Abstract
Background
Dural arteriovenous fistula of the anterior condylar confluence (ACC-DAVF) is a rare subtype of DAVFs that occurs around the hypoglossal canal. Transvenous embolization (TVE) with coils has been performed for most ACC-DAVFs with a high clinical cure rate. However, some reports call attention to hypoglossal nerve palsy associated with TVE due to coil mass compression of the hypoglossal nerve caused by coil deviation from the ACC to the anterior condylar vein (ACV). Herein, we report a case of ACC-DAVF in which an intraoperative cone-beam computed tomography (CT) contributed to avoiding hypoglossal nerve palsy.
Case presentation
A 74-year-old man presented with left pulse-synchronous tinnitus. An angiography detected left ACC-DAVF mainly supplied by the left ascending pharyngeal artery and mainly drained through the ACV. The two fistulous points were medial side of the ACC and the venous pouch just cranial of the ACC. We performed TVE detecting the fistulous points by contralateral external carotid angiography (ECAG). The diseased venous pouch and ACC were packed with seven coils but a slight remnant of the DAVF was recognized. Because a cone-beam CT revealed that the coil mass was localized in the lateral lower clivus osseous without deviation to the hypoglossal canal, we finished TVE to avoid hypoglossal nerve palsy. Postoperatively, no complication was observed. No recurrence of symptoms or imaging findings were detected during a five-month follow-up period.
Conclusion
An intraoperative cone-beam CT contributed to avoiding hypoglossal nerve palsy by estimating the relationship between the coil mass and the hypoglossal canal during TVE of ACC-DAVF.
Keywords: Anterior condylar confluence, cone-beam computed tomography, dural arteriovenous fistula, hypoglossal nerve palsy, transvenous embolization
Introduction
The anterior condylar confluence (ACC) is a small venous structure, 5 mm in maximal diameter, which is located at the extracranial aperture of the hypoglossal canal at the skull base with a rich venous network.1 Since Ernst et al. first reported in 1999 dural arteriovenous fistulas of the anterior condylar confluence (ACC-DAVFs) or of the hypoglossal canal (HC-DAVFs) as a rare subtype of DAVFs that occur around the hypoglossal canal, case reports of ACC-DAVFs have accumulated that the incidence is considered to be 3.4%–5.1% of all DAVFs.2–6 While most ACC-DAVFs present with pulse-synchronous tinnitus (75%) or orbital symptoms (30.8%), few present with hypoglossal nerve palsy (11.7%).7
Transvenous embolization (TVE) with coils has been performed for most ACC-DAVFs with a high clinical cure rate (91%) and low morbidity (2.9%).7 However, some reports call attention to hypoglossal nerve palsy associated with TVE due to coil mass compression of the hypoglossal nerve caused by coil deviation from the ACC to the anterior condylar vein (ACV), a channel of the ACC passing the hypoglossal canal.8 To avoid hypoglossal nerve palsy associated with TVE, the following techniques are recommended: to embolize the ACC selectively, to use the softest coils inside the hypoglossal canal, not to overpack the ACV, and to use an intraoperative cone-beam computed tomography (CT) to confirm the position of the catheter tip and the hypoglossal canal.5,8,9
Herein, we report a case of ACC-DAVF in which an intraoperative cone-beam CT contributed to avoiding hypoglossal nerve palsy by estimating the relationship between the coil mass and the hypoglossal canal.
Case presentation
A 74-year-old man with no history of traumatic injury presented with left pulse-synchronous tinnitus and occasional left epiphora. The symptom persisted for three months and the patient was referred to our department. CT and magnetic resonance imaging (MRI) showed no abnormal findings. MR angiography revealed high intensity around the left hypoglossal canal (Figure 1(a), (b)). A left external carotid angiography (ECAG) showed left ACC-DAVF mainly supplied by the left ascending pharyngeal artery (APA). Although the ACV showed as a main drainer, the ipsilateral angiography failed to reveal the fistulous points because of overlapping of vessels (Figure 2(a), (b)). Then a right, contralateral, ECAG was performed (Figure 2(c), (d)). The right APA and maxillary artery were flowing into the ACC and the venous pouch just cranial of the ACC. The two fistulous points were medial side of the ACC and the venous pouch. Fistulous points were not evident on the lateral side of the ACC. The ACC was drained caudally through the ACV and the lateral condylar vein (LCV) to the vertebral venous plexus (VVP), laterally to the internal jugular vein (IJV), and cranially slightly to the inferior petrosal sinus (IPS). Left vertebral angiography was also performed and showed the anterior meningeal artery flowing into the ACC.
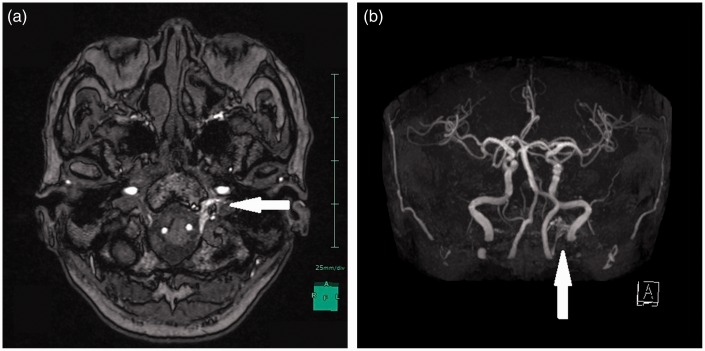
Figure 1.
Images on admission: ((a), (b)) Time-of-flight MRA source image and MRA showing high intensity around the left hypoglossal canal (white arrow).
MRA: magnetic resonance angiography; MRI: magnetic resonance imaging.
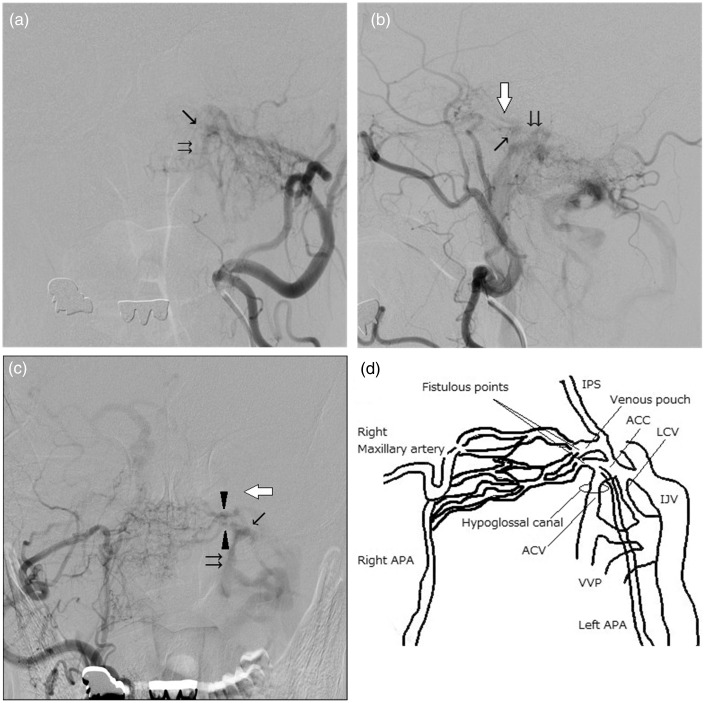
Figure 2.
Preoperative angiographic studies: ((a), (b)) A left ECAG showing left ACC-DAVF ((a) anterior-posterior view. (b) lateral view). The ACC (arrow) was mainly supplied by the left APA. Although the ACV (double arrow) showed as a main drainer, the ipsilateral angiography failed to reveal the fistulous points because of overlapping of vessels. (c) A right, contralateral, ECAG of the anterior-posterior view showing the right APA and maxillary artery flowing into the ACC and the venous pouch just cranial of the ACC. The two fistulous points (arrow head) were medial side of the ACC and the venous pouch. The ACC was drained caudally through the ACV and LCV to VVP, laterally to the IJV, and cranially slightly to the IPS (white arrow). (d) A schematic drawing of the anterior-posterior view of the feeding arteries, fistulous points, draining veins, and hypoglossal canal.
ACC: anterior condylar confluence; ACV: anterior condylar vein; APA: ascending pharyngeal artery; DAVF: dural arteriovenous fistula; ECAG: external carotid angiography; IJV: internal jugular vein; IPS: inferior petrosal sinus; LCV: lateral condylar vein; VVP: vertebral venous plexus.
We performed TVE under local anesthesia. A bolus infusion of 3000 IU heparin was given to control activated clotting time from 200 to 250 seconds. Four-F catheters (Medikit, Tokyo, Japan) were placed into the right external carotid artery and the left common carotid artery to visualize the DAVF and the venous route, respectively. A 5-F STR/4-F JB2 Chaperone guiding catheter (Terumo, Tokyo, Japan) was placed into the left IJV and the 4-F JB2, as a distal access catheter, was placed into the ACC. An Excelsior SL-10 microcatheter (Striker, Kalamazoo, MI, USA) was placed into the venous pouch just cranial of the ACC using a NEUROUTE 0.014-inch microguidewire (Hirata, Osaka, Japan).
The venous pouch was embolized with Target 360 SOFT 5 mm*10 cm (Striker) and Target 360 ULTRA 4 mm*8 cm (Figure 3(a)). Then, the Excelsior SL-10 was pushed out to the ACC and embolization continued from the medial fistulous point of the ACC (Figure 3(b)). The ACC was embolized with Target HELICAL ULTRA 3 mm*6 cm × 2, Orbit Galaxy COMPLEX FILL 6 mm*15 cm (Johnson & Johnson, New Brunswick, NJ, USA) × 2, and Axium 3D 3 mm*8 cm (Covidien, Dublin, Ireland); seven coils, total length: 68 cm.
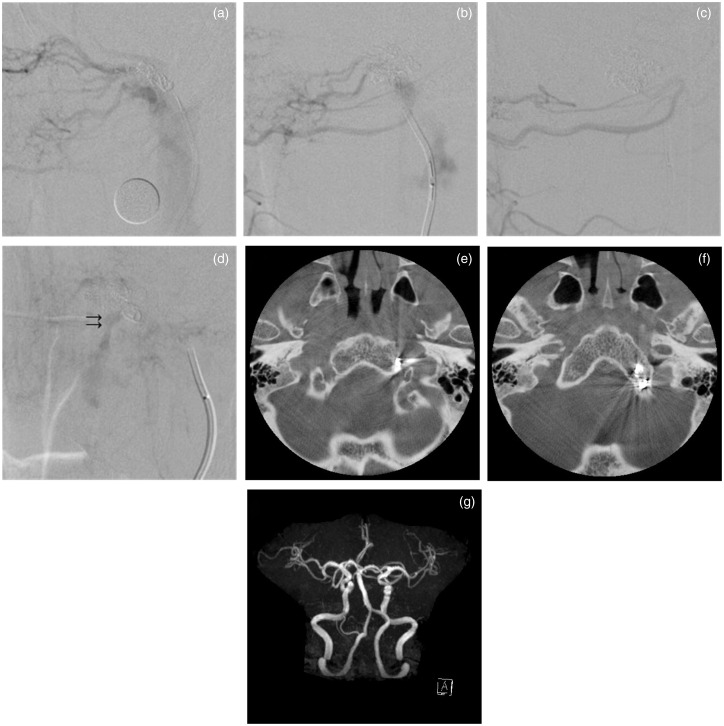
Figure 3.
Intraoperative findings during TVE. (a) A right ECAG showing the venous pouch, which was embolized with two coils, total length: 18 cm. The Excelsior SL-10 microcatheter was pushed out from the venous pouch to the ACC. (b) A sequential right ECAG showing the ACC, which was embolized with five coils, total length: 50 cm. (c) A right ECAG not visualizing the ACC-DAVF. (d) A left CCAG showing a slight remnant of the DAVF (double arrow). ((e), (f)) A cone beam CT showing that the coil mass was localized in the lateral lower clivus osseous without deviation to the hypoglossal canal. (g) Postoperative MRA five months after TVE not visualizing high intensity around the left hypoglossal canal.
ACC: anterior condylar confluence; CCAG: common carotid artery angiography; CT: computed tomography; DAVF: dural arteriovenous fistula; ECAG: external carotid artery angiography; MRA: magnetic resonance angiography; TVE: transvenous embolization.
A right ECAG did not visualize the ACC-DAVF, but a left common carotid angiography (CCAG) revealed a slight remnant of the DAVF (Figure 3(c), (d)). Because a cone-beam CT revealed that the coil mass was localized in the lateral lower clivus osseous without deviation to the hypoglossal canal, we finished TVE to avoid hypoglossal nerve palsy (Figure 3(e), (f)).
Postoperatively, no complication was observed. The patient’s symptoms and the high intensity around the left hypoglossal canal vanished during a five-month follow-up period (Figure 3(g)).
Discussion
Since ACC-DAVF was first reported by Ernst et al. in 1999, case reports have been increasing and the findings have accumulated so that the incidence is considered to be 3.4%–5.1% of all DAVFs.2–6 Spittau et al. performed systematic literature review of 120 cases (113 published cases and their seven cases) and proposed the following three subtypes:7 Type 1 (62.5%), dominant anterograde venous drainage to the IJV and/or the VVP with or without reflux to the transverse, sigmoid, cavernous sinus (CS), or IPS; Type 2 (23.3%), dominant retrograde drainage to the CS and/or orbital veins with or without anterograde drainage to the IJV and/or VVP or cortical venous reflux; and Type 3 (14.2%), dominant or exclusive venous drainage to cerebellar pial or perimedullary veins. Although pulse-synchronous tinnitus is frequent in Type 1 and 2 (92% and 75%, respectively), orbital symptoms are characteristic in Type 2 (100%) and myelopathy and intracerebral hemorrhage are characteristic in Type 3 (64.7% and 35.3%, respectively). Hypoglossal nerve palsy is rather rare and restricted to Type 1 (18.7%). While angiography is required for diagnosis and classification of subtypes, MR angiography is useful for screening.2,10 Because Type 2 and 3 tend to be published because of their atypical features, typical Type 1 may be more frequent than the systematic review estimated.7,11
The ACC communicates not only caudally to the ACV, LCV, IJV and VVP, but also cranially to the IPS and CS through Trolard’s inferior petrooccipital vein and occasionally through the basilar plexus.1 Therefore, it is important during TVE of ACC-DAVFs to detect the fistulous point and to perform selective embolization of the cranial part of the diseased sinus. In the present case, the ACC was drained slightly to the IPS, and we embolized the venous pouch just cranial of the ACC. Because the candidate for the fistulous point of ACC-DAVFs is not only the ACC but also the ACV or IPS, placement of the coils in an inappropriate site causes venous drainage pattern change and venous hypertension worsening.5,8 Contralateral ECAG, superselective microcatheter angiography, and three-dimensional rotational angiography are useful to detect the fistulous point.2,10 A double-catheter technique is reported as a rescue to occlude the cranial channels communicating to the IPS and CS.7 Although a TAE is adapted to residual flow after TVE, the neuromeningeal branch of APA causes the IX–XII nerve palsy.12
Hypoglossal nerve palsy associated with TVE should be avoided in ACC-DAVFs. The incidence of hypoglossal nerve palsy ranges from 0% to 33% in previous reports, though in the maximum case series, Hsu et al reported, sequential 14 cases of ACC-DAVF were performed TVE without hypoglossal nerve palsy (Table 1).4,7–9,13–15 Because overpacking the ACV is considered the cause of hypoglossal nerve palsy, it is emphasized to embolize the ACC selectively, to use the softest coils inside the hypoglossal canal, and not to overpack the ACV.5,8,9 Although neurological findings may be useful during embolization, especially under local anesthesia, Manabe et al. reported a case of postoperative sudden hypoglossal nerve palsy five days after embolization due to overpacking of the ACV.13 Anatomical location of coils should be evaluated carefully to prevent hypoglossal nerve palsy. In the present case, a cone-beam CT revealed no coil deviation to the hypoglossal canal, and we finished TVE to avoid hypoglossal nerve palsy. Similarly, Miyachi et al. used an intraoperative cone-beam CT to confirm the position of the catheter tip and the hypoglossal canal.8 A cone-beam CT should be performed before detaching the coils when tight packing of the ACC or coil deviation to the ACV is suspected to avoid the situation in which coils have already been packed in the hypoglossal canal. An intraoperative cone-beam CT contributes to avoiding hypoglossal nerve palsy by showing not only the position of the catheter tip and the hypoglossal canal but also the relationship between the coil mass and the hypoglossal canal.
Table 1.
Reported hypoglossal nerve palsy associated with TVE of ACC-DAVFs.
| First author | Incidence rate | Procedure | Duration of XII palsy | Proposed cause | |
|---|---|---|---|---|---|
| McDougall14 | (1997) | ND | TVE with coils | ND | ND |
| Manabe13 | (2008) | 33% (1/3) | TVE with coils + TAE | Prolonged | Overpacking of the ACV |
| Miyachi8 | (2008) | 25% (2/8) | TVE with coils + TAE | Prolonged/Transient | Overpacking of the ACV |
| Kuwayama4 | (2011) | 9.3% (4/43) | TVE with coils | ND | ND |
| Takemoto15 | (2014) | 33% (1/3) | TVE with Onyx | Transient | Neurotoxity or retrograde arterial embolization of Onyx |
| Spittau7 | (2015) | ND (One case) | TVE | ND | Overpacking of the ACV |
ACC-DAVF: dural arteriovenous fistula of the anterior condylar confluence; ACV: anterior condylar vein; ND: not described; TAE: transarterial embolization; TVE: transvenous embolization; XII: hypoglossal nerve.
Conclusions
We reported a case of ACC-DAVF. A TVE was performed detecting the fistulous points by contralateral ECAG. An intraoperative cone-beam CT contributed to avoiding hypoglossal nerve palsy by estimating the relationship between the coil mass and the hypoglossal canal.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.San Millán Ruíz D, Gailloud P, Rüfenacht DA, et al. The craniocervical venous system in relation to cerebral venous drainage. AJNR Am J Neuroradiol 2002; 23: 1500–1508. [PMC free article] [PubMed] [Google Scholar]
- 2.Ernst R, Bulas R, Tomsick T, et al. Three cases of dural arteriovenous fistula of the anterior condylar vein within the hypoglossal canal. AJNR Am J Neuroradiol 1999; 20: 2016–2020. [PMC free article] [PubMed] [Google Scholar]
- 3.Hiramatsu M, Sugiu K, Hishikawa T, et al. Epidemiology of dural arteriovenous fistula in Japan: Analysis of Japanese Registry of Neuroendovascular Therapy (JR-NET2). Neurol Med Chir (Tokyo) 2014; 54: 63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuwayama N, Kubo M, Endo S, et al. Present status in the treatment of dural arteriovenous fistulas in Japan. Jpn J Neurosurg (Tokyo) 2011; 20: 12–19. [Google Scholar]
- 5.Okahara M, Kiyosue H, Tanoue S, et al. Selective transvenous embolization of dural arteriovenous fistulas involving the hypoglossal canal. Interv Neuroradiol 2007; 13: 59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh V, Smith WS, Lawton MT, et al. Risk factors for hemorrhagic presentation in patients with dural arteriovenous fistulae. Neurosurgery 2008; 62: 628–635. [DOI] [PubMed] [Google Scholar]
- 7.Spittau B, Millán DS, El-Sherifi S, et al. Dural arteriovenous fistulas of the hypoglossal canal: Systematic review on imaging anatomy, clinical findings, and endovascular management. J Neurosurg 2015; 122: 883–903. [DOI] [PubMed] [Google Scholar]
- 8.Miyachi S, Ohshima T, Izumi T, et al. Dural arteriovenous fistula at the anterior condylar confluence. Interv Neuroradiol 2008; 14: 303–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsu YH, Lee CW, Liu HM, et al. Endovascular treatment and computed imaging follow-up of 14 anterior condylar dural arteriovenous fistulas. Interv Neuroradiol 2014; 20: 368–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abiko M, Ikawa F, Ohbayashi N, et al. Endovascular treatment for dural arteriovenous fistula of the anterior condylar confluence involving the anterior condylar vein. A report of two cases. Interv Neuroradiol 2008; 14: 313–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kiyosue H, Tanoue S, Okahara M, et al. Ocular symptoms associated with a dural arteriovenous fistula involving the hypoglossal canal: Selective transvenous coil embolization. Case report. J Neurosurg 2001; 94: 630–632. [DOI] [PubMed] [Google Scholar]
- 12.Pei W, Huai-Zhang S, Shan-Cai X, et al. Isolated hypoglossal nerve palsy due to endovascular treatment of a dural arteriovenous fistula with Onyx-18. Interv Neuroradiol 2010; 16: 286–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Manabe S, Satoh K, Matsubara S, et al. Characteristics, diagnosis and treatment of hypoglossal canal dural arteriovenous fistula: Report of nine cases. Neuroradiology 2008; 50: 715–721. [DOI] [PubMed] [Google Scholar]
- 14.McDougall CG, Halbach VV, Dowd CF, et al. Dural arteriovenous fistulas of the marginal sinus. AJNR Am J Neuroradiol 1997; 18: 1565–1572. [PMC free article] [PubMed] [Google Scholar]
- 15.Takemoto K, Tateshima S, Rastogi S, et al. Onyx embolization of anterior condylar confluence dural arteriovenous fistula. J Neurointerv Surg 2014; 6: e13. [DOI] [PubMed] [Google Scholar]