Abstract
The aim of this study was to establish predictors for successfully planned extubation, which can be followed by medical personnel. The patients who were admitted to the adult intensive care unit of a tertiary hospital and met the following criteria between January 2005 and December 2014 were collected retrospectively: intubation > 48 hours; and candidate for extubation. The patient characteristics, including disease severity, rapid shallow breath index (RSBI), maximal inspiratory pressure (MIP), maximal expiratory pressure (MEP), cuff leak test (CLT) before extubation, and outcome, were recorded. The CLT was classified as 2+ with audible flow without a stethoscope, 1+ with audible flow using a stethoscope, and negative (N) with no audible flow, even with a stethoscope. Failure to extubate was defined as reintubation within 48 hours. In total, 6583 patients were enrolled and 403 patients (6.1%) had extubation failures. Male patients dominated the patient cohort (4261 [64.7%]). The mean age was 64.5±16.3 years. The overall in-hospital mortality rate was 11.3%. The extubation failure rate for females was greater than males (7.7% vs 5.3%, P < 0.001). The group of patients who failed extubation were older (66.7 ± 14.4 vs 64.3 ± 16.4, P = 0.002), had higher APACHE II scores (16.8 ± 7.6 vs 15.9 ± 7.8, P = 0.023), lower coma scales (10.3 ± 3.7 vs 10.8 ± 3.7, P = 0.07), a higher RSBI (69.9 ± 37.3 vs 58.6 ± 30.3, P < 0.001), a lower MIP, and MEP (−35.6 ± 15.3 vs −37.8 ± 14.6, P = 0.0001 and 49.6 ± 28.4 vs 58.6 ± 30.2, P < 0.001, respectively), and a higher mortality rate (25.6% vs 10.5%, P < 0.001) compared to the successful extubation group. Based on multivariate logistic regression, a CLT of 2+ (odds ratio [OR] = 2.07, P < 0.001), a MEP ≥ 55 cmH2O (OR = 1.73, P < 0.001), and a RSBI < 68 breath/min/ml (OR = 1.57, P < 0.001) were independent predictors for successful extubation.
This study identified 3 independent risk factors for successful extubation after a successful breathing trial, including a CLT of 2+, a MEP ≥ 55 cmH2O, and a RSBI < 68 breath/min/ml. Furthermore, a nomogram integrating these 3 parameters, which represented the combined consideration of the upper airway patentency, cough strength, and respiratory capacity, was developed to better predict extubation success.
Keywords: extubation, mechanical ventilation, predictor
1. Introduction
Endotracheal intubation with or without mechanical ventilation has become the most commonly used life support intervention for critically ill patients. After the acute condition requiring intubation is resolved, the decision to extubate, followed by a smooth weaning process and passing a weaning test should be undertaken as soon as possible to avoid delayed extubation. Even after extensive evaluation of potential extubation, however, 10% to 19% of patients fail extubation and require reintubation shortly after extubation.[1–6] Of greatest importance, the reintubated patients have a higher intensive care unit (ICU) mortality rate (26%–50%).[1–6] Therefore, a useful predictor for successful extubation is urgently needed to facilitate physician decisions regarding extubation.
Several studies[7–12] have investigated the possible factors by which to accurately predict successful extubation. Some researchers[7,11,12] have incorporated several parameters, including respiratory frequency-to-tidal volume (the rapid shallow breathing index [RSBI]), thoracic compliance, arterial oxygenation, maximum occlusion pressure, and dynamic changes of these indices through the course of a spontaneous breathing trial (SBT) for differentiating patients who are successfully extubated from patients who failed extubation. Salam et al[10] used a cough peak flow more than 60 L/min, tracheal secretions less than 2.5 mL/min, and the ability to follow 4 simple tasks as an indicator of an ability to maintain a patent upper airway and clear secretions. In contrast, Mokhlesi et al[9] reported that moderate-to-copious tracheal secretions, a Glasgow coma score (GCS) less than 10, and a Paco2 more than 44 mmHg during the SBT can independently predict extubation failure. The findings of the studies[7–12] are limited by the small number of observations and cannot accurately predict the extubation outcomes or be applied to the general population. Further large-scale investigations are warranted to identify the factors, which predict successful or failed extubation. Thus, the aim of this study was to establish a model, which predicts successfully planned endotracheal extubation.
2. Material and methods
2.1. Patients and hospital setting
This study was conducted at the Chi Mei Medical Center, a 1288-bed tertiary medical center with 96 ICU beds for adults. The ICU beds include medical-led teams consisting of 48 beds (9 cardiac beds and 39 surgical beds). The ICU is covered by intensivists, senior residents, nurses, respiratory therapists, dietitians, physical therapists, and clinical pharmacists. The ICU team makes rounds at least once daily, and respiratory therapists are responsible for managing all mechanical ventilation patients, including all weaning processes and SBTs. All of the ICU patients who had acute respiratory failure required invasive mechanical ventilation via an endotracheal tube for at least 48 hours and the patients who met the weaning criteria defined as respiratory rates less than 30 breath/min, tidal volume more than 5 mL/kg of ideal body weight, and rapid shallow index less than 105 breath/min/L, and successful completion of a SBT were prepared for scheduled extubation between January 2005 and December 2014 were eligible for inclusion. Patients who were less than 18 years of age were excluded. For patients who required repeated intubation, only the first episode was included in the analysis.
2.2. Variables measured
The medical records of all included patients were retrospectively reviewed and the following information was collected: age; gender; type of ICU; the level of consciousness; site of intubation; the causes requiring intubation and the intubation details; disease severity; ICU and hospital stays; reintubation rate; and in-hospital mortality rate. In our institution, we had weaning protocol. Briefly, the weaning protocol is initiated after the clinical condition is under control and the hemodynamic status becomes stable. Then, SBT using pressure support ventilation or T-piece for two hours was performed. After successful completion of a SBT, the weaning parameters, including the respiratory rate, tidal volume, minute ventilation, RSBI, MIP, maximal expiratory pressure (MEP), and cuff leak test (CLT), were measured when the patients were presumed ready for extubation. The CLT was classified as 2+ (audible flow without a stethoscope), 1+ (audible flow with a stethoscope), and negative (N; no audible flow with a stethoscope). Failure of extubation was defined as reintubation within 48 hours after extubation. The data were retrospectively collected on a routine basis and the analysis was carried out. Therefore, no informed consent was required and the study was specifically waived by the Institution Review Board. Ethics approval was obtained from the Institution Review Board of Chi Mei Medical Center.
2.3. Statistical analysis
Continuous variables are reported as a mean ± SD with a minimum and a maximum. Categorical variables are presented as a number with percentages. In addition, the differences in baseline characteristics and clinical variables between the successful and failed extubation groups were evaluated using a Student t test for continuous variables and a Pearson chi-square test for categorical variables. For the significant variables, univariate, and multivariate logistic regression analyses were used to calculate the odds ratios (ORs) and 95% confidence intervals (CIs) to determine the association between predictive variables and successful extubation. Receiver operating characteristic (ROC) curves were plotted for the MEP and RSBI values to identify the risk of extubation failure and the area under the curve was calculated. The Youden index score was used to identify the appropriate MEP and RSBI value with the best predicted performance. Using a forward model-selection procedure, the final model for prediction was conducted. Based on the final model, the estimated probability of successful extubation was calculated. A nomogram was used in which the regression coefficients representing the strengths of correlation were proportionately transferred to the distances on a graph. In turn, the distances were linked to corresponding points and summed. SAS 9.4 for Windows (SAS Institute, Cary, NC) was used for all analyses. Significance was set at a P < 0.05 (2-tailed).
3. Results
3.1. Demographic characteristics
During the study period, a total of 14,933 adult patients were intubated, but 4532 patients were intubated for less than 48 hours. After excluding patients with repeated intubations, a total of 6583 patients were included in the analysis and 403 patients (6.1%) failed extubation (Fig. 1). The patient demographic characteristics are summarized in Table 1. The mean age of the patients was 64.5 ± 16.3 years. Males comprised most of the patients (n = 4261 [64.7%]); most of the patients were admitted to the medical ICU (n = 3465 [52.6%]). The emergency department was the most common site where intubation was performed, followed by the operating room and ICU. Acute respiratory failure was the most common indication for intubation (n = 3352 [50.9%]), followed by postoperative respiratory compromise (n = 2037 [30.9%]), and airway protection (n = 609 [9.3%]). The APACHE II scores and Glasgow coma scale on ICU admission were 15.9 ± 7.8 and 10.7 ± 3.7, respectively. An endotracheal tube was placed via the oral route in more than 95% of the patients. The lengths of ICU and hospital stay were 11.8 ± 9.3 and 32.4 ± 76.4 days, respectively. The overall in-hospital mortality rate was 11.4%. The causes of reintubation are shown in Fig. 2, and impaired cough accounted for approximately 50% of extubation failures.
Figure 1.
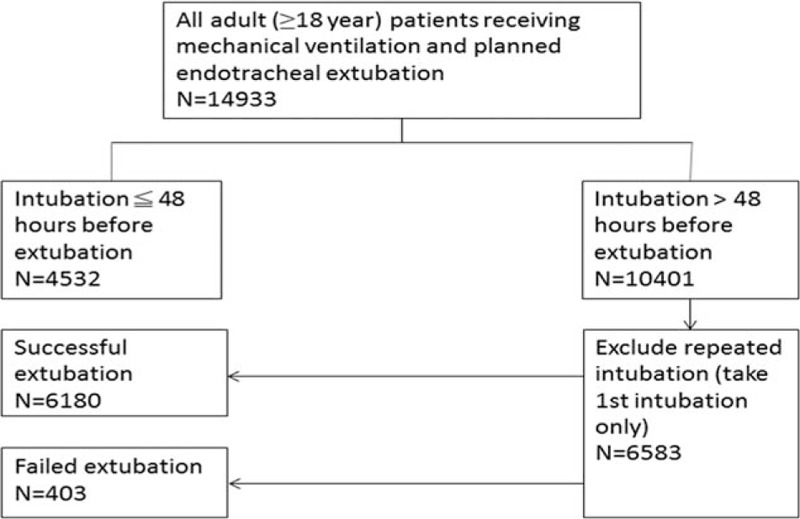
The algorithm of patients enrollment.
Table 1.
Characteristics of patients receiving mechanical ventilation for more than 48 hours and undergoing planned extubation (n = 6583).
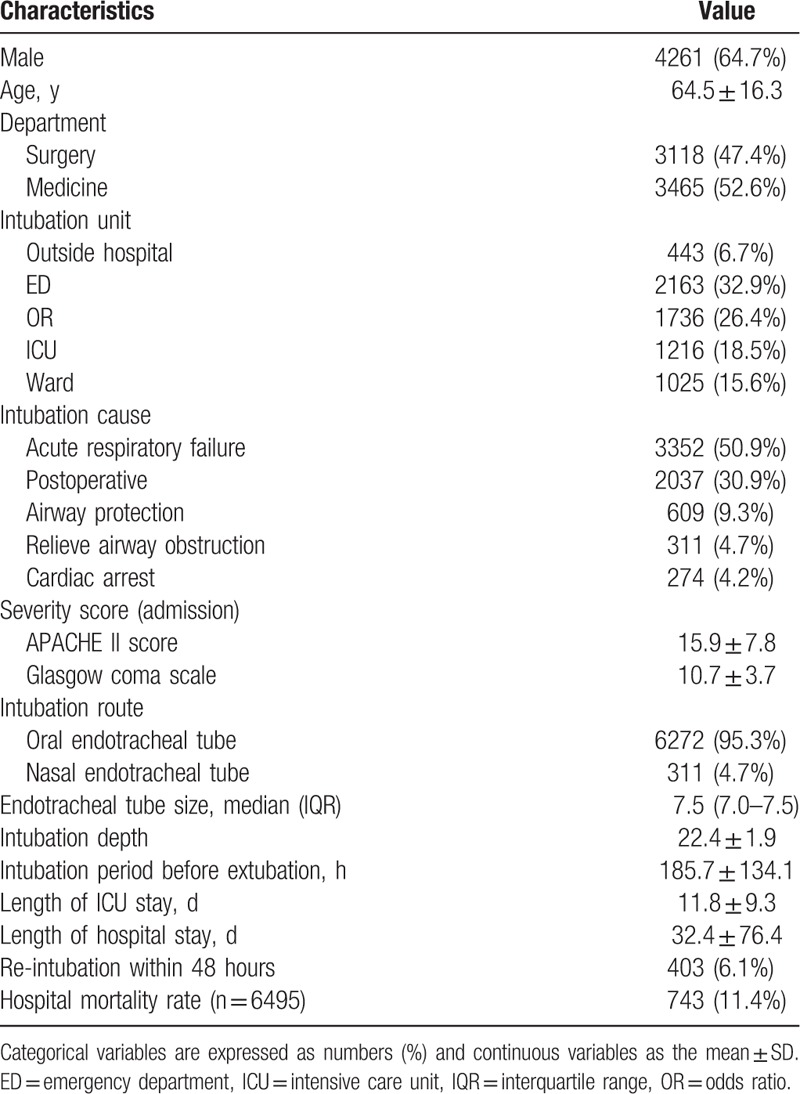
Figure 2.
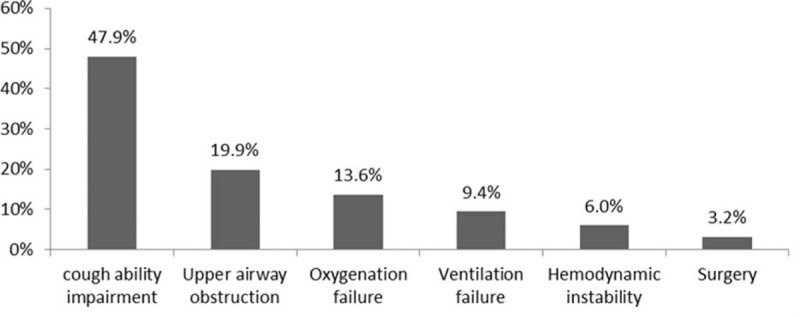
Reason for reintubation (n = 403).
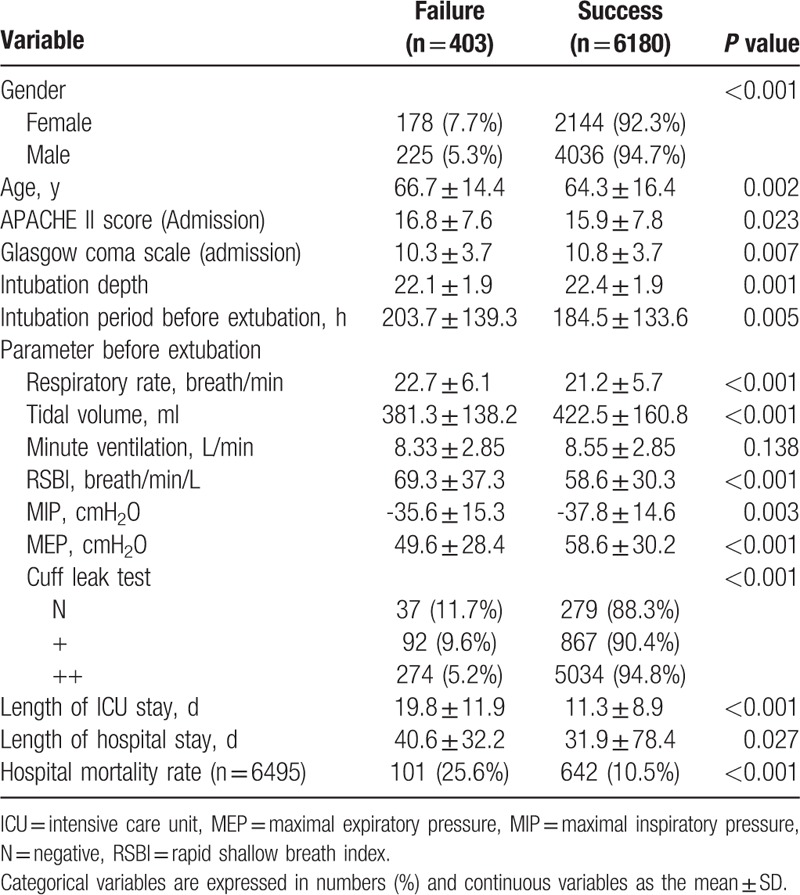
3.2. Comparison of patients with successful and failed planned extubation
Table 2 shows the comparison between patients with successful and failed extubations. The extubation failure rate amongst females was greater than males (7.7% vs 5.3%, P < 0.001). Failure group patients were older (66.7 ± 14.4 vs 64.3 ± 16.4 years, P = 0.002), had higher APACHE II scores (16.8 ± 7.6 vs 15.9 ± 7.8, P = 0.023), a lower GCS (10.3 ± 3.7 vs 10.8 ± 3.7, P = 0.07), a higher RSBI (69.9 ± 37.3 vs 58.6 ± 30.3, P < 0.001), a higher MIP and lower MEP (−35.6 ± 15.3 vs −37.8 ± 14.6, P = 0.0001 and 49.6 ± 28.4 vs 58.6 ± 30.2, P < 0.001, respectively), and a higher mortality rate (25.6% vs 10.5%, P < 0.001) compared with the successful group.
Table 2.
Comparison of patients with successful and failed planned extubations.
3.3. Predictive performance of MEP and RSBI
Figure 3 shows the ROC curve predicting successful extubation using the MEP and RSBI values. The area under the curve, which identified extubation success, was 0.60 and 0.59 for the MEP and RSBI, respectively. For the MEP, the best cut-off value was 55 cmH2O or more (sensitivity, 47.6%; specificity, 67.0%; positive predictive value [PPV], 95.8%; and negative predictive value, 7.88%). For the RSBI, the best cut-off value was less than 68 breath/min/ml (sensitivity, 46.2%; specificity, 67.7%; PPV, 95.1%; and negative predictive value, 8.52%).
Figure 3.
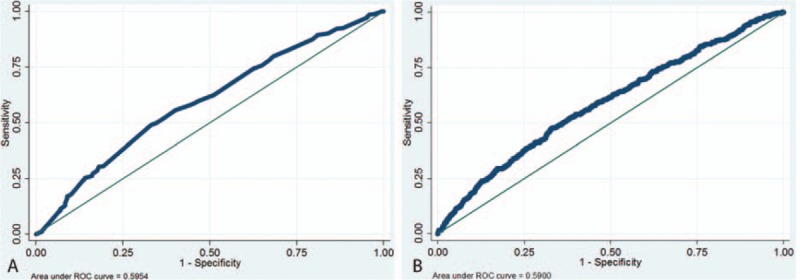
Receiver operating characteristic curve of risk for extubation failure using MEP (A) and RSBI (B). MEP = maximal expiratory pressure, RSBI = rapid shallow breath index.
3.4. Multivariate analysis
Based on multivariate logistic regression, no significant difference was detected according to age, APACHE II score, and GCS. The MIP level, a CLT = 2+ (OR = 2.07, P < 0.001), MEP of 55 cmH2O or more (OR = 1.73, P < 0.001), RSBI less than 68 breath/min/ml (OR = 1.57, P < 0.001) were independent predictors for successful extubation (Table 3). Nomograms to predict successful extubation based on these three factors were developed (Fig. 4).
Table 3.
Predictors of successful extubation.
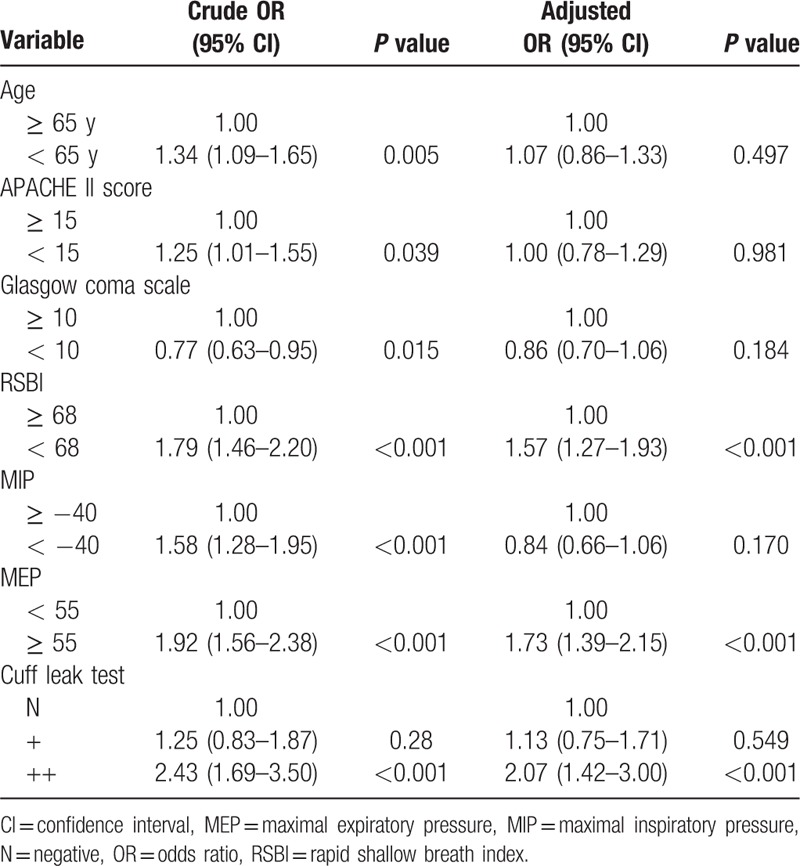
Figure 4.
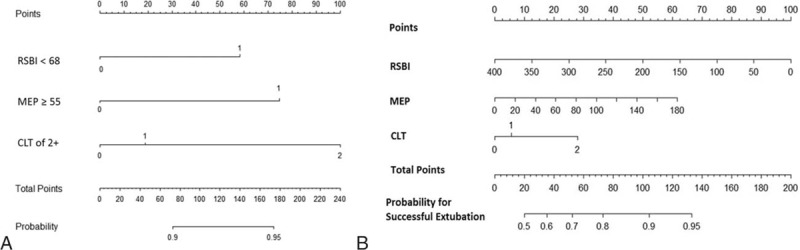
Nomogram of predicted probability for successful extubation using (A) category variables and (B) continuous variables.
4. Discussion
This is the largest study to investigate the extubation outcomes of 6583 patients with planned extubations. Based on this retrospective study, the overall rate of extubation failure was 6.1%. Additionally, we showed that extubation failure was significantly associated with age, gender, disease severity, level of consciousness, RSBI, MIP, MEP, and CLT based on univariate analysis. Furthermore, we identified 3 independent predictors of successful extubation, including the CLT, MEP, and RSBI based on multivariate analysis. The three predictors (CLT, MEP, and RSBI) represent upper airway patency, cough strength, and respiratory capability, respectively. Thus, if patients passed the CLT, had a high MEP, and had a low RSBI, the extubation success rate should be high. Finally, we integrated these three factors to create a model to predict the probability of extubation success.
Postextubation stridor (PES), which is characterized by laryngeal edema, is one of the most frequent causes of extubation failure. The incidence of PES ranges from 6% to 37% in ICU-intubated patients.[13–17] Because failed extubation caused by PES can be effectively reduced by steroids,[13,17] diagnosis of PES has become an important issue before extubation. The CLT, in which the leak volume around the endotracheal tube is measured while the cuff is deflated, has been proposed as a simple and reliable method of predicting the occurrence of PES.[15,18–20] In this study, we used a semiquantitative method (auscultation CLT), to replace the traditional quantitative measurement of the cuff leak volume. The auscultation CLT method has been shown to have excellent agreement with the cuff leak volume in a previous study.[17] Of most importance, we showed that auscultation CLT is independently and significantly associated with the extubation outcome. If the patient had a CLT = 2+ (audible flow without a stethoscope), the successful extubation rate was approximately 2-fold that of patients with a negative CLT (no audible flow with a stethoscope). Moreover, we found that among 80 patients with extubation failure extubation due to upper airway obstruction, higher portion of them were classified as CLT negative (n = 17, 45.9%) or CLT = 1 (n = 26, 28.3%) than other group with failed extubation (Table 4).
Table 4.
The association between CLT and cause of extubation failure.
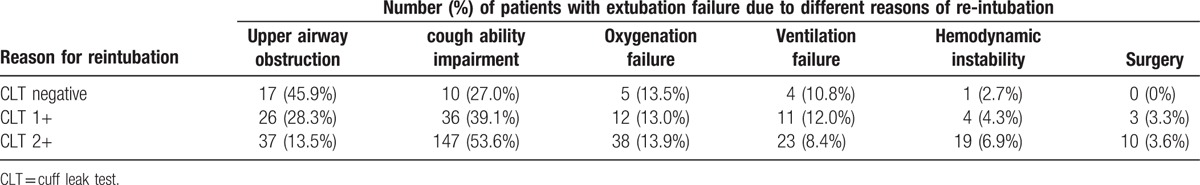
Extubation failure can occur in patients in whom secretions cannot be effectively removed,[21,22] and adequate cough strength is necessary for patients postextubation to clear secretions. Smina et al,[22] using voluntary cough peak expiratory flow (PEF) as a measurement of cough strength to predict extubation outcome, reported that patients with a PEF 60 L/min or less were 5 times more likely to have unsuccessful extubations. Szeinberg et al,[23] however, suggested that measurement of the MEP is more useful than PEF as an assessment of cough strength in patients with muscular dystrophy. Moreover, Szeinberg et al[23] concluded that patients with a MEP more than 60 cmH2O have an effective cough. In this study, 193 patients were classified as failed extubation due to cough ability impairment, and they had lower MEP (46.5 ± 25.8 cmH2O) than other groups with extubation failure. Furthermore, we also found that a MEP 55 cmH2O or more had the best predictive performance of successful extubation, according to the ROC curve analysis, and patients with a MEP 55 cmH2O or more were 1.73 times as likely to have a successful extubation after adjusting for other variables. In addition, our results showed that the overall PPV of MEP for predicting successful extubation was 95.8% at a cut-off of 55 cmH2O, thus suggesting that MEP is a useful indicator in predicting successful extubation; however, the overall sensitive and specificity of MEP 55 cmH2O or more for prediction were only 48% and 67%, respectively.
RSBI was developed by Yang and Tobin in 1991,[12] and has been commonly used as a predictor of weaning failure using a threshold value of 105 breath/min/ml. Weaning failure includes failure of a SBT in patients without extubation and extubation failure after a successful SBT. Several studies[10,22,24–26] have investigated different cut-off values of RSBI in predicting successful or failed extubation. According to Bien et al,[24] the median RSBI of re-intubated patients was significantly higher than successfully-extubated patients (69 vs 45 breath/min/ml). Similarly, another study[22] reported that significant differences in RSBI were noted between reintubated and nonreintubated patients (88 vs 60 breath/min/ml). Our findings were consistent with previous studies[10,21,22,24]; specifically, the RSBI was higher in patients with failed extubations than patients with successful extubations (69.9 ± 37.3 vs 58.6 ± 30.3, P < 0.001). Furthermore, Frutos-Vivar et al[25] used a RSBI of 57 breath/min/ml as a cut-off value and found the risk of reintubation increased from 11% to 18% if the RSBI was more than 57 breath/min/ml. In the present study, a RSBI of 68 breath/min/ml was identified as the most accurate predictor of failed extubation according to ROC analysis. After multivariate analysis, the OR for successful extubation was 1.57 (95% CI = 1.27–1.93, P < 0.001) in patients with a RSBI less than 68 breath/min/ml. The overall PPV of RSBI for predicting successful extubation was 95.2% at a cut-off of 68 breath/min/ml; the overall sensitivity and specificity of a RSBI less than 68 breath/min/ml for prediction of successful extubation were only 46% and 68%, respectively.
Although we found three independent useful predictors for successful extubation (CLT, MEP, and RSBI) based on multivariate analysis, and further identified the best cut-off values for MEP and RSBI, none was sensitive or specific enough. Therefore, we attempted to integrate three parameters (CLT, MEP, and RSBI) to create a predictive model using a nomogram to improve the power of prediction, as shown in Fig. 3. For example, if patients with a CLT = 2+, a MEP 55 cmH2O or more, and a RSBI less than 68 breath/min/ml, the probability of successful extubation was 95%. Although the predictive value of the nomogram was relatively accurate, further study is warranted to validate our findings.
Finally, the extubation failure rate was only 6.1%, which was lower than previous studies.[1–6] In contrast, the intubation time because of extubation was 7.7 ± 5.6 days, which was longer than previous reports.[17,25] Therefore, it is possible that delayed extubation may be partially responsible for the lower extubation failure rate. Another possible explanation may be that we used auscultation CLT to identify patients at risk for PES in our ICU before extubation, and recommend injection of methylprednisolone (40 mg every 6 hours over 24 hours) for prevention of PES in high-risk patients as our previous study.[17] This intervention may have reduced the extubation failure rate in this study. However, the role of steroid in the prevention of PES remains controversial which may be due to the use of different types of steroids and different administration regimens.[27] Further studies are still warranted to better define the optimal timing and dosage of steroids to prevent PES.[28]
This study had several limitations. It was conducted in a single hospital (a referral medical center), and the study population, the level of training, and the practice patterns may differ from other institutions with respect to patient characteristics or the weaning process. Despite we had weaning protocol in our institution, the final decision of extubation should be made by the physicians in charge of the patients in our institution. Thus, delayed extubation can occur until patients exhibit complete improvement in all variables. Therefore, our findings may not be generalized to other hospitals without further validation. Nevertheless, this study enrolled 6583 patients with planned extubations and 403 failed extubations during a 10-year period, which is a large-scale investigation regarding this issue. Our findings should be representative and provide useful information.
In conclusion, our large-scale study identified three independent risk factors of extubation success after a successful SBT. These predictors included a CLT = 2+, a MEP 55 cmH2O or more, and a RSBI less than 68 breath/min/ml. Indeed, the measures represented the patency of the upper airway, cough strength, and respiratory capacity, respectively. Moreover, we developed a nomogram that integrated these three parameters to better predict extubation success.
Footnotes
Abbreviations: APACHE = Acute Physiology and Chronic Health Evaluation, CLT = cuff leak test, ICU = intensive care unit, MEP = maximal expiratory pressure, MIP = maximal inspiratory pressure, RSBI = rapid shallow breath index.
KC Cheng is the guarantor of this manuscript; CCL, CCC, SRC, WLL, SCH, and KCC contributed to the conception and design of the study; SFW and MIS analyzed and interpreted the data; CCL and KCC drafted the manuscript.
The authors have no conflicts of interest to declare.
References
- 1.Epstein SK, Ciubotaru RL, Wong JB. Effect of failed extubation on the outcome of mechanical ventilation. Chest 1997; 112:186–192. [DOI] [PubMed] [Google Scholar]
- 2.Esteban A, Alia I, Gordo F, et al. Extubation outcome after spontaneous breathing trials with T-tube or pressure support ventilation. The Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med 1997; 156:459–465. [DOI] [PubMed] [Google Scholar]
- 3.Esteban A, Alia I, Tobin MJ, et al. Effect of spontaneous breathing trial duration on outcome of attempts to discontinue mechanical ventilation. Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med 1999; 159:512–518. [DOI] [PubMed] [Google Scholar]
- 4.Penuelas O, Frutos-Vivar F, Fernandez C, et al. Characteristics and outcomes of ventilated patients according to time to liberation from mechanical ventilation. Am J Respir Crit Care Med 2011; 184:430–437. [DOI] [PubMed] [Google Scholar]
- 5.Thille AW, Harrois A, Schortgen F, et al. Outcomes of extubation failure in medical intensive care unit patients. Crit Care Med 2011; 39:2612–2618. [DOI] [PubMed] [Google Scholar]
- 6.Vallverdu I, Calaf N, Subirana M, et al. Clinical characteristics, respiratory functional parameters, and outcome of a two-hour T-piece trial in patients weaning from mechanical ventilation. Am J Respir Crit Care Med 1998; 158:1855–1862. [DOI] [PubMed] [Google Scholar]
- 7.Liu Y, Wei LQ, Li GQ, et al. A decision-tree model for predicting extubation outcome in elderly patients after a successful spontaneous breathing trial. Anesth Analg 2010; 111:1211–1218. [DOI] [PubMed] [Google Scholar]
- 8.Menon N, Joffe AM, Deem S, et al. Occurrence and complications of tracheal reintubation in critically ill adults. Respir Care 2012; 57:1555–1563. [DOI] [PubMed] [Google Scholar]
- 9.Mokhlesi B, Tulaimat A, Gluckman TJ, et al. Predicting extubation failure after successful completion of a spontaneous breathing trial. Respir Care 2007; 52:1710–1717. [PubMed] [Google Scholar]
- 10.Salam A, Tilluckdharry L, Amoateng-Adjepong Y, et al. Neurologic status, cough, secretions and extubation outcomes. Intensive Care Med 2004; 30:1334–1339. [DOI] [PubMed] [Google Scholar]
- 11.Su WL, Chen YH, Chen CW, et al. Involuntary cough strength and extubation outcomes for patients in an ICU. Chest 2010; 137:777–782. [DOI] [PubMed] [Google Scholar]
- 12.Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med 1991; 324:1445–1450. [DOI] [PubMed] [Google Scholar]
- 13.Cheng KC, Chen CM, Tan CK, et al. Methylprednisolone reduces the rates of postextubation stridor and reintubation associated with attenuated cytokine responses in critically ill patients. Minerva Anestesiol 2011; 77:503–509. [PMC free article] [PubMed] [Google Scholar]
- 14.Francois B, Bellissant E, Gissot V, et al. 12-h pretreatment with methylprednisolone versus placebo for prevention of postextubation laryngeal oedema: a randomised double-blind trial. Lancet 2007; 369:1083–1089. [DOI] [PubMed] [Google Scholar]
- 15.Jaber S, Chanques G, Matecki S, et al. Post-extubation stridor in intensive care unit patients. Risk factors evaluation and importance of the cuff-leak test. Intensive Care Med 2003; 29:69–74. [DOI] [PubMed] [Google Scholar]
- 16.Lee CH, Peng MJ, Wu CL. Dexamethasone to prevent postextubation airway obstruction in adults: a prospective, randomized, double-blind, placebo-controlled study. Crit Care 2007; 11:R72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheng KC, Hou CC, Huang HC, et al. Intravenous injection of methylprednisolone reduces the incidence of postextubation stridor in intensive care unit patients. Crit Care Med 2006; 34:1345–1350. [DOI] [PubMed] [Google Scholar]
- 18.De Bast Y, De Backer D, Moraine JJ, et al. The cuff leak test to predict failure of tracheal extubation for laryngeal edema. Intensive Care Med 2002; 28:1267–1272. [DOI] [PubMed] [Google Scholar]
- 19.Miller RL, Cole RP. Association between reduced cuff leak volume and postextubation stridor. Chest 1996; 110:1035–1040. [DOI] [PubMed] [Google Scholar]
- 20.Sandhu RS, Pasquale MD, Miller K, et al. Measurement of endotracheal tube cuff leak to predict postextubation stridor and need for reintubation. J Am Coll Surg 2000; 190:682–687. [DOI] [PubMed] [Google Scholar]
- 21.Khamiees M, Raju P, DeGirolamo A, et al. Predictors of extubation outcome in patients who have successfully completed a spontaneous breathing trial. Chest 2001; 120:1262–1270. [DOI] [PubMed] [Google Scholar]
- 22.Smina M, Salam A, Khamiees M, et al. Cough peak flows and extubation outcomes. Chest 2003; 124:262–326. [DOI] [PubMed] [Google Scholar]
- 23.Szeinberg A, Tabachnik E, Rashed N, et al. Cough capacity in patients with muscular dystrophy. Chest 1988; 94:1232–1235. [DOI] [PubMed] [Google Scholar]
- 24.Bien MY, Hseu SS, Yien HW, et al. Breathing pattern variability: a weaning predictor in postoperative patients recovering from systemic inflammatory response syndrome. Intensive Care Med 2004; 30:241–247. [DOI] [PubMed] [Google Scholar]
- 25.Frutos-Vivar F, Ferguson ND, Esteban A, et al. Risk factors for extubation failure in patients following a successful spontaneous breathing trial. Chest 2006; 130:1664–1671. [DOI] [PubMed] [Google Scholar]
- 26.Upadya A, Tilluckdharry L, Muralidharan V, et al. Fluid balance and weaning outcomes. Intensive Care Med 2005; 31:1643–1647. [DOI] [PubMed] [Google Scholar]
- 27.Wittekamp BH, van Mook WN, Tjan DH, et al. Clinical review: post-extubation laryngeal edema and extubation failure in critically ill adult patients. Crit Care 2009; 13:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jaber S, Jung B, Chanques G, et al. Effects of steroids on reintubation and post-extubation stridor in adults: meta-analysis of randomised controlled trials. Crit Care 2009; 13:R49. [DOI] [PMC free article] [PubMed] [Google Scholar]


