Abstract
Objectives:
Technological advances in healthcare have shown promise when delivering interventions for mental health problems such as psychosis. The aim of this project is to develop a mobile phone intervention for people with psychosis and to conduct a feasibility study of the TechCare App.
Methods:
The TechCare App will assess participant’s symptoms and respond with a personalised guided self-help-based psychological intervention with the aim of exploring feasibility and acceptability. The project will recruit 16 service users and 8–10 health professionals from the Lancashire Care NHS Foundation Trust Early Intervention Service.
Results:
In strand 1 of the study, we will invite people to discuss their experience of psychosis and give their opinions on the existing evidence-based treatment (cognitive behavioural therapy) and how the mobile app can be developed. In strand 2, we will complete a test run with a small number of participants (n = 4) to refine the mobile intervention (TechCare). Finally, in strand 3 of the study, the TechCare App will be examined in a feasibility study with 12 participants.
Conclusion:
It has been suggested that there is a need for a rapid increase in the efforts to develop the evidence base for the clinical effectiveness of digital technologies, considering mHealth research can potentially be helpful in addressing the demand on mental health services globally.
Keywords: Early intervention in psychosis, mHealth, cognitive behavioural therapy, intelligent real-time therapy
Background
Mental illness is a major source of disease burden in the United Kingdom, costing in the region of £105 billion pounds.1 Psychosis is a severe form of mental illness that has huge social, economic and personal costs.2 The disorder has the highest prevalence in the young population between 15 and 35 years of age.3 Individuals who experience psychosis may encounter a number of symptoms such as perceptual phenomena, including auditory hallucinations and delusional ideation or other disturbances in thinking.4 At later stages of the disorder, there may be a marked deterioration in an individual’s functioning.5
The UK National Health Service (NHS England) Improving Access to Psychological Therapies for Severe Mental Illness (IAPT-SMI) initiative aims to increase the availability of psychological interventions.6 Despite such initiatives, access to psychological treatments is low, with individuals experiencing a psychotic illness being less likely to be offered psychological interventions.7 One way of tackling this poor access to treatment is through the use of mobile and wireless technologies, which have the potential to transform mental healthcare. Globally, estimates suggest close to 5 billion mobile phone subscriptions worldwide,8 with over 85% of the world’s population being covered by a commercial wireless signal.8 In the United Kingdom, it is estimated that 93% of adults own/use a mobile phone, with 66% owning a smartphone.9
The emergence and continual development of technology in this era cannot be ignored, both socially, professionally, and personally technology encroaches upon all of our daily lives. Telehealth and mobile health (mHealth) are emerging fields in providing treatment and care globally.10–13 It involves the use of telecommunications to provide healthcare, support and interventions from a distance.14–16 Telehealth has been implemented into the treatment of chronic physical illnesses including diabetes, congestive heart failure and asthma.16,17 Barak et al.18 found Internet-based interventions to be more successful for the treatment of psychological problems than for physical or medical problems. Using technology to advance psychological treatment is ‘a developing professional reality’.18
A study by Lester et al.19 showed the importance of technology in engagement within Early Intervention Services (EIS). This is important in drawing emphasis on how mHealth functions could provide continued support, but also give clients greater autonomy. Rotondi et al.20 found that for many clients, just having the access to support at their fingertips when needed was sufficient reassurance for them.
However, due to the current and developing nature of digital health technologies, these have faced criticism, such as the lack of interpersonal closeness when compared to face-to-face intervention delivery. It has been reported that clients using a face-to-face intervention compared with an online chat overall felt more satisfied, a better sense of closeness and more comfortable in disclosing their difficulties.21,22 These criticisms are important to address, as each of these factors play key roles in contributing to a therapeutic relationship,23 which has been highlighted as important in delivering efficacious treatment and encouraging engagement.19 However, in contrast, a meta-analysis of research on Internet-based psychotherapeutic interventions found it to be as efficacious as face-to-face therapy in the treatment of certain mental health difficulties such as depression, anxiety and post-traumatic stress disorder.18 This shows that in many cases, the effectiveness of the therapy is not diminished. Barak et al.18 found cognitive behavioural therapy (CBT) a much more effective therapy than others for online treatment of psychological difficulties. Furthermore, a systematic review by Alvarez-Jimenez et al.24 found that mobile- and Internet-based interventions for psychosis were feasible and acceptable and have the potential to improve health outcomes.
A number of studies have shown support for the use of mHealth in severe mental illness.10,11,13,25 Palmier-Claus et al.11 reported that overall, 67% of participants preferred using a smartphone app compared to 13% who preferred Short Message Service (SMS) and 21% who had no preference on the delivery method. Furthermore, Granholm et al.10 reported that participants increased their level of socialisation, and there was also a reduction in severity of hallucinatory behaviour when using a low-level SMS-based intervention. The key findings of these studies were the feasibility and acceptability of mHealth Apps for Severe Mental Illnesses (SMIs) and the ability of mHealth technology to overcome barriers to accessing mental health treatment through the use of a non-stigmatising approach. Moreover, mHealth interventions as reported by Palmier-Claus et al.,11 Granholm et al.,10 and Ben-Zeev et al.13 are acceptable forms of intervention and thus provide a unique and beneficial platform for engagement.
mHealth innovations are important as they have the potential to bridge the ‘therapy-practice gap’,26 going beyond the confines of the therapy setting and bringing real-time treatment in individual’s day-to-day lives and within their lived environments. The potential benefits of digital technologies in providing a new way to connect with health services and to potentially improve health outcomes are limited by a number of barriers in their use. Hollis et al.27 summarised these barriers as the insufficient evidence base, limited uptake and outcomes being anecdotal and unpublished. Hollis et al.27 further stated that for the potential of digital technologies to be fully realised, patients’ requirements need to be at the centre of developing interventions, and that there is a need for a rapid increase in the efforts to develop the evidence base for the clinical effectiveness of digital technologies.27
This project aims to integrate a momentary sampling assessment approach that is matched with a psychological intervention in real time to address low mood and paranoia. This proposal describes a feasibility project ‘Mobile Assessment and Therapy for Psychosis’ which is an integrated mobile application which is provisionally titled ‘TechCare’. Guidance regarding the development of new complex interventions suggests that it is appropriate to conduct a phase II or feasibility study.28 This study will follow guidance by the National Institute of Health Research29 on feasibility study design. Feasibility studies are conducted prior to conducting large studies in order to assess whether the study can be done. Vital parameters are examined that are needed to design the main study. The results of this feasibility study will inform the design of subsequent trials regarding expected treatment effects, identification of appropriate outcome measures and follow-up periods, estimates of recruitment and feasibility of the intervention.
Aims and objectives
The proposed study aims to address the following questions:
Can appropriate individuals be identified and recruited to a trial for the evaluation of TechCare for psychosis?
Will TechCare be an acceptable intervention for individuals with psychosis? Will they be able to engage in setting goals and reporting outcomes with care coordinators and work towards these with the TechCare App?
What would be the most appropriate primary outcome measure for a future randomised controlled trial (RCT) of the TechCare intervention?
Methods
Design
We will use a mixed-methods design, which will consist of both qualitative and quantitative components. The study will be run across three strands as follows: (1) qualitative work, (2) test run and intervention refinement and (3) feasibility trial.
Inclusion criteria
The following inclusion criteria will be used:
The service user is receiving care from the Lancashire EIS.
The service users between 18 and 35 years of age.
There has been no change in the medication for at least 2 months prior to entry into the study.
Clients must be currently stable; Lancashire Early Intervention Team uses a traffic light system to indicate current symptomatology and risks of each client. Therefore, the clients who are considered to be stable according to this system will be eligible.
A score of 3 or more on any of the positive symptoms on the Positive and Negative Syndrome Scale (PANSS) (e.g. delusions, hallucination).
Minimum score of 1 on the Calgary Depression Scale.
Exclusion criteria
We will exclude patients meeting the following criteria:
Drug induced psychosis as determined by the individual’s care team.
An acquired brain injury or learning disability as determined by participant’s care team.
Clients who are undergoing assessment, not formally diagnosed and accepted into the service.
Lacking capacity for informed consent determined by the participant’s care team.
Recruitment
The research team will contact potential referrers (care coordinators, clinical psychologists and psychiatrists) at the Lancashire EIS service. They will be provided with information about the study and will be asked to share this with potential participants. In addition, information sessions will be offered by the research teams at the recruitment sites. If participants are interested and wish to be approached to receive further information about the research, a risk assessment will be carried out with the care coordinator. This assessment will then inform the best way to approach participants.
We will also recruit health professionals such as care coordinators, clinical psychologists and EIS doctors from the Lancashire Care EIS and will adopt a purposive sampling strategy seeking to maximise the range of views accessed. We will leave participant information sheets with the clinical teams, so that potential participants can contact the research team directly.
A total of 16 qualitative interviews will be conducted with service users who will take part in strand 2 (test run) and strand 3 (feasibility trial). In addition, we will also carry out two focus groups with 8–10 health professionals (e.g. nurses, psychologists, psychiatrists and social workers). Interviews and focus groups will explore feasibility, acceptability and further development of the TechCare intervention.
Equipment
The TechCare software is being developed for use on a touchscreen mobile phone. The service users who have compatible smartphones will be able to upload the application to their phone. The team will lend a preloaded phone to those who wish to participate but do not have a smartphone. If participants encounter any technical problems with their device, they will be advised to directly contact the research assistant (RA) or the principal investigator (PI).
Defining the intervention
EISs were introduced into the NHS in the early 1990s, for people with a first episode of psychosis.19 Recent research shows that these services are cost-effective in reducing relapse and thus leading to reduction in hospital admissions.30,31 CBT is commonly used for the treatment of early psychosis32 and is a recommended treatment for first episode psychosis (National Institute of Health and Care Excellence (NICE)33). In the Lancashire Care NHS Foundation Trust (LCFT) EIS tier 1 CBT is delivered by all care coordinators who have undertaken the 3-day psychosocial intervention (PSI) training and is at the level of guided self-help interventions. These consist of understanding principles of recovery and hope, basic CBT thought–feeling–behaviour relationship, stress models, techniques for managing mood, goal setting, SMART goals and relapse prevention. The intervention will be informed by the work of Kingdon and Turkington34 on CBT for psychosis. The TechCare intervention will be an add-on to treatment-as-usual (TAU), with the EIS team continuing the routine care of each participant, which involves case management, medical treatment and crisis planning. In addition, the RA will visit the participant on a weekly basis.
Experiential sampling methodology
Experiential sampling methodology (ESM) is a structured methodology, with the capacity to examine the context and natural flow of daily occurrences in people’s lives. This is achieved by the real-time assessments of thoughts, feelings and events which are prompted at regular intervals within a day, typically via an electronic device (e.g. smartphone app). ESM has been used in psychosis with the aim of constructing an understanding of individual’s psychotic symptoms and the aetiological underpinnings of psychosis.35 ESM for psychosis has also been validated by Palmier-Claus et al.,11 which resulted in the development of the ClinTouch smartphone application. The ClinTouch system developed by Palmier-Claus et al.11 is a novel mobile assessment application, which uses ESM technology to assess individual’s symptoms of psychosis. Based on this feasibility work, which reported that the ClinTouch system was safe, feasible and acceptable for individuals with psychosis, the ClinTouch team have furthered this work through the development of ‘CareLoop’ which is a digital clinical system looking at long-term symptom monitoring of SMIs and is guided by qualitative input from service users and health professionals.36 The system prompts service users to respond to a number of structured questions about their symptoms. The key advantage of the system is that the data gathered is recorded in real time on a database, which is useful in monitoring symptoms and potentially allowing for warning signs to be highlighted to the team without delay.
Intelligent real-time therapy
There is a relatively large amount of research which suggests the efficacy of the use of mobile technologies to collect the longitudinal data on individual’s symptoms and views of their illness.37 However, there is little research suggesting the use of mobile devices to deliver psychological interventions.38 One such concept which can be considered is called intelligent real-time therapy (iRTT). This conceptual model outlines the use of mobile technologies to deliver interventions for mental health problems. This system goes beyond the momentary assessment of symptoms, by also providing service users with a remotely delivered psychological intervention such as CBT to help reduce the distress being experienced due to their symptoms.26
The proposed TechCare App will use a combination of ESM and iRTT. The system will also use differing iRTT media formats to convey user-preferred video messages, recordings, text messages, poems and images, providing an interactive interface for service users to engage with and possibly provide better engagement with health professionals.
Strand 1: qualitative component
In-depth interviews. A total of 16 service users who consent to take part in the study will be asked to take part in semi-structured interviews, in order to obtain insight into the experience of the TechCare intervention. The semi-structured interviews with the participants will be digitally recorded and will be transcribed verbatim.
Focus group. We will conduct two focus groups with 8–10 health professionals (e.g. nurses, psychologists, psychiatrists and social workers) who work with service users who experience psychosis. The focus groups will also be digitally recorded and transcribed verbatim. We will look to explore the health professional’s views on the intervention and possible areas which may need to be refined in preparation for strands 2 and 3.
Strand 2: test run and intervention refinement
In this phase, we will conduct a test run of the TechCare intervention which will last for duration of 2 weeks, with a small group of four participants who will be recruited from Lancashire Care EIS. This will allow us to preliminarily test the intervention. We will gather feedback from the participating individuals, therapists and the clinical staff (psychiatrist/care coordinators) on the relevance and acceptability of the TechCare approach. This will inform the further refinement of the intervention to the local context and how best to run the TechCare intervention in the feasibility trial. We will undertake semi-structured, one-to-one interviews with all participants in the test run to obtain their opinions on the intervention, its feasibility, acceptability, impact on their lives and their thoughts about the role of the intervention in reducing symptoms of psychosis. All interviews and focus groups will be carried out by one member of the research team (N.G.); these interviews will be digitally recorded and subsequently transcribed.
The interview schedule will include pre-determined questions (based on findings from strand 1) but will also include open-ended questions to facilitate emergence of new themes. We will investigate the acceptability of the treatment through addressing themes such as participant’s expectations of the intervention, factors associated with therapeutic alliance, its relevance to their psychotic symptoms, problems and social circumstances, their experience of the delivery method, what they found helpful or less helpful and potential changes that could be made to improve their overall experience of the TechCare intervention.
Refinement
The team will collate the quantitative data and qualitative data from this strand and work with the software development team to refine the intervention and delivery of the TechCare intervention.
Strand 3: feasibility trial
A total of 12 service users will be recruited from the Lancashire EIS for the feasibility trial. Each client’s care coordinator will play a key role in the development of individualised tier 1 psychological interventions.
Outcome measures
PANSS (for schizophrenia).39 This is a clinician administered 30-item semi-structured interview which provides balanced representation of positive symptoms and negative symptoms over a 2-week period and gauges their relationship to one another and to global/general psychopathology. The use of PANSS in mHealth interventions has been validated by Palmier-Claus et al.11 through the ClinTouch application.
The Psychotic Symptom Rating Scales (PSYRATS).40 The PSYRATS is a semi-structured interview, measuring dimensions of delusions and hallucinations. The instrument has been validated against the PANSS by Drake et al.41
CHoice of Outcome In Cbt for psychosEs (CHOICE).42 This is an outcome measure which reflects the aims of CBT for psychosis and the priorities of service users. It was developed with service users, and this shortened version is being utilised in the National IAPT for psychosis programme. Lancashire Care EIS is one of two national demonstration sites for the programme in the United Kingdom.
Warwick-Edinburgh Mental Well-Being Scale (WEMWBS).43 The WEMWBS is a measure of mental well-being, which focuses entirely on positive aspects of mental health. It consists of 14 items on one page, is quick to administer and is psychometrically robust.44 It is also a core measure with the IAPT for psychosis project and will measure improvements in positive aspects of mental health, as a result of the TechCare mobile application.
Brief Core Schema Scales (BCSS).45 This is a 24-item measure of core beliefs regarding self and others. Four scores are obtained; negative self, positive self, negative others and positive others. Fowler et al.45 found the BCSS to have good psychometric properties.
Calgary Depression Scale (CDS).46 The CDS was developed to measure the level of depression in schizophrenia. It is a 9-item scale which allows for the quantitative and subjective dimensions of depression in schizophrenia; items are scored on a scale of 0–4 with a minimum score of 0 and maximum score of 27 for an assessment. The CDS is psychometrically robust and has been validated against the Hamilton Depression Scale.47
The Work and Social Adjustment Scale (WSAS).48 This is a 5-item measure of perceived impairment in five areas: work, home management, social life, private leisure and relationships. Each item is scored from 0 (no impairment) to 8 (very severe impairment) with a total score of 40.
EuroQoL-5 Dimensions (EQ5-D). Health-related quality of life will be measured using the EuroQoL-5 Dimensions (EQ-5D);49 the measure is a standardised instrument looking at quality of life across five health domains (mobility, self-care, usual activities, pain/discomfort and anxiety/depression). The measure has been widely used in psychosis research.
TechCare application assessment questions
A range of unusual or paranoid beliefs are reported by individuals with psychosis. The TechCare App will be equipped with a ‘delusions’ and ‘mood’ menu in the setup section (adapted from Palmier-Claus et al.11), where the researcher or case manager can personalise which delusions the participant is currently experiencing based on the initial PANSS interview and other self-report questionnaires. This delusional belief will be the basis for TechCare questions asked and scored for level of preoccupation, distress and impact on behaviour. Up to two personalised delusions can be entered for each person. For those with more, the delusions with greatest conviction and distress rating will be utilised. We will also include items from the Calgary Depression Scale to assess mood. Depending on the threshold of response, the assessment question will trigger the intervention screen for that specific difficulty. The intervention screen will display a list of personalised self-help interventions such as thought–feeling–behaviour relationships, stress models, techniques for managing mood and goal setting, which will be informed by the work of Kingdon and Turkington34 on CBT for psychosis and participant tailored iRTT media (music, images and video clips) (see Figure 1). In this feasibility study, the personalised self-help interventions will be available to participants at all times in response to the symptoms reported. The TechCare self-help intervention is designed only to test the intervention to address symptoms of low mood and paranoia, with all responses made by the participant being recorded in real time through the App. The participants will also be able to access some materials on psychoeducation34 and also some other helpful links, along with the routine EIS treatment which includes a crisis plan.
Figure 1.
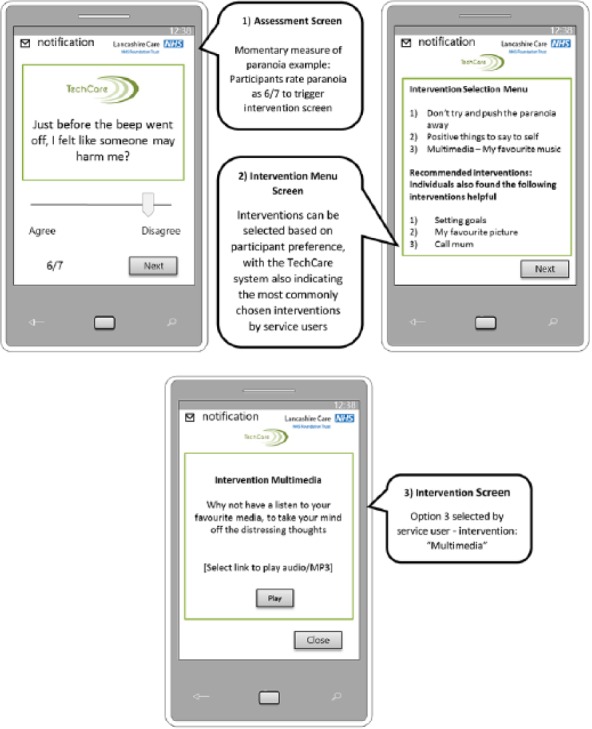
An example of ESM and iRTT in the TechCare App.
The TechCare App ESM and iRTT system will utilise intelligence at two levels:
Intelligently increasing the frequency of assessment notifications if low mood/paranoia is detected. This will be done through feedback loops which monitor symptoms over time, with the deployment of a personalised crisis plan, if prolonged duration of low mood/paranoia is detected (≃4 h).
An intelligent machine learning algorithm which provides interventions in real time based on breach of assessment thresholds and also provides recommendations on the most popular interventions. Recommendations will be based on most selected interventions by the cohort of participants on the study, with the most popular listed interventions in rank order.
A total of three notifications will be sent between 10 a.m. and 10 p.m. If low mood/paranoia is detected by the App, it will re-notify the participant every 60 min to assess symptoms in real time with personalised interventions being displayed to participants. The system will re-notify participants a total of three times with an agreed crisis response being displayed on the App if low mood/paranoia is detected for a prolonged duration of time (a period of ≃4 h). Crisis planning is a routine part of EIS treatment with all service users working with their health professionals to agree a plan of action which they can follow if they are in crisis. The crisis plan will also be displayed via the TechCare App. The crisis response will consist of an agreed plan of action in the case participants are in distress due to their symptoms and will also prompt the participant to contact the EIS service or an agreed designated contact. In the feasibility context, we will examine response rates to questions and notifications and also the participant’s selection of the intervention. The researcher and case manager will be able to view participant responses and selection of interventions by the participant over the intervention period; this data will hold important insights into the feasibility of the intervention.
Adverse event reporting
The research team will adhere to principles of Good Clinical Practice in reporting adverse events.50 The adverse events in digital interventions are generally not well reported, as we have described previously.51 Monitoring of any serious adverse events (SAEs) will be carried out throughout the study. The PI N.H. will be directly notified of all adverse events, with all SAEs being reported to the NHS Research Ethics Committee (REC). In the light of the limited literature on adverse events in digital technology,51,52 we will explore these further through the strand 1 qualitative interviews and the data on the side effects such as worsening of symptoms and/or mood which will be assessed at the weekly review assessment and will be reported to the case manager.
Results
The trial is currently ongoing, and we have completed two focus groups with health professionals and some qualitative interviews with participants, who are participating in the strand 2: test run and intervention refinement component.
Proposed analysis strategy
Quantitative data analysis
All analyses will be conducted using SPSS v20, with preliminary analysis, being conducted where appropriate. We will compare baseline and post-intervention scores on the primary and secondary outcome measures. In the feasibility context, we aim to test our hypothesis that TechCare does not lead to poorer outcomes, that is, that the post-intervention scores are at least no worse than at pre-test.
Qualitative data analysis
Once the interviews and focus groups have been completed, these will be fully transcribed in order to be analysed. We will look for themes emerging in areas of feasibility, acceptability and further development. All of these aspects will provide insight to develop the intervention further and test in a future RCT. The qualitative data will be analysed using a framework analysis.53 We will analyse each individual transcript by identifying and highlighting portions or sections of the data relating to important or emerging themes. We will then compare and contrast these themes from across transcripts to find common ones and then combine similar themes into more general themes and sub-themes taking into account data from the whole data set. The data in its original textual context will then be placed under the headings and subheadings of the themes and sub-themes and will be used to form a conceptual framework. The process of framework analysis will be ongoing throughout the data collection period. Any discrepancies will be resolved through discussion within the research team, with the final themes and findings being read for congruence and reliability.54
Discussion/conclusion
Technology is increasing at an exponential rate with digital technologies providing a key platform for the delivery of improved health outcomes. The proposed research is a feasibility project, which aims to examine the feasibility and acceptability of the TechCare intervention. The intervention is based on sound theory derived from earlier research.10,25,26 We have also closely followed the guidance by the National Institute of Health Research29 in designing feasibility studies to test the vital parameters which will inform the design of a definitive trial.
Rees and Stone55 found that clinical psychologists rated therapeutic alliance lower in the videoconferencing condition than the face-to-face intervention. This shows that therapeutic alliance may be lesser developed within mHealth interventions than face-to-face intervention, which could have a negative impact on treatment. However, Cook and Doyle21 found that clients reported feeling satisfied with the therapeutic alliance within an online therapy intervention. Moreover, the TechCare intervention has the potential to overcome some of these criticisms as it intertwines mHealth with existing therapeutic relationships (client’s relationships with their care team), potentially enhancing rather than limiting the therapeutic capacity of the relationship. The mHealth intervention will have other advantages which can offset the disadvantage due to lack of face-to-face contact. The availability of the intervention at all times in contrast to limited time with the therapist and the flexibility in the use of the intervention are potential advantages. Furthermore, a study by Lester et al.19 showed the importance of technology in engagement within EIS. This is important in drawing emphasis on how mHealth functions could provide continued support, but also give clients greater autonomy.
The study has been designed with a focus on implementation from the outset and has engaged with the target audience in each step of developing the intervention. The service users were involved in developing the protocol, obtaining ethics for the study and also assisted in the development of the layout and overall design of the intervention.
Acknowledgments
The team is grateful for the help and support of Ian Cheung of Lancashire Care NHS Foundation Trust and Andrew Holland of Maywoods Ltd. All authors contributed to the writing of the manuscript. The first author (N.H.) is guarantor of the article and corresponding author. Trial registration: ClinicalTrials.gov. Identifier: NCT02439619.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: The project has obtained ethical approval from the NRES Committee North West – Preston, REC reference: 14/NW/1192.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: N.H. and I.C. are members of The Clinical Research Group on the use of mobile technology in mental health and have received funding from Lancashire Care NHS Foundation Trust, UK, to develop an intervention for early psychosis using mobile technology. N.G. gratefully acknowledges the support and funding of his PhD Studentship with the NIHR Collaboration for Leadership in Applied Health Research and Care (CLAHRC), North West Coast, UK. C.DJ.T. gratefully acknowledges the support of the National Institute of Health Research (NIHR), Research Fellowship Award (DRF-2012-05-211). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Informed consent: Written informed consent will be obtained from all subjects before participation in the study.
References
- 1. Bhugra D. No health without public mental health: the case for action (Position statement PS4/2010). Royal College of Psychiatrists, 2010, http://www.rcpsych.ac.uk/pdf/Position%20Statement%204%20website.pdf [Google Scholar]
- 2. McCrone P. Paying the price: the cost of mental health care in England to 2026, 2008, http://www.kingsfund.org.uk/sites/files/kf/Paying-the-Price-the-cost-of-mental-health-care-England-2026-McCrone-Dhanasiri-Patel-Knapp-Lawton-Smith-Kings-Fund-May-2008_0.pdf
- 3. Kessler RC, Amminger GP, Aguilar-Gaxiola S, et al. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry 2007; 20(4): 359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Van Os J, Linscott RJ, Myin-Germeys I, et al. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med 2009; 39(2): 179–195. [DOI] [PubMed] [Google Scholar]
- 5. Keshavan MS, DeLisi LE, Seidman LJ. Early and broadly defined psychosis risk mental states. Schizophr Res 2011; 126(1–3): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jolley S, Garety P, Peters E, et al. Opportunities and challenges in Improving Access to Psychological Therapies for people with Severe Mental Illness (IAPT-SMI): evaluating the first operational year of the South London and Maudsley (SLaM) demonstration site for psychosis. Behav Res Ther 2015; 64: 24–30. [DOI] [PubMed] [Google Scholar]
- 7. Kuipers E. Cognitive behavioural therapy and family intervention for psychosis – evidence-based but unavailable? The next steps. Psychoanal Psychother 2011; 25(1): 69–74. [Google Scholar]
- 8. Kay M, Santos J, Takane M. mHealth: new horizons for health through mobile technologies. Geneva: World Health Organization, 2011, pp. 66–71. [Google Scholar]
- 9. The Office of Communication UK. Facts & figures, http://media.ofcom.org.uk/facts/ (accessed 24 May 2016).
- 10. Granholm E, Ben-Zeev D, Link PC, et al. Mobile Assessment and Treatment for Schizophrenia (MATS): a pilot trial of an interactive text-messaging intervention for medication adherence, socialization, and auditory hallucinations. Schizophr Bull 2012; 38: 414–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Palmier-Claus J, Ainsworth J, Machin M, et al. The feasibility and validity of ambulatory self-report of psychotic symptoms using a smartphone software application. BMC Psychiatr 2012; 12(1): 172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bucci S, Barrowclough C, Ainsworth J, et al. Using mobile technology to deliver a cognitive behaviour therapy-informed intervention in early psychosis (Actissist): study protocol for a randomised controlled trial. Trials 2015; 16(1): 404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ben-Zeev D, Brenner CJ, Begale M, et al. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophr Bull. Epub ahead of print 8 March 2014. DOI: 10.1093/schbul/sbu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nickelson DW. Telehealth and the evolving health care system: strategic opportunities for professional psychology. Prof Psychol: Res Pr 1998; 29(6): 527–535. [Google Scholar]
- 15. Weinstein RS, Lopez AM, Joseph BA, et al. Telemedicine, telehealth, and mobile health applications that work: opportunities and barriers. Am J Med 2014; 127(3): 183–187. [DOI] [PubMed] [Google Scholar]
- 16. Henderson C, Knapp M, Fernández JL, et al. Cost effectiveness of telehealth for patients with long term conditions (Whole Systems Demonstrator telehealth questionnaire study): nested economic evaluation in a pragmatic, cluster randomised controlled trial. BMJ 2013; 346: f1035. [DOI] [PubMed] [Google Scholar]
- 17. Hebert MA, Korabek B, Scott RE. Moving research into practice: a decision framework for integrating home telehealth into chronic illness care. Int J Med Inform 2006; 75(12): 786–794. [DOI] [PubMed] [Google Scholar]
- 18. Barak A, Hen L, Boniel-Nissim M, et al. A comprehensive review and a meta-analysis of the effectiveness of Internet-based psychotherapeutic interventions. J Tech Hum Serv 2008; 26(2–4): 109–160. [Google Scholar]
- 19. Lester H, Marshall M, Jones P, et al. Views of young people in early intervention services for first-episode psychosis in England. Psychiatr Serv 2010; 62(8): 882–887. [DOI] [PubMed] [Google Scholar]
- 20. Rotondi AJ, Haas GL, Anderson CM, et al. A clinical trial to test the feasibility of a telehealth psychoeducational intervention for person with schizophrenia and their families: intervention and 3-month findings. Rehabil Psychol 2005; 50(4): 325–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cook JE, Doyle C. Working alliance in online therapy as compared to face-to-face therapy: preliminary results. Cyberpsychol Behav 2002; 5(2): 95–105. [DOI] [PubMed] [Google Scholar]
- 22. Mallen MJ, Day SX, Green MA. Online versus face-to-face conversations: an examination of relational and discourse variables. Psychother: Theor Res 2003; 40(1–2): 155–163. [Google Scholar]
- 23. Horvath AO, Del Re AC, Flückiger C, et al. Alliance in individual psychotherapy. Psychotherapy 2011; 48(1): 9. [DOI] [PubMed] [Google Scholar]
- 24. Alvarez-Jimenez M, Alcazar-Corcoles MA, Gonzalez-Blanch C, et al. Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophr Res 2014; 156(1): 96–106. [DOI] [PubMed] [Google Scholar]
- 25. Depp CA, Mausbach B, Granholm E, et al. Mobile interventions for severe mental illness: design and preliminary data from three approaches. J Nerv Ment Dis 2010; 198(10): 715–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kelly J, Gooding P, Pratt D, et al. Intelligent real-time therapy: harnessing the power of machine learning to optimise the delivery of momentary cognitive-behavioural interventions. J Ment Health 2012; 21(4): 404–414. [DOI] [PubMed] [Google Scholar]
- 27. Hollis C, Morris R, Martin J, et al. Technological innovations in mental healthcare: harnessing the digital revolution. Br J Psychiatry 2015; 206(4): 263–265. [DOI] [PubMed] [Google Scholar]
- 28. Medical Research Council (MRC). A framework for the development and evaluation of RCTs for complex interventions to improve health. London: MRC, 2000. [Google Scholar]
- 29. NETSCC definition of pilot and feasibility studies, http://www.netscc.ac.uk/glossary/ (accessed 24 May 2016).
- 30. McCrone P, Craig TKJ, Power P, et al. Cost-effectiveness of an early intervention service for people with psychosis. Br J Psychiatry 2010; 196: 377–382. [DOI] [PubMed] [Google Scholar]
- 31. Craig TKJ, Garety P, Power P, et al. The Lambeth Early Onset (LEO) Team: randomised controlled trial of the effectiveness of specialised care for early psychosis. BMJ 2004; 329: 1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wykes T, Steel C, Everitt B, et al. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull 2008; 34(3): 523–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kuipers E, Yesufu-Udechuku A, Taylor C, et al. Management of psychosis and schizophrenia in adults: summary of updated NICE guidance. BMJ 2014; 348: g1173. [DOI] [PubMed] [Google Scholar]
- 34. Kingdon DG, Turkington D. Cognitive-behavioral therapy of schizophrenia. New York: Guilford Press, 1994. [Google Scholar]
- 35. Myin-Germeys I, Peeters FPML, Havermans R, et al. Emotional reactivity to daily life stress in psychosis and affective disorder: an experience sampling study. Acta Psychiatr Scand 2003; 107(2): 124–131. [DOI] [PubMed] [Google Scholar]
- 36. Centre for Health Informatics, The University of Manchester. CareLoop, http://www.population-health.manchester.ac.uk/healthinformatics/research/Careloop (accessed 24 May 2016).
- 37. Granholm E, Loh C, Swendsen J. Feasibility and validity of computerized ecological momentary assessment in schizophrenia. Schizophr Bull 2008; 34(3): 507–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Španiel F, Vohlídka P, Hrdlička J, et al. ITAREPS: information technology aided relapse prevention programme in schizophrenia. Schizophr Res 2008; 98(1): 312–317. [DOI] [PubMed] [Google Scholar]
- 39. Kay SR, Fiszbein A, Opler LA, et al. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 1987; 13(2): 261–276. [DOI] [PubMed] [Google Scholar]
- 40. Haddock G, McCarron J, Tarrier N, et al. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS). Psychol Med 1999; 29(4): 879–889. [DOI] [PubMed] [Google Scholar]
- 41. Drake R, Haddock G, Tarrier N, et al. The Psychotic Symptom Rating Scales (PSYRATS): their usefulness and properties in first episode psychosis. Schizophr Res 2007; 89(1): 119–122. [DOI] [PubMed] [Google Scholar]
- 42. Greenwood KE, Sweeney A, Williams S, et al. CHoice of Outcome In Cbt for psychosEs (CHOICE): the development of a new service user–led outcome measure of CBT for psychosis. Schizophr Bull 2010; 36(1): 126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Tennant R, Hiller L, Fishwick R, et al. The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007; 5(1): 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Stewart-Brown S, Tennant A, Tennant R, et al. Internal construct validity of the Warwick-Edinburgh mental well-being scale (WEMWBS): a Rasch analysis using data from the Scottish health education population survey. Health Qual Life Outcomes 2009; 7(1): 15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fowler D, Freeman D, Smith B, et al. The Brief Core Schema Scales (BCSS): psychometric properties and associations with paranoia and grandiosity in non-clinical and psychosis samples. Psychol Med 2006; 36(6): 749–759. [DOI] [PubMed] [Google Scholar]
- 46. Addington D, Addington J, Schissel B. A depression rating scale for schizophrenics. Schizophr Res 1990; 3(4): 247–251. [DOI] [PubMed] [Google Scholar]
- 47. Schennach R, Obermeier M, Seemüller F, et al. Evaluating depressive symptoms in schizophrenia: a psychometric comparison of the Calgary Depression Scale for Schizophrenia and the Hamilton Depression Rating Scale. Psychopathology 2012; 45(5): 276–285. [DOI] [PubMed] [Google Scholar]
- 48. Mundt JC, Marks IM, Shear MK, et al. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry 2002; 180(5): 461–464. [DOI] [PubMed] [Google Scholar]
- 49. Sobocki P, Ekman M, Ågren H, et al. Health-related quality of life measured with EQ-5D in patients treated for depression in primary care. Value Health 2007; 10(2): 153–160. [DOI] [PubMed] [Google Scholar]
- 50. National Institute of Health Research. Good Clinical Practice (GCP) pocket guide, https://drive.google.com/file/d/0B-EwP8Oxl7jdM005QS0wMlRJZ3c/view (2014, accessed 13 July 2015).
- 51. Naeem F, Gire N, Xiang S, et al. Reporting and understanding the safety and adverse effect profile of mobile apps for psychosocial interventions: an update. World J Psychiatry 2016; 6(2): 187–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Marley J, Farooq S. Mobile telephone apps in mental health practice: uses, opportunities and challenges. BJPsych Bull 2015; 39(6): 288–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ritchie J, Spencer L, Bryman A, et al. Analysing qualitative data, vol. 3 London: Routledge, 1994. [Google Scholar]
- 54. Srivastava A, Thomson SB. Framework analysis: a qualitative methodology for applied policy research. J Publ Admin Govern 2009; 4(2): 72–79. [Google Scholar]
- 55. Rees CS, Stone S. Therapeutic alliance in face-to-face versus videoconferenced psychotherapy. Prof Psychol: Res Pr 2005; 36(6): 649–653. [Google Scholar]


