Abstract
Introduction
Acinetobacter baumannii (A.baumannii) is rapidly emerging as a potent organism causing a multitude of nosocomial infections. The organism also carries various resistance mechanisms to antibiotics, making treatment more difficult. Very few choices are left, as A.baumannii strains have begun to develop resistance against cephalosporins, aminoglycosides and even carbapenems.
Aim
To examine the sensitivity pattern of three older antibiotics namely colistin, polymyxin B and rifampicin against carbapenem resistant A.baumannii by disk diffusion method and the sensitivity of colistin alone by Minimum Inhibitory Concentration (MIC) determination by VITEK automated system.
Materials and Methods
Hundred clinical isolates of carbapenem resistant A. baumannii were tested for sensitivity to colistin, polymyxin B and rifampicin by Kirby-Bauer disk diffusion method. They were also tested for sensitivity to colistin by VITEK 2C (biomérieux) automated microbial identification system. The zone diameters and Minimum Inhibitory Concentration values for the above two methods, respectively were observed and analysed. All the Antibiotic Susceptibility Tests were done according to the CLSI guidelines.
Results
By Kirby-Bauer disk diffusion method, 78% of the carbapenem resistant strains were found to be sensitive, 12% intermediate sensitive and 10% resistant to colistin. All the isolates were sensitive to polymyxin B and 80% were resistant to rifampicin. By the VITEK automated system, 99% of the isolates were sensitive to colistin (more in number than by disk diffusion method).
Conclusion
Polymyxins (colistin - polymyxin E and polymyxin B) are the next choice for multidrug resistant serious nosocomial infections like those of A. baumannii, till newer antibiotics are discovered to treat such infections. Rifampicin resistance was found to be very high and hence, is not advised for monotherapy.
Keywords: Carbapenemase, Disk diffusion test, Nosocomial infections
Introduction
Acinetobacter baumannii is emerging to be one of the most dreaded organisms in the hospital setting, especially in the Intensive Care Units, where it has accounted for outbreaks among the most vulnerable and critically ill patients, commonly affecting those on long term ventilator support [1]. The drug resistant nature of this organism and its unusual and unpredictable susceptibility patterns has made treatment of A. baumannii infections more difficult than before [2].
A.baumannii stain Gram negative and are oxidase negative, non-motile, cocco bacilli that produce pale lactose fermenting colonies on MacConkey agar [3].
Initially, A.baumannii infections were treated like any other Gram negative organism, with cephalosporins and aminoglycosides. But they were quick to develop resistance to these groups of drugs [4]. Then came carbapenems like meropenem and imipenem; carbapenem resistant A.baumannii infections are also on the rise now. With no new antibiotics in the past few years, treatment of such infections has become limited [5]. Clinicians now resort to older antibiotics such as the polymyxin group.
Polymyxins include colistin (polymyxin E) and polymyxin B (the rest being too toxic for human use) [6]. They were popular in the 1970s, after which their use declined due to the advent of better antibiotics [7]. In recent years, colistin is again attracting considerable interest as a potent antibiotic against many multi drug resistant pathogens [7].
Rifampicin has also been found to have activity against certain strains of A.baumannii and is a favourite choice for synergy or combination therapy with polymyxins [8].
This study examines the sensitivity patterns of colistin, polymyxin B and rifampicin against carbapenem resistant Acinetobacter baumannii. Also, it identifies the sensitivity pattern of colistin by two methods and compares the results thus obtained.
Materials and Methods
A cross-sectional pilot study was conducted that included 100 clinical isolates of carbapenem resistant A.baumannii, screened from an initial sample size of 20,282 samples received in the microbiology laboratory of PSG Hospitals, Coimbatore, Tamil Nadu, over a period of 9 months (from March 2014 to November 2014). The isolates were from specimens like tracheal aspirate, endotracheal tube tip, sputum, broncho alveolar lavage fluid, blood, ascitic fluid and wound swabs. The cases include inpatients of various wards – the Medical Intensive Care Units of General Medicine, Pulmonology, Nephrology, Gastroenterology, Neurology, wards of Neurosurgery, Trauma, Medicine, Surgery, Nephrology, Neurology, Gastroenterology and special wards. Only those A. baumannii strains that were carbapenem resistant were included in this study. Approval was obtained from the Institutional Human Ethics Committee to carry out this study.
Isolation and Identification
A.baumannii was first isolated from the specimens, after incubation at 37°C in blood agar and MacConkey agar, after microscopy (Gram negative cocco bacilli on Gram staining). They were then confirmed by biochemical tests [9] – catalase positive, oxidase negative, carbohydrate fermentation (glucose fermenter, lactose fermenter, sucrose non-fermenter, mannitol non-fermenter and non motile), citrate positive, urease positive and growth at 44°C positive.
The carbapenemase producing (carbapenem resistant) strains were then identified by Kirby-Bauer disk diffusion method [10], using meropenem disks of 10mcg, according to the norms of CLSI guidelines [11].
Antimicrobial Sensitivity Testing
These strains were then inoculated on the surface of a Mueller-Hinton agar plate from a fresh preparation of 0.5 McFarland suspension. Three antibiotic disks namely colistin (10mcg), polymyxin B (300 U) and rifampicin (5mcg), purchased from HiMedia Laboratories, Mumbai, were incorporated into the media. After incubation for 24 hours, by Kirby-Bauer disk diffusion method [10], the zone diameters were measured and categorized as sensitive, intermediate sensitive or resistant based on the breakpoints obtained from various sources [Table/Fig-1] [12–15].
[Table/Fig-1]:
| Zone Diameters of | Sensitive | Intermediate Sensitive | Resistant |
|---|---|---|---|
| Colistin* | ≥14 mm | 13 mm | ≤12 mm |
| Polymyxin B† | ≥12 mm | - | ≤11 mm |
| Rifampicin‡ | ≥20 mm | 17-19 mm | ≤16 mm |
* Galani et al [12] † Andrea L Kwa, Vincent H Tam, Matthew E Falagas [13] considering the breakpoints of Pseudomonas aeruginosa as Thomson JM, Bonomo RA [14] find resistance patterns between the two organisms similar. ‡ Thapa B, Tribuddharat C, Rugdeekha S, Techachaiwiwat W, Srifuengfung S, Dhiraputra C [15] considering the breakpoints of Staphlococcus aureus
Simultaneously, a suspension of 2-3 colonies from a pure culture was made (145μL) of 0.5 McFarland standard to which 3 mL of saline was added, followed by broth dilution. This was then subjected to VITEK 2C (bioMérieux) automated microbial identification system, making use of a Gram negative susceptibility card AST-N281. The MIC values for colistin were observed according to the breakpoints [Table/Fig-2] [11,12]. The above mentioned antibiotic susceptibility tests were all done according to the CLSI guidelines [11].
[Table/Fig-2]:
| Parameter | Sensitive | Intermediate Sensitive | Resistant |
|---|---|---|---|
| Zone Diameters by Kirby- Bauer’s Disk Diffusion method § |
≥14 mm | 13 mm | ≤12 mm |
| MIC values by VITEK automated systems|| |
≤2 μg/mL | - | ≥4 μg/mL |
Results
A 95% of the carbapenem resistant A.baumannii were from respiratory samples and the maximum number were isolated from tracheal aspirates (65%) [Table/Fig-3]. Majority of the samples were from Medical Intensive Care Units, Trauma and Neurosurgery wards following close behind [Table/Fig-4].
[Table/Fig-3]:
![[Table/Fig-3]:](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/06b5/5071932/8aa973fdce35/jcdr-10-DC15-g001.jpg)
Specimens for isolation.
[Table/Fig-4]:
Ward wise distribution of samples.
 | |
| Ward Wise Distribution of Samples | Number of Clinical Samples (n) |
| MICU – Medical Intensive Care Unit - Medicine | 26 |
| MICU – Pulmonology | 6 |
| MICU – Neurology | 2 |
| MICU – Gastroenterology | 4 |
| MICU - Nephrology | 2 |
| Neurosurgery/ Trauma ward | 16 |
| Medicine and Surgery wards | 4 |
| Pulmonology ward | 8 |
| Neurology ward | 4 |
| Gastroenterology ward | 4 |
| Miscellaneous (namely special wards) | 24 |
*MICU – Medical Intensive Care Unit
Numerical values
Following the breakpoints [Table/Fig-1], it was found that 78% of the organisms were sensitive to colistin and all of them (100%) were sensitive to polymyxin B. rifampicin resistance was seen in 80% of the organisms [Table/Fig-5].
[Table/Fig-5]:
Susceptibility of all 3 antibiotics by disk diffusion.
| No. of isolates | Sensitive | Intermediate Sensitive | Resistant |
|---|---|---|---|
| Colistin* | 78 | 12 | 10 |
| Polymyxin B† | 100 | - | - |
| Rifampicin‡ | 12 | 8 | 80 |
VITEK reported 99% to be sensitive, whereas only 78% turned out to be sensitive by disk diffusion method [Table/Fig-6].
[Table/Fig-6]:
Colistin susceptibilty observed by both methods.
| No. of Isolates | Sensitive | Intermediate Sensitive | Resistant |
|---|---|---|---|
| By Kirby-Bauer’s Disk Diffusion method§ |
78 | 12 | 10 |
| MIC Determination by VITEK automated systems|| |
99 | - | 1 |
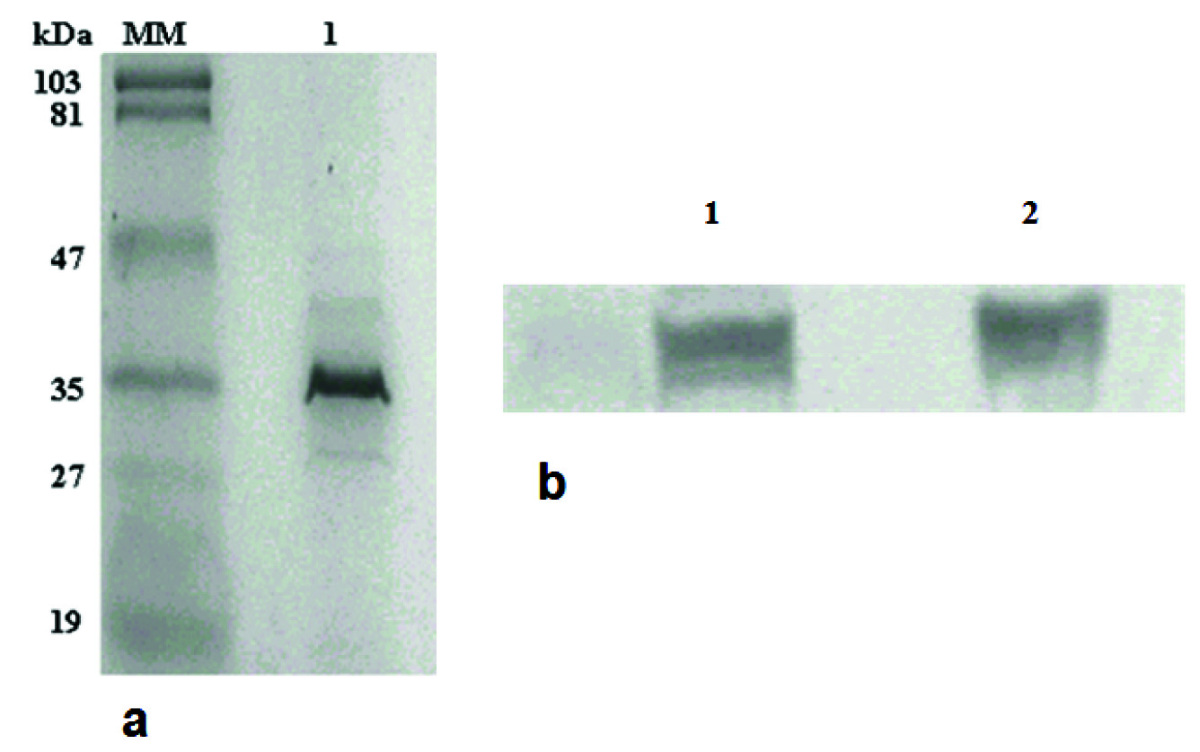
The comparison of sensitivity and resistance to colistin by the two methods – Kirby-Bauer disk diffusion method and MIC determination by VITEK shows that 90 isolates were sensitive to colistin by both the methods [Table/Fig-7].
[Table/Fig-7]:
![[Table/Fig-7]:](https://cdn.ncbi.nlm.nih.gov/pmc/blobs/06b5/5071932/8de844ca4076/jcdr-10-DC15-g003.jpg)
Comparison of results by disk diffusion and MIC determination by VITEK for colistin.
 No. of isolates sensitive to colistin by both methods
No. of isolates sensitive to colistin by both methods
 No. of isolates sensitive to colistin by disk diffusion but resistant by VITEK
No. of isolates sensitive to colistin by disk diffusion but resistant by VITEK
 No. of isolates sensitive to colistin by VITEK but resistant by disk diffusion
No. of isolates sensitive to colistin by VITEK but resistant by disk diffusion
 No. of isolates resistant to colistin by both methods
No. of isolates resistant to colistin by both methods
However, the 9 isolates that showed resistance by disk diffusion and sensitivity by VITEK had zone diameters in the range of 10-12 mm in the disk diffusion method. (≤12 mm – colistin resistant).
Discussion
A.baumannii, commonly known for causing ventilator associated pneumonia, blood stream infections, urinary tract infections and wound infections, is becoming difficult to treat with the limited options available. Also, it is one of the most easily transmitted pathogen by health care workers [16]. Carbapenem resistance is being increasingly reported, necessitating their detection at the earliest [17].
This study observed a remarkably high susceptibility rate of carbapenem resistant A.baumannii isolates to polymyxins. Hence, we infer that older antibiotics like colistin and polymyxin B could be used to treat multidrug resistant infections.
A study in New Delhi, India showed 96.4% sensitivity to polymyxin B in A.baumannii [18]. Another Indian study showed 100% sensitivity to both colistin and polymyxin B [19]. Only 1.6% of the A.baumannii isolates showed resistance to colistin and polymyxin B in a study based in Korea [20]. Studies from the west and Middle East also observed a similar trend, a 100% susceptibility to colistin and polymyxin B was reported [21].
However, invitro activities of colistin vary from its invivo actions [4,22]. Clinical efficacy of colistin has limited data because of low number of patients, study design, varying dosage regimens, differences in susceptibility testing methods and inaccurate pharmacokinetic knowledge of colistimethate sodium [23,24]. A study of the West shows 57-77% cure rate with colistin in patients with A.baumannii infections [24]. Another study from Greece reports 93% cure rate with colistin in MDR A. baumannii CNS infections [25].
This study showed a high rate of rifampicin resistance by carbapenem resistant A.baumannii. Similarly, a study from Spain showed development of high level of rifampicin resistance Invitro when used in monotherapy against carbapenem resistant A. baumannii [26].
There is an increased need for reliable susceptibility testing methods to predict the clinical response. Our study showed a slight discrepancy in the results obtained by disk diffusion and automated VITEK. It shows that there could be chances of missing out on colistin sensitive organisms in smaller set ups where only disk diffusion is carried out (since the automated VITEK is considered superior) [27]. The lack of consensus regarding breakpoints for resistance between Clinical and Laboratory Standard Institute (CLSI), British Society for Antimicrobial Chemotherapy (BSAC) and Société Française de Microbiologie (SFM) has resulted in varied interpretation of the sensitivity patterns [18]. This also brings about lacunae in studies done on this group of antimicrobials. A study based in Boston calls for the need to confirm disk diffusion methods of colistin by determining MIC values to eliminate falsely susceptible and resistant organisms [27]. A European based study emphasizes on the reliability of VITEK automated method results over the routine disk diffusion method in antibiotic susceptibility testing [28].
Then arises the question of efficacy of monotherapy. As the drug concentration of colistin decreases in the body, there is re-growth of the surviving bacteria with a higher MIC [29]. Combination therapy with rifampicin for both colistin and polymyxin B has given much better results than monotherapy [4,30].
Limitation
The invivo action of polymyxins cannot be expected to be the same as the invitro activities thus seen, because of their pharmacokinetics. More studies in the future will be required to establish the same.
Conclusion
This study shows a good number of carbapenem resistant A.baumannii to be sensitive to polymyxins – namely colistin and polymyxin B. Hence, they ought to be considered as the next drug of choice for carbapenem resistant strains. The study also shows rifampicin resistance to be high and hence is not advised for monotherapy. There are also substantial differences between the two methods of antibiotic susceptibility tests – disk diffusion and MIC determination by VITEK automated systems.
Financial or Other Competing Interests
None.
References
- [1].Kongsonae K, Naenna P, Dhiraputra C, Leelarasamee A, Pongpech P. Invitro antimicrobial activity of colistin in combination with rifampicin against carbapenem-resistant Acinetobacter baumanni. J Infect Dis Antimicrob Agents. 2012;29(3):121–33. [Google Scholar]
- [2].Fishbain J, Peleg AY. Treatment of Acinetobacter infections. Clin Infect Dis. 2010;51(1):79–84. doi: 10.1086/653120. [DOI] [PubMed] [Google Scholar]
- [3].Peleg AY, Seifert H, Paterson DL. Acinetobacter baumannii: Emergence of a successful pathogen. Clin Microbiol Rev. 2008;21:538–82. doi: 10.1128/CMR.00058-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Howard A, O’Donoghue M, Feeney A, Sleator RD. Acinetobacter baumannii An emerging opportunistic pathogen. Virulence. 2012;3:243–50. doi: 10.4161/viru.19700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Jaggi N, Sissodia P, Sharma L. Acinetobacter baumannii isolates in a tertiary care hospital: Antimicrobial resistance and clinical significance. Journal of Microbiology and Infectious Disease. 2012;2(2):57–63. [Google Scholar]
- [6].Balaji V, Jeremiah SS, Baliga PR. Polymyxins: Antimicrobial susceptibility concerns and therapeutic options. Indian J Med Microbiol. 2011;29(3):230–42. doi: 10.4103/0255-0857.83905. [DOI] [PubMed] [Google Scholar]
- [7].Biswas S, Brunel JM, Dubus JC, Reynaud-Gaubert M, Rolain JM. Colistin: An update on the antibiotic of the 21st century. Expert Rev Anti Infect Ther. 2012;10(8):917–34. doi: 10.1586/eri.12.78. [DOI] [PubMed] [Google Scholar]
- [8].Petrosillo N, Chinello P, Proietti MF, Cecchini L, Masala M, Ranchi CF, et al. Combined colistin and rifampicin therapy for carbapenem-resistant Acinetobacter baumannii infections: clinical outcome and adverse events. Clin Microbiol Infect. 2005;11(8):682–83. doi: 10.1111/j.1469-0691.2005.01198.x. [DOI] [PubMed] [Google Scholar]
- [9].Mahon CR, Lehman DC, Manuselis G. Textbook of Diagnostic Microbiology. 4th edition. Philadelphia: Saunders Elsevier; 2011. pp. 488–89. [Google Scholar]
- [10].Bauer AW, Kirby WM, Sherris JC, Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966;45:493–96. [PubMed] [Google Scholar]
- [11].Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. 2014;M100-S24(34):64–65. [Google Scholar]
- [12].Galani I, Kontopidou F, Souli M, Rekatsina PD, Koratzanis E, Deliolanis J, et al. Colistin susceptibility testing by Etest and disc diffusion methods. Int J Antimicrob Agents. 2008;31:434–39. doi: 10.1016/j.ijantimicag.2008.01.011. [DOI] [PubMed] [Google Scholar]
- [13].Kwa AL, Tam VH, Falagas ME. Polymyxins: A review of the current status including recent developments. Ann Acad Med Singapore. 2008;37:870–83. [PubMed] [Google Scholar]
- [14].Thomson JM, Bonomo RA. The threat of antibiotic resistance in Gram-negative pathogenic bacteria: beta-lactams in peril! Curr Opin Microbiol. 2005;8(5):518–24. doi: 10.1016/j.mib.2005.08.014. [DOI] [PubMed] [Google Scholar]
- [15].Thapa B, Tribuddharat C, Rugdeekha S, Techachaiwiwat W, Srifuengfung S, Dhiraputra C. Rifampin resistance in carbapenem-resistant Acinetobacter baumannii in Siriraj Hospital, Thailand. Nepal Med Coll J. 2009;11(4):232–37. [PubMed] [Google Scholar]
- [16]. Louisiana Office of Public Health – Infectious Disease Epidemiology Section (Internet), 2nd March 2008. Available from http://www.infectiousdisease.louisiana.dhh.gov.
- [17].Mahajan G, Sheemar S, Chopra S, Kaur J, Chowdhary D, Makhija SK. Carbapenem resistance and phenotypic detection of carbapenemases in clinical isolates of Acinetobacter baumannii. Indian J Med Sci. 2011;65(1):18–25. [PubMed] [Google Scholar]
- [18].Behera B, Mathur P, Das A, Kapil A, Gupta B, Bhoi S, et al. Evaluation of susceptibility testing methods for polymyxin. Int J Infect Dis. 2009;996:e1–6. doi: 10.1016/j.ijid.2009.09.001. [DOI] [PubMed] [Google Scholar]
- [19].Bhose S, Barapatre, Ghosh AK. Emergence of Multidrug Resistant Acinetobacter baumannii in an ICU. Natl J Integr Res Med. 2013;4(2):11–14. [Google Scholar]
- [20].Ko KS, Suh J, Kwon KT, Jung SI, Park KH, Kang KI, et al. High rates of resistance to colistin and polymyxin B in subgroups of Acinetobacter baumannii isolates from Korea. J Antimicrob Chemother. 2007;60:1163–67. doi: 10.1093/jac/dkm305. [DOI] [PubMed] [Google Scholar]
- [21].Peerayeh SN, Karmostaji A, Sarasiabi S, Javadpour S, Davoodian P, Moradi N. Invitro activity of tigecycline and colistin against clinical isolates of acinetobacter baumannii in Hospitals in Tehran and Bandar-Abbas, Iran. Electron Physician. 2014;6(3):919–24. doi: 10.14661/2014.919-924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Li J, Turnidge J, Milne R, Nation RL, Coulthard K. Invitro pharmacodynamic properties of colistin and colistin methanesulfonate against pseudomonas aeruginosa isolates from patients with cystic fibrosis. Antimicrob Agents Chemother. 2001;45:781–85. doi: 10.1128/AAC.45.3.781-785.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Yahav D, Farbman L, Leibovici V, Paul M. Colistin: new lessons on an old antibiotic. Clin Microbiol Infect. 2012;18:18–29. doi: 10.1111/j.1469-0691.2011.03734.x. [DOI] [PubMed] [Google Scholar]
- [24].Maragakis L, Perl TM. Acinetobacter baumannii: Epidemiolgy, antimicrobial resistance and treatment options. Clin Infect Dis. 2008;46:1254–63. doi: 10.1086/529198. [DOI] [PubMed] [Google Scholar]
- [25].Katragkou A, Roilides E. Successful treatment of multidrug-resistant acinetobacter baumannii central nervous system infections with colistin. J Clin Microbiol. 2005;43(9):4916–17. doi: 10.1128/JCM.43.9.4916-4917.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Michalopoulos AS, Falagas ME. Colistin: recent data on pharmacodynamics properties and clinical efficacy in critically ill patients. Ann Intensive Care. 2011;1:30. doi: 10.1186/2110-5820-1-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Saballs M, Pujol, Tubau F e C, Montero A, Dominguez MA, et al. Rifampicin/imipenem combination in the treatment of carbapenem-resistant Acinetobacter baumannii infections. J Antimicrob Chemother. 2006;58:697–700. doi: 10.1093/jac/dkl274. [DOI] [PubMed] [Google Scholar]
- [28].Falagas ME, Kasiakou SK. Colistin: The revival of polymyxins for the management of multidrug-resistant gram-negative bacterial infections. Clinical Infectious Disease. 2005;40:1333–41. doi: 10.1086/429323. [DOI] [PubMed] [Google Scholar]
- [29].Lo-Ten-Foe J, de Smet AMGA, Diederen BMW, Kluytmans JAJW, van Keulen PHJ. Comparative evaluation of the VITEK 2, disk diffusion, etest, broth microdilution, and Agar Dilution Susceptibility testing methods for colistin in clinical isolates, including heteroresistant enterobacter cloacae and acinetobacter baumannii strains. Antimicrob Agents Chemother. 2007;51:3726–30. doi: 10.1128/AAC.01406-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Lim TP, Tan TY, Lee W, Sasikala S, Tan TT, Hsu LY, Kwa AL. Invitro activity of polymyxin b, rifampicin, tigecycline alone and in combination against carbapenem-resistant acinetobacter baumannii in Singapore. PLoS One. 2011;6(4):e184–85. doi: 10.1371/journal.pone.0018485. [DOI] [PMC free article] [PubMed] [Google Scholar]


