Mesenteric lymphadenopathy is a rare manifestation of Gaucher disease (GD) with only 26 cases reported worldwide and its outcome remains largely unknown. In this manuscript, we described a 17-year-old girl with GD who has been treated with standard enzyme replacement therapy (ERT) for 16 years. The follow-up of her mesenteric lymphadenopathy began 13 years ago, which is one of the longest follow-up for this condition worldwide.
The patient had been definitively diagnosed with GD at the age of 1 year based on the identification of Gaucher cells in her bone marrow and decreased leukocyte β-glucosidase activity. Abdominal ultrasonography at that time revealed hepatosplenomegaly but no lymphadenopathy. Standard ERT had been initiated immediately and maintained since then, and no manifestations had recurred. Ultrasonography revealed asymptomatic abdominal lymph nodes (LNs) as large as 3 cm in diameter at the root of the mesentery when the patient was 4 years of age. After that, the routine follow-up showed increment in the size, number, and calcification of LNs. Two months before, the patient was presented with mild edema of both ankles, without other discomforts. On physical examination, a large, lobulated and hard mass was palpated in the right lower quadrant, and mild edema appeared in both ankles. Routine blood examinations showed serum albumin of 29.6 g/L (35–45 g/L) and were otherwise normal. Tuberculin test was negative. Abdominal computed tomography (CT) confirmed a large mass of LN origin at the root of the mesentery, with 7.7 cm × 10.2 cm × 8.5 cm in size. Large patches of calcification were detected inside and around the large LN. Multiple LNs, with or without calcification, were also detected at the root of the mesentery [Figure 1]. The superior mesenteric vessels were encased by the large LN; the vein was nearly occluded whereas the artery was not obviously stenosed. Obvious edema of the intestinal walls was noticed. The major veins that drain the lower limbs were not affected. Resection or biopsy was not performed due to the explicit clinical diagnosis and the high risks of surgery. Six months later, the edema disappeared without medication while abdominal CT showed no obvious changes.
Figure 1.
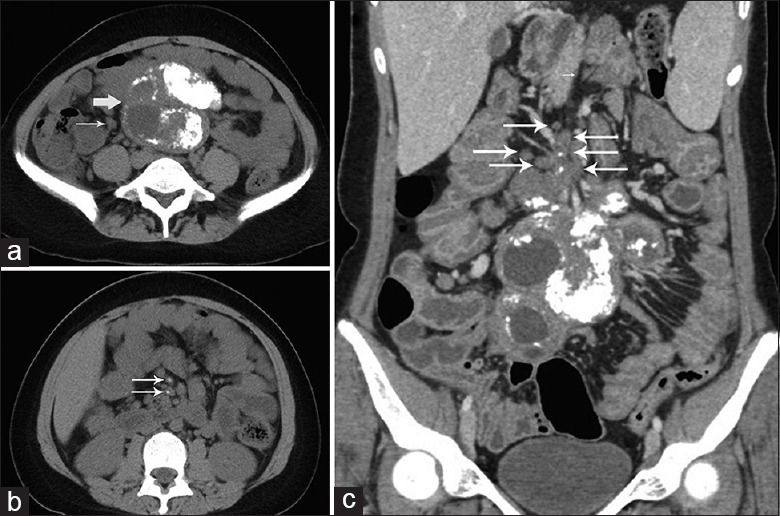
Both large (thick white arrow) and small (thin white arrows) mesenteric lymph nodes are calcified, and the lymph nodes are fused. (a) Large lymph nodes are fused with each other. Certain lymph nodes exhibit cystic degeneration and are surrounded by flecks of calcifications whereas other lymph nodes are partially or largely calcified, and certain small mesenteric lymph nodes exhibit no calcification. (b) Calcification is observed within multiple small mesenteric lymph nodes. (c) Multiple small lymph nodes are located at the outskirts of the large lymph node and tend to fuse with it.
Mesenteric lymphadenopathy is a rare manifestation of GD. Abdelwahab et al.[1] reported the largest cohort so far, including eight cases of GD with lymphadenopathy. Three of them underwent a LN biopsy, which revealed no malignancy but infiltration of Gaucher cells, which were confirmed in all other reports. This indicates that mesenteric lymphadenopathy is likely a benign complication of GD. Misdiagnosis as a malignant tumor and incorrect treatment can be avoided with increased recognition of this rare manifestation. Among all reported cases, surgical resection of enlarged LNs in GD was attempted in only three patients and has never been completed due to high risks.[1,2,3] Thus, the indications for resection should be carefully evaluated. We suggest that surgical intervention should be considered only when malignancy is suspected or when severe space-occupying effects are observed. More cases and a longer follow-up are required to further investigate the outcomes of this condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Peng Lyu
References
- 1.Abdelwahab M, SeifEldien HM. Mesenteric and mediastinal lymphadenopathy in Egyptian children with gaucher disease types 1 and 3 treated with enzyme replacement therapy. J Pediatr Hematol Oncol. 2015;37:e316–22. doi: 10.1097/MPH.0000000000000297. doi: 10.1097/mph.0000000000000297. [DOI] [PubMed] [Google Scholar]
- 2.Burrow TA, Cohen MB, Bokulic R, Deutsch G, Choudhary A, Falcone RA, Jr, et al. Gaucher disease: Progressive mesenteric and mediastinal lymphadenopathy despite enzyme therapy. J Pediatr. 2007;150:202–6. doi: 10.1016/j.jpeds.2006.10.062. doi: 10.1016/j.jpeds.2006.10.062. [DOI] [PubMed] [Google Scholar]
- 3.Lee BH, Kim DY, Kim GH, Cho KJ, Yoon HK, Yoo HW. Progressive mesenteric lymphadenopathy with protein-losing enteropathy;a devastating complication in Gaucher disease. Mol Genet Metab. 2012;105:522–4. doi: 10.1016/j.ymgme.2011.12.010. doi: 10.1016/j.ymgme.2011.12.010. [DOI] [PubMed] [Google Scholar]


