Abstract
Background
Various prevalence figures have been reported for inter-arm differences in blood pressure (IAD); variation may be explained by differing population vascular risk and by measurement method.
Aim
To review the literature to derive robust estimates of IAD prevalence relevant to community populations.
Design and setting
Systematic review and meta-analysis.
Method
MEDLINE, Embase, and CINAHL were searched for cross-sectional studies likely to represent general or primary care populations, reporting prevalence of IAD and employing a simultaneous method of measurement. Using study-level data, pooled estimates of mean prevalence of systolic IADs were calculated and compared using a random effects model.
Results
Eighty IAD studies were identified. Sixteen met inclusion criteria: pooled estimates of prevalence for systolic IAD ≥10 mmHg were 11.2% (95% confidence interval [CI] = 9.1 to 13.6) in hypertension, 7.4% (95% CI = 5.8 to 9.2) in diabetes, and 3.6% (95% CI = 2.3 to 5.0) for a general adult population (P<0.001 for subgroup differences). Differences persisted for higher cut-off values. Prevalences were lower for East Asian than for Western populations and were overestimated by sequential measurement where this could be compared with simultaneous measurement within studies (relative risk for IAD: 2.9 [95% CI = 2.1 to 4.1]). Studies with higher mean absolute systolic pressures had higher prevalences for a systolic IAD ≥10 mmHg (P = 0.04).
Conclusion
Prevalences of IADs rise in relation to underlying cardiovascular comorbidities of the population studied, and are overestimated threefold when sequential measurement is used. Population-specific variation in prevalences of IAD should be taken into account in delivering clinical care and in planning future studies.
Keywords: blood pressure determination, hypertension, prevalence, inter-arm difference, primary care
INTRODUCTION
A difference in blood pressure measurements between arms has been reported in cohorts with hypertension,1–4 diabetes,5–7 chronic kidney disease,8,9 or peripheral arterial disease.10 Differences are also reported for populations free of chronic disease.6,11–15 Inter-arm differences in blood pressure can cause errors in blood pressure interpretation and management when not recognised;2,5,16–18 they are also associated with increased cardiovascular mortality and morbidity.19–21
The reported prevalences of inter-arm differences vary greatly; they are usually higher in the presence of hypertension.2,22,23 The majority of reports are based on selected or convenience samples, usually in a secondary care setting; fewer studies have addressed the subject in populations relevant to primary care.4,5,13,14,24 However, a recent systematic review indicated that prevalence figures are lower in community than in outpatient or inpatient hospital settings.25
Current guidelines advise that blood pressure should be checked in both arms when assessing patients for hypertension, but this is often not done by GPs.26,27 Knowledge of the prevalence of an inter-arm difference in primary or community care settings allows estimation of the frequency with which, for example, a blood pressure measurement may be underestimated by ≥10 mmHg — a clinically important error affecting diagnosis and treatment decisions — if a difference has not been excluded. It can also indicate the likely workload required to confirm the existence of suspected differences. Prevalence is overestimated when a robust repeated simultaneous measurement technique is not used,2,28 and current guidelines advise that such confirmation requires simultaneous assessment.26,29
This systematic review and meta-analysis was undertaken to derive estimates of the prevalence, measured by simultaneous assessment, of systolic inter-arm differences in populations relevant to primary care settings.
METHOD
MEDLINE, Embase, and CINAHL databases were searched from their respective commencement dates to 12 November 2014 using search terms refined from previous systematic reviews (Appendix 1).2,20 Further studies were identified from personal archives and checking of reference lists for included studies. Full texts were retrieved for any studies reporting on inter-arm differences in blood pressure. Studies were eligible for inclusion if they employed a repeated simultaneous blood pressure measurement protocol, and examined a population likely to represent a general practice or primary care population. No directly relevant quality assessment tool for included studies was identified. However, application of the inclusion criteria for the method of blood pressure measurement and sampling of the population ensured that study quality for the outcome of interest was standardised.
How this fits in
Reported prevalence figures for inter-arm differences in blood pressure vary greatly between studies. Much variation can be explained by different underlying population vascular risks. Relevant prevalence figures for primary care are not well described. This study presents robust estimates of inter-arm difference prevalence applicable to general practice populations. Community prevalences are lower than reported for hospital cohorts but rise in relation to the underlying cardiovascular comorbidities of the population studied. Prevalences are overestimated threefold when sequential measurement is used.
Study populations were classified as hypertensive, diabetic, or general. Cohorts were included within the general population category unless specifically selected by diabetic or hypertensive status, thus being considered representative of a general primary care population. Where mixed cohorts were reported, authors were contacted to clarify appropriate classification and request subgroup prevalence data.
Study-level prevalence data were extracted from included studies for systolic inter-arm differences ≥10 mmHg, ≥15 mmHg, and ≥20 mmHg. Pooled estimates of mean prevalences for systolic inter-arm differences ≥10 mmHg, ≥15 mmHg, and ≥20 mmHg were calculated and compared between populations using meta-analysis of proportions undertaken in Stata (version 12.1) with the ‘metaprop’ command. A random effects model was chosen due to potential clinical heterogeneity of included studies. Statistical heterogeneity was assessed using the I2 statistic and, where present, explored with sensitivity analyses based on ethnic origin, or methodology. Univariable and multivariable meta-regression analyses were undertaken to examine the association between various study-level factors (mean age, percentage of males, mean absolute systolic blood pressure, setting [community versus clinic], country of conduct, and indication [hypertensive versus diabetic versus general population]), and the prevalence for systolic inter-arm differences ≥10 mmHg. The ‘permute’ option for the ‘metareg’ command in Stata was used to allow for multiple testing.
Where studies also reported prevalence of blood pressure differences based on sequential measurements, these data were also extracted for comparison. Differences in aggregate study prevalence were estimated for the simultaneous versus sequential methods after adjustment for within-person correlations reported elsewhere,30 according to Cochrane Review methods.31,32 Results are expressed as relative risks of diagnosing an inter-arm difference for sequential versus simultaneous assessment and pooled using random effects meta-analysis. Potential publication bias was assessed using funnel plots and the Egger test.33
RESULTS
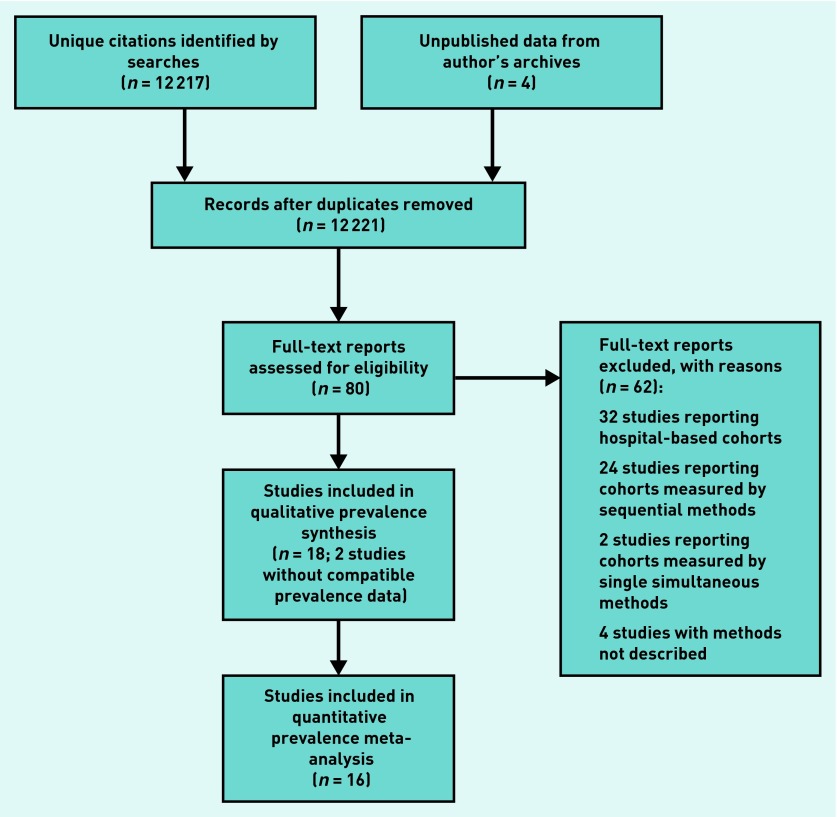
Searches identified 12 217 unique citations; 80 full texts were reviewed, and 18 studies met the inclusion criteria. One study reported no prevalence data in a form that could be included in the analysis,34 and another that rounded inter-arm differences to the nearest 5 mmHg was excluded.10 Thus 16 studies (comprising 21 subgroups) contributed data to the meta-analyses (Figure 1, Table 1).
Figure 1.
Flow chart of study.
Table 1.
Studies included in analyses
| Study (country of origin) | Study population | Method of measurement | Sample size | Prevalence of systolic differences |
|---|---|---|---|---|
| Harrison et al 196035 (US) | Patients attending clinic | Simultaneous three pairs of measurements | 447 | 5.3% ≥10 mmHg 0.1% ≥20 mmHg |
| Orme et al 199944 (UK) | Staff, visitors, and non-cardiovascular day case surgery patients at one district general hospital. Subjects without cardiovascular disease, mean age 49.1 years (20–89), 43% female |
Two automated machines in simultaneous 2 × 2 crossover design; mean of four pairs of readings | 364 | 5.2% ≥10 mmHg 0≥20 mmHg |
| Kimura et al 200436 (Japan) | Participants in community check-up for arteriosclerosis, age 62.4 years (11.1; 338 male, 702 female) | Simultaneous four-limb machine: ABI-form device (COLIN VP1000); single reading | 1090 | 9.1% >10 mmHg |
| Karagiannis et al 200517 (Greece) | Hospital staff, visitors, and patients, mean age 54 years (18.3), 195 (50.8%) female | Two Omron HEM 705CP in simultaneous 2 × 2 crossover design; mean of four pairs of readings | 384 | 3.4% >10 mmHg |
| Clark et al 20073 (UK)a | Primary care hypertensive patients, age 69.6 years (9.7), 40 male | Two Omron HEM 705CP in simultaneous 2 × 2 crossover design; mean of four pairs of readings | 94 | 19% ≥10 mmHg 6.4% ≥15 mmHg |
| Kleefstra et al 20077 (Netherlands) | Patients with type 2 diabetes mellitus | Mean of two simultaneous pairs of readings with 2 × Omron M5-1 automated machines | 169 | 9% ≥10 mmHg |
| Clark et al 20095 (UK)a | Subjects with type 2 diabetes mellitus recruited from five general practice surgeries | Two Omron HEM 705CP in simultaneous 2 × 2 crossover design; mean of four pairs of readings | 101 | 10% ≥10 mmHg 4% ≥15 mmHg |
| Lohmann et al 201137 (Germany) | Hospital outpatients with one or two cardiovascular risk factors; 76% hypertensive | Simultaneous Microlife WatchBP® Office; mean of three pairs of measurements | 118 | 10% ≥10 mmHg |
| Fonseca-Reyes et al 20121 (Mexico) | Patients attending hospital hypertension clinics | Two Omron HEM 725 CIC automatic sphygmomanometers, swapped after first pair of readings; mean of two pairs | 111 | 20.7% >5 mmHg 13.5% >10 mmHg 1.8% >20 mmHg |
| Kim 201343 (Korea) | Adult family medicine clinic patients age >40 years free of cardiovascular and renal disease, 200 (43%) with hypertension | Two pairs of simultaneous measurements with 2 × Omron MX3 | 261 males 203 females |
1.9% ≥10 mmHg 0% ≥10 mmHg |
| Okada et al 201341 (Japan) | Consecutive patients with type 2 diabetes in outpatient clinic | Simultaneous four-limb measurement (COLIN waveform analyser, device not stated). | 314 | 5.1% ≥10 mmHg |
| Sheng et al 201338 (China)a | Older Chinese (age >60 years), 1895 (60.5%) with hypertension and 285 (9.2%) with diabetes | Simultaneous four-limb machine; ABI-form device (COLIN VP1000) | 3133 | 6.4% ≥10 mmHg 1.8% ≥15 mmHg |
| Van der Hoeven et al 201345 (Netherlands)a | Staff patients and visitors to hypertension clinic comparing sequential and simultaneous measures; 132/240 (55%) with hypertension | Mean of three simultaneous repeated measures; Microlife Watch BP® Office |
240 | 11.7% ≥10 mmHg 5.0% ≥15 mmHg 1.6% ≥20 mmHg |
| Canepa et al 201342 (US) | Community sample free of diabetes, stroke, or heart disease at recruitment — the Baltimore Longitudinal Study of Ageing | Mean of second and third simultaneous pairs of readings with four-limb device COLIN VP2000 | 1045 | 4.8% ≥10 mmHg 1.1% ≥15 mmHg |
| Clark et al 2014a6 (UK)a | Community cohorts with and without diabetes recruited to the Diabetes Alliance for Research in England (DARE) | Two Omron HEM 705CP in simultaneous 2 × 2 crossover design; mean of four pairs of readings | 514 (diabetes) 286 (control) |
8.6% ≥10 mmHg 2.3% ≥15 mmHg 2.9% ≥10 mmHg 0.4% ≥15 mmHg |
| Clark et al 2014b40 (UK) | Community cohorts with and without diabetes and hypertension | Two Omron HEM 705CP in simultaneous 2 × 3 crossover design; mean of six pairs of readings | 265 (diabetes) 116 (control) |
5.2% ≥10 mmHg 0.8% ≥15 mmHg 0% ≥20 mmHg 5.2% ≥10 mmHg 2.6% ≥15 mmHg 0% ≥20 mmHg |
Published and unpublished data; all other studies published data only. ABI = ankle-brachial index.
Pooled prevalences of a systolic inter-arm difference ≥10 mmHg were 11.2% (95% confidence interval [CI] = 9.1 to 13.6) for seven populations with hypertension (3858 participants),1,3,35–39 7.4% (95% CI = 5.8 to 9.2) for six populations with diabetes (1648 participants),5–7,38,40,41 and 3.6% (95% CI = 2.3 to 5.0) for eight community-based groups without diabetes or hypertension (3751 participants)6,17,35,38,40,42–44 (P<0.001 for subgroup differences; Figure 2). Substantial statistical heterogeneity (I2 = 76%) was observed across studies in the general population group; there was a lower prevalence for the two cohorts of East Asian origin38,43 compared with the six Western groups, which accounted for heterogeneity in the latter but not the former (2.0% [95% CI = 1.4 to 2.8]; I2 = 83% versus 4.4% (95% CI = 3.5 to 5.5); I2 = 14%; P<0.001). Similarly, in the hypertensive population, prevalence was lower in the two East Asian cohorts (8.9% [95% CI = 7.9 to 9.9]; I2 = 77%)36,38 compared with the remaining Western populations (13.3% [95% CI = 11.0 to 15.7]; I2 = 6%; P<0.001 (Appendix 2, available from the authors on request). The corresponding prevalences for differences ≥15 mmHg were 4.0% (95% CI = 1.9 to 6.8) in hypertension (three cohorts; 2229 participants), 2.3% (95% CI = 1.1 to 3.9) in diabetes (four cohorts; 1165 participants), and 0.7% (95% CI = 0.1 to 1.5) without diabetes or hypertension (five cohorts; 2941 participants; P = 0.004 for subgroup differences). Prevalences were again lower for the one study of a Chinese population compared with the remaining Western cohorts. For differences ≥20 mmHg, prevalences were 1.0% (95% CI = 0.6 to 1.5) (three cohorts; 2229 participants), 0.4% (95% CI = 0 to 1.1) (four cohorts; 1165 participants), and 0.1% (95% CI = 0 to 0.4) (five cohorts; 2323 participants) respectively (P = 0.001); no statistical heterogeneity was observed (Appendix 2, available from the authors on request).
Figure 2.
Prevalence of systolic inter-arm differences ≥10 mmHg.
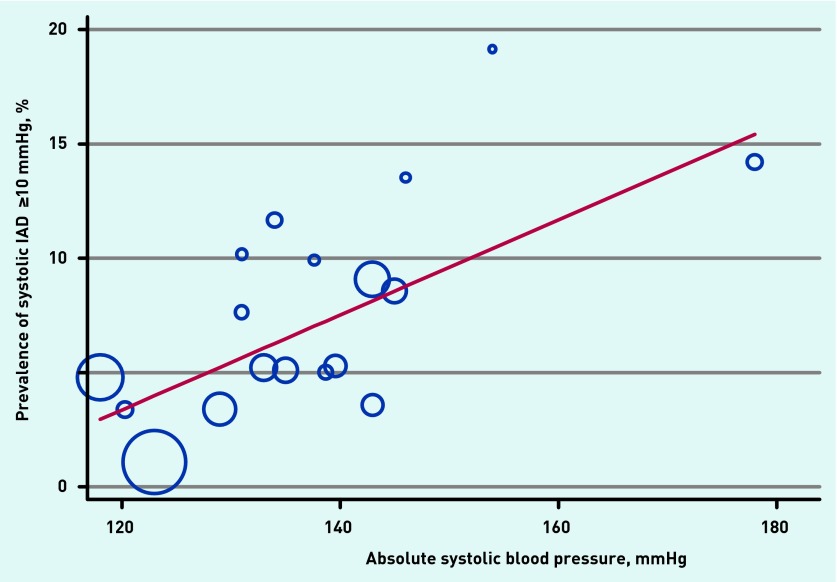
Univariable meta-regression showed two study-level factors to be associated with mean prevalence for systolic inter-arm differences ≥10 mmHg: health status (normotension versus diabetes versus hypertension) and absolute level of systolic blood pressure (Table 2). Each increase of 10 mmHg in absolute systolic blood pressure was associated with a 4% (95% CI = 0.9 to 4.0) increase in prevalence of an inter-arm difference ≥10 mmHg (Figure 3). Mean absolute systolic blood pressure increased across the health status groups (normotension 128 mmHg (standard deviation [SD] 7.4), diabetes 139 mmHg (SD 4.2), and hypertension 148 mmHg (SD 17); P = 0.02) indicating potential co-linearity of these two variables. Meta-regression of prevalence against health status after adjustment for absolute blood pressure was no longer significant, and no other study-level factors were found to be associated with inter-arm difference prevalence in multivariable analysis (Appendix 2, available from the authors on request).
Table 2.
Univariable and multivariable meta-regression analyses for systolic inter-arm blood pressure differences ≥10 mmHg
| Covariate | Univariable P-value | Multivariate modelaP-value |
|---|---|---|
| Health statusb | 0.012 | 0.509 |
| Absolute systolic blood pressure | 0.041 | 1.000 |
| Geographyc | 0.894 | 0.815 |
| Mean age | 0.668 | 0.998 |
| Percentage male | 0.497 | 1.000 |
| Settingd | 0.838 | 1.000 |
Adjusted for multiple testing.
Non-diabetic normotensive versus diabetic versus hypertensive.
Country of conduct.
Community versus clinic. P<0.05 significant.
Figure 3.
Study level association between mean systolic blood pressure and prevalence of systolic inter-arm differences ≥10 mmHg.
Five studies reported both simultaneously and sequentially measured prevalence data for systolic inter-arm differences ≥10 mmHg.7,35,37,42,45 Pooled analysis of data after adjustment for the paired nature of the data gave a prevalence of 6.4% (95% CI = 5.0 to 7.8) for measurement by a simultaneous method compared with 14.6% (95% CI = 12.5 to 16.6; P<0.001) for a sequential method; and a relative risk (RR) for diagnosis of an inter-arm difference by sequential compared with simultaneous measurement of ≥10 mmHg of 2.2 (95% CI = 1.1 to 4.5). Statistical heterogeneity between studies (I2 = 85%) was explained by a single study that reported a higher prevalence of inter-arm differences for simultaneous compared with sequential measurements,42 whereas all other studies reported lower prevalences for simultaneous measurements. This outlying study result was based on averaging the second and third pairs of readings, but sequentially measured prevalences were higher than simultaneous for each of the three individual pairs of measurements made. Sensitivity analysis by substituting the non-averaged data for this study accounted for the statistical heterogeneity (residual I2 = 37%; P = 0.17); the resulting RR was 2.9 (95% CI = 2.1 to 4.1).
Visual inspection of funnel plots suggested no publication bias through missing small studies reporting low inter-arm difference prevalences (Figure 4), and the Egger tests were not significant (P-values = 0.32, 0.26, and 0.75 for inter-arm differences ≥10 mmHg, 15 mmHg, and 20 mmHg respectively (Appendix 2, available from the authors on request).
Figure 4.
Funnel plot for prevalence of systolic inter-arm differences ≥10 mmHg.
DISCUSSION
Summary
This systematic review and meta-analysis presents a contemporary synthesis of estimates of the prevalence of systolic inter-arm differences in populations relevant to primary care. The prevalences of inter-arm difference rise in relation to cardiovascular comorbidity (such as diabetes and/or hypertension) in the population studied for all chosen cut-off values, and comparison with paired sequentially measured differences confirms that prevalence can be overestimated threefold when a simultaneous measurement method is not employed.
Strengths and limitations
This study builds on the authors’ previous reviews.2,20 The search terms are intentionally broad and therefore it is unlikely that important publications relevant to this review have been missed. The searches were supplemented with an author’s archives, contacts, and peer review activity.46,47 This meta-regression demonstrated the univariable association of rising absolute blood pressures and increasing inter-arm difference prevalences. This association did not persist on multivariable regression; however, there was co-linearity of blood pressure with clinical status. Given the relatively small number of included studies, these multivariate meta-regression analyses were potentially underpowered.
Comparison with existing literature
The prevalence figures reported here are lower than those previously reported in a previous study of hypertension (19.6% ≥10 mmHg [95% CI = 18.0 to 21.3];2 however, only four studies met that study’s inclusion criteria in 2006,23,35,44,48 and until recently there was a paucity of data truly representative of general community populations measured by simultaneous methods.6 There has been a rapid expansion of interest in inter-arm difference over the last decade;49 half of the 16 studies contributing to this review were published within the last 4 years.1,6,38,40–43,45 A number were included in the recent review by Singh and colleagues which confirmed that prevalence rates are lower for community-based cohorts compared with hospital data;25 that review reported a community prevalence for systolic differences ≥10 mmHg of 7.5% (95% CI = 5.6 to 9.4). However, their findings were based on only four cohorts,36,38,42,50 of which one study included 50% subjects with hypertension,36 another reported a mixed population (the lead author of which has provided additional subgroup data for the analyses reported here),38 and the third did not meet the inclusion criteria because it did not report repeated simultaneous measurements.50 Furthermore three studies from the authors’ own research group were misclassified in that review as outpatient studies and excluded from community prevalence analyses, despite correspondence with and provision of additional data to the review’s authors.3,5,6 These factors account for the erroneously high estimate of prevalence for the general population compared with the data presented here. Singh and colleagues also stated that community-based studies included in their review did not report data for systolic inter-arm differences ≥15 mmHg or ≥20 mmHg; data from five such studies are included in this report.6,35,38,40,44
The prevalence of an inter-arm difference in hypertension is higher at any cut-off compared with the non-hypertensive population. Prevalence varies with absolute blood pressure levels51,52 and these findings of higher prevalences with, rather than without, hypertension are consistent with other reports that did not meet the inclusion criteria for this analysis.2,22,23,53,54 The prevalence figures for diabetes are intermediate between those found for normotensive non-diabetic and hypertensive populations. Inter-arm blood pressure differences are associated with peripheral vascular and cerebrovascular disease,20,55,56 both conditions that share hypertension as a major risk factor.57 It therefore seems plausible that the prevalence of inter-arm differences, which have been described as markers of peripheral arterial disease,10,15,58,59 rise with the baseline vascular risk of the population studied.
This study’s findings suggest that prevalences of an inter-arm difference may vary by ethnicity, with lower prevalences of a ≥10 mmHg difference seen both with and without hypertension for East Asian compared with Western populations. These prevalence differences were not explained by variations in systolic blood pressures between ethnic groups. Recently, in a study designed specifically to compare inter-arm difference between ethnic groups, there were no significant differences in inter-arm prevalences between white British, South Asian, and African Caribbean cohorts.60 However, the larger MESA (MultiEthnic Study of Atherosclerosis) study has reported higher prevalence of systolic inter-arm differences ≥15 mmHg in African American and white non-Hispanic Americans compared with Hispanic or Chinese Americans.61
Few studies have directly compared simultaneous and sequential measurement techniques; the two methods appear to correlate well during a single assessment session,45,62 but not over different visits.7,63 Studies on the reproducibility of an inter-arm difference over time are mainly short term (that is, weeks),8,62 apart from a small 1-year retrospective follow-up in diabetes.7
Prevalence figures have previously been shown to be higher when a sequential rather than a simultaneous measurement technique is employed.35,62,64 Pooled data in this review show a relative risk of detecting a systolic inter-arm difference ≥10 mmHg of 2.9 for sequential compared with simultaneous measurement. A comparable risk ratio (2.2) was reported in a previous systematic review that compared pooled risks across different studies.28 The authors believe that these findings are the first pooled analysis of paired sequential and simultaneous measurements in the same groups of individuals, as opposed to pooled prevalence data derived from unmatched studies according to method of inter-arm measurement.
Prevalence of inter-arm difference declines with number of pairs of measurements,6,42,60,62 possibly in part due to white-coat effects on blood pressure.60,65 Verberk has estimated that an inter-arm difference ≥10 mmHg is twice as likely to be observed when based on a single rather than repeated pairs of simultaneous measurements.28 Recently, devices have been developed that measure two or four limbs simultaneously. Four studies reporting results from a four-limb device (COLIN VP1000 waveform analyser, Omron, Japan) are included in this analysis.36,38,41,42 Sensitivity analyses for this device did not show different prevalence estimates for any cut-off or subgroup compared to other repeated measurement protocols. It is a sophisticated waveform analysis device and it cannot therefore be assumed that single pairs of measurements obtained by other single or paired devices do not overestimate prevalence. Two studies in this review used a simultaneous two-limb device that averages three pairs of readings (WatchBP® Office, Microlife, UK).37,45 Lohmann and colleagues found no significant differences in prevalence calculated from two or three simultaneous pairs of readings using this device, and there was no evidence of different prevalence findings based on these studies compared with other methods.37
Implications for research and practice
Systolic inter-arm differences are associated with higher prevalences of peripheral arterial disease,3,10,20 and with increased cardiovascular and all-cause mortality.19–21 This study’s findings support the current advice in hypertension guidelines that inter-arm difference, when observed, should be confirmed with simultaneous measurement of both arms.26,29 However, detection methods in daily primary care need to be practical or they will not be adopted.46,66 It has been previously found that a single pair of sequential measurements can exclude the presence of an inter-arm difference on simultaneous measurement with good specificity and high negative predictive values (0.97 for ≥10 mmHg and 0.99 for ≥15 mmHg),6 and is associated with increased cardiovascular and all-cause mortality.15 Therefore, a sequential method of measurement still has a role in identifying people in need of further assessment for inter-arm difference.
The prevalence figures presented here are useful to estimate how often an inter-arm difference may be missed if not checked for in primary care. For example, with a prevalence of 10%, a systolic blood pressure might be underestimated by ≥10 mmHg through the chance selection of the lower reading arm once in every 20 assessments, leading to false reassurance about, or under-treatment of, high blood pressure.5,10,17,67
This study’s findings quantify the prevalence of inter-arm differences that may be expected in primary care populations, suggesting that an inter-arm blood pressure difference occurs in a significant minority of these patients. Historically, inter-arm difference has not been routinely checked for in primary care,27 although uptake seems to be increasing (CE Clark, unpublished data, 2016) and guideline recommendations are due for review.68 Therefore, practitioners should ensure that a difference has been looked for before making treatment decisions based on blood pressure measurements. A simultaneous method of measurement is needed to confirm the presence of an inter-arm difference and this should be the method of choice for any future studies.
Further work is required to establish the validity of individual devices for accuracy of measurement based on a single pair of measurements, and further data are required to explore more fully any ethnic variations in prevalence or implications of inter-arm differences. The authors are currently conducting an individual patient data meta-analysis that will provide population-specific evidence on prevalence.69
Acknowledgments
The authors are grateful to Prof. Jiguang Wang and Dr Niels van der Hoeven for contributing additional subgroup data from their studies,38,45 and to Prof. Nanno Kleefstra for clarifying his methods.7 Thanks are also due to Mrs Joy Choules for retrieving many of the papers included in this review.
Appendix 1. Search strategy
| Number | Database | Search term |
|---|---|---|
| 1 | Embase, MEDLINE, CINAHL | (subclavian AND stenosis).af |
| 2 | Embase, MEDLINE, CINAHL | (blood AND pressure AND NEAR AND difference).af |
| 3 | Embase, MEDLINE, CINAHL | (blood AND pressure AND NEAR AND differential).af |
| 4 | Embase, MEDLINE, CINAHL | (interarm AND NEAR AND differential).af |
| 5 | Embase, MEDLINE, CINAHL | (interarm AND NEAR AND difference).af |
| 6 | Embase, MEDLINE, CINAHL | (inter-arm AND NEAR AND difference).af |
| 7 | Embase, MEDLINE, CINAHL | (inter-arm AND NEAR AND differential).ti,ab |
| 8 | Embase, MEDLINE, CINAHL | (inter AND arm AND NEAR AND differential).af |
| 9 | Embase, MEDLINE, CINAHL | (inter AND arm AND NEAR AND difference).af |
| 10 | Embase, MEDLINE, CINAHL | 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 |
Funding
The South West General Practice Trust. Christopher E Clark is supported by a National Institute for Health Research (NIHR) Clinical Lectureship award. Rod S Taylor is supported by the NIHR Collaboration for Leadership in Applied Health Research and Care, South West Peninsula, at the Royal Devon and Exeter NHS Foundation Trust. Angela C Shore is supported by the NIHR Exeter Clinical Research facility.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Fonseca-Reyes S, Forsyth-MacQuarrie AM, García de Alba-García JE, et al. Simultaneous blood pressure measurement in both arms in hypertensive and nonhypertensive adult patients. Blood Press Monit. 2012;17(4):149–154. doi: 10.1097/MBP.0b013e32835681e2. [DOI] [PubMed] [Google Scholar]
- 2.Clark CE, Campbell JL, Evans PH, et al. Prevalence and clinical implications of the inter-arm blood pressure difference: a systematic review. J Hum Hypertens. 2006;20(12):923–931. doi: 10.1038/sj.jhh.1002093. [DOI] [PubMed] [Google Scholar]
- 3.Clark CE, Campbell JL, Powell RJ, et al. The inter-arm blood pressure difference and peripheral vascular disease: cross-sectional study. Fam Pract. 2007;24(5):420–426. doi: 10.1093/fampra/cmm035. [DOI] [PubMed] [Google Scholar]
- 4.Clark CE, Taylor RS, Shore AC, et al. The difference in blood pressure readings between arms and survival: primary care cohort study. BMJ. 2012;344:e1327. doi: 10.1136/bmj.e1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clark CE, Greaves C, Evans PH, et al. The inter-arm blood pressure difference in type 2 diabetes: a barrier to effective management? Br J Gen Pract. 2009 doi: 10.3399/bjgp09X420752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clark CE, Steele AM, Taylor RS, et al. Inter-arm blood pressure difference in people with diabetes: measurement and vascular and mortality implications: a cohort study. Diabetes Care. 2014;37(6):1613–1620. doi: 10.2337/dc13-1576. [DOI] [PubMed] [Google Scholar]
- 7.Kleefstra N, Houweling ST, Meyboom-de Jong B, et al. Measuring the blood pressure in both arms is of little use; longitudinal study into blood pressure differences between both arms and its reproducibility in patients with diabetes mellitus type 2. Ned Tijdschr Geneeskd. 2007;151(27):1509–1514. [PubMed] [Google Scholar]
- 8.Agarwal R, Bunaye Z, Bekele DM. Prognostic significance of between-arm blood pressure differences. Hypertension. 2008;51(3):657–662. doi: 10.1161/HYPERTENSIONAHA.107.104943. [DOI] [PubMed] [Google Scholar]
- 9.Quiroga B, Galán I, Garcia de Vinuesa S, et al. Interarm systolic blood pressure as a predictor of cardiovascular events in patients with chronic kidney disease. Nephrol Dial Transplant. 2015;30(5):801–806. doi: 10.1093/ndt/gfv059. [DOI] [PubMed] [Google Scholar]
- 10.Aboyans V, Criqui MH, McDermott MM, et al. The vital prognosis of subclavian stenosis. J Am Coll Cardiol. 2007;49(14):1540–1545. doi: 10.1016/j.jacc.2006.09.055. [DOI] [PubMed] [Google Scholar]
- 11.Ray WT. Assessment of blood pressure discrepancies in third-trimester hypertensive gravidas. AANA J. 2000;68(6):525–530. [PubMed] [Google Scholar]
- 12.Poon LC, Kametas N, Strobl I, et al. Inter-arm blood pressure differences in pregnant women. BJOG. 2008;115(9):1122–1130. doi: 10.1111/j.1471-0528.2008.01756.x. [DOI] [PubMed] [Google Scholar]
- 13.Cassidy P, Jones K. A study of inter-arm blood pressure differences in primary care. J Hum Hypertens. 2001;15(8):519–522. doi: 10.1038/sj.jhh.1001224. [DOI] [PubMed] [Google Scholar]
- 14.Clark CE, Powell RJ. The differential blood pressure sign in general practice: prevalence and prognostic value. Fam Pract. 2002;19(5):439–441. doi: 10.1093/fampra/19.5.439. [DOI] [PubMed] [Google Scholar]
- 15.Clark CE, Taylor RS, Butcher I, et al. Inter-arm blood pressure difference and mortality: a cohort study in an asymptomatic primary care population at elevated cardiovascular risk. Br J Gen Pract. 2016 doi: 10.3399/bjgp16X684949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agarwal S. Should blood pressure be measured in both arms? [Abstract] Chest. 2012;142:126A. [Google Scholar]
- 17.Karagiannis A, Tziomalos K, Krikis N, et al. The unilateral measurement of blood pressure may mask the diagnosis or delay the effective treatment of hypertension. Angiology. 2005;56(5):565–569. doi: 10.1177/000331970505600507. [DOI] [PubMed] [Google Scholar]
- 18.Kulkarni PK, Shekhar S, Reddy BN, et al. Blood pressure measurement: one arm or both arm? Indian J Med Sci. 2011;65(9):406–410. [PubMed] [Google Scholar]
- 19.Weinberg I, Gona P, O’Donnell CJ, et al. The systolic blood pressure difference between arms and cardiovascular disease in the Framingham Heart Study. Am J Med. 2014;127(3):209–215. doi: 10.1016/j.amjmed.2013.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clark CE, Taylor RS, Shore AC, et al. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. Lancet. 2012;379(9819):905–914. doi: 10.1016/S0140-6736(11)61710-8. [DOI] [PubMed] [Google Scholar]
- 21.Clark C, Shore A, Taylor R, et al. The inter-arm difference in blood pressure and mortality: systematic review and meta-analysis. J Hypertens. 2015;33(Suppl 1):e11. [Google Scholar]
- 22.Kristensen BO, Kornerup HJ. Which arm to measure the blood pressure? Acta Med Scand. 1982;670(Suppl):69–73. doi: 10.1111/j.0954-6820.1982.tb09877.x. [DOI] [PubMed] [Google Scholar]
- 23.Amsterdam B, Amsterdam AL. Disparity in blood pressures in both arms in normals and hypertensives and its clinical significance. N Y State J Med. 1943;43:2294–2300. [Google Scholar]
- 24.Swallow RA. Hypertension: which arm? [Letter] BMJ. 1975;3:370. doi: 10.1136/bmj.3.5979.370-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh S, Sethi A, Singh M, et al. Prevalence of simultaneously measured interarm systolic blood pressure difference and its clinical and demographic predictors: a systemic review and meta-analysis. Blood Pressure Monitor. 2015;20(4):178–185. doi: 10.1097/MBP.0000000000000115. [DOI] [PubMed] [Google Scholar]
- 26.National Institute for Health and Care Excellence Hypertension: The clinical management of primary hypertension in adults, update of clinical guidelines 18 and 34 CG127. 2011. https://www.nice.org.uk/guidance/cg127 (accessed 23 Sep 2016). [PubMed]
- 27.Heneghan C, Perera R, Mant D, Glasziou P. Hypertension guideline recommendations in general practice: awareness, agreement, adoption, and adherence. Br J Gen Pract. 2007 doi: 10.3399/096016407782604965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Verberk WJ, Kessels AGH, Thien T. Blood pressure measurement method and inter-arm differences, a meta-analysis. Am J Hypertens. 2011;24(11):1201–1208. doi: 10.1038/ajh.2011.125. [DOI] [PubMed] [Google Scholar]
- 29.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Study of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2013;31(7):1281–1357. doi: 10.1097/01.hjh.0000431740.32696.cc. [DOI] [PubMed] [Google Scholar]
- 30.Chapman JM, Clark VA, Coulson AH, et al. Problems of measurement in blood pressure surveys: inter-observer differences in blood pressure determinations. Am J Epidemiol. 1966;84(3):483–494. doi: 10.1093/oxfordjournals.aje.a120661. [DOI] [PubMed] [Google Scholar]
- 31.Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration; 2011. http://handbook.cochrane.org/ (accessed 23 Sep 2016). [Google Scholar]
- 32.Rao JN, Scott AJ. A simple method for the analysis of clustered binary data. Biometrics. 1992;48(2):577–585. [PubMed] [Google Scholar]
- 33.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zwirn P, Burnet H, Barthélémy P. Comparison between left and right humeral arterial pressure. Indirect measurement with an automatic apparatus. Ann Cardiol Angeiol (Paris) 1991;40(4):203–208. [PubMed] [Google Scholar]
- 35.Harrison EG, Roth GM, Hines EA. Bilateral indirect and direct arterial pressures. Circulation. 1960;22:419–436. doi: 10.1161/01.cir.22.3.419. [DOI] [PubMed] [Google Scholar]
- 36.Kimura A, Hashimoto J, Watabe D, et al. Patient characteristics and factors associated with inter-arm difference of blood pressure measurements in a general population in Ohasama, Japan. J Hypertens. 2004;22(12):2277–2283. doi: 10.1097/00004872-200412000-00009. [DOI] [PubMed] [Google Scholar]
- 37.Lohmann FW, Eckert S, Verberk WJ. Interarm differences in blood pressure should be determined by measuring both arms simultaneously with an automatic oscillometric device. Blood Press Monit. 2011;16(1):37–43. doi: 10.1097/mbp.0b013e328343317a. [DOI] [PubMed] [Google Scholar]
- 38.Sheng CS, Liu M, Zeng WF, et al. Four-limb blood pressure as predictors of mortality in elderly Chinese. Hypertension. 2013;61(6):1155–1160. doi: 10.1161/HYPERTENSIONAHA.111.00969. [DOI] [PubMed] [Google Scholar]
- 39.Van der Hoeven NV, Lodestijn S, Nanninga S, et al. Simultaneous compared to sequential blood pressure measurement results in smaller inter-arm blood pressure differences. J Clin Hypertens. 2013;15(11):839–844. doi: 10.1111/jch.12203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Clark CE, Casanova F, Gooding K, et al. Inter-arm blood pressure difference and arterial stiffness. J Hypertension. 2014;32(eSuppl A):e30. [Google Scholar]
- 41.Okada H, Fukui M, Tanaka M, et al. A difference in systolic blood pressure between arms and between lower limbs is a novel risk marker for diabetic nephropathy in patients with type 2 diabetes. Hypertens Res. 2013;36(5):403–407. doi: 10.1038/hr.2012.207. [DOI] [PubMed] [Google Scholar]
- 42.Canepa M, Milaneschi Y, Ameri P, et al. Relationship between inter-arm difference in systolic blood pressure and arterial stiffness in community-dwelling older adults. J Clin Hypertens. 2013;15(12):880–887. doi: 10.1111/jch.12178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim KB, Oh MK, Kim HG, et al. Inter-arm differences in simultaneous blood pressure measurements in ambulatory patients without cardiovascular diseases. Korean J Fam Med. 2013;34(2):98–106. doi: 10.4082/kjfm.2013.34.2.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Orme S, Ralph SG, Birchall A, et al. The normal range for inter-arm differences in blood pressure. Age Ageing. 1999;28(6):537–542. doi: 10.1093/ageing/28.6.537. [DOI] [PubMed] [Google Scholar]
- 45.Van der Hoeven NV, Lodestijn S, Nanninga S, et al. Simultaneous compared with sequential blood pressure measurement results in smaller inter-arm blood pressure differences. J Clin Hypertens. 2013;15(11):839–844. doi: 10.1111/jch.12203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Clark CE. Inter-arm blood pressure measurement needs to be practical and accurate. Am J Hypertens. 2011;24(11):1189–1190. doi: 10.1038/ajh.2011.139. [DOI] [PubMed] [Google Scholar]
- 47.Clark CE. Four-limb blood pressure measurement: a research tool looking for a clinical use. Hypertension. 2013;61(6):1146–1147. doi: 10.1161/HYPERTENSIONAHA.113.01098. [DOI] [PubMed] [Google Scholar]
- 48.Lane D, Beevers M, Barnes N, et al. Inter-arm differences in blood pressure: when are they clinically significant? J Hypertension. 2002;20(6):1089–1095. doi: 10.1097/00004872-200206000-00019. [DOI] [PubMed] [Google Scholar]
- 49.Clark CE. Difference in blood pressure measurements between arms: methodological and clinical implications. Curr Pharm Des. 2015;21(6):737–743. doi: 10.2174/1381612820666141024124349. [DOI] [PubMed] [Google Scholar]
- 50.Johansson JK, Puukka PJ, Jula AM. Interarm blood pressure difference and target organ damage in the general population. J Hypertens. 2014;32(2):260–266. doi: 10.1097/HJH.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 51.Sun H, Li P, Su H, et al. The detection rates of inter-arm systolic blood pressure difference vary with blood pressure levels in hypertensive patients under antihypertensive therapy. Int J Cardiol. 2014;172(3):e419–e420. doi: 10.1016/j.ijcard.2013.12.252. [DOI] [PubMed] [Google Scholar]
- 52.Sun H, Li P, Su H, et al. Brachial-brachial index of systolic blood pressure in the patients under anti-hypertensive therapy. Int J Cardiol. 2014;174(3):802–804. doi: 10.1016/j.ijcard.2014.04.118. [DOI] [PubMed] [Google Scholar]
- 53.Mehlsen J, Wiinberg N. Interarm difference in blood pressure: reproducibility and association with peripheral vascular disease. Int J Vasc Med. 2014;2014:841542. doi: 10.1155/2014/841542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.White J, Mortensen LH, Kivimaki M, et al. Interarm differences in systolic blood pressure and mortality among US army veterans: aetiological associations and risk prediction in the Vietnam experience study. Eur J Prev Cardiol. 2014;21(11):1394–1400. doi: 10.1177/2047487313496193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim J, Song TJ, Song D, et al. Interarm blood pressure difference and mortality in patients with acute ischemic stroke. Neurology. 2013;80(16):1457–1464. doi: 10.1212/WNL.0b013e31828cf87c. [DOI] [PubMed] [Google Scholar]
- 56.Madan VD, Rockman CB, Guo Y, et al. Association between interarm systolic blood pressure differential and peripheral artery disease: a population database of over 3.6 million subjects [Abstract 17204] Circulation. 2013;128(Suppl 22):A17204. [Google Scholar]
- 57.Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014;383(9932):1899–1911. doi: 10.1016/S0140-6736(14)60685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Aboyans V. Asymmetrical limbs arterial pressures: a new marker of atherosclerosis. Hypertens Res. 2013;36(5):394–395. doi: 10.1038/hr.2012.228. [DOI] [PubMed] [Google Scholar]
- 59.Shadman R, Criqui MH, Bundens WP, et al. Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol. 2004;44(3):618–623. doi: 10.1016/j.jacc.2004.04.044. [DOI] [PubMed] [Google Scholar]
- 60.Schwartz C, Koshiaris C, Clark C, et al. Does the right arm know what the left arm is doing? Ethnic variations in clinical inter-arm difference and relationship to white coat effects. J Hypertens. 2015;33(Suppl 1):e7. [Google Scholar]
- 61.Aboyans V, Criqui MH, McClelland RL, et al. Intrinsic contribution of gender and ethnicity to normal ankle-brachial index values: the Multi-Ethnic Study of Atherosclerosis (MESA) J Vasc Surg. 2007;45(2):319–327. doi: 10.1016/j.jvs.2006.10.032. [DOI] [PubMed] [Google Scholar]
- 62.Eguchi K, Yacoub M, Jhalani J, et al. Consistency of blood pressure differences between the left and right arms. Arch Intern Med. 2007;167(4):388–393. doi: 10.1001/archinte.167.4.388. [DOI] [PubMed] [Google Scholar]
- 63.Bakx JC. Blood pressure differences between left and right arms? Hart Bulletin. 2007;38(4):109. [Google Scholar]
- 64.Singer AJ, Hollander JE. Blood pressure. Assessment of interarm differences. Arch Intern Med. 1996;156(17):2005–2008. doi: 10.1001/archinte.156.17.2005. [DOI] [PubMed] [Google Scholar]
- 65.Martin U, Holder R, Hodgkinson J, McManus R. Inter-arm blood pressure differences compared with ambulatory monitoring: a manifestation of the ‘white-coat’ effect? Br J Gen Pract. 2013 doi: 10.3399/bjgp13X663055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Carlsen B, Glenton C, Pope C. Thou shalt versus thou shalt not: a meta-synthesis of GPs’ attitudes to clinical practice guidelines. Br J Gen Pract. 2007;57(545):971–978. doi: 10.3399/096016407782604820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Banks MJ, Erb N, George P, et al. Hypertension is not a disease of the left arm: a difficult diagnosis of hypertension in Takayasu’s arteritis. J Hum Hypertension. 2001;15(8):573–575. doi: 10.1038/sj.jhh.1001247. [DOI] [PubMed] [Google Scholar]
- 68.Hawkes N. Sixty seconds on … measuring blood pressure. BMJ. 2016;353:i2626. doi: 10.1136/bmj.i2626. [DOI] [PubMed] [Google Scholar]
- 69.Clark C, Campbell J, Boddy K, et al. Inter-arm blood pressure difference, cardiovascular events, cerebrovascular disease and mortality: an individual patient data meta-analysis. PROSPERO 2015: CRD42015031227. http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015031227 (accessed 23 Sep 2016).