Abstract
Objective
Evaluation of differences in the clinical performance and crestal bone levels between implants restored with single crowns with platform‐matched or platform‐switched abutments after 3 years.
Material and Methods
The study enrolled adult patients missing two or more adjacent teeth in the posterior mandible with natural teeth mesial to the implant site. Randomization followed open‐flap implant insertion and the corresponding matching or switching healing abutments placed at surgery. Conventional loading was made with cemented crowns. Clinical follow‐up took place annually after loading up to 3 years. Bone level changes were measured in standardized radiographs as the variation in crestal bone from one evaluation to the next.
Results
Sixty‐three patients with a total of 135 implants (66 platform matching, 69 platform switching) were analysed. From surgery to 36 months, mean bone loss was 0.28 ± 0.56 mm for the platform‐switching group and 0.68 ± 0.64 mm for the platform‐matching group. A statistically significant difference was found between groups (p = 0.002) with an estimate of 0.39 mm (0.15–0.64, 95% CI) in favour of platform switching.
Conclusions
After 3 years, platform‐switching restorations showed a significant effect in the preservation of marginal bone levels compared to platform‐matching restorations.
Keywords: bone level, crestal bone preservation, implant, implant success, platform match, platform switching, randomized clinical trial, standardized radiograph
Crestal bone loss around dental implants of 1.5 mm during the first year followed by a loss of 0.2 mm in the subsequent years has been generally considered acceptable for two‐piece dental implants (Albrektsson et al. 1994, Smith & Zarb 1989). However, the maintenance of crestal bone levels is crucial for the preservation of gingival margins and inter‐dental papillae (Tarnow et al. 1992, Choquet et al. 2001, Tarnow et al. 2003) and eventually for the success of the implant‐supported prosthetic rehabilitation.
It is possible to find in the literature several attempts to preserve marginal bone levels around implants. New implant designs, new surfaces, and different time to load approaches have tried to mitigate the bone resorption event, which has been considered normal provided that some boundaries defined and accepted by the scientific community are respected (Albrektsson et al. 1986, Berglundh et al. 2002). Nevertheless, some authors consider the aforementioned event a drawback in implantology and regard the strategies to enhance conditions to stabilize bone level with correspondent positive effects in soft tissues and promising long‐term results as unavoidable (Lang et al. 2009, Laurell & Lundgren 2011).
Biological, clinical, and mechanical factors have been accepted to some degree as contributors to the process leading to marginal bone loss around implants, which has been considered as a normal time‐dependent phenomenon, notably in the first year. Notwithstanding that, different authors report that a mismatch between the implant and subsequent components (healing and prosthetic abutments) leads to a positive effect in marginal bone levels (Lazzara & Porter 2006, Vigolo & Givani 2009, Canullo et al. 2009).
The increasing understanding of the underlying biological processes (Lazzara & Porter 2006, Luongo et al. 2008) and biomechanics (Maeda et al. 2007, Chang et al. 2010, Schrotenboer et al. 2008) proposed to be associated with the implant–abutment mismatch (platform switching) contributed to a growing clinical acceptance. Also, the similar results noticed for the platform switching in external and internal connections promoted the extended application of the concept to different types of connections.
Some studies show evidence of a significant number of cases where the so‐called unavoidable continuous marginal bone resorption turned to a truly radiographic marginal bone recovery over time (Oxby et al. 2015) (Donati et al. 2015) (Moergel et al. 2015). However, the difference needed between the outer limit of the implant and the healing and prosthetic abutments that effectively benefits bone preservation is not clear. Some authors suggested a minimum of 0.4 mm (Atieh et al. 2010), but others demonstrated comparable results with 0.3–0.35 mm (Prosper et al. 2009, Guerra et al. 2014).
Several systematic reviews including a limited number of studies with high heterogeneity, mentioned the valuable effect of the platform‐switching concept, but point at the urgent need for prospective, randomized controlled clinical studies with limited confounders and longer follow‐up results (Atieh et al. 2010, Al‐Nsour et al. 2012, Annibali et al. 2012, Strietzel et al. 2014, Chrcanovic et al. 2015).
Therefore, the purpose of this prospective randomized controlled multicentre clinical study was to assess differences in bone level changes between platform‐switching (PS) and platform‐matching (PM) unitary cemented restorations after 3 years of function in the posterior mandible. Secondary objectives include implant success and survival rate at 3 years post‐loading, performance of the restorative components, and nature and frequency of adverse events.
Materials and Methods
This study reports the third year results of a prospective multicentre randomized clinical trial on the effect of the platform‐switching concept on bone level preservation around CAMLOG® SCREW‐LINE implants. The trial was designed in accordance with the Declaration of Helsinki (2008) and three centres located in Germany (two) and Portugal (one) were included after approval of the competent Ethics Committees (FECI 09/1308 and CES/0156). Approval covered all evaluation periods up to 5 years.
Study population, randomization, and clinical procedures have been previously described in detail by Guerra et al. (2014) and are briefly outlined in the present work.
Study population and inclusion and exclusion criteria
The study enrolled adult patients with healed edentulous sites in the posterior mandible missing two or more adjacent teeth, presenting a natural tooth mesial to the implant site, and adequate bone volume for the insertion of dental implants without requiring bone regeneration procedures. The opposing dentition was natural teeth or implant‐supported restoration.
Exclusion criteria comprised uncontrolled systemic diseases, medications interfering with bone metabolism, radiation therapy in the head or neck area, inability to perform adequate oral health, and smoking habits superior to 10 cigarettes/day. Patients with previous history of implant failure and untreated periodontitis were also excluded. Locally, only situations of medium or thick soft tissue biotype presenting in the prospective implant position, a minimum of 4‐mm keratinized mucosa in the buccal–lingual direction were allowed. Lack of primary stability or inappropriate positioning of the implant to fulfil the prosthetic requirements also led to exclusion at surgery.
Material and clinical procedures
Each edentulous site received 2–3 neighbouring CAMLOG® SCREW‐LINE implants with Promote® plus surface (CAMLOG Biotechnologies AG, Basel, Switzerland) and a machined collar of 0.4 mm. The most adequate implant diameter (3.8, 4.3, or 5.0 mm) and length (9, 11, and 13 mm) were selected according to the available bone. Surgery was performed under local anaesthesia by raising a full‐thickness flap and respecting a minimum distance of 3 mm between implants and 1.5–2 mm between the implant and the neighbouring tooth.
After the insertion of the two implants per site, each quadrant was randomly allocated to the PS or PM group and received the corresponding transgingival healing abutments (Fig. 1a). For the randomization process, an independent person generated, prior to the surgeries, a blocked randomization list with block sizes of 4 or 6 in order to ensure a balance in sample size across groups over the time of recruitment. In each surgery, the investigators received a sealed envelop with result of the treatment arm to apply to each patient, which was opened if the patient fulfilled all inclusion criteria. If any of the implants did not meet the inclusion criteria, the quadrant was not randomized.
Figure 1.
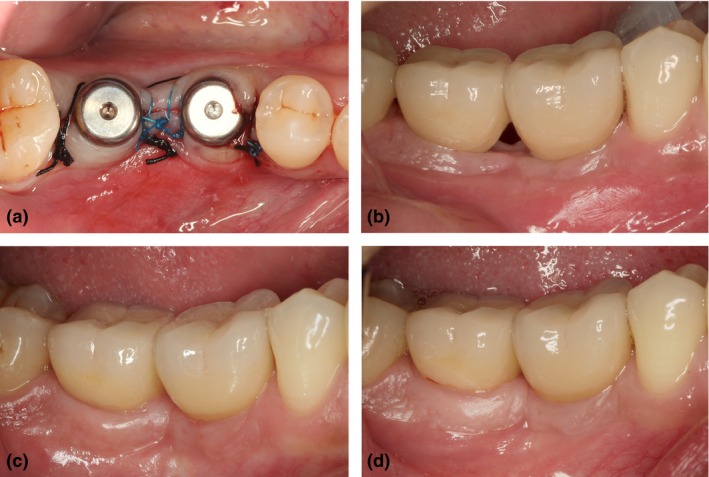
Clinical images of a representative case. (a) Healing abutments inserted according to the randomization result, (b) individual metal‐ceramic crowns cemented (loading day), (c) 1 year post‐loading evaluation, and (d) 3 years post‐loading evaluation.
Conventional load with single cement‐retained crowns was performed after 6–8 weeks in implants inserted in type I–III bone and after 12–14 weeks in type IV bone. Loading was the baseline for upcoming evaluations (Fig. 1b–d).
Primary and secondary objectives
The primary objective of the present trial was to test for equivalence of crestal bone levels around CAMLOG® SCREW‐LINE implants restored with either PS or PM abutments, assuming 0.00 mm as the true difference between bone level changes (BLC) group means and 0.2 mm as the maximum difference between group means in similarly distributed groups with 0.3 mm standard deviation. Sample size power calculation determined that 64 implants in the PS group and 64 implants in the PS group were necessary to achieve 80% power at a significant level of 0.01, and further increased to compensate for the dropout rate during the 5 years of the trial.
Bone level measurements were performed on standardized peri‐apical radiographs obtained with a customized sensor holder (Guerra et al. 2014, Messias et al. 2013) before surgery, immediately after surgery with healing abutment, at restoration placement, and every 12 months post‐loading until the 60th month appointment (Fig. 2). The marginal bone levels at the mesial and distal sides of the implant were considered the primary outcome measures and obtained by one investigator at each centre, and analysed and validated by an independent person using ImageJ 1.44 (http://imagej.nih.gov/ij/) to measure the distance from the implant shoulder to the first visible bone contact (DIB). Intra‐class correlation coefficient determined very good reliability of the measurements obtained by the investigators and the independent examiner (ICC = 0.915 using a two‐way random effects model for single measures with absolute agreement definition). Compulsory agreement between measurements from the centre and the external evaluation had to be reached for all cases presenting differences superior to 0.2 mm. Mesial and distal measurements were subsequently averaged to determine mean implant bone level.
Figure 2.
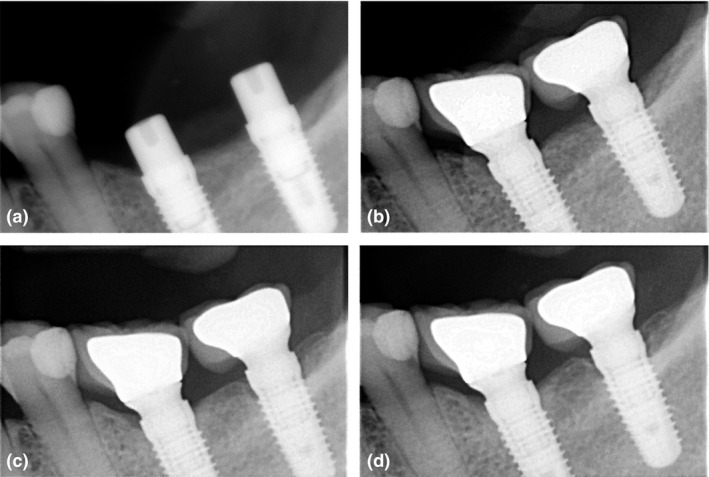
Standardized radiographic images of the case presented. (a) Surgery, (b) loading, (c) 1 year post‐loading, and (d) 3 years post‐loading.
Secondary objectives included determination of implant survival and success at each year post‐loading, evaluation of adverse events, and performance of restorative components. Implant success was determined based on the absence of mobility, radiolucency, recurrent infection, and pain, as defined by Buser et al. (2002). Restorative components were considered successful based on continuous stability and function, and absence of patient discomfort.
Plaque index (PLI: 0–3), sulcus bleeding index (SBI: 0–3), and probing pocket depth (PPD) were measured at four sites per implant at loading and all subsequent evaluations until the third year appointment.
Statistical methods
Descriptive statistics were reported for demographic characterization of the patients. For continuous variables, means and standard deviations were calculated for each treatment group, as well as mean ranks for ordinal variables and absolute and relative frequencies for categorical variables. Association between treatment group and categorical variables was performed with the chi‐square test for association or Fisher's exact test depending on the number of categories. Differences between ordinal variables in different time points were assessed with Wilcoxon signed‐rank test. The log‐rank Mantel–Cox test was used to assess equality of survival between groups.
For each group, differences in bone level measurements (DIB) per implant between consecutive evaluations were determined with repeated measures anova using post hoc multiple testing with Bonferroni correction.
Bone level changes were calculated as the difference in bone level measurements per implant (DIB) between each period of evaluation and the following and between surgery and 36 months, load and 36 months, and from 12 to 36 months.
Mixed effects models were used to determine differences between groups on bone level change accounting for possible random effects caused by correlations between implants within the same patient and between patients within each centre. The multilevel approach considered randomization group as the main fixed effects, and patients and centre (highest level) as the random effects to determine differences between PS and PM using the restricted maximum likelihood estimation method. Significance level was set at 0.05.
Results
This study presents the 3 years results of the ongoing randomized controlled clinical trial previously reported at the first year evaluation (Guerra et al. 2014).
From the initial sampling of 67 patients that received prosthesis and completed the 1 year evaluation, one patient died before the 24 months visit and two patients carrying five implants were lost to follow‐up at the 24 and 36 months visits (three PS and two PM, respectively). One additional patient experienced unexplained excessive bone loss in both implants at the 24‐month appointment and was declared as failure and dismissed from the protocol. Consequently, 63 patients with a total of 135 implants (66 PM, 69 PS) were evaluated and considered for analysis. The CONSORT flow diagram is available as Fig. S1.
Subjects and implants
No major changes in the demographical and clinical parameters, as well as in the distribution of implant length and diameter, were observed from baseline to the third year due to patient loss to follow‐up (Table 1 and Table S1). A slight improvement in hygiene habits could be detected from the day of surgery to the 3 years follow‐up (p = 0.018), with 6.7% patients presenting excellent hygiene, 85% good, and 8.3% fair.
Table 1.
Demographic and clinical parameters of the study population and implanted sites at baseline and 36 months follow‐up
| Characteristics (N) | Platform switching | Platform matching | ||
|---|---|---|---|---|
| Surgery | 36 months | Surgery | 36 months | |
| 35 | 33 | 33 | 30 | |
| Mean age (SD) (years) | 52.84 (10.38) | 52.36 (9.89) | 49.97 (14.77) | 50.30 (15.05) |
| Gender | ||||
| Male/Female | 18/17 | 17/16 | 19/14 | 18/12 |
| Quadrants randomized | ||||
| 2 Adjacent implants | 31 | 30 | 27 | 24 |
| 3 Adjacent implants | 4 | 3 | 6 | 6 |
| Implants (n) | ||||
| Total | 74 | 69 | 72 | 66 |
| Centre 1 | 12 | 12 | 12 | 12 |
| Centre 2 | 25 | 20 | 22 | 18 |
| Centre 3 | 37 | 37 | 38 | 36 |
| Bone quality; n implants (%) | ||||
| Type I | 4 (5.4) | 4 (5.8) | 4 (5.6) | 3 (4.5) |
| Type II | 40 (54.1) | 35 (50.7) | 45 (62.5) | 40 (60.6) |
| Type III | 26 (35.1) | 26 (37.7) | 22 (30.6) | 22 (33.3) |
| Type IV | 4 (5.4) | 4 (5.8) | 1 (1.4) | 1 (1.5) |
Implant success and complications
As previously reported, two implants of the PS group were lost during the healing period, prior to restoration placement (1 month after surgery), yielding 97.3% survival for an estimate follow‐up of 35.05 months (33.76–36.48, 95% CI). After load, one patient of the PM group revealed bone loss superior to 2 mm between consecutive appointments (12–24 months) and was therefore considered a failure, conferring 97.1% survival at an estimate 35.66 months (35.19–36.12, 95% CI). No differences were found between groups for the survival function (p = 0.978). No further adverse events were reported after the 12 months follow‐up.
Plaque index, sulcus bleeding index, and probing depth over time
The plaque index and sulcus bleeding index measurements obtained in each of the four sites of implant were averaged and used as single values.
Even though plaque index increased irrespective of group from the 12th to the 36th month (p < 0.01), 53.5% of all implants scored 0 and in 17.3% implants a single measurement site was affected and scored 1. Bleeding index and pocket probing depth remained stable over time (Table 2).
Table 2.
Evolution of the clinical parameters plaque index, sulcus bleeding score, and pocket probing depth from loading to 36 months
| Platform switching | Platform matching | |||
|---|---|---|---|---|
| N | Mean ± SD | N | Mean ± SD | |
| Plaque index (score 0–3) | ||||
| Loading | 68 | 0.25 ± 0.46 | 69 | 0.06 ± 0.18 |
| 12 months | 72 | 0.10 ± 0.21 | 70 | 0.09 ± 0.18 |
| 36 months | 67 | 0.26 ± 0.34 | 60 | 0.20 ± 0.24 |
| Sulcus bleeding index (score 0–3) | ||||
| Loading | 68 | 0.05 ± 0.12 | 69 | 0.01 ± 0.06 |
| 12 months | 72 | 0.21 ± 0.28 | 70 | 0.20 ± 0.29 |
| 36 months | 67 | 0.30 ± 0.32 | 60 | 0.22 ± 0.29 |
| Pocket probing depth | ||||
| Loading | 64 | 1.78 ± 0.79 | 61 | 1.69 ± 0.51 |
| 12 months | 72 | 2.21 ± 0.47 | 70 | 2.46 ± 0.51 |
| 36 months | 67 | 2.08 ± 0.60 | 60 | 2.22 ± 0.66 |
Radiographic changes in crestal bone levels
As previously reported, from the initial sampling of 142 implants that received the prosthesis, standardized radiographs were not available for 11 implants at loading and for two implants at 12 months. At the 24 months follow‐up, 131 implants were considered as no radiographs were available for one patient (two implants). Standardized radiographs were taken for all patients that attended the 36 months follow‐up and 135 implants were considered.
Figure 3 represents mean crestal bone levels within each group for successive evaluations.
Figure 3.
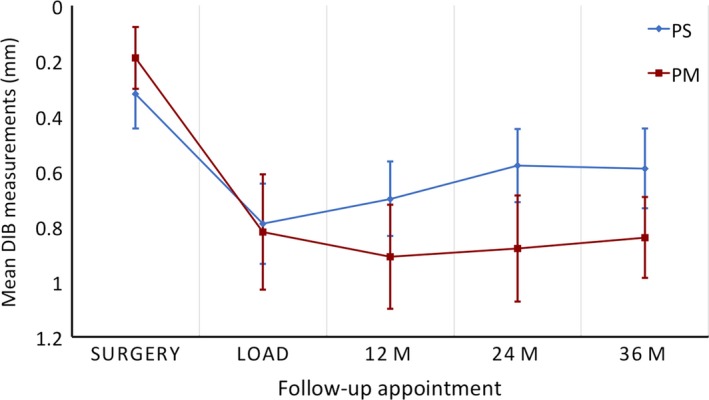
Mean (95% CI) bone level measurements (in millimetres) for each group over the five evaluation points.
Crestal bone remodelling was noticeable from surgery to load for both groups, but afterwards the trend points to bone regain in the PS group and to the stabilization of PM bone levels. For each group, repeated measures anova detected significant variations on crestal bone level over time (p < 0.01 for both groups) with surgery bone levels statistically superior to bone levels determined for all other periods. However, while the PM group only showed a significant bone loss from surgery to load and no differences in any other period, the PS implants also presented a significant bone regain of 0.11 ± 0.24 mm from 12 to 24 months, as stated in Table 3a in which a positive value represents bone gain and negative value bone loss.
Table 3.
(a) Changes in radiographic crestal bone level between successive follow‐up appointments for the PS and PM groups. Mean variation and standard deviation in millimetres. Within‐group comparisons performed with paired t test adjusted with Bonferroni correction. (b) Bone level change comparison across the two groups. Univariate analysis (t test) and multilevel analysis with patient clustering within centres of the multicentre trial. Mean differences and 95% confidence intervals (CI) in mm
| (a) | Surgery to load | Load to 12 months | 12–24 months | 24–36 months | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean ± SD | p | N | Mean ± SD | p | N | Mean ± SD | p | N | Mean ± SD | p | |
| PS | 70 | −0.5 ± 0.42 | <0.01 | 70 | 0.08 ± 0.41 | NS | 69 | 0.11 ± 0.24 | <0.01 | 69 | −0.01 ± 0.26 | NS |
| PM | 63 | −0.66 ± 0.70 | <0.01 | 61 | −0.06 ± 0.49 | NS | 64 | −0.01 ± 0.30 | NS | 64 | −0.04 ± 0.16 | NS |
| (b) | Univariate analysis (t test) | Multilevel analysis | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PS versus PM | Fixed effect (PS versus PM) | Random effects | ICC | ||||||
| Mean difference (95% CI) | p | Parameter estimate (95% CI) | p | Wald Z | p | ||||
| BLC surgery–load | 0.15 (−0.04–0.35) | 0.12 | 018 (−0.06–0.42) | 0.148 | 3.18 | 0.001 | 0.43 | ||
| BLC load–36 months | 0.25 (0.06–0.44) | 0.01 | 0.23 (−0.02–0.47) | 0.07 | 3.54 | <0.01 | 0.39 | ||
| BLC 12–36 months | 0.14 (0.02–0.26) | 0.02 | 0.11 (−0.03–0.26) | 0.13 | 3.44 | 0.001 | 0.45 | ||
| BLC surgery–36 months | 0.40 (0.20–0.60) | <0.01 | 0.39 (0.15–0.64) | 0.002 | 2.65 | 0.008 | 0.34 | ||
ICC, intra‐cluster correlation; BLC, bone level changes; PS, platform switching; PM, platform matching.
Bold values represent significant differences at the 0.05 level.
Within each randomization group (PS or PM) no statistically significant differences could be detected between 3.8, 4.3, and 5.0 diameter implants (p > 0.05 for all periods considered). Implant diameter was therefore excluded from further analysis and not introduced in the mixed model.
In order to assess differences in bone level changes between groups from surgery to 36 months, from load to 36 months, and from 12 to 36 months, the multilevel structure of analysis included implants (first level) nested within patients (second level) from three different centres (highest level). Table 3b reflects the results of the multilevel analysis and corresponding covariance explained by the inclusion of random effects [intra‐cluster correlation (ICC)], as well as the corresponding univariate analysis (t test). Significant effects owing to between‐patient variability were found for all periods analysed, as determined by the Wald Z statistics, conferring the need for the mixed analysis with both random and fixed effects. In the same table, the fixed effects parameter estimates reports the adjusted difference between PS and PM.
From surgery to 36 months, mean BLC was −0.28 ± 0.56 mm for the PS group and −0.68 ± 0.64 mm for the PM group. In this period, differences among patients accounted for 34% (ICC = 0.34) of BLC variation. The model adjusted for clustering detected a statistically significant effect of the randomization group (p = 0.002) with an estimate of 0.39 (0.15–0.64, 95% CI) in favour of the PS group. From load to 36 months, the PS group registered a mean bone gain of 0.16 ± 0.53 mm, whereas a slight decrease of −0.08 ± 0.52 mm was found in the PM group but no significant effect could be detected. However, for the same period, bone gain (BLC > 0.0 mm) was statistically associated to the PS group (p = 0.002) as represented in Fig. 4.
Figure 4.
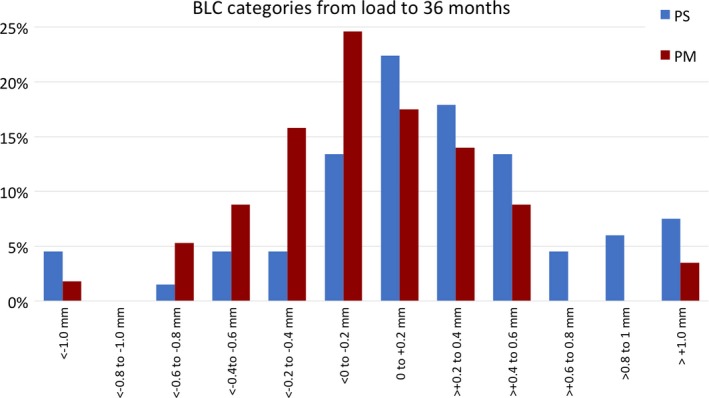
Categorization of bone level changes from loading to 36 months in 0.2 mm intervals. Relative frequencies (%) of the cases allocated to each interval per group.
Within the 2 years that preceded the 36 months follow‐up (from 12 months onwards), PS implants continued the trend for bone gain (0.1 ± 0.36 mm), whereas the PM implants stabilized with a mean BLC of −0.04 ± 0.33 mm. Even though the univariate analysis declared the mean difference between groups as significant (0.02–0.26 mm, 95% CI), the clustered analysis could not find a fixed effect of randomization on BLC from 12 to 36 months (Table 3b).
Discussion
The present multicentre RCT has evaluated, over the course of 3 years, the clinical and radiological performance of dental implants restored with either PS or PM abutments. From the surgical procedure to the 36 months evaluation, PS restored implants showed higher bone maintenance with an estimated difference of 0.39 mm (0.15–0.64, 95% CI) to the PM group. The trend could be observed in all other periods even though no statistically significant effect could be detected in the mixed model including the random effects generated by correlations between implants within patients and by correlations within patients from different centres.
The results here reported assume a particular interest in the evaluation of the effect of the use of mismatching abutments due to the careful study design employed. The study made use of implants with the same macro‐ and micro‐geometry, same flat prosthetic platform, same 0.4 mm machined collar, and an internal tube–tube implant–abutment connection for both groups allowing better comparable conditions and reducing as much as possible the existence of confounder factors as recommended by the authors of several systematic reviews (Al‐Nsour et al. 2012, Strietzel et al. 2014, Annibali et al. 2012, Laurell & Lundgren 2011). In this sense, block randomization was done only after implant installation to avoid foreknowledge of the treatment assignment and possible tendencies to favour either group by the modification of the surgical protocol. The importance of the allocation concealment and moment of randomization has, in fact, been widely recognized as one of the major factors preventing bias and overestimation of treatment effects (Cairo et al. 2012, Esposito et al. 2001).
Also, the use of healing abutments, impression posts, and prosthetic abutments commercially available and produced deliberately for both the PS concept and for the PM procedures from surgery onwards allowed a closer perspective regarding the daily basis clinical procedures and a better understanding about daily basis procedures and choices within the same implant system.
As for a start, the implant survival rate was comparable across the two groups and seems not to be influenced by the platform concept. Also, in both groups, the excellent patient compliance in regards to the oral hygiene contributed to the resulting steady soft tissue parameters plaque index, sulcus bleeding index, and probing pocket depths, which empowered the overall implant success.
Taking into consideration the practical clinical implication of the study, bone level evaluations were performed with peri‐apical radiographs, yet the most frequently used method for implant evaluation, even though they limit bone level evaluation to the mesial and distal sides of the implant, withdrawing the possibility of buccal and lingual bone analysis. Notwithstanding this, the standardization of radiographs throughout the course of the study allowed very good reproducibility and accurate measurements of proximal bone (Messias et al. 2013, Schropp et al. 2012). This ensures that variations found from one observation to the subsequent are not attributable to variations in the geometric projection of the radiograph (De Smet et al. 2002, Schulze & d'Hoedt 2001), thus focusing on true crestal bone variation and reducing the possibility of bias arising from measurement error.
The initial changes in crestal bone levels that took place equally in both groups after surgery and before loading were responsible for the great majority of the total variation that was recorded in the 36 months period. In fact, 98% of the negative variation that occurred in the PS group was associated to that period as well as 85% of the bone loss of the PM group, similarly to other studies (Cochran et al. 2009a,b, Cassetta et al. 2015, Moergel et al. 2015). As in the study of Wang et al. (2015), no statistically significant differences were found between groups for the aforementioned period, suggesting that the mismatching between implant and prosthetic components has a very limited effect on bone remodelling during the healing phase. This could be attributable to a theoretical response to device installation (Albrektsson et al. 2012) with re‐establishment of the biological width and maturation of the barrier function that takes place following bacterial invasion of the implant/abutment interface and requires 6–8 weeks of healing (Canullo et al. 2012, Hermann et al. 2000, 2001, Sculean et al. 2014).
This initial remodelling set a similar bone level basis (DIB measurement) across groups (Fig. 3) for loading and subsequent evaluations. From this point onwards, the two groups revealed different behaviours. Although the PS group presented a positive bone variation of 0.16 ± 0.54 mm, the PM group stabilized with residual negative variation of −0.08 ± 0.52 mm, reflecting a certain incapacity to revert the initial bone loss. In fact, despite the non‐significant difference for the period (Table 3b), bone gain was statistically associated to the PS group (Fig. 4) occurring in 72% of the implants against 44% of the PM implants. Several factors have been described potentially affecting crestal bone levels after load, such as local and systemic patient‐related factors, implant and prosthetic factors, surgical factors, and biological and/or biomechanical factors. In the present study with controlled action of possible confounders, namely implant geometry, and data analysis taking into consideration patient variability, the differences between groups could be attributed to the restorative process with PS or PM abutments. The mechanism that makes the PS concept beneficial for bone gain or preservation is yet to be demonstrated. On the one hand, some authors report the results of finite element analysis to attribute the phenomenon to a biomechanical optimization of stress distribution in peri‐implant bone (Tabata et al. 2011, Pessoa et al. 2014, Canullo et al. 2011b). However, for similar clinical situations regarding alveolar width and height as imposed in the inclusion criteria of the present study, the effect was considered insignificant (Pessoa et al. 2010). On the other hand, other authors associate it to the increased biological width of these restorations that present improved transmucosal barrier function and/or an inferior inflammatory infiltrate of the sulcus (Canullo et al. 2011c, Sculean et al. 2014). In fact, animal studies have shown that implant sites with narrower mucosal thickness consistently reveal marginal bone resorption to adjust for the acceptable biological width around implants (Berglundh & Lindhe 1996), which could be the clinical situation associated to PM when compared to PS restorations. This raises the issue of the minimum mismatch needed between implant and abutment to prevent marginal bone resorption. Systematic reviews of clinical studies on the PS concept described that discrepancies superior to 0.4 mm (Atieh et al. 2010) or 0.45 mm (Annibali et al. 2012) have been to the advantage of the PS implants in parallel arm and split‐mouth trials (Canullo et al. 2010, 2009, 2011a, Fickl et al. 2010, Hurzeler et al. 2007), even though inferior mismatches have also produced differences but in a fewer number of studies (Canullo et al. 2010, 2011a, Pieri et al. 2011, Prosper et al. 2009) and with smaller effect sizes. In the present study, shift was below the margin considered beneficial, ranging from 0.3 to 0.35 mm for the 3.8 and 4.3 mm and for the 5.0 mm implants, respectively. Even though no inferences could be made regarding the effect of implant diameter or horizontal shift dimension, the authors detected a significant effect of PS, increasing from surgery to each of the successive annual evaluations (Fig. 3), with an estimate of 0.39 mm (0.15–0.64, 95% CI) at 36 months. On the one hand these results fairly agree with the 0.45 mm (0.14–0.76, 95% CI) effect estimated by Annibali et al. (2012) for periods of evaluation superior to 1 year, reflecting the long‐term importance of the concept on the preservation of marginal bone levels. On the other hand, the result clearly exceeds the overall estimate for mismatches inferior to 0.45, which is 0.17 mm (0.02–0.32, 95% CI) over different follow‐up periods. Interestingly, this value is somewhat influenced by the single parallel arm multicentre study performed in university clinics (as the present one) reported by Kielbassa et al. (2009) who was unable to detect a positive effect of PS on immediately loaded implants after 1 year. The study was then extended to a longer follow‐up and the results presented after 3 years (Arnhart et al. 2012), yet with no major modifications of the results regarding the PS concept. Actually, all parallel arm designs (as the present report) appear to demote the effect size of PS on marginal bone levels when compared to split‐mouth designs as extrapolated from Annibali et al. (2012) and Chrcanovic et al. (2015) but are less prone to incur in type I errors (incorrect rejection of the null hypothesis) due to the increased number of patients recruited (independent statistical units).
Limitations of the present results are related mostly to the ongoing status of the study, with some dropouts.
Conclusion
Within the limitations of the present study, restorations with platform switching showed a significant effect in the preservation of marginal bone levels over 3 years follow‐up when compared to restorations with platform matching. The relevant 3 years results provide clinicians a better long‐term understanding on procedures and choices between PS and PM abutments within the same implant system.
Clinical Relevance.
Scientific rationale for the study: Prevention of continuous marginal bone level resorption has been one of the major challenges in implant dentistry. Some studies point to a positive contribution of the platform‐switching concept, but the literature is sparse on randomized clinical trials with limited confounders and adequate follow‐up.
Principal findings: From surgery to 3 years, the platform‐switching group was able to preserve proximal bone 0.39 mm higher than the platform‐matching group. From loading onwards, bone gain was statistically associated with the platform‐switching implants.
Practical implications: After 3 years, platform switching confidently preserves bone around adjacent implants, contributing for the long‐term success of the treatment.
Supporting information
Figure S1. CONSORT flow diagram of the study design.
Table S1. Distribution of the implants placed in each group by diameter and length at the 36 months appointment.
Acknowledgements
The authors would like to thank Françoise Peters, Alex Schäar and Peter Thommen from the Camlog Foundation for their organizational support.
Rocha S, Wagner W, Wiltfang J, Nicolau P, Moergel M, Messias A, Behrens E, Guerra F. Effect of platform switching on crestal bone levels around implants in the posterior mandible: 3 years results from a multicentre randomized clinical trial. J Clin Periodontol 2016; 43: 374–382. doi: 10.1111/jcpe.12522.
Conflict of interest and source of funding statement
The authors declare that they have no conflict of interests related to this study.
This study was funded by an unrestricted grant of the Camlog Foundation, Basel, Switzerland. Prof. F. Guerra and Prof. W. Wagner are members of the Camlog Foundation Board.
References
- Albrektsson, T. , Buser, D. & Sennerby, L. (2012) Crestal bone loss and oral implants. Clinical Implant Dentistry and Related Research 14, 783–791. [DOI] [PubMed] [Google Scholar]
- Albrektsson, T. O. , Johansson, C. B. & Sennerby, L. (1994) Biological aspects of implant dentistry: osseointegration. Periodontology 2000 4, 58–73. [DOI] [PubMed] [Google Scholar]
- Albrektsson, T. , Zarb, G. , Worthington, P. & Eriksson, A. R. (1986) The long‐term efficacy of currently used dental implants: a review and proposed criteria of success. International Journal of Oral & Maxillofacial Implants 1, 11–25. [PubMed] [Google Scholar]
- Al‐Nsour, M. M. , Chan, H. L. & Wang, H. L. (2012) Effect of the platform‐switching technique on preservation of peri‐implant marginal bone: a systematic review. International Journal of Oral & Maxillofacial Implants 27, 138–145. [PubMed] [Google Scholar]
- Annibali, S. , Bignozzi, I. , Cristalli, M. P. , Graziani, F. , La Monaca, G. & Polimeni, A. (2012) Peri‐implant marginal bone level: a systematic review and meta‐analysis of studies comparing platform switching versus conventionally restored implants. Journal of Clinical Periodontology 39, 1097–1113. [DOI] [PubMed] [Google Scholar]
- Arnhart, C. , Kielbassa, A. M. , Martinez‐de Fuentes, R. , Goldstein, M. , Jackowski, J. , Lorenzoni, M. , Maiorana, C. , Mericske‐Stern, R. , Pozzi, A. , Rompen, E. , Sanz, M. & Strub, J. R. (2012) Comparison of variable‐thread tapered implant designs to a standard tapered implant design after immediate loading. A 3‐year multicentre randomised controlled trial. European Journal of Oral Implantology 5, 123–136. [PubMed] [Google Scholar]
- Atieh, M. A. , Ibrahim, H. M. & Atieh, A. H. (2010) Platform switching for marginal bone preservation around dental implants: a systematic review and meta‐analysis. Journal of Periodontology 81, 1350–1366. [DOI] [PubMed] [Google Scholar]
- Berglundh, T. & Lindhe, J. (1996) Dimension of the periimplant mucosa. Biological width revisited. Journal of Clinical Periodontology 23, 971–973. [DOI] [PubMed] [Google Scholar]
- Berglundh, T. , Persson, L. & Klinge, B. (2002) A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. Journal of Clinical Periodontology 29(Suppl. 3), 197–212; discussion 232‐193. [DOI] [PubMed] [Google Scholar]
- Buser, D. , Ingimarsson, S. , Dula, K. , Lussi, A. , Hirt, H. P. & Belser, U. C. (2002) Long‐term stability of osseointegrated implants in augmented bone: a 5‐year prospective study in partially edentulous patients. International Journal of Periodontics and Restorative Dentistry 22, 109–117. [PubMed] [Google Scholar]
- Cairo, F. , Sanz, I. , Matesanz, P. , Nieri, M. & Pagliaro, U. (2012) Quality of reporting of randomized clinical trials in implant dentistry. A systematic review on critical aspects in design, outcome assessment and clinical relevance. Journal of Clinical Periodontology 39(Suppl. 12), 81–107. [DOI] [PubMed] [Google Scholar]
- Canullo, L. , Fedele, G. R. , Iannello, G. & Jepsen, S. (2010) Platform switching and marginal bone‐level alterations: the results of a randomized‐controlled trial. Clinical Oral Implants Research 21, 115–121. [DOI] [PubMed] [Google Scholar]
- Canullo, L. , Goglia, G. , Iurlaro, G. & Iannello, G. (2009) Short‐term bone level observations associated with platform switching in immediately placed and restored single maxillary implants: a preliminary report. International Journal of Prosthodontics 22, 277–282. [PubMed] [Google Scholar]
- Canullo, L. , Iannello, G. & Gotz, W. (2011a) The influence of individual bone patterns on peri‐implant bone loss: preliminary report from a 3‐year randomized clinical and histologic trial in patients treated with implants restored with matching‐diameter abutments or the platform‐switching concept. International Journal of Oral & Maxillofacial Implants 26, 618–630. [PubMed] [Google Scholar]
- Canullo, L. , Iannello, G. , Penarocha, M. & Garcia, B. (2012) Impact of implant diameter on bone level changes around platform switched implants: preliminary results of 18 months follow‐up a prospective randomized match‐paired controlled trial. Clinical Oral Implants Research 23, 1142–1146. [DOI] [PubMed] [Google Scholar]
- Canullo, L. , Pace, F. , Coelho, P. , Sciubba, E. & Vozza, I. (2011b) The influence of platform switching on the biomechanical aspects of the implant‐abutment system. A three dimensional finite element study. Medicina Oral, Patologia Oral y Cirugia Bucal 16, e852–e856. [DOI] [PubMed] [Google Scholar]
- Canullo, L. , Pellegrini, G. , Allievi, C. , Trombelli, L. , Annibali, S. & Dellavia, C. (2011c) Soft tissues around long‐term platform switching implant restorations: a histological human evaluation. Preliminary results. Journal of Clinical Periodontology 38, 86–94. [DOI] [PubMed] [Google Scholar]
- Cassetta, M. , Pranno, N. , Calasso, S. , Di Mambro, A. & Giansanti, M. (2015) Early peri‐implant bone loss: a prospective cohort study. International Journal of Oral and Maxillofacial Surgery 44, 1138–1145. [DOI] [PubMed] [Google Scholar]
- Chang, C. L. , Chen, C. S. & Hsu, M. L. (2010) Biomechanical effect of platform switching in implant dentistry: a three‐dimensional finite element analysis. International Journal of Oral & Maxillofacial Implants 25, 295–304. [PubMed] [Google Scholar]
- Choquet, V. , Hermans, M. , Adriaenssens, P. , Daelemans, P. , Tarnow, D. P. & Malevez, C. (2001) Clinical and radiographic evaluation of the papilla level adjacent to single‐tooth dental implants. A retrospective study in the maxillary anterior region. Journal of Periodontology 72, 1364–1371. [DOI] [PubMed] [Google Scholar]
- Chrcanovic, B. R. , Albrektsson, T. & Wennerberg, A. (2015) Platform switch and dental implants: a meta‐analysis. Journal of Dentistry 43, 629–646. [DOI] [PubMed] [Google Scholar]
- Cochran, D. L. , Bosshardt, D. D. , Grize, L. , Higginbottom, F. L. , Jones, A. A. , Jung, R. E. , Wieland, M. & Dard, M. (2009a) Bone response to loaded implants with non‐matching implant‐abutment diameters in the canine mandible. Journal of Periodontology 80, 609–617. [DOI] [PubMed] [Google Scholar]
- Cochran, D. L. , Nummikoski, P. V. , Schoolfield, J. D. , Jones, A. A. & Oates, T. W. (2009b) A prospective multicenter 5‐year radiographic evaluation of crestal bone levels over time in 596 dental implants placed in 192 patients. Journal of Periodontology 80, 725–733. [DOI] [PubMed] [Google Scholar]
- De Smet, E. , Jacobs, R. , Gijbels, F. & Naert, I. (2002) The accuracy and reliability of radiographic methods for the assessment of marginal bone level around oral implants. Dentomaxillofacial Radiology 31, 176–181. [DOI] [PubMed] [Google Scholar]
- Donati, M. , La Scala, V. , Di Raimondo, R. , Speroni, S. , Testi, M. & Berglundh, T. (2015) Marginal bone preservation in single‐tooth replacement: a 5‐year prospective clinical multicenter study. Clinical Implant Dentistry and Related Research 17, 425–434. [DOI] [PubMed] [Google Scholar]
- Esposito, M. , Coulthard, P. , Worthington, H. V. & Jokstad, A. (2001) Quality assessment of randomized controlled trials of oral implants. International Journal of Oral & Maxillofacial Implants 16, 783–792. [PubMed] [Google Scholar]
- Fickl, S. , Zuhr, O. , Stein, J. M. & Hurzeler, M. B. (2010) Peri‐implant bone level around implants with platform‐switched abutments. International Journal of Oral & Maxillofacial Implants 25, 577–581. [PubMed] [Google Scholar]
- Guerra, F. , Wagner, W. , Wiltfang, J. , Rocha, S. , Moergel, M. , Behrens, E. & Nicolau, P. (2014) Platform switch versus platform match in the posterior mandible: 1‐year results of a multicentre randomized clinical trial. Journal of Clinical Periodontology 41, 521–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermann, J. S. , Buser, D. , Schenk, R. K. , Higginbottom, F. L. & Cochran, D. L. (2000) Biologic width around titanium implants. A physiologically formed and stable dimension over time. Clinical Oral Implants Research 11, 1–11. [DOI] [PubMed] [Google Scholar]
- Hermann, J. S. , Buser, D. , Schenk, R. K. , Schoolfield, J. D. & Cochran, D. L. (2001) Biologic width around one‐ and two‐piece titanium implants. Clinical Oral Implants Research 12, 559–571. [DOI] [PubMed] [Google Scholar]
- Hurzeler, M. , Fickl, S. , Zuhr, O. & Wachtel, H. C. (2007) Peri‐implant bone level around implants with platform‐switched abutments: preliminary data from a prospective study. Journal of Oral and Maxillofacial Surgery 65, 33–39. [DOI] [PubMed] [Google Scholar]
- Kielbassa, A. M. , Martinez‐de Fuentes, R. , Goldstein, M. , Arnhart, C. , Barlattani, A. , Jackowski, J. , Knauf, M. , Lorenzoni, M. , Maiorana, C. , Mericske‐Stern, R. , Rompen, E. & Sanz, M. (2009) Randomized controlled trial comparing a variable‐thread novel tapered and a standard tapered implant: interim one‐year results. Journal of Prosthetic Dentistry 101, 293–305. [DOI] [PubMed] [Google Scholar]
- Lang, N. P. , Jepsen, S. & Working, G. (2009) Implant surfaces and design (Working Group 4). Clinical Oral Implants Research 20 (Suppl. 4), 228–231. [DOI] [PubMed] [Google Scholar]
- Laurell, L. & Lundgren, D. (2011) Marginal bone level changes at dental implants after 5 years in function: a meta‐analysis. Clinical Implant Dentistry and Related Research 13, 19–28. [DOI] [PubMed] [Google Scholar]
- Lazzara, R. J. & Porter, S. S. (2006) Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. International Journal of Periodontics and Restorative Dentistry 26, 9–17. [PubMed] [Google Scholar]
- Luongo, R. , Traini, T. , Guidone, P. C. , Bianco, G. , Cocchetto, R. & Celletti, R. (2008) Hard and soft tissue responses to the platform‐switching technique. International Journal of Periodontics and Restorative Dentistry 28, 551–557. [PubMed] [Google Scholar]
- Maeda, Y. , Miura, J. , Taki, I. & Sogo, M. (2007) Biomechanical analysis on platform switching: is there any biomechanical rationale? Clinical Oral Implants Research 18, 581–584. [DOI] [PubMed] [Google Scholar]
- Messias, A. , Tondela, J. P. , Rocha, S. , Reis, R. , Nicolau, P. & Guerra, F. (2013) Acrylic customized X‐ray positioning stent for prospective bone level analysis in long‐term clinical implant studies. Open Journal of Radiology 03, 136–142. [Google Scholar]
- Moergel, M. , Rocha, S. , Messias, A. , Nicolau, P. , Guerra, F. & Wagner, W. (2015) Radiographic evaluation of conical tapered platform‐switched implants in the posterior mandible: 1‐year results of a two‐center prospective study. Clinical Oral Implants Research 00, 1–8. doi:10.1111/clr.12644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxby, G. , Oxby, F. , Oxby, J. , Saltvik, T. & Nilsson, P. (2015) Early loading of fluoridated implants placed in fresh extraction sockets and healed bone: a 3‐ to 5‐year clinical and radiographic follow‐up study of 39 consecutive patients. Clinical Implant Dentistry and Related Research 17, 898–907. [DOI] [PubMed] [Google Scholar]
- Pessoa, R. S. , Bezerra, F. J. , Sousa, R. M. , Vander Sloten, J. , Casati, M. Z. & Jaecques, S. V. (2014) Biomechanical evaluation of platform switching: different mismatch sizes, connection types, and implant protocols. Journal of Periodontology 85, 1161–1171. [DOI] [PubMed] [Google Scholar]
- Pessoa, R. S. , Vaz, L. G. , Marcantonio, E. Jr , Vander Sloten, J. , Duyck, J. & Jaecques, S. V. (2010) Biomechanical evaluation of platform switching in different implant protocols: computed tomography‐based three‐dimensional finite element analysis. International Journal of Oral & Maxillofacial Implants 25, 911–919. [PubMed] [Google Scholar]
- Pieri, F. , Aldini, N. N. , Marchetti, C. & Corinaldesi, G. (2011) Influence of implant‐abutment interface design on bone and soft tissue levels around immediately placed and restored single‐tooth implants: a randomized controlled clinical trial. International Journal of Oral & Maxillofacial Implants 26, 169–178. [PubMed] [Google Scholar]
- Prosper, L. , Redaelli, S. , Pasi, M. , Zarone, F. , Radaelli, G. & Gherlone, E. F. (2009) A randomized prospective multicenter trial evaluating the platform‐switching technique for the prevention of postrestorative crestal bone loss. International Journal of Oral & Maxillofacial Implants 24, 299–308. [PubMed] [Google Scholar]
- Schropp, L. , Stavropoulos, A. , Spin‐Neto, R. & Wenzel, A. (2012) Implant image quality in dental radiographs recorded using a customized imaging guide or a standard film holder. Clinical Oral Implants Research 23, 55–59. [DOI] [PubMed] [Google Scholar]
- Schrotenboer, J. , Tsao, Y. P. , Kinariwala, V. & Wang, H. L. (2008) Effect of microthreads and platform switching on crestal bone stress levels: a finite element analysis. Journal of Periodontology 79, 2166–2172. [DOI] [PubMed] [Google Scholar]
- Schulze, R. K. & d'Hoedt, B. (2001) Mathematical analysis of projection errors in “paralleling technique” with respect to implant geometry. Clinical Oral Implants Research 12, 364–371. [DOI] [PubMed] [Google Scholar]
- Sculean, A. , Gruber, R. & Bosshardt, D. D. (2014) Soft tissue wound healing around teeth and dental implants. Journal of Clinical Periodontology 41 (Suppl. 15), S6–S22. [DOI] [PubMed] [Google Scholar]
- Smith, D. E. & Zarb, G. A. (1989) Criteria for success of osseointegrated endosseous implants. Journal of Prosthetic Dentistry 62, 567–572. [DOI] [PubMed] [Google Scholar]
- Strietzel, F. P. , Neumann, K. & Hertel, M. (2014) Impact of platform switching on marginal peri‐implant bone‐level changes. A systematic review and meta‐analysis. Clinical Oral Implants Research 26, 342–358. doi: 10.1111/clr.12339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabata, L. F. , Rocha, E. P. , Barao, V. A. & Assuncao, W. G. (2011) Platform switching: biomechanical evaluation using three‐dimensional finite element analysis. International Journal of Oral & Maxillofacial Implants 26, 482–491. [PubMed] [Google Scholar]
- Tarnow, D. , Elian, N. , Fletcher, P. , Froum, S. , Magner, A. , Cho, S. C. , Salama, M. , Salama, H. & Garber, D. A. (2003) Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. Journal of Periodontology 74, 1785–1788. [DOI] [PubMed] [Google Scholar]
- Tarnow, D. P. , Magner, A. W. & Fletcher, P. (1992) The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. Journal of Periodontology 63, 995–996. [DOI] [PubMed] [Google Scholar]
- Vigolo, P. & Givani, A. (2009) Platform‐switched restorations on wide‐diameter implants: a 5‐year clinical prospective study. International Journal of Oral & Maxillofacial Implants 24, 103–109. [PubMed] [Google Scholar]
- Wang, Y. C. , Kan, J. Y. , Rungcharassaeng, K. , Roe, P. & Lozada, J. L. (2015) Marginal bone response of implants with platform switching and non‐platform switching abutments in posterior healed sites: a 1‐year prospective study. Clinical Oral Implants Research 26, 220–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. CONSORT flow diagram of the study design.
Table S1. Distribution of the implants placed in each group by diameter and length at the 36 months appointment.


