Abstract
Aim
To investigate the dosimetric influence of filtered and flattening filter free (FFF) photon beam of 6 and 10 MV energies on cervix RA radiotherapy planning and to find possibilities to develop the clinically acceptable RA plans with FFFB photon beam and explore their potential benefits to cervix cancer patients.
Background
FFF photon beams enhances the treatment delivery by increased dose rate which results in shorter treatment time, this shorter treatment time reduces intrafraction motion and enhance comfort to the patients.
Materials and methods
RA plans were generated for filtered and flattening filter free photon beams of 6 and 10 MV energies using same dose–volumes constraints. RA plans were generated to deliver a dose of 50.4 Gy in 28 fractions, for a cohort of eleven patients reported with cervix carcinoma. RA plans were evaluated in terms of PTV coverage, dose to OAR's, CI, HI, total no. of monitor units (MUs) and NTID and low dose volume of normal tissues.
Results
Clinically acceptable and similar plans were generated for filtered and flattening filter free photon beams. FFFB delivered slightly higher mean target dose (52.28 Gy vs. 52.0 Gy, p = 0.000 for 6 MV and 52.42 Gy vs. 52.0 Gy, p = 0.000 for 10 MV) less homogeneous (1.062 vs. 1.052, p = 0.000 for 6 MV and 1.066 vs. 1.051, p = 0.000 for 10 MV) and less conformal (1.007 vs. 1.004, p = 0.104 for 6 MV and 1.012 vs. 1.003, p = 0.010 for 10 MV) RA plans compared to FB. FFFB delivered more doses to the bladder and rectum, also required more numbers of MUs in comparison to FB.
Conclusions
This study concludes that FB is more beneficial for cervix RA planning in comparison to FFFB, as FB generates more conformal and homogenous rapid arc plans and offers better OAR's sparing.
Keywords: Rapid arc plans, Filtered beam, Flattening filter free beam, Cervix carcinoma
1. Background
Cervix cancer is the fourth most common gynecological malignancy found in women worldwide. Developing countries are mostly affected by this type of cancer disease. According to the GLOBOCAN20131 report, almost 70% of global burden falls in developing countries. External radiotherapy is accepted as a standard of care for the management of cervix cancer worldwide.2 Purpose of external radiotherapy for cervix cancer is to achieve an optimal balance between maximum doses to tumor and minimize the risk of side effects and long term complications to OARs.
Modern LINACs are capable of delivering filtered (FB) and flattening filter free (FFFB) photon beams as well. Introduction of FFFB in radiotherapy has enhanced the treatment delivery as the removal of a flattening filter from the path of X-ray beam causes more efficient photon production and increased dose rate substantially at treatment level. Increased dose rate results in shorter treatment time, which reduces intrafraction motion and enhances patient's treatment comfort. In addition, the FFFB offers other dosimetric advantages such as reduced scatter, reduced leakage and reduced out of field scatter doses.3, 4 This reduction in out of field doses may lead to minimizing the risk of radiation induced secondary malignancies. Casemore et al.5 reported that the use of FFFB reduces scatter and associated dose to distal organs, means FFFB is associated with a lower secondary dose to distal normal organs than FB of the same photon energy.
The first clinical study published in 1991 about the use of FFFB to reduce the long treatment time for high dose radiosurgery.6 Several studies have been published about the properties of FFFB beams from different Medical electron linear accelerators (Clinac) based on dosimetric measurements and Monte Carlo measurement as well.6, 7, 8 A few investigators have also reported the feasibility of FFF beams for IMRT treatment planning.9, 10
1.1. Aim
The aim of this study is to investigate the dosimetric influence of FB and FFFB of 6 and 10 MV on cervix RA radiotherapy planning. As FFFB delivery may lead to higher treatment efficiency in conjunction with arc-based delivery configuration like RA radiotherapy delivery. This study also explores the possibilities to develop the clinically acceptable RA plans with FFFB photon beam and explores their potential benefits to cervix cancer patients. This Study evaluates the dosimetric parameters in terms of Planning Target Volume (PTV) coverage and OAR's sparing, different physical indices, monitor units (MUs) and Integral dose to normal tissues form RA plans using FB and FFFB of 6 and 10 MV.
2. Methods and material
2.1. Simulation
Patients were simulated on Siemens Somatom Sensation Open CT scanner (Siemens Medical System, Germany), in a supine position with the help of All In One board (AIO, Orfit Industry Nv, Belgium), thermoplastic mold cast (Orfit Industry Nv, Belgium) and knee rest. Computed Tomography (CT) scanswere acquired extending from L2 vertebra to proximal third femoral diaphysis, with a slice thickness of 3 mm. All scans were performed with a full bladder as per institutional protocol.
2.2. Target and OAR delineation
Contouring was done by radiation oncologist on CT images for gross target volume (GTV), clinical target volume (CTV) and planning target volume (PTV) as per Radiation Therapy Oncology Group (RTOG) guidelines and normal tissues like the bladder, rectum, femoral heads and bowel were also delineated. PTV was defined by adding a margin of 5 mm to the CTV.
2.3. Patient characteristic
A cohort of eleven patients reported with cervix carcinoma (Stages II to IIIB) who had received radiotherapy treatment for cervix carcinoma were selected retrospectively for this study. Patient's mean PTV volume was (1318.94 ± 189.03) cc ranging from 1112.02 cc to 1710.61 cc. Bladder and rectum mean volume was (379.67 ± 189.03) cc ranging from 169.72 cc to 748.0 cc and (64.68 ± 22.09) cc ranging from 45.99 cc to 101.43 cc, respectively. Overlap volume for the bladder and rectum with PTV was also calculated by Boolean operations. It was found to be an overlap of (38.58 ± 6.95)% volume ranging from 29.79 cc to 48.72 cc for Bladder minus PTV and an overlap volume of (40.77 ± 9.84)% ranging from 24.90 cc to 51.31 cc for rectum minus PTV.
2.4. Prescription and planning objectives
RA plans were generated using FB and FFFB of 6 and 10 MV to deliver a prescription dose (PD) of 50.4 Gy to the PTV in 28 fractions, at 1.80 Gy per fraction. Planning objective was to deliver 100% PD to 95% of the PTV with no more than 2% of PTV volume receiving 107% of prescription dose as per ICRU report 5011 and ICRU report 6212 recommendations. Dose objectives for the bladder and rectum were V50Gy < 50% of their volumes, and mean dose to the femoral heads were less than 20 Gy as per institutional protocol.
2.5. Planning technique
RA plans were generated for delivery on Clinac True Beam STx (Varian Medical System, Palo Alto, CA), which is capable of delivering both FB and FFFB of 6 and 10 MV. This Clinac is equipped with 60 pairs High Definition (HD)-MLC with inner 32 leaf pair of 0.25 cm and outer 28 leaf pair of 0.50 cm projection width at isocenter. Clinac was calibrated for 1 cGy/MU at the depth of dose maximum (Dmax) as per Technical Series Report No-398 (TRS-398) of the International Atomic Energy Agency (IAEA)13 for both FB and FFFB of 6 and 10 MV. Required measurement was performed for reference field size of 10 × 10 cm2, source to surface distance (SSD) 100 cm, at 10 cm depth.
Eclipse treatment planning system (TPS) (Eclipse external Beam Planning software 10.0, Varian Medical System, Palo Alto, CA) was used for treatment planning purpose. Eclipse TPS uses Progressive Resolution Optimizer (PRO) algorithm as an optimization algorithm for RA planning to determine the combination of beam weights and shapes. It uses multi-resolution approach to optimized RA plans. PRO optimized the dynamic variables like MLC speed, dose rate and gantry speed. Anisotropic Analytical Algorithm (AAA) was used for photon dose calculation of RA plans.14
All RA plans were generated for ClinacTrue beam STx operating dose rate of 600 MU per minute for FB of 6 and 10 MV. An operating dose rate of 1400 MU per minute and 2400 MU per minute were used for FFFB of 6 and 10 MV. RA plans were generated using double arc as independent optimization of two arcs allowing each arc to create a total unrelated sequence of MLC apertures, dose rates and gantry speed combinations. First clockwise (CW) arc with the gantry angle of 179–181 degrees, second counter clockwise (CCW) arc with the gantry angle of 181–179 degrees and collimator was rotated to 10–30 degrees to minimize inter-leaf leakage.
3. Dosimetric comparison
RA plans were optimized to treat cervix cancer using FB and FFFB of 6 and 10 MV. Plan quality assessments were done based on different dosimetric parameters of PTV and OARs. Acumulative Dose Volume Histogram (DVH) was generated by Eclipse TPS to evaluate different dosimetric parameters of PTV and OARs.
PTV coverage was analyzed by calculating mean dose and V93%, V95%, V100%, V107% volumes from DVH, where V93%, V95%, V100%, V107% were percentage volume of PTV receiving a dose of 93%, 95%, 100% and 107% of prescription dose to PTV respectively. DVH parameters were also analyzed for the following normal structures like bladder, rectum and both femoral heads. These normal structures were compared for FB and FFFB in terms of mean doses and their different dose volumes of V10Gy, V20Gy, V30Gy and V40Gy, where V10Gy, V20Gy, V30Gy and V40Gy were the dose volumes of 10 Gy, 20 Gy, 30 Gy and 40 Gy for respective OARs. Other than this conformity index (CI), homogeneity index (HI) and integral dose to normal tissues (NTID) was also compared for FB and FFFB of 6 and 10 MV. Low dose volumes of normal tissue were also studied, they were compared in terms of doses to the volumes of 1% (D1%), 2% (D2%) and 5% (D5%) and volumes of 2 Gy (V2Gy) and 5 Gy (V5Gy) for normal tissues.
3.1. Conformity index
Conformity index (CI) evaluates the degree of conformity of resulting dose distribution of both RA plans. CI is defined as a ratio of total tissue volume receiving reference dose to the PTV volume. It is calculated for a given isodose levels i.e. 98% (CI98%).15
CI = volume of 98% isodose level/PTV volume.
3.2. Homogeneity index
Homogeneity Index (HI) was evaluated to know the homogeneity of dose distribution with in PTV. HI is a ratio of the minimum dose received in 5% of PTV that received the highest (D5%), to the minimum dose in 95% of the PTV that received the highest dose (D95%) 15 i.e. D5%/D95%.
3.3. Integral dose (ID)
Integral dose were calculated to find out the dose to normal tissues outside the PTV. Integral dose were calculate to analyze the plan quality based on the following formula considering uniform tissue density.16, 17
NTID = mean dose × volume of normal tissue outside PTV.
4. Statistical analysis
Statistical analyses were performed by using a two sample paired t-test to compare the dosimetric difference between RA plans using FB and FFFB of 6 and 10 MV for cervix cancer. The results were analyzed with the help of International Business Machine Corporation (IBM), Statistical Package for Social Sciences software (SPSS, version 20). p-Value less than 0.05 was considered statistically significant with 95% confidence limit.
5. Results
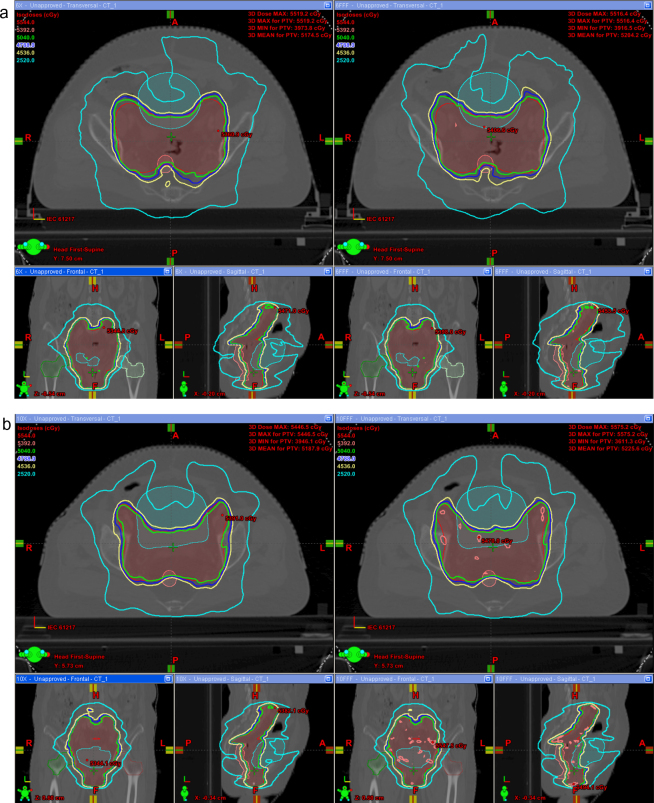
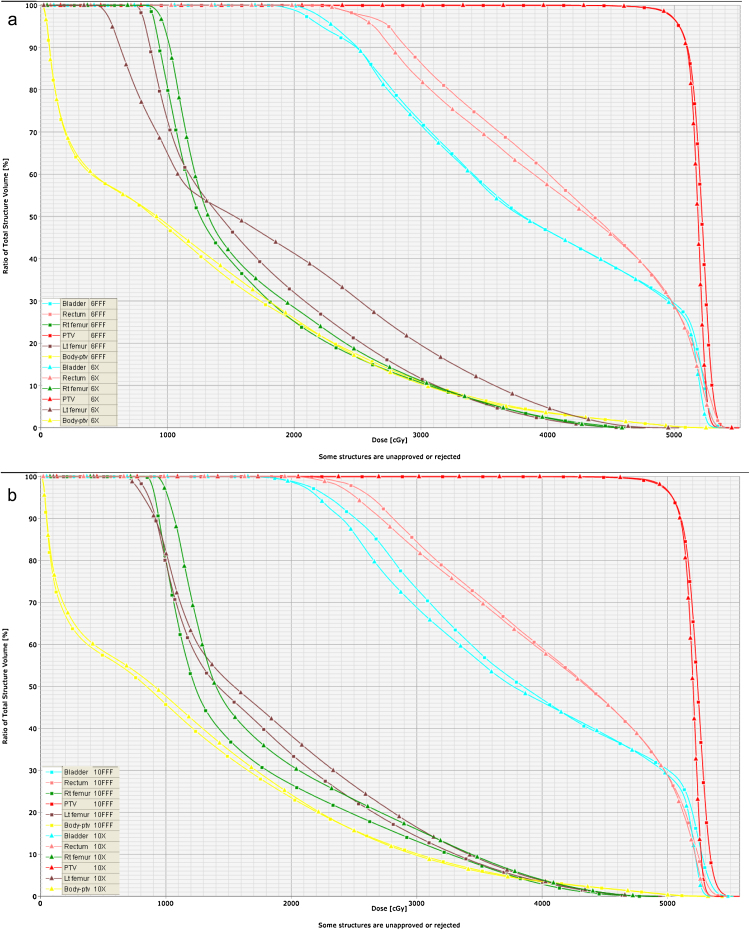
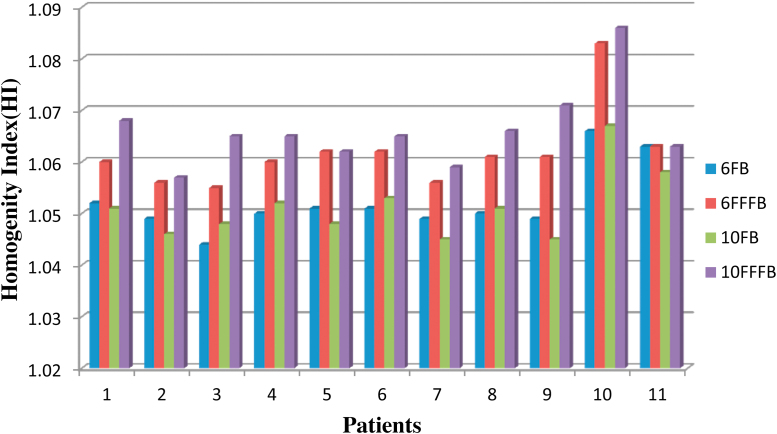
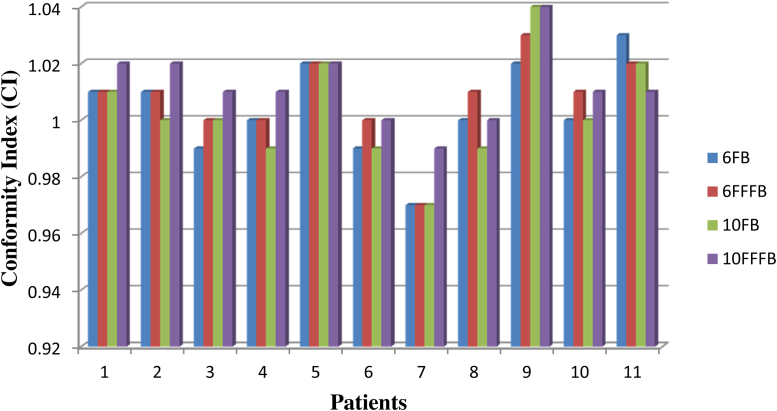
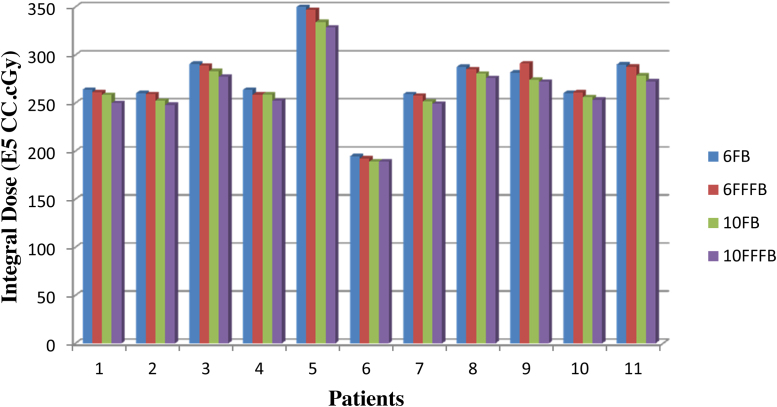
Clinically acceptable and similar RA plans were generated using FB and FFFB of 6 and 10 MV. The dosimetric parameters for PTV coverage generated by RA plans using FB and FFFB of 6 and 10 MV are summarized in Table 1. Data shows more or less similar PTV coverage for RA plans using FB and FFFB of 6 and 10 MV, except mean dose and V107% volume of PTV, which were found significant (p < 0.05) different for FB and FFFB of 6 and 10 MV. FFFB delivers slightly higher mean dose and V107% volume of the PTV in comparison to FB. A comparison of isodose distribution between RA plans using FB and FFFB of 6 and 10 MV for same patient along the axial, coronal and sagittal planes are shown in Fig. 1(a) and (b). DVH form RA plans using FB and FFFB of 6 and 10 MV are shown in Fig. 2(a) and (b). These DVH also do not show any significant difference in PTV coverage for RA plans using FB and FFFB of 6 and 10 MV, except in a high dose region. The calculated meanHI were 1.052 (FB) vs. 1.062 (FFFB), p = 0.000 for 6 MV and 1.051 (FB) vs. 1.066 (FFFB), p = 0.000 for 10 MV and mean CI were 1.004 (FB) vs. 1.007 (FFFB), p = 0.104 for 6 MV and 1.003(FB) vs. 1.012 (FFFB), p = 0.010 for 10 MV in Table 1. FB produces more homogenous and conformal dose distribution to PTV as compared to FFFB. A comparison of HI and CI for RA plans using FB and FFFB of 6 and 10 MV is shown in Fig. 3, Fig. 4, Fig. 5.
Table 1.
Dosimetric data of PTV form RA plans using FB and FFFB of 6 and 10 MV.
| PTV | 6 MV |
p-Value | 10 MV |
p-Value | ||
|---|---|---|---|---|---|---|
| FB | FFF | FB | FFF | |||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||
| Mean (Gy) | 52.00 ± 0.2 | 52.28 ± 0.24 | 0.000 | 52.00 ± 0.23 | 52.42 ± 0.28 | 0.000 |
| V93% | 99.85 ± 0.11 | 99.83 ± 0.13 | 0.146 | 99.84 ± 0.11 | 99.77 ± 0.21 | 0.127 |
| V95% | 99.64 ± 0.14 | 99.62 + 0.18 | 0.308 | 99.63 ± 0.15 | 99.54 ± 0.27 | 0.096 |
| V98% | 98.28 ± 0.22 | 98.20 ± 0.19 | 0.062 | 98.26 ± 0.25 | 98.13 ± 0.28 | 0.073 |
| V100% | 95.07 ± 0.15 | 95.03 ± 0.09 | 0.348 | 95.09 ± 0.09 | 95.09 ± 0.10 | 0.841 |
| V107% | 0.40 ± 0.83 | 2.72 ± 6.57 | 0.004 | 0.45 ± 0.95 | 5.25 ± 8.89 | 0.034 |
| HI | 1.052 ± 0.006 | 1.062 ± 0.008 | 0.000 | 1.051 ± 0.007 | 1.066 ± 0.008 | 0.000 |
| CI | 1.004 ± 0.017 | 1.007 ± 0.016 | 0.104 | 1.003 ± 0.019 | 1.012 ± 0.013 | 0.010 |
| MUs | 525.6 ± 21.12 | 633.7 ± 0.39 | 0.000 | 450.63 ± 23.25 | 647.18 ± 46.15 | 0.000 |
| ID (105 cc Gy) | 2.729 ± 0.36 | 2.718 ± 0.37 | 0.350 | 2.652 ± 0.34 | 2.607 ± 0.33 | 0.000 |
SD, standard deviation; NS, non significant.
Fig. 1.
(a) Comparison of isodose distribution from RA plans using FB and FFFB of 6 MV. (b) Comparison of isodose distribution from RA plans using FB and FFFB of 10 MV.
Fig. 2.
(a) DVH comparison for target coverage and OARs for RA plans using FB and FFFB of 6 MV. (b) DVH comparison for target coverage and OARs for RA plans using FB and FFFB of 10 MV.
Fig. 3.
Graph presenting comparison of Homogeneity Index (HI) for individual patient from RA plans using FB and FFFB of 6 and 10 MV.
Fig. 4.
Graph representing comparison of Conformity Index (CI) for individual patient from RA plans using for FB and FFFB of 6 and 10 MV.
Fig. 5.
Graph presenting Integral doses (ID) comparison for individual patient from RA plans using FB and FFFB of 6 and 10 MV.
5.1. Dose to organ at risk (OAR's)
The Dosimetric data for OARs are summarized in Table 2, they were calculated from DVH of RA plans using FB and FFFB of 6 and 10 MV.
Table 2.
DVH dosimetric data for OARs from RA plans using FB and FFFB of 6 and 10 MV.
| Structure | 6X | 6 FFF | p-Value | 10X | 10 FFF | p-Value |
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||
| Bladder | ||||||
| Mean (Gy) | 40.93 ± 1.31 | 41.30 ± 1.49 | 0.020 | 40.77 ± 1.46 | 41.26 + 1.37 | 0.031 |
| V30Gy (%) | 77.42 ± 3.83 | 79.28 ± 4.79 | 0.045 | 76.70 ± 4.67 | 78.79 + 5.15 | 0.113 |
| V40Gy (%) | 54.24 ± 5.01 | 55.34 ± 5.86 | 0.077 | 54.05 ± 5.40 | 54.80 + 5.02 | 0.165 |
| V50Gy (%) | 34.93 ± 5.36 | 35.57 ± 5.53 | 0.011 | 34.98 + 5.49 | 36.20 + 5.52 | 0.000 |
| Rectum | ||||||
| Mean (Gy) | 40.43 ± 1.42 | 41.09 ± 1.32 | 0.001 | 40.37 ± 1.54 | 41.29 + 1.25 | 0.000 |
| V30Gy (%) | 78.57 ± 5.11 | 81.74 ± 5.44 | 0.001 | 78.62 ± 5.69 | 82.41 + 4.74 | 0.001 |
| V40Gy (%) | 55.31 ± 6.11 | 57.43 ± 6.32 | 0.005 | 55.22 ± 6.54 | 57.83 + 6.11 | 0.001 |
| V50Gy (%) | 26.33 ± 5.30 | 26.92 ± 5.16 | 0.117 | 26.21 ± 5.33 | 28.72 + 4.41 | 0.009 |
| Rt. Femur | ||||||
| Mean (Gy) | 18.51 ± 0.78 | 18.51 ± 0.84 | 0.988 | 18.51 ± 0.85 | 18.32 ± 0.76 | 0.509 |
| V10Gy (%) | 79.52 ± 12.00 | 77.18 ± 7.04 | 0.357 | 79.42 ± 10.12 | 77.36 ± 9.91 | 0.428 |
| V20Gy (%) | 34.75 ± 3.60 | 34.65 ± 5.03 | 0.923 | 33.98 ± 4.12 | 33.74 ± 4.59 | 0.841 |
| V30Gy (%) | 17.04 ± 3.60 | 16.78 ± 3.48 | 0.643 | 17.71 ± 2.96 | 17.00 ± 3.19 | 0.209 |
| V40Gy (%) | 6.30 ± 2.73 | 6.21 ± 2.55 | 0.767 | 6.91 ± 2.47 | 6.34 ± 2.65 | 0.024 |
| Lt. Femur | ||||||
| Mean (Gy) | 18.83 ± 0.67 | 18.79 ± 1.70 | 0.941 | 18.78 ± 0.91 | 18.36 ± 1.11 | 0.225 |
| V10Gy (%) | 78.81 ± 11.71 | 79.11 ± 10.55 | 0.920 | 79.57 ± 11.27 | 75.73 ± 14.51 | 0.318 |
| V20Gy (%) | 36.31 ± 3.86 | 36.16 ± 8.80 | 0.950 | 35.27 ± 4.25 | 33.75 ± 4.17 | 0.125 |
| V30Gy (%) | 17.69 ± 3.46 | 16.80 ± 3.22 | 0.415 | 17.54 ± 4.28 | 16.06 ± 3.96 | 0.000 |
| V40Gy (%) | 6.41 ± 2.55 | 6.10 ± 3.10 | 0.431 | 6.73 ± 3.06 | 6.32 ± 3.04 | 0.063 |
| ID (Body-PTV) | ||||||
| D1% | 47.96 ± 0.73 | 48.12 ± 0.82 | 0.028 | 48 ± 0.81 | 48.20 ± 0.87 | 0.014 |
| D2% | 44.67 ± 1.45 | 45.07 ± 1.57 | 0.006 | 44.72 ± 1.61 | 44.97 ± 1.73 | 0.037 |
| D5% | 37.33 ± 1.98 | 38.01 ± 2.25 | 0.001 | 37.07 ± 2.24 | 37.45 ± 2.53 | 0.048 |
| V2Gy (%) | 66.68 ± 7.84 | 65.68 ± 7.74 | 0.000 | 65.22 ± 7.94 | 63.12 ± 7.81 | 0.000 |
| V5Gy (%) | 54.84 ± 6.91 | 54.47 ± 6.96 | 0.000 | 54.92 ± 7.04 | 54.02 ± 6.96 | 0.000 |
5.2. Dose to bladder
There were reductions in mean dose and dose volumes of V30Gy, V40Gy, V50Gy for FB in comparison to FFFB for 6 and 10 MV in Table 2. This reduction was significant for mean dose (p = 0.020 FB, p = 0.031 FFFB) and V50Gy (p = 0.011 FB, p = 0.000 FFFB).
5.3. Dose to rectum
There were significant (p < 0.05) reductions in mean dose and dose volumes of V30Gy, V40Gy, V50Gy for FB in comparison to FFFB for 6 and 10 MV in Table 2 except V50Gy (p = 0.117) for 6 MV.
5.4. Dose to femurs head
There were no significant (p > 0.05) difference observed for mean doses and dose volumes V10Gy, V20Gy, V30Gy, V40Gy for FB and FFFB of 6 and 10 MV in Table 2. There were noticeable reductions found in volumes of bilateral femoral heads exposed to above said doses and also in mean dose to both femoral heads for FFFB in comparison to FB of 6 and 10 MV.
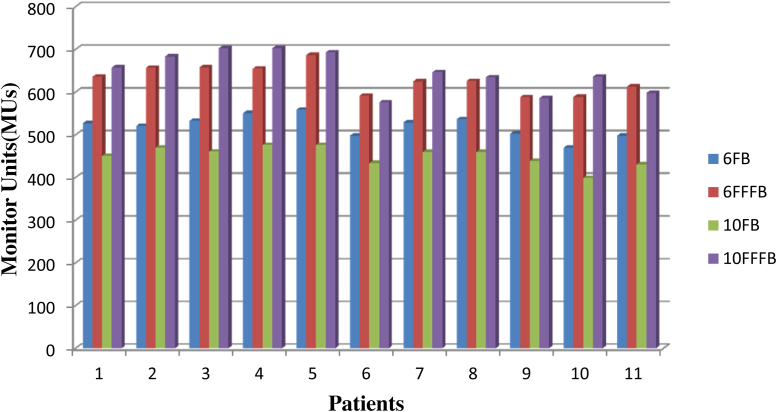
5.5. Monitor units (MUs)
To evaluate the treatment efficiency of RA plans using FB and FFFB of 6 and 10 MV, total numbers of monitor units were studied. There was a significant (p < 0.05) difference in the number of Monitor Units (MUs) for FB and FFFB 6 and 10 MV. FFFB shows a statistically significant (p < 0.05) increase in the numbers of monitor units required as compared to FB. A comparison of total numbers of monitor units (MUs) for individual patient in RA plans using FB and FFFB of 6 and 10 MV is shown in Fig. 6. There was a remarkable increase of 20.5% and 43.7% in MUs found for FFFB of 6 and 10 MV, respectively, in comparison to FB of 6 and 10 MV.
Fig. 6.
Graph presenting comparison of total numbers of Monitor units (MU's) for individual patient from RA plans using FB and FFFB of 6 and 10 MV.
5.6. Integral dose and low doses evaluation for normal tissues
FFFB delivers less ID to normal tissues in comparison to FB in Table 1. There was only 0.5% reduction observed in NTID (p = 0.350) for 6FFFB in comparison to 6 FB. But on the other hand, 10 FFFB shows a significant (p = 0.000) reduction of 1.65% in NTID compared to 10 FB. For low dose volumes of normal tissue, D1%, D2% and D5% and dose volume of V2Gy and V5Gy of normal tissues were calculated form DVH and summarized in Table 2. D1%, D2% and D3% were found significantly (p < 0.05) lower for FB as compared to FFFB of 6 and 10 MV. Apart form this, V2Gy and V5Gy were found significant (p < 0.05) lower for FFFB in comparison to FB of 6 and 10 MV.
6. Discussion
This study performs a dosimetric comparison between FB and FFFB of 6 and 10 MV in the case of cervix RA radiotherapy plans. All qualitative and quantitative evaluations were performed for data driven from dose distribution produced by FB and FFFB of 6 and 10 MV. Dosimetric data do not show any statistically significant difference (p > 0.05) for target coverage for both types of FB and FFFB of 6 and 10 MV. But there were significant (p < 0.05) increments in target mean dose for FFFB as compared to FB for both photon energies. FFFB was found to deliver slightly higher mean target dose compared to FB. Kim et al.18 reported similar findings and concluded that increased mean target dose indicated that homogeneity in target become worse. This study also noticed that FFFB generates inferior (p < 0.05) homogenous dose distribution compared to FB.
For OARs like the bladder and rectum, data shows that FFFB delivers slightly higher mean dose and dose volumes of V30Gy, V40Gy, V50Gy in comparison to FB of 6 and 10 MV. These differences were significant (p < 0.05) for mean dose and V30Gy, V40Gy for the bladder. Similarly, for the rectum, a significant (p < 0.05) difference was found in mean dose and dose volumes of V30Gy, V40Gy, V50Gy, except V50Gy (p = 0.117) for 6 MV.
An effect of sparing low-dose volumes of the bladder and rectum is a very interesting topic of ongoing research. Boice et al.19 reported that doses as low as 30 Gy increase the relative risk of secondary bladder cancer to a similar degree as 80 Gy in cervical cancer. Similar Gulliford et al.20 found that the volume of the rectum receiving as low as 30 Gy reduced the incidence of several types of patient reported late rectal toxicities by 10–18%. Hence, dosimetric benefits are larger for FB as compared to FFFB for both types of photon energies in cervix carcinomas RA planning to avoid late complication related to the bladder and rectum.
This study also indicates that increased numbers of monitor units (MUs) were required for FFFB compared to FB of both photon energies, as the intensity of FFF beam abruptly decreases with off-axis distance for field sizes larger than and equal to 10 × 10 cm2, which requires the off-axis distance-dependence intensity modulation of FFF photon beam. This necessitates large no. of MUs to deliver uniform dose to the tumor.21 Kim et al.18 also reported the same based on a study of monitoring unit efficiency for flattening-filter free photon beam in association with tumor size and location. Increased MUs for FFFB in comparison to FB were also reported by Rout et al.22 and Zwahlen et al.23 in their findings.
FFFB shows reduction in NTID and low dose volumes of normal tissues like V2Gy and V5Gy compared to FB for both photon energies. This is because of the reduction in scatter and leakage radiation form FFFB beam as a consequence of target removal from the radiation path. Kargl et al.24 reported that in the case of IMRT prostate using FFF beams results in a reduction of treatment head leakage by 52% and 65% for 6 and 10 MV, respectively. Similarly, Cashmore et al.5 also found that IMRT using FFF beams removed unwanted and unnecessary scatter dose by up to 70%.
Major limitation of this study is that it is based on planning data rather than a clinical evidence based statistics. But this study carefully investigated the dosimetric difference between FB and FFFB of 6 and 10 MV RA plans for rapid arc cervix cancer and gives an overview to better understand the difference between FB and FFFB for their future clinical use in cervix radiotherapy RA plans.
7. Conclusion
RA plans using FFFB yield similar target coverage but for same coverage FB spares more bladder and rectum compared to FFFB for both photon energies. This reduces the toxicity level to the patients post radiotherapy delivery. FB also generates more conformal and homogenous RA plans compared to FFFB. This study concludes that FB is more beneficial for cervix RA radiotherapy planning in comparison to FFFB.
Conflict of interest
None declared.
Financial disclosure
None declared.
Acknowledgements:
Authors thank to the management of Rajiv Gandhi Cancer Institute & Research Centre, New Delhi, India for their continued support and encouragement to complete this work.
References
- 1.2013. International Agency for Research on Cancer, Press Release. [Google Scholar]
- 2.Ohno T., Kato S., Sato S. Long-term survival and risk of second cancers after radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2007;69(November (3)):740–745. doi: 10.1016/j.ijrobp.2007.04.028. [DOI] [PubMed] [Google Scholar]
- 3.Georg D., Knöös T., McClean B. Current status and future perspective of flattening filter free photon beam. Med Phys. 2011;38(March (3)):1280–1293. doi: 10.1118/1.3554643. [DOI] [PubMed] [Google Scholar]
- 4.Titt U., Vassiliev O.N., Pönisch F., Dong L., Liu H., Mohan R. A flattening filter free photon treatment concept evaluation with Monte Carlo. Med Phys. 2006;33(June (6)):1595–1602. doi: 10.1118/1.2198327. [DOI] [PubMed] [Google Scholar]
- 5.Cashmore J., Ramtohul M., Ford D. Lowering whole-body doses in pediatric intensity-modulated radiotherapy through the use of unflattened photon beams. Int J Radiat Oncol Biol Phys. 2011;80(July (4)):1220–1227. doi: 10.1016/j.ijrobp.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 6.O’Brien P.F., Gillies B.A., Schwartz M., Young C., Davey P. Radiosurgery with unflattened 6MV photon beams. Med Phys. 1991;18(May–June (3)):519–521. doi: 10.1118/1.596656. [DOI] [PubMed] [Google Scholar]
- 7.Kragl G., af Wetterstedt S., Knäusl B. Dosimetric characteristics of 6 and 10 MV unflattened photon beams. Radiother Oncol. 2009;93(October (1)):141–146. doi: 10.1016/j.radonc.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 8.Hrbacek J., Lang S., Klöck S. Commissioning of photon field of a flattening filter-free linear accelerator and the accuracy of beam modelling using an anisotropic analytical algorithm. Int J Radiat Oncol Biol Phys. 2011;80(July (4)):1228–1237. doi: 10.1016/j.ijrobp.2010.09.050. [DOI] [PubMed] [Google Scholar]
- 9.Stathakis S., Esquivel C., Gutierrez A., Buckey C.R., Papanikolaou N. Treatment planning and delivery of IMRT using 6 and 18 MV photon beams without flattening filter. Appl Radiat Isot. 2009;67(September (9)):1629–1637. doi: 10.1016/j.apradiso.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 10.Vassiliev O.N., Kry S.F., Kuban D.A., Salehpour M., Mohan R., Titt U. Treatment-planning study of prostate cancer intensity modulated radiotherapy with a varian Clinac opertated without flattening filter. Int J Radiat Oncol Biol Phys. 2007;68(August (5)):1567–1571. doi: 10.1016/j.ijrobp.2007.04.025. [DOI] [PubMed] [Google Scholar]
- 11.ICRU Report 50 . International Commission on Radiation Units and Measurements; Bethesda: 1993. Prescribing, recording, and reporting photon beam therapy. [Google Scholar]
- 12.ICRU Report 62 . International Commission on Radiation Units and Measurements; Bethesda: 1999. Prescribing, recording, and reporting photon beam therapy. Supplement to ICRU report 50. [Google Scholar]
- 13.IAEA; Vienna: 2000. An International code of Practice for Dosimetry based on absorbed dose to water, IAEA Tech. Series No. 398, Absorbed dose determination in external beam radiotherapy. [Google Scholar]
- 14.Varian Medical Systems . 2010. Eclipse Algorithms Reference Guide. P/N B502679R01B. [Google Scholar]
- 15.Tyagi A., Supe S.S., Sandeep, Singh M.P. A Dosimetric analysis of 6 MV verses 15 MV photon energy plans for intensity modulated radiation therapy (IMRT) of carcinoma of cervix. Rep Pract Oncol Radiother. 2010;15(September (5)):125–131. doi: 10.1016/j.rpor.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.D'Souza W.D., Rosen I.I. Nontumor integral dose variation in conventional radiotherapy planning. Med Phys. 2003;30(August (8)):2065–2071. doi: 10.1118/1.1591991. [DOI] [PubMed] [Google Scholar]
- 17.Slosarek K., Osewski W., Grzadzial A. Integral dose: comparison between four techniques for prostate radiotherapy. Rep Pract Oncol Radiother. 2014;20(November (2)):99–103. doi: 10.1016/j.rpor.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim D.I., Kim J.I., Yoo S.H., Park J.M. Study on monitoring unit efficiency of flattening-filter free photon beam in association with tumor size and location. J Radiat Protect. 2013;38(December (4)) [Google Scholar]
- 19.Boice J.D., Jr., Day N.E., Andersen A. Second cancers following radiation treatment for cervical cancer. An International collaboration among cancer registries. J Natl Cancer Inst. 1985;74(May (5)):955–975. [PubMed] [Google Scholar]
- 20.Gulliford S.L., Foo K., Morgan R.C. Dose-volume constraints to reduce rectal side effects from prostate radiotherapy: evidence from MRC RT01 Trail ISRCTN 47772397. Int J Radiat Oncol Biol Phys. 2010;76(March (3)):747–754. doi: 10.1016/j.ijrobp.2009.02.025. [DOI] [PubMed] [Google Scholar]
- 21.Sharma S.D. Unflattened photon beams from the standard flattening filter free accelerators for radiotherapy: advantages, limitations and challenges. J Med Phys. 2011;36(July (3)):123–125. doi: 10.4103/0971-6203.83464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rout B.K., Muralidhar K.R., Ali M., Shekar M.C., Kumar A. Dosimetric study of rapid arc plans with flattened beam (FB) and flattening filter-free (FFF) beam for localized prostate cancer based on physical indices. Int J Cancer Ther Oncol. 2014;2(4):02046. [Google Scholar]
- 23.Zwahlen D.R., Lang S., Hrbacek J. The use of photon beams of a flattening filter-free linear accelerator for Hypofractionated volumetric modulated arc therapy in localized prostate cancer. Int J Radiat Oncol Biol Phys. 2012;83(August (5)):1655–1660. doi: 10.1016/j.ijrobp.2011.10.019. [DOI] [PubMed] [Google Scholar]
- 24.Kragl G., Baier F., Lutz S. Flattening filter free beams in SBRT and IMRT: dosimetric assessment of peripheral doses. Z Med Phys. 2011;21(May (2)):91–101. doi: 10.1016/j.zemedi.2010.07.003. [DOI] [PubMed] [Google Scholar]