Abstract
Background
Major depressive disorder often is characterized by a lack of cognitive and emotional flexibility, resulting in an impaired ability to adapt to situational demands. Adolescence is an important period of risk for the first onset of depression, yet relatively little is known about whether aspects of inflexibility, such as rumination and deficits in attentional shifting, could confer risk for the development of the disorder during this time.
Method
In the present study, a sample of 285 never-depressed adolescents completed self-report and behavioral measures of rumination and attentional shifting at a baseline visit, followed by up to four years of annual prospective follow-up diagnostic assessments.
Results
Survival analyses indicated that adolescents with greater levels of rumination or poorer attentional shifting experienced a shorter time until the first onset of major depressive episodes, even after accounting for baseline symptoms and demographic characteristics. Although girls were twice as likely as boys to experience the first onset of depression, rumination predicted a shorter time until depression onset only for boys. Rumination and attentional shifting were not correlated and predicted time until onset of major depression independently of one another.
Conclusions
These results provide evidence that components of cognition that are characterized by rigidity and perseveration confer risk for the first onset of major depression during adolescence. Evaluating rumination and attentional shifting in adolescence may be useful in identifying individuals who are at risk for depression and who may benefit from interventions that target or alter the development of these characteristics.
Keywords: Major depressive disorder, rumination, attentional shifting, cognitive flexibility
Major depressive disorder is highly prevalent and its onset increases dramatically during adolescence1. Depressed individuals often demonstrate a lack of cognitive and emotional flexibility, resulting in an impaired ability to adapt to situational demands. For example, depression appears to be characterized by patterns of perseverative thought such as rumination and difficulties appropriately shifting attention between tasks2. These characteristics are relevant to dimensional approaches to understanding potential cognitive mechanisms involved in the etiology of mental disorders, including depression3. Few studies to date, however, have evaluated whether these inflexible cognitive factors precede the first onset of depression in adolescence, and whether they work synergistically to contribute risk for depression.
Rumination, the tendency to passively and repetitively focus on one's dysphoric mood, has been strongly implicated in depression4. Prospective studies have demonstrated that rumination predicts a greater likelihood of onset of new depressive episodes in adults, as well as the first onset of depression in children and adolescents5. The tendency for depressed individuals to ruminate is thought to be in part a consequence of dysregulation of the default mode network (DMN)6, which is activated during periods of rest and self-focus such as rumination. Neural conceptualizations of rumination are consistent with other models that suggest that depression involves a failure to recruit top-down cognitive control of limbic activity7-9.
Attentional shifting, the ability to flexibly redirect the focus of attention between tasks, is an important component of attentional control that is relevant to depression7,10,43. Deficits in attentional shifting ability may represent a failure to engage prefrontal cortical resources to attenuate DMN activity during periods in which task engagement may be necessary, such as in transitioning between mental sets11. Attentional shifting deficits appear to be present among individuals with current or remitted depression relative to controls12,13, although evidence among children and adolescents with depressive disorders is mixed14, particularly during periods of remission15. Furthermore, there is evidence that attentional shifting deficits may be an endophenotype of mood disorders that represent underlying vulnerability12. However, it is not clear whether deficits in attentional shifting in depression are simply state-dependent correlates, scars of previous episodes, or vulnerability factors that may confer risk for the onset of depressive episodes16,43.
Although distinct constructs, attentional shifting and rumination may influence one another. An inability to disengage attention from mood-congruent stimuli in depression may facilitate the prolonged processing of such material via rumination, thereby impairing the ability to use adaptive regulatory strategies such as cognitive reappraisal10,17-19,35-37. Aberrant attentional shifting may result in excessive internally-oriented attention that results in failure to use external stimuli to disengage from rumination, rendering them inflexible to changes in environmental context10,37. Studies have demonstrated an inverse association between attentional shifting and rumination20, particularly in the context of negative emotional information17,21, although this association is less consistent among adolescents, with some studies finding no associations between attentional shifting for neutral stimuli and rumination19,22. Although it is plausible that deficits in attentional shifting and rumination are correlated, attentional shifting and rumination also could work synergistically such that rumination may be particularly likely to lead to depression among individuals who have difficulty switching attention away from ruminative processes. Thus, rumination might be a particular risk factor for depression among adolescents who also have difficulty shifting attention.
In a prior study of adolescents, attentional shifting and rumination were independently associated cross-sectionally with current depression status19. However, cross-sectional and case-controlled designs are unable to determine whether characteristics are true risk factors for the onset of the disorder, or whether they simply are correlates of existing psychopathology23. Although previous studies have indicated that rumination predicts the onset of depressive episodes in children and adolescents, no studies to date have evaluated both attentional shifting and rumination as simultaneous and potentially synergistic predictors of the first onset of major depression. Importantly, no prior studies to our knowledge have evaluated attentional shifting deficits as a predictor of the first onset of depression in adolescence.
In the present study, we sought to extend the existing literature by evaluating attentional shifting and rumination as prospective predictors of depression onset among never-depressed adolescents. We also evaluated sex differences in the relationship between attentional shifting and rumination and depression onset. This was important given that research has found that girls develop a more ruminative response style and higher rates of depression than boys by mid-adolescence1,24. However, the literature has provided mixed evidence about the presence of sex differences in the relationship between rumination and depression during adolescence25, and no studies to our knowledge have evaluated sex differences in the relationship between attentional shifting and first onset of major depression.
Method
Participants
Sample recruitment
Study participants were adolescents who participated in the Adolescent Cognition and Emotion (ACE) Project, a longitudinal study designed to examine the development of depression among Caucasian and African American adolescents. Adolescents were recruited from both public and private middle schools in the Philadelphia area utilizing two methods. Approximately 68% of the sample was recruited from mailings sent out to the Philadelphia School District as well as follow-up phone calls to families, whereas approximately 32% of the sample was recruited from advertisements in Philadelphia area newspapers.
Inclusion criteria included being 12 to 13 years of age at study entry and identifying as Caucasian/White, African American/Black, or Biracial. Further, inclusion criteria specified that adolescents had to have a mother or primary female caregiver accompany them to sessions. Approximately 93.7% of the caregivers were the adolescents' biological mothers, and therefore will henceforth be referred to as mothers. Exclusion criteria in the study included either the adolescent or mother exhibiting an English reading or speaking level inadequate to sufficiently complete study diagnostic interviews and self-report questionnaires, as well as the adolescent or mother exhibiting any psychotic disorder, developmental disorder, or severe learning disability.
Study sample
The study sample included 341 adolescents and mothers who completed the baseline assessment and at least one annual follow-up assessment. Adolescents (Mean age = 12.41 years; SD = 0.63) were diverse in terms of race (50% Caucasian, 50% African American; 2.1% were also Hispanic), sex (53.2% female), and socioeconomic status (44.9% were eligible for subsidized school lunch, a measure of financial need that accounts for the number of dependents being supported by a given family income). Participants in the current study were followed for up to 4.75 years (Mean = 34.13 months, SD = 11.09) and completed an average of 2.19 (SD = 0.91) annual follow-up assessments. Compared to 208 additional adolescents who completed the baseline assessment but did not complete a follow-up assessment, adolescents in the present sample had better attentional shifting scores (t = 2.13, p = .03) and were less likely to receive a free lunch (χ2 = 3.91, p = .05), but did not differ on any other measures or characteristics.
Procedures
All study assessments were held in the Psychology Department building on Temple University's campus. At baseline, adolescents were assessed for depressive diagnoses by a trained diagnostic interviewer. They also completed questionnaires assessing depressive symptoms and rumination, and completed a behavioral task to measure attentional shifting. Adolescents were subsequently assessed every twelve months to determine whether they had experienced the onset of a major depressive episode.
Measures
Depressive Symptoms
The Children's Depression Inventory26 (CDI) is a self-report questionnaire employed to assess depressive symptoms at baseline among adolescent participants. The 27 items are scored on a 0 to 2 scale and are summed to create a total score with higher scores indicating greater depressive symptom severity. In the current sample, total scores ranged from 0 to 32 (Mean = 6.87, SD = 5.59). The CDI has good reliability and validity in youth samples. Cronbach's α in this sample was .86.
Rumination
The Children's Response Styles Questionnaire27 (CRSQ) is a self-report questionnaire administered to adolescents to assess response styles to sad moods. The rumination subscale, which measures self-focused responses to negative affect (e.g., “Think about how alone you feel”), was used in the present study. Each item is measured on a 4-point scale (never, sometimes, often, almost always) reflecting the degree to which adolescents experience each thought or technique in response to depressed mood. Items are summed, with higher scores reflecting a greater tendency to ruminate (M = 24.76, SD = 7.98, Min = 0, Max = 48). The CRSQ has demonstrated good validity and internal consistency in youth samples. In the current sample, the rumination subscale exhibited good internal consistency (α = .85).
Attentional Shifting
The Test of Everyday Attention for Children28 (TEA-Ch) is a neurocognitive test developed for use among children and adolescents ages 6 to 16. The current study utilized one subtest of the TEA-Ch designed to measure attentional shifting, the ability to switch attention from one task or mental set to another. Attentional shifting is associated with some degree of time lapse, or latency, among all individuals. The Creature Counting subtest of the TEA-Ch measures individual differences in this latency. Specifically, the Creature Counting stimulus booklet depicts a varying number of creatures in their burrows on a winding path leading from the top of the page to the bottom of the page. Interspersed between the creatures are up and down arrows. Adolescents are instructed to count the creatures following the path from the top of the page to the bottom of the page, and to switch counting directions when coming upon an up or down arrow. A score is calculated to reflect latency for switching during correct trials only (total time/total switches), which is then scaled so that higher scores represent better attentional shifting (M = 8.56, SD = 2.55, Min = 1, Max = 18). Per scoring instructions and as has been used in prior reports19,28, the attentional shifting variable was created only for adolescents who completed at least 3 of the 7 total trials correctly, which resulted in 21 participants being removed from the sample. Compared to the other participants, these 21 participants displayed lower levels of rumination (t = -2.05, p = .04) and were more likely to be African American (χ2 = 7.29, p = .01), but did not differ from the rest of the sample in any other characteristics. To account for individual differences in psychomotor and processing speed, the TEA-Ch also contains a task (Sky Search) that involves searching for 20 pairs of matching spaceships. The TEA-Ch has good reliability and validity28.
Depression diagnoses
The Kiddie – Schedule for Affective Disorders and Schizophrenia – Epidemiological Version29 (K-SADS-E) is a semistructured diagnostic interview that was administered to adolescents and their mothers at baseline and at 12 month follow-up sessions. The K-SADS-E assesses current and past Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition (DSM-IV-TR; American Psychiatric Association, 2000) Axis I psychopathology in youth. Trained interviewers administered the interview first to mothers and then to adolescents. Based on the K-SADS-E protocol, after administering both interviews, the interviewer would then create a summary rating based on his/her “best-estimate” clinical judgment. Interviewers in the current study were limited to clinical psychology postdoctoral fellows, Clinical Psychology Ph.D. students, individuals with Clinical or Counseling Masters degrees, and post-baccalaureate research assistants. Past research examining the K-SADS-E has demonstrated good inter-rater and retest reliability (κ = .73 for Major Depression29). Inter-rater reliability for the current study was κ = .85 based on 120 pairs of ratings.
The K-SADS-E was administered to adolescents and their mothers to assess the youth's current and lifetime history of depressive diagnoses at baseline. If adolescents had a current or past episode of major depression at baseline (n = 36), they were omitted from the present analyses, which were focused on predicting the prospective first onset of major depressive episodes. This yielded a final sample size of 285. Adolescents who had a history of depression at baseline had higher baseline levels of depressive symptoms (t = 2.11, p = .04) and rumination (t = 2.03, p < .05), and were more likely to be boys (26 boys, 13 girls; χ2 = 4.28, p = .04), but did not differ from the sample included in prospective analyses on attentional shifting (t = 0.13, p = .90) or on any other demographic or study characteristics. The K-SADS-E was subsequently administered at twelve-month follow-up sessions to measure onset of depressive episodes.
Statistical Analyses
Preliminary analyses (t-tests and Chi-square tests) evaluated sex and race differences in study variables. Cox regression (survival) analysis evaluated the primary hypotheses that rumination and deficits in attentional shifting would predict a shorter time until the first onset of major depressive episodes, controlling for individual differences in processing speed, baseline symptoms of depression, sex, and age. We also evaluated whether sex would moderate the relationships between rumination or attentional shifting and time until the first onset of depressive episodes. The proportionality of hazards assumption (which assumes that the predictor variables confer similar risk for first onset of depression over time41) was upheld for all variables in the survival analyses. Rumination and attentional shifting were Z-standardized prior to entering as predictors.
Results
Preliminary Analyses
First, we tested for sex and race differences in baseline study variables. Girls did not differ from boys in levels of rumination (t = 1.01, p = .30) or attentional shifting (t = 0.47, p = .64), but they had marginally higher levels of depressive symptoms (t = 1.70, p = .09). White adolescents did not differ significantly from black adolescents in rumination (t = -1.13, p = .26), attentional shifting (t = -1.20, p = .23), or depressive symptoms (t = -0.35, p = .73). Other baseline correlates are presented elsewhere38.
Contrary to hypotheses, rumination and attentional shifting were not significantly correlated (r = -.02, p = .73).
Prospective Analyses: Predicting First Onset of Major Depressive Episodes
In total, thirty-one adolescents (10.9%) experienced the prospective first onset of a major depressive episode over the follow-up period. The average time from baseline until first onset of depression was 23.67 months (SD = 14.03). As expected, girls were significantly more likely than boys to experience the prospective onset of a major depressive episode (Wald = 4.20, p = .04, HR = 2.17, CI = 1.03-4.55). Race did not predict time until the onset of depression (Wald = 0.22, p = .64, HR = 0.85, CI = 0.43-1.68).
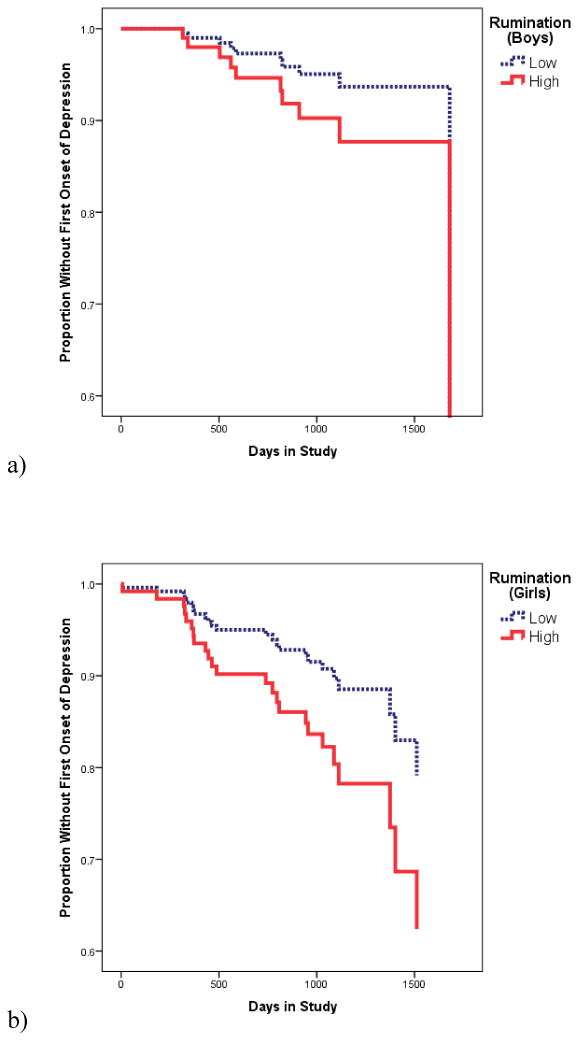
Consistent with hypotheses, multivariate Cox regression analyses indicated that rumination predicted a shorter time until the first onset of a major depressive episode (Wald = 4.73, p = .03, HR = 1.05, CI = 1.01-1.10). However, sex moderated this relationship (Table 1), such that rumination predicted a shorter time until the first onset of a major depressive episode for boys (Wald = 10.10, p = .001, HR = 2.75, CI = 1.47-5.13; Figure 1a1), but not for girls (Wald = 0.02, p = .90, HR = 0.97, CI = 0.63-1.50; Figure 1b).
Table 1. Cox Regression Analyses Evaluating Rumination and Attentional Shifting as Predictors of the First Onset of Major Depressive Episodes in Adolescence.
| Step | Predictor | Wald | p | HR | 95% CI | ΔR2 |
|---|---|---|---|---|---|---|
| 1 | Female | 3.94 | .05 | 2.57 | 1.01-6.53 | .02 |
| Age | 0.36 | .55 | 0.84 | 0.49-1.47 | ||
| Depressive Symptoms | 2.07 | .15 | 1.05 | 0.98-1.12 | ||
| Processing Speed | <0.01 | .96 | 1.00 | 0.94-1.06 | ||
| 2 | Attentional Shifting | 5.71 | .02 | 0.61 | 0.40-0.91 | .03 |
| Rumination | 10.09 | .001 | 2.75 | 1.47-5.14 | ||
| 3 | Rumination X Female | 7.95 | .005 | 0.35 | 0.17-0.73 | .03 |
Note. Change in R2 for Cox regressions represents Cox-Snell R2 change since previous step, an estimate of the relative association between survival and the predictors tested since the previous step.
Figure 1. Survival curves for relationship between rumination (plotted via a median split) and time until first onset of major depressive episode for (a) boys, and (b) girls.
Also consistent with hypotheses, impairments in attentional shifting predicted a shorter time until the first onset of a major depressive episode (Table 1; Figure 2). Sex did not moderate this relationship (interaction term: Wald = 0.02, p = .89, HR = 0.95, CI = 0.43-2.08).
Figure 2. Survival curves for relationship between attentional shifting (plotted via a median split) and time until first onset of major depressive episode.
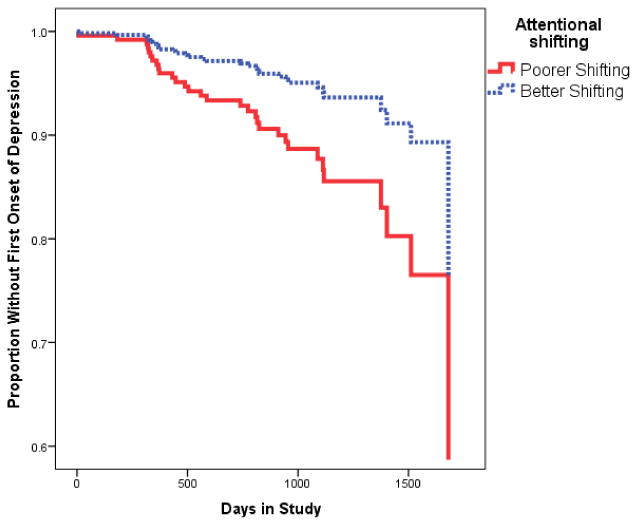
However, attentional shifting did not moderate the relationship between rumination and time until the first onset of a major depressive episode (interaction term: Wald = 0.52, p = .47, HR = 0.88, CI = 0.62-1.25), nor did attentional shifting moderate the two-way interaction between rumination and sex predicting time until depressive episode onset (three-way interaction term: Wald = 0.02, p = .90, HR = 1.06, CI = 0.46-2.44).
Discussion
Cognitive inflexibility may be an important risk factor for the onset of major depressive disorder during adolescence. Indeed, the current study found that both higher levels of rumination and poorer attentional shifting abilities were predictive of a shorter time to first onset of major depression, controlling for baseline depressive symptoms, among a community sample of adolescents. Consistent with prior literature, sex differences emerged in that girls were twice as likely as boys to experience first onset of depression during the course of the study. However, the effects of rumination in predicting episode onset were specific to boys. Rumination and attentional shifting abilities acted as independent predictors; contrary to hypotheses, these constructs were not correlated, and attentional shifting did not moderate the relationship between rumination and depression onset. These results provide evidence that rumination and shifting may be important independent factors in the development of mood disorders in adolescence.
These findings suggest that components of cognitive flexibility are predictive of first onset of major depression during adolescence. Inflexible cognition may contribute to depression by hindering one's ability to problem-solve and adapt to changing situational pressures2. Deficits in attentional shifting have been observed in individuals with current and remitted depression13,43 and previously had been hypothesized to serve as a vulnerability for the development of the disorder12,43. Cognitive inflexibility also may manifest in the form of rumination, a well-established cognitive vulnerability for depression that may impair problem-solving abilities and perpetuate depressed mood4. Indeed, both a neutral test of attentional shifting and a self-report measure of ruminative thinking style predicted first onset of major depression.
One possible shared mechanism by which attentional shifting and rumination may lead to depression is dysregulation in the DMN6. Ruminative thought and impaired attentional shifting abilities could occur in part from difficulties deactivating the DMN in order to attend to the task at hand7. It is possible that these constructs may influence or interact with each other in the development of depressogenic thinking over time, such that shifting deficits may underlie the development of perseverative, ruminative thought or exacerbate the effects of rumination as a risk factor for depression10.
However, the current study found that rumination and impaired attentional shifting were not correlated, served as independent predictors of depression onset, and did not demonstrate an interactive effect in predicting depressive episode occurrence over time within a community sample of adolescents. These results are similar to those reported in a previous cross-sectional study in which clinically depressed adolescents demonstrated higher levels of rumination and poorer attentional shifting abilities compared to controls, but no significant associations were observed between these risk factors19. This suggests that whereas rumination and attentional shifting deficits may both represent facets of inflexible cognition, they exert independent effects in predicting depression onset. These results contrast with some contemporary cognitive theories of depression that have suggested that rumination may result in part from deficits in attentional shifting, as well as with the ability to resolve interference from previously relevant information from working memory7,10,17,18,35-37. However, it is possible that rumination is more relevant to emotional attentional shifting abilities (e.g., difficulty disengaging from negative stimuli)17,20, as opposed to the neutral components of attention evaluated in the current study.
It is somewhat surprising that rumination predicted the first onset of depressive episodes among boys, but not among girls. Although girls demonstrate increased rates of depression onset compared to boys during adolescence1, a result we also observed in this study, findings have been mixed regarding sex differences in the effects of rumination as a risk factor for the disorder25. It is possible that rumination did not confer an additional level of risk among girls in the present study because girls already had increased risk for experiencing depression (i.e., there may have been a ceiling effect for girls). However, it also is possible that among a larger sample (with more participants with a first onset of a depressive episode), the apparently-smaller relationship between rumination and depression onset among girls would become statistically significant. Thus, it may not be the case that rumination does not matter among girls (indeed, the extant literature supports that rumination is an important risk factor for symptoms and episodes of depression among adolescent girls4,5,24,25,30), but rather that the additive influence of rumination among girls appeared to be less strong than among boys, at least within the current sample. It also is possible that the effect of rumination becomes more potent in girls when exposed to interpersonal stress30, which was not evaluated in the present manuscript, or that rumination becomes a stronger predictor of depression for girls later in adolescence.
The current findings have important clinical implications, by suggesting that decreasing rumination and improving attentional control may serve to prevent or alleviate depressive symptoms. Indeed, research has shown that cognitive behavioral therapy that is specifically focused on the reduction of ruminative thought decreased depressive symptoms among individuals with persistent depression31. Furthermore, interventions aimed at improving attentional control, whether through cognitive training protocols or the use of transcranial magnetic stimulation among depressed adults, have been linked to subsequent declines in depressive symptoms. Interestingly, training protocols that increased cognitive control also have been linked to subsequent declines in rumination, suggesting that these constructs may indeed be related32,33. From a prevention standpoint, evaluating rumination and attentional shifting in adolescence may help to identify individuals who are at risk for depression and who may benefit from interventions that target or alter the development of these characteristics.
The use of an initially never-depressed sample allowed for tests of rumination and attentional shifting deficits as true vulnerabilities for the development of the disorder, as opposed to correlates or byproducts of major depression23. The current research examined multiple facets of cognitive inflexibility by assessing both rumination and attentional shifting. Varied methods of data collection were employed including self-report questionnaires, a behavioral test of executive functioning, and a semi-structured diagnostic interview, which reduces the likelihood of shared method variance. As such, the current study's aims are in line with dimensional approaches to understanding psychopathology such as the National Institute of Mental Health's Research Domain Criteria initiative, by examining both aspects of negative valence (rumination) and cognitive systems (attentional shifting) using varied units of analysis3. Furthermore, findings highlight the potential importance of the DMN as an underlying source of risk for the onset of depression that may be responsible for the development of ruminative thought processes and deficits in attentional control.
Several limitations should be noted. As the measure of attentional control employed in this research involved neutral and not emotional stimuli, it will be important to assess whether emotional shifting deficits are a superior predictor of depression onset. In addition, the use of a rumination induction and state measures of ruminative thought may have helped to better evaluate the relationship between perseverative thought and deficits in attentional control. Additionally, adolescents in the prospective sample had better attentional shifting scores and were less likely to receive a free lunch, perhaps limiting the generalizability of these results somewhat to adolescents with these characteristics. Although we evaluated time until the first onset of depression, we did not evaluate predictors of the severity or duration of first depressive episodes. Finally, although results are generally consistent with a proposed imbalance in DMN activity, neural activity and connectivity were not assessed in the current design.
Future research should work towards identifying and characterizing the brain networks that may underlie dysregulation in the DMN, which may manifest in rumination and difficulties shifting attention. It also will be important to better understand the contexts in which these DMN imbalances may be most prominent, such as when at rest, while engaged in cognitively-taxing tasks, or following a negative mood or stress induction7. Given research suggesting that depression onset during early to mid-adolescence leads to impaired development of cognitive control34, as well as findings that rumination is linked to subsequent deficits in attentional abilities in adolescents22, it would be of interest to examine subsequent changes in attentional control over time. It is possible that adolescents at risk for depression possess stunted attentional shifting abilities that both predispose them for the disorder and subsequently remain lower than their nondepressed counterparts as their cognitive development continues; the experience of major depression may further contribute to impairments in cognitive maturation over time. Future work also could benefit from examining the predictive utility of methods of evaluating attentional shifting that are more easily implemented than a behavioral task. For example, the self-reported Attentional Control Scale39 contains a “shifting” subscale that is easy to administer, has been validated with behavioral tasks of attentional shifting, and is concurrently associated with symptoms of depression40. In addition, it would be useful to determine the extent to which the relationship between attentional shifting and first onset of depression is attributable to (or is independent from) general cognitive ability or other cognitive impairments42. Future longitudinal studies could benefit from implementing measures like these to evaluate whether they would have similar utility in evaluating risk for the first onset of depression.
In sum, the current research provides important preliminary evidence of the role of rumination and attentional shifting deficits in the prediction of the first onset of major depression among a community sample of adolescents. Although ruminative thought and impaired attentional control both may be manifestations of cognitive inflexibility resulting from underlying DMN dysregulation, these risk factors were unrelated in the current sample and instead exerted independent effects as predictors of depression onset. Future research should aim to better understand the nature of the relationship between these cognitive vulnerabilities, particularly by elucidating the neural circuitry that may underlie their development and role in predicting the initial development of depression during the pivotal period of adolescence.
Acknowledgments
This work was supported by NIMH grants MH79369 and MH101168 to Lauren B. Alloy. Samantha L. Connolly, Jessica L. Hamilton, Elissa J. Hamlat were supported by National Research Service Awards MH106181, MH106184, and MH102861, respectively, from the National Institute of Mental Health. Taylor A. Burke was supported by a National Science Foundation Graduate Research Fellowship.
Footnotes
The survival curves represent the proportion of the remaining sample that had (a) not yet experienced an episode or (b) not completed their final assessment. The steep drop-off that occurs at the ends of the figures reflects the fact that the length of follow-up differed for each participant, and that few participants remain in the sample at the time that the last participant experienced the first onset of a depressive episode. Sensitivity analyses demonstrated that removing the last participant who experienced a depressive episode attenuated the steep drop-off in the survival figures; however, the results reported here were statistically consistent. Additionally, analyses were repeated using logistic regression to predict the likelihood of first onset of depression, and results paralleled those of the cox regressions, regardless of whether the last participant who experienced a mood episode was included in analyses.
Contributor Information
Jonathan P. Stange, Temple University
Samantha L. Connolly, Temple University
Taylor A. Burke, Temple University
Jessica L. Hamilton, Temple University
Elissa J. Hamlat, Temple University
Lyn Y. Abramson, University of Wisconsin, Madison
Lauren B. Alloy, Temple University
References
- 1.Hankin BL, Abramson LY, Moffitt TE, et al. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. J Abnorm Psychol. 1998 Feb;107(1):128–40. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- 2.Kashdan TB, Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clin Psychol Rev. 2010 Nov;30(7):865–78. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mennin DS, Fresco DM. What, me worry and ruminate about DSM-5 and RDoC? The importance of targeting negative self-referential processing. Clin Psychol Sci Pract. 2013;20:258–267.4. doi: 10.1111/cpsp.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking Rumination. Perspect Psychol Sci. 2008 Sep;3(5):400–24. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- 5.Abela JR, Hankin BL. Rumination as a vulnerability factor to depression during the transition from early to middle adolescence: a multiwave longitudinal study. J Abnorm Psychol. 2011 May;120(2):259–71. doi: 10.1037/a0022796. [DOI] [PubMed] [Google Scholar]
- 6.Whitfield-Gabrieli S, Ford JM. Default mode network activity and connectivity in psychopathology. Annu Rev Clin Psychol. 2012;8:49–76. doi: 10.1146/annurev-clinpsy-032511-143049. [DOI] [PubMed] [Google Scholar]
- 7.Marchetti I, Koster EH, Sonuga-Barke EJ, De Raedt R. The default mode network and recurrent depression: a neurobiological model of cognitive risk factors. Neuropsychol Rev. 2012 Sep;22(3):229–51. doi: 10.1007/s11065-012-9199-9. [DOI] [PubMed] [Google Scholar]
- 8.Hamilton JP, Furman DJ, Chang C, et al. Default-mode and task-positive network activity in major depressive disorder: implications for adaptive and maladaptive rumination. Biol Psychiatry. 2011 Aug 15;70(4):327–33. doi: 10.1016/j.biopsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnstone T, van Reekum CM, Urry HL, et al. Failure to regulate: counterproductive recruitment of top-down prefrontal-subcortical circuitry in major depression. J Neurosci. 2007 Aug 15;27(33):8877–84. doi: 10.1523/JNEUROSCI.2063-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Raedt R, Koster EH. Understanding vulnerability for depression from a cognitive neuroscience perspective: A reappraisal of attentional factors and a new conceptual framework. Cogn Affect Behav Neurosci. 2010 Mar;10(1):50–70. doi: 10.3758/CABN.10.1.50. [DOI] [PubMed] [Google Scholar]
- 11.Halari R, Simic M, Pariante CM, Papadopoulos A, Cleare A, Brammer M, Fombonne E, Rubia K. Reduced activation in lateral prefrontal cortex and anterior cingulate during attention and cognitive control functions in medication-naïve adolescents with depression compared to controls. J Child Psychol Psychiatry. 2009 Mar;50(3):307–16. doi: 10.1111/j.1469-7610.2008.01972.x. [DOI] [PubMed] [Google Scholar]
- 12.Clark L, Sarna A, Goodwin GM. Impairment of executive function but not memory in first-degree relatives of patients with bipolar I disorder and in euthymic patients with unipolar depression. Am J Psychiatry. 2005 Oct;162(10):1980–2. doi: 10.1176/appi.ajp.162.10.1980. [DOI] [PubMed] [Google Scholar]
- 13.Günther T, Konrad K, De Brito SA, et al. Attentional functions in children and adolescents with ADHD, depressive disorders, and the comorbid condition. J Child Psychol Psychiatry. 2011 Mar;52(3):324–31. doi: 10.1111/j.1469-7610.2010.02320.x. [DOI] [PubMed] [Google Scholar]
- 14.Vilgis V, Silk TJ, Vance A. Executive function and attention in children and adolescents with depressive disorders: a systematic review. Eur Child Adolesc Psychiatry. 2015 Apr;24(4):365–84. doi: 10.1007/s00787-015-0675-7. [DOI] [PubMed] [Google Scholar]
- 15.Maalouf FT, Brent D, Clark L, et al. Neurocognitive impairment in adolescent major depressive disorder: state vs. trait illness markers. J Affect Disord. 2011 Oct;133(3):625–32. doi: 10.1016/j.jad.2011.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hasselbalch BJ, Knorr U, Kessing LV. Cognitive impairment in the remitted state of unipolar depressive disorder: a systematic review. J Affect Disord. 2011 Nov;134(1-3):20–31. doi: 10.1016/j.jad.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 17.Grafton B, Southworth F, Watkins E, MacLeod C. Stuck in a sad place: Biased attentional disengagement in rumination. Emotion. 2016 Feb;16(1):63–72. doi: 10.1037/emo0000103. [DOI] [PubMed] [Google Scholar]
- 18.Koster EH, De Lissnyder E, Derakshan N, De Raedt R. Understanding depressive rumination from a cognitive science perspective: the impaired disengagement hypothesis. Clin Psychol Rev. 2011 Feb;31(1):138–45. doi: 10.1016/j.cpr.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Wilkinson PO, Goodyer IM. Attention difficulties and mood-related ruminative response style in adolescents with unipolar depression. J Child Psychol Psychiatry. 2006 Dec;47(12):1284–91. doi: 10.1111/j.1469-7610.2006.01660.x. [DOI] [PubMed] [Google Scholar]
- 20.De Lissnyder E, Koster EH, Derakshan N, De Raedt R. The association between depressive symptoms and executive control impairments in response to emotional and non-emotional information. Cogn Emot. 2010;24:264–280. [Google Scholar]
- 21.Hilt LM, Leitzke BT, Pollak SD. Cognitive Control and Rumination in Youth: The Importance of Emotion. J Exp Psychopathol. 2014;5(3):302–313. doi: 10.5127/jep.038113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Connolly SL, Wagner CA, Shapero BG, et al. Rumination prospectively predicts executive functioning impairments in adolescents. J Behav Ther Exp Psychiatry. 2014 Mar;45(1):46–56. doi: 10.1016/j.jbtep.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Just N, Abramson LY, Alloy LB. Remitted depression studies as tests of the cognitive vulnerability hypotheses of depression onset: a critique and conceptual analysis. Clin Psychol Rev. 2001 Feb;21(1):63–83. doi: 10.1016/s0272-7358(99)00035-5. [DOI] [PubMed] [Google Scholar]
- 24.Hamilton JL, Stange JP, Abramson LY, Alloy LB. Stress and the Development of Cognitive Vulnerabilities to Depression Explain Sex Differences in Depressive Symptoms during Adolescence. Clin Psychol Sci. 2015 Sep 1;3(5):702–714. doi: 10.1177/2167702614545479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abela JRZ, Hankin BL. Cognitive vulnerability to depression in children and adolescents: A developmental psychopathology perspective. In: Abela JRZ, Hankin BL, editors. Handbook of depression in children and adolescents. New York: Guilford; 2008. pp. 35–78. [Google Scholar]
- 26.Kovacs M. The Children's Depression, Inventory (CDI) Psychopharmacol Bull. 1985;21(4):995–8. [PubMed] [Google Scholar]
- 27.Abela JRZ, Vanderbilt E, Rochon A. A test of the integration of the response styles and social support theories of depression in third and seventh grade children. J Soc Clin Psychol. 2004;23:653–674. [Google Scholar]
- 28.Manly T, Robertson IH, Anderson V, Nimmo-Smith I. The Test of Everyday Attention for Children (TEA-Ch) Bury St. Edmunds, England: Thames Valley Test Company; 1999. [Google Scholar]
- 29.Orvaschel H. Schedule for Affective Disorders and Schizophrenia for School-Age Children - Epidemiologic Version-5 (K-SADS-E) Nova Southeastern University; Ft. Lauderdale, FL: 1995. [Google Scholar]
- 30.Abela JR, Hankin BL, Sheshko DM, et al. Multi-wave prospective examination of the stress-reactivity extension of response styles theory of depression in high-risk children and early adolescents. J Abnorm Child Psychol. 2012 Feb;40(2):277–87. doi: 10.1007/s10802-011-9563-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Watkins ER, Mullan E, Wingrove J, et al. Rumination-focused cognitive-behavioural therapy for residual depression: phase II randomised controlled trial. Br J Psychiatry. 2011 Oct;199(4):317–22. doi: 10.1192/bjp.bp.110.090282. [DOI] [PubMed] [Google Scholar]
- 32.Hoorelbeke K, Koster EH, Vanderhasselt MA, et al. The influence of cognitive control training on stress reactivity and rumination in response to a lab stressor and naturalistic stress. Behav Res Ther. 2015 Jun;69:1–10. 33. doi: 10.1016/j.brat.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 33.Siegle GJ, Price RB, Jones NP, Ghinassi F, Painter T, Thase ME. You gotta work at it: Pupillary indices of task focus are prognostic for response to a neurocognitive intervention for rumination in depression. Clin Psychol Sci. 2014;2:455–471. [Google Scholar]
- 34.Vijayakumar N, Whittle S, Yücel M, et al. Impaired Maturation of Cognitive Control in Adolescents Who Develop Major Depressive Disorder. J Clin Child Adolesc Psychol. 2015 Feb;20:1–13. doi: 10.1080/15374416.2014.987381. [DOI] [PubMed] [Google Scholar]
- 35.Joormann J, Nee DE, Berman MG, et al. Interference resolution in major depression. Cognitive Affective Behavioral Neuroscience. 2010;10:21–33. doi: 10.3758/CABN.10.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Joormann J, Vanderlind WM. Emotion Regulation in Depression: The Role of Biased Cognition and Reduced Cognitive Control. Clin Psychol Sci. 2014;2(4):402–21. [Google Scholar]
- 37.Pe ML, Raes F, Koval P, et al. Interference resolution moderates the impact of rumination and reappraisal on affective experiences in daily life. Cogn Emot. 2013;27(3):492–501. doi: 10.1080/02699931.2012.719489. [DOI] [PubMed] [Google Scholar]
- 38.Alloy LB, Black SK, Young ME, et al. Cognitive vulnerabilities anddepression versus other psychopathology symptoms and diagnoses in earlyadolescence. J Clin Child Adolesc Psychol. 2012;41(5):539–60. doi: 10.1080/15374416.2012.703123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Derryberry D, Reed MA. Anxiety-related attentional biases and their regulation by attentional control. J Abnorm Psychol. 2002 May;111(2):225–36. doi: 10.1037//0021-843x.111.2.225. [DOI] [PubMed] [Google Scholar]
- 40.Judah MR, Grant DM, Mills AC, Lechner WV. Factor structure and validation of the Attentional Control Scale. Cogn Emot. 2014 Apr;28(3):433–51. doi: 10.1080/02699931.2013.835254. [DOI] [PubMed] [Google Scholar]
- 41.Tabachnik BG, Fidell LS. Using multivariate statistics. 5. Boston, MA: Pearson; 2007. [Google Scholar]
- 42.Gale CR, Deary IJ, Boyle SH, et al. Cognitive ability in early adulthood and risk of 5 specific psychiatric disorders in middle age: the Vietnam experience study. Arch Gen Psychiatry. 2008 Dec;65(12):1410–8. doi: 10.1001/archpsyc.65.12.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kilford EJ, Foulkes L, Potter R, Collishaw S, Thapar A, Rice F. Affective bias and current, past and future adolescent depression: a familial high risk study. J Affect Disord. 2015 Mar 15;174:265–71. doi: 10.1016/j.jad.2014.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]


