Abstract
Objectives: To estimate: 1) daily energy deficit required to reduce the weight of overweight children to within normal range; 2) time required to reach normal weight for a proposed achievable (small) target energy deficit of 0.42 MJ/day; 3) impact that such an effect may have on prevalence of childhood overweight.
Methods: Body mass index and fitness were measured in 31,424 Australian school children aged between 4.5 and 15 years. The daily energy deficit required to reduce weight to within normal range for the 7,747 (24.7%) overweight children was estimated. Further, for a proposed achievable target energy deficit of 0.42 MJ/day, the time required to reach normal weight was estimated.
Results: About 18% of children were overweight and 6.6% obese; 69% were either sedentary or light active. If an energy deficit of 0.42 MJ/day could be achieved, 60% of overweight children would reach normal weight and the current prevalence of overweight of 24.7% (24.2%–25.1%) would be reduced to 9.2% (8.9%–9.6%) within about 15 months.
Conclusions: The prevalence of overweight in Australian school children could be reduced significantly within one year if even a small daily energy deficit could be achieved by children currently classified as overweight or obese.
Keywords: childhood obesity prevention, energy balance, physical activity
Childhood obesity is considered by many to be the primary public health issue in children in developed countries and is an emerging issue in developing countries. 1 More than four decades ago, there were calls for greater effort to prevent child and adult obesity 2 but since that time the prevalence of overweight in children has increased several‐fold. For example, in Australia it has risen from around 7.5% in the 1960s to the current level of about 25%. A decade ago, Ebbeling and colleagues 1 – in a review of the causes and complications of childhood obesity – highlighted that the mechanisms that regulate body weight are extremely precise and that even a small positive daily energy balance could cause obesity in the long term. The converse is also true: a small daily energy deficit could lead to a reversal of the processes leading to obesity.
Here, we explore this latter proposition in a large sample of 31,424 Australian school children who have had assessments of body composition and physical performance competencies carried out since March 2000. The assessments were part of a service offered to Australian schools (in the Australian Capital Territory, New South Wales, South Australia and Queensland) by SmartStart for Kids, a not‐for‐profit organisation specialising in healthy exercise, eating and lifestyle programmes for school children. The specific aims were: 1) to estimate the daily energy deficit that would be required to return overweight or obese children to their normal weight range; 2) to estimate the time that it would take to reach normal weight if a given daily energy deficit could be achieved; and 3) to estimate potential impact on prevalence of childhood overweight.
Our findings support the hypothesis that childhood overweight or obesity may be caused, for most children, by a small daily energy intake surplus to the requirements of basal metabolic rate and habitual physical activity. Moreover, we demonstrate how this small daily energy excess may build up over time, leading to the much larger so‐called ‘maintenance energy gap’, 3 i.e. the additional change in energy balance required to permanently maintain a lower body weight, which makes the problem of overweight so challenging to reverse.
We also consider recent systematic reviews and meta‐analyses 4 , 5 , 6 , 7 summarising research efforts – to date, largely unsuccessful – to prevent or reverse obesity in children, and offer some insights into why failure to achieve clinically significant impact is so prevalent and what policies or strategies might increase the chances of success.
Methods
Ethics Statement
Ethical approval for the research was granted by the ACT Health Human Research Ethics Committee's Low Risk Sub‐Committee on 5 November 2014. The research provides further analysis of an existing database gathered by SmartStart for Kids. All work on which the study is based was carried out with the prior approval of the appropriate local education and health authorities who commissioned the service. Schools involved in the collection of the original data gave their informed consent and all parents gave written informed consent for children to take part. Data collection was carried out during normal school hours. School administrators and class teachers assisted with the coordination of the various class groups. Actual measurements were carried out by SmartStart for Kids trained assessors, usually three, to accommodate small groups of children moving round a set of measurement stations. All data processed in the current analysis was de‐identified so no individual child or school could be identified from any of the information available.
Settings and sample population
Children were assessed in class groups within the schools that participated in the study. Ninety‐one schools and 1,220 class groups were included over 12 school years (2000–2011).
Body composition and physical performance measures
Body composition for each child was represented by the body mass index (BMI), which is derived from weight in kg divided by the height in m2. Height was measured using a standard stadiometer (Surgical and Medical Products, Seven Hills, New South Wales, Australia) calibrated in 1 mm increments and weight was measured to the nearest 0.1 kg using Tanita TBF‐522 electronic weight and body fat monitor scales, calibrated regularly and spot‐weight checked at regular intervals. Percentage body fat was estimated using the bioelectric impedance monitor within the Tanita TBF‐522. Bioelectric impedance estimation of body fat has been shown to be a satisfactory field method for epidemiological applications. 8 Cardio‐respiratory fitness was measured using the 20 m multi‐stage fitness test. 9 Instructions were played using a calibrated CD player. Children did the test in small peer groups. One member of the SmartStart for Kids evaluation team acted as lead/runner for each group and two other members independently recorded the final stage and shuttle reached by each child. The children were encouraged by the facilitators to do their best.
Physical fitness categories
Physical fitness categories were estimated as follows. For each gender and half‐year age band in the range 4.5 to 15 years, the fitness range (maximum fitness value for gender/age – minimum fitness value for gender/age) was divided into eight equal segments and four cut‐points were set at the end of the 1st, 3rd, 5th and 7th segments, allowing us to derive a working estimate of five fitness categories for each gender/age combination.
Estimating basal metabolic rate
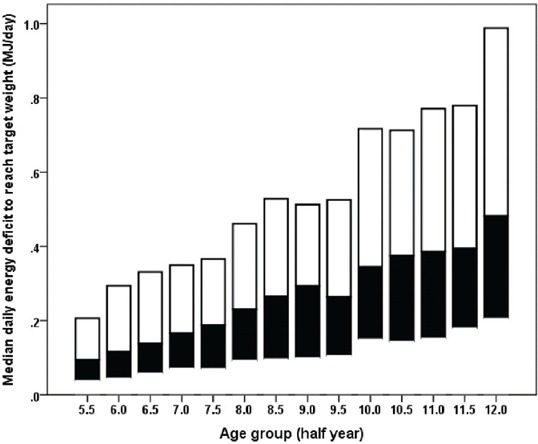
The basal metabolic rate (BMR, in MJ/day) for each child was estimated using equations developed by Schofield 10 for children and adolescents (age range 4.5–15 years). Equations used were:
 |
Estimating physical activity level (PAL) and energy requirement
In addition to the basal metabolic rate, calculation of the estimated energy requirement (EER) for each child needs an estimate of their physical activity level (PAL), i.e. the factor by which BMR is multiplied to obtain the estimated energy requirement for growth stage and habitual activity level. 11 We did not have objective measures of physical activity for each child. However, objective measures of cardio‐respiratory fitness were available and these were used as a proxy measure to categorise children into the following groups and corresponding PAL values: sedentary or light active (PAL=1.5); moderate active (PAL=1.8); and high active (PAL=2.1). Since the numbers of children in the lowest and highest categories of physical fitness were relatively small, the bottom two categories were merged to form the sedentary or light active group and the top two categories were merged to form the high active group. We were able to check this process using a group of 477 (240F, 237M) primary school children (data not included here) for whom we had objective pedometer‐based measures of physical activity and the same measure of cardiorespiratory fitness. 12 On the basis of this subsidiary analysis, this classification equates to: sedentary or low active <8,000 steps per day; 13 moderate active ≥8,000 and <12,000 steps per day; and high active ≥12,000 steps per day. Physical fitness correctly classified children's physical activity level within one category 94% of the time, which we deemed a satisfactory degree of reliability for present purposes.
The EER (MJ/day) for each child was then given by:
Estimating the daily energy deficit to normalise body weight for overweight or obese children
Using the International Obesity Task Force (IOTF) thresholds for overweight, 14 , 15 we obtained the BMI threshold for each overweight or obese child, below which they would be classified as being in the normal weight range for age and gender. This allowed us to calculate the weight that each overweight or obese child would need to reach to be within the normal range (BMI* height [m]2). The estimated daily energy deficit (Ed) required to reach normal body weight was calculated, using the equations for gender, age, height and weight, as:
where BMRwc is the basal metabolic requirement in MJ/day for the child's current weight and BMRwn is the basal metabolic requirement for their target normal range weight.
Estimating time to reach normal body weight for a given daily energy deficit
We estimated the characteristic time (Tn) to reach normal body weight for a given daily energy deficit using the approach developed by Hall et al. 16 The formula used for the calculation of Tn was:
| (1) |
where ηF and ηL account for the biochemical efficiencies for fat and lean tissue synthesis, 960 and 750 kJ/kg respectively; ρF and ρL represent the energy content per unit change of fat and lean tissue, 39.5 and 7.6 MJ/kg respectively; γF and γL are regression coefficients relating to resting metabolic rate for fat and lean tissue, 13 and 92 kJ/kg/day respectively; δ represents the contribution of physical activity
and
where α represents the ratio of change in lean tissue mass to change in fat mass, C is the Forbes constant, 10.4 kg 17 and F0 is the initial fat mass, which was estimated using bioelectric impedance (% body fat) × weight. The physical activity component, δ, appears only in the denominator of equation (1), thus increasing physical activity reduces the time required for weight loss. On the other hand, increasing fat mass increases the time required for weight loss.
For comparison, we calculated the time to reach normal body weight using a common rule of thumb that assumes a requirement of 32.2 MJ/kg of body weight loss. 18 This rule, in effect, ignores the lean tissue changes during weight loss, 19 but may still provide a useful estimate in circumstances where the more detailed calculation given above is not feasible. The time (days) required to reach the normal weight range for a given daily energy deficit (MJ/day), Ed, was calculated using the equation:
| (2) |
Results and Discussion
Children included in the sample were from kindergarten to year 9: 15,298 girls and 16,126 boys aged between 4.5 and 15 years. The distribution of the sample population by gender, half‐year age group and number of schools is shown in Table 1. About 3.8% of children were classified as underweight, 71.6% as normal weight, 18% as overweight and 6.6% as obese. These latter figures compare favourably with the proportion of overweight children nationally (aged 2–17 years) of 24.6%. 20 Based on direct measurement of cardio‐respiratory fitness, 69% of children were classified as either sedentary or light active, 25% as moderately active and 6% as highly active. Examining these proportions by school for the 91 schools (1,220 class groups) included in the study, the proportion of overweight or obese children per school class group ranged from 9% to 56% and per school from 19% to 34%, with an overall mean of 25%, while the proportion of children of low fitness ranged from 26% to 90%.
Table 1.
Distribution of sample population by gender, half‐year age group and number of schools.
| Age group (years) | Gender | Number of schools | |||||
|---|---|---|---|---|---|---|---|
| Female | Male | Total | |||||
| N | % | N | % | N | % | ||
| 4.5 | 92 | 0.6% | 95 | 0.6% | 187 | 0.6% | 35 |
| 5 | 983 | 6.4% | 987 | 6.1% | 1,970 | 6.3% | 62 |
| 5.5 | 1,594 | 10.4% | 1,715 | 10.6% | 3,309 | 10.5% | 70 |
| 6 | 1,188 | 7.8% | 1,457 | 9.0% | 2,645 | 8.4% | 66 |
| 6.5 | 851 | 5.6% | 921 | 5.7% | 1,772 | 5.6% | 67 |
| 7 | 1,095 | 7.2% | 1,000 | 6.2% | 2,095 | 6.7% | 73 |
| 7.5 | 1,041 | 6.8% | 1,077 | 6.7% | 2,118 | 6.7% | 72 |
| 8 | 871 | 5.7% | 926 | 5.7% | 1,797 | 5.7% | 75 |
| 8.5 | 872 | 5.7% | 886 | 5.5% | 1,758 | 5.6% | 76 |
| 9 | 1,018 | 6.7% | 953 | 5.9% | 1,971 | 6.3% | 77 |
| 9.5 | 1,062 | 6.9% | 1,081 | 6.7% | 2,143 | 6.8% | 82 |
| 10 | 922 | 6.0% | 1,007 | 6.2% | 1,929 | 6.1% | 79 |
| 10.5 | 896 | 5.9% | 875 | 5.4% | 1,771 | 5.6% | 75 |
| 11 | 825 | 5.4% | 826 | 5.1% | 1,651 | 5.3% | 69 |
| 11.5 | 684 | 4.5% | 758 | 4.7% | 1,442 | 4.6% | 67 |
| 12 | 456 | 3.0% | 500 | 3.1% | 956 | 3.0% | 67 |
| 12.5 | 285 | 1.9% | 316 | 2.0% | 601 | 1.9% | 47 |
| 13 | 185 | 1.2% | 246 | 1.5% | 431 | 1.4% | 21 |
| 13.5 | 197 | 1.3% | 237 | 1.5% | 434 | 1.4% | 12 |
| 14 | 140 | 0.9% | 194 | 1.2% | 334 | 1.1% | 8 |
| 14.5 | 41 | 0.3% | 69 | 0.4% | 110 | 0.4% | 7 |
| Total | 15,298 | 100% | 16,126 | 100% | 31,424 | 100% | 91 |
Daily energy deficit and time required to achieve normal weight range
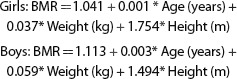
The daily energy deficit (MJ/day) and the time (days) required by overweight or obese children to attain the normal weight range for their age, height and gender are summarised in Figure 1.
Figure 1.
(a): Daily energy deficit (MJ/day) required by overweight or obese children to achieve their normal weight range. Horizontal reference lines represent the daily energy deficit that would allow 50% and 90% of children, 0.22 and 0.94 MJ/day respectively, to reach their normal weight range; (b) Median time (days) to reach normal weight range by age group by gender if an average daily energy deficit of 0.42 MJ/day could be achieved.
On the basis of Figure 1a, nearly two‐thirds of overweight or obese children could return to their normal weight range with a daily energy deficit of 0.42 MJ/day (100 kcal/day). Thus, the daily energy deficit required by the majority of children was relatively small and, therefore, likely to be easily attainable – at least in terms of the magnitude of any daily increase in physical activity or reduction in daily nutritional intake required.
The median number of days required to attain normal weight range was shorter at younger age and increased steadily through the school years (Figure 1b). This again is consistent, for the majority of children, with a small daily excess of energy intake relative to metabolic and habitual activity need that is stored as excess fat and builds up over time. Table 2 summarises the timescales over which benefits would be seen, expressed as percentiles of the population of overweight children who would return to normal weight under the three scenarios considered.
Table 2.
Percentiles of days required to reach normal weight range under three scenarios.
| Percentile | T1 (days)a | T2 (days)b | T3 (days)c |
|---|---|---|---|
| 10 | 115 | 247 | 29 |
| 20 | 132 | 289 | 67 |
| 30 | 150 | 329 | 114 |
| 40 | 168 | 373 | 171 |
| 50 | 187 | 413 | 240 |
| 60 | 209 | 459 | 339 |
| 70 | 233 | 507 | 469 |
| 80 | 258 | 563 | 655 |
| 90 | 294 | 645 | 968 |
If a daily energy deficit of 0.42 MJ/day could be achieved, more than 60% of currently overweight or obese children would return to normal weight, reducing the number of overweight children from 7,747 to 2,905 (i.e. assuming 62.5% of children – the actual figure at an energy deficit of 0.42 MJ/day – would return to normal weight) and the prevalence from the current 24.7% (24.2%–25.1%) to 9.2% (8.9%–9.6%), within around 15 months (see column headed T2, Table 2). A deficit of 0.42 MJ/day corresponds to about 7% of the median total energy requirement for a five‐year‐old child and 4.3% of that for a 12‐year‐old child.
The estimates under the column headed T1 in Table 2 are probably unrealistic, since some children would need to achieve very large energy deficits. When adequate information is available on each child then we would recommend using equation 1, column headed T2. On the basis of our comparison, the rule of thumb – equation (2), column headed T3 – underestimates the time for those with just a small amount of weight to lose and overestimates the time for those with the most weight to lose, performing reasonably well for those in between.
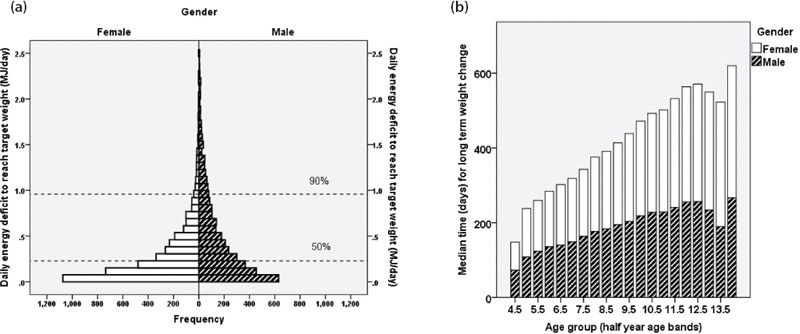
As shown in Figure 2 for the primary school years, the median energy deficit needed to return to normal weight rose steadily by school year group and the distribution, represented by the interquartile range, became wider and increasingly skewed towards higher energy deficit. This illustrates how even a small energy surplus may build up over time into a much larger energy surplus, known as the maintenance energy gap, because it represents the additional energy needed daily to maintain the new higher body weight. For the year group samples included in our study, the median energy deficit required to reduce the prevalence of overweight increased from 0.09 MJ/day (23 kcal/day) at age 5.5 to 0.48 MJ/day (115 kcal/day) at age 12, a fivefold increase over the primary school years.
Figure 2.
Median daily energy deficit (MJ/day) by age group (half year). Shaded vertical bars represent the interquartile range (white – upper quartile, black – lower quartile) and the median is represented by the junction between the bars.
Several research groups, mainly using population studies of weight gain in adults over time, have estimated the energy gap that may underlie the increases in body weight and obesity that have been observed globally. 21 , 22 , 23 , 24 Estimates of the daily energy excess in these studies ranged from 0.02 MJ/day in Swedish men 23 to 0.25 MJ/day at the 90th percentile for adults in the US. 21 While it is not possible to compare these studies directly, the estimates are consistent with population weight gain being driven by a relatively small excess in consumption over the requirement for basal metabolism and habitual energy expenditure. Wang et al. 25 and van den Berg et al. 26 have reported comparable studies in children. The former, using data from the US National Health and Nutrition Examination Surveys from 1988–1994 and 1999–2002, estimated that an energy gap of between 0.46 and 0.69 MJ/day could have prevented the weight gain seen over this 10‐year period. The latter, using data on 2,190 Dutch children participating in the PIAMA birth cohort study, estimated that a daily energy gap of between 0.289 and 0.32 MJ/day could have been responsible for the excess weight gain seen in the majority of the children who were overweight at the age of 5–7 years in their sample. Our estimates for the overweight children in our sample, median energy deficit 0.223 MJ/day (interquartile range 0.08–0.51 MJ/day), are of a similar order of magnitude, though we report a much broader range – probably as a result of having a much larger sample and mainly older children.
Key findings
Overweight and obesity is widespread in Australian school children. No class, school or community in our sample was immune. Clearly, this is a societal problem related to the way that children's lives are lived today compared with the way they would have been lived, say, 40 years ago, when the so‐called problem of childhood obesity did not exist at the epidemic levels seen today.
This study also demonstrates that school population levels of physical fitness are predominantly at the lower end of the achievable range for age. Thus, modern Australian children represented in this large sample would not appear to be receiving the best preparation for a healthy life and for development of their physical capacity in later life.
On a more positive note, the present analysis demonstrates that the daily energy deficit needed to reduce the prevalence of overweight and obesity markedly within a year is small and should be attainable by most children. The population prevalence of both overweight and low fitness would seem to indicate that this deficit would be best achieved through a combination of a relatively small reduction in daily dietary intake and an increase in daily physical activity. Importantly, the amounts of either required would not be considered large – the equivalent of about one small treat size (15g, 0.2–0.3 MJ) chocolate biscuit for the dietary restriction and about 15 minutes of extra moderate physical activity (e.g. walk, cycle or scooter to school, sport participation, active games during recess or after school) each day. Prevention would be achieved more quickly (Figure 1b) and, potentially, more easily (Figure 2) with younger children. That said, any adjustments made to lifestyle would need to be sustained each day to avoid recurrence.
What next?
If we accept that these observations confirm a significant challenge to Australian society (and many other societies globally), then the question arises as to what are the causes and what might be the solutions to the problem. Excessive availability of and exposure to foods and drinks; limited access to healthy, affordable foods; lack of daily quality physical activity in schools; loss of safe places for children to play or be active; and the emergence of television and other media that encourage sedentary pursuits are seen as the front‐running causes. 27 , 28
As to the solutions, an extensive review of interventions to prevent childhood obesity has been published recently. 4 Waters et aI, from a meta‐analysis of 37 studies globally involving 27,946 children, reported that the available evidence supported the view that such programmes were effective at reducing adiposity. Overall, a standardised mean difference in adiposity (BMI z‐score) of −0.15 kg/m2 was reported between intervention and control groups.
We examined the studies that reported BMI as an outcome in the review by Waters et al. 4 in more detail, looking specifically at the design and content of the interventions. Twelve of these interventions achieved statistically significant standardised mean reductions in adiposity (BMI z‐score). The features that set these more effective interventions apart from the others were: 1) a specific focus on children who were already obese or identified as being at risk of becoming obese (the top six most effective interventions included this element); 29 , 30 , 31 , 32 , 33 , 34 2) inclusion of multiple components addressing the main factors that influence or control children's daily eating and physical activity behaviours such as parents, teachers, curriculum and school environment or policy; 29 , 30 , 31 , 32 , 33 , 34 , 36 , 37 , 38 , 39 , 40 and 3) direct influence on both physical activity and dietary behaviours 30 , 31 , 32 , 33 , 34 , 35 , 37 , 38 , 39 , 40 , 41 or dietary behaviours only. 35
Waters et al. went on to conclude that the following are promising policies and strategies for prevention of childhood obesity:
School curriculum that includes healthy eating, physical activity and body image.
Increased sessions for physical activity and the development of fundamental movement skills throughout the school week.
Improvements in nutritional quality of the food supply in schools.
Environments and cultural practices that support children eating healthier foods and being active throughout each day.
Support for teachers and other staff to implement health promotion strategies and activities (e.g. professional development, capacity building activities).
Parent support and home activities that encourage children to be more active, eat more nutritious foods and spend less time in screen‐based activities.
Our findings would support these policies or strategies, with the added proviso that the effort involved at an individual level does not necessarily amount to that much but it does need to be sustained on a daily basis.
If these are the routes to the solution, then the questions of funding and how to embed them in our systems and community remain. In a recent systematic review, Metcalf, Henley and Wilkin carried out a meta‐analysis of interventions to increase physical activity in children and concluded that such interventions had only a small effect (about four minutes more walking or running per day) on children's overall activity levels. 6 Clearly, our present systems are failing and have been doing so for some time. 6 Successive generations of Australian school children have lost their free play and other opportunities to be active have been eroded from daily life. 41 Replacing this lost opportunity will not be easy. Communities have lost (to the national workforce) the ‘at home’ parents who in the past would have been around to oversee safe places for children to play and be active. 42 Streets are now dominated by the car and are mostly considered out‐of‐bounds for playing children. 43 On the other hand, schools would appear to offer the ideal environment in which to implement change, since almost every child goes to school, adequate recess time and activity space are available and the weather in Australia is mainly conducive to outside activity. That said, to ensure the large numbers of children and families not receiving adequate support for physical activities and the development of healthy eating behaviours are able to do so would likely require significant resources. The questions of who should fund this societal shift and how it should be implemented remain unanswered.
Limitations
There are a number of limitations that need to be considered when interpreting these findings. First, the sample of children included, though large, cannot be considered a representative sample of Australian school children. The schools and children included were determined by the individual schools or organisations that commissioned SmartStart for Kids to carry out body composition and physical performance measurements in their schools. Nonetheless, for the significant population of school children sampled over a wide geographical area within Australia, the estimates of proportions overweight or obese and of energy deficit remain valid.
Second, our use of available range of fitness for age as a proxy measure of physical activity and to estimate the PAL for each child is not standard practice. An alternative approach could have been to use norm‐based thresholds to set ordered categories of physical activity level such as those published recently by Catley and Tomkinson. 44 However, this process too is not established and the available norm data do not cover the lower age ranges included in our sample. This issue will be the topic for a future publication from further analysis of the SmartStart for Kids database.
A third limitation relates to the use of simplifying equations for estimating BMR depending on the age, gender, height and weight of each child. 10 Each child's specific body composition and physiological function is unique so, clearly, these assumptions are not strictly valid. However, we are interested here in population trends across time rather than changes within an individual child. The equations used for estimating BMR, the energy deficit required for weight loss and the time to achieve a given weight loss are best estimates of average values from population studies. Therefore, we believe that our use of them here is justified. Similarly, it is unlikely that a precise target energy deficit would be met by each child in each school for each day. Again, our interest is in reasonable average values for what might be achievable and what outcomes might be expected if this were the case.
Conclusion
The prevalence of overweight and obesity in Australian school children could be reduced markedly within around 15 months if a small daily energy deficit of 0.42 MJ/day could be achieved by those children who are currently classified as overweight or obese.
The authors have stated the following conflict of interest: F. Robert de Castella is on the Board of SmartStart for Kids, a not‐for‐profit organisation specialising in healthy exercise, eating and lifestyle programs for school children.
References
- 1. Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public health crisis, common sense cure. Lancet. 2002; 360: 473–82. [DOI] [PubMed] [Google Scholar]
- 2. Infant and adult obesity. Lancet. 1974; 1: 17–8. [PubMed] [Google Scholar]
- 3. Hill JO, Peters JC, Wyatt HR. Using the energy gap to address obesity: A commentary. J Am Diet Assoc. 2009; 109: 1848–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Waters E, de Silva‐Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children (Cochrane Review) In: The Cochrane Database of Systematic Reviews; Issue 12, 2011. Chichester (UK): John Wiley and Sons; 2011. [DOI] [PubMed] [Google Scholar]
- 5. Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school‐based physical activity interventions on body mass index in children: A meta‐analysis. CMAJ. 2009; 180: 719–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Metcalf B, Henley W, Wilkin T. Effectiveness of intervention on physical activity of children: Systematic review and meta‐analysis of controlled trials with objectively measured outcomes (EarlyBird 54). BMJ. 2012; 345: e5888. [DOI] [PubMed] [Google Scholar]
- 7. Kropski JA, Keckley PH, Jensen GL. School‐based obesity prevention programs: An evidence‐based review. Obesity (Silver Spring). 2008; 16: 1009–18. [DOI] [PubMed] [Google Scholar]
- 8. Paineau D, Chiheb S, Banu I, Valensi P, Fontan JE, Gaudelus J, et al. Comparison of field methods to estimate fat mass in children. Ann Hum Biol. 2008; 35 (2): 185–97. [DOI] [PubMed] [Google Scholar]
- 9. Ramsbottom R, Brewer J, Williams C. A progressive shuttle run test to estimate maximal oxygen uptake. Br J Sport Med. 1988; 22: 141–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr 1985; 39 Suppl 1:5–41. [PubMed] [Google Scholar]
- 11. National Health and Medical Research Council . Nutrient Reference Values for Australia and New Zealand including Recommended Dietary Intakes. Canberra (AUST): Commonwealth of Australia; 2006. p. 15–8. [Google Scholar]
- 12. Telford RM, Telford RD, Cunningham RB, Cochrane T, Davey R, Waddington G. Longitudinal patterns of physical activity in children aged 8 to 12 years: The LOOK Study. Int J Behav Nutr Phys Act. 2013; 10: 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tudor‐Locke C, Craig CL, Beets MW, Belton S, Cardon GM, Duncan S, et al. How many steps/day are enough? for children and adolescents. Int J Behav Nutr Phys Act. 2011; 8: 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ. 2000; 320: 1240–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cole TJ, Flegal KM, Nicholls D, Jackson AA. Body mass index cut offs to define thinness in children and adolescents: International survey. BMJ. 2007; 335: 194–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hall KD, Sacks G, Chandramohan D, Chow CC, Wang YC, Gortmaker SL, et al. Quantification of the effect of energy imbalance on bodyweight. Lancet. 2011; 378: 826–37 (equation 15, supplementary webappendix). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Forbes GB. Lean body mass‐body fat interrelationships in humans. Nutr Rev. 1987; 45 (8): 225–31. [DOI] [PubMed] [Google Scholar]
- 18. Wishnofsky M. Caloric equivalents of gained or lost weight. Am J Clin Nutr. 1958; 6: 542–6. [DOI] [PubMed] [Google Scholar]
- 19. Hall KD. What is the required energy deficit per unit weight loss? Int J Obes (Lond). 2008; 32 (3): 573–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Australian Bureau of Statistics . 4364.0.55.003 – Australian Health Survey: Updated Results, 2011–2012. Canberra (Aust): ABS; 2013. [Google Scholar]
- 21. Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. 1998; 280: 1371–4. [DOI] [PubMed] [Google Scholar]
- 22. Brown WJ, Williams L, Ford JH, Ball K, Dobson AJ. Identifying the energy gap: Magnitude and determinants of 5‐year weight gain in midage women. Obes Res. 2005; 13: 1431–41. [DOI] [PubMed] [Google Scholar]
- 23. Berg C, Rosengren A, Aires N, Lappas G, Toren K, Lissner L. Trends in overweight and obesity from 1985 to 2002 in Goteborg, West Sweden. Int J Obes. 2005; 29: 916–24. [DOI] [PubMed] [Google Scholar]
- 24. Ebrahimi‐Mameghani M, Scott JA, Der G, Lean MEJ, Burns CM. Changes in weight and waist circumference over 9 years in a Scottish population. Eur J Clin Nutr. 2008; 62: 1208–14. [DOI] [PubMed] [Google Scholar]
- 25. Wang YC, Gortmaker SL, Sobol AM, Kuntz KM. Estimating the energy gap among US children: A counterfactual approach. Pediatrics. 2006; 118: e1721–33. [DOI] [PubMed] [Google Scholar]
- 26. van den Berg SW, Boer JMA, Scholtens S, de Jongste JC, Brunekreef B, Smit HA, et al. Quantification of the energy gap in young overweight children. The PIAMA Birth Cohort Study. BMC Public Health. 2011; 11: 326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. National Preventative Health Taskforce Obesity Working Group . Technical Paper 1 Obesity in Australia: A Need for Urgent Action. Canberra (AUST): Commonwealth of Australia; 2009. [Google Scholar]
- 28. Centers for Disease Control and Prevention . A Growing Problem [Internet]. Atlanta (GA): CDC Division of Nutrition, Physical Activity and Obesity; 2012. [cited 2012 Jul 27]. Available from: http://www.cdc.gov/obesity/childhood/problem.html
- 29. Keller A, Klossek A, Gausche R, Hoepffner W, Kiess W, Keller E. Selective primary obesity prevention in children. Dtsch Med Wochenschr. 2009; 134: 13–8. [DOI] [PubMed] [Google Scholar]
- 30. Harvey‐Berino J, Rourke J. Obesity prevention in preschool native‐American children: A pilot study using home visiting. Obes Res. 2003; 11: 606–11. [DOI] [PubMed] [Google Scholar]
- 31. Lazaar N, Aucouturier J, Ratel S, Rance M, Meyer M, Duche P. Effect of physical activity intervention on body composition in young children; influence of body mass index status and gender. Acta Paediatr. 2007; 96: 1315–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Neumark‐Sztainer D, Story M, Hannan PJ, Rex J. New moves: A school‐based obesity prevention program for adolescent girls. Prev Med. 2003; 37: 41–51. [DOI] [PubMed] [Google Scholar]
- 33. Story M, Sherwood NE, Himes JH, Davis M, Jacobs DR, Cartwright Y, et al. An after‐school obesity prevention program for African‐American girls: The Minnesota GEMS pilot study. Ethn Dis. 2003; 13 (1 Supp 1): 54–64. [PubMed] [Google Scholar]
- 34. Marcus C, Nyberg G, Nordenfelt A, Karpmyr M, Kowalski J, Ekelund U. A 4‐year, cluster‐randomised, controlled childhood obesity prevention study: STOPP. Int J Obes (Lond). 2009; 33: 408–17. [DOI] [PubMed] [Google Scholar]
- 35. James J, Thomas P, Cavan D, Kerr D. Preventing childhood obesity by reducing consumption of carbonated drinks: Cluster randomised controlled trial. BMJ. 2004; 328: 1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Taylor RW, McAuley KA, Barbezat W, Farmer VL, Williams SM, Mann JI. Two‐year follow‐up of an obesity prevention initiative in children: The APPLE project. Am J Clin Nutr. 2008; 88: 1371–7. [DOI] [PubMed] [Google Scholar]
- 37. Spiegel SA, Foulk D. Reducing overweight through a multidisciplinary school‐based intervention. Obesity (Silver Spring). 2006; 14: 88–96. [DOI] [PubMed] [Google Scholar]
- 38. Haerens L, Deforche B, Maes L, Stevens V, Cardon G, De Bourdeauhuij I. Body mass effects of a physical activity and healthy food intervention in middle schools. Obesity (Silver Spring). 2006; 14: 847–54. [DOI] [PubMed] [Google Scholar]
- 39. Kain J, Uauy R, Albala, Vio F , Cerda R, Leyton B. School‐based obesity prevention in Chilean primary school children: Methodology and evaluation of a controlled study. Int J Obes Relat Metab Disord. 2004; 28: 483–93. [DOI] [PubMed] [Google Scholar]
- 40. Sanigorski AM, Bell AC, Kremer PJ, Cuttler R, Swinburn BA. Reducing unhealthy weight gain in children through community capacity‐building: Results of a quasi‐experimental intervention program, Be Active Eat Well. Int J Obes. 2008; 32: 1060–7. [DOI] [PubMed] [Google Scholar]
- 41. Dollman J, Norton K, Norton L. Evidence for secular trends in children's physical activity behaviour. Brit J Sports Med. 2005; 39: 892–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Australian Bureau of Statistics . 4102.0. – Fifty Years of Labour Force: Now and Then Australian Social Trends, December 2011. Canberra (AUST): ABS; 2011. [Google Scholar]
- 43. Molnar BE, Gortmaker SL, Bull FC, Buka SL. Unsafe to play? Neighborhood disorder and lack of safety predict reduced physical activity among urban children and adolescents. Am J Health Promot. 2004; 18 (5): 378–86. [DOI] [PubMed] [Google Scholar]
- 44. Catley MJ, Tomkinson GR. Normative health‐related fitness values for children: Analysis of 85347 test results on 9–17‐year‐old Australians since 1985. Brit J Sport Med. 2013; 47 (2): 98–108. [DOI] [PubMed] [Google Scholar]


