Abstract
Cocaine is a drug with relevant socioeconomic and clinical implications, which is usually recreationally used for its stimulant effects. It is widely known that the habit of snorting cocaine is associated with a peculiar type of drug-induced chronic rhinitis, which leads to inflammation of the sinonasal mucosa, slowly progressing to a destruction of nasal, palatal and pharyngeal tissues. These characteristic lesions due to cocaine abuse are commonly called cocaine-induced midline destructive lesions (CIMDL). Diagnosis is not always straightforward, since various conditions, mainly vasculitis, might mimic this acquired condition. The extent of pharyngeal involvement varies, although often a prolonged abuse can trigger a progressive destruction of oral and nasal tissues, with development of infections and recurrent inflammation. Our article focuses on cocaine as a world health problem with important ear, nose and throat implications and discusses the difficulties in diagnosing and treating CIMDL, through a case report.
Case presentation
We present a case of a Caucasian woman aged 38 years, known to our Head and Neck department for her long history of nasal cocaine abuse, leading to massive cocaine-induced midline destructive lesions (CIMDL), with almost complete resorption of the nasal pyramid. The patient had given up her drug abuse 5 years earlier, just before the beginning of surgical treatments. Regular drug tests were conducted through this period in order to confirm her rehab. She had already undergone a complete reconstruction of the nasal pyramid with local flaps and rib grafts. Nevertheless, she was suffering from a progressively widened palatal perforation, which caused passage of liquids and food from the oral cavity into the nasal cavities, swallowing difficulties and frequent epistaxis. At the time of presentation, the patient was using a palatal prosthesis, to fill the oronasal communication.
The patient presented to the Emergency Department of our hospital, reporting excruciating facial pain irradiated to the back of the neck, since 2 days. The pain was accompanied by sore throat, odynophagia and neck stiffness, moderate fever (peaking at 38°C) and chills. She also reported feeling purulent secretion drainage in her throat. The patient had been on amoxicillin clavulanate 1 g three times a day for 2 days, without any improvement. She asserted not to be on drugs for the past 5 years, which was confirmed by drug tests made during the following recovery.
The ear, nose and throat (ENT) evaluation confirmed the presence of an almost painless oronasal communication, with minimal marginal signs of necrosis, located in the middle and posterior third of the hard palate, with complete absence of the soft palate. Anterior rhinoscopy showed lack of the septum, with ubiquitous scabs and secretions. The patient was under follow-up for years, and these lesions did not seem altered compared to the latest ENT evaluation. Flexible endoscopy (see figure 1) revealed signs of rhinopharyngeal inflammation, with exposion of a bony wall, consisting of the clivus. Moreover, the endoscopic examination showed exposition of the occipital bone, which was covered with crusty material and surrounded by purulent secretions. It was the first time these lesions were identified in our patient.
Figure 1.
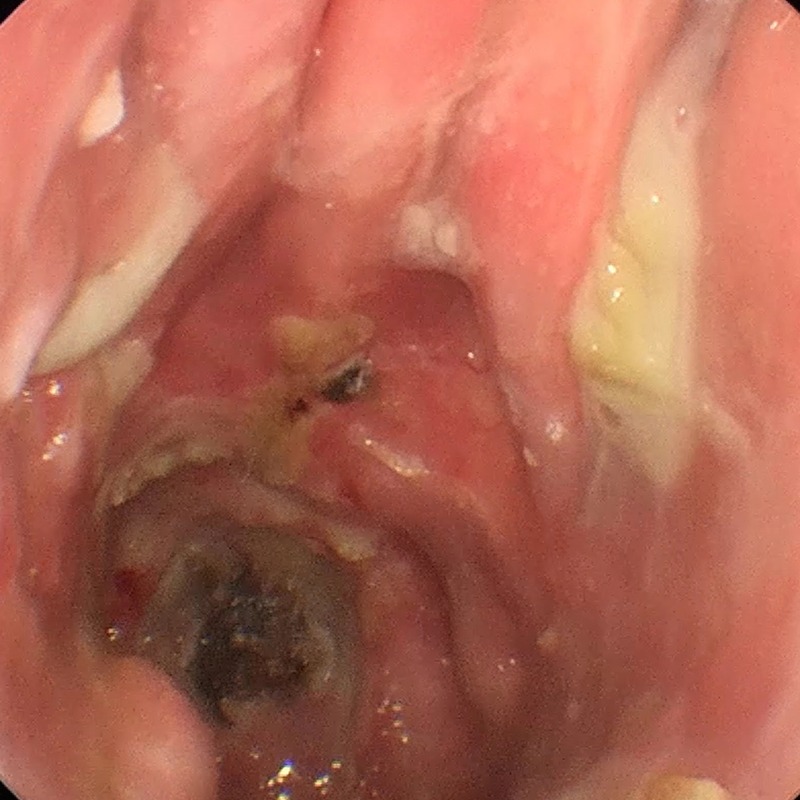
Endoscopic image showing the patient's extensive cocaine-induced midline destructive lesion, with ubiquitous crusting and mucous secretions. Hard and soft palate are lacking, as well as nasal septum and inferior nasal conchae. Clivus exposition, with signs of necrosis and inflammation at its margins, can be seen posteriorly.
After clinical evaluation, she underwent a CT with three-planar reconstructions, in order to quantify the bony erosion and to rule out meningeal and brain involvement. The CT scan confirmed complete resorption of the medial and lateral nasal cavity structures (nasal mucosa was eroded and thinned) and showed the exposition of the occipital bone's clivus, with signs of inflammation and suppuration (see figure 2).
Figure 2.
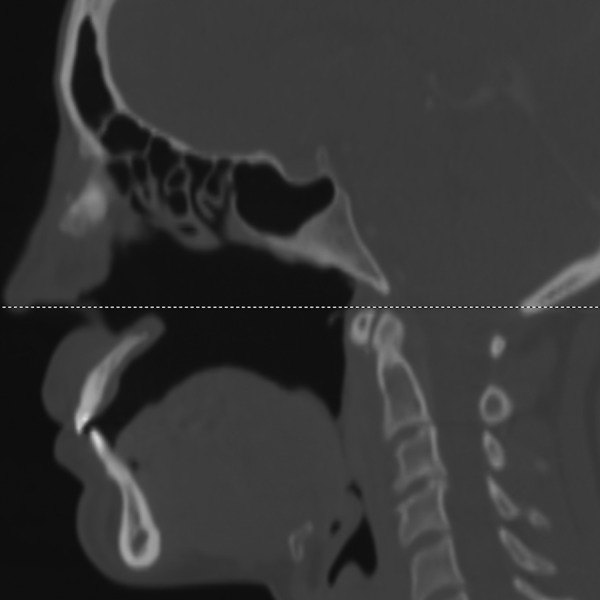
Sagittal image from a CT scan showing lack of bony nasal septum and palate (hard and soft parts). The rhinopharyngeal mucosa is eroded by prolonged cocaine abuse, with occipital bone clivus exposition.
The microbiologist prescribed a biopsy of the clivus lesion for diagnostic and therapeutic purposes. The specimens were collected under local anaesthesia and were sent for pathological and microbiological examinations. The results confirmed the presence of necrosis and chronic inflammation of the tissue and culture yielded growth of multidrug-resistant Staphylococcus aureus (S. aureus). Specimens were negative for granulomatous inflammation, typical of vasculitis. A chest CT scan was also conducted to rule out any pulmonary disease, which is common in patients with multidrug-resistant upper airways infections. The chest CT scan was normal.
We requested a neurosurgical consultation to rule out possible loss of skull base continuity, pneumocephalus, intracranial hypertension or cervical spine instability.
Routine blood exams were ordered and showed neutrophilia (15.620 WCC/mL with 82% neutrophils) and an increase in C reactive protein (CRP, 396 mg/L). Serology for HIV, hepatitis B virus and hepatitis C virus was negative.
The consulting microbiologist decided to hospitalise the patient in order to administer intravenous antibiotic therapy, based on antibiogram results (it revealed that all the bacteria isolated were sensitive to vancomycin and linezolid but resistant to erythromycin, ciprofloxacin, gentamicin, clindamicin and to tetracycline; the mic 50 and the mic 90 for vancomycin were 2 µg/mL). The patient underwent a broad-spectrum antibiotic intravenous treatment consinsting of metronidazole 500 mg four times a day, ceftazidime 2 g three times a day and vancomycin 500 mg four times a day for 10 days. Metronidazole was selected for its effect against anaerobic pathogens; vancomycin is indicated in Gram-positive infections unresponsive to other antibiotics, while ceftazidime, as part of the cephalosporins family, is ideal in treating respiratory diseases. Eight days after the beginning of intravenous therapy, inflammation signs started to decrease with an improvement in the patient's health conditions. CRP decreased from values of more than 400 mg/L to values of 58.3 mg/L.
Endoscopy and local lavages of crusts and suppuration were repeated every day during the whole hospitalisation to maintain the best sanitation possible, while the patient was ordered not to wear her palatal prosthesis during the whole treatment period in order to avoid local trauma and reinfection.
After 10 days of intravenous antibiotic treatment, the upper airway endoscopy showed no change in rhinopharynx anatomy, compared with the admission day examination, but signs of necrosis and acute inflammation were markedly decreased. General conditions, similarly, improved, along with the pain and neck stiffness.
Two weeks after hospitalisation, the defect size was stable, margins appeared healthy and there was no residual necrosis (figure 3). Microbiologist and ENT surgeon agreed for discharge; the patient was advised to keep the utmost oral and nasal cavity hygiene. She was solicited to continue saline nasal douches four times a day and to perform aerosol therapy with sodium hyaluronate 0.3%, in order to restore ciliary activity. No antibiotic therapy was prescribed at discharge.
Figure 3.

Endoscopical view of the patient after treatment and extensive douches and toilettes: rhinopharyngeal anatomy remains subverted, but acute inflammation signs decreased along with an improvement in patient's general health condition.
As far as the cocaine addiction was concerned, the patient was included in a supporting group, under psychologist guidance.
The patient is, at present, under close follow-up with endoscopic ENT evaluations every 2 months, to prevent infections, reduce the discomfort caused by scabs, secretions and dryness of nasal mucosa and to treat possible emerging lesions.
Global health problem list
The true incidence of cocaine-induced complications is unknown, probably greater than what we actually record, since abusers often disguise or deny their habit.
Cocaine addiction leads to numerous local lesions in ENT districts and can lead to a syndrome called cocaine-induced midline destructive lesions.
Skull bone clivus exposition as the only manifestation is quite impossible; therefore, when suspected, it is mandatory to look for other palatal and nasal lesions or inflammation signs.
Skull bone clivus exposition diagnosis and treatment are achieved by a multidisciplinary collaboration: ENT, microbiologist, neurosurgeon and maxillofacial surgeon.
CIMDL symptoms and signs are not always detriment, making the diagnosis difficult. Differential diagnosis is not always simple.
Surgical reconstruction can be realised using a variety of procedures and can be considered only when abuse has been interrupted.
Global health problem analysis
Cocaine was introduced into medical practice in the late nineteenth century as a local anaesthetic, due to its property of blocking sodium channels and interfering with peripheral nervous system transmission.1
Its recreational and para-recreational use varies according to local culture: while in some parts of South and Central America, people chew coca leaves, in the Western hemisphere, inhalation of the drug through the nose (snorting) is the most common habit, followed by crystallised cocaine smoking.2
Cocaine use in Europe is rising and so are midline oral–nasal tissues lesions. According to the annual report of the European Monitoring Centre for Drugs and Drug Addiction, cocaine is the most commonly used drug in Europe, primarily in the South and West of Europe. It has been calculated that almost 2.3 million young adults, aged 15–34, abused of cocaine in 2014, although the majority of people consume the drug occasionally (it is estimated that in 2014 about 1.9% of adults of such age group used cocaine).
Over 800 deaths associated with cocaine misuse were reported in 2013; Spain, Italy and the UK are the countries with the highest adult consumption rates and where the burden of dependency is more incisive on the population.3
The true incidence of cocaine-induced complications is unknown, probably greater than we actually record, since many patients do not show up to specialists and abusers often hide or deny their habit.4 Subsequently, interpreting recent data on cocaine-associated mortality is challenging.3
Cocaine addiction leads not only to health and physical systemic damages (such as malnutrition, weight loss and tendency to developing fungal and bacterial infections), but also to numerous local lesions in ENT districts, making the otolaryngologists a leading figure in the diagnosis and treatment of this disease.5
Oral cocaine use is uncommon, usually resulting in anaesthesia of the tongue and oral tissues. Inhalation, the most frequent intake route, may lead to epistaxis, chronic rhinitis, facial and temporomandibular joint pain, dysphonia, dysphagia, dysosmia or anosmia and, in most severe cases, nasopharyngeal ulceration. Nasal and palatal involvement can become extremely severe: snorting causes lytic destruction of the vomer, extending to the perpendicular plate of the ethmoid bone, resulting in nasal septum perforation, destruction of the lateral nasal walls, maxillary and ethmoid sinuses inflammation and typical deformation of nasal pyramid bones, called saddle nose deformity.6 7 In more advanced lesions, inferior, middle and superior nasal conchae are involved, with progressive resorption, allowing to an infection spread to the sphenoid sinus and the orbit.8 The progressive infection and resorption of facial tissues is commonly called cocaine-induced midline destructive lesion, an acquired life-threatening condition.9
Among these lesions, the most frequent and cited in medical literature are the palatal perforation and nasal septum alterations, the most prominent being the common finding of septum cartilage perforations.10
Though prolonged cocaine snorting may lead to erosion of rhinopharyngeal mucosa, exposing the occipital bone to the risk of serious infections. This is to the best of our knowledge the only case of clival exposure described in the literature. It is, therefore, impossible to quantify the real incidence of this condition.
Extensive cocaine abuse causes intrinsic cell degeneration and tissue damage, which may continue even after many years of abuse cessation. In our case, the patient had not been on drugs since 2011, but midline tissue absorption persisted.
Occipital bone lesions demonstrate mixed inflammatory cellular infiltrates and necrotising inflammation, caused by cocaine intrinsic properties. This drug is a potent vasoconstrictor, with sympathomimetic and catecholaminergic actions, that produces ischaemic necrosis and irritation of tissues, bringing to chronic mucosal destruction and inflammation. Microvascular damages, induced by cocaine, should be regarded as the foundation of CIMDL. A multifactorial pathogenesis has also been taken into consideration, where tissue cells are damaged by cocaine adulterants due to a decreased oxygen tension. Prolonged microvascular ischaemia might therefore force cells into apoptosis. Cell death in turn induces immunologic changes and makes the tissue exposed to inflammation and irritation.11
Furthermore, open lesions and necrosis create an ideal environment for anaerobic bacteria that cause multidrug-resistant infections, commonplace among CIMDL patients.
Skull bone clivus exposition as the only manifestation is quite impossible; for this reason, when suspected, it is essential to look for other palatal and nasal lesions or inflammation signs.
All the patients with CIMDL should follow a diagnostic protocol that includes blood exams, physical examination and radiological studies. Serologic markers of inflammation, including erythrocyte sedimentation rate (ESR) and CRP, may be elevated in some patients with CIMDL and can guide clinicians, especially during symptoms relapse and flogosis worsening. Patients with cocaine-associated sinonasal lesions are often Anca positive, so the titre and specificities of Anca may help to distinguish between CIMDL and other autoimmune diseases. ENT specialists should focus on patients' nasal and oral cavities; they can benefit from the use of upper airways endoscopy to evaluate nasal cavities and rhinopharynx, instead of a simple anterior rhinoscopy.
Radiological evaluation of cocaine-induced lesions is based on CT and MR imaging. CT imaging is superior in terms of bony erosion delimitation, while MR is the mainstay in detecting infiltrative processes of the skull base.
Neurosurgical evaluation helps ENT and clinicians to exclude the possibility of skull base perforation. The clivus is a part of the base of the skull, located between the foramen magnum and back of the sella, so the erosion of the bone could bring to the spreading of inflammation to the middle and posterior cranial fossa. Pneumocephalus (the presence of air within the cranial cavity) and intracranial hypertension (high pressure within the spaces that surround the brain) are only two of the possible complications of loss of skull base continuity. Looking at the CT scan, neurosurgeon rules out any central nervous system involvement and the need of surgical reconstruction.
CIMDL symptoms and signs are not always detriment, making the formulation of a correct diagnosis challenging.
First of all, cocaine abuse complications should be distinguished from other necrotising inflammatory damages, caused by systemic vasculitis, such as granulomatosis with polyangitis (previously Wegener's granulomatosis). Although cocaine abuse and vasculitis bring to chronic inflammation of tissues, with necrosis of the sinonasal mucosa, nasal and palatal perforation and midline destruction, they are two different conditions.12 13 granulomatosis with polyangiitis (GPA) is a systemic vasculitis, characterised by inflammation of small blood vessels, with necrotising granulomatous lesions, which affects in predominantly the upper and lower airways, in addiction to kidneys causing glomerulonefritis. Other diseases causing local necrosis, which should be taken into consideration, are solid lymphatic tumours, tertiary syphilis, traumas, chronic infections and, marginally, other malignancies.14
Localisation of lesions, which usually develop on the midline and spread laterally and posteriorly, might hint differential diagnosis against vasculitis, but these data are not sufficient. Furthermore, denial of drug abuse can challenge an accurate diagnosis.
Laboratory investigation and identification of antineutrophil cytoplasmic antibody (ANCA) can help clinicians in the differential diagnosis between lesions secondary to cocaine abuse and vasculitis. ANCA are a group of autoantibodies against antigens in the cytoplasm of neutrophil granulocytes, and they are detected in a large number of autoimmune disorders.
ANCA can be divided into two principal patterns as visualised by immunofluorescence: cytoplasmic ANCA (c-ANCA) and perinuclear ANCA (p-ANCA); the first show cytoplasmic granular fluorescence while the latter exibit perinuclear staining with nuclear extension. Another test used is enzyme-linked immunosorbent assay that helps in detecting Anca specific for PR3 or MPO.15 The c-ANCA pattern acts against proteinase 3 (PR3) while p-ANCA pattern corresponds to the presence of anti-MPO antibodies.16
The sensitivity of c-ANCA testing for diagnosing GPA ranges from 34% to 92%, and the specificity ranges from 88% to 100%.17
Occasionally, ANCA tests can result positive in patients with cocaine abuse too, showing some different patterns. Some patients' tests manifest positivity for C-Anca and PR3,18 some other for P-anca with specificity for atypical antigens such as human neutrophil elastase (HNE).19
The presence of these autoantibodies is often specific for CIMDL, because GPA is frequently anti-HNE negative. Wiesner explains how HNE anca may discriminate between CIMDL and GPA.
In conclusion, unlike GPA, CIMDL syndrome manifests characteristic P-Anca pattern directed towards elastase.19
Trimarchi et al evaluated 25 patients with sinus and nasal necrosis, due to cocaine, and 56% of them were ANCA positive (60% P-Anca, 40% C-anca).20
It is important to recognise lesions caused by cocaine from the ones caused by autoimmune diseases, not to impose a treatment with immunosuppressive drugs on the patients. In fact, induction therapy with prednisone and cyclophospamide, which are the main drugs of vasculitis treatment, is useless in CIMDL.13
Furthermore, patients with granulomatosis, such as GPA, always present not only midline involvement, but also a history of recurrent sinus infections, heart congestion and a glomerulonephritis that can evolve to kidney failure. The characteristic lung and renal involvement, histopathologic features and response to glucocorticoid therapy help clinicians in confirming diagnosis.
Since in a minority of patients ANCA positivity can underlie CIMDL and GPA, a biopsy is needed to finalise the diagnosis. Biopsies of sinonasal tissues, damaged by cocaine, reveal a mononuclear inflammatory infiltrate with necrotising inflammation, while small vessel granulomatous lesions guide to the presence of a vasculitis and exclude cocaine-induced damages. Furthermore, granulomas, microabscesses and giant cells are characteristic histopathologic hallmarks of GPA.20
Moreover, chronic invasive fungal rhinosinusitis can mimic CIMDL, but they often occur in the context of immunosuppression or immunodeficiency; however, the diagnosis of chronic invasive fungal diseases is confirmed by specific histopathology, showing fungal hyphae infiltrating mucosa or blood vessels.
When all laboratory tests, such as blood and urine exams, yield no results and the patient denies his/her addiction, the only way to reveal if the real origin of a midline lesion is a drug abuse can be detecting cocaine by conducting a drug hair test. Cocaine can be dosed in hair up to 3 months from use, while a small amount of cocaine is detected in blood only for 48 hours and persists in urine from 2 to 4 days. Cocaine does not leave marks at the root of the hair so it is incorporated into hair until the hair falls down or it is cut-off. It is essential to investigate possible antecedents of sustained cocaine abuse and snorting, focusing on the frequency and on abstinence periods. Patients have to be clearly advised that they must stop the habit in order to prevent lesion progression and prior to planning any surgical correction. The results and possible therapy success depend on patient's collaboration; in fact, if the abuse continues, any intervention, medical or surgical, is bound to fail. Stopping cocaine abuse not always interrupts lesions' progression. Our patient had not used cocaine since her first nasal surgery but long years of misuse lead to an unstoppable tissue degeneration. These particular patients should be followed up for years, after abuse cessation, in order to evaluate their clinical balance.
Daily nasal lavages and adequate oral hygiene can contribute to prevent infections, despite the use of a palatal prosthesis and cocaine-induced mucosa alterations can act as a breeding ground for bacterial growth. Nasal sprays have a cleaning and humidifying action and can be used with emollient unguents containing vitamin to relieve symptoms and bother.
In patients with multiple palatal or nasal lesions, treatment options include surgical closure of the defect or the placing of a removable obturator, when the lesion seems stabilised. The surgical technique is chosen according to the location and dimension of the lesion, duration of cocaine abuse, presence of infections and patient's general health conditions. Surgical approach demands the patient's collaboration and can only begin once the abuse has been stopped for at least 1 year. Abuse cessation can be proved by a negative hair drug test. Chronic abusers should be followed by helping groups before undertaking surgery.
Surgical reconstruction can be realised using a variety of procedures that are peculiar, also, in cleft palates fixing, such as tongue flaps, temporalis flaps, free revascularised flaps and buccal fat pad grafts.1 21 The reconstruction of the nasal structure can be achieved by using a fascio-cutaneous forearm free flap and a costal cartilage graft to restore the septum. However, if the palatal damage is extensive, a microvascular free flap, with or without bone transfer, from radial forearm or iliac crest should be carried out.22 23 Maxillofacial surgeons should keep in mind the pedicle length and the flap thickness, while choosing the flap, and must prefer free flaps to local flaps that are at high risk for partial or complete failure.8
Prosthetic obturators often match surgery, as a solution, if the patient complains about social problems and difficulties in communications, due to mutilating surgeries. These obturators are also indicated as a temporary solution or for patients who do not want to undergo surgery.24
Our patient had already undergone a complete reconstruction of the nasal pyramid with local flaps and rib grafts but, this time, for the clivus erosion, no other surgical treatments were needed. In fact, acute inflammation inhibits any surgical options; surgery should be postponed once the infection ended.
Nasal and palate reconstruction are basic in solving functional problems and aesthetic alterations. Overcoming cocaine-induced damages is very difficult and painful for the patients, who should be supported, by pharmacological and psychological treatment, while waiting for surgical reconstruction.
Learning points.
Cocaine abuse is a relevant clinical and social problem in Italy and worldwide. Though cocaine snorting always determines nasal mucosal damages, extensive septum perforations and midline destructions affect only a limited fraction of patients.
Clival exposition is an exceptional, but nevertheless dangerous complication in cocaine abusers. A quick clinical work-up and prompt appropriate treatment is mandatory. If clivus erosion is suspected, other midline lesions are present at the same time.
Otolaryngologists not only play an important role in the early and differential diagnosis of cocaine-induced midline destructive lesions (CIMDL) but are also leading components in surgical reconstruction of midline defects.
The treatment of CIMDL consists of a collaboration between clinicians, surgeons and the patient himself/herself. The cornerstone of treatment is maintaining cessation of cocaine abuse. If the abuse continues, any intervention is bound to fail.
Differential diagnosis from other midline destructive diseases, such as vasculitis, is crucial and challenging.
Footnotes
Contributors: AM did the surgery and took the biopsies. AMS helped in taking the biopsies and did the nasal endoscopy. He also helped in writing the article. KL helped in following up the patient. MM wrote the article and helped in doing the endoscopies.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Goodger NM, Wang J, Pogrel MA et al. Palatal and nasal necrosis resulting from cocaine misuse. Br Dent J 2005;198:333–4. 10.1038/sj.bdj.4812171 [DOI] [PubMed] [Google Scholar]
- 2.Marí A, Arranz C, Gimeno X et al. Nasal cocaine abuse and centrofacial destructive process: report of three cases including treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93:435–9. 10.1067/moe.2002.121989 [DOI] [PubMed] [Google Scholar]
- 3.European Monitoring Centre for Drugs and Drugs Adiction. http://www.emcdda.europa.eu/ (accessed 20 Nov 2015).
- 4.Serrano-Sanchez P, Bagan JV, Jimenez-Soriano et al. Palatal perforations secondary to inhaled cocaine abuse. Presentation of five cases. J Clin Exp Dent 2010;2:e105–9. [Google Scholar]
- 5.Gandara-Rey JM, Diniz-Freitas M, Gandara-Vila P et al. Lesions of the oral mucosa in cocaine users who apply the drug topically. Med Oral 2002;7:103–7. [PubMed] [Google Scholar]
- 6.Messinger E. Narcotic septal perforations due to drug addiction. JAMA 1962;179:964–5. 10.1001/jama.1962.03050120000013 [DOI] [PubMed] [Google Scholar]
- 7.Deutsch HL, Millard DR Jr. A new cocaine abuse complex. Involvement of nose, septum, palate, and pharynx. Arch Otolaryngol Head Neck Surg 1989;115:235–7. 10.1001/archotol.1989.01860260109024 [DOI] [PubMed] [Google Scholar]
- 8.Rubin K. The manifestation of cocaine-induced midline destructive lesion in bone tissue and its identification in human skeletal remains. Forensic Sci Int 2013;231:408.e1–11. 10.1016/j.forsciint.2013.04.034 [DOI] [PubMed] [Google Scholar]
- 9.Colletti G, Allevi F, Valassina D et al. Repair of cocaine-related oronasal fistula with forearm radial free flap. J Craniofac Surg 2013;24:1734–8. 10.1097/SCS.0b013e3182a2355a [DOI] [PubMed] [Google Scholar]
- 10.Tartaro G, Rauso R, Bux A et al. An unusual oronasal fistula induced by prolonged cocaine snort. Case report and literature review. Minerva Stomatol 2008;57:203–10. [PubMed] [Google Scholar]
- 11.Bianchi FA, Gerbino G, Tosco P et al. Progressive midfacial bone erosion and necrosis: case report and differential diagnosis. J Craniomaxillofac Surg 2014;42:1698–703. 10.1016/j.jcms.2014.06.002 [DOI] [PubMed] [Google Scholar]
- 12.Stahelin L, Fialho SC, Neves FS et al. Cocaine-induced midline destruction lesions with positive ANCA test mimicking Wegener's granulomatosis. Rev Bras Rheumatol 2012;52:431–7. 10.1590/S0482-50042012000300012 [DOI] [PubMed] [Google Scholar]
- 13.Rachapalli SM, Kiely PD. Cocaine-induced midline destructive lesions mimicking ENT-limited Wegener's granulomatosis. Scand J Rheumatol 2008;37:477–80. 10.1080/03009740802192043 [DOI] [PubMed] [Google Scholar]
- 14.Padilla-Rosas M, Jimenez-Santos CI, García-González CL et al. Palatine perforation induced by cocaine. Med Oral Patol Oral Cir Bucal 2006;11:239–42. [PubMed] [Google Scholar]
- 15.Savige J, Dimech W, Fritzler M et al. , International Group for Consensus Statement on Testing and Reporting of Antineutrophil Cytoplasmic Antibodies (ANCA). Addendum to the International Consensus Statement on testing and reporting of antineutrophil cytoplasmic antibodies. Quality control guidelines, comments and recommendations for testing in other autoimmune diseases. Am J Clin pathol 2003;120:312–18. [DOI] [PubMed] [Google Scholar]
- 16.Bradwell AR, Stokes RP. Advanced Atlas of autoantibody patterns. Birmingham: The Binding Site; 1999. [Google Scholar]
- 17.Schönermarck U, Lamprecht P, Csernok E et al. Prevalence and spectrum of rheumatic diseases associated with proteinase 3-antineutrophil cytoplasmic antibodies (ANCA) and myeloperoxidase-ANCA. Rheumatology (Oxford) 2001;40:178–84. 10.1093/rheumatology/40.2.178 [DOI] [PubMed] [Google Scholar]
- 18.Rowshani AT, Schot LJ, ten Berge IJM. C-anca as a serological pitfall. Lancet 2004;363:728 10.1016/S0140-6736(04)15694-8 [DOI] [PubMed] [Google Scholar]
- 19.Wiesner O, Russell KA, Lee AS et al. Antineutrophil cytoplasmatic antibodies reacting with human neutrophil elastase as a diagnostic marker for cocaine-induced midline destructive lesions but not vasculitis. Arthritis Rheum 2004;50:2954–65. 10.1002/art.20479 [DOI] [PubMed] [Google Scholar]
- 20.Trimarchi M, Nicolai P, Lombardi D et al. Sinonasal osteocartilaginous necrosis in cocaine abusers: experience in 25 patients. Am J Rhinol 2003;17:33–43. [PubMed] [Google Scholar]
- 21.Di Cosola M, Turco M, Acero J et al. Cocaine related syndrome and palatal reconstruction: report of a series of cases. Int J Oral Maxillofac surg 2007;36:721–7 10.1016/j.ijom.2007.03.015 [DOI] [PubMed] [Google Scholar]
- 22.Futran ND, Haller JR. Considerations for free-flap reconstruction of the hard palate. Arch Otolaryngol Head Neck Surg 1999;125:665. [DOI] [PubMed] [Google Scholar]
- 23.Colletti G, Autelitano L, Chiapasco M et al. Comprehensive surgical management of cocaine-induced midline destructive lesions. J Oral Maxillofac Surg 2014;72:1395.e1–10. [DOI] [PubMed] [Google Scholar]
- 24.Genden EM, Wallace DI, Okay D et al. reconstruction of the hard palate using the radial forearm free flap: indications and outcomes. Head Neck 2004;26:808–14. 10.1002/hed.20026 [DOI] [PubMed] [Google Scholar]


