Abstract
OBJECTIVE:
The objective of this study is to evaluate if gonadotropin-releasing hormone agonist (GnRHa) trigger is a better alternative to human chorionic gonadotropin (hCG) in polycystic ovary syndrome (PCOS) of Indian origin undergoing in vitro fertilization (IVF) cycles with GnRH antagonist for the prevention of ovarian hyperstimulation syndrome (OHSS).
DESIGN:
Prospective randomized control trial.
SETTING:
Tertiary care center.
MATERIALS AND METHODS:
A total of 227 patients diagnosed with PCOS, undergoing IVF in an antagonist protocol were recruited and randomly assigned into two groups: Group A (study group): GnRHa trigger 0.2 mg (n = 92) and Group B (control group): 250 μg of recombinant hCG as trigger (n = 101) 35 h before oocyte retrieval. We chose segmentation strategy, freezing all embryos in both the groups.
STATISTICAL ANALYSIS:
Continuous variables were expressed as mean ± standard deviation independent sample t-test and Kolmogorov-Smirnov test were used for continuous variables which were normally distributed and Mann-Whitney U-test for data not normally distributed.
MAIN OUTCOME MEASURES:
Primary outcome: OHSS (mild, moderate, and severe) rates. Secondary outcomes: Maturity rate of the oocytes, fertilization rate, availability of top quality embryos on day 3 (Grade 1 and Grade 2).
RESULTS
The incidence of moderate to severe OHSS in the hCG group was 37.6% and 0% in the GnRHa group with P < 0.001. The GnRHa group had significantly more mature oocytes retrieved (19.1 ± 11.7 vs. 14.1 ± 4.3), more fertilized oocytes (15.6 ± 5.6 vs. 11.7 ± 3.6), and a higher number of top quality cleavage embryos on day 3 (12.9 ± 4.7 vs. 7.5 ± 4.3) than the hCG group.
CONCLUSIONS:
The most effective strategy which significantly eliminates the occurrence of OHSS in PCOS following ovarian stimulation in antagonist IVF cycles is the use of GnRHa trigger yielding more mature oocytes and good quality embryos when compared with hCG trigger.
KEY WORDS: Antagonist, gonadotropin-releasing hormone agonist trigger, human chorionic gonadotropin trigger, ovarian hyperstimulation syndrome, polycystic ovary syndrome
INTRODUCTION
With a steady increase in the number of assisted reproductive technology cycles over the years, there has been an increase in the incidence of ovarian hyperstimulation syndrome (OHSS), posing an important medical problem for the clinicians.[1] Most of them are mild accounting for about 20%-33%[2,3] with no adverse consequences to the patient. However, when OHSS is severe, it is associated with morbidity, the consequences may be lethal[4] and fatalities have also been reported.[5] In in vitro fertilization (IVF) cycles following ovarian stimulation, the reported incidence of moderate to severe OHSS is 3%–8%, which increases to 10%–20% in a high-risk population of polycystic ovary syndrome (PCOS).[6,7]
Exogenous human chorionic gonadotropin (hCG), surrogate for the endogenous mid-cycle surge of luteinizing hormone (LH) has been the gold standard trigger for final oocyte maturation in all IVF cycles. Due to its increased half-life when compared with LH and prolonged stimulatory effect on multiple corpora lutea is responsible for the entire cascade of OHSS through the vascular endothelial growth factor (VEGF) pathway mainly.[8,9] It has been proposed that the administration of a gonadotropin-releasing hormone agonist (GnRHa) instead of hCG, to induce the final oocyte maturation which is feasible in a GnRH-antagonist protocol[10] significantly reduces or eliminates the risk of OHSS.[11,12,13,14,15,16]
There have been concerns regarding the effectiveness of GnRHa to induce optimal oocyte yield and mature oocytes[12] which may lead to the reluctance of its routine use in PCOS for the prevention of OHSS. Like all other clinicians, we were also reluctant to use GnRHa in place of hCG as trigger in PCOS patients undergoing IVF cycles. The present study addresses if GnRHa trigger is a better alternative to hCG in all PCOS of Indian origin in terms of OHSS prevention, maturity of the oocytes, fertilization, and embryo quality.
MATERIALS AND METHODS
Study design and participants
This prospective randomized study was conducted in a university-affiliated tertiary care center. A total of 227 patients diagnosed with PCOS, undergoing IVF in an antagonist protocol between May 2013 and November 2015 was recruited for the study. Approval for the study was obtained from the Institutional Review Board and Ethics Committee. All participants before allocation signed an informed written consent form after counseling about alternative options of OHSS prevention (cycle cancelation). The study followed the Consolidated Standards of Reporting Trials guidelines for reporting of randomized controlled trials (RCTs).
Sample size
The overall incidence of OHSS in high-risk groups undergoing IVF has been reported as 32%[1,4] and based on earlier publications,[11,12,13,14] we hypothesized that GnRHa trigger should lead to an 80% relative decline in the incidence of OHSS. Based on a two-sided significance level of 0.05 and 95% power, it was anticipated that with a fallout rate of about 10%, at least 88 patients would need to be recruited over an 18–24 month period.
Patient population
Inclusion criteria were: (i) All PCOS defined as per the ESHRE/ASRM Rotterdam criteria (2003) demonstrating two of the three criteria: (a) Oligo or anovulation, (b) clinical and/or biochemical signs of hyperandrogenism, (c) polycystic ovaries (as defined on ultrasonography): 12 or more follicles measuring 2–9 mm in diameter or increased ovarian volume (>10 cc) were recruited for the study, (ii) age 20–37 years, (iii) normal early follicular phase serum follicle stimulating hormone (FSH) concentration (<10.0 IU/L), (iv) body mass index (BMI) >18 and <30 kg/m2, (v) presence of both ovaries, (vi) indication for IVF/intracytoplasmic sperm injection (ICSI), (vii) stimulation in a GnRH antagonist protocol, (viii) willingness to participate in the study.
Exclusion criteria were: (i) Age >37 years, (ii) donor cycles using GnRHa trigger, (iii) patients with hypogonadotropic hypogonadism, (iv) surgical retrieval of sperms. Patients were recruited for the trial for only one cycle.
Randomization
Eligible PCOS women were recruited and randomly assigned into the two groups (Groups A and B) in a ratio of 1:1 by means of computer-generated sequence using sealed opaque envelopes. Selection into the groups and randomization into the appropriate treatment protocol was performed by a study coordinator, and the sequence of allocation was concealed. The study was not blinded because the patients, as well as the clinicians, were aware of the treatment group.
Ovarian stimulation, patient monitoring, and cryopreservation
All subjects were pretreated with oral contraceptive pills in the previous cycle. Before starting stimulation, day 2 FSH, LH, estradiol (E2), progesterone (P4), anti-mullerian hormone (AMH), and a baseline transvaginal scan was performed in all the patients. Controlled ovarian stimulation was started on day 2/3 of cycle with recombinant FSH, (Recagon, Organon). The starting dosage was individualized taking into consideration the patient's age, BMI, antral follicle count (AFC), AMH, and previous ovarian response to stimulation and ranged from 112.5 to 175 IU daily for 4 days. Thereafter, the dose was adjusted on the basis of ovarian response and serum E2. Flexible multiple dose protocol was followed wherein GnRH antagonist, Ganirelix (Orgalutran, Organon) 0.25 mg/day subcutaneous (s.c) was started when the leading follicle was >14 mm and/or serum E2 concentration was >300 pg/mL. Both gonadotropin and antagonist were continued till the day of ovulation trigger. Monitoring of follicular growth was achieved with serial ultrasound and serum E2 measurements and the dose of gonadotropins adjusted accordingly if necessary. GnRHa was administered at least 12 h after the last dose of GnRH antagonist. On the day of trigger, serum E2, LH, and P4 concentrations were measured. When three leading follicles achieved 17 mm diameter, final oocyte maturation was triggered with a single dose of 0.2 mg of Triptorelin (Decapeptyl, Ferring), s.c in Group A and with recombinant hCG (rhCG), (Ovitrelle, Serono) 250 mcg s.c in Group B. Transvaginal ultrasound-guided oocyte retrieval was performed 35 h post-trigger under intravenous sedation with single lumen oocyte retrieval needle progesterone. Coasting was not done in any cycle. Oral medroxy acetate, 10 mg twice daily for a week was administered starting on the day of oocyte pick-up to avoid spotting and breakthrough bleeding.
Intra cytoplasmic sperm injection (ICSI) was performed in all cases as per the standard operating procedure of the hospital. Fertilization was assessed 18 h following ICSI by the appearance of two pronuclei. Cleavage stage embryos were graded as per the Istanbul consensus: Grade 1 (good): <10% fragmentation, stage-specific cell size and no multinucleation. Grade 2 (fair): 10%-25% fragmentation, stage-specific cell size for majority of cells and no evidence of multinucleation. Grade 3 (poor): Severe fragmentation (>25%), cell-size not stage-specific and evidence of multinucleation. Embryos were vitrified by open system using cyrolock with 15% ethylene glycol, 15% dimethylsulfoxide, and 0.5 mol/L sucrose as cryoprotectants (Sage Vitrification Kit, Origio). Grade 1 and 2 embryos were taken as top quality embryos which were frozen and all others being discarded.
Safety and tolerability assessment
The diagnosis of OHSS was based on the criteria by Navot et al.[8] An assessment for signs and symptoms of OHSS was performed on day 4 and 7 following oocyte retrieval which included a history and physical examination by a clinician. In case of symptoms such as abdominal distension/pain, nausea, vomiting, diarrhea, or any difficulty in breathing, patients were advised to present themselves at any point of time within 2 weeks of trigger administration. Based on the clinical symptoms, transvaginal sonography to assess the ovarian size, free fluid in pouch of Douglas, paracolic gutters, Morrison's pouch, pleura, and a blood sample for E2 and to detect hemoconcentration defined as a hematocrit of 45%[8] was performed.
Immunoassay of hormones
Serum concentrations of FSH, LH, E2, and P4 were assayed using an automated electrochemiluminescent immunoassay system (e411 Roche Cobas). Assay sensitivity for FSH was 0.1 mIU/mL and for LH was 0.1 mIU/mL. Linearity for FSH and LH was 200 mIU/mL. The minimum detection limit of E2 was 5.0 pg/mL and linearity up to 4300.0 pg/mL. The intra-(CVw) and inter-assay (CVb) coefficients of variation (CV) were 1.8% and 1.8%, 5.3%, and 5.1% at a mean value of 1.2 and 103 mIU/mL, respectively for FSH. Similarly, CV's for LH were 1.2% and 0.9%, 2.0%, and 2.2% at concentrations of 5.81 and 159 mIU/mL. The CV's for E2 was 5.7% and 1.9%, 6.2%, and 2.8% for concentrations of 34.8 pg/mL and 1018 pg/mL, respectively. AMH was measured using generation 2 ELISA kit (Beckman Coulter, sensitivity: 0.08 ng/mL, linearity: 0.16–22.5 ng/mL) having CVw of 5.4% and 3.6% and CVb of 5.6% and 4.5% at concentrations of 4.42 ng/mL and 14.03 ng/mL, respectively.
Outcome measures
Primary outcome
OHSS (mild, moderate, and severe) rates.
Secondary outcomes
Maturity rate of the oocytes, fertilization rate, availability of top quality embryos on day 3 (Grade 1 and Grade 2). Oocyte maturity was defined as the ratio of metaphase II (MII) oocytes to the total number of oocytes collected. Fertilization rate was defined as the ratio of normal fertilized oocytes (two pronuclei) to the number of MII oocytes.
Statistical analysis
Data were analyzed using Statistical Package for Social Sciences version 16.0 (SPSS Inc., USA). Continuous variables were expressed as mean ± standard deviation and Chi-squared test for categorical variables where appropriate. Independent sample t-test and Kolmogorov-Smirnov test were used for continuous variables which were normally distributed and Mann-Whitney U-test for data not normally distributed. P < 0.05 was considered statistically significant.
RESULTS
Participant flow
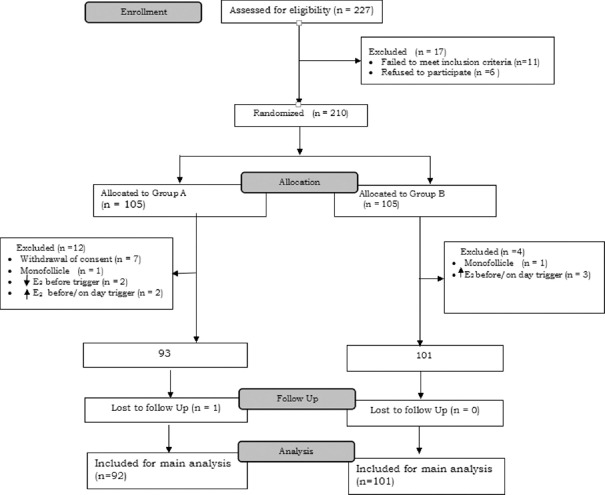
The participant flow is shown in Figure 1. Of the 227 PCOS patients screened for the study at our center, 210 were stimulated for IVF cycle. During stimulation before trigger, cycles were canceled in nine patients (Group A [n = 5]; Group B [n = 4]). In two patients, IVF cycle was converted into intrauterine insemination due to monofollicular growth and in Group A, two patients had a significant drop in E2 levels and hence cycles were canceled. Patients with high E2 levels >6000 ng/mL were excluded from analysis as additional measures (step-down protocol, cabergoline, intravenous [IV] albumin) was undertaken. Thus, 92 PCOS in Group A and 101 in Group B were included in the main analysis.
Figure 1.
CONSORT flowchart of the trial
Baseline and stimulation cycle characteristics
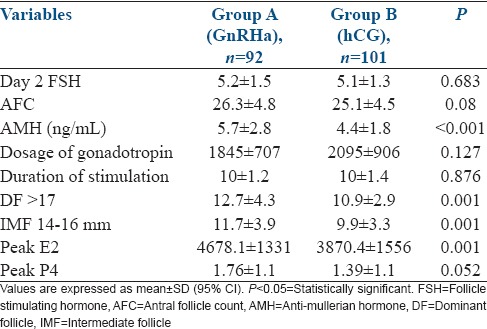
The age, BMI, causes, duration of infertility, parity, and seminal parameters were similar in both groups [Table 1]. There were no significant differences with respect to AFC, duration of stimulation and the total dosage of gonadotropins. The AMH, number of dominant follicles (DFs) >17 mm, the number of intermediate follicles (IMFs) between 14 and 16 mm and peak E2 levels on the day of trigger was found to higher in the study group as compared to the control group [Table 2].
Table 1.
Baseline characteristics
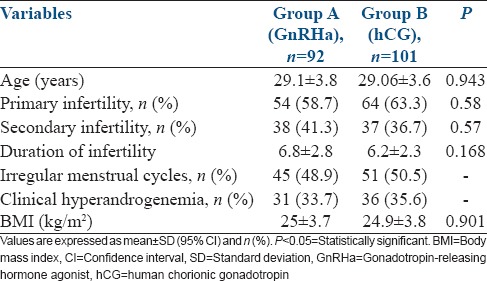
Table 2.
Stimulation cycle characteristics
Outcomes
Primary outcome
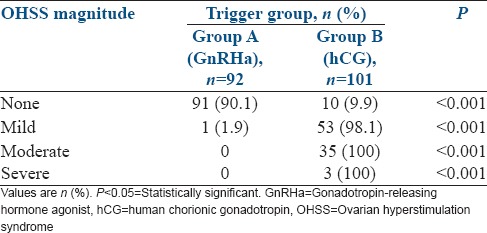
Mild form of OHSS was seen in about 54 patients, of which 53 (98.1%) was in the hCG group and only 1 patient (1.8%) was in the GnRHa group. The incidence of moderate to severe OHSS in the hCG group was 37.6% and 0% in the GnRHa group with P < 0.001 [Table 3].
Table 3.
Primary outcome
Secondary outcomes
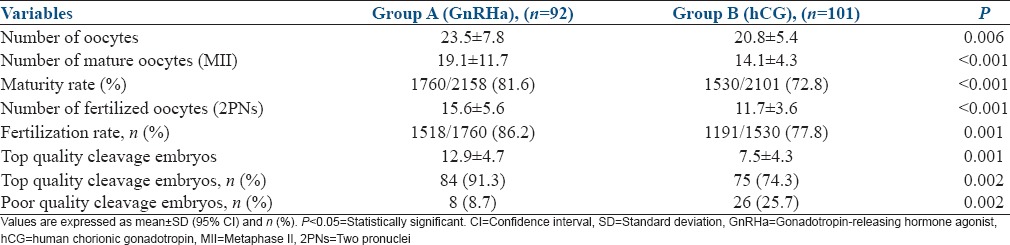
The GnRHa group had significantly more mature oocytes retrieved (19.1 ± 11.7 vs. 14.1 ± 4.3), more normally fertilized oocytes (15.6 ± 5.6 vs. 11.7 ± 3.6) and a higher number of top quality cleavage embryos on day 3 (12.9 ± 4.7 vs. 7.5 ± 4.3) than the hCG group [Table 4].
Table 4.
Secondary outcomes
DISCUSSION
Ovarian hyperstimulation syndrome is encountered in clinical practice as an iatrogenic complication by an exaggerated response of ovarian stimulation in the aim to produce multiple follicles so as to increase the number of oocytes available.[1,17] Severe OHSS is a potentially life-threatening, grave complication and occurs in about 2%-6% of IVF cycles resulting in hospitalization in about 1.9% of cases.[18] It is associated with massive ovarian enlargement, shift of protein-rich fluid from the intravascular space to the third space (abdominal, thoracic cavity), liver dysfunction, electrolyte imbalance resulting in significant morbidity and rarely, mortality due to thromboembolic disease, adult respiratory distress syndrome, and hepatorenal failure.[1,4]
The main culprit triggering the syndrome is the presence of hCG[19] either exogenous or endogenous. Exogenous hCG administration results in early OHSS, an acute event usually occurring within 9 days after oocyte retrieval.[19,20] Late OHSS occurs after the initial 10-day period and is due to the endogenous hCG produced by an implanting embryo[4,20] or the administration of hCG for luteal phase support. hCG increases the ovarian vascular permeability and is responsible for activating the VEGF pathway resulting in OHSS. Prostaglandins, inhibin, renin-angiotensin-aldosterone system, insulin-like growth factor 1, interleukin-6, and other inflammatory mediators have all been implicated in the etiology of OHSS.[21] However, VEGF has been identified as the major mediator.[22] In addition, hCG has been shown to increase VEGF expression in the human granulosa cells, which in turn raises serum VEGF concentration thereby increasing the severity of OHSS.[21,22]
Exogenous hCG has been used to induce final follicular maturation in all IVF cycles as both hCG and LH bind to and activate the same receptor, LH receptor (LHR) which promotes follicular maturation, luteinization, and ovulation.[23] However, the hCG molecule has a high biological activity, which is about 6–7 times higher than the endogenous LH with a half-life exceeding 24 h, while, the half-life of LH is 60 min. hCG has a greater affinity to LHR as compared to LH, and thus exerts a more prolonged luteotrophic action for 8–9 days, multiple corpus luteum development and raised serum levels of E2 and P4 throughout the luteal phase,[3] all of which increase the risk of developing OHSS.[6] This risk is similar for both urinary derived and rhCG.[24]
Various strategies have been used for preventing or decreasing the risks of OHSS: (1) Individualized controlled stimulation: Stimulation protocol is personalized after an assessment of primary risk factors.[25,26] (2) Choosing the right protocol: (a) Reducing the exposure to gonadotropins by “mild stimulation” protocols, where the administration of FSH is delayed until the mid to late follicular phase.[1] (b) Use of chronic low-dose protocol in PCOS.[27] (c) Use of GnRH antagonist protocols: Cochrane review showed that the incidence of severe OHSS was significantly lower in an antagonist protocol than in an agonist protocol (relative risk, 0.61; 95% confidence interval [CI], 0.42–0.89; P = 0.01).[28] One of the advantages of GnRH antagonist protocol in high-risk patients is the potential use of GnRHa trigger. (3) Reduced dose of hCG trigger: As compared with the standard dose of 10,000 IU of hCG for trigger, doses of 5000 IU have been used without impairing the clinical outcome,[29] but questions do remain over its ability to reduce the risk of OHSS.[30] (4) Use of alternative agents as trigger – (a) GnRHa: In gonadotropin only or antagonist-stimulated cycles. (b) Recombinant LH: Mimics the natural LH surge and with a half-life of 10 h, a shorter and/or lower LH peak, it is expected that there should be a minimal risk of causing OHSS.[31] A poor cost/benefit ratio and decreased pregnancy rates reduces its applicability in the clinical situation.[1] (5) Use of insulin-sensitizing agents: A Cochrane review by Tso et al. showed that the use of metformin 3 months before IVF lowers the risk of OHSS by 63%.[32] (6) Coasting: Coasting does not eliminate OHSS and may result in compromised cycle outcomes in terms of lower oocyte yield, decreased implantation and pregnancy rates, especially in cases of prolonged coasting.[33,34] DiLuigi et al. demonstrated that GnRHa prevents the development of OHSS in high-risk patients leading to improved clinical outcomes when compared to coasting.[35] (7) Cryopreservation of all embryos: Although early OHSS associated with hCG administration may still occur.[36] (8) Avoidance of hCG for luteal phase support in patients prone for OHSS.[1] Cochrane review showed that hCG potentiated the risk of OHSS with no effect on the clinical pregnancy and live birth rate.[37] (9) In vitro maturation (IVM): IVM is not widely used due to a reduced live birth rate in comparison with the standard IVF.[1] (10) Cycle cancellation: Cycle cancellation and withholding hCG is the only guaranteed method for the prevention of early OHSS.[38] However, in many cases, this will be the last resort for clinicians considering the financial impact and psychological distress that it causes to the patients. (11) Other possible strategies for preventing OHSS: (a) GnRH antagonist salvage: A decrease or plateau in serum E2 levels within 24–48 h after the initial administration of GnRH antagonist in IVF cycles may interrupt the development or progression of the condition while salvaging the current cycle.[1] (b) IV albumin and hydroxyethyl starch (HES): Binds to the vasoactive agents responsible for the development of OHSS and facilitate their removal from the circulation. HES is preferable over albumin as it is nonbiological and there was a statistically significant decrease in severe OHSS with HES use without any effect on pregnancy rates (Cochrane review by Youssef et al.)[39] The routine use of them to prevent OHSS cannot be recommended and requires more compelling evidence. (c) Dopamine agonists: Cabergoline acts at the VEGF receptor and thereby prevents VEGF-mediated vascular permeability through its antiangiogenic properties. Tang et al. in their Cochrane review[40] and Leitao et al.[41] in their systemic review[41] found cabergoline to be effective in preventing the occurrence of moderate and severe OHSS without any negative impact on the oocytes retrieved or clinical pregnancy. (d) Vasopressin-induced VEGF secretion blockade: A novel therapy, vasopressin V1a receptor antagonist, relcovaptan inhibits VEGF by modulating vasoconstriction and vascular smooth muscle proliferation, though further research in this area is required.[42] (e) Glucocorticoids: Inhibits both VEGF gene expression in the vascular smooth muscle cells and vasodilatation, though this does not eliminate the risk of OHSS and the nonspecificity of action may result in undesirable side effects.[43]
Of the various strategies enumerated above for the prevention of OHSS, the most effective strategy to date is the use of GnRHa as trigger in antagonist cycles, which virtually eliminates its occurrence as proven in various studies.[1,11,12,13,14,15,16] Itskovitz et al. in 1988,[44] first introduced the concept that GnRHa trigger eliminates OHSS in high-risk patients, 10 years even before the GnRH antagonist era. With GnRH antagonists becoming more clinically in usage, GnRHa have gained much interest and has become possible to trigger final oocyte maturation and ovulation as an alternative to hCG.[12,45] The GnRHa displaces the antagonist from its receptor, activating the receptor, which causes a flare-up effect, inducing gonadotropin release. The GnRHa-induced surge, although effectively stimulates ovulation and oocyte maturation, there exist differences in regards to its duration and profile when compared to that of the natural cycle LH surge.[12,45] The GnRHa-induced LH surge consists of two phases: A short ascending limb (~4 h) and a long descending limb (~20 h), with a total duration of 24–36 h.[12] While, the LH surge of the natural cycle is characterized by three phases: A rapidly ascending phase of 14 h, a plateau phase lasting for 14 h, and a descending phase of 20 h, in total of 48 h.[12] Thus, the total amount of gonadotropins released with GnRHa trigger is significantly reduced when compared to natural cycle. The shorter duration of the endogenous LH surge induced by GnRHa trigger and the rapid demise of the corpora lutea by withdrawal of LH support reduces the risk of OHSS.[12,15,16,45] VEGF proves to be significantly lower in patients receiving GnRHa instead of hCG, both at the messenger RNA and protein level.[12]
We chose segmentation strategy,[46] freezing all embryos in both groups, followed by frozen-thawed embryo transfer in the subsequent cycle for these reasons. (1) Deferring fresh embryo transfer to prevent early onset OHSS. (2) To avoid the possibility of occurrence of late-onset OHSS in case of pregnancy by early embryonic hCG. Late-onset forms tend to be more often severe and of longer duration.[4] (3) Concerns of luteal phase deficiency following GnRHa trigger with fresh embryo transfers significantly lowering the implantation and ongoing pregnancy rates.[2,10,11] The optimal type of luteal phase support with a fresh transfer is still subjected to research and has not reached its final form.[47] (4) The advent of vitrification has enabled us in obtaining a high survival of embryos after warming with significantly higher ongoing pregnancy rates,[48] better obstetric and perinatal outcomes.[49] (5) To avoid embryo exposure to extremely high steroid levels. It has been shown that a high ovarian response to ovarian stimulation and the accompanying supraphysiologic steroid levels impairs the endometrial receptivity, as well as being embryo-toxic.[50]
In this study, although the number of DFs, IMFs, and peak E2 on the day of trigger (12.74 ± 4.3 vs. 10.91 ± 2.9), (11.7 ± 3.9 vs. 9.9 ± 3.3), and (4878.1 ± 2531 vs. 3870.4 ± 1556), respectively was all higher in the study group as compared with the hCG group [Table 2], yet none developed moderate or severe OHSS (0% in GnRHa group vs. 37.6% in hCG group) [Table 3]. In concordance, two randomized studies in patients at risk of OHSS by Babayof et al.[51] and Engmann et al.[13] reported an incidence of 31% OHSS in the hCG group versus 0% in the GnRHa trigger group. Similar results were obtained by Griesinger et al.[52] and Manzanares et al.[53] in PCOS and high responders with an incidence of 0% OHSS in the GnRHa group. Cochrane review showed that the GnRHa was associated with lower risk of OHSS (mild, moderate, or severe) than hCG (eight RCTs, odds ratio [OR]: 0.15, 95% CI: 0.05–0.47) in fresh autologous cycles.[47] In a recent systematic review and meta-analysis by Youssef et al. 2015,[54] GnRHa seem to be safer than traditional hCG due to the associated low risk of OHSS in fresh autologous cycles (ten RCTs, OR: 0.06, 95% CI: 0.02–0.19).[54] However, majority of studies evaluated the role of GnRHa in normoresponders with normal to low risk of developing OHSS. The role of agonist trigger in terms of OHSS incidence was further elucidated used the donor-recipient model in randomized clinical trials and none of the patients developed OHSS whereas the OHSS incidence after hCG triggering was between 4% and 17%.[55,56] Cochrane review also confirmed a lower incidence of OHSS in the donors triggered with GnRHa group than in the hCG group (three RCTs, OR: 0.05, 95% CI: 0.01–0.28).[47]
In addition, the use of GnRHa trigger has resulted in higher patient convenience during the luteal phase, with less abdominal distension and discomfort as reported by Hernández et al.[57] and Cerrillo et al.[58] The patients in this study who were followed up on day 4 and 7 following oocyte retrieval were totally asymptomatic and almost none had nausea, vomiting, abdominal distension/pain in the GnRHa group. Only one patient in the GnRHa group manifested with nausea and mild abdominal discomfort on the 3rd day postoocyte retrieval and settled with symptomatic treatment. On the contrary, in the hCG group, 35 patients had moderate OHSS, 13 of whom required hospitalization for 3–5 days and 3 patients (2.9%) had severe OHSS requiring intensive care in the hospital for 5–7 days.
With GnRHa trigger and fresh embryo transfer, the addition of hCG with standard luteal phase support to improve implantation and clinical pregnancy results in an increased risk of OHSS.[59] A high incidence of early-onset OHSS (22%) after GnRHa trigger was reported in a retrospective study in a population of high-responder patients who received a low-dose hCG rescue protocol. Here, the investigators proceeded with modified luteal phase protocol instead of a freeze-all policy, despite retrieval of as many as 50–65 oocytes in some patients.[59] In a similar study by Datta et al.[60] an incidence of mild-to-moderate OHSS of 16.2% with GnRHa trigger and 31.0% with hCG trigger in high responders with the addition of a single hCG dose of 1500 IU in the luteal phase was reported. However, this again was a retrospective study with a small sample size (GnRHa [n = 62]; hCG [n = 29]). On the contrary, an RCT in a high-risk population consisting of patients with a follicle count between 15 and 25 did not show any OHSS (0% in GnRHa vs. 2% in hCG), despite the use of the aforementioned low-dose hCG 1500 IU rescue in the luteal phase.[2,45] Thus, the need to set an upper cutoff limit of follicles for the use of hCG in luteal support in fresh transfer and freeze all policy after GnRHa trigger have been commented by Humaidan et al.[2] In the literature, two cases of severe OHSS after GnRHa trigger in GnRH antagonist protocol without the administration of any hCG for luteal phase support possibly due to GnRH receptor, FSH receptor, or LHR gene mutations has been reported.[61]
A possible advantage of the GnRHa-induced surge over the hCG-induced surge is the simultaneous induction of a surge of FSH resembling that of a natural cycle. Although the exact role of this mid-cycle FSH surge has not been clear, it has been shown that it promotes nuclear maturation with the resumption of meiosis.[12] This might explain the retrieval of more metaphase oocytes after GnRHa trigger compared with hCG trigger.[11,12,44,45] The retrieval of more mature oocytes in the GnRHa triggered group in this study when compared to the hCG group [Table 4] supports the previous clinical findings of a possible beneficial effect of the mid-cycle FSH surgeon oocyte maturity.
There has been no difference in the fertilization rates and embryo quality scores when GnRHa is used as trigger instead of hCG.[13,52,57] A meta-analysis by Griesinger et al. reported that the use of GnRHa to trigger final oocyte maturation in IVF compared well with hCG triggered cycles with respect to the number of mature oocytes obtained and subsequent embryonic cleavage.[62] In this study, there was a statistically significant higher number of mature oocytes, higher fertilization, and top quality embryos on day 3 favoring GnRHa trigger [Table 4].
The strengths of this study, being a randomized control trial performed in Indian Asian PCOS population with an adequate sample size. The study had some limitations too. Although there were good number of top quality embryos available on day 3, they could have been cultured to blastocyst and then frozen instead of freezing all cleavage embryos on day 3. Furthermore, the outcome in frozen-thawed cycles including the live birth rate is being collected and will be reported when available.
CONCLUSIONS
The most effective strategy which virtually eliminates the occurrence of OHSS in PCOS after ovarian stimulation in antagonist IVF cycles, is the use of GnRHa trigger in combination with cryopreservation leading to an “OHSS free clinic,” which can soon be a reality. Thus, the trigger of choice in PCOS should be GnRHa yielding more mature oocytes and good quality embryos when compared with hCG trigger. Furthermore, GnRHa triggering provides a higher patient convenience in the luteal phase, reducing the treatment burden and morbidity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Humaidan P, Quartarolo J, Papanikolaou EG. Preventing ovarian hyperstimulation syndrome: Guidance for the clinician. Fertil Steril. 2010;94:389–400. doi: 10.1016/j.fertnstert.2010.03.028. [DOI] [PubMed] [Google Scholar]
- 2.Humaidan P, Polyzos NP, Alsbjerg B, Erb K, Mikkelsen AL, Elbaek HO, et al. GnRHa trigger and individualized luteal phase hCG support according to ovarian response to stimulation: Two prospective randomized controlled multi-centre studies in IVF patients. Hum Reprod. 2013;28:2511–21. doi: 10.1093/humrep/det249. [DOI] [PubMed] [Google Scholar]
- 3.Yen SS, Llerena O, Little B, Pearson OH. Disappearance rates of endogenous luteinizing hormone and chorionic gonadotropin in man. J Clin Endocrinol Metab. 1968;28:1763–7. doi: 10.1210/jcem-28-12-1763. [DOI] [PubMed] [Google Scholar]
- 4.Papanikolaou EG, Pozzobon C, Kolibianakis EM, Camus M, Tournaye H, Fatemi HM, et al. Incidence and prediction of ovarian hyperstimulation syndrome in women undergoing gonadotropin-releasing hormone antagonist in vitro fertilization cycles. Fertil Steril. 2006;85:112–20. doi: 10.1016/j.fertnstert.2005.07.1292. [DOI] [PubMed] [Google Scholar]
- 5.Delvigne A, Rozenberg S. Review of clinical course and treatment of ovarian hyperstimulation syndrome (OHSS) Hum Reprod Update. 2003;9:77–96. doi: 10.1093/humupd/dmg005. [DOI] [PubMed] [Google Scholar]
- 6.Delvigne A, Rozenberg S. Epidemiology and prevention of ovarian hyperstimulation syndrome (OHSS): A review. Hum Reprod Update. 2002;8:559–77. doi: 10.1093/humupd/8.6.559. [DOI] [PubMed] [Google Scholar]
- 7.Nastri CO, Teixeira DM, Moroni RM, Leitão VM, Martins WP. Ovarian hyperstimulation syndrome: Pathophysiology, staging, prediction and prevention. Ultrasound Obstet Gynecol. 2015;45:377–93. doi: 10.1002/uog.14684. [DOI] [PubMed] [Google Scholar]
- 8.Navot D, Bergh PA, Laufer N. Ovarian hyperstimulation syndrome in novel reproductive technologies: Prevention and treatment. Fertil Steril. 1992;58:249–61. doi: 10.1016/s0015-0282(16)55188-7. [DOI] [PubMed] [Google Scholar]
- 9.Damewood MD, Shen W, Zacur HA, Schlaff WD, Rock JA, Wallach EE. Disappearance of exogenously administered human chorionic gonadotropin. Fertil Steril. 1989;52:398–400. doi: 10.1016/s0015-0282(16)60906-8. [DOI] [PubMed] [Google Scholar]
- 10.Fauser BC, de Jong D, Olivennes F, Wramsby H, Tay C, Itskovitz-Eldor J, et al. Endocrine profiles after triggering of final oocyte maturation with GnRH agonist after cotreatment with the GnRH antagonist ganirelix during ovarian hyperstimulation for in vitro fertilization. J Clin Endocrinol Metab. 2002;87:709–15. doi: 10.1210/jcem.87.2.8197. [DOI] [PubMed] [Google Scholar]
- 11.Humaidan P, Bredkjaer HE, Bungum L, Bungum M, Grøndahl ML, Westergaard L, et al. GnRH agonist (buserelin) or hCG for ovulation induction in GnRH antagonist IVF/ICSI cycles: A prospective randomized study. Hum Reprod. 2005;20:1213–20. doi: 10.1093/humrep/deh765. [DOI] [PubMed] [Google Scholar]
- 12.Humaidan P, Kol S, Papanikolaou EG. Copenhagen GnRH Agonist Triggering Workshop Group. GnRH agonist for triggering of final oocyte maturation: Time for a change of practice? Hum Reprod Update. 2011;17:510–24. doi: 10.1093/humupd/dmr008. [DOI] [PubMed] [Google Scholar]
- 13.Engmann L, DiLuigi A, Schmidt D, Benadiva C, Maier D, Nulsen J. The effect of luteal phase vaginal estradiol supplementation on the success of in vitro fertilization treatment: A prospective randomized study. Fertil Steril. 2008;89:554–61. doi: 10.1016/j.fertnstert.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 14.Kol S. Luteolysis induced by a gonadotropin-releasing hormone agonist is the key to prevention of ovarian hyperstimulation syndrome. Fertil Steril. 2004;81:1–5. doi: 10.1016/j.fertnstert.2003.05.032. [DOI] [PubMed] [Google Scholar]
- 15.Humaidan P, Alsbjerg B. GnRHa trigger for final oocyte maturation: Is HCG trigger history? Reprod Biomed Online. 2014;29:274–80. doi: 10.1016/j.rbmo.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 16.Griesinger G, Schultz L, Bauer T, Broessner A, Frambach T, Kissler S. Ovarian hyperstimulation syndrome prevention by gonadotropin-releasing hormone agonist triggering of final oocyte maturation in a gonadotropin-releasing hormone antagonist protocol in combination with a “freeze-all” strategy: A prospective multicentric study. Fertil Steril. 2011;95:2029–33. doi: 10.1016/j.fertnstert.2011.01.163. [DOI] [PubMed] [Google Scholar]
- 17.Tan BK, Mathur R. Management of ovarian hyperstimulation syndrome. Produced on behalf of the BFS Policy and Practice Committee. Hum Fertil (Camb) 2013;16:151–9. doi: 10.3109/14647273.2013.788313. [DOI] [PubMed] [Google Scholar]
- 18.Mocanu E, Redmond ML, Hennelly B, Collins C, Harrison R. Odds of ovarian hyperstimulation syndrome (OHSS)-time for reassessment. Hum Fertil (Camb) 2007;10:175–81. doi: 10.1080/14647270701194143. [DOI] [PubMed] [Google Scholar]
- 19.Lyons CA, Wheeler CA, Frishman GN, Hackett RJ, Seifer DB, Haning RV., Jr Early and late presentation of the ovarian hyperstimulation syndrome: Two distinct entities with different risk factors. Hum Reprod. 1994;9:792–9. doi: 10.1093/oxfordjournals.humrep.a138598. [DOI] [PubMed] [Google Scholar]
- 20.Mathur RS, Akande AV, Keay SD, Hunt LP, Jenkins JM. Distinction between early and late ovarian hyperstimulation syndrome. Fertil Steril. 2000;73:901–7. doi: 10.1016/s0015-0282(00)00492-1. [DOI] [PubMed] [Google Scholar]
- 21.Pellicer A, Albert C, Mercader A, Bonilla-Musoles F, Remohí J, Simón C. The pathogenesis of ovarian hyperstimulation syndrome: In vivo studies investigating the role of interleukin-1 beta, interleukin-6, and vascular endothelial growth factor. Fertil Steril. 1999;71:482–9. doi: 10.1016/s0015-0282(98)00484-1. [DOI] [PubMed] [Google Scholar]
- 22.Neulen J, Yan Z, Raczek S, Weindel K, Keck C, Weich HA, et al. Human chorionic gonadotropin-dependent expression of vascular endothelial growth factor/vascular permeability factor in human granulosa cells: Importance in ovarian hyperstimulation syndrome. J Clin Endocrinol Metab. 1995;80:1967–71. doi: 10.1210/jcem.80.6.7775647. [DOI] [PubMed] [Google Scholar]
- 23.Ascoli M, Fanelli F, Segaloff DL. The lutropin/choriogonadotropin receptor, a 2002 perspective. Endocr Rev. 2002;23:141–74. doi: 10.1210/edrv.23.2.0462. [DOI] [PubMed] [Google Scholar]
- 24.Al-Inany HG, Aboulghar M, Mansour R, Proctor M. Recombinant versus urinary human chorionic gonadotrophin for ovulation induction in assisted conception. Cochrane Database Syst Rev. 2005;2:CD003719. doi: 10.1002/14651858.CD003719.pub2. [DOI] [PubMed] [Google Scholar]
- 25.La Marca A, Sunkara SK. Individualization of controlled ovarian stimulation in IVF using ovarian reserve markers: From theory to practice. Hum Reprod Update. 2014;20:124–40. doi: 10.1093/humupd/dmt037. [DOI] [PubMed] [Google Scholar]
- 26.Fiedler K, Ezcurra D. Predicting and preventing ovarian hyperstimulation syndrome (OHSS): The need for individualized not standardized treatment. Reprod Biol Endocrinol. 2012;10:32. doi: 10.1186/1477-7827-10-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hamilton-Fairley D, Kiddy D, Watson H, Sagle M, Franks S. Low-dose gonadotrophin therapy for induction of ovulation in 100 women with polycystic ovary syndrome. Hum Reprod. 1991;6:1095–9. doi: 10.1093/oxfordjournals.humrep.a137491. [DOI] [PubMed] [Google Scholar]
- 28.Al-Inany HG, Abou-Setta AM, Aboulghar M. Gonadotrophin-releasing hormone antagonists for assisted conception. Cochrane Database Syst Rev. 2006;3:CD001750. doi: 10.1002/14651858.CD001750.pub2. [DOI] [PubMed] [Google Scholar]
- 29.Schmidt DW, Maier DB, Nulsen JC, Benadiva CA. Reducing the dose of human chorionic gonadotropin in high responders does not affect the outcomes of in vitro fertilization. Fertil Steril. 2004;82:841–6. doi: 10.1016/j.fertnstert.2004.03.055. [DOI] [PubMed] [Google Scholar]
- 30.Kashyap S, Parker K, Cedars MI, Rosenwaks Z. Ovarian hyperstimulation syndrome prevention strategies: Reducing the human chorionic gonadotropin trigger dose. Semin Reprod Med. 2010;28:475–85. doi: 10.1055/s-0030-1265674. [DOI] [PubMed] [Google Scholar]
- 31.Emperaire JC, Edwards RG. Time to revolutionize the triggering of ovulation. Reprod Biomed Online. 2004;9:480–3. doi: 10.1016/s1472-6483(10)61629-x. [DOI] [PubMed] [Google Scholar]
- 32.Tso LO, Costello MF, Albuquerque LE, Andriolo RB, Macedo CR. Metformin treatment before and during IVF or ICSI in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2014;11:CD006105. doi: 10.1002/14651858.CD006105.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garcia-Velasco JA, Isaza VA, Quea G, Pellicer A. Coasting for the prevention of ovarian hyperstimulation syndrome: Much ado about nothing? Fertil Steril. 2006;85:547–54. doi: 10.1016/j.fertnstert.2005.07.1335. [DOI] [PubMed] [Google Scholar]
- 34.D’Angelo A, Brown J, Amso NN. Coasting (withholding gonadotrophins) for preventing ovarian hyperstimulation syndrome. Cochrane Database Syst Rev. 2011;2:CD002811. doi: 10.1002/14651858.CD002811.pub2. [DOI] [PubMed] [Google Scholar]
- 35.DiLuigi AJ, Engmann L, Schmidt DW, Maier DB, Nulsen JC, Benadiva CA. Gonadotropin-releasing hormone agonist to induce final oocyte maturation prevents the development of ovarian hyperstimulation syndrome in high-risk patients and leads to improved clinical outcomes compared with coasting. Fertil Steril. 2010;94:1111–4. doi: 10.1016/j.fertnstert.2009.10.034. [DOI] [PubMed] [Google Scholar]
- 36.Queenan JT, Jr, Veeck LL, Toner JP, Oehninger S, Muasher SJ. Cryopreservation of all prezygotes in patients at risk of severe hyperstimulation does not eliminate the syndrome, but the chances of pregnancy are excellent with subsequent frozen-thaw transfers. Hum Reprod. 1997;12:1573–6. doi: 10.1093/humrep/12.7.1573. [DOI] [PubMed] [Google Scholar]
- 37.van der Linden M, Buckingham K, Farquhar C, Kremer JA, Metwally M. Luteal phase support for assisted reproduction cycles. Cochrane Database Syst Rev. 2011;10:CD009154. doi: 10.1002/14651858.CD009154.pub2. [DOI] [PubMed] [Google Scholar]
- 38.Schenker JG, Weinstein D. Ovarian hyperstimulation syndrome: A current survey. Fertil Steril. 1978;30:255–68. doi: 10.1016/s0015-0282(16)43508-9. [DOI] [PubMed] [Google Scholar]
- 39.Youssef MA, Al-Inany HG, Evers JL, Aboulghar M. Intra-venous fluids for the prevention of severe ovarian hyperstimulation syndrome. Cochrane Database Syst Rev. 2011;2:CD001302. doi: 10.1002/14651858.CD001302.pub2. [DOI] [PubMed] [Google Scholar]
- 40.Tang H, Hunter T, Hu Y, Zhai SD, Sheng X, Hart RJ. Cabergoline for preventing ovarian hyperstimulation syndrome. Cochrane Database Syst Rev. 2012;2:CD008605. doi: 10.1002/14651858.CD008605.pub2. [DOI] [PubMed] [Google Scholar]
- 41.Leitao VM, Moroni RM, Seko LM, Nastri CO, Martins WP. Cabergoline for the prevention of ovarian hyperstimulation syndrome: Systematic review and meta-analysis of randomized controlled trials. Fertil Steril. 2014;101:664–75. doi: 10.1016/j.fertnstert.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 42.Cenksoy C, Cenksoy PO, Erdem O, Sancak B, Gursoy R. A potential novel strategy, inhibition of vasopressin-induced VEGF secretion by relcovaptan, for decreasing the incidence of ovarian hyperstimulation syndrome in the hyperstimulated rat model. Eur J Obstet Gynecol Reprod Biol. 2014;174:86–90. doi: 10.1016/j.ejogrb.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 43.Nauck M, Karakiulakis G, Perruchoud AP, Papakonstantinou E, Roth M. Corticosteroids inhibit the expression of the vascular endothelial growth factor gene in human vascular smooth muscle cells. Eur J Pharmacol. 1998;341:309–15. doi: 10.1016/s0014-2999(97)01464-7. [DOI] [PubMed] [Google Scholar]
- 44.Itskovitz J, Boldes R, Barlev A, Erlik Y, Kahana L, Brandes JM. The induction of LH surge and oocyte maturation by GnRH analogue (Buserelin) in women undergoing ovarian stimulation for in vitro fertilization. Gynecol Endocrinol. 1988;2(Suppl 1):165. [Google Scholar]
- 45.Humaidan P, Papanikolaou EG, Tarlatzis BC. GnRHa to trigger final oocyte maturation: A time to reconsider. Hum Reprod. 2009;24:2389–94. doi: 10.1093/humrep/dep246. [DOI] [PubMed] [Google Scholar]
- 46.Devroey P, Polyzos NP, Blockeel C. An OHSS-free clinic by segmentation of IVF treatment. Hum Reprod. 2011;26:2593–7. doi: 10.1093/humrep/der251. [DOI] [PubMed] [Google Scholar]
- 47.Youssef MA, Van der Veen F, AlInany HG, Mochtar MH, Griesinger G, Nagi Mohesen M, et al. Gonadotropinreleasing hormone agonist versus HCG for oocyte triggering in antagonistassisted reproductive technology. Cochrane Database Syst Rev. 2014;10:CD008046. doi: 10.1002/14651858.CD008046.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Balaban B, Urman B, Ata B, Isiklar A, Larman MG, Hamilton R, et al. A randomised controlled study of human day 3 embryo cryopreservation by slow freezing or vitrification: Vitrification is associated with higher survival, metabolism and blastocyst formation. Hum Reprod. 2008;23:1976–82. doi: 10.1093/humrep/den222. [DOI] [PubMed] [Google Scholar]
- 49.Maheshwari A, Pandey S, Shetty A, Hamilton M, Bhattacharya S. Obstetric and perinatal outcomes in singleton pregnancies resulting from the transfer of frozen thawed versus fresh embryos generated through in vitro fertilization treatment: A systematic review and meta-analysis. Fertil Steril. 2012;98:368–77. doi: 10.1016/j.fertnstert.2012.05.019. [DOI] [PubMed] [Google Scholar]
- 50.Fatemi HM, Popovic-Todorovic B. Implantation in assisted reproduction: A look at endometrial receptivity. Reprod Biomed Online. 2013;27:530–8. doi: 10.1016/j.rbmo.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 51.Babayof R, Margalioth EJ, Huleihel M, Amash A, Zylber-Haran E, Gal M, et al. Serum inhibin A, VEGF and TNFalpha levels after triggering oocyte maturation with GnRH agonist compared with HCG in women with polycystic ovaries undergoing IVF treatment: A prospective randomized trial. Hum Reprod. 2006;21:1260–5. doi: 10.1093/humrep/dei475. [DOI] [PubMed] [Google Scholar]
- 52.Griesinger G, von Otte S, Schroer A, Ludwig AK, Diedrich K, Al-Hasani S, et al. Elective cryopreservation of all pronuclear oocytes after GnRH agonist triggering of final oocyte maturation in patients at risk of developing OHSS: A prospective, observational proof-of-concept study. Hum Reprod. 2007;22:1348–52. doi: 10.1093/humrep/dem006. [DOI] [PubMed] [Google Scholar]
- 53.Manzanares MA, Gómez-Palomares JL, Ricciarelli E, Hernández ER. Triggering ovulation with gonadotropin-releasing hormone agonist in in vitro fertilization patients with polycystic ovaries does not cause ovarian hyperstimulation syndrome despite very high estradiol levels. Fertil Steril. 2010;93:1215–9. doi: 10.1016/j.fertnstert.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 54.Youssef MA, Abdelmoty HI, Ahmed MA, Elmohamady M. GnRH agonist for final oocyte maturation in GnRH antagonist co-treated IVF/ICSI treatment cycles: Systematic review and meta-analysis. J Adv Res. 2015;6:341–9. doi: 10.1016/j.jare.2015.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Melo M, Busso CE, Bellver J, Alama P, Garrido N, Meseguer M, et al. GnRH agonist versus recombinant HCG in an oocyte donation programme: A randomized, prospective, controlled, assessor-blind study. Reprod Biomed Online. 2009;19:486–92. doi: 10.1016/j.rbmo.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 56.Sismanoglu A, Tekin HI, Erden HF, Ciray NH, Ulug U, Bahceci M. Ovulation triggering with GnRH agonist vs. hCG in the same egg donor population undergoing donor oocyte cycles with GnRH antagonist: A prospective randomized cross-over trial. J Assist Reprod Genet. 2009;26:251–6. doi: 10.1007/s10815-009-9326-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hernández ER, Gómez-Palomares JL, Ricciarelli E. No room for cancellation, coasting, or ovarian hyperstimulation syndrome in oocyte donation cycles. Fertil Steril. 2009;91(4 Suppl):1358–61. doi: 10.1016/j.fertnstert.2008.03.077. [DOI] [PubMed] [Google Scholar]
- 58.Cerrillo M, Rodríguez S, Mayoral M, Pacheco A, Martínez-Salazar J, Garcia-Velasco JA. Differential regulation of VEGF after final oocyte maturation with GnRH agonist versus hCG: A rationale for OHSS reduction. Fertil Steril. 2009;91(4 Suppl):1526–8. doi: 10.1016/j.fertnstert.2008.08.118. [DOI] [PubMed] [Google Scholar]
- 59.Seyhan A, Ata B, Polat M, Son WY, Yarali H, Dahan MH. Severe early ovarian hyperstimulation syndrome following GnRH agonist trigger with the addition of 1500 IU hCG. Hum Reprod. 2013;28:2522–8. doi: 10.1093/humrep/det124. [DOI] [PubMed] [Google Scholar]
- 60.Datta AK, Eapen A, Birch H, Kurinchi-Selvan A, Lockwood G. Retrospective comparison of GnRH agonist trigger with HCG trigger in GnRH antagonist cycles in anticipated high-responders. Reprod Biomed Online. 2014;29:552–8. doi: 10.1016/j.rbmo.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 61.Fatemi HM, Popovic-Todorovic B, Humaidan P, Kol S, Banker M, Devroey P, et al. Severe ovarian hyperstimulation syndrome after gonadotropin-releasing hormone (GnRH) agonist trigger and “freeze-all” approach in GnRH antagonist protocol. Fertil Steril. 2014;101:1008–11. doi: 10.1016/j.fertnstert.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 62.Griesinger G, Diedrich K, Devroey P, Kolibianakis EM. GnRH agonist for triggering final oocyte maturation in the GnRH antagonist ovarian hyperstimulation protocol: A systematic review and meta-analysis. Hum Reprod Update. 2006;12:159–68. doi: 10.1093/humupd/dmi045. [DOI] [PubMed] [Google Scholar]