Abstract
Objective
The therapeutic alliance is recognized as an important contributor to treatment outcomes. In this study, the session-to-session interplay of the alliance (as perceived by the patient) and alcohol involvement (drinking days and heavy drinking days between successive treatment sessions) was examined. The analyses also tested the extent to which pretreatment changes in drinking altered these interrelationships.
Method
Participants (N = 63) seeking treatment for an alcohol use disorder received 12-weeks of CBT for alcohol dependence and completed weekly assessments of the alliance.
Results
Higher session alliance scores at a given session significantly predicted lower alcohol involvement (both drinking days and heavy drinking days) in the period until the next treatment session, controlling for previous alcohol involvement. This relationship was further moderated by pretreatment change (changes in drinking prior to the first treatment session). Among those who demonstrated low pretreatment change, alliances continued to predict alcohol involvement. In contrast, alliances were not associated with alcohol involvement among those who significantly reduced their drinking prior to the first treatment session (high pretreatment changers). Finally, alcohol involvement during the period preceding a treatment session did not significantly predict alliance ratings.
Conclusions
These data demonstrate that more positive patient ratings of the alliance at any given treatment session are associated with less alcohol involvement during the period until the next treatment session, most particularly among patients who have not initiated reductions in their drinking prior to the first treatment session. For such patients, efforts to maximize therapeutic alliances may be warranted and productive.
Keywords: therapeutic alliance, alcohol use disorders, drinking behavior, treatment
A consensus is evident in the psychotherapy literature that establishment of a therapeutic alliance between the patient and therapist is an important component of the behavior change process. Perhaps the most important conclusion following from multiple reviews of this literature (Horvath & Greenberg, 1994; Horvath, Del Re, Fluckiger, & Symonds, 2011; Orlinsky, Ronnestad, & Willutzki, 2004; Martin, Garske, & Davis, 2000) is that there is a moderate but consistent positive relationship between patient ratings of the therapeutic alliance and outcome. The Horvath et al. (2011) meta-analysis, for example, included 190 studies (representing more than 14,000 patients) and found a small to moderate relationship between the therapeutic alliance and treatment outcome (r = .28). Furthermore, patients’ ratings of the alliance often have been stronger predictors of treatment outcome than therapists’ ratings (Horvath, 1994; Horvath & Symonds, 1991), although this has not consistently been the case (Martin et al., 2000). Finally, the available research suggests that the relationship of the therapeutic alliance to outcome is evident across therapeutic approaches. Horvath and Symonds (1991), Martin et al. (2000), and Horvath et al. (2011) investigated this question in their reviews and found that the relationship between alliance and outcome replicates across several types of psychotherapy (e.g., psychodynamic, cognitive, eclectic). It is notable that this conclusion has held up after taking into account theoretical and methodological concerns including the influence of psychotherapy theory on the development of alliance measure items, method of alliance questionnaire or inventory development, differences in methods of alliance measurement such as patient or therapist self-reports versus independent observer ratings (Horvath et al., 2011; Lingiardi & Colli, 2015).
Research on the therapeutic alliance in the treatment of alcohol and other substance use disorders does not have the same robust history of such research in the treatment of other psychiatric disorders, such as depression or anxiety disorders. However, the topic has been receiving considerably more attention, and, with few exceptions (Barber et al., 2001), the data align well with those reported in the broader psychotherapy literature. In reviewing the literature on the role of the therapeutic alliance in substance use disorder treatment, Meier, Barrowclough, and Donmall (2005) found that the therapeutic alliance, assessed early in treatment, was a consistent predictor of treatment engagement and retention. The alliance also was found to predict early improvements in treatment, but was less consistent in predicting posttreatment outcomes. Given this conclusion, it is important to ask whether the alliance predicts symptom outcome when taking into account prior symptom changes. In this regard, reviews of the studies that have controlled for symptom change prior to the assessment of alliance (Barber et al., 1999; Crits-Christoph, Gibbons, & Mukherjee, 2013) have shown an average effect of r=.19 between the alliance and subsequent outcome, controlling for prior symptom change (Crits-Christoph et al., 2013). Most of these studies included samples of individuals being treated for depression or anxiety; two included individuals with a substance use disorder (Barber et al., 1999; Crits-Christoph et al., 2009), with effect sizes of r=.24 and r=.21, respectively.
Another important question is the degree to which the therapeutic alliance mediates (is a mechanism of behavior change) and thus plays a causal role in treatment outcomes assessed at a given point in time. This is a central point that Kazdin and Nock (2003) raised in their discussion of methodological questions pertaining to the delineation of mechanisms of behavior change. They noted that study of mechanisms of change in treatment necessitates multiple assessments of the mechanism (therapeutic alliance, in the present context) and symptomatology (alcohol involvement, in the present context). It follows from this argument that research designs that feature multiple assessments are needed to demonstrate that the proposed mechanism (therapeutic alliance) comes before the outcome (change in alcohol involvement), controlling for symptom change prior to the assessment of alliance and even prior to the initiation of the treatment episode in question.
In this context, a rich research opportunity may be afforded through studies in which therapeutic alliances and symptoms are monitored on a session by session basis over the entire course of treatment, as opposed to assessing the alliance at particular pre-determined points (e.g., after session 2) and outcome only after cessation of treatment. This is the approach that Falkenström, Granström, and Holmqvist (2013) took in their evaluation of the alliance and symptomatic improvement, session by session, among patients in primary care psychotherapy. In this study, the most common presenting problems were anxiety, relationship difficulties, and depression. Using multilevel models, the authors systematically evaluated the relationship of the alliance with symptom levels reported at the next treatment session, controlling for symptom change prior to the assessment of the alliance. The results from the session-to-session analyses showed that alliance ratings predicted subsequent symptomatic change, and that symptomatic change predicted alliance. The particularly noteworthy finding from this study was the session-to-session prediction of symptom change by the therapeutic alliance, even when controlling for symptom change preceding the session.
An additional consideration that arises in the context of addictions treatment is the extent to which changes in drinking behavior have already been initiated prior to the beginning of the formal course of treatment (e.g., changes occurring between the decision to contact a treatment program for services and the actual start of treatment). Multiple studies have demonstrated significant reductions in alcohol consumption among some individuals prior to the onset of a course of treatment (e.g., Epstein et al., 2005; Kaminer, Burleson, & Burke, 2008; Morgenstern et al., 2007; Penberthy et al., 2007; Stasiewicz et al., 2013). In one of these reports, Stasiewicz et al. (2013) identified a pair of pretreatment change patterns, one reflecting a rapid positive change in drinking (increases in abstinent days and decreases in drinks per drinking day) prior to the first treatment session and the second reflecting minimal change in drinking prior to the first treatment session. An important consideration of these findings in the present context is that the role and evaluation of the therapeutic alliance in the behavior change process could plausibly vary as a function of the extent to which an individual has already made significant changes in drinking behavior before the first treatment session. For example, the contribution of the therapeutic alliance to the change process during treatment may be less central in cases where the patient has already initiated behavior change.
Taken together, research on the therapeutic alliance in alcohol treatment has been informative but predominantly on a global and descriptive level. The present study advances research in this area in three ways. First, past research has been limited most significantly by not assessing the therapeutic alliance continuously over the course of treatment. In response, the session-to-session interplay of the patient’s perception of the therapeutic alliance and alcohol involvement between successive treatment sessions was evaluated in this study during a 12-session course of treatment for an alcohol use disorder. It was hypothesized that the therapeutic alliance assessed immediately after any given treatment session predicts alcohol involvement during the period until the next treatment session, independent of alcohol consumption leading up to the session. Second, additional analyses were performed to investigate the similarly important relationship of alcohol involvement prior to a given treatment session to the patient’s rating of the therapeutic alliance for that session, independent of the prior session’s rating of the alliance. Finally, the analyses tested the extent to which pretreatment changes in drinking altered these interrelationships.
Method
Participants
Participants were 63 individuals (female n=20) seeking outpatient alcohol use disorder treatment who were recruited from the community through local newspaper and radio advertisements. Inclusion criteria were (a) being between 18 and 65 years of age, (b) meeting DSM-IV (American Psychiatric Association, 1994) criteria for a diagnosis of current alcohol dependence (assessed using the electronic version of the Mini International Neuropsychiatric Interview {MINI}, Sheehan et al., 1997, 1998), and (c) living within commuting distance of the program site. Exclusion criteria were (a) meeting criteria for a current organic mental disorder, schizophrenia, delusional (paranoid) disorder, or any of the other psychotic disorders, (b) presenting with gross neurocognitive impairment, as evidenced by a poor performance on a structured mental status examination (MMSE; Folstein, Folstein, & McHugh, 1975), or (c) having been in substance abuse treatment during the previous 12 months (except for self-help groups). The participant recruitment flow chart is displayed in Figure 1. It reflects 66 participants having a valid first treatment session. The present analyses include 63 participants, reflecting the loss of three individuals for whom data were not available to calculate pretreatment change. Participants included in the analyses attended an average of 9.43 (SD= 3.51, R= 1–12) treatment sessions.
Figure 1.
Participant recruitment flow chart.
Participants were predominantly Caucasian (74.6%; 20.6% African American, 3.2% American Indian/Alaska Native, and 1.6% Hispanic American) and had a mean age of 48.27 (SD=10.64) years. Approximately 53% reported part-time or full-time employment (21.7% unemployed; 10% disabled; 14.3% retired). Thirty-five percent reported being married, and 36.7% reported receiving previous outpatient treatment for alcohol problems (but not in the past 12 months). During the 6-month period prior to the baseline assessment, participants reported in the Timeline Follow-back interview (Sobell & Sobell, 1992) 31.7% (SD=28.7) days abstinent and 59.0% (SD = 29.7) heavy drinking days (defined as 5 or more standard drinks for men and 4 or more standard drinks for women) (NIAAA, 2004; Wechsler & Nelson, 2001).
Measures
Demographic
characteristics, current status information (e.g., marital status, employment), and substance abuse treatment history were obtained using a comprehensive background questionnaire administered during the baseline assessment.
Mini International Neuropsychiatric Interview (MINI; Sheehan et al., 1997, 1998)
The electronic version of the MINI was used to confirm meeting DSM-IV diagnostic criteria for current alcohol dependence.
Timeline Follow-back (TLFB; Sobell & Sobell, 1992)
The TLFB is a calendar-based retrospective recall interview of daily alcohol use. The TLFB was used to assess number of drinking days and number of heavy drinking days over the 6-month period prior to the baseline assessment and throughout the 12-week treatment period. The reliability and accuracy of the TLFB measure have been consistently demonstrated in this population for both alcohol and other substance use (e.g., Ehrman & Robins, 1994; Sobell & Sobell, 1992, 1996).
Working Alliance Inventory (Horvath & Greenberg, 1986; Tracey & Kokotovic, 1989)
The WAI, developed to assess the therapeutic alliance, consists of subscales that address patient/therapist agreement on the goals of therapy (Goals), patient/therapist agreement about the tasks of therapy (Tasks), and the bond between the patient and therapist (Bond). Ratings are made on a 7-point Likert-type scale ranging from 1 (“never”) to 7 (“always”) on the extent to which the respondent agrees with the statement. In the present study, the 12-item short version of the patient WAI was used (WAI-S). Developed by Tracey and Kokotovic (1989), the WAI-S is comparable to the longer, 36-item WAI (Busseri & Tyler, 2003) and has satisfactory reliability and validity (Tracey & Kokotovic, 1989). Because the Tasks, Bond, and Goals subscales are highly correlated, the WAI total score was used in all analyses.
Procedure
Participants were recruited through radio and newspaper advertisements. Individuals calling the project phone number were screened for initial inclusion and provided a description of the treatment program. If the initial eligibility criteria were met, participants were scheduled for a baseline/intake interview (~ 90 minutes). During the baseline appointment, informed consent was obtained and measures administered. Clients were informed that the purpose of the project was “to study the treatment process and the outcomes associated with treatment participation,” and that they would be asked to complete several brief measures after each treatment session. Clients also were informed that their participation in the project was voluntary, that their responses to the questions on the measures had no bearing on their access to treatment, and that they had the right to refuse to answer any particular questions during the interview or on the questionnaires. The research was approved by the University at Buffalo Social and Behavioral Sciences Institutional Review Board.
All participants received 12-weeks of standard Cognitive Behavioral Therapy (CBT; Kadden et al., 1992) for alcohol dependence (the first session was 90 minutes and the successive sessions were 60 minutes each) through the research site’s outpatient clinical research center. Seven sessions were designated as core sessions, which included Introduction to Coping Skills Training, Coping with Cravings and Urges to Drink, Managing Thoughts About Alcohol and Drinking, Problem Solving, Drink Refusal Skills, Planning for Emergencies and Coping with a Lapse, and Seemingly Irrelevant Decisions. The therapist and patient collaborated in the identification of additional sessions as judged best to meet the patient’s clinical needs (e.g., Starting Conversations, Assertiveness, Anger Management, Managing Negative Thinking, and Enhancing Social Support Networks). The final (twelfth) session focused on reviewing treatment gains and termination.
All treatment sessions were administered within an outpatient clinical research clinic by therapists with a minimum of 5 years experience in treating patients with alcohol use disorders. Prior to study recruitment, the therapists underwent training related to the CBT intervention as presented in the Project MATCH training manual (Kadden et al., 2003). During this training period, the therapists met as a group with the clinical supervisor for four hours per week (in 1–2 hour blocks) over 9 weeks. Group training sessions included detailed discussion of theory and procedures related to CBT, instruction on session by session content, role play, and discussion of applying the CBT approach to specific patient problems. All of the training was guided by the training manual, with occasional complementary readings. Therapists were also expected to complete readings and activities (e.g., paired role play) outside of the weekly meetings. Therapists throughout were blind to the study hypotheses.
Once recruitment began and therapists began seeing patients, therapists received weekly supervision (60 to 90 minutes in duration) for the duration of the study. During the initial months of seeing patients, supervision focused on honing the therapist’s CBT skills as applied to specific patient presenting problems. All patient sessions were audiotaped, and the clinical supervisor reviewed a subset of recorded sessions as one means of providing feedback to therapists. Therapists were instructed to alert the supervisor to particularly challenging sessions (for critique); the supervisor also picked random sessions for review. During the early months of the study, most supervisory feedback pertained to delivery of the CBT content with fidelity to the treatment manual. As therapists’ skill level increased, supervision became more focused on nuances of patients’ presenting problems (but still with a focus on consistent delivery of CBT). Therapists were provided with one-page session summary sheets for each of the session topics. Therapists were instructed to review these summary sheets as a refresher of session content before each patient session. Therapists also completed a checklist following each session; the checklist included an item assessing the extent to which the guidelines/outline for that session’s topic were followed. Therapists provided their ratings on a 3-point scale (1=not at all, 2=somewhat, 3=extensively). Across therapists and sessions, the mean rating was 2.52 (SD=0.51); 52.2% of the sessions were rated 3 (extensively), 47.1% were rated 2 (somewhat), and only 0.7% were rated 1 (not at all). These data provide a strong positive indication on treatment fidelity, at least from the perspective provided through these therapist reports.
At the end of each treatment session, participants provided ratings of the therapeutic alliance using the WAI-S, based on their perceptions of that day’s session, and information on alcohol use since the previous treatment session. To encourage and facilitate accurate reporting, clients were assured that the information they provided to the research staff on their perceptions of the therapeutic alliance and any alcohol consumption (indeed, any information provided more broadly) would not be shared with their therapists. This assurance was described in the informed consent document and verbally by the research staff.
Procedures utilized to address treatment dropouts and missed or cancelled appointments included calls and letters to reschedule. If a participant had 4 consecutive weeks of non-contact with the clinic (i.e., missed more than four consecutive weeks of treatment), then his/her chart was placed in an inactive status. (Research staff continued their outreach to participants for the scheduled research follow-up appointments, regardless of their treatment completion status.)
Data Analytic Strategy
First, to explore and provide a description of change during the course of treatment, independent growth curve models (Hierarchical Linear Modeling; HLM 7.0; Raudenbush et al., 2011) were examined for each of the main drinking outcomes (number of drinking days and number of heavy drinking days) and therapeutic alliance. As noted earlier, heavy drinking days were defined as 4 or more drinks per occasion for females, and 5 or more for males. For each outcome, the intercept, linear, quadratic, and cubic effects (all growth parameters were centered at Session 1) were modeled controlling for age, gender, and race (i.e., on intercept only). Non-significant higher-order growth parameters were then trimmed from models to increase model stability and to appropriately interpret lower order terms and deviance statistics were inspected for model fit using Laplace estimation1 (Raudenbush et al., 2011; Raudenbush & Bryk, 2002). Data examined were collected over the 12 weekly treatment sessions (i.e., 12 time points). Drinking data from were summed (i.e., number of drinking days, number of heavy drinking days) based on the number of days between treatment sessions, and therefore intervals varied from person to person. All models with drinking as the outcome were analyzed as an overdispersed Poisson model with variable exposure (i.e., number of days within each treatment interval), providing estimates of drinking rates per day. Parameters in the Poisson models were estimated using restricted penalized quasi-likelihood estimation (restricted PQL) with robust standard errors due to the nature of the data (i.e., counts). PQL provides maximum likelihood estimates for generalized linear mixed models, and has been found to perform favorably for Poisson models when compared to other methods (see Raudenbush et al., 2011). Further, the addition of an overdispersion parameter adds “an error term that increases the variance compared to the variance implied by the normal Poisson model” (Hox, 2010, p. 155), thereby correcting for violations of the assumption implied by Poisson models that the variance of the outcome is equal to the mean. In contrast, the growth curve for therapeutic alliance was modeled as continuous with all parameters estimated using restricted maximum likelihood estimation (REML). REML and other restricted estimation procedures were chosen over FML (full maximum likelihood) because they provide less biased variance estimates, particularly with smaller sample sizes (e.g., Hox, 2010).
Next, to explore the effect of pretreatment change on change for each of the outcomes, percent change in drinking (pretreatment change) was entered as a cross level moderator (i.e., between subjects variable) on the intercept and growth parameters. Percent change in drinking was calculated using an average history of drinking four weeks prior to initiating treatment (rates of drinking for weeks 5 through 17 prior to treatment, 12 weeks in total) and rate of drinking during the 1-week period prior to treatment session 1. Specifically, average history of weekly drinking (i.e., 7 days) was subtracted from drinking the week prior to treatment session 1 (i.e., 7 days) and then divided by history of drinking. Change during the four weeks prior to entering treatment was chosen because previous research has suggested that changes in drinking may occur approximately one month prior to treatment (see Staseiwciz et al., 2013). Therefore, negative values represented decreases in pretreatment drinking and positive numbers represented increases (−1.0 = 100% decrease in drinking and abstinence at the start of treatment).
To examine our main hypothesis, multilevel time-lagged regression models (measures within persons) were estimated using Hierarchical Linear Modeling (HLM 7.0; Raudenbush et al., 2011). Due to our interest in examining behavioral treatment process variables, reports of drinking outcomes were predicted from the report of client-rated therapeutic alliance from the previous time point, controlling for reports of drinking (i.e., drinking reports from the prior time point entered as a level-1 predictor). Consistent with recommendations by Enders and Tofighi (2007), prior reports of therapeutic alliance were entered into the models centered on the person’s own mean to examine how changes around the person’s own mean predicted drinking outcomes. Further, all level-1 predictors were entered as random effects and modeled as an overdispersed Poisson with variable exposure (restricted PQL estimation). Second, to examine the relationship of pretreatment change on therapeutic alliance predicting changes in drinking, all models were examined with pretreatment change as a level-2 moderator (grand mean centered) on all effects and the intercept. For all analyses, missing data on level 1 were handled using restricted maximum likelihood estimation, as maximum likelihood estimations have been shown to perform well under conditions of missing completely at random and missing at random (see Schafer & Graham, 2002, for a review).
All follow-up simple slope analyses were conducted using values at the 15th and 85th percentiles on the variable of interest (e.g., pretreatment change, therapeutic alliance). These percentiles for low and high values when probing interactions were selected for two reasons. First, they are roughly equivalent to +/− one standard deviation (i.e., +/− 1 SD equals 68.2% of the distribution, 15th percentile minus 85th percentile equals 70% of the distribution). Second, and perhaps more importantly, we wanted to ensure that the values chosen fell within the distribution of possible scores.
Results
Unconditional Models and Intra-Class Correlations
Prior to running the descriptive growth curve analyses and analyses for the primary aims, intra-class correlations (ICCs) were calculated for the unconditional models for each outcome to examine the proportion of variance accounted for due to clustering (i.e., correlation among observations within person). The ICCs for the unconditional models for number of drinking days, number of heavy drinking days, and working alliance were .667, .713, and .751, respectively. This suggests that 67–75% of the variance in outcome measures are accounted for by the grouping structure of the data (measures within person), confirming the need to analyze the data accounting for nesting.
Examination of Change in Drinking and Therapeutic Alliance
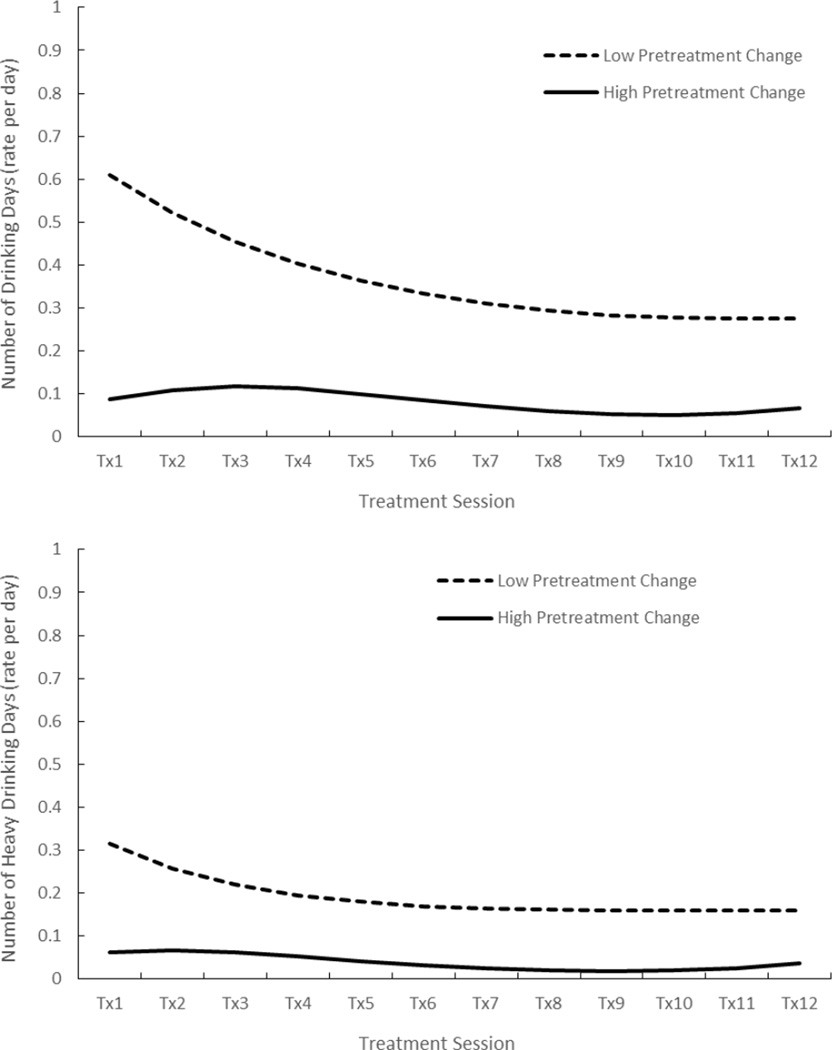
To examine changes in drinking and therapeutic alliance over the course of treatment, growth curve analyses were conducted for each outcome (see top of Table 1 for summary). In general, significant changes in the expected directions were observed for all drinking outcomes and therapeutic alliance. Specifically, decreases in number of drinking days and number of heavy drinking days were observed during the course of treatment, whereas significant increases in therapeutic alliance were observed. However, as expected, changes in drinking varied based on level of pretreatment change (see bottom of Table 1 and Figure 2 for summary). Specifically, pretreatment change was associated with drinking at the beginning of treatment, such that individuals demonstrating greater pretreatment change had significantly fewer drinking days (b = .995, SE = .134 p < .001) and heavy drinking days (b = 1.258, SE = .145 p < .001) than individuals with lower pretreatment change. Further, pretreatment change moderated changes in drinking during the course of treatment, such that greater drinking prior to treatment session 1 (i.e., low pretreatment change) was associated with greater decreases in drinking during the course of treatment (i.e., significant linear × pretreatment change interactions when time was centered on treatment session 1). Follow-up analyses revealed that among those low on pretreatment change, significant decreases were observed at the start of treatment for number of drinking days (b = −.167, SE = .066, p = .011) and heaving drinking days (b = −.229, SE = .096, p = .018). In contrast, those high on pretreatment change demonstrated significant increases in number of drinking days at the beginning of treatment (i.e., Time effect; b = .289, SE = .130, p = .027) that quickly slowed and was followed by a subsequent decrease in drinking (i.e., Time2 effect; b = −.085, SE = .029, p = .004), with a similar pattern observed for number of heavy drinking days. Although significant growth parameters (e.g., Time, Time2, and Time3) were noted for those high on pretreatment change, inspection of the graph and estimated means suggests minor changes overall from week to week in drinking. In fact, those who demonstrated significant changes during the pretreatment intervals made little additional positive gains in drinking outcomes during the course of treatment beyond the significant changes seen during pretreatment (i.e., prior to the first treatment session). Further, pretreatment change was significantly associated with drinking at the end of treatment (i.e., time re-centered at session 12), such that those with greater levels of pretreatment change (i.e., negative values) demonstrated lower number of drinking days (b = .681, SE = .172 p < .001) and heavy drinking days (b = .902, SE = .206 p < .001).
Table 1.
Summary of Growth Curve Analyses
| Intercept | Linear (Time) | Quadratic (Time2) | Cubic (Time3) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | p | β | SE | p | β | SE | p | β | SE | p | |
| Growth Curve | ||||||||||||
| 1. Drinking Days1 | −1.103 | .123 | <.001 | −.082 | .014 | <.001 | ns | Ns | ns | ns | ns | ns |
| × Age | .002 | .013 | .896 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| × Race | −.103 | .225 | .649 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| × Gender | −.077 | .445 | .863 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| 2. Heavy Drink Days2 | −1.647 | .148 | <.001 | −.179 | .040 | <.001 | .011 | .004 | .004 | ns | ns | ns |
| × Age | −.013 | .013 | .330 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| × Race | −.168 | .300 | .577 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| × Gender | −.349 | .474 | .466 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| 3. WAI | 5.526 | .106 | <.001 | .239 | .049 | <.001 | −.033 | .010 | <.001 | .002 | .0006 | .007 |
| × Age | −.0005 | .008 | .945 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| × Race | −.271 | .172 | .119 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| × Gender | .314 | .192 | .107 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Growth × Pretreatment Change | ||||||||||||
| 1. Drinking Days | −1.323 | .141 | <.001 | .029 | .092 | .754 | −.031 | .021 | .135 | .002 | .001 | .096 |
| × PreTx | 1.369 | .145 | <.001 | −.323 | .050 | <.001 | .067 | .011 | <.001 | −.004 | .001 | <.001 |
| × Age | .001 | .011 | .924 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| × Gender | −.120 | .250 | .634 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| × Race | .160 | .447 | .721 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| 2. Heavy Drink Days | −1.971 | .167 | <.001 | −.028 | .125 | .821 | −.034 | .029 | .250 | .003 | .002 | .107 |
| × PreTx | 1.304 | .165 | <.001 | −.320 | .089 | <.001 | .095 | .018 | <.001 | −.006 | .001 | <.001 |
| × Age | −.024 | .009 | .011 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| × Gender | −.123 | .303 | .687 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| × Race | −.288 | .375 | .445 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| 3. WAI | 5.526 | .105 | <.001 | .239 | .049 | <.001 | −.033 | .010 | <.001 | .002 | .0006 | .004 |
| × PreTx3 | −.111 | .134 | .408 | −.024 | .074 | .745 | .011 | .015 | .461 | −.0007 | .0009 | .455 |
| × Age | −.0006 | .008 | .944 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| × Gender | −.285 | .169 | .098 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| × Race | .307 | .191 | .113 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
Note: PreTx = pretreatment change; percent change in drinking (number of drinking days) prior to first treatment session; Gender = 0 Female, 1 Male; Race = 0 Caucasian, 1 Minority. β = unstandardized estimate; SE = standard error; ns = non-significant term trimmed from final model. Growth parameters were modeled as fixed and centered at session 1.
Model comparison test (Deviance statistic based on Laplace estimation) for final model versus full model confirmed that the addition of quadratic and cubic effects did not improve model fit; χ2(2) = 1.993, p >.500.
Model comparison test (Deviance statistic based on Laplace estimation) for final model versus full model confirmed that the addition of the cubic effect did not improve model fit, supporting the trimmed (final) model; χ2(2) = 1.993, p >.500.; χ2(1) = 0.075, p >.500.
Percent change in number of drinking days was entered as the pretreatment change variable.
Figure 2.
Growth curve for number of drinking days (top panel) and heavy drinking days (bottom panel) by low (15th percentile) and high (85th percentile) pretreatment change.
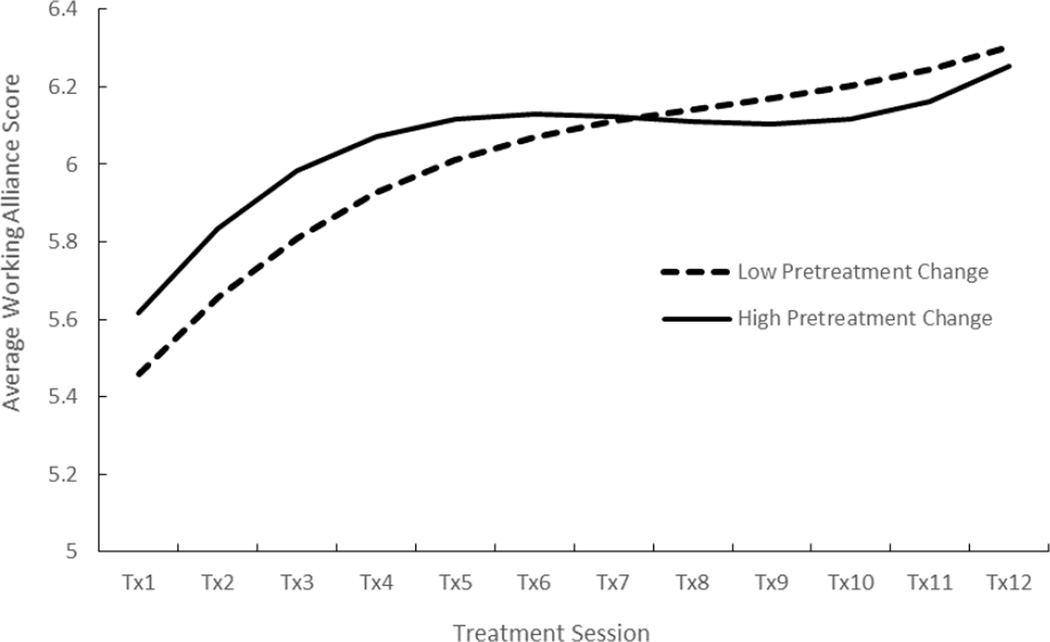
In contrast, changes in therapeutic alliance were not moderated by pretreatment change. Specifically, pretreatment changes were not associated with therapeutic alliance at the beginning of treatment (b = −.111, SE = .134, p = .408) or at end of treatment (b = .042, SE = .157, p = .791). Rather, therapeutic alliance significantly increased over the course of treatment for all participants regardless of pretreatment change status (see Figure 3).
Figure 3.
Growth curve for therapeutic alliance by pretreatment change.
Prior Therapeutic Alliance Predicting Drinking Outcomes
To examine the effect of prior session therapeutic alliance ratings on current drinking outcomes, each drinking outcome was predicted from prior reports of therapeutic alliance, controlling for age, gender, race, and drinking in the week prior to the index session (see Table 2 for summary of results). Results indicated that prior therapeutic alliance significantly predicted changes in number of drinking days (b = −.367, SE = .093 p < .001) and heavy drinking days (b = −.506, SE = .147 p < .001), such that higher therapeutic alliance scores (relative to the person’s own mean) predicted lower drinking in the following week.
Table 2.
Summary of Results for Prior Therapeutic Alliance Predicting Drinking Outcomes
| # Drinking Days | # Heavy Drinking Days | |||||
|---|---|---|---|---|---|---|
| β | SE | P | β | SE | p | |
| Prior WAI | ||||||
| Intercept | −1.371 | .141 | <.001 | −2.128 | .166 | <.001 |
| × Age | .001 | .014 | .976 | −.010 | .014 | .477 |
| × Gender | −.091 | .293 | .759 | −.076 | .342 | .824 |
| × Race | .171 | .523 | .744 | −.228 | .585 | .698 |
| Prior Drinking | .046 | .016 | .005 | .087 | .054 | .116 |
| Prior Therapeutic Alliance | −.367 | .093 | <.001 | −.506 | .147 | .001 |
| Prior WAI × Pretreatment Change | ||||||
| Intercept | −1.534 | .140 | <.001 | −2.380 | .138 | <.001 |
| × PreTx Change | 1.001 | .167 | <.001 | 1.071 | .164 | <.001 |
| × Age | .004 | .012 | .741 | −.011 | .010 | .286 |
| × Gender | −.014 | .291 | .963 | −.184 | .324 | .572 |
| × Race | .158 | .487 | .747 | −.227 | .592 | .661 |
| Prior Drinking | .074 | .025 | .005 | .109 | .073 | .139 |
| × PreTx Change | −.097 | .028 | <.001 | .014 | .060 | .816 |
| Prior Therapeutic Alliance | −.205 | .131 | .125 | −.306 | .169 | .076 |
| × PreTx Change | −.424 | .149 | .006 | −.418 | .185 | .028 |
Note: PreTx Change = percent change in drinking (number of drinking days) prior to first treatment session; Gender = 0 Female, 1 Male; Race = 0 Caucasian, 1 Minority. β = unstandardized estimate; SE = standard error. All effects were modeled as random.
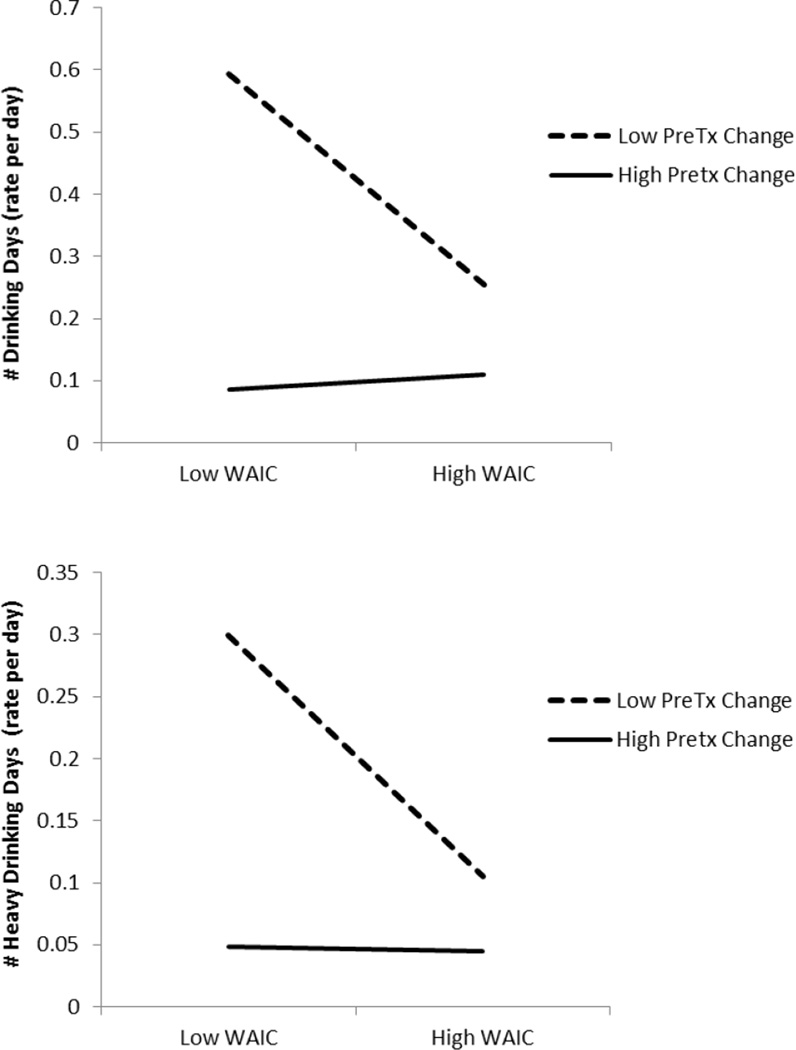
Further examination of therapeutic alliance predicting number of drinking days and heavy drinking days in the subsequent week revealed that pretreatment change significantly moderated such effects (see bottom of Table 2 and Figure 4). Specifically, among those with low levels of pretreatment change, the analyses revealed significant simple slopes for the therapeutic alliance predicting number of drinking days (b = −.462, SE = .101 p < .001) and number of heavy drinking days (b = −.569, SE = .165 p = .001). In contrast, among those with high levels of pretreatment change, simple slopes for the therapeutic alliance were non-significant for both number of drinking days (b = .136, SE = .228, p = .551) and number of heavy drinking days (b = −.041, SE = .240, p = .865).
Figure 4.
Therapeutic Alliance × PreTx Change predicting total number for drinking days (top panel) and total number of heavy drinking days (bottom panel). Therapeutic alliance and pretreatment change are graphed at the 15th (low) and 85th (high) percentiles.
Prior Drinking Predicting Therapeutic Alliance
To examine the effect of prior drinking (i.e., prior to index treatment session) on current therapeutic alliance, therapeutic alliance was predicted from prior reports of number of drinking days and number of heavy drinking days in the week prior to the treatment session, controlling for age, gender, race, and previous week’s therapeutic alliance rating (see Table 3 for summary of results). Results indicated that neither number of drinking days nor number of heavy drinking days in the week before a treatment session predicted changes in therapeutic alliance. Furthermore, examination of number of drinking days and heavy drinking days (in the week before a treatment session) predicting therapeutic alliance revealed that pretreatment change did not significantly moderate such effects.
Table 3.
Summary of Results for Prior Drinking Predicting Therapeutic Alliance.
| β | SE | P | |
|---|---|---|---|
| 1. Prior Drinking Days | |||
| Intercept | 6.11 | .048 | <.001 |
| × Age | .003 | .004 | .372 |
| × Gender | −.231 | .090 | .013 |
| × Race | .178 | .090 | .013 |
| Prior Drinking | −.001 | .005 | .797 |
| Prior Therapeutic Alliance | .452 | .057 | <.001 |
| 2. Prior Heavy Drinking Days | |||
| Intercept | 6.11 | .046 | <.001 |
| × Age | .004 | .004 | .334 |
| × Gender | −.230 | .090 | .014 |
| × Race | .181 | .103 | .084 |
| Prior Drinking | −.009 | .007 | .230 |
| Prior Therapeutic Alliance | .453 | .056 | <.001 |
| 3. Prior Drink Days × Pretreatment Change | |||
| Intercept | 6.11 | .048 | <.001 |
| × PreTx Change | .002 | .071 | .982 |
| × Age | .003 | .004 | .371 |
| × Gender | −.232 | .092 | .015 |
| × Race | .178 | .103 | .090 |
| Prior Drinking | .0004 | .005 | .932 |
| × PreTx Change | −.011 | .011 | .344 |
| Prior Therapeutic Alliance | .448 | .057 | <.001 |
| × PreTx Change | .004 | .072 | .957 |
| 4. Prior Drink Days × Pretreatment Change | |||
| Intercept | 6.11 | .047 | <.001 |
| × PreTx Change | −.018 | .084 | .830 |
| × Age | .004 | .004 | .309 |
| × Gender | −.234 | .090 | .012 |
| × Race | .184 | .101 | .073 |
| Prior Drinking | −.012 | .009 | .168 |
| × PrTtx Change | .010 | .021 | .653 |
| Prior Therapeutic Alliance | .448 | .056 | <.001 |
| × PreTx Change | −.057 | .071 | .431 |
Note: PreTx Change = percent change in drinking (number of drinking days) prior to first treatment session; Gender = 0 Female, 1 Male; Race = 0 Caucasian, 1 Minority. β = unstandardized estimate; SE = standard error. All effects were modeled as random.
Discussion
Consistent with our primary hypothesis, patient ratings of the therapeutic alliance at a given treatment session predicted alcohol involvement during the period until the next treatment session. Specifically, higher therapeutic alliance scores predicted fewer drinking days and fewer heavy drinking days in the period until the next treatment session. However, consideration of pretreatment change moderated this finding, with the pattern being significant for patients with lower levels of pretreatment change and not for those with higher levels of pretreatment change.
This pattern of results for the therapeutic alliance predicting subsequent symptomatology, controlling for prior symptom change, is consistent with past research (Barber et al., 1999; Crits-Christoph et al., 2013), including studies assessing patients with substance use disorders (Barber et al., 1999; Crits-Christoph et al., 2009). These data extend previous pursuits in two important ways. First, the present data extend almost all past studies by assessing the therapeutic alliance and symptomatology at every treatment session, not just predetermined points in the course of treatment (e.g., after just the second treatment session). Falkenström et al. (2013) was an exception in its evaluation of therapeutic alliance and symptomatology at all treatment sessions in their evaluation of psychotherapy for concerns such as anxiety, relationship problems, and depression, and the present data extend this approach in the context of alcohol use disorders. Second, this study showed that pretreatment changes in symptomatology have implications for the study of therapeutic alliance, and perhaps treatment process more broadly. In the context of treatment of alcohol use disorders, the relationship between the therapeutic alliance and drinking session by session over the course of treatment was evident primarily for those exhibiting less pretreatment change in drinking. As such, the therapeutic alliance may be particularly salient to the behavior change process in cases where the patient has not already initiated or experienced changes in symptomatology prior to the first treatment session. However, it is possible that there is a restricted range in within-treatment drinking among individuals who have already reduced their drinking, which may have attenuated an association with alliance.
In this study, prior drinking (that is, drinking during the period since the previous treatment session) did not predict the following session’s rating of the therapeutic alliance. This highlights further the relation between the therapeutic alliance with subsequent alcohol consumption, independent of drinking prior to that session. This pattern of results, throughout a treatment episode, is relevant to the ongoing discussion on the extent to which changes in symptomatology are predicted by the therapeutic alliance or are instead, at least in part, related to earlier changes in symptomatology (Zilcha-Mano et al., 2014). Falkenström et al. (2013), for example, found support for a reciprocal model, with the therapeutic alliance predicting symptomatic change and prior symptom change predicting the therapeutic alliance. In the present study, we found support only for the former. Similarly, Zilcha-Mano et al. (2014) found that symptomatology did not predict subsequent ratings of the therapeutic alliance.
We noted earlier that one strength of this study is its session by session measurement of the therapeutic alliance and that this design feature characterizes few studies in the alcohol treatment literature. However, in arguing the advantages of repeated measurement of the therapeutic alliance, Falkenstrom, Hatcher, Skjulsvik, Larsson, and Holmqvist (2015) also identified a concern about variance of factor structure of a measure of the therapeutic alliance over the course of repeated measurements. In this regard, if factor structure changes, then a positive bias (inflated alpha level) tends to be introduced in the data. Falkenstrom et al. developed a version of the WAI that is designed for session by session measurement of the therapeutic alliance and that showed invariant factor structure over repeated measurements in the context of psychotherapy administered in the primary care setting. The measure, called the Session Alliance Inventory, would be indicated for use in any replication of this and other studies of the therapeutic alliance that feature session by session measurement over multiple treatment sessions.
There are limitations to this research that should be recognized. First, only one treatment approach, cognitive behavioral, was used. However, past research has generally shown that findings related to the therapeutic alliance are consistent across different therapeutic modalities (Horvath & Symonds, 1991; Horvath et al., 2011; Martin et al., 2000). Further, delivery of the treatment was manual-guided, and the treatment itself was time-limited. It also should be noted that the participants in the present study had not received treatment for an alcohol use disorder during the past year, and the extent to which these findings would generalize to persons returning to treatment (e.g., following a relapse) are not known. Another point is that the therapeutic alliance was assessed using the Working Alliance Inventory, and the use of other measures of the therapeutic alliance in a similar context awaits further research. Related to our use of the WAI, our data showed a general increase in the alliance across sessions, along with a tendency to use only the upper end of the scale of making ratings of the alliance. Both of these findings may reflect the common methodological concern in the field in the use of self-report alliance measures, which is that for several reasons patients tend to report that the alliance is improving over time even though their tendency is to rate the alliance as “good” from the first measurement. Therefore, the validity and application of our findings should be interpreted with these methodological limitations in mind.
A final limitation is that, in this study, the source of measurement of the therapeutic alliance and outcome (alcohol consumption) was the same (patient self-reports). Horvath et al. (2011) identified the “same source” factor as a possible moderator of the therapeutic alliance effect sizes observed in the empirical literature and found no statistical difference. However, Horvath et al. also observed significant heterogeneity among the relevant studies in the same source effect, as more recent studies tended to show a larger discrepancy. Furthermore, there was a trend toward larger effect size when data sources were the same. Although this bias would not seem to explain the pattern of findings observed in this study, it is important to be aware that same source may have affected the validity of our findings to some degree.
This study’s data have potential clinical implications. An overriding message, consistent with considerable past research, is that the therapeutic alliance is directly relevant to a patient’s clinical course in the treatment of an alcohol use disorder. Indeed, these data show that the therapeutic alliance at any given session predicts drinking behavior during the period until the next treatment session, with higher alliances predicting fewer drinking days. Further, this effect seems particularly relevant among patients who had relatively lower levels of pretreatment change in their drinking. Thus, treatment pursuits might be enhanced through systematic assessment and consideration of patient levels of behavior change activity prior to the first treatment session as well as through ongoing assessment of the therapeutic alliance over the course of treatment.
Future research is needed to replicate and extend these findings and to explore their clinical implications. It will be of interest, for example, to determine whether providing feedback to therapists on patient ratings of the therapeutic alliance after each treatment session, with or without clinical supervision focused on such ratings, enhances subsequent ratings of the therapeutic alliance and, of course, symptomatology during the period until the next treatment session. It also may be fruitful to investigate the session-to-session interplay of other process variables, such as perceived therapist empathy, that also may uniquely predict symptomatology during the period until the next treatment session. Finally, this study’s findings suggest that assessment of pretreatment change, initiated by the patient prior to the initial treatment session, may warrant consideration in both clinical and research pursuits.
Public Health Significance.
The annual societal and personal consequences associated with alcohol misuse are profound. This study shows that more positive patient ratings of the therapeutic alliance in treatment are associated with less alcohol involvement between treatment sessions, most particularly among patients who have not already initiated reductions in their drinking prior to the first treatment session. Efforts to maximize therapeutic alliances in such cases may warrant attention in the treatment of alcohol use disorders.
Acknowledgments
This study was funded by National Institute on Alcohol Abuse and Alcoholism Grant R21-AA017112. The development of this report was supported in part by NIAAA Grants K23-AA021768 (Robert C. Schlauch) and T32-AA07583 (Mark A. Prince). We gratefully acknowledge the contributions of Darlene Cutonilli, Molly Rath, Eugenia Riollano, and Jennifer Smith.
Footnotes
Because PQL is based on a quasi-likelihood procedure, deviance testing using log-likelihood functions is not recommended, even though the estimates are usually considered adequate. Therefore, to conduct deviance testing after trimming non-significant higher order growth parameters (i.e., cubic and/or quadratic effects), deviance statistics were estimated using Laplace approximation, which is an alternative method of estimation for the deviance statistic for comparing nested models (see Raudenbush et al., 2011; Scientific Software International, Inc., 2005–2016, for details).
Contributor Information
Gerard J. Connors, Research Institute on Addictions, University at Buffalo, 1021 Main Street, Buffalo, NY 14203
Stephen A. Maisto, Department of Psychology, Syracuse University, 430 Huntington Hall, Syracuse, NY 13244
Robert C. Schlauch, Department of Psychology, University of South Florida, 4202 East Fowler Avenue, Tampa, FL 33620
Ronda L. Dearing, Graduate College of Social Work, University of Houston, 3511 Cullen Boulevard, Houston, TX 77204
Mark A. Prince, Department of Psychology, 1876 Campus Delivery, Colorado State University, Fort Collins, CO 80523
Mark R. Duerr, Research Institute on Addictions, University at Buffalo, 1021 Main Street, Buffalo, NY 14203
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- Barber JL, Crits-Christoph P, Thase ME, Weiss R, Frank A, Onken L, Gallop R. Therapeutic alliance as a predictor of outcome in treatment of cocaine dependence. Psychotherapy Research. 1999;9:54–73. [Google Scholar]
- Barber JP, Luborsky L, Gallop R, Crits-Christoph P, Frank A, Weiss RD, Thase ME, Connolly MB, Gladis M, Foltz C, Siqueland L. Therapeutic alliance as a predictor of outcome and retention in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Journal of Consulting and Clinical Psychology. 2001;69:119–124. doi: 10.1037//0022-006x.69.1.119. [DOI] [PubMed] [Google Scholar]
- Busseri MA, Tyler JD. Interchangeability of the Working Alliance Inventory and Working Alliance Inventory, Short Form. Psychological Assessment. 2003;15:193–197. doi: 10.1037/1040-3590.15.2.193. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Gallop R, Temes CM, Woody G, Ball SA, Martino S, Carroll KM. The alliance in motivational enhancement therapy and counseling as usual for substance use problems. Journal of Consulting and Clinical Psychology. 2009;77:1125–1135. doi: 10.1037/a0017045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crits-Christoph P, Gibbons MBC, Mukherjee D. Psychotherapy process-outcome research. In: Lambert MJ, editor. Bergin and Garfield’s handbook of psychotherapy and behavior change. 6th. Hoboken, NJ: Wiley; 2013. pp. 298–340. [Google Scholar]
- Ehrman RN, Robins SJ. Reliability and validity of 6 month timeline reports of cocaine and heroin use in a methadone population. Journal of Consulting and Clinical Psychology. 1994;6:843–850. doi: 10.1037//0022-006x.62.4.843. [DOI] [PubMed] [Google Scholar]
- Enders CK, Tofighi D. Centering predictor variables in cross-sectional multilevel models: A new look at an old issue. Psychological Methods. 2007;12:121–138. doi: 10.1037/1082-989X.12.2.121. [DOI] [PubMed] [Google Scholar]
- Epstein EE, Drapkin ML, Yusko DA, Cook SM, McCrady BS, Jensen NK. Is alcohol assessment therapeutic? Pretreatment change in drinking among alcohol-dependent women. Journal of Studies on Alcohol. 2005;66:369–378. doi: 10.15288/jsa.2005.66.369. [DOI] [PubMed] [Google Scholar]
- Falkenström F, Granström F, Holmqvist R. Therapeutic alliance predicts symptomatic improvement session by session. Journal of Counseling Psychology. 2013;60:317–328. doi: 10.1037/a0032258. [DOI] [PubMed] [Google Scholar]
- Falkenstrom F, Hatcher RL, Skjulsvik T, Larsson M, Holmqvist R. Development and validation of a 6-item Working Alliance Questionnaire for repeated administrations during psychotherapy. Psychological Assessment. 2015;27:169–183. doi: 10.1037/pas0000038. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-Mental State: A practical guide for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Horvath AO. Research on the alliance. In: Horvath AO, Greenberg LS, editors. The working alliance: Theory, research, and practice. New York, NY: John Wiley & Sons; 1994. pp. 259–286. [Google Scholar]
- Horvath AO, Del Re AC, Fluckiger C, Symonds D. Alliance in individual psychotherapy. Psychotherapy. 2011;48:9–16. doi: 10.1037/a0022186. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. The development of the Working Alliance Inventory. In: Greenberg LS, Pinsof WM, editors. The psychotherapeutic process: A research handbook. New York, NY: Guilford Press; 1986. pp. 529–556. [Google Scholar]
- Horvath AO, Greenberg LS, editors. The working alliance: Theory, research, and practice. New York, NY: John Wiley & Sons; 1994. [Google Scholar]
- Horvath AO, Symonds BD. Relation between working alliance and outcome in psychotherapy: A meta-analysis. Journal of Counseling Psychology. 1991;38:139–149. [Google Scholar]
- Hox JJ. Multilevel analysis: Techniques and applications. 2nd. New York: Routledge; 2010. [Google Scholar]
- Kadden R, Carroll K, Donovan D, Monti P, Abrams D, Litt M, Hester R. Cognitive-behavioral coping skills therapy manual. Rockville, MD: NIAAA; 1992. [Google Scholar]
- Kaminer Y, Burleson JA, Burke RH. Can assessment reactivity predict treatment outcome among adolescents with alcohol and other substance use disorders? Substance Abuse. 2008;29:63–69. doi: 10.1080/08897070802093262. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Lingiardi V, Colli A. Therapeutic alliance and alliance ruptures and resolutions: Theoretical definitions, assessment issues, and research findings. In: Gelo OCG, Pritz A, Rieken B, editors. Psychotherapy research: Foundations, process, and outcome. New York: Springer-Verlag; 2015. pp. 311–329. [Google Scholar]
- Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2000;68:438–450. [PubMed] [Google Scholar]
- Meier PS, Barrowclough C, Donmall MC. The role of the therapeutic alliance in the treatment of substance misuse: A critical review of the literature. Addiction. 2005;100:304–316. doi: 10.1111/j.1360-0443.2004.00935.x. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Irwin TW, Wainberg ML, Parson JT, Muench F, Bux DA, Jr, Kahler CW, Marcus S, Schultz-Heik J. A randomized controlled trial of goal choice interventions for alcohol use disorders among men who have sex with men. Journal of Consulting and Clinical Psychology. 2007;75:72–84. doi: 10.1037/0022-006X.75.1.72. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA) NIAAA Council approves definition of binge drinking. NIAAA Newsletter. 2004;3:4. [Google Scholar]
- Orlinsky DE, Ronnestad MH, Willutzki U. Fifty years of psychotherapy process-outcome research: Continuity and change. In: Lambert MJ, editor. Bergin and Garfield’s handbook of psychotherapy and behavior change. 5th. Hoboken, NJ: Wiley; 2004. pp. 307–389. [Google Scholar]
- Penberthy JK, Ait-Daoud N, Breton M, Kovatchev B, DiClemente CC, Johnson BA. Evaluating readiness and treatment seeking effects in a pharmacotherapy trial for alcohol dependence. Alcoholism: Clinical and Experimental Research. 2007;31:1538–1544. doi: 10.1111/j.1530-0277.2007.00448.x. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong YF, Congdon RT, du Toit M. HLM 7 : Hierarchical linear and nonlinear modeling. Lincolnwood, IL: Scientific Software International, Inc; 2011. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd. Thousand Oaks, CA: Sage Publications, Inc; 2002. [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Scientific Software International, Inc. Comparing non-linear models in HLM. 2005–2016 Retrieved from http://www.ssicentral.com/hlm/help7/faq/FAQ_Comparing_non-linear_models_in_HLM.pdf. [Google Scholar]
- Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar G. The Mini-International Neuropsychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Janavs J, Weiller E, Bonara LI, Keskiner A, Schinka J, Knapp E, Sheehan MF, Dunbar GC. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. European Psychiatry. 1997;12:232–241. [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported ethanol consumption. In: Allen J, Litten R, editors. Techniques to assess alcohol consumption. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Sobell LC, Sobell MB. Alcohol timeline followback (TLFB) user’s manual. Toronto: Addiction Research Foundation; 1996. [Google Scholar]
- Stasiewicz PR, Schlauch RC, Bradizza CM, Bole CW, Coffey SF. Pretreatment changes in drinking: Relationship to treatment outcomes. Psychology of Addictive Behaviors. 2013;27:1159–1166. doi: 10.1037/a0031368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tracey TJ, Kokotovic AM. Factor structure of the Working Alliance Inventory. Psychological Assessment. 1989;1:207–210. [Google Scholar]
- Wechsler H, Nelson TF. Binge drinking and the American college student: What’s five drinks? Psychology of Addictive Behaviors. 2001;15:287–291. doi: 10.1037//0893-164x.15.4.287. [DOI] [PubMed] [Google Scholar]
- Zilcha-Mano S, Dinger U, McCarthy KS, Barber JP. Does alliance predict symptoms throughout treatment, or is it the other way around? Journal of Consulting and Clinical Psychology. 2014;82:931–935. doi: 10.1037/a0035141. [DOI] [PMC free article] [PubMed] [Google Scholar]