Abstract
Respiratory syncytial virus (RSV) is one of the most important pathogenic infections of children and requires in-depth research worldwide, and especially in developing countries. We used a novel multiplex real-time PCR to test 5483 patients (≤ 14 years old) hospitalized with respiratory illness in Guangzhou, China, over a 3-year period. Of these patients, 729 were positive for RSV-A (51.2%, 373/729) or RSV-B (48.8%, 356/729), but none was infected with both viruses. Two seasonal peaks in total RSV were detected at the changes from winter to spring and from summer to autumn. RSV-B was dominant in 2013 and RSV-A in 2015, whereas RSV-A and RSV-B cocirculated in 2014. The clinical presentations of 645 RSV-positive patients were analyzed. Bronchiolitis, dyspnea, coryza, vomiting, poor appetite, and diarrhea occurred more frequently in RSV-A-positive than RSV-B-positive patients, whereas chill, headache, myalgia, debility, and rash etc. were more frequent in RSV-B-positive than RSV-A-positive patients, suggesting specific clinical characteristics for RSV-A and RSV-B. Coinfectons with other pathogens were common and diverse. Bronchiolitis, fever (≥ 38°C), and poor appetite were more frequent in patients with single RSV infections than in coinfected patients, suggesting the key pathogenic activity of RSV. Analysis of the relationships between the comparative viral load and clinical presentations showed significant differences in bronchiolitis, fever (≥ 38°C), and rash etc. among patients with different viral loads. This study provides a novel rapid method for detecting RSV subgroups, and provides new insights into the epidemiology and clinical implications of RSV.
Introduction
Respiratory syncytial virus (RSV), of the family Paramyxoviridae, is a nonsegmented, negative-strand RNA virus that expresses 11 proteins [1]. RSV is amongst the most important pathogenic infections of childhood and is associated with significant morbidity and mortality, especially in developing countries [2]. The clinical manifestations of RSV infection range from mild upper-respiratory-tract illnesses (URTIs) or otitis media to severe and potentially life-threatening lower-respiratory-tract illnesses (LRTIs). The most common form of LRTI in RSV-infected infants is bronchiolitis, but pneumonia and croup are also seen [2–6]. There are two major antigenic subgroups of RSV, A and B, based on antigenic differences in their glycoproteins G and F [7–10]. The epidemiological features of RSV-A and RSV-B have differed in previous studies, and although strains of both subtypes often cocirculate, one subtypes generally predominates, depending on the region and climate [5, 6, 11, 12]. Therefore, the in-depth epidemiological characterization of RSV in specific areas is required worldwide, and especially in developing countries.
RSV is detected with direct or indirect immunofluorescence, enzyme-linked immunosorbent assay, viral culture, or increasingly, with reverse transcription–polymerase chain reaction (RT–PCR), especially real-time RT–PCR [6, 13]. Real-time PCR has many advantages in the detection of viruses, including its high specificity, high sensitivity, quantifiability, and simplicity of operation. It has been used for early diagnosis and the evaluation of drug efficacy and therapeutic effects, although the quantitative analysis of viruses in respiratory specimens is still impracticable. The results are usually simply positive or negative, although quantification is possible from Ct values or with plaque assays [14, 15]. The results from two independent respiratory specimens, such as throat swabs, nasopharyngeal swabs, or bronchial alveolar lavage fluid, can differ, even when both specimens are taken from the same individual at a same time, because they are dependent the sampling skill and features of the samples themselves. Thus, inconsistent results can be produced. However, comparative quantification PCR using a housekeeping gene, such as β-actin (ACTB) or glyceraldehyde 3-phosphate dehydrogenase (GAPDH), might be suitable for the analysis of these types of respiratory specimens.
In this study, we investigated the epidemiological features of RSV (subgroups A and B) in pediatric patients (≤ 14 years old) hospitalized with respiratory illness in Guangzhou, China, between January 2013 and December 2015, using a newly established multiplex real-time PCR, including the housekeeping gene, human ACTB.
Materials and Methods
Ethics Statement
The study was approved by The First Affiliated Hospital of Guangzhou Medical University Ethics Committee for research on human beings, and the next of kin, caretakers, or guardians on behalf of the minors/children gave signed informed consent for participation in the study.
Respiratory sample collection
Throat swab samples from pediatric patients (≤ 14 years old) hospitalized with acute respiratory-tract illness (ARTI) were collected at two hospitals between January 2013 and December 2015 for routine screening for respiratory viruses, Mycoplasma pneumoniae (MP), and Chlamydophila pneumoniae (CP). The samples were collected with established clinical protocols [16]. The samples were refrigerated at 2–8°C in viral transport medium, transported on ice to the State Key Laboratory of Respiratory Diseases, and analyzed immediately or stored at −80°C before analysis as described in detail previously [17].
The patients’ clinical presentations were collected from their medical records using designed presentation cards, and were categorized retrospectively into the following six groups: URTI, LRTI, systemic influenza-like symptoms, gastrointestinal illness, neurological symptoms, and others. Patients with nasal obstruction, coryza, sneezing, coughing, pharyngeal discomfort, or hoarseness were categorized as having URTI. Patients with pneumonia, bronchiolitis, increasing lung markings, dyspnea, or an abnormal pulmonary breath sound were categorized as having LRTI. Patients with high fever (≥ 38°C), chills, dizziness, headache, myalgia, or debility were categorized as having systemic influenza-like symptoms. Patients with vomiting, poor appetite, or diarrhea were categorized as having a gastrointestinal illness. Patients with convulsions were categorized as having neurological symptoms. Patients with other symptoms, including but not limited to rash, were classified as “others”. Some patients were assigned to several clinical presentation groups. Increasing lung markings, pneumonia, and bronchiolitis were diagnosed with chest radiography. Abnormal pulmonary breath sounds included phlegmatic rales, wheezy rales, bubbling rales, and moist rales. Other clinical symptoms were identified with a normal medical examination and clinical descriptions.
Multiplex real-time PCR to detect RSV-A, RSV-B, and human ACTB
RNA and DNA were extracted from the respiratory samples with the QIAamp Viral RNA Mini Kit and QIAamp DNA Mini Kit (Qiagen, Shanghai, China), respectively, in accordance with the manufacturer’s protocols. The primers and TaqMan probes designed to detect RSV subgroups A and B, by amplifying the RSV G gene, and to detect the mRNA of internal control, human ACTB, are listed in Table 1. Multiplex real-time RT–PCR was conducted using our optimized reaction buffer and cycling conditions. Each 25 μl reaction mixture contained 1× reaction buffer (50 mM Tris-Cl [pH 8.9], 75 mM KCl, 4 mM MgCl2, 10% glycerol), 0.6 mM deoxynucleoside triphosphates (dNTPs) (Promega, Beijing, China), 0.4 μM each primer (for RSV A, RSV B, and human ACTB) (BGI, Shenzhen, China), fluorescent probes for RSV A and RSV B (0.04 μM), fluorescent probe for human ACTB (0.06 μM) (TaKaRa, Dalian, China) (Table 1), 50 U of M-MLV reverse transcriptase (Promega, Beijing, China), 1 U of Taq DNA polymerase (Promega, Beijing, China), and 5 μl of template RNA. The cycling conditions were 48°C for 10 min, 94°C for 2 min, and then 40 cycles of 94°C for 10 s and 55°C for 35 s. The amplified nucleic acids were detected with the Applied Biosystems 7500 Real-Time PCR System (Life Technologies, Singapore).
Table 1. Primers and probes used in multiplex real-time PCR to detect RSV-A, RSV-B, and human ACTB.
| Target a | Primers and probes | Sequences b |
|---|---|---|
| RSV-A | ||
| Forward | 5’-ACTGCAATCAYACAAGATGCAACRA-3’ | |
| Reverse | 5’-CAGATTGRAGAAGCTGATTCCA-3’ | |
| Probe | 5’-FAM-CCAGATCAAGAACACAACCCCARCATACCT-BHQ1-3’ | |
| RSV-B | ||
| Forward | 5’-ACTTACCTTACTCAAGTCTCACCAGAAA-3’ | |
| Reverse | 5’-TTGTRGCTGARTTTGTGTGGAT-3’ | |
| Probe | 5’-Texas red-TTAGCCCATCCMAACAAYCCACAACC-BHQ2-3’ | |
| Human beta actin | ||
| Forward | 5’-TGGCACCCAGCACAATGA-3’ | |
| Reverse | 5’-GCCGATCCACACGGAGTACT-3’ | |
| Probe | 5’-JOE-ATCAAGATCATTGCTCCTCCTGAGCGC-BHQ1-3’ |
Note:
a Conserved G gene specific for RSV-A and RSV-B, and human ACTB gene were used for detection.
b TaqMan probes were used; Y represents C or T; R represents A or G; M represents A or C.
Specificity of the multiplex real-time PCR in detecting RSV-A, RSV-B, and human ACTB
Each of 15 cultured RSV-A- or RSV-B-positive samples, stored at the State Key Laboratory of Respiratory Diseases and a panel of respiratory pathogens commonly found in the respiratory tract were used to determine the specificity of the multiplex real-time PCR. The nucleic acids were extracted from samples positive for RSV-A, RSV-B, influenza A virus (InfA), influenza B virus (InfB), four types of parainfluenza (PIV1–4), adenovirus (ADV), enterovirus (EV), human metapneumovirus (HMPV), four strains of human coronavirus (HCoV-229E, OC43, NL63, and HKU1), rhinovirus (RV), human bocavirus (HBoV), MP, CP, Streptococcus pneumonia, Staphylococcus aureus, and Haemophilus influenza, and tested with the multiplex real-time PCR.
Sensitivity of multiplex real-time PCR in detecting RSV-A, RSV-B, and human ACTB
RNA transcripts of RSV-A, RSV-B, and human ACTB were used as standards to determine the assay sensitivity. Primers for RSV-A, RSV-B, and ACTB containing the T7 promoter sequence were used to amplify the target DNAs with the PrimeScript One Step RT–PCR Kit ver. 2 (TaKaRa, Dalian, China): RSV-A forward primer: 5′-TAATACGACTCACTATAACTGCAATCAYACAAGATGCAACRA-3′; RSV-A reverse primer: 5′-CAGATTGRAGAAGCTGATTCCA-3′; RSV-B forward primer: 5′-TAATACGACTCACTATAACTTACCTTACTCAAGTCTCACCAGAAA-3′; RSV-B reverse primer: 5′-TTGTRGCTGARTTTGTGTGGAT-3′; human ACTB forward primer: 5′-TAATACGACTCACTATAGGCATCCACGAAACTACCTT-3′; and human ACTB reverse primer: 5′-GCCGGACTCGTCATACTCCT-3′. The target DNAs were purified with a TIANprep DNA gel extraction kit (Tiangen, Beijing, China), and the RNAs were transcribed in vitro with a TranscriptAid T7 High Yield Transcription Kit (Thermo Scientific, Lithuania). The purity and concentrations of the RNA transcripts were established with a NanoDrop spectrophotometer (Thermo Scientific, NanoDrop Technologies, USA). The sensitivity and standard curves for the multiplex real-time PCR were established for RSV-A, RSV-B, and human ACTB by testing the transcripts of known concentrations serially diluted in diethyl-pyrocarbonate-treated water.
Common respiratory pathogens detected in RSV-positive patients
RSV-positive samples were tested simultaneously for the following 17 respiratory pathogens: InfA, InfB, PIV1–4, ADV, EV, HMPV, HCoV-229E, HCoV-OC43, HCoV-NL63, HCoV-HKU1, RV, HBoV, MP and CP. The testing procedure, using kits from Guangzhou HuYanSuo Medical Technology Co., Ltd, has been described in a previous report [17].
Comparative quantitation of RSV-A and RSV-B infections in throat swabs
Standard curves for the multiplex real-time PCR were constructed with RNA transcripts. The viral loads and the expression of human ACTB mRNA were calculated from the corresponding standard curves. The comparative viral loads (CVLs) of RSV-A and RSV-B were calculated by dividing the viral load by the amount of human ACTB transcripts in the same sample. CVL was used as the comparative quantity in the analysis.
Statistical analysis
As described in detail previously [17], all statistical analyses were performed with the SPSS statistical software (version 19.0; SPSS Inc., Chicago, IL, USA). To compare categorical data, the χ2 test and Fisher’s exact test were used, as appropriate. All tests were two-tailed, and p < 0.05 was considered statistically significant.
Results
Specificity and sensitivity of multiplex real-time PCR in detecting RSV-A, RSV-B, and human ACTB
A panel of samples positive for RSV-A, RSV-B, and other common respiratory pathogens were tested with the multiplex real-time PCR, and no nonspecific reactions were observed. Serial dilutions of the target RNA transcripts were tested with the multiplex real-time PCR. The fluorescent signals observed at various dilutions of the two viral subgroups and human ACTB transcripts were used to calculate the minimal amounts of detectable RSV-A RNA (20 copies), RSV-B RNA (40 copies), and ACTB mRNA (60 copies) in 5 μl of RNA solution, and good linear relationships were found from 50 to 5 × 1010 copies of RSV-A (r2 = 0.9973), 500 to 5 × 1010 copies of RSV-B (r2 = 0.9989), and 500 to 5 × 1010 copies of ACTB mRNA (r2 = 0.9984) in 5 μl of RNA solution. The slopes of the standard curves were −3.30 for RSV-A, −3.35 for RSV-B, and −3.31 for human ACTB mRNA.
Distributions of RSV-A and RSV-B in pediatric patients
In total, 5483 pediatric patients (≤14 years old) hospitalized with ARTI between January 2013 and December 2015were enrolled in this study. The male-to-female ratio was 1.74 (3481:2002) and the median age was 2.00 years (interquartile range, 0.75–4.00). Of the 5483 patients, 729 (13.3%) were positive for RSV-A or RSV-B, but no patient was coinfected with RSV-A and RSV-B. The male-to-female ratio was 2.41:1 (515:214) in the RSV-positive patients and 1.66:1 (2966:1788) in the RSV-negative patients (p < 0.001). The median age of the RSV-positive patients was 0.83 years (interquartile range, 0.42–2.00). Among these 729 patients, 373 (51.2%) were positive for RSV-A and 356 (48.8%) were positive for RSV-B. The male-to-female ratios were 2.33 (261:112) for RSV-A-positive patients and 2.49 (254:102) for RSV-B-positive patients. The median ages of the RSV-A- and RSV-B-positive patients were 0.83 years (interquartile range, 0.42–1.96) and 0.92 years (interquartile range, 0.42–2.00), respectively.
In this study, we tested the RSV-positive patients for another 17 common respiratory pathogens. Copathogens were common, and were found in 128 of the 729 (17.6%) RSV-positive patients: in 56 (15.0%, 56/128) RSV-A-positive patients and 72 (22.2%, 72/128) RSV-B positive patients (p = 0.065). Fifteen of these 17 pathogens (88.2%) were detected, and the most frequent copathogens were RV (26.6%, 34/128), InfA (21.1%, 27/128), EV (14.8%, 19/128), MP (11.7%, 15/128), ADV (10.9%, 14/128), HBoV (9.4%, 12/128), and HCoV-OC43 (8%, 6.3/128), followed by HMPV, InfB, PIV3, CP, PIV1, PIV4, HCoV-HKU1, and HCoV-229E at rates lower than 5%. PIV2 and HCoV-NL63 were not found in these patients (Table 2). MP was detected in 18.1% (13/72) of RSV-B-positive patients and 3.6% (2/56) of RSV-A-positive patients (p = 0.003) (Table 2). However, there were no significant differences in the detection rates for the other 16 copathogens in the RSV-A- or RSV-B-positive patients or the positive rates were too small to analyze (Table 2).
Table 2. Distribution of copathogens in RSV-positive patients.
| Co-pathogena | Total(n = 128) | Co-pathogen with RSV-A (n = 56) | Co-pathogen with RSV-B (n = 72) | p valueb |
|---|---|---|---|---|
| RV | 34(26.6) | 14(25) | 20(27.8) | 0.233 |
| infA | 27(21.1) | 11(19.6) | 16(22.2) | 0.269 |
| EV | 19(14.8) | 10(17.9) | 9(12.5) | 0.897 |
| MP | 15(11.7) | 2(3.6) | 13(18.1) | 0.003 |
| ADV | 14(10.9) | 9(16.1) | 5(6.9) | 0.321 |
| HBoV | 12(9.4) | 7(12.5) | 5(6.9) | 0.616 |
| HCoV-OC43 | 8(6.3) | 4(7.1) | 4(5.6) | 0.947 |
| HMPV | 6(4.7) | 4(7.1) | 2(2.8) | 0.446 |
| infB | 3(2.3) | 0(0) | 3(4.2) | -c |
| PIV3 | 3(2.3) | 2(3.6) | 1(1.4) | - |
| CP | 3(2.3) | 0(0) | 3(4.2) | - |
| PIV1 | 2(1.6) | 0(0) | 2(2.8) | - |
| PIV4 | 2(1.6) | 0(0) | 2(2.8) | - |
| HCoV-HKU1 | 2(1.6) | 0(0) | 2(2.8) | - |
| HCoV-229E | 1(0.8) | 0(0) | 1(1.4) | - |
| PIV2 | 0(0) | 0(0) | 0(0) | - |
| HCoV-NL63 | 0(0) | 0(0) | 0(0) | - |
Note: Data are number (%) in each group, except where specifically stated.
a RSV-positive patients were tested for 17 common respiratory pathogens.
b Two-tailed χ2 test, comparing the copathogen distribution between RSV-A-positive and RSV-B-positive patients.
c Not done because the number of positive samples obtained was small.
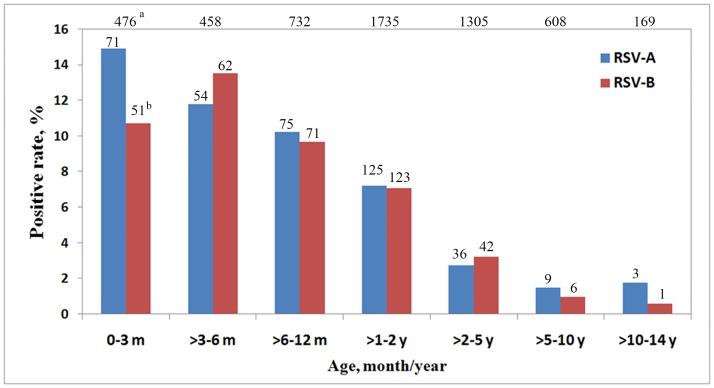
In this study, 710 of the 729 (97.4%) RSV-positive patients were children under 5 years old (p < 0.001), and 632 of the 729 (86.7%; p < 0.001) patients were under 2 years old. When the patients were divided into seven groups by age, the detection rate peaks for RSV-A and RSV-B occurred in patients aged 0–3 months (14.9%, 71/476) and >3–6 months (14.9%, 62/458), respectively, and the frequencies then declined with age (Fig 1).
Fig 1. Age distributions of patients with RSV-A and RSV-B.
aTotal number of patients in each age group; bThe number of RSV-A or RSV-B positive patients in each age group; m: month(s); y: year(s).
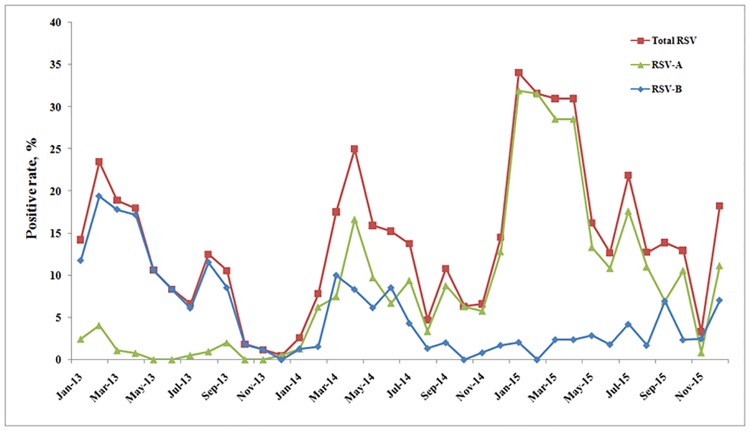
In general, the frequency of RSV infections peaked twice every year (Fig 2). Large peaks in the RSV detection rate occurred in February 2013 (23.5%, 23/98), April 2014 (25%, 66/264), and January 2015 (34.0%, 33/97). Small peaks in the RSV detection rates occurred in August 2013 (12.5%, 26/208), September 2014 (10.8%, 16/148), and July 2015 (21.8%, 26/119). RSV-B circulated predominantly in 2013 and RSV-A in 2015, whereas in 2014, RSV-B and RSV-A cocirculated (Fig 2).
Fig 2. Seasonal distribution of RSV subgroups in pediatric patients hospitalized with acute respiratory-tract illness over a 3-year period.
Note: Total RSV, sum of RSV-A and RSV-B; no patients were coinfected with RSV-A and RSV-B.
Distribution of clinical presentations in RSV-A- and RSV-B-positive patients
We analyzed the clinical presentations of 645 of the 729 (88.5%) RSV-positive patients. Patients with incomplete clinical data were excluded from this analysis. We compared the clinical characteristics of the RSV-A- and RSV-B-positive patients, the characteristics of single RSV infections and coinfections, and the characteristics of patients with different CVLs (Table 3).
Table 3. Clinical presentations in RSV-positive patients.
| Patients with RSV-A and RSV-B | Patients with single RSV-A and co-pathogens | Patients with different comparative viral loadd | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | RSV-A (n = 327) | RSV-B (n = 318) | p valueb | Single RSV (n = 540) | Co-pathogens(n = 105) | p valuec | <1 (n = 269) | 1–8 (n = 228) | 8–64 (116) | >64 (n = 32) | p valuee |
| URTI | |||||||||||
| Nasal obstruction | 125(38.2) | 107(33.6) | 0.226 | 200(37) | 32(30.5) | 0.2 | 105(39) | 82(36) | 36(31) | 10(31.3) | 0.454 |
| Coryza | 164(50.2) | 111(34.9) | <0.001 | 230(42.6) | 45(42.9) | 0.96 | 122(45.4) | 100(43.9) | 44(37.9) | 9(28.1) | 0.191 |
| Sneeze | 6(1.8) | 5(1.6) | 0.797 | 10(1.9) | 1(1) | 0.515 | 6(2.2) | 4(1.8) | 1(0.9) | 0(0) | 0.684 |
| Cough | 323(98.8) | 307(96.5) | 0.06 | 528(97.8) | 102(97.1) | 0.693 | 265(98.5) | 219(96.1) | 114(98.3) | 32(100) | 0.22 |
| Expectoration | 47(14.4) | 53(16.7) | 0.421 | 82(15.2) | 18(17.1) | 0.612 | 37(13.8) | 39(17.1) | 22(19) | 2(6.3) | 0.238 |
| Pharyngeal discomfort | 2(0.6) | 1(0.3) | 0.579 | 3(0.6) | 0(0) | 0.444 | 1(0.4) | 2(0.9) | 0(0) | 0(0) | 0.664 |
| Hoarseness | 4(1.2) | 3(0.9) | 0.732 | 6(1.1) | 1(1) | 0.886 | 3(1.1) | 1(0.4) | 3(2.6) | 0(0) | 0.229 |
| LRTI | |||||||||||
| Abnormal pulmonary breath sound a | 322(98.5) | 310(97.5) | 0.373 | 528(97.8) | 104(99) | 0.397 | 266(98.9) | 224(98.2) | 112(96.6) | 30(93.8) | 0.151 |
| Dyspnoea | 211(64.5) | 181(56.9) | 0.048 | 323(59.8) | 69(65.7) | 0.257 | 164(61) | 137(60.1) | 67(57.8) | 24(75) | 0.361 |
| Increasing lung markings | 40(12.2) | 38(11.9) | 0.912 | 64(11.9) | 14(13.3) | 0.67 | 38(14.1) | 24(10.5) | 13(11.2) | 3(9.4) | 0.598 |
| Bronchiolitis | 189(57.8) | 125(39.3) | <0.001 | 274(50.7) | 40(38.1) | 0.018 | 148(55) | 107(46.9) | 50(43.1) | 9(28.1) | 0.009 |
| Pneumonia | 22(6.7) | 14(4.4) | 0.198 | 28(5.2) | 8(7.6) | 0.32 | 15(5.6) | 14(6.1) | 6(5.2) | 1(3.1) | 0.91 |
| Systemic influenza-like symptoms | |||||||||||
| Fever (≥38°C) | 229(70) | 230(72.3) | 0.52 | 393(72.8) | 66(62.9) | 0.04 | 211(78.4) | 155(68) | 77(66.4) | 16(50) | 0.001 |
| Chill | 12(3.7) | 27(8.5) | 0.01 | 36(6.7) | 3(2.9) | 0.134 | 14(5.2) | 16(7) | 8(6.9) | 1(3.1) | 0.719 |
| Dizziness | 2(0.6) | 4(1.3) | 0.393 | 5(0.9) | 1(1) | 0.979 | 3(1.1) | 1(0.4) | 1(0.9) | 1(3.1) | 0.498 |
| Headache | 2(0.6) | 12(3.8) | 0.006 | 12(2.2) | 2(1.9) | 0.838 | 4(1.5) | 5(2.2) | 4(3.4) | 1(3.1) | 0.655 |
| Myalgia | 1(0.3) | 12(3.8) | 0.002 | 11(2) | 2(1.9) | 0.93 | 2(0.7) | 6(2.6) | 4(3.4) | 1(3.1) | 0.256 |
| Debilitation | 2(0.6) | 12(3.8) | 0.006 | 12(2.2) | 2(1.9) | 0.838 | 3(1.1) | 6(2.6) | 4(3.4) | 1(3.1) | 0.446 |
| Gastrointestinal illness | |||||||||||
| Vomiting | 79(24.2) | 45(14.2) | 0.001 | 109(20.2) | 15(14.3) | 0.16 | 51(19) | 48(21.1) | 22(19) | 3(9.4) | 0.474 |
| Poor appetite | 121(37) | 72(22.6) | <0.001 | 172(31.9) | 21(20) | 0.015 | 89(33.1) | 63(27.6) | 35(30.2) | 6(18.8) | 0.288 |
| Diarrhoea | 50(15.3) | 26(8.2) | 0.005 | 68(12.6) | 8(7.6) | 0.148 | 32(11.9) | 26(11.4) | 14(12.1) | 4(12.5) | 0.996 |
| Neurologic symptom | |||||||||||
| Convulsion | 10(3.1) | 8(2.5) | 0.676 | 15(2.8) | 3(2.9) | 0.964 | 7(2.6) | 7(3.1) | 3(2.6) | 1(3.1) | 0.988 |
| Others | |||||||||||
| Rash etc | 3(0.9) | 31(9.7) | <0.001 | 22(4.1) | 12(11.4) | 0.002 | 9(3.3) | 10(4.4) | 11(9.5) | 4(12.5) | 0.02 |
Note: Data are number (%) in each group, except where specifically stated. Percentages sum to over 100% because some patients had more than one diagnosis.
a Including phlegmatic rales, wheezing rales, bubbling rales, and moist rales.
b Two-tailed χ2 test, comparing the distribution of each illness or diagnosis between the RSV-A-positive and RSV-B-positive patients.
c Two-tailed χ2 test, comparing the distribution of each illness or diagnosis between patients singly infected with RSV and coinfected patients.
d Comparative viral loads of RSV-A and RSV-B were calculated by dividing the viral load by the copies of human ACTB mRNA, which were calculated from standard curves, and used as comparative quantities for analysis.
e Two-tailed χ2 test, comparing the distribution of each illness or diagnosis in patients with different comparative viral loads.
Significant differences were found between the RSV-A- and RSV-B-positive patients in the frequency of coryza (p < 0.001), dyspnea (p = 0.048), bronchiolitis (p < 0.001), chill (p = 0.01), headache (p = 0.006), myalgia (p = 0.002), debility (p = 0.006), vomiting (p = 0.001), poor appetite (p < 0.001), diarrhea (p = 0.005), and rash etc. (p < 0.001) (Table 3).
There were significant differences in the clinical characteristics of patients solely infected with RSV (RSV-A or RSV-B) and those coinfected, in the frequencies of bronchiolitis (p = 0.018), fever (≥ 38°C) (p = 0.04), poor appetite (p = 0.015), and rash etc. (p = 0.002) (Table 3).
In this study, CVL was divided into four levels: < 1, 1–8, 8–64, and > 64. Significant differences in the clinical characteristics of patients with different CVLs were found for bronchiolitis (p = 0.009), in which 55% of patients (148/269) were CVL < 1, 46.9% (107/228) were CVL = 1–8, 43.1% (50/116) were CVL = 8–64, and 28.1% (9/32) were CVL > 64; fever (≥ 38°C) (p = 0.001), in which 78.4% (211/269) were CVL < 1, 68% (155/228) were CVL = 1–8, 66.4% (77/116) were CVL = 8–64, and 50% (16/32) were CVL > 64; and rash etc. (p = 0.02), in which 3.3% (9/269) were CVL < 1, 4.4% (10/228) were CVL = 1–8, 9.5% (11/116) were CVL = 8–64, and 12.5% (4/32) were CVL > 64 (Table 3).
Discussion
RSV is one of the most important pathogenic infections of children and is associated with significant morbidity and mortality [18–20]. RSV infection is a global epidemic, imposing a high public-health burden, and circulates with different patterns in different areas [21, 22]. Therefore, research into the epidemiological behavior of RSV, especially in developing countries, is essential. In this study, we analyzed the epidemiological characteristics of RSV-A and RSV-B infections in pediatric patients (≤ 14 years old) hospitalized with respiratory illness in Guangzhou, China over a 3-year period, using our newly established multiplex real-time PCR.
In this study, the multiplex real-time PCR amplified the G gene conserved in and specific to RSV-A and RSV-B and the human ACTB gene. The specificity and sensitivity of the method were analyzed. No nonspecific reactions were observed, and good linear relationships were observed for the three target genes. Parallel standard curves (with almost the same slopes) increased the quality of the CVL calculation.
In this 3-year study, 13.3% (729/5483) of patients were RSV positive, most were children under 2 years old (86.7%, 632/729) (p < 0.001), and more male patients than female patients were infected with RSV (p < 0.001) (Fig 1). This distribution is consistent with previous reports of RSV in both developed and developing countries [3, 23, 24]. The prevalences of RSV-A (51.2%, 373/729) and RSV-B (48.8%, 356/729) were similar in this study, and showed the same tendencies with age, insofar as most positive patients under 2 years old (Fig 1). The pattern in the seasonal distributions of RSV-A and RSV-B was found. RSV-B was the dominant subtype in 2013, RSV-A was dominant in 2015, and RSV-A and RSV-B cocirculated in 2014 (Fig 2). RSV is known to occur in well-defined recurrent epidemics during the cold season in temperate climates [2], whereas in tropical and subtropical areas, RSV infections are reported to peak more often in the wet season. However, locations close to the equator show less consistent patterns, some with almost continuous RSV activity and varying seasonal peaks [25]. In this study, two seasonal peaks of RSV occurred at the changes of seasons from winter to spring and from summer to autumn. This pattern is similar to the previous report [24].
Copathogens were common (17.6%, 128/729) and diverse (88.2%, 15/17) in the RSV-positive patients, as reported previously [2, 26–29], and the most frequently detected copathogens were RV, InfA, EV, MP, ADV, HBoV, and HCoV-OC43, which all occurred at rates > 5% (Table 2). When we compared the clinical presentations of patients with single RSV infections and those with coinfections, more bronchiolitis (p = 0.018), fever (≥ 38°C) (p = 0.04), and poor appetite (p = 0.015) were present in the singly infected patients than in the co-infected patients, suggesting the key pathogenic activity of RSV. On the contrary, more rash etc. (p = 0.002) was observed in the co-infected patients than in those with single RSV infections, indicating the nonmainstream activity of rash etc. in patients with RSV infection (Table 3). However, the knowledge of viral–viral interactions in vivo are poorly understood, and the clinical relevance of the infection of copathogens in these patients and their association with severe illness are unclear [26, 29].
RSV infection has a large spectrum of clinical manifestations, ranging from URTI to LRTI. In this study, we analyzed the clinical presentations of 645 RSV-positive patients (Table 3). The relationships between the clinical characteristics and the RSV subgroups (RSV-A, RSV-B) differed from previously reported results. Some studies found no differences in the symptoms of patients infected with the two RSV subtypes [30–32]. However, some reported that RSV-A was associated with a more-severe clinical disease [33–35], whereas in other studies, RSV-B infections were reported to cause more severe disease [36, 37]. In this study, the LRTIs bronchiolitis (p < 0.001) and dyspnea (p = 0.048), the URTI coryza (p < 0.001), and the gastrointestinal illnesses vomiting (p = 0.001), poor appetite (p < 0.001), and diarrhea (p = 0.005) were more frequently found in the RSV-A-positive patients than in the RSV-B-positive patients. However, the systemic influenza-like symptoms chill (p = 0.01), headache (p = 0.006), myalgia (p = 0.002), and debility (p = 0.006), and rash etc. (p < 0.001) were found more frequently in the RSV-B-positive patients than in the RSV-A-positive patients (Table 3). These data suggest specific clinical presentations for RSV-A and RSV-B infections, and provide clues for the diagnosis and clinical distinction of the different RSV subtypes.
Many factors affect the clinical manifestations of patients, including the infectious organism, environment, nutrition, and socioeconomic status. Viral infections are an important issue that attracts much research attention, and one focus of research is the relationship between the viral load and disease progression or the sensitivity of the disease. In the study of patients chronically infected with the hepatitis B virus, monitoring the homogeneous serum hepatitis B viral DNA levels with sensitive, absolutely quantitative real-time PCR assays is strongly recommended for the management of patients [38]. However, it is still challenging to quantify respiratory viruses in respiratory-tract specimens. Whether the RSV load correlates with disease severity remains controversial, because some previous analyses of hospitalized children have shown a significant association [15, 39–41], whereas others have not [42, 43]. The virus was quantified with quantitative RT–PCR, plaque assay, or both in these studies. However, the initial quality of the samples influences their subsequent analysis, and it is difficult to control how many valid cells can be obtained from the respiratory tract. To exclude the effects of sampling, a comparative quantitative analysis of viral load should be used for respiratory specimens to evaluate drug efficacy, therapeutic effects, etc.
In this study, we established a multiplex real-time PCR that included the housekeeping gene, human ACTB. The detection of human ACTB was used first to monitor the quality of sampling, and secondly, as a baseline for the calculation of viral load in the respiratory specimens. We thus made a limited attempt to analyze the association between CVL and clinical presentation. RSV (-A or -B) and human ACTB were quantified with a standard curve for each. The CVL was then calculated and used for the analysis. In this study, CVL was divided into four levels: < 1, 1–8, 8–64, and > 64. Significant differences were found in bronchiolitis (p = 0.009) and fever (≥ 38°C) (p = 0.001) according to the CVL, with the frequencies declining as the CVL increased (Table 3). The peak frequencies of bronchiolitis and fever occurred in low-CVL patients, which might attributable to the combined effects of the lung damage caused by the virus, the host immunopathological effect, the replication/clearance of the virus, the progression of the disease, etc. [44–46]. In the advanced stage of RSV infection, virus is gradually cleared, and immunopathological effect becomes the more important influence factor. While the disease progressions of the patients before hospitalization, like the onset of disease, were not recorded clearly, the shortcoming made it hard to analyze deeply, and more mechanism study must be done to uncover the inner relationship.
Significant differences were also seen in the frequency of rash etc. (p = 0.02), which increased as CVL increased (Table 3). However, other factors or pathogens might be responsible for this trend because rash occurred more often in patients with co-pathogen infections than in those with single RSV infections (p = 0.002) (Table 3).
In this work, a novel rapid method for detecting RSV subgroups was established, and the epidemiology and clinical manifestations of RSV infection in Guangzhou, China were analyzed. CVL was used as the comparative quantity in the analysis, while more studies, especially mechanism studies and longitudinal studies, should investigate the feasibility of new CVL evaluation methods, similar to the preliminary attempt made in this cross-sectional study.
Acknowledgments
We thank the study volunteers for their generous participation. We thank Haiping Huang, Jing Zhang, Jing Ma for technical assistance.
Data Availability
Data are available from the State Key Laboratory of Respiratory Diseases for researchers who meet the criteria for access to confidential data, Please contact with Rong Zhou (e-mail: zhourong@gird.cn; Tel.: +86 20 34282614) for details.
Funding Statement
This study was supported by Guangzhou Science and Technology Program key projects (RZ) (201508020252) (http://www.gzsi.gov.cn/), Guangzhou Science and Technology Program key projects (XL) (201504010032) (http://www.gzsi.gov.cn/), National Natural Science Foundation of China (WKL) (31500143) (http://www.nsfc.gov.cn/). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Cane PA. Molecular epidemiology of respiratory syncytial virus. Rev Med Virol. 2001;11(2):103–16. Epub 2001/03/23. 10.1002/rmv.305 [pii]. . [DOI] [PubMed] [Google Scholar]
- 2.Borchers AT, Chang C, Gershwin ME, Gershwin LJ. Respiratory syncytial virus—a comprehensive review. Clin Rev Allergy Immunol. 2013;45(3):331–79. Epub 2013/04/12. 10.1007/s12016-013-8368-9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pavia AT. Viral infections of the lower respiratory tract: old viruses, new viruses, and the role of diagnosis. Clin Infect Dis. 2011;52 Suppl 4:S284–9. Epub 2011/04/06. 10.1093/cid/cir043 cir043 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Papenburg J, Boivin G. The distinguishing features of human metapneumovirus and respiratory syncytial virus. Rev Med Virol. 2010;20(4):245–60. Epub 2010/06/30. 10.1002/rmv.651 . [DOI] [PubMed] [Google Scholar]
- 5.Salimi V, Tavakoli-Yaraki M, Yavarian J, Bont L, Mokhtari-Azad T. Prevalence of human respiratory syncytial virus circulating in Iran. J Infect Public Health. 2015. Epub 2015/07/06. S1876-0341(15)00102-1 [pii] 10.1016/j.jiph.2015.05.005 . [DOI] [PubMed] [Google Scholar]
- 6.Hirsh S, Hindiyeh M, Kolet L, Regev L, Sherbany H, Yaary K, et al. Epidemiological changes of respiratory syncytial virus (RSV) infections in Israel. PLoS One. 2014;9(3):e90515 Epub 2014/03/07. 10.1371/journal.pone.0090515 PONE-D-13-35880 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hendry RM, Godfrey E, Anderson LJ, Fernie BF, McIntosh K. Quantification of respiratory syncytial virus polypeptides in nasal secretions by monoclonal antibodies. J Gen Virol. 1985;66 (Pt 8):1705–14. Epub 1985/08/01. 10.1099/0022-1317-66-8-1705 . [DOI] [PubMed] [Google Scholar]
- 8.Tsutsumi H, Onuma M, Suga K, Honjo T, Chiba Y, Chiba S, et al. Occurrence of respiratory syncytial virus subgroup A and B strains in Japan, 1980 to 1987. J Clin Microbiol. 1988;26(6):1171–4. Epub 1988/06/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mufson MA, Orvell C, Rafnar B, Norrby E. Two distinct subtypes of human respiratory syncytial virus. J Gen Virol. 1985;66 (Pt 10):2111–24. Epub 1985/10/01. 10.1099/0022-1317-66-10-2111 . [DOI] [PubMed] [Google Scholar]
- 10.Sullender WM. Respiratory syncytial virus genetic and antigenic diversity. Clin Microbiol Rev. 2000;13(1):1–15, table of contents. Epub 2000/01/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gilca R, De Serres G, Tremblay M, Vachon ML, Leblanc E, Bergeron MG, et al. Distribution and clinical impact of human respiratory syncytial virus genotypes in hospitalized children over 2 winter seasons. J Infect Dis. 2006;193(1):54–8. Epub 2005/12/03. JID34543 [pii] 10.1086/498526 . [DOI] [PubMed] [Google Scholar]
- 12.Imaz MS, Sequeira MD, Videla C, Veronessi I, Cociglio R, Zerbini E, et al. Clinical and epidemiologic characteristics of respiratory syncytial virus subgroups A and B infections in Santa Fe, Argentina. J Med Virol. 2000;61(1):76–80. Epub 2000/04/04. [pii]. . [DOI] [PubMed] [Google Scholar]
- 13.Gottschalk J, Zbinden R, Kaempf L, Heinzer I. Discrimination of respiratory syncytial virus subgroups A and B by reverse transcription-PCR. J Clin Microbiol. 1996;34(1):41–3. Epub 1996/01/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaunt ER, Hardie A, Claas EC, Simmonds P, Templeton KE. Epidemiology and clinical presentations of the four human coronaviruses 229E, HKU1, NL63, and OC43 detected over 3 years using a novel multiplex real-time PCR method. J Clin Microbiol. 2010;48(8):2940–7. Epub 2010/06/18. 10.1128/JCM.00636-10 JCM.00636-10 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.El Saleeby CM, Bush AJ, Harrison LM, Aitken JA, Devincenzo JP. Respiratory syncytial virus load, viral dynamics, and disease severity in previously healthy naturally infected children. J Infect Dis. 2011;204(7):996–1002. Epub 2011/09/02. 10.1093/infdis/jir494 jir494 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu WK, Liu Q, Chen DH, Liang HX, Chen XK, Huang WB, et al. Epidemiology and clinical presentation of the four human parainfluenza virus types. BMC Infect Dis. 2013;13:28 Epub 2013/01/25. 10.1186/1471-2334-13-28 1471-2334-13-28 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu WK, Liu Q, Chen de H, Liang HX, Chen XK, Chen MX, et al. Epidemiology of acute respiratory infections in children in guangzhou: a three-year study. PLoS One. 2014;9(5):e96674 Epub 2014/05/07. 10.1371/journal.pone.0096674 PONE-D-13-48629 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mazur NI, Martinon-Torres F, Baraldi E, Fauroux B, Greenough A, Heikkinen T, et al. Lower respiratory tract infection caused by respiratory syncytial virus: current management and new therapeutics. Lancet Respir Med. 2015. Epub 2015/09/29. S2213-2600(15)00255-6 [pii] 10.1016/S2213-2600(15)00255-6 . [DOI] [PubMed] [Google Scholar]
- 19.Abraha HY, Lanctot KL, Paes B. Risk of respiratory syncytial virus infection in preterm infants: reviewing the need for prevention. Expert Rev Respir Med. 2015:1–21. Epub 2015/10/13. 10.1586/17476348.2015.1098536 . [DOI] [PubMed] [Google Scholar]
- 20.Smyth RL, Openshaw PJ. Bronchiolitis. Lancet. 2006;368(9532):312–22. Epub 2006/07/25. S0140-6736(06)69077-6 [pii] 10.1016/S0140-6736(06)69077-6 . [DOI] [PubMed] [Google Scholar]
- 21.Hall CB, Weinberg GA, Iwane MK, Blumkin AK, Edwards KM, Staat MA, et al. The burden of respiratory syncytial virus infection in young children. N Engl J Med. 2009;360(6):588–98. Epub 2009/02/07. 10.1056/NEJMoa0804877 360/6/588 [pii]. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haynes AK, Manangan AP, Iwane MK, Sturm-Ramirez K, Homaira N, Brooks WA, et al. Respiratory syncytial virus circulation in seven countries with Global Disease Detection Regional Centers. J Infect Dis. 2013;208 Suppl 3:S246–54. Epub 2013/12/07. 10.1093/infdis/jit515 jit515 [pii]. . [DOI] [PubMed] [Google Scholar]
- 23.Abzug MJ, Beam AC, Gyorkos EA, Levin MJ. Viral pneumonia in the first month of life. Pediatr Infect Dis J. 1990;9(12):881–5. Epub 1990/12/01. . [DOI] [PubMed] [Google Scholar]
- 24.Mathisen M, Strand TA, Sharma BN, Chandyo RK, Valentiner-Branth P, Basnet S, et al. RNA viruses in community-acquired childhood pneumonia in semi-urban Nepal; a cross-sectional study. BMC Med. 2009;7:35 Epub 2009/07/29. 10.1186/1741-7015-7-35 1741-7015-7-35 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weber MW, Mulholland EK, Greenwood BM. Respiratory syncytial virus infection in tropical and developing countries. Trop Med Int Health. 1998;3(4):268–80. Epub 1998/06/12. . [DOI] [PubMed] [Google Scholar]
- 26.Jennings LC, Anderson TP, Werno AM, Beynon KA, Murdoch DR. Viral etiology of acute respiratory tract infections in children presenting to hospital: role of polymerase chain reaction and demonstration of multiple infections. Pediatr Infect Dis J. 2004;23(11):1003–7. Epub 2004/11/17. 00006454-200411000-00007 [pii]. . [DOI] [PubMed] [Google Scholar]
- 27.Calvo C, Garcia-Garcia ML, Blanco C, Vazquez MC, Frias ME, Perez-Brena P, et al. Multiple simultaneous viral infections in infants with acute respiratory tract infections in Spain. J Clin Virol. 2008;42(3):268–72. Epub 2008/05/06. 10.1016/j.jcv.2008.03.012 S1386-6532(08)00108-X [pii]. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Midulla F, Scagnolari C, Bonci E, Pierangeli A, Antonelli G, De Angelis D, et al. Respiratory syncytial virus, human bocavirus and rhinovirus bronchiolitis in infants. Arch Dis Child. 2010;95(1):35–41. Epub 2009/10/14. 10.1136/adc.2008.153361 adc.2008.153361 [pii]. . [DOI] [PubMed] [Google Scholar]
- 29.Ruuskanen O, Lahti E, Jennings L, Murdoch D. Viral pneumonia. Lancet. 2011;377(9773):1264–75. 10.1016/S0140-6736(10)61459-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hendry RM, Talis AL, Godfrey E, Anderson LJ, Fernie BF, McIntosh K. Concurrent circulation of antigenically distinct strains of respiratory syncytial virus during community outbreaks. J Infect Dis. 1986;153(2):291–7. Epub 1986/02/01. . [DOI] [PubMed] [Google Scholar]
- 31.McIntosh ED, De Silva LM, Oates RK. Clinical severity of respiratory syncytial virus group A and B infection in Sydney, Australia. Pediatr Infect Dis J. 1993;12(10):815–9. Epub 1993/10/01. . [DOI] [PubMed] [Google Scholar]
- 32.Russi JC, Chiparelli H, Montano A, Etorena P, Hortal M. Respiratory syncytial virus subgroups and pneumonia in children. Lancet. 1989;2(8670):1039–40. Epub 1989/10/28. S0140-6736(89)91048-9 [pii]. . [DOI] [PubMed] [Google Scholar]
- 33.Hall CB, Walsh EE, Schnabel KC, Long CE, McConnochie KM, Hildreth SW, et al. Occurrence of groups A and B of respiratory syncytial virus over 15 years: associated epidemiologic and clinical characteristics in hospitalized and ambulatory children. J Infect Dis. 1990;162(6):1283–90. Epub 1990/12/01. . [DOI] [PubMed] [Google Scholar]
- 34.McConnochie KM, Hall CB, Walsh EE, Roghmann KJ. Variation in severity of respiratory syncytial virus infections with subtype. J Pediatr. 1990;117(1 Pt 1):52–62. Epub 1990/07/01. . [DOI] [PubMed] [Google Scholar]
- 35.Jafri HS, Wu X, Makari D, Henrickson KJ. Distribution of respiratory syncytial virus subtypes A and B among infants presenting to the emergency department with lower respiratory tract infection or apnea. Pediatr Infect Dis J. 2013;32(4):335–40. Epub 2013/01/23. 10.1097/INF.0b013e318282603a . [DOI] [PubMed] [Google Scholar]
- 36.Hornsleth A, Klug B, Nir M, Johansen J, Hansen KS, Christensen LS, et al. Severity of respiratory syncytial virus disease related to type and genotype of virus and to cytokine values in nasopharyngeal secretions. Pediatr Infect Dis J. 1998;17(12):1114–21. Epub 1999/01/07. . [DOI] [PubMed] [Google Scholar]
- 37.Tran DN, Pham TM, Ha MT, Tran TT, Dang TK, Yoshida LM, et al. Molecular epidemiology and disease severity of human respiratory syncytial virus in Vietnam. PLoS One. 2013;8(1):e45436 Epub 2013/01/26. 10.1371/journal.pone.0045436 PONE-D-12-19390 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Caliendo AM, Valsamakis A, Bremer JW, Ferreira-Gonzalez A, Granger S, Sabatini L, et al. Multilaboratory evaluation of real-time PCR tests for hepatitis B virus DNA quantification. J Clin Microbiol. 2011;49(8):2854–8. Epub 2011/06/24. 10.1128/JCM.00471-11 JCM.00471-11 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fodha I, Vabret A, Ghedira L, Seboui H, Chouchane S, Dewar J, et al. Respiratory syncytial virus infections in hospitalized infants: association between viral load, virus subgroup, and disease severity. J Med Virol. 2007;79(12):1951–8. Epub 2007/10/16. 10.1002/jmv.21026 . [DOI] [PubMed] [Google Scholar]
- 40.Buckingham SC, Bush AJ, Devincenzo JP. Nasal quantity of respiratory syncytical virus correlates with disease severity in hospitalized infants. Pediatr Infect Dis J. 2000;19(2):113–7. Epub 2000/02/29. . [DOI] [PubMed] [Google Scholar]
- 41.DeVincenzo JP, El Saleeby CM, Bush AJ. Respiratory syncytial virus load predicts disease severity in previously healthy infants. J Infect Dis. 2005;191(11):1861–8. Epub 2005/05/05. JID33894 [pii] 10.1086/430008 . [DOI] [PubMed] [Google Scholar]
- 42.Semple MG, Dankert HM, Ebrahimi B, Correia JB, Booth JA, Stewart JP, et al. Severe respiratory syncytial virus bronchiolitis in infants is associated with reduced airway interferon gamma and substance P. PLoS One. 2007;2(10):e1038 Epub 2007/10/18. 10.1371/journal.pone.0001038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wright PF, Gruber WC, Peters M, Reed G, Zhu Y, Robinson F, et al. Illness severity, viral shedding, and antibody responses in infants hospitalized with bronchiolitis caused by respiratory syncytial virus. J Infect Dis. 2002;185(8):1011–8. Epub 2002/04/04. JID010815 [pii] 10.1086/339822 . [DOI] [PubMed] [Google Scholar]
- 44.Legg JP, Hussain IR, Warner JA, Johnston SL, Warner JO. Type 1 and type 2 cytokine imbalance in acute respiratory syncytial virus bronchiolitis. Am J Respir Crit Care Med. 2003;168(6):633–9. Epub 2003/05/30. 10.1164/rccm.200210-1148OC 200210-1148OC [pii]. . [DOI] [PubMed] [Google Scholar]
- 45.Polack FP, Teng MN, Collins PL, Prince GA, Exner M, Regele H, et al. A role for immune complexes in enhanced respiratory syncytial virus disease. J Exp Med. 2002;196(6):859–65. Epub 2002/09/18. 10.1084/jem.20020781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hall CB, Douglas RG Jr., Schnabel KC, Geiman JM. Infectivity of respiratory syncytial virus by various routes of inoculation. Infect Immun. 1981;33(3):779–83. Epub 1981/09/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the State Key Laboratory of Respiratory Diseases for researchers who meet the criteria for access to confidential data, Please contact with Rong Zhou (e-mail: zhourong@gird.cn; Tel.: +86 20 34282614) for details.