Abstract
Background
The aim of this study was to assess the clinical results of treatment for unstable posterior pelvic fractures using a pedicle screw-rod fixator compared to use of a locking compression plate.
Material/Methods
A retrospective study was performed between June 2010 and May 2014 and the data were collected from 46 patients with unstable posterior pelvic ring fractures. All patients were treated using either a pedicle screw-rod fixator (study group, 24 patients) or locking compression plate (control group, 22 patients). In these patients, causes of injury included traffic accidents (n=27), fall from height (n=12), and crushing accidents (n=7). The quality of reduction and radiological grading were assessed. Clinical assessments included the operation time, times of X-ray exposures, bleeding volume during operation, incision length, and Majeed postoperative functional evaluation.
Results
No iatrogenic neurovascular injuries occurred during the operations in these 2 groups. The average follow-up time was 24.5 months. All fractures were healed. The significant differences (P<0.05) between the 2 groups were operation duration, size of incision, and intraoperative bleeding volume. Statistically significant differences in the Majeed postoperative functional evaluation and times of X-ray exposures were not found between the 2 groups.
Conclusions
Similar clinical effects were achieved in treating the posterior pelvic ring fractures using the pedicle screw-rod fixator and the locking compression plate. However, the pedicle screw-rod fixator has the advantages of smaller incision, shorter duration of the operation, and less bleeding volume compared to using the locking compression plate.
MeSH Keywords: Fractures, Bone; Internal Fixators; Pelvic Bones
Background
Resulting from high-energy trauma such as traffic accidents and falls, unstable posterior pelvic ring fractures, with hemorrhage and a high mortality rate, usually lead to rotatory and vertical instability of the pelvis because of the disruption of the complex structure of the sacrum, sacroiliac joint, and ilium [1,2]. The purpose of the treatment is to rigidly stabilize anatomical structures of the pelvis and to avoid serious associated complications [3,4]. However, posterior pelvic ring fractures are relatively difficult to manage because the pelvis has an irregular and complex cortical surface and is also a weight-bearing structure bearing 70% of body weight [5,6]. Associated with surgery for pelvic ring fractures, long-term problems usually include restricted activities of daily living, post-operative pain, nonunion, and malunion [7]. Dynamic imbalance of the pelvis caused by malunion often results in dysfunctions of weight bearing, which is also a serious complication [8]. In view of these, challenges still exist for orthopedic surgeons to acquire high-quality reduction of the posterior pelvic ring [9].
Over the past several decades, a variety of management techniques have been employed to restore the integrity of the pelvis and its relevant structures, and to relieve compression of the nerves and blood vessels [10–12]. Among these techniques, the locking compression plate (LCP) is one of the most effective methods for stabilizing the posterior pelvic ring, due to its convenience and relatively low trauma [6]. The pedicle screw-rod fixator, due to its effective immobilization and minimal invasion, is also applied in the clinical management of posterior pelvic ring fractures [1]. At present, few reports have compared these 2 kinds of fixations. This study aimed to evaluate the clinical effects of applying the pedicle screw-rod fixator and locking compression plate in the management of unstable posterior pelvic ring fractures.
Material and Methods
Ethics statement
This study was reviewed and approved by the Institutional Review Board of the Shanghai General Hospital affiliated to Shanghai Jiao Tong University. The study was performed following the principles of the 1964 Declaration of Helsinki.
A retrospective analysis of posterior pelvic ring fractures was performed in this study between June 2010 and May 2014 in our trauma center. The inclusion criteria were as follows:
(1) unstable posterior pelvic ring fracture (including type B2, type B3, and type C1), (2) hemodynamic stability, (3) clear consciousness, (4) without serious medical conditions, (5) complete or fundamental repositioning of the fracture after preoperative traction, and (6) completely collected follow-up data. Exclusion criteria were open fractures with contaminated wound, serious osteoporosis, and type A, type C2, and type C3 fractures. A total of 46 patients were enrolled according to these criteria. The causes of injury were traffic accident in 27 patients, fall from height for 12 patients, and crushing by a motor vehicle in 7 patients. The pelvic fractures were OTA 61 type B in 39 cases (15 type B2 and 24 type B3) and type C in 6 cases (6 type C1). Among them, 24 patients (study group) were treated with use of a pedicle screw-rod fixator and the other 22 patients (control group) were treated with a locking compression plate. Among them, 31 patients (17 in study group and 14 in control group) were poly-traumatized, including traumatic head injuries in 8 patients, chest trauma (rib fractures, pneumothorax, and traumatic hemopneumothorax) in 7 patients, and femoral fractures and tibiofibular fractures in 16 patients. Traumatic skin injury of different levels were found in all patients. The general data on these 2 groups are shown in Tables 1 and 2.
Table 1.
The general data of two groups.
| Internal fixation with pedicle screw and rod group | Internal fixation with locking compression plate group | P value | |
|---|---|---|---|
| Sex (Male: Female) | 13: 11 | 10: 12 | 0.565 |
| Age (years) | 35.41±8.17 | 33.36±7.16 | 0.371 |
| Fracture type (B2:B3:C1) | 9: 12: 3 | 6: 12: 4 | 0.432 |
| Follow-up period (months) | 24.96±4.80 | 24.05±5.14 | 0.548 |
Table 2.
Additional data of two groups.
| Internal fixation with pedicle screw and rod group | Internal fixation with locking compression plate group | |
|---|---|---|
| Osseous union (n) | 24 | 21 |
| Complication: malunion (n) | 0 | 1 |
| Complication: Incision infection (n) | 0 | 3 |
| Additional anterior ring stabilization (n) | 21 | 13 |
| Isolated pelvic fracture vs. additional fractures (n) | 7: 17 | 8: 14 |
| Time point of the Majeed functional evaluation score (month) | Started from the 6th month in follow-up period | Started from the 6th month in follow-up period |
Radiological examinations of anteroposterior, inlet, and outlet views of the pelvis were examined in all these patients preoperatively. Before the surgery, to better evaluate the condition of fracture dislocation and pelvic fracture stability, computed tomography (CT) scanning followed by 3-dimensional (3D) reconstruction were performed as well.
Surgical procedures
Since posterior pelvic ring fracture is usually combined with anterior pelvic ring fracture, to restore the stability and integrity of unstable pelvic ring fracture, the anterior pelvic ring fracture should be taken into account as well. After general anesthesia, the prone position for all patients was employed and the posterior pelvic ring was fixed with either a pedicle screw-rod fixator or locking compression plate.
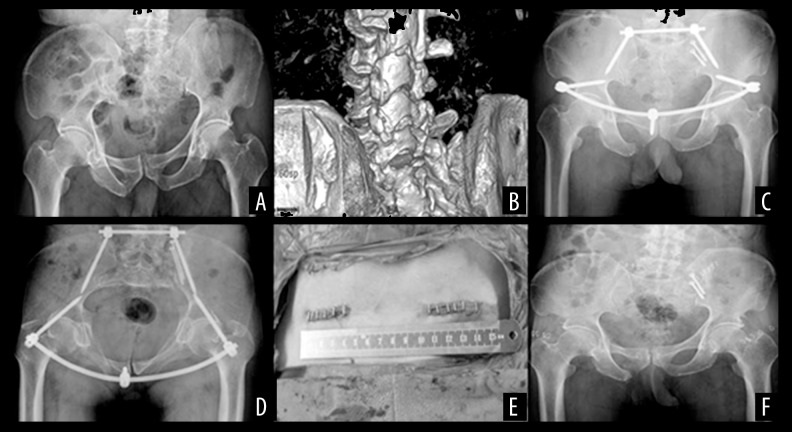
In the study group, after marking the outline of bilateral sides of the iliac posterior superior spine, a 3–4-cm incision was made 1 cm lateral to the iliac posterior superior spine. After opening the back fascia and dissecting the crista iliaca, the pedicle screw opener was used at the junction of the back 2/3 and front 1/3 of the crista iliaca cortical bone to make an osseous tunnel between the cortexes of the ilium towards the iliac anterior inferior spine. After checking to ensure the tunnel did not penetrate the bony cortex of the medial or lateral sides, we inserted screws (Johnson & Johnson Co, USA) that were 60–80 mm long and 7 mm wide. The end of each screw (U-type clamp) was inserted into the cancellous bone to make it adjustable and no higher than the crista iliaca level. The proper length of the rod was selected after measuring the distance between the screws on both sides. After linking the screws on each side through the sub-back fascia, the rod was fixed. The adjustments of stretching or compressing of the pedicle screw-rod fixator was performed according to the dislocation conditions of the posterior pelvic ring to complete the reduction and fixation (Figure 1).
Figure 1.
A 43-year-old male patient, pelvic fracture due to a crushing injury. (A, B) Preoperative X-ray plain film showed posterior pelvic ring fracture with avulsion fracture of posterior superior iliac spine. (C, D) The postoperative X-ray plain film showed satisfactory reduction of the fracture with rod-pedicle screw fixator. (E) The incision after the operation. (F) The fracture was healed 1 year after the operation.
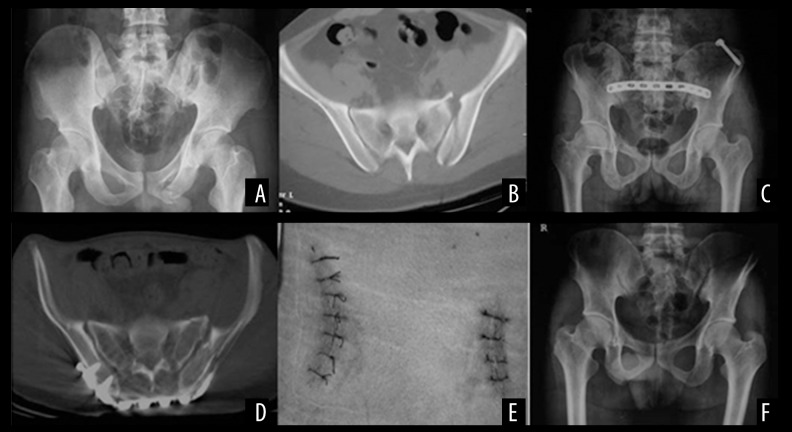
In the control group, the outline of bilateral sides of the iliac posterior superior spine, iliac posterior inferior spine, and parts of the crista iliaca were marked. An arc incision, 2 cm lateral to the iliac posterior superior spine, was made at the crista iliaca, with an average length of 8 cm. After we dissected the iliac posterior superior spine, iliac posterior inferior spine, and crista iliaca, 4 cm of gluteal muscles were stripped off along the lateral surface of the ilium, followed by application of gauze to stop bleeding, after which a 4.5-mm LCP with 10–11 holes (Synthes Co., Switzerland) was bent for molding according to the shape of posterior pelvis, with each side having 2–3 holes left. The LCP was inserted into both sides through the subcutaneous tunnel, then the plate was reversed and both ends were inserted into the tunnel between the gluteal muscles and the ilium. The plate was compacted to make it stick closely to the iliac bone surface, and then 2–3 screws on each end of the plate were fixed and tightened without penetrating the medial side cortex of the ilium. After carefully stopping bleeding, cleaning the surgical field, and suturing the gluteal muscles to the starting point, the incision was closed (Figure 2).
Figure 2.
A 39-year-old male patient, pelvic fracture due to a traffic accident. (A, B) Preoperative X-ray plain film and CT images displayed posterior pelvic ring fracture. (C, D) The postoperative X-ray plain film showed satisfactory reduction of the fracture with locking compression plate (LCP). (E) The postoperative incision. (F) At 1 year after the operation, the fracture was healed.
Postoperative rehabilitation and follow-up
After the operations, all patients were sent to the ICU for 24-h observation, and no emergency situation was found during the ICU stay. When returned to the orthopedic ward, all patients were maintained on a non-weight-bearing status on the affected side, postoperatively. The patients were encouraged to perform active and passive exercises as long as the pain could be tolerated, 3–4 days after the operation. Crutch-assisted walking was allowed at 2 weeks after the operation for type B2 and B3 fractures, and at 4 weeks for type C1 fractures. Full weight-bearing was allowed on the basis of the evidence of osseous union with follow-up radiography at about 3 months postoperatively. Follow-ups were done and pelvic radiographs were taken to evaluate the reduction and the osseous union at 1, 3, and 6 months. From the 6th month during the follow-up period, the Majeed functional evaluation scoring of all patients was performed in both groups every 6 months (at 6, 12, and 18 months). Pelvic radiographs need to be taken at 1 year after the internal fixator is taken out at 6 months after the operation.
Statistical analysis
Data analysis was performed with SPSS 19.0 statistical software (SPSS Co., USA). Measurement data are presented as mean and SD, and the t test was used for comparisons between these 2 groups, with statistical significance set as P<0.05.
Results
No iatrogenic neurovascular injury was found during the operations in these 2 groups. All 46 patients were followed up for 14–33 months (mean 24.5 months). There was no loosening or disruption of the internal fixation in either group after the operation. In the control group, malunion of a pubic rami fracture was observed in 1 patient, and incision infections were observed in 2 patients; however, after using antibiotics, the symptoms of infection in these 2 patients were controlled. There were statistically significant differences (P<0.05) in operation time, incision length, and intraoperative bleeding volume between the study group and control group.
We performed Majeed functional evaluation scoring after the operation in both groups. In the study group, the scores ranged from 64 to 94 points (81.25±8.96 points); the results were excellent in 10 patients, good in 10, and fair in 4, with an excellence rate of 83.3%. Three patients who were evaluated as fair had obvious pain in the sacroiliac joint. In the control group, the Majeed functional evaluation scores ranged from 60 to 92 points (79.59±10.33 points), with the result being rated as excellent in 10 patients, good in 8, and fair in 4, with an excellence rate of 81.8%. In 3 patients evaluated as fair, we found shortened lower extremity and limp in 1 patient and obvious pain of the sacroiliac joint in 2 patients. No statistically significant difference (P>0.05) between the 2 groups was found in the excellence rate. The times of X-ray exposures in the study group were 2–3 s (2.46±0.51), and 2–3 s in the control group as well (2.50±0.51). No statistically significant difference (P>0.05) was found between these 2 groups in durations of X-ray exposures (Table 3).
Table 3.
Comparison between the 2 groups.
| Internal fixation with pedicle screw and rod group | Internal fixation with locking compression plate group | P value | |
|---|---|---|---|
| Operation time (min) | 22.08±1.91 | 38.18±2.97 | <0.0001 |
| Incision length (cm) | 3.63±0.49 | 7.70±0.55 | <0.0001 |
| Intraoperative bleeding volume (ml) | 43.42±4.90 | 161.59±21.24 | <0.0001 |
| Times of X-ray exposures (s) | 2.46±0.51 | 2.50±0.51 | 0.78 |
| The Majeed functional evaluation score | 81.25±8.96 | 79.60±10.30 | 0.56 |
In this study, all 46 patients had different levels of anterior pelvic ring fractures. Thus, in order to minimize the damage of LCP to the surrounding tissue, in the LCP group 13 patients with bilateral pubic rami fractures or unstable unilateral pubic rami fractures were treated with combined anterior stabilization. All 24 patients in the pedicle screw-rod group were treated with combined anterior stabilization due to its minimal damage to the surrounding tissue. For poly-traumatized patients in both 2 groups, additional fractures and injuries (e.g., skin injuries, traumatic head injuries, chest trauma, femoral fractures, and tibiofibular fractures) were managed by different departments and treatment teams during the whole treatment period and good results were obtained.
Discussion
Pelvic fractures with posterior ring instability, including sacroiliac (SI) diastasis, fracture-dislocation of the SI joint, and sacral fractures are usually accompanied with vertical and rotational instability, and are regarded as unstable pelvic fractures [13–15]. Currently, surgical interventions are necessary for treating posterior pelvic ring fractures and it remains a challenge to orthopedic surgeons [6]. Various techniques, including minimally invasive pedicle screw-rod fixator, LCP, transiliac bars, percutaneous sacroiliac screws, and external fixation, have been investigated for use in posterior pelvic fixation. However, due to complicated and irregular pelvic anatomical structures, no consensus has been achieved regarding the optimal fixation for these fractures, although the treatment continues to evolve [1]. To reduce the incidences of short-term and long-term complications, such as persistence pain, abnormal gait, and dysfunction, proper reduction and fixation should be performed at an early stage. Postoperative discomfort and dysfunction might be used as predictable outcomes for detecting patients who were not treated promptly [16]. Current fixation methods still require improvements in reduction handling, soft tissue irritation, and anatomical matching between the internal fixator and pelvis.
As one of the most widely used fixation methods, LCP has the advantages of simple manipulation, less trauma, and secure fixation [17]. Biomechanical studies have been performed by previous researchers. Mehin et al. found that a locking plate used for fixing pelvic ring fractures is as strong as the conventional plate combined with lag screws. Its application can improve the treatment of pelvic ring fractures [18]. Compared to screw fixation, Sahin et al. used the locking plate to fix bilateral sacroiliac dislocations and reported achieving sufficient strength [19]. Before fixation, it is necessary to pre-bend the plate according to the irregular cortical morphology of the posterior pelvic ring; this procedure is technically demanding. However, repeatedly bending the plate may reduce its strength or even damage the threads of the screw holes, and the manual pre-bending is not always precise. Effective reduction should be first performed for the posterior ring fracture to match the plate when placing the LCP, which is also a challenge to surgeons, especially those without sufficient experience. There also is a potential risk to the blood vessels and nerves when soft tissue is stripped off [7]. The subcutaneous plate easily stimulates local soft tissue, which would further irritates the already damaged soft tissue. When in supine position, the LCP makes some patients feel uncomfortable [6]; therefore, it may be better to place it in an area with thick subcutaneous fat. Another concern is its limited reduction function, and it cannot effectively be used for reduction for the compression or separation of sacral fractures. Moreover, LCP is not suited for the fixation of bilateral iliac fractures, especially for comminuted fractures [20]. During the internal fixation procedure, fluoroscopy should be performed repeatedly to guide the correct placement of the screws. Using LCP, the operation time and the intraoperative bleeding volume were obviously increased. Hence, the insufficient reduction potential, damage to the threads of screw holes during pre-contouring procedure, and potential injury to the nerve and blood vessels, as well as the length of the incision and intraoperative bleeding volume, are the main concerns in using LCP.
In consideration of these limitations of LCP, the novel adjustable minimally invasive pedicle screw-rod fixator has obviously advantages. This fixator functions as a suspension bridge structure similar to the sacroiliac complex. When treating a posterior pelvic ring fracture accompanied with the anterior ring damage, fixation at the posterior ring using pedicle screw-rod fixator, with its arc structure, partly maintains the integrity of the pelvic ring, which can facilitate the reconstruction of osseous structure for the anterior ring as well. As a minimally invasive procedure, only 2 small incisions are needed to place this fixator during the operation, which significantly shortens the operation time and reduces intraoperative bleeding volume. The soft tissues attached to the posterior wing were not stripped off, which could avoid iatrogenic injury to nerves and blood vessels. The incisions healed well and no deep infections or wound complications occurred in the study group after surgery. A similar technique was also performed by Sar et al. [21] in a biomechanical study; 2 pedicle screws and 1 connecting bar were used to fix the posterior pelvic ring, and biomechanical testing showed satisfactory results. This device offers 2 functionalities that can be used for reducing compressed or separated fractures by adjusting the length of the connecting rod. Schildhauer et al. [22] utilized the pedicle screw-rod fixator to fix sacral fractures, which provide satisfactory outcome and sufficient biomechanical strength. With this fixator, open-book pelvic fractures can be reduced by lengthening the connected rod, while closed-book pelvic fractures can be reduced by shortening the connected rod to restore the anatomical structures. Our study results indicate that the average operation time, intraoperative bleeding volume, and the size of incision in the pedicle screw-rod fixator group were much better than in the LCP group, and we achieved satisfactory clinical and radiological outcomes in the current study. However, some concerns should also be taken into account [23,24]. First, the screw should be strong enough during the procedure of reduction and adjustment. Second, due to lack of sufficient underlying muscle in the sacroiliac area, the pedicle screw-rod used at this site should be buried in the iliac cortex to avoid skin problems when using a supine position.
For posterior combined with unstable anterior pelvic ring fracture, especially the bilateral pubic rami fractures or unstable unilateral pubic rami fractures, additional fixation of the anterior pelvic ring may have benefits. First, better pelvic ring integrity can be achieved. Second, the pain of activity after the operation will be relieved to a certain extent. For stable anterior pelvic ring fractures, as long as the fracture can be healed, no negative effects are shown in the functional outcome. To poly-traumatized patients, the main additional fractures and injuries were traumatic head injuries, chest trauma (e.g., rib fractures, pneumothorax, and traumatic hemopneumothorax), femoral fractures, and tibiofibular fractures. In the inclusion criteria, we selected patients with clear consciousness and without serious medical conditions, effectively excluding patients with serious traumatic head injuries. After the treatment for head injuries, no negative effects were found on pelvic functional outcome. After the recovery of rib fractures, pneumothorax, and traumatic hemopneumothorax, no special effects of chest trauma on pelvic functional outcome were shown, but femoral and tibiofibular fractures usually needed 6–12 months for complete recovery. During this period some effects, mainly of pain and limited mobility, were shown in the pelvic functional outcome. After 12 months, these negative effects on pelvic functional outcome were no longer obvious.
Limitations of the present study should be acknowledged. First, the sample size was relatively small and more cases should be compared by using these 2 methods to evaluate the efficacy. Second, our study lacked long-term functional results and long duration of follow-up, which need to be features of future studies, as well as biomechanical analyses between pedicle screw-rod fixator and LCP.
Conclusions
Base on the results of this study, we conclude that both of these methods can stabilize unstable posterior pelvic fractures (types B2, B3, and C1). However, use of the pedicle screw-rod fixator is less invasive, has less blood loss and greater technical safety, and can be performed more quickly. Its application can achieve good clinical and radiological outcomes, and can be a good choice for treating posterior pelvic ring fractures.
Acknowledgements
We would like to thank Christopher Nagelli for proposing some valuable suggestions to improve the process.
Footnotes
Declaration of conflicting interest
There is no special conflict of interest regarding this manuscript.
Source of support: Support for this research was provided by grants from the Shanghai Science and Technology Committee Foundation Department Major Project (Grant No. 11JC1410400); the Shanghai Health System Important Disease Joint Research Project (Grant No. 2013 ZYJB0005); the Shanghai Shenkang Hospital Development Center Clinical Management Optimization Project (Grant No. SHDC20136031), and the National Natural Science Foundation of China (No. 81272002)
References
- 1.Saiki K, Hirabayashi S, Horie T, et al. Anatomically correct reduction and fixation of a Tile C-1 type unilateral sacroiliac disruption using a rod and pedicle screw system between the S1 vertebra and the ilium: experimental and clinical case report. J Orthop Sci. 2002;7:581–86. doi: 10.1007/s007760200104. [DOI] [PubMed] [Google Scholar]
- 2.Smith W, Williams A, Agudelo J, et al. Early predictors of mortality in hemodynamically unstable pelvis fractures. J Orthop Trauma. 2007;21:31–37. doi: 10.1097/BOT.0b013e31802ea951. [DOI] [PubMed] [Google Scholar]
- 3.Dyer GS, Vrahas MS. Review of the pathophysiology and acute management of haemorrhage in pelvic fracture. Injury. 2006;37:602–13. doi: 10.1016/j.injury.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 4.Simonian PT, Routt ML, Jr, Harrington RM, et al. Biomechanical simulation of the anteroposterior compression injury of the pelvis. An understanding of instability and fixation. Clin Orthop Relat Res. 1994;309:245–56. [PubMed] [Google Scholar]
- 5.Chen HW, Liu GD, Fei J, et al. Treatment of unstable posterior pelvic ring fracture with percutaneous reconstruction plate and percutaneous sacroiliac screws: A comparative study. J Orthop Sci. 2012;17:580–87. doi: 10.1007/s00776-012-0257-1. [DOI] [PubMed] [Google Scholar]
- 6.Hao T, Changwei Y, Qiulin Z. Treatment of posterior pelvic ring injuries with minimally invasive percutaneous plate osteosynthesis. Int Orthop. 2009;33:1435–39. doi: 10.1007/s00264-009-0756-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halawi MJ. Pelvic ring injuries: Surgical management and long-term outcomes. J Clin Orthop Trauma. 2016;7:1–6. doi: 10.1016/j.jcot.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br. 1988;70:1–12. doi: 10.1302/0301-620X.70B1.3276697. [DOI] [PubMed] [Google Scholar]
- 9.Phieffer LS, Lundberg WP, Templeman DC. Instability of the posterior pelvic ring associated with disruption of the pubic symphysis. Orthop Clin North Am. 2004;35:445–49. v. doi: 10.1016/j.ocl.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 10.Cole PA, Gauger EM, Anavian J, et al. Anterior pelvic external fixator versus subcutaneous internal fixator in the treatment of anterior ring pelvic fractures. J Orthop Trauma. 2012;26:269–77. doi: 10.1097/BOT.0b013e3182410577. [DOI] [PubMed] [Google Scholar]
- 11.Gardner MJ, Mehta S, Mirza A, Ricci WM. Anterior pelvic reduction and fixation using a subcutaneous internal fixator. J Orthop Trauma. 2012;26:314–21. doi: 10.1097/BOT.0b013e318220bb22. [DOI] [PubMed] [Google Scholar]
- 12.Vaidya R, Colen R, Vigdorchik J, et al. Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: initial clinical series. J Orthop Trauma. 2012;26:1–8. doi: 10.1097/BOT.0b013e318233b8a7. [DOI] [PubMed] [Google Scholar]
- 13.Simonian PT, Routt ML., Jr Biomechanics of pelvic fixation. Orthop Clin North Am. 1997;28:351–67. doi: 10.1016/s0030-5898(05)70294-7. [DOI] [PubMed] [Google Scholar]
- 14.Bushnell BD, Dirschl DR. Small bowel obstruction from entrapment in a sacral fracture stabilized with iliosacral screws: Case report and review of the literature. J Trauma. 2008;65:933–37. doi: 10.1097/01.ta.0000197857.26410.16. [DOI] [PubMed] [Google Scholar]
- 15.Denis F, Davis S, Comfort T. Sacral fractures: An important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;227:67–81. [PubMed] [Google Scholar]
- 16.Brenneman FD, Katyal D, Boulanger BR, et al. Long-term outcomes in open pelvic fractures. J Trauma. 1997;42:773–77. doi: 10.1097/00005373-199705000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Chen W, Hou Z, Su Y, et al. Treatment of posterior pelvic ring disruptions using a minimally invasive adjustable plate. Injury. 2013;44:975–80. doi: 10.1016/j.injury.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 18.Mehin R, Jones B, Zhu Q, Broekhuyse H. A biomechanical study of conventional acetabular internal fracture fixation versus locking plate fixation. Can J Surg. 2009;52:221–28. [PMC free article] [PubMed] [Google Scholar]
- 19.Sahin O, Demirors H, Akgun RC, Tuncay IC. Internal fixation of bilateral sacroiliac dislocation with transiliac locked plate: A biomechanical study on pelvic models. Acta Orthop Traumatol Turc. 2013;47:411–16. doi: 10.3944/aott.2013.2840. [DOI] [PubMed] [Google Scholar]
- 20.Zhang Q, Chen W, Wu X, et al. Comparative study of W-shaped angular plate and reconstruction plate in treating posterior wall fractures of the acetabulum. PLoS One. 2014;9:e92210. doi: 10.1371/journal.pone.0092210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sar C, Kilicoglu O. S1 pediculoiliac screw fixation in instabilities of the sacroiliac complex: Biomechanical study and report of two cases. J Orthop Trauma. 2003;17:262–70. doi: 10.1097/00005131-200304000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Schildhauer TA, Josten C, Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: A new concept allowing early weight-bearing. J Orthop Trauma. 2006;20:S44–51. [PubMed] [Google Scholar]
- 23.Goldstein A, Phillips T, Sclafani SJ, et al. Early open reduction and internal fixation of the disrupted pelvic ring. J Trauma. 1986;26:325–33. doi: 10.1097/00005373-198604000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Hirvensalo E, Lindahl J, Bostman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res. 1993;297:28–32. [PubMed] [Google Scholar]