Abstract
Drinking within recommended limits is highly prevalent in much of the world, and strong epidemiological associations exist between moderate alcohol consumption and risk of several major chronic diseases, including coronary heart disease, diabetes, and breast cancer. In many cases, plausible biological mediators for these associations have been identified in randomized trials, but gold-standard evidence that moderate drinking causes or prevents any chronic disease remains elusive and important concerns about available evidence have been raised. Although long-term randomized trials to test the observed associations have been termed impossible, clinical investigators have now successfully completed randomized trials of complex nutritional interventions in a variety of settings, along with trials of alcohol consumption itself of up to two years duration. The successful completion of these trials suggests that objections to the execution of a full-scale long-term clinical trial of moderate drinking on chronic disease are increasingly untenable. We present potential lessons learned for such a trial and discuss key features to maximize its feasibility and value.
Ethanol is among the psychoactive substances most widely used by humans worldwide, and has perhaps a longer history of discretionary human use than any equivalent molecule. Indeed, over half of Americans report alcohol use within the last month, a proportion that has remained largely stable over decades.(Substance Abuse and Mental Health Services Administration, 2014) The World Health Organization estimates that 38% of all individuals aged 15 and older worldwide consumed alcohol in the past 12 months.(Global Status Report on Alcohol and Health,(2014) Further, although alcohol abuse remains a global scourge, most drinkers appear to consume alcohol largely within recommended limits (i.e., ≤2 drinks per day for men and ≤1 for women).
Given the widespread use of alcohol within recommended limits, or moderate drinking, it might be assumed that the health effects of this use would be clearly and firmly established. Unfortunately, this assumption is mistaken. Although literally hundreds of studies on moderate drinking in humans have been published, these essentially all are either observational (i.e., descriptive studies or analytic designs) or small trials that are limited in time and scope. Truly experimental studies that would shed light on the health consequences of alcohol consumption within recommended limits have, to date, simply not been attempted. This deficit has spawned impressive controversy about the true health consequences of moderating drinking that has reached the highest levels of the U.S. and international biomedical infrastructure.(Lauer and Sorlie, 2009, Moller, 2016)
Here, we address this issue in several steps. First, we briefly review the existing data on alcohol use and chronic disease to summarize its posited effects, both negative and positive. Second, we review existing intermediate-term trials of alcohol consumption that bear on the feasibility of longer-term experimental studies, including an updated systematic review of all alcohol trials. Third, we examine selected recent successful trials of other complex behavioral factors, particularly related to diet, that also speak to the feasibility of a long-term alcohol trial. Finally, we review general principles that can be drawn from these experiences that should inform future efforts to provide definitive evidence about the chronic health consequences of regular alcohol consumption.
Existing Studies
Our knowledge regarding the health effects of alcohol consumption within recommended limits might best be grouped into two complementary approaches – observational studies that have now reached epic proportions in sample size and duration, and feeding studies that have assessed the immediate and short-term effects of alcohol on behavior, biochemical pathways, and similar social or physiological endpoints. Clearly, neither of these approaches represents gold-standard evidence in biomedical research – only a long-term randomized trial of clinical endpoints would meet that standard – but they have particular limitations that necessitate caution in their interpretation.
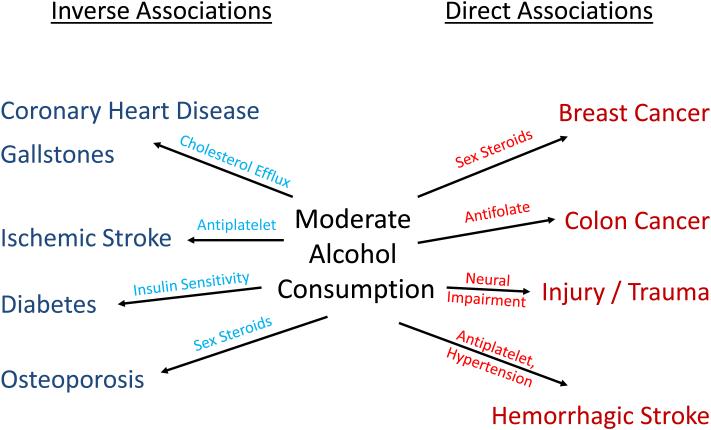
Observational studies of the effects of alcohol consumption on chronic disease have identified a number of consistent associations (Figure).(Gunzerath et al., 2004) Perhaps the most consistent adverse effect of moderate drinking identified in these studies is a dose-dependent higher risk of breast cancer that appears to rise throughout the usual range of consumption. Pooled analyses from large cohort studies suggest a 5-10% relative increment in risk for each 10 gram/day increment in intake.(Romieu et al., 2015, Smith-Warner et al., 1998) Although studies differ, many suggest the largest increase in risk for hormone-sensitive tumors, an important link to the effect of alcohol in feeding studies noted below.(Lew et al., 2009, Li et al., 2010) Although other cancers have also been associated with alcohol consumption, higher risk associated with intake within recommended limits has most strongly been linked to upper digestive (i.e., oral, esophageal) malignancies, with impressive synergy noted between drinking and smoking.(Ansary-Moghaddam et al., 2009) The International Agency for Research on Cancer has also implicated alcohol use in colorectal cancer, although cohort studies do not consistently find higher risk within recommended limits of consumption.(International Agency for Research on Cancer, 2010, Cho et al., 2004)
Fig. 1.
Proposed associations of moderate alcohol consumption with chronic disease.
Other adverse health consequences of alcohol intake within recommended limits are less well-documented. Hepatotoxicity and cirrhosis are not confirmed consequences of this level of alcohol exposure,(Corrao et al., 1991) although they may be among individuals with risk factors like hepatitis virus B or C infection.(Poynard et al., 1997) In some studies, injuries requiring hospital attention also increase with alcohol use within recommended limits,(Cherpitel et al., 1995) although it is unclear if this may reflect episodic binges among otherwise moderate drinkers. Hypertension is clearly a consequence of heavy drinking,(Klatsky, 1996) but has also been variably associated with more moderate intake particularly among men;(Briasoulis et al., 2012) underreporting has been cited to explain this inconsistency.(Klatsky et al., 2006) Similarly, heavy drinking is a risk factor for atrial fibrillation, but consumption within recommended limits has only variably been associated with higher risk. (Conen et al., 2008, Tolstrup et al., 2016)
Possible benefit related to moderate alcohol intake has been subjected to rigorous observational study since the early 1970’s,(Klatsky et al., 1974) with isolated anecdotal reports dating back considerably longer.(Leary, 1931) The best documented of the diseases found to be lower among moderate drinkers is myocardial infarction, which has been examined in dozens of large-scale prospective studies. Cumulative meta-analysis suggests that a risk reduction of approximately 29% has been largely unchanged by new studies since ~1990, highlighting the stability of this estimate.(Ronksley et al., 2011) Lower risk appears to plateau at approximately 1-2 drinks daily (i.e., at the upper limits of recommended intake). Alcohol consumption has also been associated with lower incidence of myocardial infarction among high-risk subjects, such as diabetic individuals, whose higher baseline risk could provide for greater power in a clinical trial,(Koppes et al., 2006) and with lower risk of other forms of coronary heart disease that might comprise a composite endpoint, such as revascularization and unstable angina.(Mukamal et al., 2006, Britton et al., 2009)
Congestive heart failure, the most common cause of hospitalization among elders in the U.S., also appears to be lower among drinkers within recommended limits; the degree to which this reflects direct effects on the heart and vasculature versus indirect effects via lower risk of myocardial infarction is not yet settled.(Padilla et al., 2010)
Despite the strong similarities between myocardial infarction and stroke, their relationships with alcohol consumption in observational studies differ meaningfully. One of the two major stroke types, hemorrhagic stroke, is associated in a direct, positive manner with alcohol intake.(Reynolds et al., 2003) Ischemic stroke, the much more common form in Western nations, is associated with alcohol intake in a J-shaped manner, with lower risk that nadirs at less-than-daily drinking and with apparent risk reduction closer to 20%.
A third major chronic disease inversely associated with alcohol intake within recommended limits is diabetes, with a dose-response relationship largely similar to that for coronary heart disease.(Koppes et al., 2005) Finally, several other conditions have been inversely related to moderate drinking in at least several observational studies, including osteoporosis, hip fracture, cholelithiasis, and dementia.(Leitzmann et al., 1999, Berg et al., 2008, Letenneur, 2007)
Effects of Alcohol in Interventional Studies
Despite the lack of large, long-term trials of alcohol consumption, it has been subjected to dozens of smaller studies, mainly in crossover designs, that aim to test its effects on established biochemical pathways leading to major chronic diseases. While these feeding studies clearly cannot replace a formal randomized trial on hard endpoints, they provide unconfounded estimates of physiological effects of alcohol that, in combination with epidemiology, provide useful insight into the probable long-term effects of moderate drinking (Figure).(Rimm et al., 1999)
Feeding studies have predominantly examined the effects of alcohol on lipids, glycemia, and inflammation.(Brien et al., 2011) First, alcohol consumption raises levels of high-density lipoprotein cholesterol (HDL-C) and its major protein cargo, apolipoprotein-A1. All types of alcoholic beverage have this effect.(van der Gaag et al., 1999) Although this increase might be expected to lower risk of CHD, debate about the causal effect of HDL-C continues; nonetheless, alcohol also increases the capacity of plasma to efflux cholesterol from macrophages,(Beulens et al., 2004) which has been associated with lower CHD risk independent of HDL-C.(Rohatgi et al., 2014) In tandem, alcohol consumption increases circulating triglycerides, but only at above-recommended doses.(Brien et al., 2011) Second, alcohol intake increases levels of adiponectin, an adipokine that increases insulin sensitivity in animal models and is inversely associated with risk of diabetes.(Brien et al., 2011) Concordant with this, alcohol consumption reduces levels of fasting insulin and hemoglobin A1c.(Schrieks et al., 2015) Third, alcohol intake reduces circulating levels of fibrinogen, an acute phase reactant produced by the liver, much like C-reactive protein. Although some studies have also found that alcohol intake reduces other markers of inflammation,(Sierksma et al., 2002, Marfella et al., 2006) these effects have not been demonstrated with sufficient consistency to be firmly established.
Intervention studies also suggest effects of alcohol on at least two important pathways. The first of these are measures of platelet function, although platelet assays tend to be insufficiently well-standardized to enable ready pooling. Nonetheless, acute measurements following ethanol ingestion suggest that alcohol can prolong bleeding time and in vitro estimates of platelet coagulability; limited feeding studies over several days also support this finding.(Deykin et al., 1982, Elmer et al., 1984, Pikaar et al., 1987) These effects might be expected to reduce ischemic events at the cost of increased hemorrhagic events, roughly consistent with the epidemiological evidence noted above. The second suggestive pathway is an increase in sex steroid hormones, particularly estrone and dehydroepiandrosterone sulfate. The latter has been observed among both sexes,(Sierksma et al., 2004, Reichman et al., 1993) while the former has been observed among both pre- and postmenopausal women.(Mahabir et al., 2004) As with platelet function, these effects correspond surprisingly concordantly with epidemiological observations, as they would generally be expected to increase breast cancer risk but increase bone density.
Intermediate-Term Interventional Studies
Feeding studies have provided alcohol for widely disparate durations of time (and doses), ranging from single-dose experiments to trials over several weeks. However, two studies of twelve months duration or longer now exist, and these provide useful evidence both of plausibility for a long-term trial and of the generalizability of short-term trials to longer-term outcomes.
From an historical standpoint, investigators from the US Department of Agriculture conducted two seminal crossover studies, testing three months of alcohol exposure among premenopausal women and four months among postmenopausal women.(Reichman et al., 1993, Hartman et al., 2005) The earlier trial was the first ever to administer alcohol to an ambulatory population over several months and provided important evidence of the hormonal effects of alcohol, with a highly rigorous study design, large sample size for an intensive feeding study, and careful menstrual and dietary controls. As expected, levels of HDL-C rose, further supporting adherence of the subjects to their assigned arms. However, a few features limit the degree to which these trials inform a possible long-term trial, particularly in their intensive nature and stringent degree of control. All food and drink were provided to participants, clearly not a possibility for a long-term trial, and subjects presented repeatedly for phlebotomy and biochemical measurements. Alcohol was provided in the form of grain alcohol mixed with fruit juice.
Israeli investigators have performed two similar parallel-design trials among diabetic adults that comprised three months of intervention for the first trial and a full two years for the second.(Shai et al., 2007, Gepner et al., 2015) In both trials, the beverages used were commercially available – Israeli red or white wines (13-17 grams of ethanol daily) versus an Israeli non-alcoholic malt beverage (for the first trial) or mineral water (for the second).
The primary focus of the initial three-month trial was improvement in glycemic parameters and confirmed a benefit on fasting but not post-load glucose. Another focus of the trial was potential side effects of alcohol consumption, which directly inform the feasibility of longer-term trials. Although several modest differences were noted, the only symptom that differed significantly was improved ability to fall asleep in the alcohol group compared with control. Of equal note, from 109 enrolled subjects, 12 withdrew prior to study onset (most from the control group), which suggests that many participants will have unstated or even subconscious preferences that need to be aggressively solicited prior to enrollment and randomization. Put differently, the dropout suggests that perceived ‘value’ to participants needs to be as similar as possible in both arms.
This shorter trial provided the basis for a second, larger effort that is the longest randomized study of alcohol consumption yet performed. Shai and colleagues randomized 224 diabetic subjects in a 1:1:3 ratio to consume mineral water, white wine, or red wine, which was provided free of charge for two years. The trial focused on alcohol abstainers and excluded individuals who consumed more than 1 drink per week, a restriction that provides important context to the results. Subjects randomized to white wine demonstrated significant improvement in their fasting glucose compared to those assigned to water, while those in the red wine arm had a significant increase in their HDL-C, changes largely consistent with previous trials. Self-reported adherence to daily beverage intake approximated 80% in all three arms. Once again, the only symptomatic difference was an improvement in sleep among those in the wine groups. However, attrition differed significantly across arms, with two-year rates of retention of 94%, 88%, and 77% in the water, red wine, and white wine arms, respectively. While all three figures are promising, the difference among them may be explained by recruitment specifically of alcohol abstainers who found daily drinking difficult.
A particularly intriguing trial of alcohol consumption was conducted in Italy, where insulin-treated diabetic patients admitted with myocardial infarction were randomized to receive advice regarding a Mediterranean-type diet with or without the addition of 4 ounces daily of an Italian red wine for one year.(Marfella et al., 2006) The control group was asked to consume no alcohol, and thus this trial did not attempt to separate the effects of alcohol from those related to the non-alcoholic constituents of wine. The protocol included multiple visits over one year, including repeated echocardiography. A total of 131 patients enrolled in the study, of whom three withdrew consent and two were removed due to noncompliance (although reasons were not specified). Another eight patients died during the study period, presumably reflecting the entry criteria that required concomitant insulin-requiring diabetes and acute coronary heart disease. HDL-C rose significantly in both alcohol and abstention arms, but twice as much in the alcohol arm, confirming that compliance was good; repeated food diaries also confirmed adherence to abstention in the appropriate subjects.
Results of the trial were provocative. The alcohol arm had lower measures of several inflammatory factors, including C-reactive protein, IL-18, TNF-α, and IL-6, and lower levels of nitrotyrosine, a marker of oxidation. Fasting insulin levels and HOMA-IR also dropped significantly more in the alcohol arm than among controls. Perhaps most importantly, echocardiographic measures of left ventricular function improved more in the alcohol-treated subjects than controls, including left ventricular ejection fraction and myocardial performance index. These differences have potential prognostic implications for patients with coronary heart disease, even if it remains impossible to determine if they relate to a benefit of red wine or alcohol more generally.
To ensure that we identified all feeding studies of one year or longer that might inform a truly long-term trial, we performed an updated systematic review using our previously published search strategy.(Brien et al., 2011) As in our previous review, which concluded in 2009, we searched for alcohol intervention studies in adults from 2010 through June 2016 using Medline, without language restrictions for potentially relevant articles. The search strategy is included in Supplemental Table 1. Although the focus of the original review was on randomized controlled trials, whether crossover or parallel design, we present all studies which experimentally manipulated oral alcohol consumption here. Because we previously confirmed high inter-rater reliability for abstract review for this search, we used one investigator (KJM) to review abstracts for eligibility, and any that appeared to include experimental alcohol administration was selected for full text review for confirmation. From relevant studies, we extracted information on sample size, the duration of alcohol administration, the duration of additional follow-up (e.g., in a crossover), and the specific alcohol type (beer, wine, spirits, or ethanol).
The literature search identified 1,983 potentially eligible abstracts, from which 71 were selected for full-text review (Supplemental Figure 1; Supplemental Table 3). From these, we identified 60 studies that experimentally administered alcohol (Supplemental Table 2), of which one reported two different trials. Although a wide range of exposures and durations have been described, only the aforementioned Israeli trial of 2015 administered alcohol for as long as one year.
Trials of Other Complex Dietary Interventions
Although alcohol trials beyond two years have yet to be completed, the same cannot be said for other dietary interventions of equal or even greater complexity, where large trials with hard endpoints have now shown clear benefits of specific dietary patterns.
In the Lyon Diet Heart Study,(de Lorgeril et al., 1999) participants in the experimental group received formal advice to increase their intake of bread, green and root vegetables, fish, and fruit and replace red meat with poultry, beginning shortly after their index hospitalization and repeated at annual study visits. That group also received a supply of modified margarine enriched in α-linolenic acid, while participants in the control arm received no specific dietary advice.
Adherence to these dietary recommendations was ultimately confirmed by plasma fatty acid analysis, which demonstrated higher plasma levels of linolenic acid and eicosapentaenoic acid (a long-chain marine n-3 fatty acid) and lower levels of stearic acid (a saturated fatty acid) among intervention compared with control subjects.(de Lorgeril et al., 1994) Thus, despite a relatively modest intensity of intervention, participants differed significantly in key measures that differentiated their diets.
Although the sample size was increased (due to low event rates), the trial was stopped early because of a statistical benefit to treatment. When follow-up was completed after an average of four years of follow-up, assignment to the Mediterranean diet resulted in a 50-70% lower risk of recurrent cardiovascular events than did assignment to control.
The PREDIMED trial followed a somewhat similar model, enrolling high-risk adults albeit in primary prevention and randomizing them to a control low-fat diet or a Mediterranean diet supplemented with a discrete fat source (in this case, either olive oil or tree nuts).(Estruch et al., 2013) Testing of biomarkers related to olive oil or nut intake confirmed adherence over time, as did a number of formal questionnaires. Drop-out, while modest at 7%, was approximately twice as high in the low-fat diet arm as in the combined Mediterranean diet arm. Participants met twice with dieticians on a personal basis, followed by quarterly individual and group meetings led by dieticians. Of note, the advice received by usual drinkers in the Mediterranean diet arm included a recommendation to consume a glass of wine daily with meals, and daily wine intake (but not overall alcohol intake) was greater among those in the Mediterranean diet arms than among those randomized to a low-fat diet.
The PREDIMED investigators also increased the duration of their study due to lower-than-expected event rates, yet the trial was closed early due to a clear benefit in favor of the Mediterranean diet. Ultimately, a total of 7,447 participants enrolled and were followed for a median of 4.8 years. Relative to the low-fat arm, assignment to either Mediterranean diet arm led to a 30% decrease in the risk of cardiovascular disease
A few other long-term trials of diet exist, although none have dramatically changed clinical practice. University of Copenhagen investigators conducted a six-month trial of a Nordic diet compared with a standard Danish diet among 181 adults, using an innovative but expensive model in which all foods were provided in a research ‘supermarket.’(Poulsen et al., 2014) To improve adherence, participants underwent formal cooking instruction and received tailored cookbooks. The trial showed benefits on both weight and blood pressure among those randomized to the Nordic diet, with continued benefit amongst those who remained adherent six months later.(Poulsen et al., 2015) In the POUNDS LOST Trial,(Sacks et al., 2009) a comparison of weight-loss diets over two years, participants were assigned one of four diets based upon macronutrient content, although participants bought and prepared their own foods. Participants attended individual counseling sessions every eight weeks and group sessions at least two of every four weeks for the entire study period. All four diets resulted in weight loss, although weight loss primarily occurred in the first six months with weight gain thereafter. Across three biomarkers – HDL-cholesterol, respiratory quotient, and urinary nitrogen excretion – changes in biomarkers confirmed the expected directions of effect for each of the diets, although the target goals for macronutrient content were generally not reached.
An important controversy surrounds the largest diet trial to date, the Women’s Health Initiative (WHI), a complex factorial RCT that tested postmenopausal estrogens, calcium with vitamin D, and a low-fat diet. The dietary arm asked participants to reduce total fat to 20% of caloric intake, increase fruit and vegetable consumption to 5 or more servings per day, and increase grains to 6 or more servings daily. An intensive behavioral modification program required 18 group sessions with trained nutritionists in the first year and 4 sessions per year in subsequent years. No specific advice regarding other micro- or macronutrients was included.
Based upon dietary questionnaires, the WHI dietary strategy was moderately but imperfectly successful.(Howard et al., 2006) From a baseline of 38% of energy intake from fat in both arms, participants in the low-fat diet arm reported a mean intake of 29% of calories from fat at year 6, compared with 37% among control subjects. Although this result suggests a clear difference between the groups, it was approximately half as large as originally targeted. Moreover, the two groups did not differ in follow-up triglyceride levels despite sizable differences in reported carbohydrate intake, raising questions about overestimation of adherence.(Michels and Willett, 2009) Despite the moderate differences observed between the two groups, they did not differ in the incidence of cardiovascular disease, diabetes, or cancer.(Howard et al., 2006, Beresford et al., 2006, Tinker et al., 2008)
Lessons for a Randomized Trial of Moderate Drinking
In our opinion, previous trials of both alcohol consumption and other nutritional interventions offer specific, practical lessons for the design and conduct of a trial of moderate drinking (Table). First and foremost, they highlight that complex trials over many years can and should be done. When contrasted with the change in behavior required for a moderate drinking trial, the full-scale interventions implemented in the Lyon Diet Heart Study and PREDIMED, as but two examples, were substantially more challenging, comprehensive, and diverse, requiring modifications in virtually every aspect of participants’ diet. While the difficulty of altering alcohol consumption should not be underestimated, we would argue that it is certainly no more difficult than modifying a complete diet. Indeed, the PREDIMED diet, while not a trial of alcohol intake per se, addressed wine as but one of many components of the Mediterranean diet. If full diets (including wine) can be successfully modified to demonstrate cardiovascular benefit, then it would seem feasible to address alcohol in a similar manner.
Table.
Lessons from Previous Trials of Alcohol Consumption and Other Dietary Interventions
| Lesson | Supporting Evidence |
|---|---|
| 1. Even complex interventions are feasible | Long-term trials that manipulated full diets (including alcohol) have been successfully completed |
| 2. Use beverages that participants already consume to maximize adherence |
Culturally-concordant changes to diet are easiest to effect, and all intermediate-term alcohol trials in free-living populations have used commercially-available beverages |
| 3. Test a dose of alcohol that would be acceptable to individuals who would also accept abstention |
Extreme changes in intake are difficult to sustain, and all intermediate-term trials in free- living populations have compared one drink daily to abstention |
| 4. Provide an incentive or compensation to adopt changes in alcohol consumption |
Long-term dietary trials have provided at least some food component, even if limited, as have longer-term trials of alcohol |
| 5. Ensure that all arms appear attractive to participants |
Drop-out rates are typically higher in the arms that are perceived as less desirable |
| 6. Recruit individuals at above-average risk for endpoints of interest |
Higher-risk individuals may be more likely to enter and remain adherent in prevention trials and have been used in previous dietary and alcohol trials |
| 7. Establish endpoints using known effects of alcohol |
Coronary heart disease and diabetes are the outcomes most consistently associated with benefit from moderate drinking; HDL-C appears to be a reasonable biomarker of compliance at the population level |
Second, previous trials of alcohol strongly suggest that a long-term trial of alcohol consumption is feasible when beverages most culturally acceptable to the population in question are used. At the same time, the WHI experience suggests that dietary changes that are too extreme will be difficult to implement effectively. Put differently, asking participants to change both their alcohol intake and their alcoholic beverage preference at the same time risks substantial loss of adherence, and hence natural beverage preferences should be preserved where possible. Insofar as the epidemiological evidence generally suggests similar effects of all alcoholic beverages for coronary heart disease,(Rimm et al., 1996) if not necessarily for all biochemical measures,(Chiva-Blanch et al., 2013) use of diverse commercially-available beverages likely to be consumed regularly in any long-term trial seems advisable. In practice, such a design could be implemented in several ways. These include allowing participants to choose their own beverage if randomized to alcohol, using only one form of alcohol and restricting to participants who prefer that beverage type, or – if the differences between beverages are to be studied – only randomizing individuals who already consume all three beverage types with regularity. In all cases, participants will need counseling to recognize the differences in energy content of their beverage choices.
A third lesson, and corollary to the previous one, also borrows from previous alcohol trials and the WHI experience. Longer-term trials in free-living populations have tested one serving of alcohol per day versus abstention, while dose-response relationships have been examined only in more controlled settings. While a long-term trial testing multiple doses of alcohol would powerfully inform debate about the risks and benefits of moderate drinking, it would also necessitate much larger changes in alcohol intake among participants. For example, even if non-drinkers were excluded, very light drinkers might be randomized to increase their alcohol intake more than 10-fold (i.e., from 1 to 14 drinks per week); the WHI experience cautions against expecting such large changes to endure over time. The two-year Israeli trial similarly suggests that long-term alcohol intake is unlikely to endure among true abstainers. Randomizing occasional drinkers to modify their intake downward to abstention or upward to one drink daily (i.e., changing modestly in both directions) seems most likely to succeed.
Fourth, the most successful trials in both alcohol and other dietary interventions have relied on more than advice alone. While a trial that simply randomly assigned individuals to receive advice to drink alcohol regularly or not would have several advantages, particularly in cost, it may ultimately prove uninformative if insufficient contrast in ethanol intake between the intervention arms emerges. Whether actual alcoholic beverages should be provided is unclear, as regulatory hurdles differ widely both within and between countries, but long-term adherence based solely on advice – even sustained advice – should not be readily assumed.
Fifth, in the first Israeli alcohol trial and in PREDIMED, drop-out rates were higher in the control arms than in the intervention arms, presumably because the control arms appeared less desirable. Indeed, in those trials, the intervention arm received olive oil, nuts, or wine, any of which might have been viewed as desirable for potential subjects. Hence, the need to provide some tangible product to improve adherence (the fourth lesson) should be balanced by attention to the attraction that each arm might hold to potential participants. Marked asymmetry in this regard can lead to asymmetric retention rates.
Sixth, the successful long-term dietary and longer-term alcohol trials in free-living populations have focused upon clinical populations, recruiting individuals at above-average risk for the endpoints in question (e.g., diabetic adults in Israeli and Italian alcohol trials, high-risk adults in PREDIMED, survivors of acute myocardial infarction in Lyon). This has an obvious advantage in requiring smaller sample sizes, due to higher event rates, but may also lead to recruitment of individuals with greater personal investment in the trial’s success. While clinical judgment is needed to tailor the appropriate entry criteria for any trial, the success of these trials suggests that individuals at above-average risk are likely to serve as the best source population for alcohol trials going forward.
Finally, the existing clinical trial and epidemiological evidence provides useful insight into the endpoints that a clinical trial of moderate drinking might be best poised to tackle. Specifically, in the absence of a gold-standard biosensor for alcohol (the subject of a recent federal contest),(Announcement of Requirements and Registration, (2015) HDL-C has served as a consistent marker of adherence in nearly all feeding studies of alcohol consumption, although more specific markers have been used in clinical trials of alcohol misuse,(Jatlow et al., 2014) and metabolomic approaches offer promise for identifying yet others.(Andersen et al., 2014) Even if HDL-C is an imperfect marker at the individual level, groups of individuals assigned to alcohol or abstention should readily demonstrate differences in HDL-C observable within a few weeks of assignment, providing early insight into compliance and avoiding the difficulty in interpretation that plagued the WHI. Epidemiological studies also suggest that coronary heart disease and diabetes represent the most plausibly improved endpoints in a trial of moderate drinking, with somewhat weaker evidence for ischemic (but not hemorrhagic) stroke; a composite outcome of major cardiovascular events similar to that used in pharmaceutical trials appears feasible. Safety signals to be studied should include at least hypertension, injury, and breast cancer.
Conclusions
In summary, a long-term trial of moderate drinking is no longer beyond consideration. Dietary trials that could easily be considered far more difficult have been successfully completed, and alcohol trials of up to two years confirm the feasibility of manipulating alcohol intake, provided the right beverage, dose, and population are used. Definitive answers to the controversies surrounding moderate alcohol intake may finally be forthcoming.
Supplementary Material
Acknowledgements
This work was supported by grants U13AA023452, U34AA023258, and U10AA025286 from the National Institute on Alcohol Abuse and Alcoholism.
Footnotes
Disclosures: Drs. Hendriks and Dragsted have conducted short-term feeding studies with alcohol at institutions (TNO, University of Copenhagen) that have received partial support from members of the alcohol industry. Dr. Krystal has served on the advisory boards and/or holds stock in several companies with interests in psychiatric disorders.
References
- Global Status Report on Alcohol and Health. World Health Organization; Geneva: 2014. [Google Scholar]
- SERVICES, D. O. H. A. H., editor. Announcement of Requirements and Registration for “A Wearable Alcohol Biosensor” Challenge. Washington, D.C.: 2015. [Google Scholar]
- ANDERSEN MB, KRISTENSEN M, MANACH C, PUJOS-GUILLOT E, POULSEN SK, LARSEN TM, ASTRUP A, DRAGSTED L. Discovery and validation of urinary exposure markers for different plant foods by untargeted metabolomics. Anal Bioanal Chem. 2014;406:1829–44. doi: 10.1007/s00216-013-7498-5. [DOI] [PubMed] [Google Scholar]
- ANSARY-MOGHADDAM A, HUXLEY RR, LAM TH, WOODWARD M. The risk of upper aero digestive tract cancer associated with smoking, with and without concurrent alcohol consumption. Mt Sinai J Med. 2009;76:392–403. doi: 10.1002/msj.20125. [DOI] [PubMed] [Google Scholar]
- BERESFORD SA, JOHNSON KC, RITENBAUGH C, LASSER NL, SNETSELAAR LG, BLACK HR, ANDERSON GL, ASSAF AR, BASSFORD T, BOWEN D, BRUNNER RL, BRZYSKI RG, CAAN B, CHLEBOWSKI RT, GASS M, HARRIGAN RC, HAYS J, HEBER D, HEISS G, HENDRIX SL, HOWARD BV, HSIA J, HUBBELL FA, JACKSON RD, KOTCHEN JM, KULLER LH, LACROIX AZ, LANE DS, LANGER RD, LEWIS CE, MANSON JE, MARGOLIS KL, MOSSAVAR-RAHMANI Y, OCKENE JK, PARKER LM, PERRI MG, PHILLIPS L, PRENTICE RL, ROBBINS J, ROSSOUW JE, SARTO GE, STEFANICK ML, VAN HORN L, VITOLINS MZ, WACTAWSKI-WENDE J, WALLACE RB, WHITLOCK E. Low-fat dietary pattern and risk of colorectal cancer: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295:643–54. doi: 10.1001/jama.295.6.643. [DOI] [PubMed] [Google Scholar]
- BERG KM, KUNINS HV, JACKSON JL, NAHVI S, CHAUDHRY A, HARRIS KA, JR., MALIK R, ARNSTEN JH. Association between alcohol consumption and both osteoporotic fracture and bone density. Am J Med. 2008;121:406–18. doi: 10.1016/j.amjmed.2007.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BEULENS JW, SIERKSMA A, VAN TOL A, FOURNIER N, VAN GENT T, PAUL JL, HENDRIKS HF. Moderate alcohol consumption increases cholesterol efflux mediated by ABCA1. J Lipid Res. 2004;45:1716–23. doi: 10.1194/jlr.M400109-JLR200. [DOI] [PubMed] [Google Scholar]
- BRIASOULIS A, AGARWAL V, MESSERLI FH. Alcohol consumption and the risk of hypertension in men and women: a systematic review and meta-analysis. J Clin Hypertens (Greenwich) 2012;14:792–8. doi: 10.1111/jch.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BRIEN SE, RONKSLEY PE, TURNER BJ, MUKAMAL KJ, GHALI WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ. 2011;342:d636. doi: 10.1136/bmj.d636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BRITTON KA, GAZIANO JM, SESSO HD, DJOUSSE L. Relation of alcohol consumption and coronary heart disease in hypertensive male physicians (from the Physicians' Health Study) The American journal of cardiology. 2009;104:932–5. doi: 10.1016/j.amjcard.2009.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CHERPITEL CJ, TAM T, MIDANIK L, CAETANO R, GREENFIELD T. Alcohol and non-fatal injury in the U.S. general population: a risk function analysis. Accid Anal Prev. 1995;27:651–61. doi: 10.1016/0001-4575(95)00011-n. [DOI] [PubMed] [Google Scholar]
- CHIVA-BLANCH G, ARRANZ S, LAMUELA-RAVENTOS RM, ESTRUCH R. Effects of wine, alcohol and polyphenols on cardiovascular disease risk factors: evidences from human studies. Alcohol Alcohol. 2013;48:270–7. doi: 10.1093/alcalc/agt007. [DOI] [PubMed] [Google Scholar]
- CHO E, SMITH-WARNER SA, RITZ J, VAN DEN BRANDT PA, COLDITZ GA, FOLSOM AR, FREUDENHEIM JL, GIOVANNUCCI E, GOLDBOHM RA, GRAHAM S, HOLMBERG L, KIM DH, MALILA N, MILLER AB, PIETINEN P, ROHAN TE, SELLERS TA, SPEIZER FE, WILLETT WC, WOLK A, HUNTER DJ. Alcohol intake and colorectal cancer: a pooled analysis of 8 cohort studies. Ann Intern Med. 2004;140:603–13. doi: 10.7326/0003-4819-140-8-200404200-00007. [DOI] [PubMed] [Google Scholar]
- CONEN D, TEDROW UB, COOK NR, MOORTHY MV, BURING JE, ALBERT CM. Alcohol consumption and risk of incident atrial fibrillation in women. JAMA. 2008;300:2489–96. doi: 10.1001/jama.2008.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CORRAO G, ARICO S, RUSSO R, CARLE F, GALATOLA G, TORCHIO PF, MOIRAGHI AR, DI ORIO F, DE LA PIERRE M. Alcohol consumption and non-cirrhotic chronic hepatitis: a case-control study. Int J Epidemiol. 1991;20:1037–42. doi: 10.1093/ije/20.4.1037. [DOI] [PubMed] [Google Scholar]
- DE LORGERIL M, RENAUD S, MAMELLE N, SALEN P, MARTIN JL, MONJAUD I, GUIDOLLET J, TOUBOUL P, DELAYE J. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994;343:1454–9. doi: 10.1016/s0140-6736(94)92580-1. [DOI] [PubMed] [Google Scholar]
- DE LORGERIL M, SALEN P, MARTIN J-L, MONJAUD I, DELAYE J, MAMELLE N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: Final report of the Lyon Diet Heart Study. Circulation. 1999;99:779–785. doi: 10.1161/01.cir.99.6.779. [DOI] [PubMed] [Google Scholar]
- DEYKIN D, JANSON P, MCMAHON L. Ethanol potentiation of aspirin-induced prolongation of the bleeding time. N Engl J Med. 1982;306:852–4. doi: 10.1056/NEJM198204083061406. [DOI] [PubMed] [Google Scholar]
- ELMER O, GORANSSON G, ZOUCAS E. Impairment of primary hemostasis and platelet function after alcohol ingestion in man. Haemostasis. 1984;14:223–8. doi: 10.1159/000215060. [DOI] [PubMed] [Google Scholar]
- ESTRUCH R, ROS E, MARTINEZ-GONZALEZ MA. Mediterranean diet for primary prevention of cardiovascular disease. N Engl J Med. 2013;369:676–7. doi: 10.1056/NEJMc1306659. [DOI] [PubMed] [Google Scholar]
- GEPNER Y, GOLAN R, HARMAN-BOEHM I, HENKIN Y, SCHWARZFUCHS D, SHELEF I, DURST R, KOVSAN J, BOLOTIN A, LEITERSDORF E, SHPITZEN S, BALAG S, SHEMESH E, WITKOW S, TANGI-ROSENTAL O, CHASSIDIM Y, LIBERTY IF, SARUSI B, BEN-AVRAHAM S, HELANDER A, CEGLAREK U, STUMVOLL M, BLUHER M, THIERY J, RUDICH A, STAMPFER MJ, SHAI I. Effects of Initiating Moderate Alcohol Intake on Cardiometabolic Risk in Adults With Type 2 Diabetes: A 2-Year Randomized, Controlled Trial. Annals of internal medicine. 2015;163:569–79. doi: 10.7326/M14-1650. [DOI] [PubMed] [Google Scholar]
- GUNZERATH L, FADEN V, ZAKHARI S, WARREN K. National Institute on Alcohol Abuse and Alcoholism report on moderate drinking. Alcohol Clin Exp Res. 2004;28:829–47. doi: 10.1097/01.alc.0000128382.79375.b6. [DOI] [PubMed] [Google Scholar]
- HARTMAN TJ, BAER DJ, GRAHAM LB, STONE WL, GUNTER EW, PARKER CE, ALBERT PS, DORGAN JF, CLEVIDENCE BA, CAMPBELL WS, TOMER KB, JUDD JT, TAYLOR PR. Moderate alcohol consumption and levels of antioxidant vitamins and isoprostanes in postmenopausal women. Eur J Clin Nutr. 2005;59:161–8. doi: 10.1038/sj.ejcn.1602051. [DOI] [PubMed] [Google Scholar]
- HOWARD BV, VAN HORN L, HSIA J, MANSON JE, STEFANICK ML, WASSERTHEIL-SMOLLER S, KULLER LH, LACROIX AZ, LANGER RD, LASSER NL, LEWIS CE, LIMACHER MC, MARGOLIS KL, MYSIW WJ, OCKENE JK, PARKER LM, PERRI MG, PHILLIPS L, PRENTICE RL, ROBBINS J, ROSSOUW JE, SARTO GE, SCHATZ IJ, SNETSELAAR LG, STEVENS VJ, TINKER LF, TREVISAN M, VITOLINS MZ, ANDERSON GL, ASSAF AR, BASSFORD T, BERESFORD SA, BLACK HR, BRUNNER RL, BRZYSKI RG, CAAN B, CHLEBOWSKI RT, GASS M, GRANEK I, GREENLAND P, HAYS J, HEBER D, HEISS G, HENDRIX SL, HUBBELL FA, JOHNSON KC, KOTCHEN JM. Low-fat dietary pattern and risk of cardiovascular disease: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295:655–66. doi: 10.1001/jama.295.6.655. [DOI] [PubMed] [Google Scholar]
- INTERNATIONAL AGENCY FOR RESEARCH ON CANCER 2010 . IARC Monogr Eval Carcinog Risks Hum. Lyon: Alcohol consumption and ethyl carbamate. [PMC free article] [PubMed] [Google Scholar]
- JATLOW PI, AGRO A, WU R, NADIM H, TOLL BA, RALEVSKI E, NOGUEIRA C, SHI J, DZIURA JD, PETRAKIS IL, O'MALLEY SS. Ethyl glucuronide and ethyl sulfate assays in clinical trials, interpretation, and limitations: results of a dose ranging alcohol challenge study and 2 clinical trials. Alcohol Clin Exp Res. 2014;38:2056–65. doi: 10.1111/acer.12407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KLATSKY AL. Alcohol and hypertension. Clin Chim Acta. 1996;246:91–105. doi: 10.1016/0009-8981(96)06230-4. [DOI] [PubMed] [Google Scholar]
- KLATSKY AL, FRIEDMAN GD, SIEGELAUB AB. Alcohol consumption before myocardial infarction. Results from the Kaiser-Permanente epidemiologic study of myocardial infarction. Ann Intern Med. 1974;81:294–301. doi: 10.7326/0003-4819-81-3-294. [DOI] [PubMed] [Google Scholar]
- KLATSKY AL, GUNDERSON EP, KIPP H, UDALTSOVA N, FRIEDMAN GD. Higher prevalence of systemic hypertension among moderate alcohol drinkers: an exploration of the role of underreporting. J Stud Alcohol. 2006;67:421–8. doi: 10.15288/jsa.2006.67.421. [DOI] [PubMed] [Google Scholar]
- KOPPES LL, DEKKER JM, HENDRIKS HF, BOUTER LM, HEINE RJ. Moderate alcohol consumption lowers the risk of type 2 diabetes: a meta-analysis of prospective observational studies. Diabetes Care. 2005;28:719–25. doi: 10.2337/diacare.28.3.719. [DOI] [PubMed] [Google Scholar]
- KOPPES LL, DEKKER JM, HENDRIKS HF, BOUTER LM, HEINE RJ. Meta-analysis of the relationship between alcohol consumption and coronary heart disease and mortality in type 2 diabetic patients. Diabetologia. 2006;49:648–52. doi: 10.1007/s00125-005-0127-x. [DOI] [PubMed] [Google Scholar]
- LAUER MS, SORLIE P. Alcohol, cardiovascular disease, and cancer: treat with caution. J Natl Cancer Inst. 2009;101:282–3. doi: 10.1093/jnci/djp006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LEARY T. Therapeutic value of alcohol, with special consideration of relations of alcohol to cholesterol, and thus to diabetes, to arteriosclerosis, and to gallstones. N Engl J Med. 1931;205:231–242. [Google Scholar]
- LEITZMANN MF, GIOVANNUCCI EL, STAMPFER MJ, SPIEGELMAN D, COLDITZ GA, WILLETT WC, RIMM EB. Prospective study of alcohol consumption patterns in relation to symptomatic gallstone disease in men. Alcohol Clin Exp Res. 1999;23:835–41. [PubMed] [Google Scholar]
- LETENNEUR L. Moderate alcohol consumption and risk of developing dementia in the elderly: the contribution of prospective studies. Ann Epidemiol. 2007;17:S43–S45. [Google Scholar]
- LEW JQ, FREEDMAN ND, LEITZMANN MF, BRINTON LA, HOOVER RN, HOLLENBECK AR, SCHATZKIN A, PARK Y. Alcohol and Risk of Breast Cancer by Histologic Type and Hormone Receptor Status in Postmenopausal Women: The NIH-AARP Diet and Health Study. Am J Epidemiol. 2009 doi: 10.1093/aje/kwp120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LI CI, CHLEBOWSKI RT, FREIBERG M, JOHNSON KC, KULLER L, LANE D, LESSIN L, O'SULLIVAN MJ, WACTAWSKI-WENDE J, YASMEEN S, PRENTICE R. Alcohol consumption and risk of postmenopausal breast cancer by subtype: the women's health initiative observational study. J Natl Cancer Inst. 2010;102:1422–31. doi: 10.1093/jnci/djq316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MAHABIR S, BAER DJ, JOHNSON LL, DORGAN JF, CAMPBELL W, BROWN E, HARTMAN TJ, CLEVIDENCE B, ALBANES D, JUDD JT, TAYLOR PR. The effects of moderate alcohol supplementation on estrone sulfate and DHEAS in postmenopausal women in a controlled feeding study. Nutr J. 2004;3:11. doi: 10.1186/1475-2891-3-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MARFELLA R, CACCIAPUOTI F, SINISCALCHI M, SASSO FC, MARCHESE F, CINONE F, MUSACCHIO E, MARFELLA MA, RUGGIERO L, CHIORAZZO G, LIBERTI D, CHIORAZZO G, NICOLETTI GF, SARON C, D'ANDREA F, AMMENDOLA C, VERZA M, COPPOLA L. Effect of moderate red wine intake on cardiac prognosis after recent acute myocardial infarction of subjects with Type 2 diabetes mellitus. Diabet Med. 2006;23:974–81. doi: 10.1111/j.1464-5491.2006.01886.x. [DOI] [PubMed] [Google Scholar]
- MICHELS KB, WILLETT WC. The Women's Health Initiative Randomized Controlled Dietary Modification Trial: a post-mortem. Breast cancer research and treatment. 2009;114:1–6. doi: 10.1007/s10549-008-9972-x. [DOI] [PubMed] [Google Scholar]
- MOLLER L. Q&A – How can I drink alcohol safely? Geneva: 2016. [Online] Available: http://www.euro.who.int/en/health-topics/disease-prevention/alcohol-use/data-and-statistics/q-and-a-how-can-i-drink-alcohol-safely [Accessed 27 July 2016] [Google Scholar]
- MUKAMAL KJ, CHUNG H, JENNY NS, KULLER LH, LONGSTRETH WT, JR., MITTLEMAN MA, BURKE GL, CUSHMAN M, PSATY BM, SISCOVICK DS. Alcohol consumption and risk of coronary heart disease in older adults: the Cardiovascular Health Study. J Am Geriatr Soc. 2006;54:30–7. doi: 10.1111/j.1532-5415.2005.00561.x. [DOI] [PubMed] [Google Scholar]
- PADILLA H, MICHAEL GAZIANO J, DJOUSSE L. Alcohol consumption and risk of heart failure: a meta-analysis. Phys Sportsmed. 2010;38:84–9. doi: 10.3810/psm.2010.10.1812. [DOI] [PubMed] [Google Scholar]
- PIKAAR NA, WEDEL M, VAN DER BEEK EJ, VAN DOKKUM W, KEMPEN HJ, KLUFT C, OCKHUIZEN T, HERMUS RJ. Effects of moderate alcohol consumption on platelet aggregation, fibrinolysis, and blood lipids. Metabolism. 1987;36:538–43. doi: 10.1016/0026-0495(87)90163-6. [DOI] [PubMed] [Google Scholar]
- POULSEN SK, CRONE C, ASTRUP A, LARSEN TM. Long-term adherence to the New Nordic Diet and the effects on body weight, anthropometry and blood pressure: a 12-month follow-up study. Eur J Nutr. 2015;54:67–76. doi: 10.1007/s00394-014-0686-z. [DOI] [PubMed] [Google Scholar]
- POULSEN SK, DUE A, JORDY AB, KIENS B, STARK KD, STENDER S, HOLST C, ASTRUP A, LARSEN TM. Health effect of the New Nordic Diet in adults with increased waist circumference: a 6-mo randomized controlled trial. Am J Clin Nutr. 2014;99:35–45. doi: 10.3945/ajcn.113.069393. [DOI] [PubMed] [Google Scholar]
- POYNARD T, BEDOSSA P, OPOLON P. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825–32. doi: 10.1016/s0140-6736(96)07642-8. [DOI] [PubMed] [Google Scholar]
- REICHMAN ME, JUDD JT, LONGCOPE C, SCHATZKIN A, CLEVIDENCE BA, NAIR PP, CAMPBELL WS, TAYLOR PR. Effects of alcohol consumption on plasma and urinary hormone concentrations in premenopausal women. J Natl Cancer Inst. 1993;85:722–7. doi: 10.1093/jnci/85.9.722. [DOI] [PubMed] [Google Scholar]
- REYNOLDS K, LEWIS B, NOLEN JD, KINNEY GL, SATHYA B, HE J. Alcohol consumption and risk of stroke: a meta-analysis. JAMA. 2003;289:579–88. doi: 10.1001/jama.289.5.579. [DOI] [PubMed] [Google Scholar]
- RIMM EB, KLATSKY A, GROBBEE D, STAMPFER MJ. Review of moderate alcohol consumption and reduced risk of coronary heart disease: is the effect due to beer, wine, or spirits. BMJ. 1996;312:731–6. doi: 10.1136/bmj.312.7033.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RIMM EB, WILLIAMS P, FOSHER K, CRIQUI M, STAMPFER MJ. Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors. BMJ. 1999;319:1523–8. doi: 10.1136/bmj.319.7224.1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ROHATGI A, KHERA A, BERRY JD, GIVENS EG, AYERS CR, WEDIN KE, NEELAND IJ, YUHANNA IS, RADER DR, DE LEMOS JA, SHAUL PW. HDL cholesterol efflux capacity and incident cardiovascular events. N Engl J Med. 2014;371:2383–93. doi: 10.1056/NEJMoa1409065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ROMIEU I, SCOCCIANTI C, CHAJES V, DE BATLLE J, BIESSY C, DOSSUS L, BAGLIETTO L, CLAVEL-CHAPELON F, OVERVAD K, OLSEN A, TJONNELAND A, KAAKS R, LUKANOVA A, BOEING H, TRICHOPOULOU A, LAGIOU P, TRICHOPOULOS D, PALLI D, SIERI S, TUMINO R, VINEIS P, PANICO S, BUENO-DE-MESQUITA HB, GILS CH, PEETERS P, LUND E, SKEIE G, WEIDERPASS E, QUIROS JR, CHIRLAQUE MD, ARDANAZ E, SANCHEZ MJ, DUELL EJ, AMIANO P, BORGQUIST S, WIRFALT E, HALLMANS G, JOHANSSON I, NILSSON LM, KHAW KT, WAREHAM N, KEY TJ, TRAVIS RC, MURPHY N, WARK PA, FERRARI P, RIBOLI E. Alcohol intake and breast cancer in the European Prospective investigation into Cancer and Nutrition: Short title: Alcohol intake and breast cancer: Alcohol intake and breast cancer. Int J Cancer. 2015 doi: 10.1002/ijc.29469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RONKSLEY PE, BRIEN SE, TURNER BJ, MUKAMAL KJ, GHALI WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671. doi: 10.1136/bmj.d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SACKS FM, BRAY GA, CAREY VJ, SMITH SR, RYAN DH, ANTON SD, MCMANUS K, CHAMPAGNE CM, BISHOP LM, LARANJO N, LEBOFF MS, ROOD JC, DE JONGE L, GREENWAY FL, LORIA CM, OBARZANEK E, WILLIAMSON DA. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360:859–73. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SCHRIEKS IC, HEIL AL, HENDRIKS HF, MUKAMAL KJ, BEULENS JW. The Effect of Alcohol Consumption on Insulin Sensitivity and Glycemic Status: A Systematic Review and Meta-analysis of Intervention Studies. Diabetes Care. 2015;38:723–732. doi: 10.2337/dc14-1556. [DOI] [PubMed] [Google Scholar]
- SHAI I, WAINSTEIN J, HARMAN-BOEHM I, RAZ I, FRASER D, RUDICH A, STAMPFER MJ. Glycemic effects of moderate alcohol intake among patients with type 2 diabetes: A Multi-center, randomized clinical intervention trial. Diabetes Care. 2007 doi: 10.2337/dc07-1103. [DOI] [PubMed] [Google Scholar]
- SIERKSMA A, SARKOLA T, ERIKSSON CJ, VAN DER GAAG MS, GROBBEE DE, HENDRIKS HF. Effect of moderate alcohol consumption on plasma dehydroepiandrosterone sulfate, testosterone, and estradiol levels in middle-aged men and postmenopausal women: a diet-controlled intervention study. Alcohol Clin Exp Res. 2004;28:780–5. doi: 10.1097/01.alc.0000125356.70824.81. [DOI] [PubMed] [Google Scholar]
- SIERKSMA A, VAN DER GAAG MS, KLUFT C, HENDRIKS HF. Moderate alcohol consumption reduces plasma C-reactive protein and fibrinogen levels; a randomized, diet-controlled intervention study. Eur J Clin Nutr. 2002;56:1130–6. doi: 10.1038/sj.ejcn.1601459. [DOI] [PubMed] [Google Scholar]
- SMITH-WARNER SA, SPIEGELMAN D, YAUN S-S, ADAMI HO, VAN DEN BRANDT PA, FOLSOM AR, GOLDBOHM RA, GRAHAM S, HOWE GR, MARSHALL JR, MILLER AB, POTTER JD, SPEIZER FE, WILLETT WC, WOLK A, HUNTER DJ. Alcohol and breast cancer in women: a pooled analysis of cohort studies. J Am Med Assoc. 1998;279:535–540. doi: 10.1001/jama.279.7.535. [DOI] [PubMed] [Google Scholar]
- SUBSTANCE ABUSE AND MENTAL HEALTH SERVICES ADMINISTRATION 2014 . In: Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. ADMINISTRATION, S. A. A. M. H. S., editor. Rockville: [Google Scholar]
- TINKER LF, BONDS DE, MARGOLIS KL, MANSON JE, HOWARD BV, LARSON J, PERRI MG, BERESFORD SA, ROBINSON JG, RODRIGUEZ B, SAFFORD MM, WENGER NK, STEVENS VJ, PARKER LM. Low-fat dietary pattern and risk of treated diabetes mellitus in postmenopausal women: the Women's Health Initiative randomized controlled dietary modification trial. Arch Intern Med. 2008;168:1500–11. doi: 10.1001/archinte.168.14.1500. [DOI] [PubMed] [Google Scholar]
- TOLSTRUP JS, WIUM-ANDERSEN MK, ORSTED DD, NORDESTGAARD BG. Alcohol consumption and risk of atrial fibrillation: Observational and genetic estimates of association. European journal of preventive cardiology. 2016 doi: 10.1177/2047487316641804. [DOI] [PubMed] [Google Scholar]
- VAN DER GAAG MS, VAN TOL A, SCHEEK LM, JAMES RW, URGERT R, SCHAAFSMA G, HENDRIKS HF. Daily moderate alcohol consumption increases serum paraoxonase activity; a diet-controlled, randomised intervention study in middle-aged men. Atherosclerosis. 1999;147:405–10. doi: 10.1016/s0021-9150(99)00243-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.