate the complex and delicate nature of the patient–health practitioner relationship, particularly when the patient’s expectation is not met as a result of allocating a lower triage category. While there are some suggestions that patients should be able to have input into their triage assessment, opponents of this view point to issues such as ethics (fairness, justice and equity), resource limitations, actual ability to meet the patients’ expectations, and the level of knowledge, education and clinical decision making that goes into triage assessment that most patients do not have [13, 18, 36, 37]. Furthermore, involving the patients’ input would require the development and implementation of specific patient education programs, which are hampered by cost and lack of evidence of their success.
Although brief, triage is a complex decision making process, performed by experienced and trained ED registered nurses [26]. It is deigned to sort and prioritise care to reduce the negative impact on the prognosis of a prolonged delay before treatment [38]. The triage process itself requires engagement and two way communication with the patient and, where appropriate, their family. However, improvements in this process may be required so that triage can become more patient centred. Further research is needed to investigate the patient’s perceived urgency at the start and end of their ED episode as their perceptions may change as a result of their ED experience, receiving assurance from clinical experts, and seeing other, perhaps sicker, patients in the department.
Of considerable clinical concern is the subgroup of patients (20 %) who tended to under-rate their priority compared to health practitioner assessments. Our study did not show statistically significant factors that may influence this perception. However, there are significant clinical risks in this group that reinforces the need for professional assessment, active and ongoing management of the triage process and professional observation of those waiting. Further research is required to identify the characteristics of those who tend to over or underrate their urgency, and also to understand if there is a correlation between personality type and expectations of either higher or lower triage scores. The significance of pain assessment as a key determinant of the patient urgency perception is important as there are significant personality and cultural influences on not only the perception of pain but also on the public expression of that perception [39].
One key implication of this research relates to the importance of managing around patient expectations. Given that nearly 1 in 2 patients in our study expected to have been allocated a higher priority than they actually were, opportunity exists for health care practitioners to communicate further with patients regarding the triage process which would provide an opportunity for patients to engage in and understand the clinical decision making around their triage category. This addresses the imbalance between expectation and reality through reassurance, by identifying and addressing the patient’s concern. It also allows for a ‘patient voice’ which may incorporate other contextual issues into the assessment that are causing the patient and their carers concern. An example of this ‘patient voice’ is “Ryan’s Rule”, an initiative recently introduced into Queensland Health which allows patients to escalate demand for extra help if they “are concerned about a patient in hospital who is getting worse or not improving” [40]. Given that the triage process is usually fast and short, allowing time for further patient/carer input can improve the safety and quality of care.
Strengths and limitations
This is one of the first studies to explore in some depth the patient perceptions of their priority and the relationship between that perception and the triage category assigned by triage nurses. It explores the value of the “patient voice” and identifies options for incorporating processes that may better understand and capture those perceptions into the priorities assigned.
The major limitation of this study is its sample size and representativeness. Overall, 697 (43 %) of the 1608 patients attending the EDs did not participate in this study. Since we were unable to access their medical records without their consent, we cannot assess the impact/bias their exclusion from the study might have had on the results. It is possible that there would be a higher concordance between actual triage and patients’ perceptions for those who were seriously ill. Furthermore, only a subgroup of the participants consented for access to their medical records. However, as our analysis showed there were no statistically significant differences between the consented and non-consented participants in major socio-demographic and health related variables. It is also recognised that this study was undertaken in a single state and despite all the efforts to capture a representative sample of the presenting patients, the final sample did not include seriously ill patients for practical reasons. Furthermore, the data collection was conducted in autumn and this may mask seasonal variations in attendances. Further investigations in other locations, times and with different patient groups may be required to enable comparisons and generalisability of the findings.
We asked the respondents to rate their perception of the expected priority before the start of the treatment. However, as some patients had already started their treatment, their retrospective responses may have been affected and biased. Furthermore, our study did not include some other factors that may contribute to differences in patient perceptions such as personality traits, experience, and health literacy. Further research would be of benefit to explore the impact of these and other factors such as geography (e.g. urban vs rural), diagnosis and health system differences (e.g. triage practices in different EDs), particularly for those who tend to overrate or underrate their assessment. This greater understanding may assist with aligning triage process management with patient expectations and thus help achieve improved clinical and organisational satisfaction.
Conclusions
Our findings show a gap in patient–practitioner understanding of the priority of patients attending emergency departments, which can have implications for the management of the emergency care system. While patient centred care is acknowledged as an important part of system development, improved and open communication and the incorporation of the ‘patient voice’ into the triage process require a careful balance between understanding the patient’s perspectives and the objective assessment of a trained health professional who needs to prioritise the allocation of the resources in accordance with the urgency of the presented conditions. Patients’ involvement in the decision making process and particularly in the triage assessment is sensitive, difficult, and the subject of opposing opinions about its fairness. Further work is required on how to manage the expectations by acknowledging the discrepancy between the two parties.
Acknowledgements
We thank the research participants who patiently accepted our invitation and took part in this study. We also thank our team of interviewers and the staff of the eight hospitals who facilitated the data collection. Thanks also go to the members of the Emergency Health Services Queensland (EHSQ) study team and Advisory Group who obtained the funding, and supervised and led the research project.
Funding
This paper is based on a research project on demand for emergency health services in Queensland funded by an Australian Research Council (ARC) Linkage grant (LP0882650) in partnership with Queensland Ambulance Service (QAS).
Availability of data and materials
The data supporting the findings is not available for sharing. The ethics conditions and requirements preclude the use of data by people outside the research team, and using it for purposes other than the specified project. The data will be stored for seven years after the completion of the project. This period is to ensure that all enquiries related to analyses and publications can be checked and responded properly.
Authors’ contributions
GT is responsible for acquisition of data. GT and GF have made substantial contributions to conception and design of the study. GT is responsible for the analysis and interpretation of data and drafting the manuscript. All authors critically reviewed and revised the subsequent drafts of the paper. All authors declare that they have made substantive intellectual contributions to the study and agree to be accountable for all aspects of the work. All authors read and approved the final version of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Consent to publish the aggregated results was obtained as part of the Information Sheet provided to the participants.
Ethics approval and consent to participate
Ethics approvals for the study were provided by Human Research Ethics Committees of Queensland University of Technology (Ref. No. 1000001131), The Prince Charles Hospital (Ref No. HREC/10/QPCH/98), and Mater Hospital (Ref. No. 1621 AC).
Participants were provided with an Information Sheet which also advised that the return of the completed questionnaire was accepted as an indication of their consent to participate (no signed Consent Form required). However, a separately signed Consent Form was required in order to allow the research team to access their medical records for the purposes of this study.
Abbreviations
- 95 % CI
95 % Confidence Interval
- ED
Emergency department
- EDIS
Emergency Department Information System
- GP
General practitioner
- SPSS
Statistical Package for the Social Sciences
Contributor Information
Ghasem-Sam Toloo, Phone: 07-3138 3801, Email: sam.toloo@qut.edu.au.
Peter Aitken, Email: Peter.Aitken2@health.qld.gov.au.
Julia Crilly, Email: Julia.Crilly@health.qld.gov.au.
Gerry FitzGerald, Email: gj.fitzgerald@qut.edu.au.
References
- 1.ACEM: Policy on Patients' Rights to Access Emergency Department Care. Australasian College for Emergency Medicine; 2011. [https://www.acem.org.au/getattachment/04898090-617f-4401-be8e-8067af8ba4e1/Policy-on-Patients-Rights-to-Access-Emergency-Depa.aspx]. Accessed 10 Oct 2016.
- 2.Felland LE, Hurley RE, Kemper NM. Safety net hospital emergency departments: creating safety valves for non-urgent care. Issue Brief. 2008;120:1–4. [PubMed]
- 3.FitzGerald G, Toloo S, Rego J, Ting J, Aitken P, Tippett V. Demand for public hospital emergency department services in Australia: 2000–2001 to 2009–2010. Emerg Med Australas. 2012;24:72–78. doi: 10.1111/j.1742-6723.2011.01492.x. [DOI] [PubMed] [Google Scholar]
- 4.Lowthian JA, Curtis AJ, Cameron PA, Stoelwinder JU, Cooke MW, McNeil JJ. Systematic review of trends in emergency department attendances: an Australian perspective. Emerg Med J. 2010;28:373–377. doi: 10.1136/emj.2010.099226. [DOI] [PubMed] [Google Scholar]
- 5.Bernstein SL. Frequent emergency department visitors: the End of inappropriateness. Ann Emerg Med. 2006;48:18–20. doi: 10.1016/j.annemergmed.2006.03.033. [DOI] [PubMed] [Google Scholar]
- 6.Carret MLV, Fassa AG, Kawachi I. Demand for emergency health service: factors associated with inappropriate use. BMC Health Serv Res. 2007;7:131. doi: 10.1186/1472-6963-7-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Selasawati HG, Naing L, Wan Aasim WA, Winn T, Rusli BN. Factors associated with inappropriate utilisation of Emergency Department Services. Asia Pac J Public Health. 2007;19:29. doi: 10.1177/10105395070190020601. [DOI] [PubMed] [Google Scholar]
- 8.Siminski P, Cragg S, Middleton R, Masso M, Lago L, Green J, Edgar K. Primary care patients views on why they present to the Emergency Departments: Innapropriate attendances or inappropriate policy. Aust J Prim Health. 2005;11:87–95. doi: 10.1071/PY05026. [DOI] [Google Scholar]
- 9.Vardy J, Mansbridge C, Ireland A. Are emergency department staffs’ perceptions about the inappropriate use of ambulances, alcohol intoxication, verbal abuse and violence accurate? Emerg Med J. 2009;26:164–168. doi: 10.1136/emj.2007.056259. [DOI] [PubMed] [Google Scholar]
- 10.FitzGerald G, Toloo GS. General practice patients in the emergency department. Med J Aust. 2013;198:573–574. doi: 10.5694/mja13.10513. [DOI] [PubMed] [Google Scholar]
- 11.Nagree Y, Camarda VJ, Fatovich DM, Cameron PA, Dey I, Gosbell AD, McCarthy SM, Mountain D. Quantifying the proportion of general practice and low-acuity patients in the emergency department. Med J Aust. 2013;198:612–615. doi: 10.5694/mja12.11754. [DOI] [PubMed] [Google Scholar]
- 12.ACEM: Quality Standards for EMERGENCY DEPARTMENTS and other HOSPITAL-BASED EMERGENCY CARE SERVICES. The Australasian College for Emergency Medicine (ACEM); 2015. [https://acem.org.au/Structured-Documents/Quality-Standards.aspx]. Accessed 10 Oct 2016.
- 13.Salisbury C, Coulter A. Urgent care and the patient. Emerg Med J. 2010;27:181–182. doi: 10.1136/emj.2009.073064. [DOI] [PubMed] [Google Scholar]
- 14.ACEM: Policy on the Australasian Triage Scale (v04). Australasian College for Emergency Medicine; 2013. [https://www.acem.org.au/getattachment/693998d7-94be-4ca7-a0e7-3d74cc9b733f/Policy-on-the-Australasian-Triage-Scale.aspx]. Accessed 10 Oct 2016.
- 15.Ng CWL, Lim GH, McMaster F, Molina J, Seow E, Heng BH. Patient satisfaction in an observation unit: the Consumer Assessment of Health Providers and Systems Hospital Survey. Emerg Med J. 2009;26:586–589. doi: 10.1136/emj.2008.063297. [DOI] [PubMed] [Google Scholar]
- 16.Liaw S, Hill T, Bryce H, Adams G. Emergency and primary care at a Melbourne hospital: reasons for attendance and satisfaction. Aust Health Rev. 2001;24:120–134. doi: 10.1071/AH010120a. [DOI] [PubMed] [Google Scholar]
- 17.Jeanmonod R, Boyd M, Loewenthal M, et al. The nature of emergency department interruptions and their impact on patient satisfaction. Emerg Med J. 2010;27:376–379. doi: 10.1136/emj.2008.071134. [DOI] [PubMed] [Google Scholar]
- 18.Meek R, Phiri W. Australasian Triage Scale: Consumer perspective. Emerg Med Australas. 2005;17:212–217. doi: 10.1111/j.1742-6723.2005.00725.x. [DOI] [PubMed] [Google Scholar]
- 19.Agarwal S, Banerjee J, Baker R, Conroy S, Hsu R, Rashid A, Camosso-Stefinovic J, Sinfield P, Habiba M. Potentially avoidable emergency department attendance: interview study of patients’ reasons for attendance. Emerg Med J 2011. doi:10.1136/emermed-2011-200585 [DOI] [PubMed]
- 20.FitzGerald G, Toloo S, Rego J: Shaping the future demand for ambulance: understanding patient’s reasons and decision making [oral presentation]. In Book Shaping the future demand for ambulance: understanding patient’s reasons and decision making [oral presentation] (Editor ed.^eds.). City; 2012.
- 21.Guttman N, Zimmerman DR, Nelson MS. The many faces of access: reasons for medically nonurgent emergency department visits. J Health Polit Policy Law. 2003;28:1089–1120. doi: 10.1215/03616878-28-6-1089. [DOI] [PubMed] [Google Scholar]
- 22.Masso M, Bezzina AJ, Siminski P, Middleton R, Eagar K. Why patients attend emergency departments for conditions potentially appropriate for primary care: Reasons given by patients and clinicians differ. Emerg Med Australas. 2007;19:333–340. doi: 10.1111/j.1742-6723.2007.00968.x. [DOI] [PubMed] [Google Scholar]
- 23.Toloo S, Rego J, FitzGerald G, Vallmuur K, Ting J. Emergency Health Services: Demand and Service Delivery Models. Monograph 3: Patients' Reasons and Perceptions. Brisbane: Queensland University of Technology; 2013. [http://eprints.qut.edu.au/65395/].
- 24.Gerdtz MF, Collins M, Chu M, Grant A, Tchernomoroff R, Pollard C, Harris J, Wassertheil J. Optimizing triage consistency in Australian emergency departments: The Emergency Triage Education Kit. Emerg Med Australas. 2008;20:250–259. doi: 10.1111/j.1742-6723.2008.01089.x. [DOI] [PubMed] [Google Scholar]
- 25.López L, Wilper AP, Cervantes MC, Betancourt JR, Green AR. Racial and Sex differences in emergency department triage assessment and test ordering for chest pain, 1997–2006. Acad Emerg Med. 2010;17:801–808. doi: 10.1111/j.1553-2712.2010.00823.x. [DOI] [PubMed] [Google Scholar]
- 26.Goransson K, Ehrenberg A, Marklund B, Ehnfors M. Accuracy and concordance of nurses in emergency department triage. Scand J Caring Sci. 2005;19:432–438. doi: 10.1111/j.1471-6712.2005.00372.x. [DOI] [PubMed] [Google Scholar]
- 27.Toloo GS, FitzGerald GJ, Aitken PJ, Ting JY, McKenzie K, Rego J, Enraght-Moony E. Ambulance use is associated with higher self-rated illness seriousness: user attitudes and perceptions. Acad Emerg Med. 2013;20:576–583. doi: 10.1111/acem.12149. [DOI] [PubMed] [Google Scholar]
- 28.Rego J, FitzGerald G, Toloo S, Vallmuur K. Why do Queenslanders seek care in emergency departments? A population study. Emerg Med Australas. 2015;27:516–521. doi: 10.1111/1742-6723.12474. [DOI] [PubMed] [Google Scholar]
- 29.Esmailian M, Zamani M, Azadi F, Ghasemi F. Inter-rater agreement of emergency nurses and physicians in Emergency Severity Index (ESI) Triage. Emerg. 2014;2:158–161. [PMC free article] [PubMed] [Google Scholar]
- 30.Vance J, Sprivulis P. Triage nurses validly and reliably estimate emergency department patient complexity. Emerg Med Australas. 2005;17:382–386. doi: 10.1111/j.1742-6723.2005.00761.x. [DOI] [PubMed] [Google Scholar]
- 31.Creaton A, Liew D, Knott J, Wright M. Interrater reliability of the Australasian Triage Scale for mental health patients. Emerg Med Australas. 2008;20:468–474. doi: 10.1111/j.1742-6723.2008.01131.x. [DOI] [PubMed] [Google Scholar]
- 32.Ruud SE, Hjortdahl P, Natvig B. Is it a matter of urgency? A survey of assessments by walk-in patients and doctors of the urgency level of their encounters at a general emergency outpatient clinic in Oslo Norway. BMC Emerg Med. 2016;16:22. doi: 10.1186/s12873-016-0086-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rassin M, Nasie A, Bechor Y, Weiss G, Silner D. The characteristics of self-referrals to ER for non-urgent conditions and comparison of urgency evaluation between patients and nurses. Accid Emerg Nurs. 2006;14:20–26. doi: 10.1016/j.aaen.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 34.Gifford MJ, Franaszek JB, Gibson G. Emergency physicians’ and patients’ assessments: Urgency of need for medical care. Ann Emerg Med. 1980;9:502–507. doi: 10.1016/S0196-0644(80)80187-9. [DOI] [PubMed] [Google Scholar]
- 35.Hunt RC, DeHart KL, Allison EJ, Whitley TW. Patient and physician perception of need for emergency medical care: A prospective and retrospective analysis. Am J Emerg Med. 1996;14:635–639. doi: 10.1016/S0735-6757(96)90077-7. [DOI] [PubMed] [Google Scholar]
- 36.Salisbury C, Bell D. Access to urgent health care. Emerg Med J. 2010;27:186–188. doi: 10.1136/emj.2009.073056. [DOI] [PubMed] [Google Scholar]
- 37.Salisbury C, Trivella M, Bruster S. Demand for and supply of out of hours care from general practitioners in England and Scotland: Observational study based on routinely collected data. Br Med J. 2000;320:618. doi: 10.1136/bmj.320.7235.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Farrohknia N, Castrén M, Ehrenberg A, Lind L, Oredsson S, Jonsson H, Asplund K, Göransson KE. Emergency department triage scales and their components: a systematic review of the scientific evidence. Scand J Trauma Resusc Emerg Med. 2011;19:42. doi: 10.1186/1757-7241-19-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liao KY-H, Henceroth M, Lu Q, LeRoy A. Cultural differences in pain experience among four ethnic groups: a qualitative pilot study. J Behav Health. 2016;5:75–81. [Google Scholar]
- 40.Queensland Health: Ryan's Rule [https://www.health.qld.gov.au/metronorth/patients-visitors/rights/ryans-rule/default.asp]. Accessed 10 Oct 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the findings is not available for sharing. The ethics conditions and requirements preclude the use of data by people outside the research team, and using it for purposes other than the specified project. The data will be stored for seven years after the completion of the project. This period is to ensure that all enquiries related to analyses and publications can be checked and responded properly.


