Abstract
Although it is widely acknowledged that there are not enough clinicians trained in either Behavioral Sleep Medicine (BSM) in general or in Cognitive Behavioral Therapy for Insomnia (CBT-I) in specific, what is unclear is whether this problem is more acute in some regions relative to others. Accordingly, a geographic approach was taken to assess this issue. Using national directories as well as e-mail listservs (Behavioral Sleep Medicine group and Behavioral Treatment for Insomnia Roster), the present study evaluated geographic patterning of CBSM and BSM providers by city, state, and country. Overall, 88% of 752 BSM providers worldwide live in the United States (n = 659). Of these, 58% reside in 12 states with ≥ 20 providers (CA, NY, PA, IL, MA, TX, FL, OH, MI, MN, WA, and CO), and 19% reside in just 2 states (NY and CA). There were 4 states with no BSM providers (NH, HI, SD, and WY). Of the 167 U.S. cities with a population of > 150,000, 105 cities have no BSM providers. These results clearly suggest that a targeted effort is needed to train individuals in both the unserved and underserved areas.
Cognitive Behavioral Therapy for Insomnia (CBT-I) has demonstrated efficacy (e.g., Irwin, Cole, & Nicassio, 2006; Mitchell, Gehrman, Perlis, & Umscheid, 2012; Morin, Culbert, & Schwartz, 1994; Murtagh & Greenwood, 1995;Okajima, Komada, & Inoue, 2011), efficacy relative to hypnotic medication (e.g., Edinger, Wohlgemuth, Krystal, & Rice, 2005; Edinger et al., 2009; Jacobs, Pace-Schott, Stickgold, & Otto, 2004; Jungquist et al., 2010; McClusky, Milby, Switzer, Williams, & Wooten, 1991; Morin, Colecchi, Stone, Sood, & Brink, 1999; Sivertsen et al., 2006; Smith et al., 2002), and effectiveness in a number of clinical populations with comorbid insomnia (Currie, Wilson, Pontefract, & deLaplante, 2000; Lichstein, Wilson, & Johnson, 2000; M. Perlis et al., 2000; M. L. Perlis, Sharpe, Smith, Greenblatt, & Giles, 2001; Savard, Simard, Ivers, & Morin, 2005; Smith, Huang, & Manber, 2005). Despite the clear clinical utility of CBT-I, most patients will not receive this form of treatment. This is likely for a variety of reasons, including the initial costs of treatment, the time commitment involved, the stigma of psychotherapy, the ease and acceptability of pharmacother-apy (at least in the short run), and the lack of public awareness about CBT-I as the only treatment with durable results following treatment and the demonstrated potential for producing recovery. Even if these factors were fully addressed, there would remain at least one profound barrier to treatment access: There are very few therapists who have been trained in, and provide, CBT-I. As of 2015, 206 individuals in the United States were credentialed by the American Board of Sleep Medicine (ABSM) to provide CBT-I and approximately only 10% of the 2,334 accredited centers in the United States have a PhD sleep specialist on staff (personal communication with American Academy of Sleep Medicine staff). Thus, CBT-I is not widely available at the specialty care level. The absolute unavailability of CBT-I notwithstanding, there is also the issue of whether the problem is more acute in some countries, states, and cities as opposed to others. Accordingly, a geographic approach was taken to evaluate this issue. The aim of the present brief report was to identify and describe (a) where CBT-I and/or Behavioral Sleep Medicine (BSM) providers are located, (b) which areas are best-served by CBT-I/BSM providers, and (c) which areas most need providers.
METHODS
The American Board of Sleep Medicine (ABSM) listing of clinicians certified in Behavioral Sleep Medicine (CBSM; http://www.absm.org/BSMSpecialists.aspx) and the Society of Behavioral Sleep Medicine website (http://www.behavioralsleep.org) listing of practicing behavioral sleep medicine providers were reviewed and updated to reflect the current location of each credentialed provider using the American Academy of Sleep Medicine (AASM) and Sleep Research Society member directories and Internet searches. In an effort to gain a more complete representation of the number and location of BSM providers, survey data was also gathered in order to catalog the location of providers without affiliations with either the ABSM or Society of Behavioral Sleep Medicine (SBSM). Surveys were posted to the Behavioral Sleep Medicine Group email listserv (http://www.behavsleepmed.com, n = 551) as well as the Behavioral Therapy for Insomnia Roster (BTIR, n = 352). The survey itself was comprised of 8 demographic items (name, profession, degrees, contact information, etc.) and 5 questions pertaining to professional practice (board certifications, years in practice, years as a CBT-I provider, etc.). The nonexclusive membership of these two groups allowed for the inclusion of several hundred additional non–CBSM or SBSM-affiliated BSM providers in our geographical analysis. The location data were cataloged in spreadsheets, duplicates were removed, and frequencies were tabulated and plotted by city, state, and country. Population estimates are based on (2014) census data from the U. S. Census Bureau.
RESULTS
The total number of CBT-I/BSM specialists identified in this analysis was 752 individuals. Of the 752 identified BSM providers, n = 659 (88%) are in the United States. With the exception of Canada (n = 37), no other country has greater than 7 BSM providers and 182 nations are entirely unserved (See Table 1 for list of countries by number of BSM providers, and Figure 1 for the world map).
TABLE 1.
BSM Specialists by Country
| Country | Number of providers |
|---|---|
| USA | 659 |
| Canada | 37 |
| Australia | 7 |
| Israel | 6 |
| South Africa | 5 |
| France | 4 |
| China | 3 |
| England | 3 |
| Germany | 3 |
| Italy | 3 |
| Japan | 3 |
| Norway | 3 |
| Columbia | 2 |
| Netherlands | 2 |
| New Zealand | 2 |
| Taiwan | 2 |
| Brazil | 1 |
| Denmark | 1 |
| Ireland | 1 |
| Korea | 1 |
| Puerto Rico | 1 |
| Scotland | 1 |
| Spain | 1 |
| Thailand | 1 |
FIGURE 1.
World map of BSM provider locations.
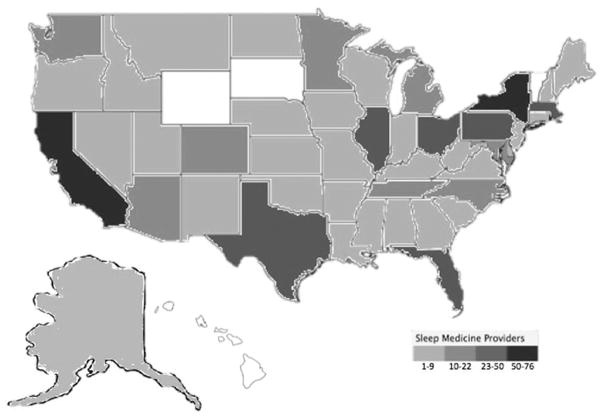
Although the United States contains the vast majority of CBT-I/BSM providers, they are not evenly dispersed across the nation (see Figures 2 and 3). Particular divisions (as defined by the U.S. census bureau) are relatively underserved. The nine divisions that comprise the entire United States, as defined by the U.S. census bureau, include New England, Middle Atlantic, South Atlantic, East North Central, East South Central, West North Central, West South Central, Mountain, and Pacific. Of these divisions, the East South Central (KY, TN, MS, and AL) is the most underserved, with only n = 29 of the 659 total BSM providers in the United States. In contrast, the Middle Atlantic division (NY, PA, NJ) contains the most BSM providers (n = 117), despite being composed of only 3 states. The Pacific (CA, WA, and OR), South Atlantic (WV, MD, DC, DE, VA, NC, SC, GA, and FL) and East North Central (OH, MI, IN, IL, and WI) divisions also have a relatively high number of BSM providers (108, 101, and 101, respectively). See Table 2 for a list of divisions organized by number of BSM providers.
FIGURE 2.
U.S. map of BSM provider locations.
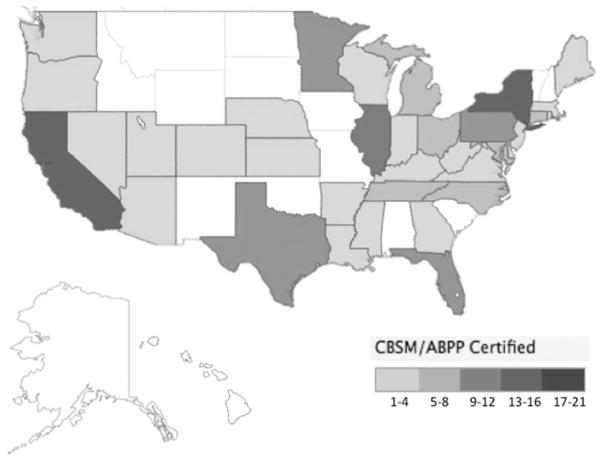
FIGURE 3.
ABSM ABPP certified BSM provider locations.
TABLE 2.
BSM Specialists by Census Division
| Division | Number of providers |
|---|---|
| Middle Atlantic | 117 |
| Pacific | 111 |
| South Atlantic | 101 |
| East North Central | 101 |
| New England | 55 |
| Mountain | 51 |
| West South Central | 49 |
| West North Central | 48 |
| East South Central | 29 |
This unequal distribution of BSM providers is also evident at the state level (see Table 3 for a list of states in order of decreasing BSM providers). Fifty-eight percent of the BSM providers in the United States reside in 12 states with ≥ 20 providers (CA, NY, PA, IL, MA, TX, FL, OH, MI, MN, WA, and CO), and 19% reside in just 2 states (NY and CA). Thirty-two states, including the District of Columbia, had fewer than 10 BSM providers, and there were 4 states with no BSM providers (HI, NH, SD, and WY). There is an even greater shortage of BSM providers certified by the American Board of Sleep Medicine (ABSM-CBSMs). There are n = 216 CBSM providers, 206 of which reside in the United States. Similar to the analysis of BSM providers in general, states such as CA, NY, IL, PA, and TX have a relatively high number of CBSMs. There are also several states (AL, SC, AK, RI, OK, ID, ND, IA, MT, NH, HI, SD, WY) without any certified providers. See Table 4 for a list of states organized by number of certified BSM providers.
TABLE 3.
BSM Providers by State
| State | Number of providers |
|---|---|
| CA | 73 |
| NY | 70 |
| PA | 41 |
| IL | 36 |
| MA | 34 |
| TX | 33 |
| FL | 27 |
| OH | 27 |
| CO | 24 |
| MN | 24 |
| MI | 23 |
| WA | 22 |
| MD | 17 |
| NC | 14 |
| TN | 14 |
| AZ | 12 |
| MO | 11 |
| DC | 10 |
| CT | 9 |
| VA | 9 |
| WI | 9 |
| AL | 8 |
| OR | 8 |
| AR | 7 |
| SC | 7 |
| WV | 7 |
| IN | 6 |
| ME | 6 |
| NJ | 6 |
| AK | 5 |
| DE | 5 |
| GA | 5 |
| KS | 5 |
| LA | 5 |
| NE | 5 |
| RI | 5 |
| KY | 4 |
| NM | 4 |
| NV | 4 |
| OK | 4 |
| UT | 4 |
| MS | 3 |
| ID | 2 |
| ND | 2 |
| IA | 1 |
| MT | 1 |
| VT | 1 |
| HI | 0 |
| NH | 0 |
| SD | 0 |
| WY | 0 |
TABLE 4.
Certified BSM Providers by State
| State | Number of providers |
|---|---|
| NY | 22 |
| CA | 21 |
| IL | 16 |
| PA | 15 |
| TX | 14 |
| OH | 11 |
| MN | 11 |
| FL | 10 |
| NC | 8 |
| MI | 7 |
| TN | 7 |
| CO | 5 |
| MD | 5 |
| AZ | 5 |
| CT | 5 |
| MA | 4 |
| WA | 4 |
| KY | 4 |
| WI | 3 |
| UT | 3 |
| OR | 2 |
| AR | 2 |
| WV | 2 |
| ME | 2 |
| GA | 2 |
| KS | 2 |
| LA | 2 |
| NE | 2 |
| MO | 1 |
| DC | 1 |
| VA | 1 |
| IN | 1 |
| NJ | 1 |
| DE | 1 |
| NM | 1 |
| NV | 1 |
| MS | 1 |
| VT | 1 |
| AL | 0 |
| SC | 0 |
| AK | 0 |
| RI | 0 |
| OK | 0 |
| ID | 0 |
| ND | 0 |
| IA | 0 |
| MT | 0 |
| HI | 0 |
| NH | 0 |
| SD | 0 |
| WY | 0 |
State-level analyses are effective for identifying large areas that are underserved in terms of BSM providers; however, such analyses lack the specificity needed to identify geographical areas within a state that may be underserved. A tendency of CBT-I/BSM providers to aggregate to larger cities can be observed using data specific to the city level. Figure 4 demonstrates this effect with a density of the concentration of BSM providers by geographical region. As can be seen in Figure 4, certain urban centers and the suburbs surrounding them, such as Chicago, New York, Philadelphia, San Francisco, and Los Angeles, contain a relatively high density of BSM providers. As can be seen in Tables 5 and 6, there are no identified BSM providers in 2 of the 15 most populous cities in the United States (Jacksonville and San Jose) and Los Angeles, Houston, Phoenix, and Dallas (2nd, 4th, 6th, and 9th respectively in terms of population) all have ratios of over 1 million residents to each provider. In contrast to those cities, Chicago, Philadelphia, Austin, and San Francisco (3rd, 5th, 11th, and 14th in terms of population) have the best ratios of residents to providers at less than 300,000 residents per provider.
FIGURE 4.
Density map of BSM providers by city in the United States.
TABLE 5.
Resident to Provider Ratio in 15 Most Populous Cities
| City | Population | Providers | Number of residents per provider |
|---|---|---|---|
| Austin | 885,400 | 5 | 177,080 |
| Philadelphia | 1,553,165 | 7 | 221,881 |
| Chicago | 2,718,782 | 12 | 226,565 |
| San Francisco | 837,442 | 3 | 279,147 |
| San Diego | 1,355,896 | 4 | 338,974 |
| San Antonio | 1,409,019 | 3 | 469,673 |
| New York | 8,405,837 | 16 | 525,365 |
| Columbus | 822,553 | 1 | 822,553 |
| Indianapolis | 843,393 | 1 | 843,393 |
| Houston | 2,195,914 | 2 | 1,097,957 |
| Dallas | 1,257,676 | 1 | 1,257,676 |
| Los Angeles | 3,884,307 | 3 | 1,294,769 |
| Phoenix | 1,513,367 | 1 | 1,513,367 |
| San Jose | 988,537 | 0 | N/A |
| Jacksonville | 842,583 | 0 | N/A |
TABLE 6.
Largest U.S. Cities That Have No BSM Providers (20 Largest Cities)
| City | State | Population | Rank |
|---|---|---|---|
| San Jose | California | 1,015,785 | 10 |
| Jacksonville | Florida | 853,382 | 12 |
| Charlotte | North Carolina | 809,958 | 17 |
| Detroit | Michigan | 680,250 | 18 |
| El Paso | Texas | 679,036 | 19 |
| Oklahoma City | Oklahoma | 620,602 | 27 |
| Las Vegas | Nevada | 613,599 | 29 |
| Fresno | California | 515,986 | 34 |
| Sacramento | California | 485,199 | 35 |
| Long Beach | California | 473,577 | 36 |
| Mesa | Arizona | 464,704 | 38 |
| Virginia Beach | Virginia | 450,980 | 40 |
| Colorado Springs | Colorado | 445,830 | 42 |
| Raleigh | North Carolina | 439,896 | 43 |
| Miami | Florida | 430,332 | 44 |
| Tulsa | Oklahoma | 399,682 | 47 |
| Wichita | Kansas | 388,413 | 49 |
| Arlington | Texas | 383,204 | 51 |
| Bakersfield | California | 368,759 | 52 |
| Tampa | Florida | 358,699 | 53 |
DISCUSSION
The present study explored geographic patterning of CBT-I/BSM providers in the United States and worldwide. Not only are there very few providers, but they are also disproportionately located in only a few areas of the United States and in only a few countries worldwide. The majority of CBT-I/BSM providers reside in the United States. Worldwide, with the exception of Canada, no other country has greater than 7 BSM providers and 182 nations are entirely unserved. Within the United States, 58% of the providers reside in CA, NY, PA, IL, MA, TX, FL, OH, MI, MN, WA, and CO. The two states with the most providers, NY and CA, contain 19% of the U.S. BSM providers while states such as NH, HI, SD, and WY have no providers.
Study Limitations
The primary limitation of the present study, and any effort to catalog the number of CBT-I/BSM providers that presently exist, depends on how such individuals are identified. At present, this is limited to those that are certified in behavioral sleep medicine, those that have registered on provider lists, and those that belong to dedicated behavioral sleep medicine listservs. While the use of provider lists and listservs for the present represent study represent our effort to be more inclusive, using such sources (a) provides no means of ascertaining the individuals’ relative expertise and (b) still does not provide adequate survey coverage. With respect to the latter, there are likely to be many individuals that conduct CBT-I or provide BSM treatments for other sleep disorders that are unaffiliated with any of these professional agencies, and even if affiliated, they may not have received or responded to our request for identifying information. Thus, the present estimates are most probably conservative ones. At this juncture, it is abundantly clear that there is a need to develop strategies to reach out to those who are unaffiliated to, at minimum, self-identify as providers and, at maximum, to be provided the kind of incentives and inducements to participate in the further development of our discipline. Ideally, state, national, and international societies that are dedicated to, or have strong commitments to, Behavioral Sleep Medicine should work toward this end.
Study Conclusions
One question that arises from these data is, “Why are specific regions well served while others are not?” One answer is that sleep medicine in general has yet to become a health focus for developing nations. With respect to the aggregation of CBT-I/BSM clinicians in high-population cities and regions of the United States, the uneven distribution is likely an artifact of population density. This notwithstanding, it is also possible that regions with well-known training programs simply produce the largest number of CBT-I/BSM providers and that many of these individuals reside in, or settle in, the areas where training is available. This suggests that training programs need to be established and developed in such unserved or underserved regions as the East South Central and Mountain regions, particularly South Carolina and Georgia, and Wyoming and South Dakota. Short of establishing new university-based programs, perhaps one way to expedite the goal of “universal” BSM coverage is to reach out to state and local professional organizations (e.g., state psychology associations and nurse practitioner societies) and to offer access to training (or local trainings) via the Society of Behavioral Sleep Medicine, the CBT-I program affiliated with the Veterans Affairs system (Manber et al., 2012), or via other continuing education training programs such as those offered by Oxford University, Ryerson University, University of Pennsylvania, or the Center for Deployment Psychology. Similar outreach efforts could be made for the international community.
Footnotes
For an additional list of CBT-I providers (in addition to the ABSM and SBSM lists), please see http://www.med.upenn.edu/cbti/provder_directory.html
Color versions of one or more figures in the article can be found online at www.tandfonline.com/hbsm
Contributor Information
Arthur Thomas, Department of Biology, University of Pennsylvania, Philadelphia, Pennsylvania, Behavioral Sleep Medicine Program, Department of Psychiatry, University of Pennsylvania, Philadelphia, Pennsylvania.
Michael Grandner, Department of Psychiatry, College of Medicine, University of Arizona, Tucson, Arizona.
Sara Nowakowski, Department of Obstetrics & Gynecology, Department of Psychiatry & Behavioral Sciences, The University of Texas (Medical Branch), Galveston, Texas.
Genevieve Nesom, Behavioral Sleep Medicine Program, Department of Psychiatry, University of Pennsylvania, Philadelphia, Pennsylvania.
Charles Corbitt, Behavioral Sleep Medicine Program, Department of Psychiatry, University of Pennsylvania, Philadelphia, Pennsylvania.
Michael L. Perlis, Behavioral Sleep Medicine Program, Department of Psychiatry, University of Pennsylvania, Philadelphia, Pennsylvania, Center for Sleep and Circadian Neurobiology, University of Pennsylvania, Philadelphia, Pennsylvania
References
- Currie SR, Wilson KG, Pontefract AJ, deLaplante L. Cognitive-behavioral treatment of insomnia secondary to chronic pain. Journal of Consulting and Clinical Psychology. 2000;68(3):407–416. doi: 10.1037//0022-006x.68.3.407. [DOI] [PubMed] [Google Scholar]
- Edinger JD, Olsen MK, Stechuchak KM, Means MK, Lineberger MD, Kirby A, Carney CE. Cognitive behavioral therapy for patients with primary insomnia or insomnia associated predominantly with mixed psychiatric disorders: A randomized clinical trial. Sleep. 2009;32(4):499–510. doi: 10.1093/sleep/32.4.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edinger JD, Wohlgemuth WK, Krystal AD, Rice JR. Behavioral insomnia therapy for fibromyalgia patients: A randomized clinical trial. Archives of Internal Medicine. 2005;165(21):2527–2535. doi: 10.1001/archinte.165.21.2527. [DOI] [PubMed] [Google Scholar]
- Irwin MR, Cole JC, Nicassio PM. Comparative meta-analysis of behavioral interventions for insomnia and their efficacy in middle-aged adults and in older adults 55+ years of age. Health Psychology. 2006;25(1):3–14. doi: 10.1037/0278-6133.25.1.3. [DOI] [PubMed] [Google Scholar]
- Jacobs GD, Pace-Schott EF, Stickgold R, Otto MW. Cognitive behavior therapy and pharmacotherapy for insomnia: A randomized controlled trial and direct comparison. Archives of Internal Medicine. 2004;164(17):1888–1896. doi: 10.1001/archinte.164.17.1888. [DOI] [PubMed] [Google Scholar]
- Jungquist CR, O’Brien C, Matteson-Rusby S, Smith MT, Pigeon WR, Xia Y, … Perlis ML. The efficacy of cognitive-behavioral therapy for insomnia in patients with chronic pain. Sleep Medicine. 2010;11(3):302–309. doi: 10.1016/j.sleep.2009.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichstein KL, Wilson NM, Johnson CT. Psychological treatment of secondary insomnia. Psychology of Aging. 2000;15(2):232–240. doi: 10.1037//0882-7974.15.2.232. [DOI] [PubMed] [Google Scholar]
- Manber R, Carney C, Edinger J, Epstein D, Friedman L, Haynes PL, … Trockel M. Dissemination of CBTI to the non-sleep specialist: Protocol development and training issues. Journal of Clinical Sleep Medicine. 2012;8(2):209–218. doi: 10.5664/jcsm.1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClusky HY, Milby JB, Switzer PK, Williams V, Wooten V. Efficacy of behavioral versus triazolam treatment in persistent sleep-onset insomnia. American Journal of Psychiatry. 1991;148(1):121–126. doi: 10.1176/ajp.148.1.121. [DOI] [PubMed] [Google Scholar]
- Mitchell MD, Gehrman P, Perlis M, Umscheid CA. Comparative effectiveness of cognitive behavioral therapy for insomnia: A systematic review. BMC Family Practice. 2012;13:40. doi: 10.1186/1471-2296-13-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin CM, Colecchi C, Stone J, Sood R, Brink D. Behavioral and pharmacological therapies for late-life insomnia: A randomized controlled trial. Journal of the American Medical Association. 1999;281(11):991–999. doi: 10.1001/jama.281.11.991. [DOI] [PubMed] [Google Scholar]
- Morin CM, Culbert JP, Schwartz SM. Nonpharmacological interventions for insomnia: A meta-analysis of treatment efficacy. American Journal of Psychiatry. 1994;151(8):1172–1180. doi: 10.1176/ajp.151.8.1172. [DOI] [PubMed] [Google Scholar]
- Murtagh DR, Greenwood KM. Identifying effective psychological treatments for insomnia: A meta-analysis. Journal of Consulting and Clinical Psychology. 1995;63(1):79–89. doi: 10.1037//0022-006x.63.1.79. [DOI] [PubMed] [Google Scholar]
- Okajima I, Komada Y, Inoue D. A meta-analysis on the treatment effectiveness of cognitive behavioral therapy for primary insomnia. Sleep and Biological Rhythms. 2011;9(1):24–34. [Google Scholar]
- Perlis M, Aloia M, Millikan A, Boehmler J, Smith M, Greenblatt D, Giles D. Behavioral treatment of insomnia: A clinical case series study. Journal of Behavioral Medicine. 2000;23(2):149–161. doi: 10.1023/a:1005413117932. [DOI] [PubMed] [Google Scholar]
- Perlis ML, Sharpe M, Smith MT, Greenblatt D, Giles D. Behavioral treatment of insomnia: Treatment outcome and the relevance of medical and psychiatric morbidity. Journal of Behavioral Medicine. 2001;24(3):281–296. doi: 10.1023/a:1010770807823. [DOI] [PubMed] [Google Scholar]
- Savard J, Simard S, Ivers H, Morin CM. Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer: Part I. Sleep and psychological effects. Journal of Clinical Oncology. 2005;23(25):6083–6096. doi: 10.1200/JCO.2005.09.548. [DOI] [PubMed] [Google Scholar]
- Sivertsen B, Omvik S, Pallesen S, Bjorvatn B, Havik OE, Kvale G, … Nordhus IH. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: A randomized controlled trial. Journal of the American Medical Association. 2006;295(24):2851–2858. doi: 10.1001/jama.295.24.2851. [DOI] [PubMed] [Google Scholar]
- Smith MT, Huang MI, Manber R. Cognitive behavior therapy for chronic insomnia occurring within the context of medical and psychiatric disorders. Clinical Psychology Review. 2005;25(5):559–592. doi: 10.1016/j.cpr.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Smith MT, Perlis ML, Park A, Smith MS, Pennington J, Giles DE, Buysse DJ. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. American Journal of Psychiatry. 2002;159(1):5–11. doi: 10.1176/appi.ajp.159.1.5. [DOI] [PubMed] [Google Scholar]