Abstract
Objective
To assess the clinical status of chronic spontaneous urticaria (CSU) and understand treatment approaches in Italy through specialists who treat CSU (dermatologists and allergy specialists) and CSU patients' experience.
Design
Multicentre survey.
Setting
Online structured questionnaires (one for physicians and one for patients).
Participants
Physicians and patients with CSU in Italy.
Interventions
None.
Primary/secondary outcomes
Physician and patient attitudes/experiences.
Results
Survey results from 160 allergy and 160 dermatology specialists show that specialists see a median of 40 (IQR 20–80) patients with CSU/year. While most specialists (56%) know the CSU guidelines, only 27% use them regularly (36% of allergy specialists vs 18% of dermatologists). This is reflected in treatment choices with differences between physicians who use guidelines regularly and those who do not: 91.6% vs 71.7% choose standard-dose, non-sedating antihistamines as first-line treatment; 85.9% vs 56.0% select up-dosing for second-line treatment and 65.3% vs 37.2% add leukotriene receptor antagonists or H2-antihistamines as third-line treatment. The diaries from 1385 patients highlight that, regardless of treatment regimen, 29.4% of currently treated patients are refractory to therapy. Specialists aim to resolve symptoms and only 7.8% report improving quality of life (QoL) as a priority. Only 16.6% of specialists are familiar with and use the Urticaria Activity Score while 46.9% do not know it. Overall, 537 patients with CSU were surveyed (median age 37 years, IQR 30–46; 44.3% men; median disease duration 5 years, IQR 3–20). Approximately 62% confirm that CSU negatively impacts their QoL. Patients also complain of difficulties in getting information and support: <5% of medical centres provide patient support services.
Conclusions
In Italy, the gap between guideline-based care and QoL-related needs in CSU patients affects treatment satisfaction. This information could be used to improve the management of CSU in Italy.
Keywords: chronic spontaneous urticaria, patient assessment, physician assessment, multicenter study, survey
Strengths and limitations of this study.
A strength of the study is the representative sample of specialists who treat CSU and patients with CSU in Italy, giving insight into the management of this condition from dermatologists' and allergy specialists' experiences.
CSU specialists and patients are represented, with a maximum margin of error of ±5.3% (95% CI) and a maximum margin of error of ±4.2% (95% CI), respectively.
The conclusions drawn from the clinicians' perspective are supported by the collection of data from 1385 patient diaries.
The methodology minimises bias because the physician survey was conducted online, without the involvement of an interviewer; the physicians were responsible for compiling the survey and the patient diaries autonomously.
Limitations include those inherent to the survey/questionnaire format, such as subjective bias.
Introduction
Urticaria is a disease characterised by the spontaneous development of weals (papules or plaques) that are associated with itching, a burning sensation and/or pain; in some cases, they are also associated with angioedema.1 Weals typically resolve within several hours to a day with no residual appearance. Angioedema is also sudden in appearance, but the swelling of the subcutaneous (lower dermis and subcutis) or submucosal tissues is associated with pain rather than itching and a slower resolution than that for weals, generally up to 72 hours.1
Most cases of urticaria tend to be acute (<6 weeks); however, urticaria lasting for 6 weeks or more is considered chronic and is further classified as two subtypes, chronic spontaneous urticaria (CSU) and inducible urticaria. The cause of the spontaneous appearance of daily or episodic weals in CSU, with or without angioedema, can be known or unknown,1 and symptoms can last for more than 5 years.2 3
An estimated 0.5–1% of the population, including children and adults, may be affected by CSU.2 4 CSU is associated with a large societal burden, an impact on patients' personal life, reduced work performance and direct and indirect healthcare costs.5
The care of patients with CSU is challenging due to inability to identify the underlying cause, the unpredictable disease course, the high disease burden and the often limited efficacy of approved therapies.5 Furthermore, CSU can have a significant impact on the patient's quality of life (QoL), and patients with CSU often experience depression and anxiety related to the disease.4 6–8 Failed attempts to treat long-term symptoms can often lead to frustration on the part of the patient and the physician,5 and patients with long-term unresolved symptoms often present to a number of physicians in varying specialties in an attempt to seek relief.4
Data regarding CSU in Italy are currently limited. This survey aimed to assess the clinical status of CSU in Italy from the perspective of specialists who treat CSU (dermatologists and allergy specialists) and patients who have the disease. The specialists' therapeutic approach and the patients' experiences were assessed, with a focus on potential barriers to diagnosis and treatment that patients with CSU in Italy may experience.
Methods
Study design
This multicentre Italian survey comprised two questionnaires, one for physicians and one for patients with CSU. Only data from patients and physicians who accepted to be interviewed were collected. The survey was designed by an independent market research company (Stethos Marketing Research, Milan, Italy) and was tested with pilot interviews to specialists. Survey results were also collected and analysed by Stethos Marketing Research and stratified according to geographical area and hospital/centre size. Owing to the qualitative nature of these surveys, no inferential analyses were performed.
The research was conducted in conformity with the Code of Conduct 2014 of the European Pharmaceutical Market Research Association (EphMRA).
Physician survey
Data were collected from a sample of physicians, specifically specialists in dermatology or allergy, to assess their diagnostic-therapeutic approach to CSU. Physicians and centres were selected from a proprietary database of Stethos Marketing Research. In order to obtain a good level of confidence, 320 physicians—160 dermatologists and 160 allergy specialists—from across Italy who were directly involved in the diagnosis and treatment of CSU were enrolled.
Physicians were asked to complete a survey exploring their approach to the management of CSU and also provided completed patient diaries. The survey, consisting of 28 questions, some of them with subquestions (for a total of 37), was conducted online using a computer-assisted web interviewing (CAWI) platform with self-administered structured questions in Italian. The questions explored topics such as characteristics and records of patients with CSU seen in the clinical practice, patient management, treatments used, drivers for therapy, perceived goals, main drawbacks of therapy and the level of knowledge of existing guidelines (blank physician questionnaire forms, in Italian and translated into English, are provided in online supplementary files 1 and 2, respectively). The specialists completed online web patient diaries for the last five CSU patients examined during the study reference period. The objective was to collect at least 1000 patient diaries to allow for a robust data set including information about the diagnosis, the previous and current treatments and the frequency of visits (blank patient diaries forms, in Italian and translated into English, are provided in online supplementary files 3 and 4, respectively). This sample of interviewees was to be representative of the population of the CSU specialists in Italy, with a maximum margin of error of ±5.3 and a 95% CI.
bmjopen-2016-012378supp_file1.pdf (351.1KB, pdf)
bmjopen-2016-012378supp_file2.pdf (401.9KB, pdf)
bmjopen-2016-012378supp_file3.pdf (292.1KB, pdf)
bmjopen-2016-012378supp_file4.pdf (301KB, pdf)
Patient survey
The patient sample was targeted to ensure a good distribution by geographical area and size of the treating hospital. This was achieved by ranking the centres by the number of CSU patients being treated: the centres with the highest number of patients were selected. A random sample of patients with CSU being treated in each of these centres was asked to participate in the survey, before/after a routine assessment at the dermatology/allergy department. Planned enrolment was about 500 patients with CSU (an average of four to five patients from each centre). This sample of respondents to the patient survey was to be representative of the population of patients with CSU in Italy (0.5–1% of the Italian population), with a maximum margin of error of ±4.2 and a 95% CI.
The patient surveys were self-administered via a CAWI system platform and comprised 46 questions; some of them with subquestions (for a total of 50), including those where the respondents could provide demographic details, disease characteristics and disease history, rate their QoL and their treatment satisfaction. To investigate the journey of a patient with CSU arriving at a dermatology/allergy hospital centre, the survey questions aimed to identify the steps followed and the possible barriers encountered during the diagnostic and therapeutic pathway and to assess the impact of the condition on the patients' QoL (blank patient questionnaire forms, in Italian and translated into English, are provided in online supplementary files 5 and 6, respectively).
bmjopen-2016-012378supp_file5.pdf (490.8KB, pdf)
bmjopen-2016-012378supp_file6.pdf (361.5KB, pdf)
Results
Specialist perspective
Demographic distribution of specialists
In total, 320 physicians (160 allergy and 160 dermatology specialists) from 194 centres in Northern (35.1%), Central (26.8%) and Southern (38.1%) Italy participated in the survey and collected 1385 online patient diaries. The data were collected from 29 January 2014 to 7 April 2014. The distribution of allergy and dermatology specialists working in hospital practice (18.8% vs 16.9%), hospital and private practice (49.4% vs 40.0%) or private practice only (31.9% vs 43.1%) was similar between groups.
Patients managed by the specialists
The allergy and dermatology specialists reported managing a median of 40 (IQR 20–80) patients with CSU annually, among whom the incidence of angioedema was 35.9%. Almost half of the patients treated by these specialists were considered to have severe disease (n=681; 49.2%) while the remaining patients were considered to have mild CSU (n=704; 50.8%), as assessed by the evaluation of the 1385 patient diaries. The distribution of patients in relation to disease severity did not change when the patient data from allergy and dermatology specialists (n=662 and n=723, respectively) were assessed separately. The number and frequency of the patient symptoms were considered the key parameters for determining disease severity by both specialist groups, while the impact of CSU on patients QoL, the efficacy of the therapy and the comorbidities were deemed relevant by fewer specialists.
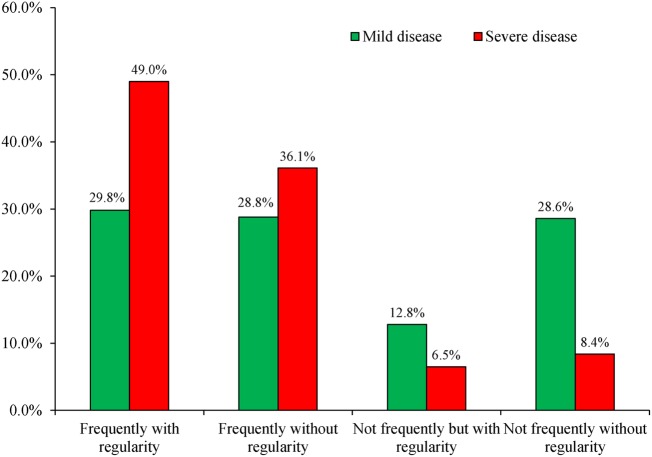
Among all the patients managed by the surveyed specialists, 39.3% had symptoms that appeared frequently and regularly; more patients with severe disease reported frequent and regular symptoms (49.0%). The majority of patients (71.7%) had frequent symptoms, with or without regularity. In patients with mild disease, the symptoms tended to manifest in an unpredictable manner (figure 1).
Figure 1.
Frequency and regularity of symptoms of chronic spontaneous urticaria in patients with mild disease as reported by their physicians.
Patient referral and disease diagnosis
Data from the patient diaries showed that patients were commonly referred to a CSU specialist by a general practitioner (32.6%), after visitation to the emergency department (21.2%), or, in 20.9% of patients, they sought a specialist themselves when symptoms appeared. Some patients were referred to the allergy and dermatology specialists by other specialists, including dermatologists (11.0%), allergy specialists (6.0%) or other specialists (2.2%). It was unknown how the remaining patients (6.2%) were referred to the specialist. The first symptoms reported by patients to specialists were hives (47.9%), itching (47.7%), urticaria (37.5%) and angioedema (24.8%). The latter was most frequently reported by severe patients (33.2%) compared with mild patients (15.9%). The diagnosis of CSU was established by a dermatologist in 67.3% of cases (either the surveyed (46.0%) or previous (21.3%) dermatologist) and an allergy specialist in 22.3% of cases (either the surveyed (14.4%) or previous (7.9%) allergy specialist). General practitioners (10.0%) or other specialists (0.4%) were involved markedly less frequently in diagnosing CSU. Among the 320 specialists surveyed, the diagnosis of CSU was established an average of 7 months (median of 4 months, IQR 2–10.5) after the onset of the first symptoms in patients.
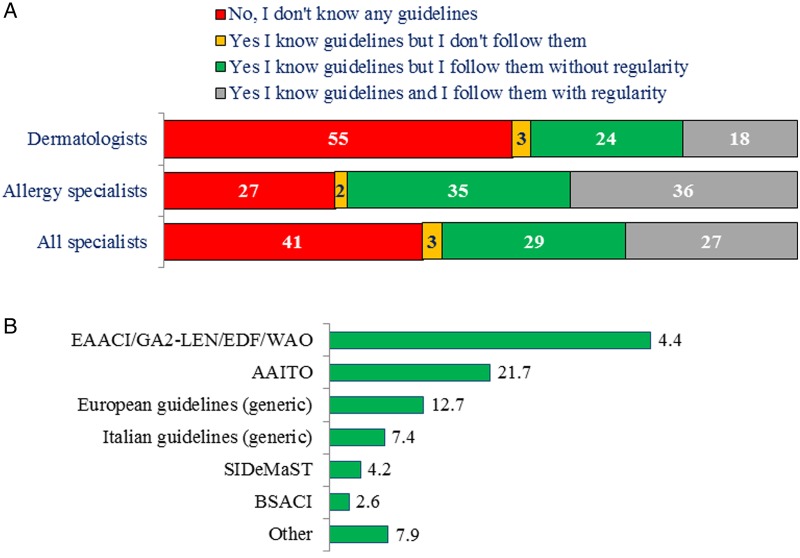
Specialists' knowledge of treatment guidelines
Among the 320 specialists surveyed, 56% were familiar with and used CSU guidelines, however, only 27% used them regularly. Compared with dermatologists, allergy specialists were twice as likely to regularly use guidelines (36% vs 18%) and more of them knew of the CSU guidelines (73% vs 45%; figure 2A). A total of 189 specialists confirmed that they knew CSU guidelines; the guidelines that were most frequently mentioned as known (the relevant survey question was open-ended) were those by the European Academy of Allergy and Clinical Immunology (EAACI/GA2LEN/EDF/WAO; 43.4%)9 and Associazione Allergologi Immunologi Territoriali e Ospedalieri (AAITO; 21.7%).10 The less-frequently known and used guidelines included those by Società Italiana di Dermatologia medica, chirurgica, estetica e delle Malattie Sessualmente Trasmesse (SIDeMaST; 4.2%),11 British Society for Allergy and Clinical Immunology (BSACI; 2.6%)12 and others (figure 2B).
Figure 2.
(A) Awareness and use of chronic spontaneous urticaria guidelines among the specialists surveyed and (B) guidelines known or followed. All values are percentages.
Symptomatic treatment of CSU
When queried about the ‘ideal sequence’ of symptomatic treatment for a patient with CSU (reflecting the approved indications at the time of the survey, in 2014), the majority (77.2%) of all specialists surveyed indicated that a standard dose of a non-sedating antihistamine (nsAH) was ideal as first-line treatment, while an increased-dose (<4 times the standard dose) nsAH was selected by 64.4% of specialists for second-line treatment. While 45.1% of specialists chose an increased-dose nsAH in combination with a leukotriene antagonist (LTRA)/H2-antihistamine as third-line treatment, 36.1% indicated an increased-dose nsAH in combination with steroids would be an ideal third-line treatment; 30.9% of physicians indicated that they would reserve the latter as fourth-line treatment, and 54.9% chose an increased-dose nsAH in combination with ciclosporin as a preferred fifth-line or sixth-line treatment.
Notably, knowledge and use of the CSU guidelines were reflected in treatment choices, with differences between physicians who use guidelines regularly and those who do not: 91.6% vs 71.7%, respectively, choose standard-dose nsAH as first-line treatment; 85.9% vs 56.0% select increased-dose nsAH for second-line treatment and 65.3% vs 37.2% add LTRA or H2-antihistamines to increased-dose nsAH for third-line treatment. The combination of increased-dose nsAH and steroids was considered for third-line treatment by 26.0% vs 39.5% of physicians, respectively, and for fourth-line treatment by 50.7% vs 24.2%; increased-dose nsAH in combination with ciclosporin was preferred for fifth-line treatment by 62.0% vs 52.2% of specialists.
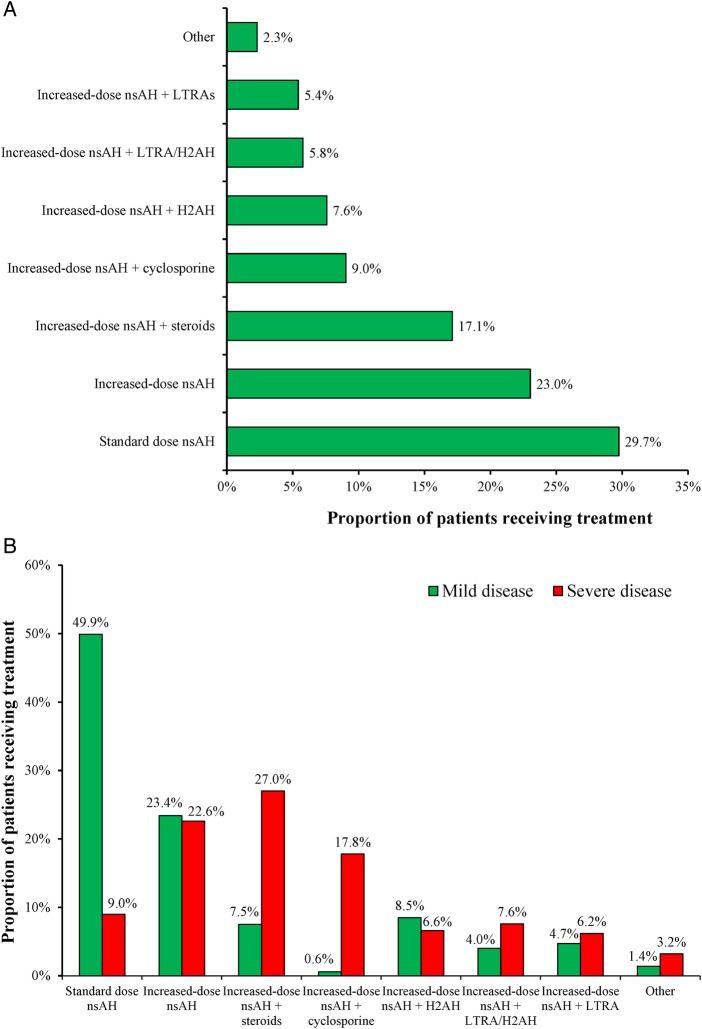
For the 1157 (83.5%) patients with CSU seen by the allergy and dermatology specialists, who were receiving treatment at the time of the survey, the majority received a standard-dose non-sedating H1-antihistamine or increased-dose non-sedating H1-antihistamine (figure 3A). Fewer patients were receiving an increased-dose nsAH either in combination with steroids, ciclosporin, H2-antihistamine, LTRA/H2-antihistamine or LTRA (figure 3A).
Figure 3.
(A) Therapies received by the 1157 patients with chronic spontaneous urticaria currently treated by 320 specialists surveyed and (B) therapies received by patients with severe and mild forms of the disease. H2AH, H2-antihistamine; LTRA, leukotriene receptor antagonist; nsAH, non-sedating antihistamine.
Comparing patients who had mild and severe disease, increased disease severity was associated with more complex treatment regimens, predominantly increased-dose nsAH in combination with steroids or ciclosporin. While standard-dose nsAHs were used as treatment for patients with mild disease, markedly fewer patients with severe disease received this treatment (figure 3B).
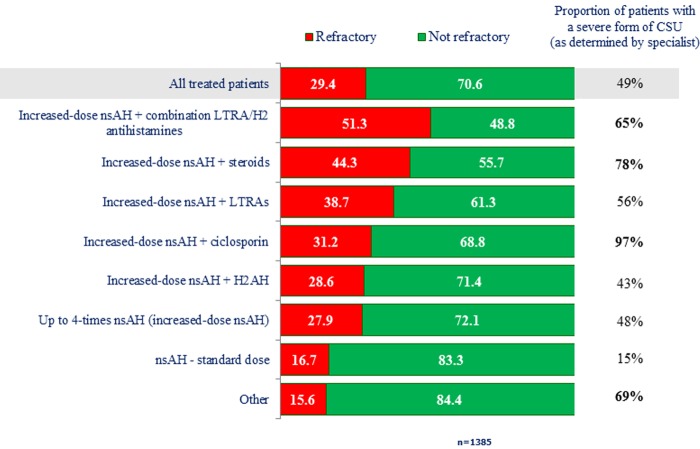
Refractory CSU
Regardless of the type of treatment received, 29.4% of all the patients with CSU currently treated were refractory to their therapy when the survey was conducted. Examining unresponsiveness for each current treatment showed that increased treatment was associated with increasing rates of unresponsiveness/disease severity (figure 4).
Figure 4.
Rates of refractory disease according to current treatment and disease severity. CSU, chronic spontaneous urticaria; H2AH, H2-antihistamine; LTRA, leukotriene receptor antagonist; nsAH, non-sedating antihistamine.
Treatment goals
For the specialists surveyed, the main goal of treatment was to reduce the symptoms of CSU, in particular itching (87.8%) and hives (46.2%). Only 7.8% of physicians reported improving QoL as a priority, although 15.0% did consider this a second priority. Generally, there were no significant differences between allergy and dermatology specialists for treatment goals, except for a greater tendency of allergy specialists to report improvement of QoL as a second treatment goal (15.0%) compared with dermatologists (10.0%).
Disease activity assessment
Of all the specialists, 46.9% did not know the Urticaria Activity Score (UAS). Although 36.6% knew of the scale, only 16.6% were familiar with and used the scale. Furthermore, 51.6% of the specialists did not know the UAS 7 days (UAS7), which uses the sum of the daily UAS scores to supply a weekly UAS value, and only 6.6% used it. Finally, only 16.9% of the specialists surveyed were familiar with and used the Chronic Urticaria Quality of Life Questionnaire (CU-QoL).
There were no significant differences between the allergy and dermatology specialists in the familiarity and usage of the UAS/UAS7 scales; the proportion of specialists who were unfamiliar with the UAS (41.9% and 51.9%, respectively) and UAS7 (48.1% and 55.0%, respectively) scales was high in both groups.
Complexity of disease diagnosis
When all the specialists were asked to rate the level of complexity in diagnosing CSU on a scale of 1 to 10 (1=not at all complex; 10=extremely complex), 40% considered that there was a high level of complexity (≥8) in diagnosing CSU. When the 210 specialists who rated the level of complexity as >5 were queried about the elements that increase the complexity of diagnosing CSU, over half (55.2%) chose ‘several tests to diagnose CSU’, while 44.3% responded that it was due to ‘the great difficulty in identifying the cause of the pathology’; there were no significant differences in the responses to this questions between the allergy and dermatology specialists.
A quarter of all specialists surveyed (n=83) revealed that they consult with another specialist, and there is generally a high level of collaboration between allergy and dermatology specialists. In 95.3% of cases, the dermatologists requesting a colleague's opinion will turn to an allergy specialist, whereas 62.5% of allergy specialists will request a dermatologist's opinion and 70.0% the opinion of another allergy specialist.
Patient perspective
Demographic and disease characteristics
In total, 537 patient surveys were conducted between 6 May 2014 to 12 June 2014. The patients who responded to the survey (55.7% women) had a mean age of 39 years (median 37 years, IQR 30–46). Mean and median ages were similar between men (mean 39 years; median 38, IQR 31–46) and women (mean 39; median 37 years, IQR 29–46). Almost 84% of respondents were aged 50 years or under (table 1).
Table 1.
Baseline demographic characteristics of patients with CSU
| Characteristic or demographic | Patient survey respondents (N=537) |
|---|---|
| Gender, n (% patients) | |
| Female | 299 (55.7) |
| Male | 238 (44.3) |
| Age group, n (% patients) (years) | |
| ≤30 | 139 (25.9) |
| 31–40 | 175 (32.6) |
| 41–50 | 135 (25.1) |
| 51–60 | 66 (12.3) |
| >60 | 22 (4.1) |
| Geographical region, n (% patients) | |
| North-West | 141 (26.3) |
| North-East | 61 (11.4) |
| Centre | 106 (19.7) |
| South | 229 (42.6) |
| Disease severity, n (% patients) | |
| Mild | 120 (22.3) |
| Moderate | 323 (60.1) |
| Severe | 56 (10.4) |
CSU, chronic spontaneous urticaria.
At the time of the survey, patients had an average disease duration of 13 years (median 5 years, IQR 3–20) and 45.6% of patients had lived with the disease for 2–5 years (table 1). The majority of patients surveyed had moderate disease (table 1).
Impact of CSU on QoL
Almost two-thirds (61.6%) of patient respondents indicated that their CSU had a negative impact on their QoL, with a rating of 4–6 (1=no impact on QoL; 6=significant impact on QoL), while only 4.3% reported the CSU had no influence on their QoL. The frequency of patients rating the impact of CSU on their QoL as ≥4 to 6 varied with disease severity, from a minimum of 35.8% of patients with mild disease to 70.0% and 80.4% of patients with moderate and severe disease, respectively. One-third (33.9%) of patients with severe CSU rated the level of disease influence on their QoL as 6 (significant), compared with 5.9% and 3.3% of patients with moderate and severe disease, respectively.
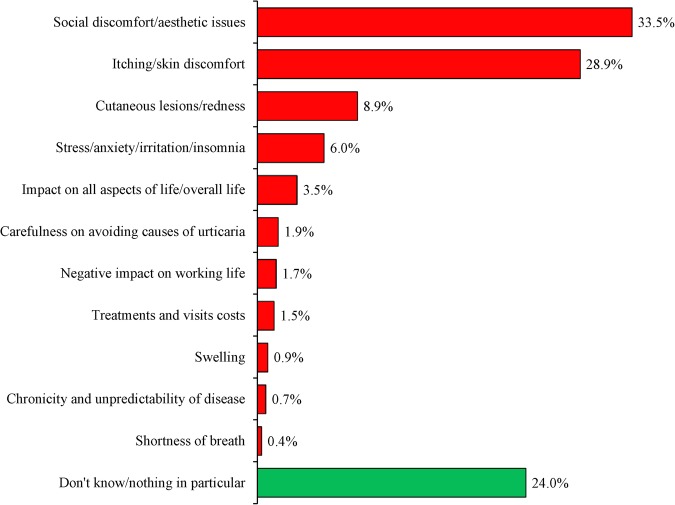
The most frequent reasons cited for decreased QoL were social discomfort/aesthetic issues (33.5%) and itching/skin discomfort (28.9%; figure 5). The frequency of reasons cited as negatively influencing QoL did not vary greatly when the patients were stratified by disease severity; however, a greater number of patients with severe CSU than those with moderate or mild disease reported stress/anxiety/irritation/insomnia (12.5% vs 5.9% and 0.8%) and negative impact on working life (7.1% vs 0.9% and 0.8%) as influencing their QoL.
Figure 5.
The most frequent reasons for decreased quality of life as reported in the survey of patients with chronic spontaneous urticaria (N=357). Reasons shown are the answers to question 29 of the survey “What aspect of your disease would you indicate as the most impactful on your life?”.
Choice of physician
One-third of patients (35.2%) had seen other physicians prior to their current one. On average patients had previously changed at least two specialists. The most frequent reason for changing physicians was ‘dissatisfaction with the medical staff of the previous facility’ (23.3%), followed by ‘the current center/physician is closer to where I live’ (20.6%), ‘previous physicians were not able to find the right therapy’ (19.6%), ‘previous physicians took too long to diagnose my disease’ (18.0%), ‘innovative therapies that I couldn't access before are available in the new center’ (14.8%) and ‘other’ (3.7%). The number of specialists that the patient changed in the past did not vary significantly when the sample was stratified by disease severity.
Provision of support services and patient information channels
Less than 5% of respondents indicated that the medical centre that they attended provided patient support services. When support services were provided, these included support for families, psychological support and use of specific lotions.
Hard copy disease-related material (eg, brochures about CSU) was distributed to 34.6% of respondents when they attended their care facility. The types of brochures provided included information/advice about: diet and lifestyle (65.1%), pathology evolution and symptoms (50.5%), general CSU information (45.7%), therapies (38.7%), patient diaries (21.0%) and modes of administration (19.9%).
When asked about the communication channels they used to access updates or information about their disease, 67.7% of patients responded that they had obtained information from internet sources at least once, including CSU-related websites, general internet searches and online forums, while 41.3% asked a dermatologist. The types of channels through which patients received their information are summarised in table 2.
Table 2.
Sources of disease information accessed by the patients with CSU who responded to the survey
| Source of information, n (% of patients) | Patient survey respondents (N=537) |
|---|---|
| Dermatologist | 222 (41.3) |
| Online forums | 158 (29.4) |
| Internet in general | 137 (25.5) |
| Printed documentation | 133 (24.8) |
| CSU-dedicated website | 69 (12.8) |
| Conferences | 63 (11.7) |
| Hospital nurses | 38 (7.1) |
| Other | 18 (3.4) |
| Patient association | 10 (1.9) |
| None | 60 (11.2) |
CSU, chronic spontaneous urticaria.
Discussion
On the basis of the survey results, the specialists who treat CSU throughout Italy are managing a median 40 patients with CSU each year. About half of CSU patients seen by allergy and dermatology specialists have mild CSU whereas the other half have severe disease. However, due to high proportion of specialists of both groups who were not familiar with the UAS and UAS7 scales, the classification of disease severity may not have been sufficiently objective. The limited use of such scales was probably due to the fact that the 2009 EAACI/GA2LEN/EDF/WAO urticaria guidelines (the current version at the time the survey was conducted) did not mention them.9 The importance of this clinical tool has to be stressed for initial disease severity grading and for monitoring treatment efficacy.
A third of patients are referred to a CSU specialist by a general practitioner and a fifth by emergency department staff or self-referral at symptom onset. Notably, more dermatologists than allergy specialists established the diagnosis of CSU. This may simply reflect the fact that, in Italy, dermatology specialists outnumber allergy specialists by three to one, therefore dermatologists are more accessible to patients than allergy specialists. General practitioners were only involved in the diagnosis of 10% of patients with CSU, emphasising the complexity of diagnosing the disease and the need of referral to a specialist to establish a diagnosis. Overall, diagnosis was established on average 7 months after the appearance of the first symptoms, although time to diagnosis was increased with disease severity, possibly because a more accurate medical history has to be collected from each patient. Highlighting the complexity of the disease itself, 40% of specialists surveyed felt that CSU diagnosis was complex and the difficulty in identifying the cause of the pathology and the multiplicity of tests available for diagnosis were listed as factors contributing to the level of complexity in disease diagnosis. On the other hand, the international guidelines strongly recommend only very limited routine diagnostic evaluations in CSU to reduce the number of diagnostic tests.1
For most of the allergy and dermatology specialists, the ideal sequence of treatment, at the time of the survey, would be a standard and an increased dose of an nsAH as first-line treatment and second-line treatment, respectively. For third-line treatment for non-responders, specialists tended to favour treatment with an increased dose nsAH in combination with a LTRA and an H2-antihistamine or an increased dose nsAH in combination with a steroid or ciclosporin, a regimen especially preferred in more severe disease. Nevertheless, regardless of treatment regimen, over a quarter of all patients with CSU were refractory to the therapy they were receiving, and even complex/aggressive treatment regimens failed to resolve symptoms in almost half of the patients with severe disease. It should be noted that, at the time of the survey, a new therapeutic option was not yet authorised for CSU treatment. However, since then the approach to patients with refractory CSU has changed: the current EAACI/GA2LEN/EDF/WAO guidelines describe omalizumab as a third-line treatment for urticaria and the Italian regulatory authorities recommend to use omalizumab when patients do not respond to a standard dosage of nsAH.1
Moreover, data suggest that continuous therapy is associated to improved outcomes in terms of QoL.5 However, this is not always reflected in real life: a survey in patients with CSU in Germany and France showed that 78% of patients were taking medication for their CSU, but only 33% of these were taking it regularly for symptom prevention.13
For the specialists surveyed, the main goal of CSU treatment was key symptom resolution (itching and hives) and few considered improving QoL a priority. Importantly, the updated EAACI/GA2LEN/EDF/WAO guidelines strongly recommend complete symptom control, as safely as possible, to be the goal of treatment.1 In a similar way, the 2009 EAACI/GA2LEN/EDF/WAO guidelines recommended that the aim of treatment was to achieve complete symptom relief.9 Appropriate management of CSU requires evidence-based guidance; however, only half of the specialists surveyed (more allergy specialists than dermatologists) knew of and used any of the CSU guidelines available, with allergy specialists twice as likely as dermatologists to use guidelines. Notably, the level of knowledge and use of the guidelines correlated with the treatment choices and therapies selected by physicians not using guidelines were more likely to be widely different and not in accordance with recommendations.
Similarly, there was a gap in the knowledge of the specialists regarding the main scales used to assess disease activity, with only approximately half of the surveyed specialists acknowledging familiarity with the UAS and UAS7, and only one-sixth acknowledging familiarity with and using the CU-QoL questionnaire. The 2014 EAACI/GA2LEN/EDF/WAO guidelines provide a strong recommendation that disease activity should be assessed in clinical care using the UAS7 and that the CU-QoL is one of the validated instruments for assessing QoL impairment and for monitoring disease activity.1 In the 2009 EAACI/GA2LEN/EDF/WAO guidelines, the UAS and UAS7 were not mentioned but the CU-QoL that had been generated and tested in the Italian language14 and had only recently been validated in other languages was recognised as a suitable instrument for the assessment of the health burden of CSU and its treatment.9
Among patients surveyed across Italy, the prevalence of CSU has been found to be about the same in women and in men, unlike reports from other countries.3 15 Similar to patients with CSU in other countries,16 about two-thirds of patients reported that CSU had a negative impact on their QoL, affecting their personal and professional life, and the frequency and level of impact increased with disease severity. More patients with severe disease than those with moderate or mild disease cited stress/anxiety/irritation/insomnia and negative impact on working life as impacting QoL.
In their efforts to obtain symptom relief, over a third of patients had on average consulted two previous physicians. Surprisingly, the number of specialists changed did not vary significantly when stratified by disease severity. The most common reason for switching providers was dissatisfaction with medical staff. Attending multiple medical centres due to dissatisfaction with treatment and reports of reduced QoL are in accordance with existing literature in patients with CSU.4 6–8 A patient survey conducted in Germany and France also reiterated the impact CSU has on QoL and lack of satisfaction with physician care,16 with patients indicating they were only ‘somewhat satisfied’ with the care they were receiving. Satisfaction with treatment increased if the physician discussed the impact of CSU on emotions with their patient.
There appear to be a mismatch between patients with CSU and specialists as, while two-third of the patients reported CSU affecting their QoL, only 8% of specialists considered improving QoL as a priority. Our results suggest that there is a need for specialists to routinely use the CU-QoL, in order to assess how patients are affected by the disease, and the UAS to monitor the disease and provide the most appropriate treatment. It is therefore important for specialists to focus their attention on the burden and the unmet needs of CSU and establishing more satisfying treatment schemes.
Furthermore, most patients did not have patient support services available to them at their medical centre.
The limitations of the present study include those inherent in the survey/questionnaire format. Although the questionnaires were designed to minimise bias, there is always a subjective element remaining (eg, respondents tend to avoid scoring at the end of scales and answer in a way they perceive to be desired by the investigator/be more socially acceptable).17 A strength of the study is that, by selecting a representative sample of patients with CSU and of specialists involved in the treatment of CSU in Italy, it provides a snapshot of the management of this condition from both perspectives, thereby highlighting current gaps in guideline-based care and unmet patient needs.
Conclusions
In general, patients with CSU in Italy are similar to patients with CSU in other countries. However, there are some gaps in the care of these patients resulting in treatment dissatisfaction and a decreased QoL. These results should be used to improve the treatment of patients with CSU in Italy, in particular by reinforcing the knowledge of the available tools, such as the UAS and CU-QoL questionnaires, which can be used to assist specialists in treating patients with CSU.
Acknowledgments
The authors thank all participants in this survey; Vincenza Vinaccia, Veronica Graus and Lorenzo Carraro of Novartis, Katia Massaroni, formerly of Novartis, and Nicola Negri, formerly of Stethos, for their constructive feedback and suggestions during preparation of the manuscript. Medical writing assistance in drafting the outline and second draft for this manuscript as well as formatting for submission was provided by Sheridan Henness, PhD, and Cécile Duchesnes, PhD, of Springer Healthcare Communications, while the first draft was prepared by Nila Bhana, an independent medical writer, on behalf of Springer Healthcare Communications.
Footnotes
Contributors: MR and NR were responsible for conception and design of the survey. MR was responsible for the acquisition of data; MR and NR had full access to the final data and performed the analysis. MR, NR and OR contributed to data interpretation and to the drafting and critical revision of the manuscript. All authors approved the final version and have final responsibility for content.
Funding: Funding for the conduct of the survey, as well as for medical writing assistance and article processing charges, was provided by Novartis Farma, Italy.
Competing interests: OR has been consultant and speaker for Meda, Novartis, MSD and Menarini in the last 5 years. MR is a partner of Stethos Srl and holds shares of this company. Stethos Srl collaborates with Novartis Farma, Italy on several market research studies. NR is an employee of Novartis Farma, Italy.
Ethics approval: The research was conducted in conformity with the Code of Conduct 2014 of the European Pharmaceutical Market Research Association (EphMRA).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Zuberbier T, Aberer W, Asero R et al. The EAACI/GA(2) LEN/EDF/WAO Guideline for the definition, classification, diagnosis, and management of urticaria: the 2013 revision and update. Allergy 2014;69:868–87. 10.1111/all.12313 [DOI] [PubMed] [Google Scholar]
- 2.Greenberger PA. Chronic urticaria: new management options. World Allergy Organ J 2014;7:31 10.1186/1939-4551-7-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gaig P, Olona M, Muñoz Lejarazu D et al. Epidemiology of urticaria in Spain. J Investig Allergol Clin Immunol 2004;14:214–20. [PubMed] [Google Scholar]
- 4.Ben-Shoshan M, Blinderman I, Raz A. Psychosocial factors and chronic spontaneous urticaria: a systematic review. Allergy 2013;68:131–41. 10.1111/all.12068 [DOI] [PubMed] [Google Scholar]
- 5.Maurer M, Weller K, Bindslev-Jensen C et al. Unmet clinical needs in chronic spontaneous urticaria. A GA2LEN task force report. Allergy 2011;66:317–30. 10.1111/j.1398-9995.2010.02496.x [DOI] [PubMed] [Google Scholar]
- 6.Ue AP, Souza PK, Rotta O et al. Quality of life assessment in patients with chronic urticaria. An Bras Dermatol 2011;86:897–904. [DOI] [PubMed] [Google Scholar]
- 7.Engin B, Uguz F, Yilmaz E et al. The levels of depression, anxiety and quality of life in patients with chronic idiopathic urticaria. J Eur Acad Dermatol Venereol 2008;22:36–40. 10.1111/j.1468-3083.2007.02324.x [DOI] [PubMed] [Google Scholar]
- 8.Staubach P, Eckhardt-Henn A, Dechene M et al. Quality of life in patients with chronic urticaria is differentially impaired and determined by psychiatric comorbidity. Br J Dermatol 2006;154:294–8. 10.1111/j.1365-2133.2005.06976.x [DOI] [PubMed] [Google Scholar]
- 9.Zuberbier T, Asero R, Bindslev-Jensen C et al. EAACI/GA(2)LEN/EDF/WAO guideline: management of urticaria. Allergy 2009;64:1427–43. 10.1111/j.1398-9995.2009.02178.x [DOI] [PubMed] [Google Scholar]
- 10.Tedeschi A, Girolomoni G, Asero R. AAITO position paper. Chronic urticaria: diagnostic workup and treatment. Eur Ann Allergy Clin Immunol 2007;39:225–31. [PubMed] [Google Scholar]
- 11.Vena GA, Cassano N, Pigatto PD et al. Orticaria. In: Linee Guida e Raccomandazioni SideMaST. Pisa, Italy: Pacini Editore, 2011. [Google Scholar]
- 12.Powell RJ, Leech SC, Till S et al. , British Society for Allergy and Clinical Immunology. BSACI guideline for the management of chronic urticaria and angioedema. Clin Exp Allergy 2015;45:547–65. 10.1111/cea.12494 [DOI] [PubMed] [Google Scholar]
- 13.Maurer M, Ortonne JP, Zuberbier T. Chronic urticaria: an internet survey of health behaviours, symptom patterns and treatment needs in European adult patients. Br J Dermatol 2009;160:633–41. 10.1111/j.1365-2133.2008.08920.x [DOI] [PubMed] [Google Scholar]
- 14.Baiardini I, Pasquali M, Braido F et al. A new tool to evaluate the impact of chronic urticaria on quality of life: chronic urticaria quality of life questionnaire (CU-QoL). Allergy 2005;60:1073–8. 10.1111/j.1398-9995.2005.00833.x [DOI] [PubMed] [Google Scholar]
- 15.Marzano AV, Pigatto P, Cristaudo A et al. Management of chronic spontaneous urticaria: practical parameters. G Ital Dermatol Venereol 2015;150:237–46. [PubMed] [Google Scholar]
- 16.Maurer M, Ortonne JP, Zuberbier T. Chronic urticaria: a patient survey on quality-of-life, treatment usage and doctor-patient relation. Allergy 2009;64:581–8. 10.1111/j.1398-9995.2008.01853.x [DOI] [PubMed] [Google Scholar]
- 17.Choi BC, Pak AW. A catalog of biases in questionnaires. Prev Chronic Dis 2005;2:A13. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-012378supp_file1.pdf (351.1KB, pdf)
bmjopen-2016-012378supp_file2.pdf (401.9KB, pdf)
bmjopen-2016-012378supp_file3.pdf (292.1KB, pdf)
bmjopen-2016-012378supp_file4.pdf (301KB, pdf)
bmjopen-2016-012378supp_file5.pdf (490.8KB, pdf)
bmjopen-2016-012378supp_file6.pdf (361.5KB, pdf)