Abstract
Corticosteroid injections for hand tendinitis can lead to a rare significant complication of tendon spontaneous rupture. However, only sporadic cases were reported in the literature before. This study was designed to gauge the clinical effect of tendon repair in patients of tendon spontaneous rupture after corticosteroid injection and analyze our experience.
This was a retrospective observational study of 13 patients (8 women and 5 men) operated between July 2011 and December 2015 for tendon spontaneous rupture after corticosteroid injection. Demographic data, clinical features, imaging data, and surgical treatments were carefully reviewed.
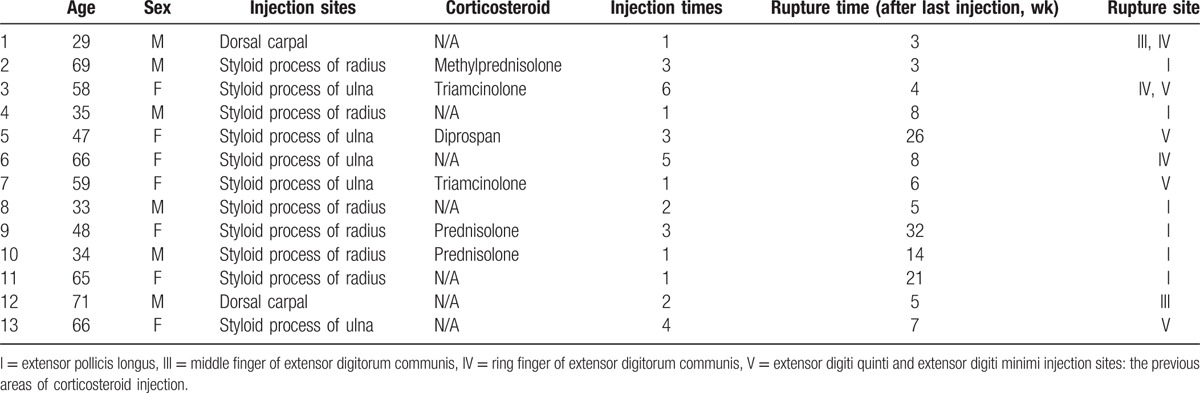
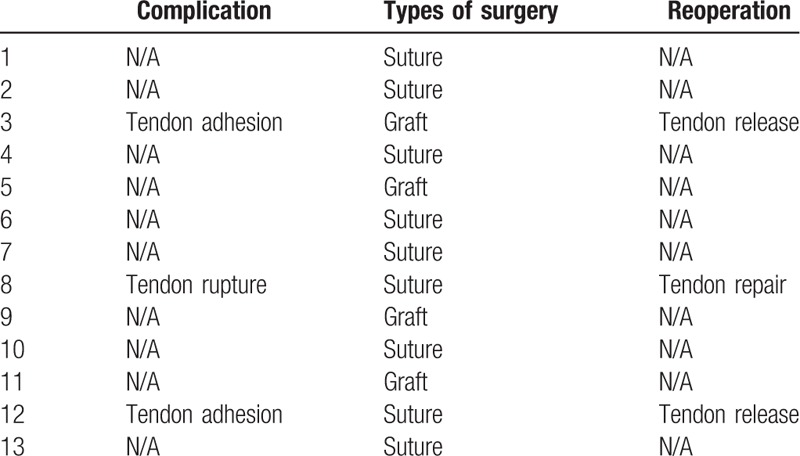
The average age was 52.308 ± 15.381 years (range 29–71). The average injection times were 2.538 ± 1.664 times (range 1–6). The average rupture time (after last injection) was 10.923 ± 9.500 weeks (range 3–32). Nine patients were treated by tendon suture (69% of cases), and 4 patients were treated by tendon grafting (31% of cases). All patients received follow-up in our outpatient clinic. The sites of the tendon rupture (15 tendons of 13 patients had involved) include extensor pollicis longus (6 tendons, 40% of cases), extensor digiti quinti and extensor digiti minimi (4 tendons, 27% of cases), ring finger of extensor digitorum communis (3 tendons, 20% of cases), and middle finger of extensor digitorum communis (2 tendons, 13% of cases). Two patients who had tendon adhesion (15% of cases) were treated by tendon release. One patient who had tendon rerupture (8% of cases) was treated by tendon grafting. No patient had complications of infections, vascular, or nerve injury.
Tendon spontaneous rupture is a serious complication after corticosteroid injection for tendinitis. Rigid standard of corticosteroid injection is very important. Magnetic resonance imaging was contributory to preoperative assess tendon defect and can be used to monitor healing quality of tendons during the follow-up.
Keywords: corticosteroid injection, spontaneous, tendon rupture
1. Introduction
Tendinitis refers to inflammation or irritation of a tendon, which is generally caused by overuse of the affected tendons.[1] The treatments include rest, nonsteroidal anti-inflammatory drugs, physical therapy, laser therapy, and shock wave therapy.[2–4] Corticosteroid injection is widely used as a conservative treatment for tendinitis. Injections of a corticosteroid medication around tendons can reduce the inflammation. It can reduce pain and improve function.[5,6] Corticosteroid injections are well tolerated and more effective than other conservative treatments in the short term.[7] Unfortunately, significant side effects have been reported as tendon degeneration and rupture.[8–11] It can inhibit tendon repair, delay tendon sheath healing, and produce tendon degeneration.[12] Collagen fragmentation and biomechanical changes may be the possible causes.[13,14] The treatment of tendon rupture is debridement and repair. The reconstruction of the tendon was performed using autogenous tendon grafting, for example, palmaris longus (PL) is the most common graft.[15,10]
We aimed to analyze the cases of tendon spontaneous rupture after corticosteroid injection in our hospital. We reviewed the demographic data, preoperative assessment, repair technique, and the clinical therapy outcome in order to reduce postoperative complications.
2. Patients and methods
All the patients were retrospectively identified who had been presented with pain or deformity after corticosteroid injections in our hospital between July 2011 and December 2015. Data from patients included sex, age, corticosteroid injection sites (the previous areas of corticosteroid injection), types of corticosteroid (if applicable), injection times, rupture time (after last injection), and sites of the tendon rupture (Table 1). Imaging data, surgical treatments, and complications were also recorded. The inclusion criteria were individuals of tendon spontaneous rupture after corticosteroid injection in our hospital. The exclusion criteria are patients had history of injury, patients were compared with type 2 diabetes, rheumatoid arthritis, or other autoimmune diseases. A total of 13 patients with 15 tendons were identified. Ethical approval was given by the medical ethics committee of the First Affiliated Hospital, College of Medicine, Zhejiang University (reference number: 331, date: 03/01/2011).
Table 1.
Patients data.
All the radiologic exams including X-ray and magnetic resonance imaging (MRI) were carefully recorded. X-ray anteroposterior and lateral films of hands and wrists were performed in all patients to exclude bony abnormity. MRI was contributory to identify tendon injury or inflammation before the operation. The tendon ends also can be identified. We can choose direct suturing if the defect between the tendon ends is no more than 0.5 cm. On the contrary, tendon grafting was carried out using the PL or other tendons. The absence of PL or not can be observed in MRI (Fig. 1). The rupture of tendons was suspected, and the patient was recommended to mobilization with a splint before the operation. The goal of operation is restoration of hand function and return to work. Patients were performed by tendon repair under regional anesthesia. A brachial tourniquet was used, and the procedure was carried out with surgical loupes. All surgeries were performed by 1 surgeon (HL).
Figure 1.
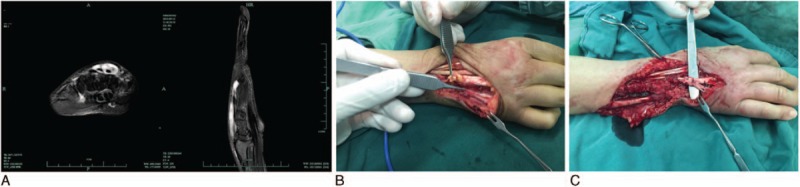
These images show a 58-year-old female with extensor digiti quinti, extensor digiti minimi, and ring finger of extensor digitorum communis tendons spontaneous rupture (A) T2-weighted magnetic resonance imaging shows tendons defect and inflammation. (B) Grossly, in surgery (C) tendon palmaris longus grafting for defect.
Data were expressed as mean ± standard deviation. Statistical analysis was performed using the software Microsoft Excel (Microsoft Corporation, Redmond, WA).
The diagnosis was speculated by clinical sign, imaging information, and history of corticosteroid injection. Diagnosis was confirmed by the degenerative appearance of tendons and frayed edges of tendons during operation.
Three days after the surgery, the patients were able to perform rehabilitation by the physical therapists. Patients used braces with the wrist in neutral position for 3 weeks (tendon suture) and 6 weeks (tendon grafting). A clinical questionnaire was completed over the telephone and at the clinic. All the patients had been interviewed and completed regular follow-up visits. The clinical and radiographic examinations would be performed regularly in the follow-up study.
3. Results
The average age was 52.308 ± 15.381 years (range 29–71). Sites of the tendon rupture (15 tendons of 13 patients have involved) included extensor pollicis longus (6 tendons, 40% of cases), extensor digiti quinti and extensor digiti minimi (4 tendons, 27% of cases), ring finger of extensor digitorum communis (3 tendons, 20% of cases), and middle finger of extensor digitorum communis (2 tendons, 13% of cases). The injection sites were 6 patients with styloid process of radius (46% of cases), 5 patients with styloid process of ulna (38% of cases), and 2 patients with dorsal carpal (15% of cases). The average injection times were 2.538 ± 1.664 times (range 1–6). The average rupture time (after last injection) was 10.923 ± 9.500 weeks (range 3–32). Types of surgery were as follows: 9 patients were treated by tendon suture (69% of cases) and 4 patients were treated by tendon grafting (31% of cases).
Grossly, all patients appeared to significant degeneration of the tendon during operation (Fig. 2). Postoperative complications were tendon adhesion and tendon rupture. Two patients of tendon adhesion (15% of cases) were treated by tendon release 3 months after first operation. One patient of rerupture (8% of cases) was treated by tendon grafting. No patient had complications of infections, vascular, or nerve injury (Table 2).
Figure 2.

This image shows significant degeneration of the tendon in surgery.
Table 2.
Complications and management.
4. Discussion
Corticosteroid injections can lead to serious consequences in quality of tendons.[16] Patients of our study expect good functional recovery, especially the young patients. Postoperative rehabilitation must be more careful than simple rupture of tendon. The goal of operation is restoration of hand function and return to work. Ultrasound or MRI used to locate the ruptured tendon ends before the operation.[17] In our study, MRI can clearly demonstrate the defect and inflammation. Preoperative MRI is beneficial to estimate the defect of tendons. Tendon grafting is necessary for the patients of tendon defect.[18] The cause of 1 rerupture patient may be due to direct suture of the tendon. We choose the PL for tendon grafting. The tension of the repair should be checked satisfactory in the surgery.[19] Immobilization and tendon release in supplemental operation are also needed. MRI also can be used to monitor healing quality of tendons during the follow-up.[20]
The usage of corticosteroid injections for wrist and hand pain is ambiguous sometimes in China or other country.[21] Some patients of our study who had no tenosynovitis still received corticosteroid injections. Actually, 6 patients (46% of cases) did not even know they were receiving corticosteroid injections. In our study, the application of Prednisolone (Jiangxi national medicine co., LTD, Jiangxi, China), Triamcinolone (Laboratorio Italiano Biochimico Farmaceutico LISAPHARMA S.p.A., Como, Italy), or Methylprednisolone (national medicine RongSheng pharmaceutical co., LTD, Henan, China) still have some problems which need to be standardized further. This is an underlying risk factor for tendon spontaneous rupture. Standard corticosteroid injections management is an important guarantee. We called for doctors, educators, regulators, and others to evaluate the risks and develop policies governing the use of corticosteroid injections.
One of the most common reason (46% of cases) for corticosteroid injections is for tenosynovitis of radialstyloid (the first dorsal compartment of wrist).[22] But the extensor pollicis longus (the third dorsal compartment of wrist) is the most common ruptured tendon. After analyzing the reasons of spontaneous rupture, we think 2 factors to be the main reason: mistaken injection sites and corticosteroid extravasation. The longest rupture time after last injection in our study was 32 weeks. It is also critical to note the delayed spontaneous rupture for both the public and doctors. For most young patients, a protective splint should be done to guard against tendon rerupture.
There are some limitations to our study. First, we had a relatively small group of patients available to assess due to the disease's rarity. Therefore, a multicenter study is needed. Second, the corticosteroid species, doses, and the frequency of injection were not documented in detail. It still lacks detailed tutorials and standard conveniences for corticosteroid injection. Educating both the public and doctors is crucial in the future.
5. Conclusion
Tendon spontaneous rupture is a serious complication after corticosteroid injection for tendinitis. Standard corticosteroid injections management is an important guarantee for reducing the occurrence of this event. Educating both the public and doctors is crucial. Tendon grafting is recommended in the patients of tendon defect. MRI was contributory to preoperatively assess tendon defect and can be used to monitor healing quality of tendons during the follow-up.
Acknowledgments
First and foremost, I would like to show my deepest gratitude to my colleagues QC, HY, HS, GY, and XL who provided me with valuable assist in every stage of writing this paper. Meanwhile, I also appreciate Zhejiang traditional Chinese Medicine Research Program (the grant number 2016ZA124), Zhejiang Medicine and Hygiene Research Program (the grant number 2016KYB101), and Sanmen Social Development of Science and Technology Projects (the grant number 15302) for sponsoring our research. Last but not least, I would like to thank all my friends, especially my lovely wife for her translation, encouragement, and support.
Footnotes
Abbreviations: MRI = magnetic resonance imaging, PL = palmaris longus.
Competing interests: The authors declare that they have no competing interests.
Authors’ contributions: HL, QC, HY, HS, and XL performed the data collection. HL designed the study and performed the analysis. HL drafted the manuscript. All authors read and approved the final manuscript.
Zhejiang traditional Chinese medicine Research Program (the grant number 2016ZA124), Zhejiang Medicine and Hygiene Research Program (the grant number 2016KYB101), and Sanmen Social Development of Science and Technology Projects (the grant number 15302) support the work.
The authors have no conflicts of interest to disclose.
References
- 1.Sevier TL, Helfst RH, Stover SA, et al. Clinical trends on tendinitis. Work 2000; 14:123–126. [PubMed] [Google Scholar]
- 2.Bjordal JM, Lopes-Martins RA, Iversen VV. A randomised, placebo controlled trial of low level laser therapy for activated Achilles tendinitis with microdialysis measurement of peritendinous prostaglandin E2 concentrations. Br J Sports Med 2006; 40:76–80.discussion 76–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rompe J, Zoellner J, Nafe B. Shock wave therapy versus conventional surgery in the treatment of calcifying tendinitis of the shoulder.[J]. Clinical Orthopaedics & Related Research 2001; 387:72–82. [DOI] [PubMed] [Google Scholar]
- 4.Lecomte J, Buyse H, Taymans J, et al. Treatment of tendinitis and bursitis: a comparison of nimesulide and naproxen sodium in a double-blind parallel trial. Eur J Rheumatol Inflamm 1994; 14:29–32. [PubMed] [Google Scholar]
- 5.Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet 2010; 376:1751–1767. [DOI] [PubMed] [Google Scholar]
- 6.Anderson B, Kaye S. Treatment of flexor tenosynovitis of the hand (’trigger finger’) with corticosteroids. A prospective study of the response to local injection. Arch Intern Med 1991; 151:153–156. [PubMed] [Google Scholar]
- 7.Gaujoux-Viala C, Dougados M, Gossec L. Efficacy and safety of steroid injections for shoulder and elbow tendonitis: a meta-analysis of randomised controlled trials. Ann Rheum Dis 2009; 68:1843–1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gottlieb NL, Riskin WG. Complications of local corticosteroid injections. JAMA 1980; 243:1547–1548. [PubMed] [Google Scholar]
- 9.Neustadt DH. Complications of local corticosteroid injections. JAMA 1981; 246:835–836. [DOI] [PubMed] [Google Scholar]
- 10.Yamada K, Masuko T, Iwasaki N. Rupture of the flexor digitorum profundus tendon after injections of insoluble steroid for a trigger finger. J Hand Surg Eur Vol 2011; 36:77–78. [DOI] [PubMed] [Google Scholar]
- 11.Mills SP, Charalambous CP, Hayton MJ. Bilateral rupture of the extensor pollicis longus tendon in a professional goalkeeper following steroid injections for extensor tenosynovitis. Hand Surg 2009; 14:135–137. [DOI] [PubMed] [Google Scholar]
- 12.Smith AG, Kosygan K, Williams H, et al. Common extensor tendon rupture following corticosteroid injection for lateral tendinosis of the elbow. Br J Sports Med 1999; 33:423–424.discussion 4–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hugate R, Pennypacker J, Saunders M, et al. The effects of intratendinous and retrocalcaneal intrabursal injections of corticosteroid on the biomechanical properties of rabbit Achilles tendons. J Bone Joint Surg Am Vol 2004; 86-A:794–801. [DOI] [PubMed] [Google Scholar]
- 14.Mikolyzk DK, Wei AS, Tonino P, et al. Effect of corticosteroids on the biomechanical strength of rat rotator cuff tendon. J Bone Joint Surg Am Vol 2009; 91:1172–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bickel KD. Flexor pollicis longus tendon rupture after corticosteroid injection. J Hand Surg 1996; 21:152–153. [DOI] [PubMed] [Google Scholar]
- 16.Fredberg U. Local corticosteroid injection in sport: review of literature and guidelines for treatment. Scand J Med Sci Sports 1997; 7:131–139. [DOI] [PubMed] [Google Scholar]
- 17.Malavolta EA, Assuncao JH, Guglielmetti CL, et al. Accuracy of preoperative MRI in the diagnosis of disorders of the long head of the biceps tendon. Eur J Radiol 2015; 84:2250–2254. [DOI] [PubMed] [Google Scholar]
- 18.Leversedge FJ, Zelouf D, Williams C, et al. Flexor tendon grafting to the hand: an assessment of the intrasynovial donor tendon—a preliminary single-cohort study. J Hand Surg 2000; 25:721–730. [DOI] [PubMed] [Google Scholar]
- 19.Jakubietz MG, Jakubietz DF, Gruenert JG, et al. Adequacy of palmaris longus and plantaris tendons for tendon grafting. J Hand Surg 2011; 36:695–698. [DOI] [PubMed] [Google Scholar]
- 20.Tsujimoto Y, Ryoke K, Yamagami N, et al. Delineation of extensor tendon of the hand by MRI: usefulness of “soap-bubble” mip processing technique. Hand Surg 2015; 20:93–98. [DOI] [PubMed] [Google Scholar]
- 21.Fadale PD, Wiggins ME. Corticosteroid injections: their use and abuse. J Am Acad Orthop Surg 1994; 2:133–140. [DOI] [PubMed] [Google Scholar]
- 22.Moore JS. De Quervain's tenosynovitis. Stenosing tenosynovitis of the first dorsal compartment. J Occup Environ Med 1997; 39:990–1002. [DOI] [PubMed] [Google Scholar]


