Abstract
Climate change is anticipated to alter the production, use, release, and fate of environmental chemicals, likely leading to increased uncertainty in exposure and human health risk predictions. Exposure science provides a key connection between changes in climate and associated health outcomes. The theme of the 2015 Annual Meeting of the International Society of Exposure Science—Exposures in an Evolving Environment—brought this issue to the fore. By directing attention to questions that may affect society in profound ways, exposure scientists have an opportunity to conduct “consequential science”—doing science that matters, using our tools for the greater good and to answer key policy questions, and identifying causes leading to implementation of solutions. Understanding the implications of changing exposures on public health may be one of the most consequential areas of study in which exposure scientists could currently be engaged. In this paper, we use a series of case studies to identify exposure data gaps and research paths that will enable us to capture the information necessary for understanding climate change-related human exposures and consequent health impacts. We hope that paper will focus attention on under-developed areas of exposure science that will likely have broad implications for public health.
Keywords: climate change, exposure science, extreme events, indoor environments, non-targeted analysis, sensors
Subject terms: Risk factors, Climate-change impacts, Environmental monitoring
INTRODUCTION
Environmental changes—local, regional and global—are accompanying changes in climate. These environmental changes will alter exposures to chemical, physical, and other stressors that have the potential to produce new or exacerbated adverse impacts on human health.1, 2, 3 For example, the Interagency Working Group on Climate Change and Health4 hypothesized that humans will experience increased prevalence of respiratory diseases due to greater exposures to pollen, molds, air pollution, aerosolized marine toxins and dust. Climate change may further exacerbate existing cardiovascular disease due to heat stress and higher exposures to airborne particles.4
As was pointed out by the U.S. Global Change Research Program,5 “…the ability to evaluate, track, and project health effects varies across climate impacts. For instance, health outcomes differ in terms of whether complete, long-term datasets exist that allow us to quantify observed changes, and whether existing models are able to project impacts at the time scales and geographic scales of interest. …” The USGCRP further acknowledged the need for data that can be used to characterize the impacts of climate change on human health.
Exposure science provides a key connection between changes in climate and associated health outcomes. The theme of the 2015 Annual Meeting of the International Society of Exposure Science (ISES)—Exposures in an Evolving Environment—brought this issue to the fore (meeting abstracts are available at http://isesweb.org/Meetings/Docs/ISES2015_AbstractBook%20FINAL.pdf). By directing attention to questions that have the potential to affect society in profound ways, exposure scientists have an opportunity to conduct what Michael Brauer, Professor at the School of Population and Public Health, University of British Columbia and ISES’s 2015 Wesolowski Award winner referred to as “consequential science”—doing science that matters and using our tools for the greater good.
When planning exposure science research in an age of climate change, exposure scientists should be cognizant of the fact that the Earth is not experiencing a “new normal” but is instead evolving as a result of on-going and continuous climate change that includes natural modes of climate variability, but that also includes increasingly dominant influences of human-driven change.6, 7 Research hypotheses and approaches will therefore also have to address the complications arising not only from the fact that climate change-related impacts will be situation-, chemical class-, location-, season-, and source-specific,8 but will also be a moving target. Further, research approaches will be driven by temporal, geographical and data collection considerations. For example, melting of glacial ice may reintroduce persistent organic pollutants into the environment9 resulting in higher levels of these chemicals in fish in Arctic diet;10 exposure data needs for this issue would be geographically circumscribed and local entities may be appropriate for conducting the research. In contrast, geographic changes for vector-borne infectious diseases may require research over large areas (e.g., several countries) and include multiple research groups. Other types of predicted changes in human exposures related to climate change include: changes in exposures to pesticides and other contaminants in water used for irrigation associated with modifications to agricultural practices;11 changes in fate and transport processes for chemicals and pathogens;11 increased ozone exposures, allergen exposures, chemical exposures associated with wildfires, thermal extremes, exposures associated with extreme weather events, vector-borne infectious diseases, food- and water borne diseases, and exposure to harmful algal blooms;12 and indoor and outdoor exposures related to dampness and flooding.13 These exposures are unlikely to be temporally constant, but will rather continue to shift as the globe continues to respond to climate change.
Exposure scientists will need to consider a range of tools and be flexible and creative in facing the difficult and complex challenges posed by climate change. How can exposure scientists plan for the near and more distant future? What kind of novel exposure metrics can be used to measure individual level “exposure” to climate change? Which tools are available now and which will need to be developed? What kinds of skill sets are needed and who can participate in collecting data?
To our knowledge, a wide-reaching exploration of areas in which exposure scientists can contribute to our understanding of the impacts of climate change on human exposures has not been conducted. In this paper, we identify various important climate change-related exposure data gaps and research paths in a series of case studies. Each case study examines key research needs or approaches that vary in geographic and temporal scale, chemical/stressor type(s), and type of personnel needed; the case studies each conclude with proposed key areas of research that can provide the foundation for understanding how changes in exposures affect human health (Figure 1). As noted above, the 2015 ISES Meeting was an important motivation for this paper and for the case study topics presented.
Figure 1.
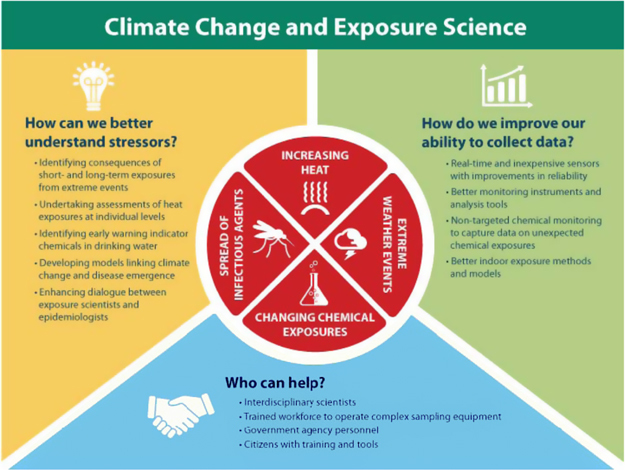
Research needs for exposure science and climate change.
CASE STUDIES
The following case studies describe three overarching areas of importance for exposure scientists researching climate change: (i) issues associated with specific stressors or environments considered here to be a priority in terms of public health protection; (ii) available and developing instruments and analytical approaches for assessing climate change-related exposures; and (iii) strategies for increasing the collection of exposure data by involving non-traditional stakeholders.
Stressors/Environments
Exposure science-related issues and paths forward associated with four climate change-related stressors are described here: chemical and biological exposures associated with extreme events, methods for assessing heat exposure, climate change and infectious disease agents, and disinfection byproducts (DBPs) and drought.
Chemical and Biological Exposures from Extreme Events
The US and other parts of the world are experiencing climate-related regional changes in the frequency and intensity of a variety of extreme events such as severe storms, flooding rains, hurricanes, droughts, and wildfires.12, 14, 15
The US Global Change Research Program’s Third National Climate Assessment provides a thorough examination of extreme events that have been and will be altered by climate change in the US.12 The results from this examination indicate that precipitation, hurricanes, droughts, and severe storms will change in magnitude and severity in the future.
Extreme events can cause a variety of well-known health risks including death or injury associated with hurricanes and floodwaters. There is less research on the long-term health ramifications after the extreme event has struck a location, which can occur from weeks to years after the event has left an area. These negative outcomes can be due to a loss of infrastructure and public services, degradation of ecosystem services, loss of economic stability, damage to property, and destruction of facilities that contain or house hazardous material.16, 17
Monitoring health outcomes of extreme events poses a variety of difficulties.18 The interactions between extreme events and potential health impacts are affected by geography and landscape, response of local populations, and vulnerable populations.19 This becomes especially difficult to monitor if the biological or chemical threats released by the extreme event are transported to locations away from the event. For example, heavy precipitation and flooding can quickly mobilize and transport contaminants to new locations causing hazards that can be overlooked by those monitoring or providing surveillance of health outcomes, because the contamination is outside the area being investigated.20 Populations also move away from the impacted areas to escape the disaster or for economic reasons.21 As these displaced populations can be difficult to track, monitoring health exposures and outcomes after an extreme event might not capture the full extent of the populations impacted.
Droughts pose further difficulties because of their slow evolving nature and because they cause other extreme events, such as dust storms and wildfires, which can increase air quality hazards and also transfer chemical or biological hazards over long distances.22, 23 Increased indoor and outdoor air pollution and health effects have been associated with populations thousands of kilometers downwind from the fires.24, 25
To accurately identify and assess exposures that impact human health after extreme events, research is needed to identify the long and short-term potential chemical and biological exposures associated during and after each event type. This will require long-term efforts because as noted above, exposures can occur both during and after the event and at locations at the event as well as far off-site. Exposure scientists should engage with public health officials responsible for monitoring to ensure that long-term monitoring includes relevant biological and chemical exposures related to various extreme events. As each extreme event can manifest its own unique issues, researchers will need to be flexible and creative in order to capture the unique exposures related to each event.
Assessing heat exposure: An increasing body of literature indicates that the frequency, duration, and intensity of extreme events are on the rise in response to our changing climate and will continue to be for the foreseeable future.7, 15, 26 Investigations into how changes in extreme events—including extreme temperature—impact public health require a robust exposure metric that can be used in epidemiological studies to generate empirical evidence linking exposures to extreme heat and impaired health.
Globally, record daytime and nighttime high temperatures have increased. Today, in the US, a record high temperature is twice as likely to be broken as a record low, and night time temperature records show a strong upward trend.27 Increases in extreme heat may impact health in many ways, with effects ranging from hospitalizations for cardiovascular and cerebrovascular diseases to mortalities and other heat-related illness, some of which are mediated through air pollution.28, 29, 30, 31, 32 To quantify the empirical evidence regarding heat exposures and impaired health, epidemiological studies have relied on different exposure metrics. Strengths and weaknesses of these metrics are briefly described here; harmonization of metrics to improve our ability to interpret heat-related exposure data is needed.
Average temperatures: Average outdoor temperature, often used by epidemiologists to investigate heat-related acute health outcomes,33, 34 include average daily, weekly or monthly temperature, or average of maximum daily temperature over week, months or season. Although these metrics may have excellent spatial or temporal coverage for short study duration and are very useful in the study of acute health outcomes, they represent weather as opposed to climate and provide no information on local climatology.
Heat waves: Heat waves are commonly defined as a certain number of consecutive days exceeding location-specific thresholds.35 Thus, frequency and duration of heat waves by definition address climate variability, whereas long-term changes in the patterns of these heat wave characteristics provide information on changing climate. One major drawback to using this exposure metric is frequency (e.g., heat waves are uncommon in substantial parts of the US) and inability to capture isolated days where high maximum temperature may have direct implications for health.
Extreme heat events: Extreme heat events are calculated based on local climatology derived using a long baseline (usually 30 years). This metric overcomes the limitation of infrequency (such as in the case of heat waves), considers the local climatology of an area, can be specific to a time of year (day of year, calendar month, or season), and can be created from a baseline of relative (percentile value) or absolute values (measure of temperature) that show the change over a long period of time and responds well to large-scale climate phenomena such as El Niño Southern Oscillation (ENSO) events.36
Several data sources can be used to derive extreme heat-related exposure metrics. The CLIMDEX project has produced a suite of indices for the more extreme aspects of climate. The indices use daily temperature data from both gridded and station-based datasets and are used in global and regional research;37 however, they are dependent on the operational schedule of observation stations and have a varying temporal scale. To our knowledge, none of the 27 metrics created by the CLIMDEX project have been used in epidemiological studies.
Another source of data derives from the National Environmental Public Health Tracking (EPHT) program, a US effort managed by the Centers for Disease Control and Prevention (CDC). EPHT, which includes historical and future projections of extreme hot temperature indicators, relies on the North American Land Data Assimilation System data that are converted into county-level estimates. EPHT historical extreme hot temperature indicators span from 1979 to present date. These metrics were successfully used in a study of mortality and morbidity in several US states.38
When creating or using extreme heat metrics, exposure scientists should consider the differences between station-level measurements versus gridded data. The gridded data are generated using statistical interpolation, which tend to smooth the extreme values that are of most interest, in this particular case. Station-level data may not be consistently available and will often have poor spatial resolution. Furthermore, future studies are needed to characterize how such extreme heat metrics are influenced by naturally occurring inter-annual and decadal oscillation patterns, and how such impact varies across season and geographic regions.
Although research on impacts of extreme heat have focused on ambient temperatures, indoor spaces can be a significant modifying factor. The presence or absence of air conditioning and the amount of time spent indoors can have important implications for assessing “heat” exposure, as can frequency of window opening.39 For example, McCormack et al.40 found that increasing indoor temperature impacted COPD morbidity. Advances in wearable temperature-sensing technology will greatly enable assessments of heat exposure at the personal level and will lead to potentially important adaptive strategies for avoiding excessive heat exposures.
In summary, the temporal aspect of climate change must be reflected in the heat metric used by exposure scientists. Changing characteristics of extreme events will be a critical reflection of changing variance. A dialog among exposure scientists and epidemiologists on strengths and weaknesses as well as harmonization of different exposure metrics and assessment strategies (incorporating aspects of indoor versus outdoor exposures), and on distinguishing the role of natural climate variability versus changing climate, is needed for enhancing comparison of findings across studies.
Climate change and exposure to infectious disease agents
A large number of infectious disease agents cause morbidity and mortality both in the US and abroad, including foodborne, water borne, vector borne, zoonotic, and soil-associated agents. In the US, the burden of illness caused by infectious diseases each year is substantial. Foodborne diseases alone, many of which have strong links to the environment, are estimated to cause 9.4 million episodes of illness, resulting in 55,961 hospitalizations and 1351 deaths.41 Waterborne diseases are also important, with between 4.26 and 11.69 million annual cases of acute gastrointestinal illness attributed to public drinking water systems in the US.42 Approximately 75% of all recently emerging infectious diseases in humans, including diseases such as Lyme disease, West Nile virus infection, SARS, and avian influenza originated in animals43 with emergence often associated with ecological change.44 Vector-borne diseases remain highly important in the US. The number of Lyme disease cases is estimated at 300,000 cases per year,45, 46 and since its introduction in 1999, over 3 million West Nile virus infections have resulted in close to 780,000 illnesses.47
Climate disruption has had a significant impact on the environment, and in future years will have an increasingly important role as a driver of changes in the ecology of these diseases, influencing both disease incidence and distribution. Severe storms, heat waves, and weather patterns have been linked to outbreaks of many environmentally-sensitive infectious diseases. West Nile Virus transmission intensity has been associated with warmer than normal summer temperatures.48 Rift Valley Fever outbreaks in East Africa have been correlated with ENSO events.49 Plague transmission in the Southwest and Rocky Mountain region has been linked to temperature and rainfall patterns leading to increases in wild rodent populations.50 Water-borne disease outbreaks have been associated with heavy rains and also with drought conditions.51, 52, 53
It is very challenging to link changes in transmission patterns of infectious diseases directly to climate change for multiple reasons. First, climate change takes place very slowly, requiring disease surveillance data to be collected systematically and consistently over many years. Second, meaningful correlations rely on multifactorial datasets consisting of both disease surveillance and weather data, collected over comparable temporal and spatial scales. For example, exposure to precipitation, soil moisture, and humidity could impact infectious disease research, particularly for respiratory and vector-borne diseases. Third, and perhaps most significant, climate is the only one of a multitude of possible ecological and epidemiologic factors that mediate disease risk in humans.54 For example, it has been suggested that climate change and El Niño are contributing factors to the current Zika epidemic in the Americas.55 Although this is within the range of possibility, attribution is particularly challenging without knowing the relative contribution of numerous other factors including global travel and the frequency and range of movement of infected humans, poverty and overcrowding, introduction of the disease into an immunologically naïve human population, and limited public health resources in some affected areas. Progress is being made, however, in understanding how the multiple drivers of disease emergence work together and interact with weather patterns and trends associated with climate change.
Research priorities include strengthening public health surveillance for the purpose of establishing baselines, tracking climate-sensitive disease trends, and validating change in disease occurrence patterns over time. Exposure scientists can enhance this effort by working across disciplines to help improve surveillance systems needed to define the critical linkages between climate change, weather, environmental change and disease emergence and to develop predictive models.
DBPs and drought
Climate change will likely significantly affect our water resources. Climate change is already linked to prolonged and severe droughts in many parts of the US, notably in the Southeast and Western states. In addition to placing restraints on fresh water resources, droughts concentrate contaminants in rivers and lakes. Contaminants enter surface waters through several routes, including treated wastewater effluents, agricultural run-off and historical industrial activity, and during times of drought, these contaminants will concentrate in these surface waters; in fact, some rivers can become composed primarily of treated wastewater. Prime examples include the Santa Ana River in Southern California, which is 90% treated wastewater during the dry season, from April through October,56 and the Trinity River in Texas, which consists almost entirely of wastewater effluent under base flow conditions.57
In addition to contaminants, natural organic matter (NOM) and bromide and iodide (Br− and I-) salts concentrate in rivers during times of drought,58 which will react with chlorine and monochloramine during drinking water disinfection to form hypobromous acid and hypoiodous acid, which in turn react with NOM to produce brominated and iodinated DBPs.58 Because brominated and iodinated DBPs have greater toxicity compared to chlorinated DBPs,58 the link between climate change-related drought and adverse human health effects is an important area of research for exposure scientists. In addition, many anthropogenic contaminants can react with disinfectants to form DBPs.59, 60 Notable examples include iopamidol, a medical imaging compound, which reacts with chlorine to form the highly genotoxic DBP iodoacetic acid,61 and the fungicide tolylfluanide, which reacts with ozone to form the carcinogenic DBP N-nitrosodimethylamine (NDMA).62
Drought also results in less desirable water sources being used for potable drinking water, including brackish groundwater and seawater, as well as reuse of wastewater. In fact, many coastal cities such as Hong Kong use seawater for toilet flushing, and disinfection of these waters can produce more toxic brominated and iodinated DBPs, which could adversely impact marine ecosystems.63, 64, 65, 66 Wastewater reuse, which is less expensive than seawater desalination, is gaining public acceptance and has already been adopted in Singapore, as well as Orange County California, both of which use advanced treatment and recharge before potable use. In addition to droughts, climate change can also induce extreme weather events like floods, which result in more run-off of fertilizers, pesticides, NOM, and other materials that further complicate disinfection and DBP formation chemistry.
Exposure scientists can elucidate the impacts of climate change-related drought by identifying indicator chemicals for drinking water and wastewater facilities that are readily measureable and could serve as early warnings of system stress associated with climate change. These chemicals could include Br− and I− and possibly other important, emerging contaminants that form toxic DBPs in drinking water treatment. It is also imperative to find cost-effective ways to remove Br−, I−, and total organic carbon as well as important wastewater chemicals that can serve as toxic DBP precursors. Safe tap water is central for public health and exposure science is key to understanding how climate change-related drought impacts tap drinking water exposures and health.
Instruments/Analytical Approaches
Exposure science instrumentation and analytical approaches are crucial for addressing health impacts associated with climate change. The following examples are described here: use of sensors in data collection, advances in non-targeted chemical analyses, and analytical approaches for assessing changes in exposures in indoor home environments.
Sensors
Small sensors are a relatively new research technology that is rapidly gaining in popularity. Historically, small sensors were typically relegated to commercial applications using proprietary hardware and software. The recent rise of small sensor methods is likely attributable to the widespread availability of inexpensive microprocessor boards and the rapid growth of open source version websites67 that store user-updated control software. Using these techniques, it is now possible for even an untrained layperson to follow directions to construct innovative approaches to measurements.
The US EPA delineates five broad tiers of air pollution sensors,68 with the highest tiers (tiers 3–5) mainly within the domain of advanced research, high sensitivity, and regulatory action communities. Tiers 1 and 2 are comprised of relatively inexpensive (<$1000 USD, and often much <$100) sensors that generally offer a lower level of precision, accuracy, and chemical specificity. Because of this low price point and reasonable, if uncertain, accuracy, these sensors are most commonly used by citizen scientists, advocacy groups, and even some academic investigators. In the context of climate change, small sensors hold promise in monitoring of both environmental conditions, as well as personal human exposure.
Sensors are versatile in their capabilities, detecting, for example, most of the criteria pollutants including PM, ozone, and carbon monoxide, VOCs, occupational hazards, and numerous physical and meteorological metrics. These methods typically employ electrochemical, thermal resistance, or optical photometer or fluorescence techniques. Several sensors also address biological endpoints, such as electrocardiography, pulse oximetry, or motion. Small sensors have utility in informing across many aspects of climate change effects, which include air quality, meteorology, water quality, human health responses, and others. Depending on hardware, some sensors can report measurements each second, though this is often at ineffectively high-method detection limits. Because sensors are low cost, easy to build and deploy, and are capable of producing prodigious quantities of data, caution is warranted in managing the large datasets that can be produced, and how to best address the voluminous information provided. Further, sensors rarely include robust quality assurance procedures, an essential component of any measurement. This is an important consideration of small sensor use where quality and precision of sensors vary greatly across manufacturer and technology, with some sensors observed to have a high degree of inaccuracy and imprecision. A significant open question to be addressed is calibrating and validating a sensor measurement; lacking this, the reported values are little more than an approximation. This can also be an important concern with commercialized small sensors, where consumers are left to interpret this uncertain data.
Despite these concerns, there are plausible opportunities to integrate inexpensive, small-sensor initiatives in monitoring for exposure effects related to climate change, particularly for long-term monitoring in logistically difficult locations (e.g., remote locations) or where there is a high risk of loss or damage. Because of their low cost, many sensors can be densely distributed across spatial domains, or they can be effectively installed within personal microenvironments (homes, workplaces, etc.) to address monitoring approaches not reflected by traditional ambient monitors. This makes small sensors particularly advantageous for investigations centered on environmental justice issues, transient or spatially diffuse events, or for long-term trend monitoring.
Exposure scientists should consider incorporating sensor technologies into their assessment of climate change-related exposures. However, careful consideration of limitations associated with data reliability and interpretation is required. Novel do-it-yourself sensors hold great promise for expanding the reach of scientific inquiry, including a wider range of stakeholders by engaging citizen scientists, and ultimately in answering many key exposure questions in more sustainable and creative ways.
Non-targeted analysis
Climate change is anticipated to alter the production, use, release, and fate of environmental chemicals, likely leading to increased uncertainty in exposure and risk predictions.8 New computational and analytical tools are being rapidly developed that will facilitate more efficient and tractable assessments of chemical safety (http://www2.epa.gov/research/chemical-safety-sustainability-strategic-research-action-plan-2016-2019) and are therefore a means to address this uncertainty. These 21st century tools now need to be honed to both anticipate (via models) and screen (via measurements) for alterations in chemical exposure profiles as a function of changing climate. One emerging screening tool, known as non-targeted analysis (NTA), holds tremendous promise for tracking climate change effects on chemical exposures and environmental health.
With respect to the vast number of environmental chemicals (synthetic and natural), monitoring data are quite limited, with most laboratories examining few priority chemicals during routine analyses. For example, whereas more than 80,000 chemicals are listed on the US Toxic Substances Control Act (TSCA) inventory,69 only a few hundred are monitored in human biological specimens as part of a recurring national survey.70 The lack of monitoring data stems, in part, from reliance on targeted analytical methods for environmental health research, which are ideal for compliance monitoring for small sets of “known” chemicals, but not well-suited for the broad discovery of chemical “unknowns;” understanding exposures to “unknowns” will be essential as the chemical-specific impacts of climate change are not currently well-understood.
Non-targeted analysis methods are those that assign chemical formulas and structures to unknown compounds without the use of reference standards or target substance lists.71 Instruments coupling gas chromatography or liquid chromatography with high-resolution mass spectrometry are most commonly used for NTA. These methods, and similar “suspect screening” methods, have been successfully applied to characterize chemical unknowns in environmental media including water,72 lake sediment,73 dust,74 food,75 and products;76 and in biological media including animal tissue,77 and human blood,78 urine,79 and teeth.80
Mathematical models for forecasting modulations in chemical exposures as a function of climate change suggest shifts in chemical use patterns, environmental fate and transport processes, and exposure pathways.8, 11 These changes will likely ultimately manifest as alterations in the chemical content of many, if not all, media. Given these anticipated changes, NTA methods, in combination with existing targeted methods, are necessary to efficiently monitor and catalog changes in chemical exposure profiles. Vast amounts of new data generated from NTA must then be mined, using cutting edge data science techniques, to evaluate the impacts of changing chemical exposures on human and environmental health.
Proper utilization of these methods will require a fundamental shift in routine monitoring strategies. It is likely not feasible in the short term (0–3 years) for individual laboratories, currently using only targeted methods, to consider routine application of NTA methods. However, steps can be taken now to ensure that NTA methods are viable for most analytical labs within the next decade. Widespread application of NTA methods will require effective leveraging of pooled resources—specifically, sharing of curated chemical libraries, mass spectral databases, authentic chemical standards, and data processing/analysis software. Official laboratory networks and research consortia will also be necessary to facilitate broad coverage geographically, temporally, and across media. With proper planning and communication, it is likely that new monitoring networks will be established within the US and worldwide within the next decade (see, e.g., the NORMAN Network: http://www.norman-network.net/). Exposure and climate scientists are therefore strongly encouraged to begin collectively considering how these NTA methods and monitoring networks can be used to test research hypotheses that link modifications in chemical exposure with changing climate. 81, 82
Methods for biological agents in indoor home environments
In a changing climate, it is anticipated that acute (e.g., hurricanes and flooding) and chronic (e.g., changing profiles in outdoor pollen and indoor allergens and microbes) events will affect exposures to biological agents in the indoor environment.83 Indoor air often contains biogenic agents including bacteria, fungi, and allergens from plants (pollen) and animals (dust mites, insects, rodents and furry pets).84 Microbial agents and pollens infiltrate homes from outdoors; once inside, microorganisms find surfaces that can provide nutrient and moisture sources sufficient for growth. On the other hand, animal allergens have exclusive niches inside the home because of the presence of the organisms from which they are derived.
The current methods for assessing indoor biological agents include questionnaires administered to residents, inspection by trained technicians, dust sampling, and air sampling. Although reporting the presence of a pet is straightforward, dust mite exposure assessment often relies upon dust sampling followed by immunoassay for the allergen(s) (Chew et al.85). Air sampling is required for pollen grain and mold spore assessment; however, some allergen assays have been developed, which enable assessment of their allergen content in dust samples.86, 87 In addition, researchers have focused on fungal fragments as a major source of exposure rather than spores or colony-forming units.88, 89 Given that fungal fragments can remain airborne for longer periods of time, they could be a more constant source of exposure, which has been underestimated with traditional short-term air sampling methods. Thus, long-term air sampling methodologies (e.g., electrostatic cloths that can either passively collect dust from the air or be used to wipe settled dust), which are easy-to-use and not burdensome to residents would be ideal. Also, having time-defined exposures throughout the year would capture changes in types and concentrations of pollens and fungi that might occur with climate change.
Indoor post-disaster exposure assessment after extreme weather events is often hampered by a lack of electricity, equipment, and trained technicians that can operate complicated sampling equipment. Recent advances in using electrostatic cloths to passively collect dust have overcome these limitations.90 Further, the cloths can be collected and stored for long periods of time until resources become available to analyze them for indoor biological agents such as allergens or microbial agents. Another advantage of the electrostatic cloths is that they can be used to wipe television screens to actively collect dust samples once residents are able to move back to their homes. In conjunction with a data logger to measure how much time the television is being used, investigators could estimate “time spent indoors” in order to calculate dose (i.e., concentration per unit time). Heretofore, dose has not been commonly used in post-disaster exposure assessment of indoor biological agents; rather, concentrations have been used as proxies for exposure.91
Researchers now have improved analytical options—with improved detection limits—for measuring biological agents in home environments.92 For example, centrifugal filter tubes can be used to concentrate dust extracts, increasing the overall sensitivity of the method. Another advance includes the use of the halogen assay to quantify immunologically active allergen containing particles with very low sensitivity.93, 94
Further technological advances that improve our ability to measure agents in indoor home environments include sensors that can both sample and analyze environmental chemicals such as volatile organic compounds (VOCs). For example, real-time VOC sensors have been developed to examine exposures to microbial agents.95 Mold odor as reported by residents has been associated not only with asthma exacerbations but also with the development of childhood asthma.96 Children spend most of their time in indoor environments83 surrounded by building materials and furnishings that can sustain mold growth,97 which leads to emissions of microbial VOCs (mVOCs) such as 3-methyl furan.98 In addition, higher humidity levels in homes can lead to increased release of formaldehyde from building materials and furnishings.99 As both formaldehyde and mVOCs are respiratory irritants,100 detection at levels below the odor threshold of humans by real-time VOC sensors could permit the removal of hidden mold growth before the occurrence of substantial building damage or respiratory symptoms/disease.
In summary, exposure scientists can contribute to improved understanding of changes to indoor environments associated with climate change (e.g., from effects from extreme events such as floods or more chronic changes affecting exposures to biological and chemical agents) by using current technological advances. Specific climate-related problems that require improvements include collecting exposure information during extreme event-related power outages, obtaining data that capture variations in exposures depending upon location within the home, and sensor data reliability.
Obtaining Exposure Data in the Field: Participants in Exposure Science
Numerous academic programs in the US and elsewhere focus on exposure science. In addition, agencies such as the US EPA and CDC have a large contingent of scientists whose focus is on exposure to chemicals, pathogens and other stressors. In this section, we describe two other groups of participants whose involvement can be a source of important information on exposures related to climate change: the citizenry and the military.
Citizen science
Citizen science has been defined by Cornell University as “projects in which volunteers partner with scientists to answer real-world questions”.101 Citizen science projects can provide monitoring data, which over time and space, reflect changes in the local, regional, or global environment.
Leisure activities and hobbies may be tapped to generate environmental monitoring data that can help describe the effects of climate change. As of 2011, there were 47 million bird-watchers in the US;102 this group has been engaged by Project FeederWatch, a citizen science project sponsored by the Cornell Lab of Ornithology, to tally and report the number of each bird species they see in their yards for two consecutive days each week. They also enter weather data (high and low temperatures, rainfall duration and amount, snow cover). For the 2014–2015 season, over 12,000 birders across the US and Canada submitted checklists (Personal Communication, Anne Marine Johnson, Project Assistant, Project FeederWatch, Cornell Lab of Ornithology, 159 Sapsucker Woods Road, Ithaca, NY 14850, http://feederwatch.org, 607-254-2416). It would not be possible to collect high quality bird count data103 on this scale using existing scientific research funding.
Project FeederWatch data have revealed that warmer winter temperatures in Northeast correlate with changes in the community composition of birds at feeders.104 In 2014, a summary of Project FeederWatch results from 1980 to 2013 showed how the winter range of Anna’s Hummingbirds has expanded into the Northwestern U.S. The FeederWatch data will be used to understand if this expansion is associated with changes in climate, habitat, or in how hummingbirds associate with people.105
Project FeederWatch could further evolve into an environmental monitoring program for North America by having participants report additional data read from air quality sensors. Personal and environmental air quality sensors could be worn by birders or installed in yards. This environmental monitoring effort could become global by engaging the international birder community (for Project FeederWatch, participants rely on local weather stations for information about temperature and the project does not deploy sensors to individual participants).
The Federal government encourages citizen science on an even larger scale using crowd-sourcing, an open invitation for volunteers to provide information or help solve a problem.106 The public participates in the entire scientific process forming research questions, conducting experiments, making discoveries, and solving complex real-world problems.
Actively engaging volunteers in scientific research expands the temporal and geographic extent of data collection efforts.101 In return, scientific information is made available to community members who develop a greater awareness and understanding of their local environments as well as the personal satisfaction of contributing to our understanding of global environmental change.
Exposure scientists can work with citizen scientists to enhance global environmental monitoring. For example, scientists should consider engaging volunteer programs already collecting environmental data, and providing them with additional training; promoting environmental monitoring as part of the K-12 science curriculum, promoting “challenges” and crowd-sourcing within the scientific and public communities, and engaging citizen scientists with data summaries and highlights of exciting findings.
The military: exposures and climate change
In terms of environmental exposure, the US military is primarily concerned about direct health impacts due to heat and cold stress among other exposures. Although US service members are issued proper equipment, clothing, and training to handle various environmental exposures, the Armed Forces Health Surveillance Center (AFHSC) notes that “heat injuries are a significant threat to the health of U.S. military members and the effectiveness of military operations” and that “enhancements in protective technologies deserve continued research”.107, 108 Secondarily, the US military requires regional situational awareness for climate-sensitive diseases such as malaria, dengue, and leishmaniasis, and other vector-borne diseases that could impact the health and effectiveness of military personnel in an operating area. Finally, the US military is interested in monitoring health exposure implications caused by extreme weather, natural disasters, or significant long-term climate anomalies.
For decades, the US military’s public health and bioenvironmental functions have leveraged weather and climate monitoring in order to inform and mitigate potential environmental exposure risk to its personnel. All branches of the military have various internal programs to adapt and prevent heat and cold injuries. The Army for instance charges commanders with developing and implementing such measures and programs through its Training and Doctrine Command (TRADOC) Regulation 350-6. Since the 1950s, the Wet Bulb Globe Temperature, or WBGT, has provided health officials with a relatively consistent measure of heat stress risk using a combination of temperature, humidity, wind speed, solar angle, and cloud cover measurements.109 Currently, military installations employ single station WBGT observing platforms, which limit utility away from main bases. Monitoring is also often complicated by the fact that body armor and other gear can increase WBGT by 5–10° F. Efforts like those by the Army Research Laboratory to employ an algorithm-driven Hot Environment Assessment Tool (HEAT) based on conditions sensed using portable electronic devices (e.g., smart phones) along with potential future weather or climate prediction efforts to model WBGTs around the world enhance the military’s ability to gauge heat stress risk.110
The AFHSC collaborates with the National Aeronautics and Space Administration, US Department of Agriculture, and other US Government and international organizations to monitor climate-related infectious disease risks globally.49, 111 Furthermore, from a strategic perspective, the DoD recently released its Climate Change Adaptation Roadmap (CCAR), which included recommendations for the Department to assess the effects of projected climate change on the distribution of disease vectors.
The DoD is intent on monitoring and tracking changes in health and climate patterns worldwide in the interest of national security. Advances in surveillance and exposure tools to measure and monitor heat and cold stress as well as potential for climate-sensitive diseases will enhance US military personnel effectiveness.
In summary, US military personnel are exposed to unique environmental hazards, and as climate changes, assessment and adaptation to these environmental changes are essential. In addition to advances in environmental exposure tools and surveillance mentioned above, weather and climate monitoring and prediction are key to the US military decision maker’s toolkit in assessing personnel risk. To provide relevant climate situational awareness, the 14th Weather Squadron (DoD’s largest climate center) leverages its Climate Monitoring, Analysis, and Prediction, or CMAP capability to monitor and inform AFHSC, bioenvironmental teams, commanders, and others on climate variability and long-term changes that could impact or exacerbate health concerns for US military personnel and those we support. Ultimately, a combination of exposure tools and models such as those mentioned in this section and others will help the US military gain a firm understanding of health risks posed to its personnel associated with changes in climate.
DISCUSSION
According to the National Academy of Sciences,13 “A central aim of public-health professionals is to maximize the influence of accurate data and professional judgment on decision-making—to make decisions as comprehensive and objective as possible.”112 As described in the case studies in this paper, there are numerous technological, engagement and data gaps surrounding climate change-related exposures that limit our ability to provide accurate data for decision-making. In this paper, we described various approaches for obtaining data essential to understanding public health implications of climate change as well as data and technology needs for using these approaches. Given the local, regional and global aspects of the climate change/exposure science problem, it is not surprising that approaches and data needs cover widely disparate areas.
Exposure scientists need to be engaged in developing the essential technologies and engaging the relevant parties (e.g., communities, government agencies, universities, industry) to ensure that the data needed to understand the human health implications of changing exposures can be collected within appropriate timeframes. Exposure impacts and their consequences should also be important considerations for policy-makers as they strive to determine the appropriate level of climate change mitigation versus adaptation.14 Questions to consider include: When will the tools described in this paper be ready for use and have sufficient accuracy and precision such that robust data are generated for relevant geographic and temporal timescales? Are our students currently receiving the relevant training113 so that they will be able to provide foundational data and data interpretation in the coming years? Who will provide the leadership needed to focus the field so that high quality, relevant data are harmonized and collected?
It could be argued that understanding the implications of changing exposures on public health may be one of the most consequential areas of study in which exposure scientists could currently be engaged. We therefore hope that this paper serves as a starting point for focusing attention on under-developed areas of exposure science that will likely have broad implications for public health.
The challenges are daunting, but advances in technology and in our ability to produce and disseminate transparent information are creating opportunities that can and ought to be harnessed. We anticipate that exposure science will be an essential part of characterizing, communicating, and mitigating the risks associated with climate change.
Disclaimer
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention/the Agency for Toxic Substances and Disease Registry, the US Air Force or Navy, or the US Environmental Protection Agency. The United States Environmental Protection Agency through its Office of Research and Development collaborated in the research described here. It has been subjected to Agency administrative review and approved for publication. Dr. LaKind received support from the CDC Foundation and Dr. LaKind consults to both governmental agencies and private clients.
Competing interests
The authors declare no conflict of interest.
References
- 1.Fiore AM, Naik V, Leibensperger EM. Air quality and climate connections. J Air Waste Manag Assoc. 2015;65:645–685. doi: 10.1080/10962247.2015.1040526. [DOI] [PubMed] [Google Scholar]
- 2.Levy BS and Patz JA (eds). Climate Change and Public Health. Oxford University Press. 2015..
- 3.Smith KR, Woodward A, Campbell-Lendrum DD, Chadee D, Honda Y, Liu Q, Field CB, Barros VR. Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge University Press: Cambridge, UK; 2014. Human health: impacts, adaptation, and co-benefits; pp. pp 709–754. [Google Scholar]
- 4.NIEHS. The Interagency Working Group on Climate Change and Health. A Human Health Perspective on Climate Change. A Report Outlining the Research Needs on the Human Health Effects of Climate Change. April 22, 2010. Environmental Health Perspectives and the National Institute of Environmental Health Sciences, 2010. (https://webcache.googleusercontent.com/search?q=cache:kSPEVJkYmNEJ or https://www.niehs.nih.gov/health/materials/a_human_health_perspective_on_climate_change_full_report_508.pdf+&cd=1&hl=en&ct=clnk&gl=us).
- 5.USGCRP. Crimmins A, Balbus J. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. U.S. Global Change Research Program: Washington, DC, USA; 2016. p. p. 312. [Google Scholar]
- 6.IPCC. Climate Change 2013:The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Stocker, TF, D Qin, G-K Plattner et al (eds). Cambridge University Press: Cambridge, United Kingdom and New York, NY, USA, 2013, pp 1535..
- 7.Trenberth KE, Fasullo JT, Shephard T. Attribution of climate extreme events. Nat Clim Change. 2015;5:725–730. doi: 10.1038/nclimate2657. [DOI] [Google Scholar]
- 8.Balbus JM, Boxall ABA, Fenske RA, Mckone TE, Zeise L. Implications of global climate change for the assessment and management of human health risks of chemicals in the natural environment. Environ Toxicol Chem. 2013;32:62–78. doi: 10.1002/etc.2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bogdal C, Schmid P, Zennegg M, Anselmetti FS, Scheringer M, Hungerbühler K. Blast from the past: melting glaciers as a relevant source for persistent organic pollutants. Environ Sci Technol. 2009;43:8173–8177. doi: 10.1021/es901628x. [DOI] [PubMed] [Google Scholar]
- 10.Carrie J, Wang F, Sanei H, Macdonald RW, Outridge PM, Stern GA. Increasing contaminant burdens in an arctic fish, Burbot (Lota lota, in a warming climate. Environ Sci Technol. 2010;44:316–322. doi: 10.1021/es902582y. [DOI] [PubMed] [Google Scholar]
- 11.Boxall AB, Hardy A, Beulke S, Boucard T, Burgin L, Falloon PD. Impacts of climate change on indirect human exposure to pathogens and chemicals from agriculture. Environ Health Perspect. 2009;117:508–514. doi: 10.1289/ehp.0800084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Melillo JM, Richmond TC, Yohe GW (eds). Climate change impacts in the United States: the third national climate assessment. U.S. Global Change Research Program. U.S. Government Printing Office: Washington, DC, USA. 2014, pp 841.
- 13.National Academy of Sciences (NAS) Climate Change, the Indoor Environment, and Health. Committee on the Effect of Climate Change on Indoor Air Quality and Public Health; Institute of Medicine. National Academies Press: Washington, DC. 2011.
- 14.IPCC (Intergovernmental Panel on Climate Change) Field CB, Barros V. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. A Special Report of Working Groups I and II of the Intergovernmental Panel on Climate Change. Cambridge University Press: Cambridge; 2012. p. pp. 582. [Google Scholar]
- 15.Stocker TF, Qin D, Plattner G-K, Alexander LV, Allen SK, Bindoff NL, Qin D, Stocker TF. Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge University Press: Cambridge, UK; 2013. Technical Summary. [Google Scholar]
- 16.Cutter SL, Solecki W, Bragado N, Carmin J, Fragkias M, Ruth M et al. Urban Systems, Infrastructure, and Vulnerability. Climate Change Impacts in the United States: The Third National Climate Assessment. In: Melillo JM, Richmond TC et al. Global Change Research Program 2014 Available at: http://nca2014.globalchange.gov/report/sectors/urban.
- 17.Klinger C, Landeg O, Murray V . Power outages, extreme events and health: a systematic review of the literature from 2011–2012. PLoS Curr 2014; 6. [DOI] [PMC free article] [PubMed]
- 18.Keim ME. Building human resilience: the role of public health preparedness and response as an adaptation to climate change. Am J Prev Med. 2008;35:508–516. doi: 10.1016/j.amepre.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 19.Lane K, Charles-Guzman K, Wheeler K, Abid Z, Graber N, Matte T. Health effects of coastal storms and flooding in urban areas: a review and vulnerability assessment. J Environ Public Health. 2013;2013:913064. doi: 10.1155/2013/913064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mac Kenzie WR, Hoxie NJ, Proctor ME, Gradus MS, Blair KA, Peterson DE. A massive outbreak in Milwaukee of Cryptosporidium infection transmitted through the public water supply. N Engl J Med. 1994;331:161–167. doi: 10.1056/NEJM199407213310304. [DOI] [PubMed] [Google Scholar]
- 21.Jordan P, Turner K, Nicol D, Boyer D . Developing a risk analysis procedure for post-wildfire mass movement and flooding in British Columbia. 1st Specialty Conference on Disaster Medicine. Available at: http://www.for.gov.bc.ca/hfd/pubs/rsi/fsp/Misc/Misc071.pdf, 2006.
- 22.Luber G, Knowlton K, Balbus J, Frumkin H, Hayden M, Hess J et al. Human Health. Climate Change Impacts in the United States: The Third National Climate Assessment. In: Melillo JM, Richmond T et al. U.S. Global Change Research Program 2014, pp. 220–256 Available at: http://nca2014.globalchange.gov/report/sectors/human-health.
- 23.Panikkath R, Jumper CA, Mulkey Z. Multilobar lung infiltrates after exposure to dust storm: the Haboob lung syndrome. Am J Med. 2013;126:e5–e7. doi: 10.1016/j.amjmed.2012.08.012. [DOI] [PubMed] [Google Scholar]
- 24.Le G, Breysse PN, Eftim S, McDermott A, Geyh A, Berman J. Canadian forest fires and the effects of long-range transboundary air pollution on hospitalizations among the elderly. ISPRS Int J Geo-Inf. 2014;3:713–731. doi: 10.3390/ijgi3020713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sapkota A, Symons JM, Kleissl J, Wang L, Parlange MB, Ondov J. Impact of the 2002 Canadian forest fires on PM air quality in Baltimore city. Environ Sci Technol. 2005;39:24–32. doi: 10.1021/es035311z. [DOI] [PubMed] [Google Scholar]
- 26.Bradbury J, DeConcini C . The connection between climate change and recent extreme weather events. Available at: http://pdf.wri.org/connection_between_climate_change_and_extreme_weather.pdf. Accessed on 16 October, 2015; 2012.
- 27.Huber D, Gulledge J . Extreme weather and climate change. center for climate and energy solutions. Available at: http://www.c2es.org/publications/extreme-weather-and-climate-change. Accessed on 4 September 2015; 2011.
- 28.Basu R, Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev. 2002;24:190–202. doi: 10.1093/epirev/mxf007. [DOI] [PubMed] [Google Scholar]
- 29.Braga ALF, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect. 2002;110:859–863. doi: 10.1289/ehp.02110859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ye X, Wolff R, Yu W, Vaneckova P, Pan X, Tong S. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect. 2012;120:19–28. doi: 10.1289/ehp.1003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rainham DGC, Smoyer-Tomic KE. The role of air pollution in the relationship between a heat stress index and human mortality in Toronto. Environ Res. 2003;93:9–19. doi: 10.1016/S0013-9351(03)00060-4. [DOI] [PubMed] [Google Scholar]
- 32.Hess JJ, Saha S, Luber G. Summertime acute heat illness in U.S. emergency departments from 2006 through 2010: analysis of a nationally representative sample. Environ Health Perspect. 2014;122:1209–1215. doi: 10.1289/ehp.1306796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kovats RS, Hajat S, Wilkinson P. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, UK. Occup Environ Med. 2004;61:893–898. doi: 10.1136/oem.2003.012047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tan J, Zheng Y, Tang X, Guo C, Li L, Song G. The urban heat island and its impact on heat waves and human health in Shanghai. Int J Biometeorol. 2010;54:75–84. doi: 10.1007/s00484-009-0256-x. [DOI] [PubMed] [Google Scholar]
- 35.Fuhrmann CM, Sugg MM, Konrad CE, Waller A. Impact of extreme heat events on emergency department visits in North Carolina (2007–2011) J Commun Health. 2016;41:146–156. doi: 10.1007/s10900-015-0080-7. [DOI] [PubMed] [Google Scholar]
- 36.Romeo Upperman C, Parker J, Jiang C, He X, Murtugudde R, Sapkota A. Frequency of extreme heat event as a surrogate exposure metric for examining the human health effects of climate change. PLoS ONE. 2015;10:e0144202. doi: 10.1371/journal.pone.0144202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alexander L, Donat M, Takayama Y, Yang H . The CLIMDEX project: creation of long-term global gridded products for the analysis of temperature and precipitation extremes. Presented at the WCRP Open Science Conference, Denver; 2011.
- 38.Reid CE, Mann JK, Alfasso R, English PB, King GC, Lincoln R. Evaluation of a heat vulnerability index on abnormally hot days: an environmental public health tracking study. Environ Health Perspect. 2012;120:715–720. doi: 10.1289/ehp.1103766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Allen RW, Adar SD, Avol E, Cohen M, Curl CL, Larson T. Modeling the residential infiltration of outdoor PM2.5 in the multi-ethnic study of atherosclerosis and air pollution (MESA air) Environ Health Perspect. 2012;120:824–830. doi: 10.1289/ehp.1104447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCormack MC, Belli AJ, Saha A, Diette GB, Williams DL, Matsui EC. Indoor and outdoor heat exposure is associated with increased COPD morbidity (meeting abstract) Am J Respir Crit Care Med. 2014;189:A2198. [Google Scholar]
- 41.Scallan E, Griffin PM, Angulo FJ, Tauxe RV, Hoekstra RM. Foodborne illness acquired in the United States—unspecified agents. Emerg Inf Dis. 2011;17:16–22. doi: 10.3201/eid1701.P21101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Colford JM, Roy S, Beach MJ, Hightower A, Shaw SE, Wade TJ. A review of household drinking water intervention trials and an approach to the estimation of endemic waterborne gastroenteritis in the United States. J Water Hlth. 2006;4:71–88. doi: 10.2166/wh.2006.018. [DOI] [PubMed] [Google Scholar]
- 43.Taylor LH, Latham SM. Woolhouse MEJ. Risk factors for human disease emergence. Phil Trans R Soc Lond B. 2001;356:983–989. doi: 10.1098/rstb.2001.0888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Woolhouse M, Gaunt E. Ecological origins of novel human pathogens. Crit Rev Microbiol. 2007;33:231–242. doi: 10.1080/10408410701647560. [DOI] [PubMed] [Google Scholar]
- 45.Hinckley AF, Connally NP, Meek JI, Johnson BJ, Kemperman MM, Feldman KA. Lyme disease testing by large commercial laboratories in the United States. Clin Inf Dis. 2014;59:676–681. doi: 10.1093/cid/ciu397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nelson CA, Saha S, Kugeler KJ, Delorey MJ, Shankar MB, Hinckley AF. Incidence of clinician-diagnosed Lyme disease, United States, 2005–2010. Emerg Inf Dis. 2015;21:1625–1631. doi: 10.3201/eid2109.150417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Petersen LR, Carson PJ, Biggerstaff BJ, Custer B, Borchardt SM, Busch MP. Estimated cumulative incidence of West Nile virus infection in US adults, 1999–2010. Epidemiol Inf. 2013;141:591–595. doi: 10.1017/S0950268812001070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hartley DM, Barker CM, Le Menach A, Niu T, Gaff HD, Reisen WK. Effects of temperature on emergence and seasonality of West Nile virus in California. Am J Trop Hyg. 2012;86:884–894. doi: 10.4269/ajtmh.2012.11-0342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Anyamba A, Chretien JP, Small J, Tucker CJ, Formenty PB, Richardson JH. Prediction of a Rift Valley fever outbreak. Proc Natl Acad Sci USA. 2009;106:955–959. doi: 10.1073/pnas.0806490106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Parmenter RR, Yadav EP, Parmenter CA, Ettestad P, Gage KL. Incidence of plague associated with increased winter-spring precipitation in New Mexico. Am J Trop Med Hyg. 1999;61:814–821. doi: 10.4269/ajtmh.1999.61.814. [DOI] [PubMed] [Google Scholar]
- 51.Curriero FC, Patz JA, Rose JB, Lele S. The association between extreme precipitation and waterborne disease outbreaks in the United States, 1948–1994. Am J Pub Health. 2001;91:1194–1199. doi: 10.2105/AJPH.91.8.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patz JA, Vavrus SJ, Uejio CK, McLellan SL. Climate change and waterborne disease risk in the Great Lakes region of the US. Am J Prev Med. 2008;35:451–458. doi: 10.1016/j.amepre.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 53.Nichols G, Lane C, Asgari N, Verlander NQ, Charlett A. Rainfall and outbreaks of drinking water related disease in England and Wales. J Water Health. 2009;7:1–8. doi: 10.2166/wh.2009.143. [DOI] [PubMed] [Google Scholar]
- 54.Lederberg J, Hamburg MA, Smolinski MS. Microbial Threats to Health: Emergence, Detection, and Response. National Academies Press: Washington, DC; 2003. [PubMed] [Google Scholar]
- 55.Paz S, Semenza JC. El Niño and climate change—contributing factors in the dispersal of Zika virus in the Americas? Lancet. 2016;387:745. doi: 10.1016/S0140-6736(16)00256-7. [DOI] [PubMed] [Google Scholar]
- 56.National Research Council, National Academy of Sciences Water Reuse: Potential for Expanding the Nation’s Water Supply through Reuse of Municipal Wastewater. The National Academies Press: Washington, DC, 2012.
- 57.Fono LJ, Kolodziej EP, Sedlak DL. Attenuation of wastewater-derived contaminants in an effluent-dominated river. Environ Sci Technol. 2006;40:7257–7262. doi: 10.1021/es061308e. [DOI] [PubMed] [Google Scholar]
- 58.Richardson SD, Plewa MJ, Wagner ED, Schoeny R, DeMarini DM. Occurrence, genotoxicity, and carcinogenicity of regulated and emerging disinfection by-products in drinking water: a review and roadmap for research. Mutat Res. 2007;636:178–242. doi: 10.1016/j.mrrev.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 59.Richardson SD, Ternes TA. Water analysis: emerging contaminants and current issues. Anal Chem. 2014;86:2813–2848. doi: 10.1021/ac500508t. [DOI] [PubMed] [Google Scholar]
- 60.Postigo C, Richardson SD. Transformation of pharmaceuticals during oxidation/disinfection processes in drinking water treatment. J Haz Mater. 2014;279:461–475. doi: 10.1016/j.jhazmat.2014.07.029. [DOI] [PubMed] [Google Scholar]
- 61.Duirk SE, Lindell C, Cornelison CC, Kormos J, Ternes TA, Attene-Ramos M. Formation of toxic iodinated disinfection by-products from compounds used in medical imaging. Environ Sci Technol. 2011;45:6845–6854. doi: 10.1021/es200983f. [DOI] [PubMed] [Google Scholar]
- 62.Schmidt CK, Brauch HJN. N-dimethosulfamide as precursor for N-nitrosodimethylamine (NDMA) formation upon ozonation and its fate during drinking water treatment. Environ Sci Technol. 2008;42:6340–6346. doi: 10.1021/es7030467. [DOI] [PubMed] [Google Scholar]
- 63.Gong T, Zhang X. Detection, identification and formation of new iodinated disinfection byproducts in chlorinated saline wastewater effluents. Water Res. 2015;68:77–86. doi: 10.1016/j.watres.2014.09.041. [DOI] [PubMed] [Google Scholar]
- 64.Liu J, Zhang X. Comparative toxicity of new halophenolic DBPs in chlorinated saline wastewater effluents against a marine alga: Halophenolic DBPs are generally more toxic than haloaliphatic ones. Water Res. 2014;65:64–72. doi: 10.1016/j.watres.2014.07.024. [DOI] [PubMed] [Google Scholar]
- 65.Yang M, Zhang X. Halopyrroles: a new group of highly toxic disinfection byproducts formed in chlorinated saline wastewater. Environ Sci Technol. 2014;48:11846–11852. doi: 10.1021/es503312k. [DOI] [PubMed] [Google Scholar]
- 66.Yang M, Zhang X. Comparative developmental toxicity of new aromatic halogenated DBPs in a chlorinated saline sewage effluent to the marine polychaete Platynereis dumerilii. Environ Sci Technol. 2013;47:10868–10876. doi: 10.1021/es401841t. [DOI] [PubMed] [Google Scholar]
- 67.Begel A, Bosch J, Storey MA, Doll B, Laundry D, Fullerton D. Social networking meets software development: perspectives from GitHub, MSDN, Stack Exchange, and TopCoder. IEEE Softw. 2013;30:52–66. doi: 10.1109/MS.2013.13. [DOI] [Google Scholar]
- 68.USEPA (US Environmental Protection Agency). Air Sensor Guidebook. EPA/600/R-14/159. RTP, NC; 2014.
- 69.USEPA (US Environmental Protection Agency). TSCA Chemical Substance Inventory. Available at: http://www.epa.gov/oppt/existingchemicals/pubs/tscainventory/index.html. Accessed on September 2015; 2015.
- 70.Sobus JR, DeWoskin RS, Tan YM, Pleil JD, Phillips MB, George BJ. Uses of NHANES biomarker data for chemical risk assessment: trends, challenges, and opportunities. Environ Health Perspect. 2015;123:919–927. doi: 10.1289/ehp.1409177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Krauss M, Singer H, Hollender J. LC-high resolution MS in environmental analysis: From target screening to the identification of unknowns. Anal Bioanal Chem. 2010;397:943–951. doi: 10.1007/s00216-010-3608-9. [DOI] [PubMed] [Google Scholar]
- 72.Alves Filho EG, Sartori L, Silva LM, Silva BF, Fadini PS, Soong R. Non-targeted analyses of organic compounds in urban wastewater. Magn Reson Chem. 2015;53:704–710. doi: 10.1002/mrc.4169. [DOI] [PubMed] [Google Scholar]
- 73.Chiaia-Hernandez AC, Schymanski EL, Kumar P, Singer HP, Hollender J. Suspect and nontarget screening approaches to identify organic contaminant records in lake sediments. Anal Bioanal Chem. 2014;406:7323–7335. doi: 10.1007/s00216-014-8166-0. [DOI] [PubMed] [Google Scholar]
- 74.Rager JE, Strynar MJ, Liang S, McMahen RL, Richard AM, Grulke CM. Linking high resolution mass spectrometry data with exposure and toxicity forecasts to advance high-throughput environmental monitoring. Environ Int. 2016;88:269–280. doi: 10.1016/j.envint.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 75.Tengstrand E, Rosén J, Hellenäs KE, Aberg KM. A concept study on non-targeted screening for chemical contaminants in food using liquid chromatography-mass spectrometry in combination with a metabolomics approach. Anal Bioanal Chem. 2013;405:1237–1243. doi: 10.1007/s00216-012-6506-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Onghena M, van Hoeck E, Vervliet P, Scippo ML, Simon C, van Loco J. Development and application of a non-targeted extraction method for the analysis of migrating compounds from plastic baby bottles by GC-MS. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2014;31:2090–2102. doi: 10.1080/19440049.2014.979372. [DOI] [PubMed] [Google Scholar]
- 77.Shaul NJ, Dodder NG, Aluwihare LI, Mackintosh SA, Maruya KA, Chivers SJ. Nontargeted biomonitoring of halogenated organic compounds in two ecotypes of bottlenose dolphins (Tursiops truncatus from the Southern California Bight. Environ Sci Technol. 2015;49:1328–1338. doi: 10.1021/es505156q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Soltow QA, Strobel FH, Mansfield KG, Wachtman L, Park Y, Jones DP. High-performance metabolic profiling with dual chromatography-Fourier-transform mass spectrometry (DC-FTMS) for study of the exposome. Metabolomics. 2013;9:S132–S143. doi: 10.1007/s11306-011-0332-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Peters RJ, van Engelen MC, Touber ME, Georgakopoulus C, Nielen MW. Searching for in silico predicted metabolites and designer modifications of (cortico)steroids in urine by high-resolution liquid chromatography/time-of-flight mass spectrometry. Rapid Commun Mass Spectrom. 2009;23:2329–2337. doi: 10.1002/rcm.4153. [DOI] [PubMed] [Google Scholar]
- 80.Andra SS, Austin C, Wright RO, Arora M. Reconstructing pre-natal and early childhood exposure to multi-class organic chemicals using teeth: Towards a retrospective temporal exposome. Environ Int. 2015;83:37–45. doi: 10.1016/j.envint.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Altenburger R, Ait-Aissa S, Antczak P, Backhaus T, Barceló D. Future water quality monitoring—adapting tools to deal with mixtures of pollutants in water resource management. Sci Total Environ. 2015;512-513:540–551. doi: 10.1016/j.scitotenv.2014.12.057. [DOI] [PubMed] [Google Scholar]
- 82.Petrie B, Barden R, Kasprzyk-Hordern B. A review on emerging contaminants in wastewaters and the environment: current knowledge, understudied areas and recommendations for future monitoring. Water Res. 2015;72:3–27. doi: 10.1016/j.watres.2014.08.053. [DOI] [PubMed] [Google Scholar]
- 83.IOM (Institute of Medicine) Climate Change, The Indoor Environment, and Health. The National Academies Press; Washington, DC, 2011.
- 84.Burge H. Bioaerosols. CRC Lewis Publishers: Boca Raton; 1995. [Google Scholar]
- 85.Chew GL, Burge HB, Dockery DW, Muilenberg ML, Weiss ST, Gold DR. Limitations of a home characteristics questionnaire as a predictor of indoor allergen levels. Am J Respir Crit Care Med. 1998;157:1536–1541. doi: 10.1164/ajrccm.157.5.9708011. [DOI] [PubMed] [Google Scholar]
- 86.Gadermaier G, Wopfner N, Wallner M, Egger M, Didierlaurent A, Regl G. Array-based profiling of ragweed and mugwort pollen allergens. Allergy. 2008;63:1543–1549. doi: 10.1111/j.1398-9995.2008.01780.x. [DOI] [PubMed] [Google Scholar]
- 87.Feo Brito F, Alonso AM, Carnes J, Martin-Martin R, Fernandez-Caldas E, Galindo PA. Correlation between Alt a 1 levels and clinical symptoms in Alternaria alternata-monosensitized patients. J Investig Allergol Clin Immunol. 2012;22:154–159. [PubMed] [Google Scholar]
- 88.Green BJ, Tovey ER, Sercombe JK, Blachere FM, Beezhold DH, Schmechel D. Airborne fungal fragments and allergenicity. Mycology. 2006;44:S245–S255. doi: 10.1080/13693780600776308. [DOI] [PubMed] [Google Scholar]
- 89.Adhikari A, Reponen T, Rylander R. Airborne fungal cell fragments in homes in relation to total fungal biomass. Indoor Air. 2013;23:142–147. doi: 10.1111/j.1600-0668.2012.00799.x. [DOI] [PubMed] [Google Scholar]
- 90.Cozen W, Avol E, Diaz-Sanchez D, McConnell R, Gauderman WJ, Cockburn MG. Use of an electrostatic dust cloth for self-administered home allergen collection. Twin Res Hum Genet. 2008;11:150–155. doi: 10.1375/twin.11.2.150. [DOI] [PubMed] [Google Scholar]
- 91.Rabito FA, Iqbal S, Kiernan MP, Holt E, Chew GL. Children’s respiratory health and mold levels in New Orleans after Katrina: a preliminary look. J Allergy Clin Immunol. 2008;121:622–625. doi: 10.1016/j.jaci.2007.11.022. [DOI] [PubMed] [Google Scholar]
- 92.Hung LL, Miller JD, Dillon HK. Field Guide for the Determination of Biological Contaminants in Environmental Samples. American Industrial Hygiene Association: Fairfax, VA; 2005. [Google Scholar]
- 93.Green BJ, Yli-Panula Y, Tovey ER. Halogen immunoassay, a new method for the detection of sensitization to fungal allergens: comparisons with conventional techniques. Allergol Int. 2006;55:131–139. doi: 10.2332/allergolint.55.131. [DOI] [PubMed] [Google Scholar]
- 94.Rivera-Mariani FE, Matsui EC, Breysse PN. Performance of the halogen immunoassay to assess airborne mouse allergen-containing particles in a laboratory animal facility. J Expo Sci Environ Epidemiol. 2014;24:3–82. doi: 10.1038/jes.2012.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chen C, Tsow F, Campbell KD, Iglesias R, Forzani E, Tao NJ. A wireless hybrid chemical sensor for detection of environmental volatile organic compounds. IEEE Sens J. 2013;13:1748–1755. doi: 10.1109/JSEN.2013.2239472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tischer CG, Hohmann C, Thiering E, Herbarth O, Muller A, Henderson J. ENRIECO Consortium. Meta-analysis of mould and dampness exposure on asthma and allergy in eight European birth cohorts: an ENRIECO initiative. Allergy. 2011;66:1570–1579. doi: 10.1111/j.1398-9995.2011.02712.x. [DOI] [PubMed] [Google Scholar]
- 97.Hoang CP, Kinney KA, Corsi RL, Szaniszlo PJ. Resistance of green building materials to fungal growth. Int Biodeter Biodegrad. 2010;64:104–113. doi: 10.1016/j.ibiod.2009.11.001. [DOI] [Google Scholar]
- 98.Moularat S, Robine E, Ramalho O, Oturan MA. Detection of fungal development in a closed environment through the identification of specific VOC: demonstration of a specific VOC fingerprint for fungal development. Sci Total Environ. 2008;407:139–146. doi: 10.1016/j.scitotenv.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 99.Arundel AV, Sterling EM, Biggin JH, Sterling TD. Indirect health effects of relative humidity in indoor environments. Environ Health Perspect. 1986;65:351–361. doi: 10.1289/ehp.8665351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Walinder R, Ernstgard L, Johanson G, Norback D, Venge P, Wieslander G. Acute effects of a fungal volatile compound. Environ Health Perspect. 2005;113:1775–1778. doi: 10.1289/ehp.8193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Cornell University. Defining citizen science. Available at: http://www.birds.cornell.edu/citscitoolkit/about/definition. Accessed 24 July 2015; 2015.
- 102.Carver E . Birding in the United States: a demographic and economic analysis. U.S. Fish and Wildlife Service, Division of Economics, Arlington VA. Available at: http://www.fws.gov/southeast/economicImpact/pdf/2011-BirdingReport—FINAL.pdf. Accessed 24 July 2015; 2013.
- 103.Dhondt AA, DeCoste JC, Ley DH, Hochachka WM. Diverse wild bird host range of Mycoplasma gallisepticum in Eastern North America. PLoS ONE. 2014;9:e103553. doi: 10.1371/journal.pone.0103553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cornell Lab of Ornithology. 2014–2015 Project FeederWatch end-of-season news note. Available at: http://feederwatch.org/wp-content/uploads/2015/04/2015-News-Note.pdf. Accessed 24 July 2015; 2015.
- 105.Cornell Lab of Ornithology. 2013–2014 Project FeederWatch end-of-season news note. Available at: http://feederwatch.org/wp-content/uploads/2014/04/2014-News-Note.pdf. Accessed on 24 July 2015; 2014.
- 106.Federal crowdsourcing and citizen science. Available at: https://crowdsourcing-toolkit.sites.usa.gov/. Accessed on 6 October 2015.
- 107.Connor RR . Update: cold weather injuries, active and reserve components, U.S. Armed Forces, July 2009–June 2014. AFHSC Med Surveill Month Rep. [PubMed]
- 108.Armed Forces Health Surveillance Center (AFHSC). Update: heat injuries, active component, U.S. Armed Forces. AAFHSC Med Surveill Month Rep. 2014;22:17–20. [Google Scholar]
- 109.Budd GM. Wet-bulb globe temperature (WBGT)—its history and limitations. J Sci Med Sport. 2008;11:20–32. doi: 10.1016/j.jsams.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 110.Sauter D . Hot Environment Assessment Tool (HEAT) User’s Guide. ARL-MR-0809 2012, 10.
- 111.Chretien J, Anyamba A, Small J, Britch S, Sanchez JL, Halbach AC et al. Global climate anomalies and potential infectious disease risks: 2014-2015. PLoS Curr Outbreaks 2015. [DOI] [PMC free article] [PubMed]
- 112.IOM (Institute of Medicine). The Future of Public Health. National Academy Press: Washington, DC. 1988.
- 113.Pleil JD, Blount BC, Waidyanatha S, Harper M. Establishing exposure science as a distinct scientific discipline. J Exp Sci Environ Epidemiol. 2012;22:317–319. doi: 10.1038/jes.2012.5. [DOI] [PMC free article] [PubMed] [Google Scholar]


