Abstract
Birth defects resulting from diabetic pregnancy are associated with apoptosis of a critical mass of progenitor cells early during the formation of the affected organ(s). Insufficient expression of genes that regulate viability of the progenitor cells is responsible for the apoptosis. In particular, maternal diabetes inhibits expression of a gene, Pax3, that encodes a transcription factor which is expressed in neural crest and neuroepithelial cells. As a result of insufficient Pax3, cardiac neural crest and neuroepithelial cells undergo apoptosis by a process dependent on the p53 tumor suppressor protein. This, then provides a cellular explanation for the cardiac outflow tract and neural tube and defects induced by diabetic pregnancy.
Keywords: Diabetic pregnancy, Congenital defects, Neural tube defect, Cardiac outflow tract defect, Apoptosis, Oxidative stress, Pax3, p53
Introduction
The offspring of women with diabetes mellitus are at significantly increased risk of congenital malformation [1–9]. While improvements in diabetes control in recent decades have reduced the incidence of this diabetic complication, referred to as “diabetic embryopathy”, malformations are still up to five times more common in diabetic pregnancies than in nondiabetic pregnancy [6, 8, 10–13]. The malformations are induced early during organogenesis, therefore, they only occur in pregnancies in which maternal diabetes, either type 1 (T1DM) or type 2 (T2DM), is present at the onset of pregnancy. Gestational diabetes, which is associated with insulin resistance brought on in the latter half of pregnancy, does not induce structural malformations because it occurs after the period of organogenesis [14]. While some studies have observed an increase in malformations in pregnancies diagnosed with gestational diabetes, it is thought that these women actually had T2DM before pregnancy that had not been diagnosed [1, 13]. Maternal obesity prior to pregnancy also increases the incidence of malformations [15–18]. However, it is not clear whether obese women whose offspring developed malformations had undiagnosed T2DM [19], or whether other metabolic disturbances might be responsible. For example, adequate folic acid availability has been recognized for several years to reduce the risk for neural tube, and other, defects [20–22]. There is evidence that obese women are less likely to take folic acid supplements or to consume a diet rich in nutrients such as folate [23, 24]. As well, a study of postmenopausal women revealed that serum folate levels are inversely related to body fat composition [25].
Almost any organ system is susceptible to malformation during diabetic pregnancy [5, 26–29]. However, neural tube defects (NTD), including spina bifida and anencephaly, and cardiovascular defects, especially cardiac outflow tract defects (COTD), transposition of the great arteries, and atrial or ventricular septal defects, are the most common to occur [5, 6, 26]. The malformations are induced at the earliest stages of organogenesis, prior to the seventh week of gestation in humans [30].
Several investigators have employed rodent models to study the effects of diabetic pregnancy, or in vitro culture in high glucose-containing media, on postimplantation embryonic development [31–37]. In general, these models result in malformation of craniofacial structures and the neural tubes and growth retardation. There are several biochemical disturbances that have been proposed to play a role in the defective development, such as increased protein kinase C activity [38–40], decreased arachidonic acid uptake [41, 42], defective prostaglandin synthesis [43, 44], PPAR signaling [45–48], random DNA mutations [49, 50], and oxidative stress [37, 51–55]. However, none of these studies revealed how these biochemical disturbances could disturb morphogenesis.
Orderly cell death regulates normal processes in metazoan embryogenesis such as dorsoventral patterning of the neural tube, bone formation, fusion of the oral palate and neural tube, and craniofacial development [56–65]. Inappropriate cell death, on the other hand, has the potential to lead to defective development. Indeed, apoptosis has been associated with teratogens such as ethanol, retinoic acid, hypoxia, ionizing radiation, and hyperthermia [66], and, as described in this review, maternal diabetes. A critical question that needs to be answered is, how does apoptosis in response to maternal diabetes (or any teratogen) occur in a targeted fashion? Otherwise, if all cells of the embryo underwent cell death, the entire embryo would die; alternatively, if only a portion of the cells of all structures of the embryo underwent cell death, the embryo would be small for gestational age, but structurally normal. In this review, the mechanisms by which apoptosis in neural crest and neural tube progenitors occurs and causes malformation of the cardiac outflow tracts and neural tube will be discussed.
Altered gene expression in embryos of diabetic mice leads to apoptosis and malformations
Altered expression of Pax3 in mouse embryos of diabetic mothers
The Pax gene family encodes transcription factors that are primarily expressed during development. The mammalian Pax genes were identified by the presence of a highly conserved 384 bp sequence encoding a DNA-binding paired box that was originally discovered in the Drosophila segmentation genes, paired (prd), gooseberry-proximal (gsb-p), and gooseberry-distal (gsb-d), and tissue-specific genes, Pox meso and Pox neuro [67–70]. There are nine known mammalian Pax genes. They are grouped into four classes based on their paired domain homology, the presence or absence of a complete or partial homeodomain, and the presence or absence of a conserved octapeptide [68, 71]. In contrast to the Hox genes, which are expressed in a region-specific anterior–posterior pattern, the Pax genes may be expressed along the entire anterior–posterior axis, or in a tissue-specific fashion. Paired box genes have been found in several animal phyla from nematodes to vertebrates [67, 70]. Pax3 is expressed in the vertebrate neural tube, neural crest, and somitic mesoderm; expression in mice begins in the dorsal region of the neural folds on day 8.5 [72]. Mutations in the DNA-binding domains of human PAX3 are associated with Waardenburg syndrome type I, which involves lateral displacement of the medial canthus of the eye, aniridia, white forelock, and congenital deafness [73–75]. The mouse Splotch alleles map to the Pax3 locus [73, 76–79]. Pax3Sp/Sp embryos develop NTD (exencephaly, spina bifida, or both), lack skeletal musculature, and exhibit defects in neural crest-derived cell populations [80, 81]. Defective cardiac neural crest (CNC) development leads to COTD; embryos die of cardiac failure by day 14.5, probably due to impaired formation of conductive tissue of the heart, another process which is dependent on CNC [81–85]. Notably, NTD and COTD are among the most common defects induced by diabetic pregnancy in humans [6, 26]. Heterozygous Splotch (Pax3+/Sp) embryos are viable and do not develop the structural defects that occur in Pax3Sp/Sp embryos, although in pigmented strains, they develop white “splotches” of fur on the belly, due to deficiency of neural crest-derived melanocytes.
The morphological similarity between the NTD and COTD in embryos of diabetic mice, in which insulin-deficient diabetes had been induced by the pancreatic β cell toxin, streptozotocin (STZ), and Pax3Sp/Sp embryos [86, 87], suggests that diabetic embryopathy phenocopies the effects of Pax3 mutation. This appears to be due to inhibition of Pax3 expression, as Pax3 expression is significantly reduced in embryos of diabetic mice as determined by in situ hybridization and reverse transcription-PCR (RT-PCR) of day 8.5 embryos [86]. Pax3 expression is also reduced in migrating neural crest and somites on days 9.5 and 10.5, as demonstrated by in situ hybridization [86], although, as described later, the decreased expression of Pax3 in neural crest is probably due to prior elimination of these cells by apoptosis [87]. These observations indicate that congenital malformations induced during diabetic pregnancy appear to be caused by misexpression of genes that control essential developmental processes. While there may be many genes whose expression could be affected by maternal diabetes, inasmuch as Pax3 deficiency is sufficient to cause malformation Pax3-expressing structures, simply inhibiting its expression below a critical threshold during diabetic pregnancy is sufficient to induce defects of Pax3-dependent structures.
Pax3 inhibits cell death
While Pax3 loss-of-function leads to deficient development of dependent structures, Pax3 gain-of-function is associated with immortalization or unregulated proliferation. For example, several of the Pax genes induce transformation when stably expressed in fibroblasts [88]. Many forms of pediatric alveolar rhabdomyosarcoma are associated with a rearrangement of the PAX3 gene, leading to expression of a fusion protein containing the DNA-binding domain of PAX3 and the trans-activation domain of Forkhead [89–92]. PAX3 is also expressed in many neural crest-derived tumors, such as neuroblastoma and melanoma, and is associated with an aggressive malignant phenotype and poor prognosis [93–98]. Notably, knocking down PAX3 (or PAX3-Forkhead) mRNA with antisense oligonucleotides induces cell death [98–100]. PAX3 also is crucial for proliferation of melanocytes in response to UV light [101]. These observations suggest that Pax3 may prevent cell cycle withdrawal, and/or cell death.
In embryos of diabetic mice and Pax3Sp/Sp embryos, neuroepithelial cells of the neural folds undergo apoptosis [86]. This indicates that elimination of the cells on the leading edges of neural folds halted neural tube closure. More recently, the depletion of migrating CNC cells in embryos of diabetic mice and Pax3LacZ/LacZ embryos (carrying LacZ reporters transcribed under the control of Pax3 control elements, but which disrupt Pax3 3 coding sequences) was also shown to be associated with increased apoptosis [87, 102]. These observations indicate that during normal embryogenesis, Pax3 prevents neuroepithelial and neural crest apoptosis. Sulik noted that cells that would normally be rapidly proliferating were more susceptible to apoptosis during the pathogenesis of malformations [66]. Rapid proliferation is a common feature that drives the movement of the neural folds toward each other and the migration of neural crest toward their destinations [103, 104]. Thus, if Pax3 is necessary for proliferation of neural crest and neuroepithelial cells, insufficient expression of Pax3 could lead to apoptosis. This, then, explains how selective apoptosis, leading to congenital malformations, can occur.
Additional evidence for apoptosis in animal models of diabetic embryopathy has been obtained in recent years. For example, increased numbers of apoptotic cells have been observed within the fused neural tubes of day 11.5–13.5 mouse embryos [105–107]. However, these observations of apoptosis were scattered, and were observed after neural tube fusion, suggesting that they may be involved in further maturation of the CNS, rather than NTD. Maternal diabetes also increases the incidence of apoptosis in the mandible, a neural crest derivative, of day 11 rat embryos [108], and in the endocardial cushion of day 13.5 mouse embryos [109]. Abnormal temporal-spatial pattern of apoptosis during remodeling of pharyngeal arch arteries has also been noted in day 12.0–14.5 rat embryos of diabetic mothers [110]. This is likely to reflect the disturbances in cardiac outflow tract septation that is dependent on CNC cells, rather than a direct effect of maternal diabetes on apoptosis of progenitor cells. Pervasive apoptosis has also been observed in day 10 rat embryos of diabetic mothers [111]. However, these embryos were also growth retarded and developmentally delayed. Thus, there may be conditions, in which the intrauterine diabetic exposure induces global cell death. This is likely to result in fetal demise, rather than specific structural malformation.
Mechanisms by which maternal diabetes disrupts Pax3 gene expression
The current understanding of how diabetic pregnancy disrupts Pax3 gene expression is discussed briefly here. A more detailed description has been recently reported [112].
Excess glucose transported to the embryo is responsible for the adverse effects of diabetic pregnancy on embryogenesis
Many metabolic disturbances that occur during T1DM or T2DM, including hyperglycemia, β-hydroxybutyrate, somatomedin inhibitors, and hyper- or hypoinsulinemia, have been considered to be responsible for diabetic embryopathy [32–34, 113, 114]. However, hyperglycemia is the only common feature of T1DM and T2DM. The offspring of women with either T1DM or T2DM are prone to the same kinds of defects, and the risk for spontaneous abortion or congenital malformations is correlated with poor glycemic control [9, 11, 13, 115–117]. In the rat, glucose concentration in embryo neuroepithelium reaches equilibrium with glucose concentration in maternal serum [118]. Indeed, we have shown, both in vivo and in vitro, that excess glucose delivered to the embryo is necessary and sufficient to inhibit Pax3 expression, and induce neuroepithelial apoptosis and NTD [119]. Transient hyperglycemia before the onset of Pax3 expression is also sufficient to induce CNC apoptosis and COTD [87]. The early embryo expresses the high Km Glut2 glucose transporter [120]. Thus, Glut2 would rapidly transport glucose into embryo cells when glucose concentrations are above its Km (~15 mM), as can occur during episodes of hyperglycemia. Expression of Glut2 is essential for embryo susceptibility to hyperglycemia-induced NTD [121]. Thus, excess glucose delivery to the embryo appears to be responsible for the adverse effects of pregnancies affected by either T1DM or T2DM on embryo development.
Oxidative stress mediates the effects of high glucose to inhibit Pax3 expression, thereby inducing apoptosis
Excess glucose metabolism increases the production of superoxide by the electron transport chain; if these free radicals are not scavenged, oxidative stress will result [122]. There is ample experimental support that oxidative stress contributes to malformations in animal models exposed to a high glucose milieu [37, 51–55]. In addition to increased superoxide production from increased oxidative metabolism, the pathways responsible for oxidative stress are complex; they include decreased expression of γ-glutamyl-cysteine synthetase, which would decrease production of the antioxidant, reduced glutathione (GSH) [123, 124], and increased activity of the hexosamine flux pathway and diacylglycerol/protein kinase C signaling [40, 125]. Both of these latter pathways would decrease production of NADPH, which is needed to produce GSH from oxidized glutathione (GSSG). In addition, the increased oxygen consumption caused by increased glucose metabolism creates a relative state of hypoxia in embryos, which, in turn, increases superoxide production [126].
Oxidative stress may lead to oxidation of proteins, lipids, and DNA and can induce apoptosis [127]. However, if oxidative stress resulting from excess glucose metabolism was directly responsible for cell death, all cells of the embryo would be equally susceptible. Rather than inducing limited defects in organogenesis, the entire embryo would be affected. However, oxidative stress inhibits expression of Pax3 in vivo and in vitro, and activation of pathways that contribute to oxidative stress, such as hexosamine flux and hypoxia, also inhibit Pax3 expression [125, 126, 128]. Importantly, oxidative stress which is sufficient to inhibit Pax3 expression is not sufficient to induce DNA strand breaks [128]. Thus, the oxidative stress induced by diabetic pregnancy appears to induce apoptosis in a cell-selective fashion, leading to specific malformations, by inhibiting expression of genes which regulate cell viability in a cell-selective fashion. The biochemical and molecular mechanisms by which oxidative stress inhibits expression of Pax3 still remain to be elucidated. However, the window of susceptibility in the mouse embryo is approximately 24 h before the onset of Pax3 expression [87, 102, 126, 128].
Could inhibition of Pax3 expression or Pax3-dependent processes be a common cause of NTD?
Ionizing radiation and certain anticonvulsant drugs increase risk for NTD and increase oxidative stress [129, 130]. Thus, it is possible that inhibition of Pax3 expression is a common mechanism leading to NTD in response to various sources of oxidative stress.
Folic acid might also affect Pax3 expression, or complement Pax3-dependent processes. Folic acid increases the conversion of homocysteine, which is an oxidant, to methionine, and folic acid is reported to have antioxidant properties independent of lowering homocysteine levels [131–133]. Thus, folic acid may prevent the generation of oxidative stress, as well as contribute to suppression of endogenous oxidative stress. Folic acid has been reported to reduce the incidence of malformations in rodent models of diabetic pregnancy [134, 135]. This could be explained by the effects of folic acid to reduce oxidative stress. However, it has also been reported that folic acid can suppress NTD in Pax3Sp2H/Sp2H embryos [136]. This would indicate that a folic acid-dependent process(es) might be regulated by Pax3, or that Pax3 and folic acid both regulate a common developmental process. On the other hand, folic acid was not found to suppress NTD in Pax3Sp/Sp embryos [137]. The differences between the compensatory effects of folic acid in Pax3Sp2H/Sp2H and Pax3Sp/Sp embryos could be explained by differential penetrance of the Splotch2H and Splotch mutations on NTD. However, it should be noted that the Pax3Sp/Sp embryos whose mothers had been treated with folic acid were examined on day 18.5 [137]. Since Pax3Sp/Sp embryos are not normally viable past day 14.5 due to cardiac insufficiency [81], this suggests that folic acid might have compensated for Pax3 deficiency with regard to CNC development. It still needs to be resolved whether folic acid could be involved in pathways distal to Pax3 during neural tube closure.
With regard to diabetic pregnancy, one study found that folic acid deficiency or aberrant metabolism does not explain increased defects in human pregnancies affected by pre-gestational T1DM or T2DM [138]. However, further research is needed to investigate whether folic acid regulates Pax3 expression or Pax3 downstream effects, and whether folic acid requirements might be greater in diabetic pregnancies.
The p53 tumor suppressor protein mediates effects of Pax3 deficiency in neuroepithelium and neural crest
Inactivating p53 prevents apoptosis, NTD, and COTD in Pax3-deficient embryos
The observation that apoptosis was increased in neuro-epithelium of embryos of diabetic mice or Pax3Sp/Sp embryos suggested either that Pax3 inhibits apoptosis, or else, that if a Pax3-dependent development fails, cells undergo apoptosis. Evidence in support of the former mechanism, and specifically, that Pax3 inhibits apoptosis that is regulated by the p53 tumor suppressor protein, was obtained by inactivating p53 by either genetic or chemical means [139]. By crossing mice with a germline p53 mutation [140] with Pax3+/Sp mice to generate Pax3Sp/Sp p53−/− embryos, or treating pregnant Pax3+/Sp mice with pifithrin-α, an inhibitor of p53 nuclear and mitochondrial translocation [141–143], it was demonstrated that apoptosis and NTD failed to occur in Pax3Sp/Sp embryos in which p53 was inactivated [139]. This indicated that Pax3 is not required to direct expression of genes that control neural tube closure, but it is required to block p53-dependent apoptosis.
A role of Pax3 to inhibit p53-dependent apoptosis during CNC migration and cardiac outflow tract septation has recently been reported [102]. Pax3Sp/Sp embryos exhibit defects in CNC migration and outflow tract septation [81]. CNC cells arise from neuroepithelium between the midotic placode and the third somite, make an epithelial to mesenchymal transformation, and migrate through pharyngeal arches 3, 4, and 6 to the primitive, single outflow tract of the heart [144, 145]. CNC are required for septation of the cardiac outflow tract into the aorta and pulmonary arteries [146–148]. Mouse embryos with mutant Splotch alleles develop COTD, but it has been disputed whether the onset of CNC migration was delayed, whether either the numbers of migrating cells or rate of migration was reduced, or whether migration was normal, but CNC inductive properties on the vascular was defective [83–85, 144, 149]. Using Pax3LacZ/LacZ mouse embryos, it was recently shown that the onset of CNC migration is normal, but that during day 9.0–9.5, there are progressively fewer CNC that can be detected. Instead, there are progressively more apoptotic cells where CNC would normally be detected [102]. This indicated that Pax3 is not required for the initiation of CNC migration, but it is required for CNC viability while they are migrating toward the heart. Notably, both CNC apoptosis and COTD failed to occur in Pax3LacZ/LacZ embryos that were p53-null, or whose mothers had been treated with a p53 inhibitor [102]. This indicated that, as in the neural tube, Pax3 is not needed to induce genes which regulate CNC migration or outflow tract septation, but it is needed to prevent p53-mediated CNC apoptosis during CNC migration. It should be noted that, although development of Pax3-expressing somitic derivatives was defective, this was not associated with increased apoptosis, and defective skeletal muscle development was not prevented by inactivating p53. In fact, Pax3LacZ/LacZ fetuses that were p53-null, or whose mothers had been treated with a p53 inhibitor, survived and displayed normal heart development when examined on day 18.5, the day before normal term delivery, however, they are not viable, probably due failure of skeletal muscles required for respiration to develop [102]. This suggests that Pax3 regulates other processes instead of, or in addition to, inhibition of p53 in somites.
Time course of developmental effects of maternal diabetes to induce apoptosis, NTD, and COTD
Use of chemical agents to induce or inhibit oxidative stress, or inhibit p53-dependent apoptosis, at specific times of gestation, has elucidated the approximate stages of development which are susceptible to perturbations in glucose metabolism or Pax3 insufficiency:
Day 7.5: the primitive streak forms. Transient hyperglycemia (or oxidative stress or hypoxia) inhibits processes necessary to induce expression of Pax3 [119, 126, 128].
Day 8.5: Pax3 expression, neural tube closure, and neural crest migration begins [72]. Pax3 expression is significantly reduced in pregnancies in which hyperglycemia, or oxidative or hypoxic stress was induced on day 7.5, even though blood glucose or markers of oxidative stress have returned to normal [119, 126, 128]. Nuclear and/or mitochondrial translocation of p53 must be inhibited within approximately the first 4 h of Pax3 expression (approximately noon-4:00 p.m. on day 8.5) [102].
Day 9.0–9.5: defective CNC migration and apoptosis are detectable in embryos whose Pax3 expression was inhibited or are expressing null Pax3 alleles; these defects do not occur if p53-dependent processes were inhibited on day 8.5 [87, 102].
Day 10.5: defective neural tube closure and apoptosis are detectable in embryos whose Pax3 expression was inhibited or are expressing null Pax3 alleles; these defects do not occur if p53-dependent processes were inhibited on day 8.5 [119, 150].
Days 9.5–12.5 CNC cells migrate to the heart and participate in septation of the single outflow tract into the aorta and pulmonary arteries. Outflow tract septation fails in embryos whose CNC had undergone apoptosis prior to reaching the heart, and fetuses die by day 14.5. Inhibiting p53-dependent processes on day 8.5 rescues cardiac outflow tract septation and fetal viability in Pax3-deficient fetuses [102].
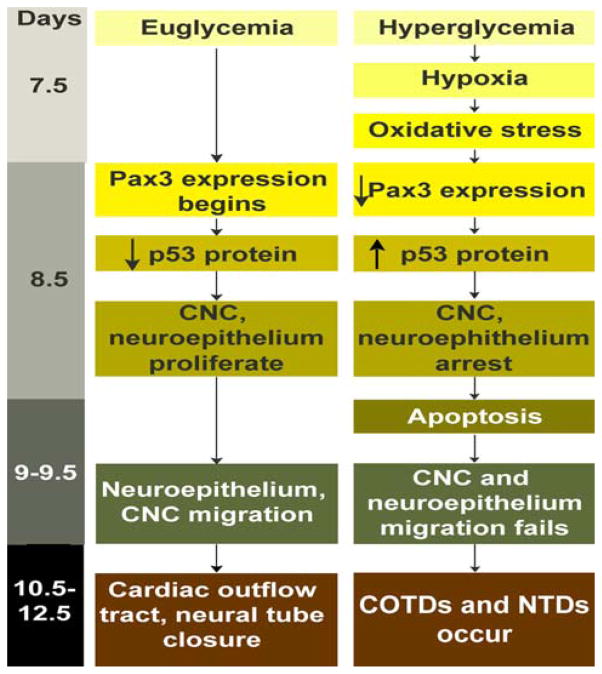
These results indicate that all of the effects of maternal diabetes on apoptosis that lead to COTD and NTD can be attributed to effects of oxidative stress, which occur approximately 24 h before the onset of Pax3 expression, to inhibit induction of Pax3; that the initiation of neural tube folding and CNC migration occurs independent of Pax3; that Pax3 must inhibit p53 synthesis or stability within the first few hours of its expression, although elimination of Pax3-deficient cells may not be completed until 24–48 h later; and that preventing p53-dependent apoptosis of neuroepithelium and CNC allows the neural tube to close and cardiac outflow tracts to septate. A diagram describing the pathways by which these processes occur in control and diabetic pregnancies is shown in Fig. 1.
Fig. 1.
Flow chart of developmental events during control pregnancies, in which embryos are exposed to normal glucose levels (euglycemia), and diabetic pregnancies, in which embryos are exposed to elevated glucose levels (hyperglycemia)
Regulation of p53 by Pax3
The prevention of apoptosis and malformations in Pax3-deficient embryos by inactivating p53 suggests that p53 might be regulated by Pax3 at the level of transcription or translation. While there were no differences in p53 mRNA levels between Pax3+/+, Pax3+/Sp, and Pax3Sp/Sp embryos, p53 protein levels were increased in Pax3Sp/Sp embryos [150]. This suggests that Pax3 inhibits p53-dependent apoptosis, not by inhibiting p53 gene expression, but by inhibiting p53 translation or stability. It should be noted that Pax5, -2, and -8 (which fall into the same Pax paralogous group as each other, but a different paralogous group from Pax3) can inhibit p53 expression at the level of transcription [151]. This suggests that down regulation of p53 may occur in response to several of the Pax proteins, but at different levels of control.
Since Pax3 is a transcription factor, it might control expression of genes which regulate p53 translation [152, 153] or turnover [154]. While it has not been determined how Pax3 regulates p53 steady state levels in normal embryo cells, transfection of PAX3 and p53 expression vectors into p53-null human lung carcinoma cells has suggested that stability of p53 may be reduced in the presence of PAX3 [155].
Regulation of neuroepithelial/neural crest cell viability by Pax3 suppression of p53
Currently, it is not known how p53 regulates apoptosis of neural crest or neuroepithelial cells in Pax3-deficient embryos. However, it may be secondary to cell cycle withdrawal. For example, the Warburg effect (in which the anaerobic:aerobic metabolism ratio is high even when O2 is not limiting) is characteristic of embryonic and cancer cells, and provides anabolic substrates for rapidly growing cells [156, 157]. p53 suppresses the Warburg effect, in part by transcriptional activation of genes that regulate respiration, and by inhibiting activity of glycolytic enzymes that prevent replicative senescence [158, 159]. Thus, Pax3, by inhibiting p53, may maintain CNC and neuroepithelium in a rapidly proliferating mode.
In hepatoma cells, stimulating oxidative pathways inhibits cell cycling, whereas stimulating glycolysis promotes cell cycling. However, folate, tetrahydrofolate, or purines can override the effects of oxidative pathways to inhibit cell cycling [160]. Thus, it is interesting to speculate that, in the early embryo, folic acid might function distal to Pax3 to promote purine synthesis and cell cycling. This might explain the effects of folic acid in embryos of diabetic rats and Pax3Sp2H/Sp2H embryos to reduce NTD [134–136] despite the presence of w.t. p53.
Effects of maternal diabetes on preimplantation embryos, apoptosis, pregnancy loss, and malformations
The focus of this review has been the apoptosis of neural crest and neuroepithelium in the pathogenesis of diabetic embryopathy. However, there is also evidence that maternal diabetes can induce apoptosis of the preovulatory oocyte or preimplantation embryo in animal models. This can be a cause of diminished fertility, although, recently, there has been evidence that it can be a cause of embryonic malformation. This topic has been discussed in more detail recently [161, 162] but is addressed briefly here.
Using STZ-induced diabetic mice, it has been shown that germinal vesicle breakdown of preovulatory follicles is delayed and preimplantation embryo development is abnormal; these effects are prevented by insulin administration [163, 164]. There is also increased apoptosis of granulosa and cumulus cells [165]. Culture of preimplantation embryos from diabetic mice in media containing physiological glucose does not reverse the effects of diabetes [163, 166]. These results suggest that diabetes impairs oocyte and follicular development that leads to irreversible adverse effects on the preimplantation embryo. However, culture of embryos from nondiabetic mice in high glucose media from the 2-cell to blastocyst stage causes the same abnormalities as does maternal diabetes, indicating that the early preimplantation embryo is also vulnerable to the adverse effects of maternal diabetes [167, 168]. By the blastocyst stage, there are significantly reduced numbers of embryo cells, and this is associated with increased apoptosis [169–171]. The apoptosis is due to increased expression of the pro-apoptotic protein, Bax, which occurs in response to p53 [172, 173].
Paradoxically, exposure of preimplantation embryos to elevated glucose does not increase glucose uptake, as in the post-implantation embryo, but it decreases glucose uptake due to decreased expression of Glut-1, -2, and -3 [174]. A novel insulin-responsive glucose transporter, Glut-8, is expressed by blastocysts [175]. Thus, during diabetic pregnancy, insulin-stimulated glucose uptake via Glut-8 might be reduced. Taken together, the adverse effects of maternal diabetes on preimplantation embryo cells appear to be mediated by glucose deprivation, whereas effects on post-implantation embryo cells appear to be mediated by glucose excess. There are also reports that markers of oxidative stress are increased in blastocysts cultured in high glucose [171], although, it still remains to be determined how decreased glucose availability would generate oxidative stress.
These effects of maternal hyperglycemia on ovarian follicle and preimplantation embryo development could be partially responsible for the decreased fertility of diabetic women. However, until a recent report from Wyman et al. [176], there was no evidence that maternal diabetes prior to organogenesis could lead to structural malformation of the post-implantation embryo. The Moley group transferred zygotes or blastocysts from STZ-induced diabetic mice to pseudopregnant nondiabetic recipients. When the pregnancies were examined on day 14.5, there was a higher rate of malformations (affecting the cranium, abdominal wall, and limbs) in embryos derived from zygotes or blastocysts transferred from diabetic mothers than in embryos derived from transfer from nondiabetic mothers. One interpretation of this result is that exposure of the preovulatory oocyte to a diabetic environment may influence expression of genes involved in organogenesis well before these genes would be induced. This could be explained by epigenetic modifications, such as chromatin acetylation or methylation, leading to suboptimal expression of affected genes later in development, or, effects on oocyte mitochondria so that they are unable to meet all of the energetic demands of rapidly growing embryonic structures during organogenesis. However, another interpretation is that STZ, which a nitrosourea compound, causes alkylation of DNA and carbamoylation of proteins [177], rather than maternal diabetes, was responsible for defective oogenesis. Since the ability of insulin treatment to prevent the effects of STZ-induced diabetes was not examined, this possibility can not be excluded at this time. There were also increased reabsorptions and growth retardation of embryos derived from zygotes and blastocysts transferred from diabetic mothers. The reabsorptions could be due to structural malformation of an essential organ (such as the heart or placenta), or misexpression of (embryonic and/or extraembryonic) genes that are essential during post-implantation development, leading to embryo demise. The growth retardation could be due to overall decreased proliferation or increased apoptosis. The molecular mechanisms responsible for these various outcomes (malformation, embryo demise, growth retardation) could be the same, with only the severity of the effect on the oocyte or zygote explaining the different outcomes.
Using a different experimental design, embryos were obtained from nondiabetic mothers and then cultured in vitro from the two-cell to blastocyst stage in media containing elevated D-glucose, or elevated L-glucose as an osmotic control [176]. When these embryos were transferred to pseudopregnant nondiabetic recipients and then examined on day 14.5, no malformations were observed in either treatment group. There were, however, fewer implantations and more reabsorptions, as well as growth retardation, among the embryos that had been cultured in elevated D-glucose. This result suggests that apoptosis of a limited number of cells of the blastocyst due to elevated glucose leads to growth retardation, but elimination of a critical mass of cells of the blastocyst will lead to implantation failure or demise of the entire embryo. However, since the fates of cells of the inner cell mass are not yet determined, specific organ systems of individual embryos are not affected. The failure of high glucose exposure only during the two cell to blastocyst stage to cause malformations suggests that, unlike the embryo at this stage of development is not susceptible to the effects of diabetes to cause malformations.
Summary
Pax3 is a developmental control gene whose expression is inhibited by oxidative stress in response to excess glucose metabolism. The oxidative stress must occur approximately 24 h before Pax3 expression begins, suggesting that there is a sequence of developmental steps that must be set in motion to induce Pax3 expression. Since Pax3 expression is sensitive to cellular redox status, it may function as a developmental energy sensor that functions to preserve the “stem-ness” of neuroepithelial and neural crest cells. It may do so by suppressing the activity of p53 to promote withdrawal from the cell cycle and terminal differentiation. However, if Pax3 levels are insufficient, p53 steady state levels rise, ultimately leading to apoptosis of neuroepithelium or neural crest. With the loss of the progenitor cells of the neural tube and the CNC which participate in cardiac outflow tract remodeling, NTD and COTD result. It is likely that there are other genes, expressed in other organ systems, that are sensitive to cellular redox status. Thus, misexpression of genes which regulate progenitor cell viability at critical stages of organogenesis may be a general mechanism responsible for malformations in diabetic pregnancy.
Acknowledgments
This work was supported by grants from the NIH (RO1 DK52865 and RO1 DK58300), the American Diabetes Association, and the Juvenile Diabetes Research Foundation to MRL.
Abbreviations
- T1DM
Type 1 diabetes mellitus
- T2DM
Type 2 diabetes mellitus
- STZ
Streptozotocin
- NTD
Neural tube defect(s)
- COTD
Cardiac outflow tract defect(s)
- CNC
Cardiac neural crest Glut Glucose transporter(s)
- GSH
Reduced glutathione
- GSSG
Oxidized glutathione
Contributor Information
James H. Chappell, Jr., Email: james.chappell@joslin.harvard.edu, Section on Developmental and Stem Cell Biology, Joslin Diabetes Center, One Joslin Place, Boston, MA 02215, USA
Xiao Dan Wang, Email: xiaodan.wang@joslin.harvard.edu, Section on Developmental and Stem Cell Biology, Joslin Diabetes Center, One Joslin Place, Boston, MA 02215, USA.
Mary R. Loeken, Email: mary.loeken@joslin.harvard.edu, Section on Developmental and Stem Cell Biology, Joslin Diabetes Center, One Joslin Place, Boston, MA 02215, USA
References
- 1.Farrell T, Neale L, Cundy T. Congenital anomalies in the offspring of women with type 1, type 2 and gestational diabetes. Diabet Med. 2002;19:322–326. doi: 10.1046/j.1464-5491.2002.00700.x. [DOI] [PubMed] [Google Scholar]
- 2.White P. Pregnancy complicating diabetes. Am J Med. 1949;7:609–616. doi: 10.1016/0002-9343(49)90382-4. [DOI] [PubMed] [Google Scholar]
- 3.Correa A, Gilboa SM, Besser LM, et al. Diabetes mellitus and birth defects. Am J Obstet Gynecol. 2008;199:237.e1–237.e9. doi: 10.1016/j.ajog.2008.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mills JL, Knopp RH, Simpson JL, et al. Lack of relation of increased malformation rates in infants of diabetic mothers to glycemic control during organogenesis. N Eng J Med. 1988;318:671–676. doi: 10.1056/NEJM198803173181104. [DOI] [PubMed] [Google Scholar]
- 5.Miodovnik M, Mimouni F, Dignan PSJ, et al. Major malformations in infants of IDDM women: vasculopathy and early first-trimester poor glycemic control. Diabetes Care. 1988;11:713–718. doi: 10.2337/diacare.11.9.713. [DOI] [PubMed] [Google Scholar]
- 6.Loffredo CA, Wilson PD, Ferencz C. Maternal diabetes: an independent risk factor for major cardiovascular malformations with increased mortality of affected infants. Teratology. 2001;64:98–106. doi: 10.1002/tera.1051. [DOI] [PubMed] [Google Scholar]
- 7.Kitzmiller JL, Cloherty JP, Younger MD, et al. Diabetic pregnancy and perinatal morbidity. Am J Obstet Gynecol. 1978;131:560–580. doi: 10.1016/0002-9378(78)90120-5. [DOI] [PubMed] [Google Scholar]
- 8.Hawthorne G, Robson S, Ryall EA, Sen D, Roberts SH, Ward Platt MP. Prospective population based survey of outcome of pregnancy in diabetic women: results of the Northern Diabetic Pregnancy Audit, 1994. Br Med J. 1997;315:279–281. doi: 10.1136/bmj.315.7103.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greene MF, Hare JW, Cloherty JP, Benacerraf BR, Soeldner JS. First-trimester hemoglobin A1 and risk for major malformation and spontaneous abortion in diabetic pregnancy. Teratology. 1989;39:225–231. doi: 10.1002/tera.1420390303. [DOI] [PubMed] [Google Scholar]
- 10.The DCCT Research Group. Pregnancy outcomes in the diabetes control and complications trial. Am J Obstet Gynecol. 1996;174:1343–1353. doi: 10.1016/s0002-9378(96)70683-x. [DOI] [PubMed] [Google Scholar]
- 11.Langer O, Conway DL. Level of glycemia and perinatal outcome in pregestational diabetes. J Matern Fetal Med. 2000;9:35–41. doi: 10.1002/(SICI)1520-6661(200001/02)9:1<35::AID-MFM8>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 12.Suhonen L, Hiilesmaa V, Teramo K. Glycaemic control during early pregnancy and fetal malformations in women with type I diabetes mellitus. Diabetologia. 2000;43:79–82. doi: 10.1007/s001250050010. [DOI] [PubMed] [Google Scholar]
- 13.Aberg A, Westbom L, Kallen B. Congenital malformations among infants whose mothers had gestational diabetes or preexisting diabetes. Early Hum Dev. 2001;61:85–95. doi: 10.1016/s0378-3782(00)00125-0. [DOI] [PubMed] [Google Scholar]
- 14.Freinkel N. Of pregnancy and progeny. Diabetes. 1980;29:1023–1035. doi: 10.2337/diab.29.12.1023. [DOI] [PubMed] [Google Scholar]
- 15.Moore LL, Singer MR, Bradlee ML, Rothman KJ, Milunsky A. A prospective study of the risk of congenital defects associated with maternal obesity and diabetes mellitus. Epidemiology. 2000;11:689–694. doi: 10.1097/00001648-200011000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Shaw GM, Velie EM, Schaffer D. Risk of neural tube defect-affected pregnancies among obese women. JAMA. 1996;275:1093–1096. doi: 10.1001/jama.1996.03530380035028. [DOI] [PubMed] [Google Scholar]
- 17.Watkins ML, Rasmussen SA, Honein MA, Botto LD, Moore CA. Maternal obesity and risk for birth defects. Pediatrics. 2003;111:1152–1158. [PubMed] [Google Scholar]
- 18.Werler MW, Louik C, Shapiro S, Mitchell AA. Prepregnant weight in relation to risk of neural tube defects. JAMA. 1996;275:1089–1092. doi: 10.1001/jama.1996.03530380031027. [DOI] [PubMed] [Google Scholar]
- 19.Waller DK, Shaw GM, Rasmussen SA, et al. Prepregnancy obesity as a risk factor for structural birth defects. Arch Pediatr Adolesc Med. 2007;161:745–750. doi: 10.1001/archpedi.161.8.745. [DOI] [PubMed] [Google Scholar]
- 20.MRC Vitamin Research Group. Prevention of neural tube defects: results of the MRC vitamin study. Lancet. 1991;338:132–137. [PubMed] [Google Scholar]
- 21.Honein MA, Paulozzi LJ, Mathews TJ, Erickson JD, Wong LYC. Impact of folic acid fortification of the US food supply on the occurrence of neural tube defects. JAMA. 2001;285:2981–2986. doi: 10.1001/jama.285.23.2981. [DOI] [PubMed] [Google Scholar]
- 22.De Wals P, Tairou F, Van Allen MI, et al. Reduction in neural-tube defects after folic acid fortification in Canada. N Engl J Med. 2007;357:135–142. doi: 10.1056/NEJMoa067103. [DOI] [PubMed] [Google Scholar]
- 23.Laraia BA, Bodnar LM, Siega-Riz AM. Pregravid body mass index is negatively associated with diet quality during pregnancy. Public Health Nutr. 2007;10:920–926. doi: 10.1017/S1368980007657991. [DOI] [PubMed] [Google Scholar]
- 24.Case AP, Ramadhani TA, Canfield MA, Beverly L, Wood R. Folic acid supplementation among diabetic, overweight, or obese women of childbearing age. J Obstet Gynecol Neonatal Nurs. 2007;36:335–341. doi: 10.1111/j.1552-6909.2007.00163.x. [DOI] [PubMed] [Google Scholar]
- 25.Mahabir S, Ettinger S, Johnson L, et al. Measures of adiposity and body fat distribution in relation to serum folate levels in postmenopausal women in a feeding study. Eur J Clin Nutr. 2008;62:644–650. doi: 10.1038/sj.ejcn.1602771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Becerra JE, Khoury MJ, Cordero JF, Erickson JD. Diabetes mellitus during pregnancy and the risks for the specific birth defects: a population-based case-control study. Pediatrics. 1990;85:1–9. [PubMed] [Google Scholar]
- 27.Schaefer-Graf UM, Buchanan TA, Xiang A, Songster G, Montoro M, Kjos SL. Patterns of congenital anomalies and relationship to initial maternal fasting glucose levels in pregnancies complicated by type 2 and gestational diabetes. Am J Obstet Gynecol. 2000;182:313–320. doi: 10.1016/s0002-9378(00)70217-1. [DOI] [PubMed] [Google Scholar]
- 28.Nielsen GL, Norgard B, Puho E, Rothman KJ, Sorensen HT, Czeizel AE. Risk of specific congenital abnormalities in offspring of women with diabetes. Diabet Med. 2005;22:693–696. doi: 10.1111/j.1464-5491.2005.01477.x. [DOI] [PubMed] [Google Scholar]
- 29.Macintosh MCM, Fleming KM, Bailey JA, et al. Perinatal mortality and congenital anomalies in babies of women with type 1 or type 2 diabetes in England, Wales, and Northern Ireland: population based study. Br Med J. 2006;333:177–180. doi: 10.1136/bmj.38856.692986.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mills JL, Baker L, Goldman AS. Malformations in infants of diabetic mothers occur before the seventh gestational week: implications for treatment. Diabetes. 1979;28:292–293. doi: 10.2337/diab.28.4.292. [DOI] [PubMed] [Google Scholar]
- 31.Hod M, Star S, Passonneau JV, Unterman TG, Freinkel N. Effect of hyperglycemia on sorbitol and myo-inositol content of cultured rat conceptus: failure of aldose reductase inhibitors to modify myo-inositol depletion and dysmorphogenesis. Biochem Biophys Res Commun. 1986;140:974–980. doi: 10.1016/0006-291x(86)90731-x. [DOI] [PubMed] [Google Scholar]
- 32.Buchanan TA, Denno KM, Sipos GF, Sadler TW. Diabetic teratogenesis: in vitro evidence for a multifactorial etiology with little contribution from glucose per se. Diabetes. 1994;43:656–660. doi: 10.2337/diab.43.5.656. [DOI] [PubMed] [Google Scholar]
- 33.Eriksson UJ, Hakan Borg LA, Forsberg H, Styrud J. Diabetic embryopathy: studies with animal and in vitro models. Diabetes. 1991;40(Suppl 2):94–98. doi: 10.2337/diab.40.2.s94. [DOI] [PubMed] [Google Scholar]
- 34.Sadler TW, Hunter ESI, Wynn RE, Phillips LS. Evidence for multifactorial origin of diabetes-induced embryopathies. Diabetes. 1989;38:70–74. doi: 10.2337/diab.38.1.70. [DOI] [PubMed] [Google Scholar]
- 35.Reece EA, Pinter E, Leranth CZ, et al. Ultrastructural analysis of malformations of the embryonic neural axis induced by in vitro hyperglycemic conditions. Teratology. 1985;32:363–373. doi: 10.1002/tera.1420320306. [DOI] [PubMed] [Google Scholar]
- 36.Zusman I, Yaffe P, Ornoy A. Effects of metabolic factors in the diabetic state on the in vitro development of preimplantation mouse embryos. Teratology. 1987;35:77–85. doi: 10.1002/tera.1420350111. [DOI] [PubMed] [Google Scholar]
- 37.Viana M, Herrera E, Bonet B. Terotogenic effects of diabetes mellitus in the rat. Prevention by vitamin E. Diabetologia. 1996;39:1041–1046. doi: 10.1007/BF00400652. [DOI] [PubMed] [Google Scholar]
- 38.Gareskog M, Wentzel P. Altered protein kinase C activation associated with rat embryonic dysmorphogenesis. Pediatr Res. 2004;56:849–857. doi: 10.1203/01.PDR.0000145295.88601.B9. [DOI] [PubMed] [Google Scholar]
- 39.Gareskog M, Wentzel P. N-Acetylcysteine and alpha-cyano-4-hydroxycinnamic acid alter protein kinase C (PKC)-delta and PKC-zeta and diminish dysmorphogenesis in rat embryos cultured with high glucose in vitro. J Endocrinol. 2007;192:207–214. doi: 10.1677/joe.1.06966. [DOI] [PubMed] [Google Scholar]
- 40.Hiramatsu Y, Sekiguchi N, Hayashi M, et al. Diacylglycerol production and protein kinase C activity are increased in a mouse model of diabetic embryopathy. Diabetes. 2002;51:2804–2810. doi: 10.2337/diabetes.51.9.2804. [DOI] [PubMed] [Google Scholar]
- 41.Engstrom E, Haglund A, Eriksson UJ. Effects of maternal diabetes or in vitro hyperglycemia on uptake of palmitic and arachidonic acid by rat embryos. Pediatr Res. 1991;30:150–153. doi: 10.1203/00006450-199108000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Goldman AS, Baker L, Piddington R, Marx B, Herold R, Egler J. Hyperglycemic-induced teratogenesis is mediated by a functional deficiency of arachidonic acid. Proc Natl Acad Sci USA. 1985;82:8227–8231. doi: 10.1073/pnas.82.23.8227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schoenfeld A, Erman A, Warchaizer S, Ovadia J, Bonner J, Hod M. Yolk sac concentration of prostaglandin E(2) in diabetic pregnancy: further clues to the etiology of diabetic embryopathy. Prostaglandins. 1995;50:121–126. doi: 10.1016/0090-6980(95)00084-4. [DOI] [PubMed] [Google Scholar]
- 44.Wentzel P, Welsh N, Eriksson UJ. Developmental damage, increased lipid peroxidation, diminished cyclooxygenase-2 gene expression, and lowered prostaglandin E2 levels in rat embryos exposed to a diabetic environment. Diabetes. 1999;48:813–820. doi: 10.2337/diabetes.48.4.813. [DOI] [PubMed] [Google Scholar]
- 45.Higa R, Gonzalez E, Pustovrh MC, et al. PPARdelta and its activator PGI2 are reduced in diabetic embryopathy: involvement of PPARdelta activation in lipid metabolic and signalling pathways in rat embryo early organogenesis. Mol Hum Reprod. 2007;13:103–110. doi: 10.1093/molehr/gal104. [DOI] [PubMed] [Google Scholar]
- 46.Capobianco E, Martinez N, Higa R, White V, Jawerbaum A. The effects of maternal dietary treatments with natural PPAR ligands on lipid metabolism in fetuses from control and diabetic rats. Prostaglandins Leukot Essent Fatty Acids. 2008;79:191–199. doi: 10.1016/j.plefa.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 47.Capobianco E, White V, Higa R, Martinez N, Jawerbaum A. Effects of natural ligands of PPARgamma on lipid metabolism in placental tissues from healthy and diabetic rats. Mol Hum Reprod. 2008;14:491–499. doi: 10.1093/molehr/gan039. [DOI] [PubMed] [Google Scholar]
- 48.Martinez N, Capobianco E, White V, Pustovrh MC, Higa R, Jawerbaum A. Peroxisome proliferator-activated receptor alpha activation regulates lipid metabolism in the feto-placental unit from diabetic rats. Reproduction. 2008;136:95–103. doi: 10.1530/REP-08-0028. [DOI] [PubMed] [Google Scholar]
- 49.Lee AT, Plump A, DeSimone C, Cerami A, Bucala R. A role for DNA mutations in diabetes-associated teratogensis in transgeneic embryos. Diabetes. 1995;44:20–24. doi: 10.2337/diab.44.1.20. [DOI] [PubMed] [Google Scholar]
- 50.Lee AT, Reis D, Eriksson UJ. Hyperglycemia-induced embryonic dysmorphogenesis correlates with genomic DNA mutation frequency in vitro and in vivo. Diabetes. 1999;48:371–376. doi: 10.2337/diabetes.48.2.371. [DOI] [PubMed] [Google Scholar]
- 51.Siman CM, Eriksson UJ. Vitamin E decreases the occurrence of malformations in the offspring of diabetic rats. Diabetes. 1997;46:1054–1061. doi: 10.2337/diab.46.6.1054. [DOI] [PubMed] [Google Scholar]
- 52.Sivan E, Reece EA, Wu YK, Homko CJ, Polansky M, Boren-stein M. Dietary vitamin E prophylaxis and diabetic embryopathy: morphologic and biochemical analysis. Am J Obstet Gynecol. 1996;175:793–799. doi: 10.1016/s0002-9378(96)80001-9. [DOI] [PubMed] [Google Scholar]
- 53.Wentzel P, Eriksson UJ. Antioxidants diminish developmental damage induced by high glucose and cyclooxygenase inhibitors in rat embryos in vitro. Diabetes. 1998;47:677–684. doi: 10.2337/diabetes.47.4.677. [DOI] [PubMed] [Google Scholar]
- 54.Hagay ZJ, Weiss Y, Zusman I, et al. Prevention of diabetes-associated embryopathy by overexpression of the free radical scavenger copper zinc superoxide dismutase in transgenic mouse embryos. Am J Obstet Gynecol. 1995;173:1036–1041. doi: 10.1016/0002-9378(95)91323-8. [DOI] [PubMed] [Google Scholar]
- 55.Weksler-Zangen S, Yaffe P, Ornoy A. Reduced SOD activity and increased neural tube defects in embryos of the sensitive but not of the resistant Cohen diabetic rats cultured under diabetic conditions. Birth Defects Res A Clin Mol Teratol. 2003;67:429–437. doi: 10.1002/bdra.10043. [DOI] [PubMed] [Google Scholar]
- 56.Copp AJ. Neurulation in the cranial region—normal and abnormal. J Anat. 2005;207:623–635. doi: 10.1111/j.1469-7580.2005.00476.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lawson A, England MA. Neural fold fusion in the cranial region of the chick embryo. Dev Dyn. 1998;212:473–481. doi: 10.1002/(SICI)1097-0177(199808)212:4<473::AID-AJA1>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 58.Weil M, Jacobson MD, Raff MC. Is programmed cell death required for neural tube closure? Curr Biol. 1997;7:281–284. doi: 10.1016/s0960-9822(06)00125-4. [DOI] [PubMed] [Google Scholar]
- 59.Naruse I, Keino H. Apoptosis in the developing CNS. Prog Neurobiol. 1995;47:135–155. doi: 10.1016/0301-0082(95)00024-p. [DOI] [PubMed] [Google Scholar]
- 60.Cecconi F, Alvarez-Bolado G, Meyer BI, Roth KA, Gruss P. Apaf1 (CED-4 homolog) regulates programmed cell death in mammalian development. Cell. 1998;94:727–737. doi: 10.1016/s0092-8674(00)81732-8. [DOI] [PubMed] [Google Scholar]
- 61.Mori C, Nakamura N, Okamoto Y, Osawa M, Shiota K. Cytochemical identification of programmed cell death in the fusing fetal mouse palate by specific labelling of DNA fragmentation. Anat Embryol. 1994;190:21–28. doi: 10.1007/BF00185843. [DOI] [PubMed] [Google Scholar]
- 62.Lynch MP, Capparelli C, Stein JL, Stein GS, Lian JB. Apoptosis during bone-like tissue development in vitro. J Cell Biochem. 1998;68:31–49. [PubMed] [Google Scholar]
- 63.Homma S, Yaginuma H, Oppenheim RW. Programmed cell death during the earliest stages of spinal cord development in the chick embryo: a possible means of early phenotypic selection. J Comp Neurol. 1994;345:377–395. doi: 10.1002/cne.903450305. [DOI] [PubMed] [Google Scholar]
- 64.Graham A, Heyman I, Lumsden A. Even-numbered rhombomeres control the apoptotic elimination of neural crest cells from odd-numbered rhombomeres in the chick hindbrain. Development. 1993;119:233–245. doi: 10.1242/dev.119.1.233. [DOI] [PubMed] [Google Scholar]
- 65.Clarke PG. Developmental cell death: morphological diversity and multiple mechnisms. Anat Embryol. 1990;181:195–213. doi: 10.1007/BF00174615. [DOI] [PubMed] [Google Scholar]
- 66.Sulik KK, Cook CS, Webster WS. Teratogens and craniofacial malformations: relationships to cell death. Development. 1988;103(Suppl):213–232. doi: 10.1242/dev.103.Supplement.213. [DOI] [PubMed] [Google Scholar]
- 67.Walther C, Guenet JL, Simon D, et al. Pax: a murine multigene family of paired box-containing genes. Genomics. 1991;11:424–434. doi: 10.1016/0888-7543(91)90151-4. [DOI] [PubMed] [Google Scholar]
- 68.Chalepakis G, Tremblay P, Gruss P. Pax genes, mutants and molecular function. J Cell Sci Suppl. 1992;16:61–67. doi: 10.1242/jcs.1992.supplement_16.8. [DOI] [PubMed] [Google Scholar]
- 69.Gruss P, Walther C. Pax in development. Cell. 1992;69:719–722. doi: 10.1016/0092-8674(92)90281-g. [DOI] [PubMed] [Google Scholar]
- 70.Stuart ET, Kioussi C, Gruss P. Mammalian pax genes. Ann Rev Genet. 1994;28:219–236. doi: 10.1146/annurev.ge.28.120194.001251. [DOI] [PubMed] [Google Scholar]
- 71.Robson EJ, He SJ, Eccles MR. A PANorama of PAX genes in cancer and development. Nat Rev Cancer. 2006;6:52–62. doi: 10.1038/nrc1778. [DOI] [PubMed] [Google Scholar]
- 72.Goulding MD, Chalepakis G, Deutsch U, Erselius JR, Gruss P. Pax-3, a novel murine DNA binding protein expressed during early neurogenesis. EMBO J. 1991;10:1135–1147. doi: 10.1002/j.1460-2075.1991.tb08054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chalepakis G, Goulding M, Read A, Strachan T, Gruss P. Molecular basis of splotch and Waardenburg Pax-3 mutations. Proc Natl Acad Sci USA. 1994;91:3685–3689. doi: 10.1073/pnas.91.9.3685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lalwani AK, Brister JR, Fex J, et al. Further elucidation of the genomic structure of PAX3, and identification of two different point mutations within the PAX3 homeobox that cause Waardenburg syndrome type 1 in two families. Am J Hum Genet. 1995;56:75–83. [PMC free article] [PubMed] [Google Scholar]
- 75.Waardenburg PJ. A new syndrome combining developmental anomalies of the eyelids, eyebrows and nose root with pigmentary defects of the iris and head hair and with congenital deafness. Am J Hum Genet. 1951;3:195–253. [PMC free article] [PubMed] [Google Scholar]
- 76.Epstein DJ, Vekemans M, Gros P. Splotch (Sp-2H), a mutation affecting development of the mouse neural tube, shows a deletion within the paired homeodomain of Pax-3. Cell. 1991;67:767–774. doi: 10.1016/0092-8674(91)90071-6. [DOI] [PubMed] [Google Scholar]
- 77.Epstein DJ, Vogan KJ, Trasler DG, Gros P. A mutation within intron 3 of the Pax-3 gene produces aberrantly spliced mRNA transcripts in the splotch (Sp) mouse mutant. Proc Natl Acad Sci USA. 1993;90:532–536. doi: 10.1073/pnas.90.2.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Goulding M, Sterrer S, Fleming J, et al. Analysis of the Pax-3 gene in the mouse mutant splotch. Genomics. 1993;17:355–363. doi: 10.1006/geno.1993.1332. [DOI] [PubMed] [Google Scholar]
- 79.Vogan KJ, Epstein DJ, Trasler DG, Gros P. The Splotch-delayed (Sp-d) mouse mutant carries a point mutation within the paired box of the Pax-3 gene. Genomics. 1993;17:364–369. doi: 10.1006/geno.1993.1333. [DOI] [PubMed] [Google Scholar]
- 80.Auerbach R. Analysis of the developmental effects of a lethal mutation in the house mouse. J Exp Zool. 1954;127:305–329. [Google Scholar]
- 81.Franz T. Persistent truncus arteriosus in the Splotch mutant mouse. Anat Embryol (Berl) 1989;180:457–464. doi: 10.1007/BF00305120. [DOI] [PubMed] [Google Scholar]
- 82.St Amand TR, Lu JT, Zamora M, et al. Distinct roles of HF-1b/Sp4 in ventricular and neural crest cells lineages affect cardiac conduction system development. Dev Biol. 2006;291:208–217. doi: 10.1016/j.ydbio.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 83.Epstein JA, Li J, Lang D, et al. Migration of cardiac neural crest cells in Splotch embryos. Development. 2000;127:1869–1878. doi: 10.1242/dev.127.9.1869. [DOI] [PubMed] [Google Scholar]
- 84.Conway SJ, Godt RE, Hatcher CJ, et al. Neural crest is involved in development of abnormal myocardial function. J Mol Cell Cardiol. 1997;29:2675–2685. doi: 10.1006/jmcc.1997.0499. [DOI] [PubMed] [Google Scholar]
- 85.Conway SJ, Henderson DJ, Kirby ML, Anderson RH, Copp AJ. Development of a lethal congenital heart defect in the splotch (Pax3) mutant mouse. Cardiovasc Res. 1997;36:163–173. doi: 10.1016/s0008-6363(97)00172-7. [DOI] [PubMed] [Google Scholar]
- 86.Phelan SA, Ito M, Loeken MR. Neural tube defects in embryos of diabetic mice: role of the Pax-3 gene and apoptosis. Diabetes. 1997;46:1189–1197. doi: 10.2337/diab.46.7.1189. [DOI] [PubMed] [Google Scholar]
- 87.Morgan SC, Relaix F, Sandell LL, Loeken MR. Oxidative stress during diabetic pregnancy disrupts cardiac neural crest migration and causes outflow tract defects. Birth Defects Res A Clin Mol Teratol. 2008;82:453–463. doi: 10.1002/bdra.20457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Maulbecker CC, Gruss P. The oncogenic potential of Pax genes. EMBO J. 1993;12:2361–2367. doi: 10.1002/j.1460-2075.1993.tb05890.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Barr FG, Fitzgerald JC, Ginsberg JP, Vanella ML, Davis RJ, Bennicelli JL. Predominant expression of alternative PAX3 and PAX7 forms in myogenic and neural tumor cell lines. Cancer Res. 1999;59:5443–5448. [PubMed] [Google Scholar]
- 90.Barr FG, Galili N, Holick J, Biegel JA, Rovera G, Emanuel BS. Rearrangement of the PAX3 paired box gene in the paediatric solid tumor alveolar rhabdomyosarcoma. Nature Genet. 1993;3:113–117. doi: 10.1038/ng0293-113. [DOI] [PubMed] [Google Scholar]
- 91.Galili N, Davis R, Fredericks WJ, et al. Fusion of a fork head domain gene to PAX3 in the solid tumor alveolar rhabdomyosarcoma. Nature Genet. 1993;5:230–235. doi: 10.1038/ng1193-230. [DOI] [PubMed] [Google Scholar]
- 92.Shapiro DN, Sublett JE, Li B, Downing JR, Naeve CW. Fusion of PAX3 to a member of the forkhead family of transcription factors in human alveolar rhabdomyosarcoma. Cancer Res. 1993;53:5108–5112. [PubMed] [Google Scholar]
- 93.Blake J, Ziman MR. Aberrant PAX3 and PAX7 expression. A link to the metastatic potential of embryonal rhabdomyosarcoma and cutaneous malignant melanoma? Histol Histopathol. 2003;18:529–539. doi: 10.14670/HH-18.529. [DOI] [PubMed] [Google Scholar]
- 94.Gershon TR, Oppenheimer O, Chin SS, Gerald WL. Temporally regulated neural crest transcription factors distinguish neuroectodermal tumors of varying malignancy and differentiation. Neoplasia. 2005;7:575–584. doi: 10.1593/neo.04637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Schulte TW, Toretsky JA, Ress E, Helman L, Neckers LM. Expression of PAX3 in Ewing’s sarcoma family of tumors. Biochem Mol Med. 1997;60:121–126. doi: 10.1006/bmme.1997.2567. [DOI] [PubMed] [Google Scholar]
- 96.Kubic JD, Young KP, Plummer RS, Ludvik AE, Lang D. Pigmentation PAX-ways: the role of Pax3 in melanogenesis, melanocyte stem cell maintenance, and disease. Pigment Cell Melanoma Res. 2008;21:627–645. doi: 10.1111/j.1755-148X.2008.00514.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Vachtenheim J, Novotna H. Expression of genes for microphthalmia isoforms, Pax3 and MSG1, in human melanomas. Cell Mol Biol (Noisy-le-grand) 1999;45:1075–1082. [PubMed] [Google Scholar]
- 98.Scholl FA, Kamarashev J, Murmann OV, Geertsen R, Dummer R, Schafer BW. PAX3 is expressed in human melanomas and contributes to tumor cell survival. Cancer Res. 2001;61:823–826. [PubMed] [Google Scholar]
- 99.He SJ, Stevens G, Braithwaite AW, Eccles MR. Transfection of melanoma cells with antisense PAX3 oligonucleotides additively complements cisplatin-induced cytotoxicity. Mol Cancer Ther. 2005;4:996–1003. doi: 10.1158/1535-7163.MCT-04-0252. [DOI] [PubMed] [Google Scholar]
- 100.Bernasconi M, Remppis A, Fredericks WJ, Rauscher FJ, Schafer BW. Induction of apoptosis in rhabdomyosarcoma cells through down-regulation of PAX proteins. Proc Natl Acad Sci USA. 1996;93:13164–13169. doi: 10.1073/pnas.93.23.13164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yang G, Li Y, Nishimura EK, et al. Inhibition of PAX3 by TGF-beta modulates melanocyte viability. Mol Cell. 2008;32:554–563. doi: 10.1016/j.molcel.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 102.Morgan SC, Lee H-Y, Relaix F, Sandell L, Lavorse J, Loeken MR. Cardiac outflow tract septation failure in Pax3-deficient embryos is due to p53-dependent regulation of migrating cardiac neural crest. Mech Dev. 2008;125:757–767. doi: 10.1016/j.mod.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sadler TW. Embryology of neural tube development. Am J Med Genet C Semin Med Genet. 2005;135C:2–8. doi: 10.1002/ajmg.c.30049. [DOI] [PubMed] [Google Scholar]
- 104.Salvarezza SB, Rovasio RA. Exogenous retinoic acid decreases in vivo and in vitro proliferative activity during the early migratory stage of neural crest cells. Cell Prolif. 1997;30:71–80. doi: 10.1046/j.1365-2184.1997.00071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sun FY, Kawasaki E, Akazawa S, et al. Apoptosis and its pathway in early post-implantation embryos of diabetic rats. Diabetes Res Clin Pract. 2005;67:110–118. doi: 10.1016/j.diabres.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 106.Jiang B, Kumar SD, Loh WT, et al. Global gene expression analysis of cranial neural tubes in embryos of diabetic mice. J Neurosci Res. 2008;86:3481–3493. doi: 10.1002/jnr.21800. [DOI] [PubMed] [Google Scholar]
- 107.Gao Q, Gao YM. Hyperglycemic condition disturbs the proliferation and cell death of neural progenitors in mouse embryonic spinal cord. Int J Dev Neurosci. 2007;25:349–357. doi: 10.1016/j.ijdevneu.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 108.Wentzel P, Gareskog M, Eriksson UJ. Decreased cardiac glutathione peroxidase levels and enhanced mandibular apoptosis in malformed embryos of diabetic rats. Diabetes. 2008;57:3344–3352. doi: 10.2337/db08-0830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kumar SD, Dheen ST, Tay SS. Maternal diabetes induces congenital heart defects in mice by altering the expression of genes involved in cardiovascular development. Cardiovasc Diabetol. 2007;6:34. doi: 10.1186/1475-2840-6-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Molin DG, Roest PA, Nordstrand H, et al. Disturbed morphogenesis of cardiac outflow tract and increased rate of aortic arch anomalies in the offspring of diabetic rats. Birth Defects Res A Clin Mol Teratol. 2004;70:927–938. doi: 10.1002/bdra.20101. [DOI] [PubMed] [Google Scholar]
- 111.Gareskog M, Cederberg J, Eriksson UJ, Wentzel P. Maternal diabetes in vivo and high glucose concentration in vitro increases apoptosis in rat embryos. Reprod Toxicol. 2007;23:63–74. doi: 10.1016/j.reprotox.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 112.Loeken MR. Advances in understanding the molecular causes of diabetes-induced birth defects. J Soc Gynecol Investig. 2006;13:2–10. doi: 10.1016/j.jsgi.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 113.Horton WE, Jr, Sadler TW. Effects of maternal diabetes on early embryogenesis. Alterations in morphogenesis produced by the ketone body, B-hydroxybutyrate. Diabetes. 1983;32:610–616. doi: 10.2337/diab.32.7.610. [DOI] [PubMed] [Google Scholar]
- 114.Unterman TG, Buchanan TA, Freinkel N. Access of maternal insulin to the rat conceptus prior to allantoic placentation. Diabetes Res. 1989;10:115–120. [PubMed] [Google Scholar]
- 115.Towner D, Kjos SL, Leung B, et al. Congenital malformations in pregnancies complicated by NIDDM. Diabetes Care. 1995;18:1446–1451. doi: 10.2337/diacare.18.11.1446. [DOI] [PubMed] [Google Scholar]
- 116.Schaefer UM, Sonster G, Xiang A, Berkowitz K, Buchanan TA, Kjos SL. Congenital malformations in offspring of women with hyperglycemia first detected during pregnancy. Am J Obstet Gynecol. 1997;177:1165–1171. doi: 10.1016/s0002-9378(97)70035-8. [DOI] [PubMed] [Google Scholar]
- 117.Lauenborg J, Mathiesen E, Ovesen P, et al. Audit on stillbirths in women with pregestational type 1 diabetes. Diabetes Care. 2003;26:1385–1389. doi: 10.2337/diacare.26.5.1385. [DOI] [PubMed] [Google Scholar]
- 118.Sussman I, Matschinsky FM. Diabetes affects sorbitol and myoinositol levels of neuroectodermal tissue during embryogenesis in rat. Diabetes. 1988;37:974–981. doi: 10.2337/diab.37.7.974. [DOI] [PubMed] [Google Scholar]
- 119.Fine E, Horal M, Chang T, Fortin G, Loeken M. Evidence that hyperglycemia causes altered gene expression, apoptosis, and neural tube defects in a mouse model of diabetic pregnancy. Diabetes. 1999;48:2454–2462. doi: 10.2337/diabetes.48.12.2454. [DOI] [PubMed] [Google Scholar]
- 120.Hogan A, Heyner S, Charon MJ, et al. Glucose transporter gene expression in early mouse embryos. Development. 1991;113:363–372. doi: 10.1242/dev.113.1.363. [DOI] [PubMed] [Google Scholar]
- 121.Li R, Thorens B, Loeken MR. Expression of the gene encoding the high Km glucose transporter 2 by the early postimplantation mouse embryo is essential for neural tube defects associated with diabetic embryopathy. Diabetologia. 2007;50:682–689. doi: 10.1007/s00125-006-0579-7. [DOI] [PubMed] [Google Scholar]
- 122.Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature. 2001;414:813–820. doi: 10.1038/414813a. [DOI] [PubMed] [Google Scholar]
- 123.Sakamaki H, Akazawa S, Ishibashi M, et al. Significance of glutathione-dependent antioxidant system in diabetes-induced embryonic malformations. Diabetes. 1999;48:1138–1144. doi: 10.2337/diabetes.48.5.1138. [DOI] [PubMed] [Google Scholar]
- 124.Trocino RA, Akazawa S, Ishibashi M, et al. Significance of glutathione depletion and oxidative stress in early embryogenesis in glucose-induced rat embryo culture. Diabetes. 1995;44:992–998. doi: 10.2337/diab.44.8.992. [DOI] [PubMed] [Google Scholar]
- 125.Horal M, Zhang Z, Virkamaki A, Stanton R, Loeken MR. Activation of the hexosamine pathway causes oxidative stress and abnormal embryo gene expression: involvement in diabetic teratogenesis. Birth Defects Res Part A Clin Mol Teratol. 2004;70:519–527. doi: 10.1002/bdra.20056. [DOI] [PubMed] [Google Scholar]
- 126.Li R, Chase M, Jung SK, Smith PJS, Loeken MR. Hypoxic stress in diabetic pregnancy contributes to impaired embryo gene expression and defective development by inducing oxidative stress. Am J Physiol Endocrinol Metab. 2005;289:E591–E599. doi: 10.1152/ajpendo.00441.2004. [DOI] [PubMed] [Google Scholar]
- 127.Jabs T. Reactive oxygen intermediates as mediators of programmed cell death in plants and animals. Biochem Pharmacol. 1999;57:231–245. doi: 10.1016/s0006-2952(98)00227-5. [DOI] [PubMed] [Google Scholar]
- 128.Chang TI, Horal M, Jain S, Wang F, Patel R, Loeken MR. Oxidant regulation of gene expression and neural tube development: insights gained from diabetic pregnancy on molecular causes of neural tube defects. Diabetologia. 2003;46:538–545. doi: 10.1007/s00125-003-1063-2. [DOI] [PubMed] [Google Scholar]
- 129.Agrawal A, Choudhary D, Upreti M, Rath PC, Kale RK. Radiation induced oxidative stress: I. Studies in Ehrlich solid tumor in mice. Mol Cell Biochem. 2001;223:71–80. doi: 10.1023/a:1017900810837. [DOI] [PubMed] [Google Scholar]
- 130.Nicol CJ, Zielenski J, Tsui LC, Wells PG. An embryo-protective role for glucose-6-phosphate dehydrogenase in developmental oxidative stress and chemical teratogenesis. FASEB J. 2000;14:111–127. doi: 10.1096/fasebj.14.1.111. [DOI] [PubMed] [Google Scholar]
- 131.Nakano E, Higgins JA, Powers HJ. Folate protects against oxidative modification of human LDL. Br J Nutr. 2001;86:637–639. doi: 10.1079/bjn2001478. [DOI] [PubMed] [Google Scholar]
- 132.Chern CL, Huang RF, Chen YH, Cheng JT, Liu TZ. Folate deficiency-induced oxidative stress and apoptosis are mediated via homocysteine-dependent overproduction of hydrogen peroxide and enhanced activation of NF-kappaB in human Hep G2 cells. Biomed Pharmacother. 2001;55:434–442. doi: 10.1016/s0753-3322(01)00095-6. [DOI] [PubMed] [Google Scholar]
- 133.Rosenquist TH, Ratashak SA, Selhub J. Homocysteine induces congenital defects of the heart and neural tube: effect of folic acid. Proc Natl Acad Sci USA. 1996;93:15227–15232. doi: 10.1073/pnas.93.26.15227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zabihi S, Eriksson UJ, Wentzel P. Folic acid supplementation affects ROS scavenging enzymes, enhances Vegf-A, and diminishes apoptotic state in yolk sacs of embryos of diabetic rats. Reprod Toxicol. 2007;23:486–498. doi: 10.1016/j.reprotox.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 135.Oyama K, Sugimura Y, Murase T, et al. Folic acid prevents congenital malformations in the offspring of diabetic mice. Endocr J. 2008;56:29–37. doi: 10.1507/endocrj.k08e-180. [DOI] [PubMed] [Google Scholar]
- 136.Fleming A, Copp AJ. Embryonic folate metabolism and mouse neural tube defects. Science. 1998;280:2107–2109. doi: 10.1126/science.280.5372.2107. [DOI] [PubMed] [Google Scholar]
- 137.Gefrides LA, Bennett GD, Finnell RH. Effects of folate supplementation on the risk of spontaneous and induced neural tube defects in Splotch mice. Teratology. 2002;65:63–69. doi: 10.1002/tera.10019. [DOI] [PubMed] [Google Scholar]
- 138.Kaplan JS, Iqbal S, England BG, Zawacki CM, Herman WH. Is pregnancy in diabetic women associated with folate deficiency? Diabetes Care. 1999;22:1017–1021. doi: 10.2337/diacare.22.7.1017. [DOI] [PubMed] [Google Scholar]
- 139.Pani L, Horal M, Loeken MR. Polymorphic susceptibility to the molecular causes of neural tube defects during diabetic embryopathy. Diabetes. 2002;51:2871–2874. doi: 10.2337/diabetes.51.9.2871. [DOI] [PubMed] [Google Scholar]
- 140.Jacks T, Remington L, William BO, et al. Tumor spectrum analysis in p53-mutant mice. Curr Biol. 1994;4:1–7. doi: 10.1016/s0960-9822(00)00002-6. [DOI] [PubMed] [Google Scholar]
- 141.Komarov PG, Komarova EA, Kondratov RV, et al. A chemical inhibitor of p53 that protects mice from the side effects of cancer therapy. Science. 1999;285:1733–1737. doi: 10.1126/science.285.5434.1733. [DOI] [PubMed] [Google Scholar]
- 142.Endo H, Saito A, Chan PH. Mitochondrial translocation of p53 underlies the selective death of hippocampal CA1 neurons after global cerebral ischaemia. Biochem Soc Trans. 2006;34:1283–1286. doi: 10.1042/BST0341283. [DOI] [PubMed] [Google Scholar]
- 143.Murphy PJ, Galigniana MD, Morishima Y, et al. Pifithrin-alpha inhibits p53 signaling after interaction of the tumor suppressor protein with hsp90 and its nuclear translocation. J Biol Chem. 2004;279:30195–30201. doi: 10.1074/jbc.M403539200. [DOI] [PubMed] [Google Scholar]
- 144.Chan WY, Cheung CS, Yung KM, Copp AJ. Cardiac neural crest of the mouse embryo: axial level of origin, migratory pathway and cell autonomy of the splotch (Sp2H) mutant effect. Development. 2004;131:3367–3379. doi: 10.1242/dev.01197. [DOI] [PubMed] [Google Scholar]
- 145.Kirby ML, Gale TF, Stewart DE. Neural crest cells contribute to normal aorticopulmonary septation. Science. 1983;220:1059–1061. doi: 10.1126/science.6844926. [DOI] [PubMed] [Google Scholar]
- 146.Besson WT, Kirby ML, Mierop LHV, Teabeaut JR. Effects of the size of lesions of the cardiac neural crest at various embryonic ages on incidence and type of cardiac defects. Circulation. 1986;73:360–364. doi: 10.1161/01.cir.73.2.360. [DOI] [PubMed] [Google Scholar]
- 147.Nishibatake M, Kirby ML, Mierop LHV. Pathogenesis of persistent truncus arteriosus and dextroposed aorta in the chick embryo after neural crest ablation. Circulation. 1987;75:255–264. doi: 10.1161/01.cir.75.1.255. [DOI] [PubMed] [Google Scholar]
- 148.Bockman DE, Redmond ME, Waldo K, Davis H, Kirby ML. Effect of neural crest ablation on development of the heart and arch arteries in the chick. Am J Anat. 1987;180:332–341. doi: 10.1002/aja.1001800403. [DOI] [PubMed] [Google Scholar]
- 149.Moase CE, Trasler DG. Delayed neural crest cell emigration from Sp and Spd mouse neural tube explants. Teratology. 1990;42:171–182. doi: 10.1002/tera.1420420208. [DOI] [PubMed] [Google Scholar]
- 150.Pani L, Horal M, Loeken MR. Rescue of neural tube defects in Pax-3-deficient embryos by p53 loss of function: implications for Pax-3- dependent development and tumorigenesis. Genes Dev. 2002;16:676–680. doi: 10.1101/gad.969302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Stuart ET, Haffner R, Oren M, Gruss P. Loss of p53 function through PAX-mediated transcriptional repression. EMBO J. 1995;14:5638–5645. doi: 10.1002/j.1460-2075.1995.tb00251.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Fu L, Ma W, Benchimol S. A translation repressor element resides in the 3′ untranslated region of human p53 mRNA. Oncogene. 1999;18:6419–6424. doi: 10.1038/sj.onc.1203064. [DOI] [PubMed] [Google Scholar]
- 153.Mazan-Mamczarz K, Galban S, Lopez De Silanes I, et al. RNA-binding protein HuR enhances p53 translation in response to ultraviolet light irradiation. Proc Natl Acad Sci USA. 2003;100:8354–8359. doi: 10.1073/pnas.1432104100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Appella E, Anderson CW. Post-translational modifications and activation of p53 by genotoxic stresses. Eur J Biochem. 2001;268:2764–2772. doi: 10.1046/j.1432-1327.2001.02225.x. [DOI] [PubMed] [Google Scholar]
- 155.Underwood TJ, Amin J, Lillycrop KA, Blaydes JP. Dissection of the functional interaction between p53 and the embryonic proto-oncoprotein PAX3. FEBS Lett. 2007;581:5831–5835. doi: 10.1016/j.febslet.2007.11.056. [DOI] [PubMed] [Google Scholar]
- 156.Warburg O. On respiratory impairment in cancer cells. Science. 1956;124:269–270. [PubMed] [Google Scholar]
- 157.Warburg O. On the origin of cancer cells. Science. 1956;123:309–314. doi: 10.1126/science.123.3191.309. [DOI] [PubMed] [Google Scholar]
- 158.Kondoh H, Lleonart ME, Gil J, et al. Glycolytic enzymes can modulate cellular life span. Cancer Res. 2005;65:177–185. [PubMed] [Google Scholar]
- 159.Ma W, Sung HJ, Park JY, Matoba S, Hwang PM. A pivotal role for p53: balancing aerobic respiration and glycolysis. J Bioenerg Biomembr. 2007;39:243–246. doi: 10.1007/s10863-007-9083-0. [DOI] [PubMed] [Google Scholar]
- 160.Olivotto M, Caldini R, Chevanne M, Cipolleschi MG. The respiration-linked limiting step of tumor cell transition from the non-cycling to the cycling state: its inhibition by oxidizable substrates and its relationships to purine metabolism. J Cell Physiol. 1983;116:149–158. doi: 10.1002/jcp.1041160205. [DOI] [PubMed] [Google Scholar]
- 161.Doblado M, Moley KH. Glucose metabolism in pregnancy and embryogenesis. Curr Opin Endocrinol Diabetes Obes. 2007;14:488–493. doi: 10.1097/MED.0b013e3282f1cb92. [DOI] [PubMed] [Google Scholar]
- 162.Jungheim ES, Moley KH. The impact of type 1 and type 2 diabetes mellitus on the oocyte and the preimplantation embryo. Semin Reprod Med. 2008;26:186–195. doi: 10.1055/s-2008-1042957. [DOI] [PubMed] [Google Scholar]
- 163.Diamond MP, Moley KH, Pellicer A, Vaughn WK, DeCherney AH. Effects of streptozotocin- and alloxan-induced diabetes mellitus on mouse follicular and early embryo development. J Reprod Fertil. 1989;86:1–10. doi: 10.1530/jrf.0.0860001. [DOI] [PubMed] [Google Scholar]
- 164.Beebe LFS, Kaye PL. Maternal diabetes and retarded preimplantation development of mice. Diabetes. 1991;40:457–461. doi: 10.2337/diab.40.4.457. [DOI] [PubMed] [Google Scholar]
- 165.Chang AS, Dale AN, Moley KH. Maternal diabetes adversely affects preovulatory oocyte maturation, development, and granulosa cell apoptosis. Endocrinology. 2005;146:2445–2453. doi: 10.1210/en.2004-1472. [DOI] [PubMed] [Google Scholar]
- 166.Lea RG, McCracken JE, McIntryre SS, Smith W, Baird JD. Disturbed development of the preimplantation embryo in the insulin-dependent diabetic BB/E rat. Diabetes. 1996;45:1463–1470. doi: 10.2337/diab.45.11.1463. [DOI] [PubMed] [Google Scholar]
- 167.Diamond MP, Harbert-Moley K, Logan J, et al. Manifestation of diabetes mellitus on mouse follicular and pre-embryo development: effect of hyperglycemia per se. Metabolism. 1990;39:220–224. doi: 10.1016/0026-0495(90)90039-f. [DOI] [PubMed] [Google Scholar]
- 168.Diamond MP, Pettway ZY, Logan J, Moley K, Vaughn W, DeCherney AH. Dose-response effects of glucose, insulin, and glucagon on mouse pre-embryo development. Metabolism. 1991;40:566–570. doi: 10.1016/0026-0495(91)90045-x. [DOI] [PubMed] [Google Scholar]
- 169.Pampfer S, DeHertogh R, Venderheyden I, Michiels B, Vercheval M. Decreased inner cell mass proportion in blastocysts from diabetic rats. Diabetes. 1990;39:471–476. doi: 10.2337/diab.39.4.471. [DOI] [PubMed] [Google Scholar]
- 170.Pampfer S, Vanderheyden I, McCracken JE, Vesela J, DeHertogh R. Increased cell death in rat blastocysts exposed to maternal diabetes in utero and to high glucose or tumor necrosis factor-a in vitro. Development. 1997;124:4827–4836. doi: 10.1242/dev.124.23.4827. [DOI] [PubMed] [Google Scholar]
- 171.Leunda-Casi A, Genicot G, Donnay I, Pampfer S, De Hertogh R. Increased cell death in mouse blastocysts exposed to high D-glucose in vitro: implications of an oxidative stress and alterations in glucose metabolism. Diabetologia. 2002;45:571–579. doi: 10.1007/s00125-001-0752-y. [DOI] [PubMed] [Google Scholar]
- 172.Moley KH, Chi MM, Knudson CM, Korsmeyer SJ, Mueckler MM. Hyperglycemia induces apoptosis in pre-implantation embryos through cell death effector pathways. Nat Med. 1998;4:1421–1424. doi: 10.1038/4013. [DOI] [PubMed] [Google Scholar]
- 173.Keim AL, Chi MM, Moley KH. Hyperglycemia-induced apoptotic cell death in the mouse blastocyst is dependent on expression of p53. Mol Reprod Dev. 2001;60:214–224. doi: 10.1002/mrd.1080. [DOI] [PubMed] [Google Scholar]
- 174.Moley KH, Chi MMY, Mueckler MM. Maternal hyperglycemia alters glucose transport and utilization in mouse preimplantation embryos. Am J Phys Endocrinol Metab. 1998;38:E38–E47. doi: 10.1152/ajpendo.1998.275.1.E38. [DOI] [PubMed] [Google Scholar]
- 175.Carayannopoulos MO, Chi MM, Cui Y, et al. GLUT8 is a glucose transporter responsible for insulin-stimulated glucose uptake in the blastocyst. Proc Natl Acad Sci USA. 2000;97:7313–7318. doi: 10.1073/pnas.97.13.7313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Wyman A, Pinto AB, Sheridan R, Moley KH. One-cell zygote transfer from diabetic to nondiabetic mouse results in congenital malformations and growth retardation in offspring. Endocrinology. 2008;149:466–469. doi: 10.1210/en.2007-1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Gilman AG, Goodman LS, Gilman A. The pharmacological basis of therapeutics. Macmillan; New York: 1980. [Google Scholar]