Abstract
Study Objectives:
The current study sought to determine whether sleep duration and change in sleep duration are associated with all-cause mortality in a community sample of middle-aged and older adults while accounting for several confounding factors including prevalent sleep-disordered breathing (SDB).
Methods:
Habitual sleep duration was assessed using self-report (< 7, 7–8, ≥ 9 h/night) at the baseline and at the follow-up visits of the Sleep Heart Health Study. Techniques of survival analysis were used to relate habitual sleep duration and change in sleep duration to all-cause mortality after adjusting for covariates such as age, sex, race, body mass index, smoking history, prevalent hypertension, diabetes, cardiovascular disease, antidepressant medication use, and SDB severity.
Results:
Compared to a sleep duration of 7–8 h/night, habitually long sleep duration (≥ 9 h/night), but not short sleep duration (< 7 h/night), was associated with all-cause mortality with an adjusted hazards ratio of 1.25 (95% confidence interval [CI]: 1.05, 1.47). Participants who progressed from short or normal sleep duration to long sleep duration had increased risk for all-cause mortality with adjusted hazard ratios of 1.75 (95% CI: 1.08, 2.78) and 1.63 (95% CI: 1.26, 2.13), respectively. Finally, a change from long to short sleep duration was also associated with all-cause mortality.
Conclusion:
Long sleep duration or a shift from long to short sleep duration are independently associated with all-cause mortality.
Citation:
Aurora RN, Kim JS, Crainiceanu C, O'Hearn D, Punjabi NM. Habitual sleep duration and all-cause mortality in a general community sample. SLEEP 2016;39(11):1903–1909.
Keywords: sleep duration, mortality
Significance.
Although habitual sleep duration has been associated with all-cause mortality, it remains to be determined whether this association is independent of the effects of sleep-disordered breathing. Moreover, little is known about how changes in sleep duration over time influence mortality. The current study utilizes polysomnographic data in a cohort of middle-aged and older men and women and demonstrates that long sleep duration is associated with all-cause mortality independent of several confounding conditions including sleep-disordered breathing. In addition, progression to habitually long sleep or curtailing sleep from long to short sleep are both independently associated with all-cause mortality. Critical gaps exist on the putative links between long sleep duration and adverse outcomes including all-cause mortality.
INTRODUCTION
Over recent years there has been considerable interest in the association between habitual sleep duration and adverse health outcomes including mortality. Substantial research has previously focused on whether optimizing sleep quantity and quality decrease medical comorbidities and improve health-related endpoints. Habitual sleep duration may, in fact, represent an important target for health promotion as it could have substantial implications for general health, comparable to other well-established risk factors such as obesity and hypercholesterolemia. Habitual sleep duration is determined by a complex interaction between multiple factors including lifestyle choices, environment, and innate biological drive. In addition, prevalent medical comorbidities can influence habitual sleep duration which, in turn, could influence the development and progression of a number of chronic conditions. In fact, accruing evidence has demonstrated an association between habitually short sleep duration and cardiovascular disease, hypertension, obesity, type 2 diabetes, and cancer.1–8 Interestingly, the predominance of available evidence suggests that both short and long sleep duration may be independent predictors of all-cause mortality, pointing to a U-shaped association between habitual sleep duration and all-cause mortality.2,3,8,9 However, interpretation of the existing literature is challenging due to several methodological limitations. For example, while most studies have accounted for surrogates of sleep-disordered breathing (SDB) such as body mass index (BMI), excessive daytime sleepiness, or self-reported snoring, evidence accounting for polysomnographically-determined SDB, in the association between sleep duration and adverse outcomes is limited.5,6,10 SDB, which may alter sleep duration by fragmenting sleep, is an independent risk factor for many of the same adverse health effects that have been noted with sleep duration including stroke, cardiovascular disease, hypertension, impaired glucose metabolism, and all-cause mortality.11–17 Thus, residual confounding by SDB makes it difficult to draw inferences from the prevailing literature about habitual sleep duration and all-cause mortality. Even more importantly, the preponderance of available studies have examined habitual sleep duration as a fixed exposure while it is well recognized that it is a time-varying behavior. The use of a single time point to represent habitual sleep duration represents an important limitation in the current state of the art and makes interpretation of the available data challenging. Thus, the overall aim of the current study was to examine whether habitual sleep duration and/or longitudinal change in sleep duration are associated with all-cause mortality after accounting for several confounding factors including prevalent comorbidities such as SDB. Using data from the Sleep Heart Health Study (SHHS), information on habitual sleep duration collected during two visits was used to test hypotheses regarding the associations between sleep duration, the change in sleep duration, and all-cause mortality.
METHODS
Study Design and Population
The SHHS is a prospective cohort study of cardiovascular consequences of SDB. Details of the study design have been reported previously.18 Briefly, between 1995 and 1998 study participants were recruited from prospective cohort studies including the Framingham Offspring and Omni Study, the Atherosclerosis Risk in Communities Study, the Cardiovascular Health Study, the Strong Heart Study, and the cohort studies of respiratory disease in Tucson and of hypertension in New York. Eligible participants were at least 40 y of age and were not being treated for SDB with positive airway pressure therapy, oral appliance, oxygen, or tracheostomy. A total of 6,441 participants completed the baseline examination. Of this group, 4,278 completed the follow-up assessments between 2000 and 2003. All study participants provided written consent and the study protocol was approved by the institutional review board of each field site.
Data Collection
All study participants completed a number of assessments at the first and at the second visits that included a detailed health interview, full-montage unattended home polysomnogram, anthropometry, measurements of blood pressure, as well as interviewer-administered questionnaires on sleep habits and prescription medication use. Prevalent cardiovascular disease was defined as a history of physician-diagnosed angina, heart failure, myocardial infarction, stroke, and coronary revascularization, determined by adjudicated surveillance data provided by the parent cohorts or by self-report at enrollment. Information on several health behaviors, such as smoking, was obtained by self-report. Anthropometric measures including weight and height were obtained along with three measurements of resting blood pressure by trained technicians. Habitual sleep duration was determined with the following question: “How many hours of sleep do you usually get at night (or your main sleep period) on weekdays or workdays?” at the two visits. Sleep duration was categorized for both visits as follows: (a) short sleep duration was defined as less 7 h/night; (b) normal sleep duration was defined as 7–8 h/night; and (c) long sleep duration was defined as ≥ 9 h/night. Further subdivisions of short sleep duration (i.e., < 5 and 6 h/night) were also examined. Results derived from analyses using these subdivisions were not materially different when compared to results obtained from using < 7 h/night to define habitually short sleep duration. Change in sleep duration between the first and second visits was modeled by constructing categories representing all possible pairs of change in sleep duration between the two visits. A total of nine subgroups that described the visit 1 to visit 2 change in sleep duration were delineated as follows: short to short (S-S), short to normal (S-N), short to long (S-L), normal to short (N-S), normal to normal (N-N), normal to long (N-L), long to short (L-S), long to normal (L-N), and long to long (L-L).
The sleep study was conducted at home using a portable monitor (P-Series, Compumedics, Abbotsford, Australia). The following signals were recorded: C3/A1 and C4/A2 electroencephalograms, bilateral electrooculograms, a single bipolar electrocardiogram, a chin electromyogram, oxyhemoglobin saturation by pulse oximetry, chest and abdominal excursion by inductance plethysmography, airflow by an oronasal thermocouple, and body position by a mercury gauge. Details of polysomnographic equipment, hookup procedures, failure rates, scoring, and quality assurance and control have been previously published.19 Apneas were identified if airflow was absent or nearly absent for at least 10 sec. Hypopneas were identified when there was at least 30% reduction in airflow or thoracoabdominal movement below baseline values for at least 10 sec associated with a 4% decrease in oxygen saturation. Apneas were further classified as obstructive if movement on either the chest or abdominal inductance channels was noted, or as central if no displacement was observed on both of these channels. The apnea-hypopnea index (AHI) was defined as the number of apneas and hypopneas per hour of sleep.
Deaths from any cause, the primary endpoint for this report, were identified and confirmed for the cohort using multiple concurrent approaches including follow-up interviews, written annual questionnaires or telephone contacts with study participants or next-of-kin, surveillance of local hospital records and community obituaries, and linkage with the Social Security Administration Death Master File as previously described.15 Using these methods, 1,509 deaths were identified in the incident cohort with a censoring date of December 7, 2011.
Statistical Analysis
Mortality rates were calculated by dividing the number of deaths by number of accumulated person-years at risk. Habitual self-reported sleep duration at the first visit was categorized as follows: < 7 h/night (short), 7–8 h/night (normal), and ≥ 9 h/ night (long). Kaplan-Meier survival curves were used to evaluate the association between sleep duration at the first visit, change in sleep duration between the two visits, and all-cause mortality. Proportional hazards regression models were then constructed to calculate unadjusted as well as adjusted hazard ratios for all-cause mortality. Age, sex, race, smoking status, and body mass index (BMI) were considered as covariates in all of the multivariable models. Age and BMI were modeled as linear terms in the primary models. Quadratic or categorical terms for age and BMI were also examined and were found to not alter the parameter estimates or overall inferences regarding sleep duration and all-cause mortality. To account for potential confounding, preexisting medical conditions such as prevalent hypertension, cardiovascular disease (angina, heart failure, myocardial infarction, stroke, and coronary revascularization), diabetes, smoking status (current, former, or never) and SDB severity at the baseline visit were considered as covariates. SDB severity was assessed using the AHI, which was considered as a continuous and categorical variable (< 5.0, 5.0–14.9, 15.0–29.9, and ≥ 30 events/h). Because the findings from the inclusion of AHI as continuous versus categorical variable were similar, AHI was included as a continuous variable. Additionally, use of antidepressant medications were used as a surrogate for depression and added to the multivariable models. Sensitivity analyses were also conducted to include the five-item mental health index from the Medical Outcomes Study 36-Item Short Form Health Survey as a surrogate marker of depression.20,21 Four final models were generated to characterize the association between habitual sleep duration at the first visit and mortality. Model 1 included age, sex, race, and BMI as covariates. Model 2 included the variables from model 1 as well as smoking status defined as never, former, or current. Model 3 added medical conditions such as prevalent hypertension, cardiovascular disease, diabetes, and SDB severity to model 2. The final model (model 4) included use of antidepressant medications and the covariates included in model 3. Interactions between age, sex, AHI, and sleep duration were included to examine the differential effects of age, sex, and AHI on the association between sleep duration and mortality. To define the influence of change in sleep duration, all of the aforementioned analyses were repeated after replacing habitual sleep duration from the first visit with a categorical variable reflecting the change in sleep duration from visit 1 to visit 2 while adjusting for baseline covariates for medical comorbidity and AHI. Finally, the effect of time-varying covariates (e.g., smoking, BMI, AHI, hypertension, diabetes, and cardiovascular disease) on the association between change in sleep duration and all-cause mortality was also assessed using the proportional hazards regression model. All analyses were conducted using STATA 13.0 (College Station, TX).
RESULTS
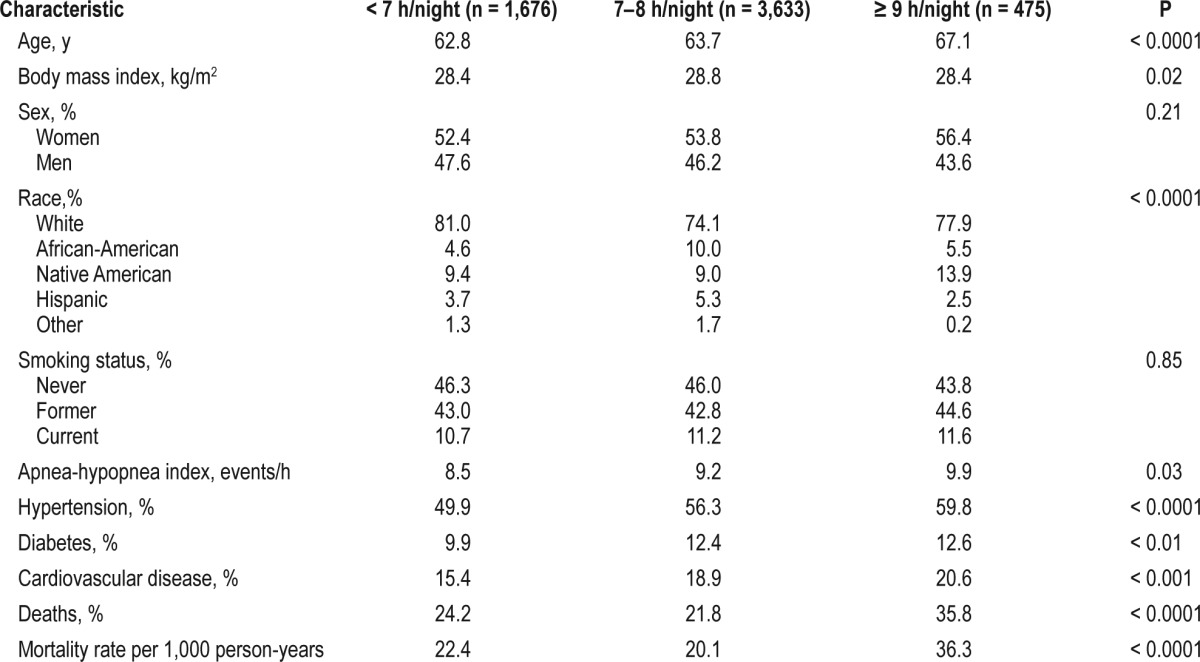
Of the 6,441 participants enrolled in the SHHS inception cohort, complete data on sleep duration and other covariates were available for 5,784 participants constituting the baseline analysis sample. The average time from the baseline visit to the end of the follow-up period was 10.8 y (standard deviation [SD] 3.2). Demographic and covariate data by sleep duration category (short, normal, long) are presented in Table 1. Significant differences in baseline covariates were observed between categories of sleep duration. Those reporting sleeping ≥ 9 h/night were older, more likely to include Native Americans, and had a higher AHI. In addition, prevalent hypertension, cardiovascular disease, and diabetes were also more common in participants with a habitual sleep duration of ≥ 9 h/night. Mortality rates also varied as function of habitual sleep duration. Over the follow-up period, there were a total of 1,509 deaths in the cohort with a mortality rate of 36.3 and 22.4 per 1,000-person years in those participants reporting ≥ 9 and < 7 h/night of habitual sleep. Not surprisingly, the group reporting normal sleep duration (7–8 h/night) had the lowest mortality rate of 20.1 per 1,000-person years.
Table 1.
Sample characteristics by self-reported sleep duration at the baseline visit.
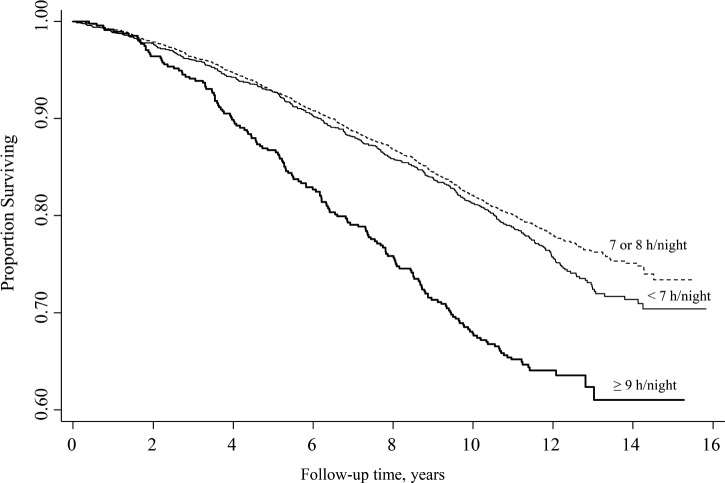
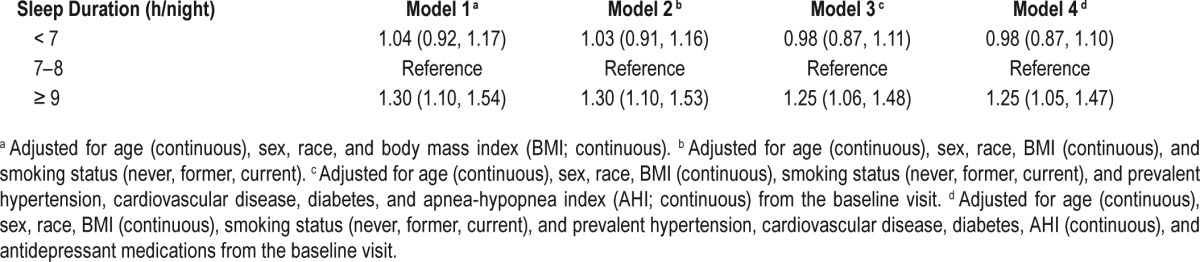
The unadjusted Kaplan-Meier survival curves by sleep duration categories as assessed during the first SHHS visit are shown in Figure 1. The follow-up period for the survival curves was from the baseline sleep study to the end of the follow-up period (average time 10.8 y). Although a small difference in the survival curves was observed between short and normal sleep duration groups (P < 0.07), participants reporting habitually long sleep duration at the first visit had the highest mortality of the three groups (P < 0.0001 for homogeneity of survival curves shown in Figure 1). Further division of those sleeping ≤ 7 h/night into subgroups (≤ 5 and 6 h/night) showed no material differences in the survival curves and thus the < 7 h/night criterion was retained to define short sleep duration. Using the normal sleep duration group as reference, the age, sex, race, and BMI adjusted hazard ratios for short and long sleep duration were 1.04 (95% confidence interval [CI] 0.92, 1.17) and 1.30 (95% CI 1.10, 1.54), respectively. After adjusting for demographic factors, prevalent health conditions, smoking status, and antidepressant medication use (a surrogate for depression), a statistically significant association was not observed between short sleep duration and all-cause mortality (model 4; Table 2). In contrast, compared to participants with normal sleep duration at the first visit, those with habitually long sleep duration had a 25% excess mortality (hazard ratio: 1.25; 95% CI 1.05, 1.47). Interactions between sleep duration and SDB severity (i.e., AHI), age, and sex were also assessed. Inclusion of such interaction terms showed no statistically signifi-cant effects, indicating that the association between baseline sleep duration and all-cause mortality was not heterogeneous across age, sex, or AHI categories.
Figure 1.
Kaplan-Meier survival curves for all-cause mortality as a function of self-reported sleep duration at the baseline visit.
Table 2.
Adjusted hazard ratios for self-reported sleep duration and all-cause mortality.
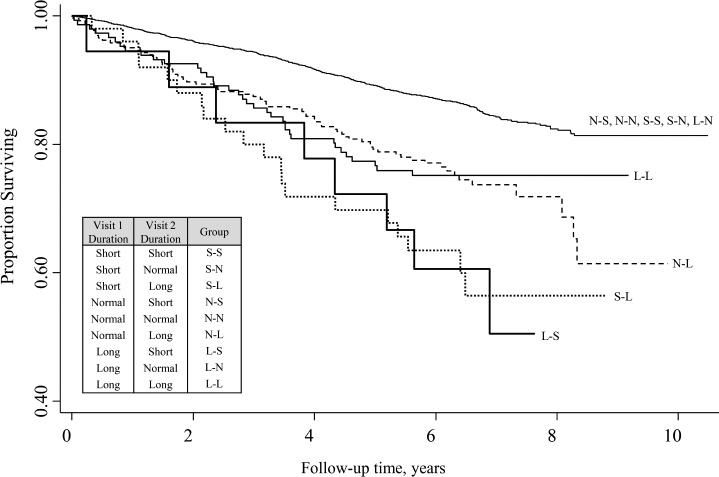
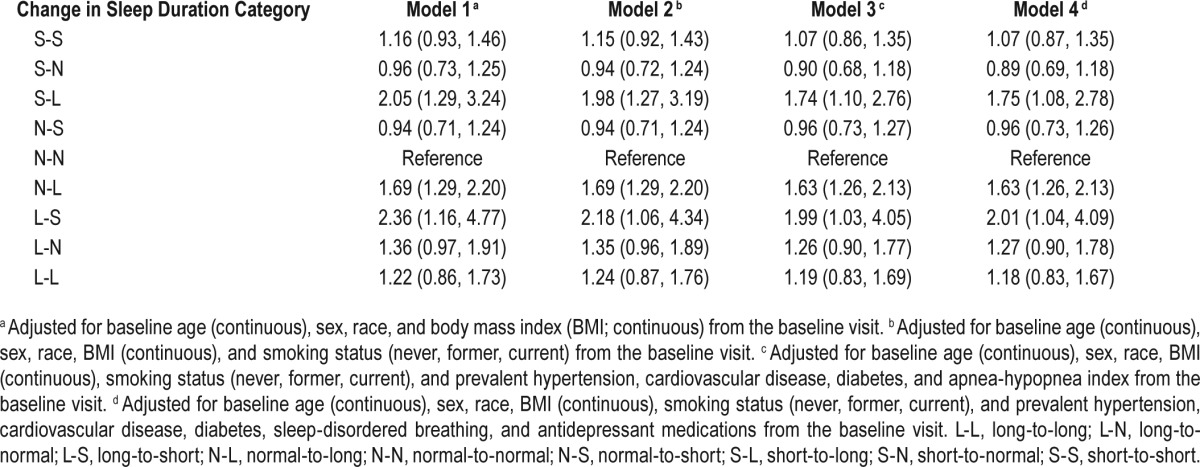
To determine whether the change in sleep duration predicted all-cause mortality, a total of 4,278 participants from the SHHS inception cohort were examined because of availability of complete data on self-reported sleep duration from both visits. The average time from the second visit to the end of the follow-up period was 5.2 y and was relatively uniform across participants with little variability (SD 0.1). Kaplan-Meier survival curves were initially constructed as a function of change in sleep duration between the baseline and follow-up visit. Because no differences in the survival curves were observed for several categories, their survival data were graphically represented as a collective group to ease exposition (Figure 2; top panel). Specific subgroups of sleep duration change had higher mortality compared to others. First, participants who reported habitually long sleep duration at both visits had a lower survival experience when compared to the other groups. Second, the survival experience was markedly worse for those extending their sleep and becoming long habitual sleepers (i.e., N-L and S-L subgroups). Finally, of all the groups, survival appeared to be the worst for participants who shortened their sleep from ≥ 9 h to under 7 h (L-S) although the sample size of that subgroup was small (n = 18). Table 3 shows the distribution of the 4,278 participants as a function of sleep duration at the first and second visits and the respective age and sex-adjusted hazard ratios for mortality in the various subgroups. To account for potential confounding, several multivariable proportional models were constructed as before (Table 4). After accounting for demographic variables, prevalent medical conditions, smoking status, anti-depressant medication use, and SDB severity at the baseline visit, a statistically significant increase in the risk for mortality was observed in participants who reported a shift from either short or normal sleep duration to long sleep duration. Specifically, there was a 75% higher mortality in participants who transitioned from short to long habitual sleep duration (hazard ratio 1.75; 95% CI 1.08, 2.78) and a 63% increase in mortality in those participants that transition from normal to long sleep duration (hazard ratio 1.63; 95% CI 1.26, 2.13). Finally, in the subgroup that transitioned from habitually long to short sleep duration, the risk for all-cause mortality was 2.01 (95% CI 1.04, 4.09) when compared to habitually normal sleepers at both time points. Sensitivity analyses were conducted by restricting the sample of 4,278 participants with follow-up data on sleep duration to only those participants who had complete data on all of the covariates, including prevalent medical comorbidity and SDB severity from repeat polysomnography (n = 2,834). Multivariable proportional hazards models were constructed as in Table 4 but with the inclusion of time-varying covariates. These models showed that the adjusted hazard ratios regarding the change in sleep duration to all-cause mortality were materially unchanged (data not shown).
Figure 2.
Kaplan-Meier survival curves for all-cause mortality as a function of change in self-reported sleep duration between the baseline and follow-up visits.
Table 3.
Age and sex-adjusted hazard ratios based on habitual sleep duration from the first and second visits.
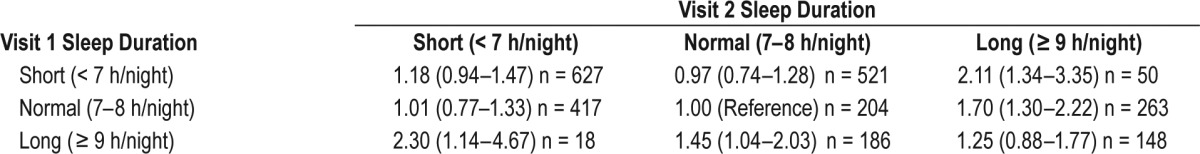
Table 4.
Adjusted hazard ratios for change in self-reported sleep duration and all-cause mortality.
DISCUSSION
The results of the current study revealed several important findings regarding the association between habitual sleep duration and all-cause mortality in a community cohort of middle-aged and older adults. First, independent of several confounding variables, including the presence and severity of SDB, habitually long sleep duration, but not short sleep duration, was associated with increased all-cause mortality. Second, change in sleep duration and specifically progression to habitually long sleep also was independently associated with all-cause mortality. Finally, study participants curtailing sleep from long (≥ 9 h/night) to short sleep duration (< 7 h/night) had an approximate doubling of their mortality risk compared with those consistently reporting normal sleep duration.
The question of how much sleep is needed to optimize health and function has been a topic of significant scientific, clinical, and public debate. Over recent years, there has been considerable controversy regarding the adverse health effects of sleeping less than 7 or 8 h/night. Part of the challenge in delineating the public health burden imposed by short sleep duration is the conflicting evidence derived from several large cohort studies across different countries.7,8,22,23 For example, in the seminal study of over 1 million people, Kripke and coworkers8 reported an independent association between short and long sleep duration and mortality after accounting for demographic variables, prescription sleep medication use, prevalent medical comorbidities, and health habits. Similarly, work by Gangwisch et al.4 also showed that both short and long sleep duration are associated with mortality. However, the finding of a higher mortality in the study by Gangwisch et al. was only observed in older (60–86 y) but not middle-aged adults (32–59 y). Differences in inferences about sleep duration across available studies may be, in part, due to demographic variability of the cohorts examined as well as possibility of differential effects of short sleep duration. Indeed, differential susceptibility to the effects of short or long sleep duration have been noted in a number of population subsets. For example, extremes of sleep duration are associated with mortality in those with preexisting illnesses and functional limitations whereas no such association is observed in those without these conditions.24 Part of the susceptibility to the effects of varying sleep duration may be related to sex given that some studies have reported an association between short sleep duration and mortality in men but not women.25,26 Variability in defining habitually short sleep across different studies could also help explain the inconsistencies in the available literature. Studies that have used extreme thresholds to define “short” sleep duration (e.g., < 5 h/night) have found associations with mortality but even in these studies the magnitude of association is, at best, modest.7,10 Countering the weight of studies that have shown an independent association with short sleep duration and all-cause mortality, there are at least an equal number of studies that have not found such an association,2,3 especially after accounting for inflammatory markers and other health factors.27 The current analysis of the SHHS data are in line with the latter group of studies that do not support an association between short sleep duration and mortality. It is also certainly possible that survival bias could explain the lack of association between short sleep duration and mortality because the SHHS recruited participants that were being followed in other epidemiological studies of respiratory and cardiovascular disease.
The fact that an association was found between long sleep duration and mortality indicates that perhaps there is a “J-shaped” rather than “U-shaped” association between sleep duration and mortality, a finding that has been previously reported by others.22,23 In fact, a comprehensive assessment of the literature on sleep duration substantiates a strong and consistent association between habitually long sleep duration and mortality.2,3 This observed association is thought to possibly reflect confounding by subclinical or unmeasured disease,28 and in particular, SDB.23 The effect of objectively defined SDB in the context of sleep duration and mortality has not been previously described. It has been hypothesized that because SDB may be associated with sleep fragmentation and unrefreshing sleep, individuals with SDB may extend their total sleep time to compensate for worse sleep quality.29 The results herein suggest that SDB does not confound the association between long sleep duration and mortality and addresses an important deficiency in the existing literature.
Very few studies have examined the potential influence of longitudinal changes in sleep duration and health outcomes including all-cause mortality.30–32 A persistent pattern of short sleep duration32 or transitioning into a short or long sleeper30,31 has been associated with increased mortality. In the current study, a strong association was observed between all-cause mortality and transitioning to short sleep duration subsequent to initially reporting long sleep duration. However, the small sample size makes it challenging to make inferences about this particular subgroup. It is worth noting that in people progressing to short from normal sleep duration, a statistically significant association with mortality was not seen despite an adequate sample size. Additionally, the current study suggests that extension of sleep duration to ≥ 9 h also predicts mortality even after adjustment for multiple covariates and potential confounders, including SDB.
There are a number of strengths and limitations of the current study that merit consideration. Strengths include the fairly large and diverse community-based sample that increases the generalizability of the results, the availability of objectively defined SDB, the inclusion of a number of important demographic and health-related covariates, a relatively long follow-up period, and the longitudinal assessment of sleep duration as a correlate of all-cause mortality. Limitations include potential misclassification resulting from lack of objectively measured sleep, the possibility of residual confounding from unmeasured health conditions, and the inclusion of only middle-aged and older adults. In addition, given the fact that analyses of sleep duration and mortality were based on workday sleep duration, misclassification of habitual sleep duration is certainly possible as sleep extension on the weekends and nap duration were not considered. Furthermore, data on retirement, which is commonly associated with a transition to longer sleep, were not available. Such information would help delineate whether long sleep duration is related to incipient disease or a psychosocial event. Finally, cause-specific mortality (e.g., cancer death, stroke death) was not available for the cohort and thus inferences regarding how sleep duration could increase mortality are not possible. These limitations notwithstanding, the results presented help to fill an important gap in the existing literature regarding the association between sleep duration and all-cause mortality.
Sleep is a fundamental, physiological function and a critical component of good health. Although a considerable number of prospective, observational studies have tried to determine the amount of sleep necessary to optimize health, several inherent challenges remain that need to be addressed. For example, accurate quantification of actual sleep remains a challenge and pathways that could mediate the association between sleep duration and mortality, especially long sleep duration, need to be delineated. The amalgamation of evidence has adjusted for numerous covariates, yet a robust association between long sleep duration and mortality persists. However, it remains unclear if long sleep duration is truly a risk factor for adverse outcomes or an indicator of subclinical disease causing higher mortality. Clearly, the amount of sleep necessary to optimize health needs to be better understood and elucidated.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Punjabi has received grant support from Resmed and Respironics for research unrelated to the current manuscript. The other authors have indicated no financial conflicts of interest. The Sleep Heart Health Study was supported by the following National Heart, Lung and Blood Institute (NHLBI) cooperative agreements: U01HL53940 (University of Washington), U01HL53941 (Boston University), U01HL53938 (University of Arizona), U01HL53916 (University of California, Davis), U01HL53934 (University of Minnesota), U01HL53931 (New York University), U01HL53937 and U01HL64360 (Johns Hopkins University), U01HL63463 (Case Western Reserve University), and U01HL63429 (Missouri Breaks Research). Dr. Aurora is supported by a NHLBI K23 HL118414. Dr. Punjabi is supported by NIH grants R01 HL075078 and R01 HL117167.
REFERENCES
- 1.Amagai Y, Ishikawa S, Gotoh T, Kayaba K, Nakamura Y, Kajii E. Sleep duration and incidence of cardiovascular events in a Japanese population: the Jichi Medical School cohort study. J Epidemiol. 2010;20:106–10. doi: 10.2188/jea.JE20090053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18:148–58. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 4.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28:1289–96. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 5.Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165:863–7. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- 6.Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29:1009–14. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 7.Ikehara S, Iso H, Date C, et al. Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Sleep. 2009;32:295–301. doi: 10.1093/sleep/32.3.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 9.Zawisza K, Tobiasz-Adamczyk B, Galas A, Brzyska M. Sleep duration and mortality among older adults in a 22-year follow-up study: an analysis of possible effect modifiers. Eur J Ageing. 2015;12:119–29. doi: 10.1007/s10433-014-0318-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel SR, Zhu X, Storfer-Isser A, et al. Sleep duration and biomarkers of inflammation. Sleep. 2009;32:200–4. doi: 10.1093/sleep/32.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gottlieb DJ, Yenokyan G, Newman AB, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122:352–60. doi: 10.1161/CIRCULATIONAHA.109.901801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marin JM, Agusti A, Villar I, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012;307:2169–76. doi: 10.1001/jama.2012.3418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Connor GT, Caffo B, Newman AB, et al. Prospective study of sleep-disordered breathing and hypertension: the Sleep Heart Health Study. Am J Respir Crit Care Med. 2009;179:1159–64. doi: 10.1164/rccm.200712-1809OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Punjabi NM, Shahar E, Redline S, Gottlieb DJ, Givelber R, Resnick HE. Sleep-disordered breathing, glucose intolerance, and insulin resistance: the Sleep Heart Health Study. Am J Epidemiol. 2004;160:521–30. doi: 10.1093/aje/kwh261. [DOI] [PubMed] [Google Scholar]
- 15.Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6:e1000132. doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Redline S, Yenokyan G, Gottlieb DJ, et al. Obstructive sleep apneahypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010;182:269–77. doi: 10.1164/rccm.200911-1746OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yeboah J, Redline S, Johnson C, et al. Association between sleep apnea, snoring, incident cardiovascular events and all-cause mortality in an adult population: MESA. Atherosclerosis. 2011;219:963–8. doi: 10.1016/j.atherosclerosis.2011.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quan SF, Howard BV, Iber C, et al. The Sleep Heart Health Study: design, rationale, and methods. Sleep. 1997;20:1077–85. [PubMed] [Google Scholar]
- 19.Redline S, Sanders MH, Lind BK, et al. Methods for obtaining and analyzing unattended polysomnography data for a multicenter study. Sleep Heart Health Research Group. Sleep. 1998;21:759–67. [PubMed] [Google Scholar]
- 20.Cuijpers P, Smits N, Donker T, ten Have M, de Graaf R. Screening for mood and anxiety disorders with the five-item, the three-item, and the two-item Mental Health Inventory. Psychiatry Res. 2009;168:250–55. doi: 10.1016/j.psychres.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 21.Friedman B, Heisel M, Delavan R. Validity of the SF-36 five-item Mental Health Index for major depression in functionally impaired, community-dwelling elderly patients. J Am Geriatr Soc. 2005;53:1978–85. doi: 10.1111/j.1532-5415.2005.00469.x. [DOI] [PubMed] [Google Scholar]
- 22.Cai H, Shu XO, Xiang YB, et al. Sleep duration and mortality: a prospective study of 113 138 middle-aged and elderly Chinese men and women. Sleep. 2015;38:529–36. doi: 10.5665/sleep.4564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Castro-Costa E, Dewey ME, Ferri CP, et al. Association between sleep duration and all-cause mortality in old age: 9-year follow-up of the Bambui Cohort Study, Brazil. J Sleep Res. 2011;20:303–10. doi: 10.1111/j.1365-2869.2010.00884.x. [DOI] [PubMed] [Google Scholar]
- 24.Magee CA, Holliday EG, Attia J, Kritharides L, Banks E. Investigation of the relationship between sleep duration, all-cause mortality, and preexisting disease. Sleep Med. 2013;14:591–6. doi: 10.1016/j.sleep.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 25.Amagai Y, Ishikawa S, Gotoh T, et al. Sleep duration and mortality in Japan: the Jichi Medical School Cohort Study. J Epidemiol. 2004;14:124–8. doi: 10.2188/jea.14.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kojima M, Wakai K, Kawamura T, et al. Sleep patterns and total mortality: a 12-year follow-up study in Japan. J Epidemiol. 2000;10:87–93. doi: 10.2188/jea.10.87. [DOI] [PubMed] [Google Scholar]
- 27.Hall MH, Smagula SF, Boudreau RM, et al. Association between sleep duration and mortality is mediated by markers of inflammation and health in older adults: the Health, Aging and Body Composition Study. Sleep. 2015;38:189–95. doi: 10.5665/sleep.4394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stamatakis KA, Punjabi NM. Long sleep duration: a risk to health or a marker of risk? Sleep Med Rev. 2007;11:337–9. doi: 10.1016/j.smrv.2007.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bliwise DL, King AC, Harris RB. Habitual sleep durations and health in a 50-65 year old population. J Clin Epidemiol. 1994;47:35–41. doi: 10.1016/0895-4356(94)90031-0. [DOI] [PubMed] [Google Scholar]
- 30.Ferrie JE, Shipley MJ, Cappuccio FP, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30:1659–66. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heslop P, Smith GD, Metcalfe C, Macleod J, Hart C. Sleep duration and mortality: the effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women. Sleep Med. 2002;3:305–14. doi: 10.1016/s1389-9457(02)00016-3. [DOI] [PubMed] [Google Scholar]
- 32.Hublin C, Partinen M, Koskenvuo M, Kaprio J. Sleep and mortality: a population-based 22-year follow-up study. Sleep. 2007;30:1245–53. doi: 10.1093/sleep/30.10.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.