Abstract
Colonic volvulus usually occurs as a single event that can affect various parts of the colon. The usual sites affected being the sigmoid colon (75%) and the caecum (22%). The phenomenon of multiple sites simultaneously undergoing volvulus is an extremely rare occurrence. Synchronous double colonic volvulus is extremely rare and to the best of our knowledge, this is the 4th reported case of simultaneous sigmoid and caecal volvulus in the English literature. The clinical presentation and the radiological findings are that of large bowel obstruction. Classic radiological findings may not be present or may be overlooked due to its rarity. Treatment of this condition is early surgical intervention to prevent the sequalae of a colonic volvulus and its associated mortality. We report a case of an 80-year-old man with synchronous volvulus of the sigmoid colon and caecum.
Background
Synchronous volvulus of the sigmoid colon and caecum is an extremely rare clinical entity. To the best of our knowledge, this is the fourth reported case of synchronous volvulus involving both the sigmoid colon and caecum. Its rarity requires it to reported and brought to the attention to practicing surgeons as an unusual cause of large bowel obstruction. Prompt surgical intervention is key to decreasing the morbidity and mortality associated with this uncommon condition.
Case presentation
An 80-year-old man, a patient with known hypertension and previous ischaemic stroke presented to our institution with a 2-day history of sudden onset abdominal distension and abdominal pain. He also reported of multiple episodes of vomiting and retching associated with constipation and inability to pass flatus. The patient has a history of chronic constipation and his drug history is significant for nifedipine 20 mg once daily. No recent weight loss or a family history of cancer was elicited.
He suffered an ischaemic stroke 1 year prior and lost the ability to move the entire right side of his body. He resides in an extended care facility for elderly individuals.
Examination revealed an elderly man in mild painful distress. His vital signs were significant for a tachycardia of 110 bpm and regular with the rest falling within normal limits. Mild dehydration was noted. Inspection of the abdomen revealed a markedly distended abdomen with mild tenderness to palpation throughout with the absence of guarding and rebound tenderness figure 1.
Figure 1.

Distended abdomen on inspection.
Digital rectum examination revealed an empty rectum, enlarged prostate with no other masses palpable.
Investigations
Full blood count and electrolytes were within normal limits.
Chest X-ray: Chilaiditi sign with dilated loops of bowel causing elevation of both hemidiaphragms figure 2.
Figure 2.
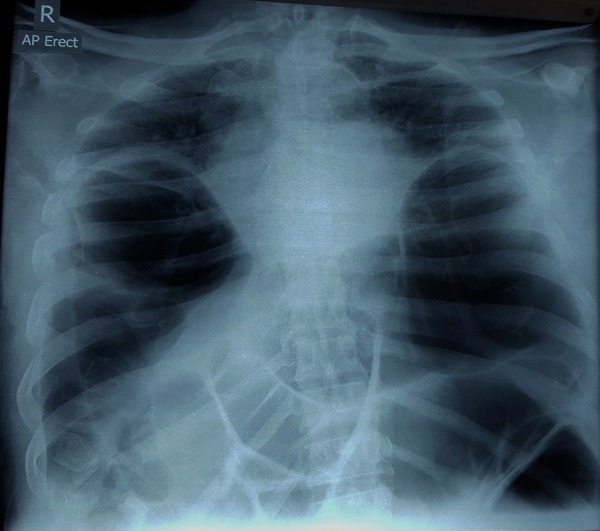
Chest X-ray demonstrating Chilaiditi's sign with bilateral elevated hemidiaphragms and dilated large bowel.
Abdominal X-ray: Dilated loops of large bowel figures 3 and 4.
Figure 3.
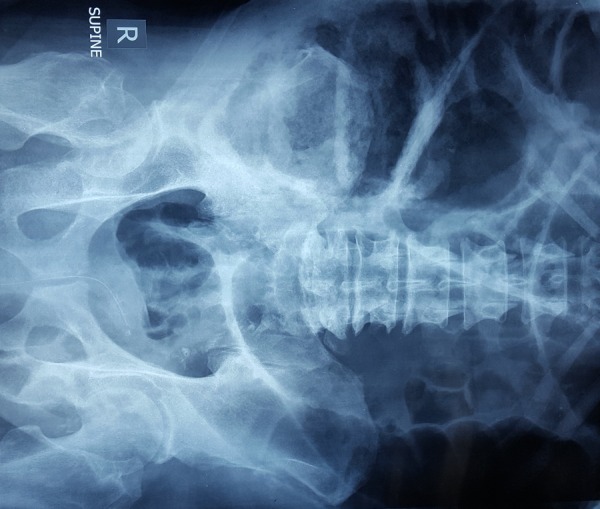
Abdominal X-rays demonstrating dilated loops of large bowel.
Figure 4.
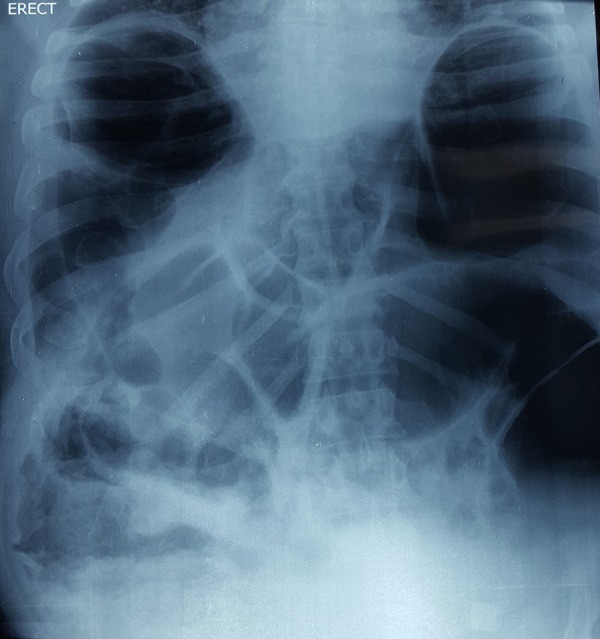
Abdominal X-rays demonstrating dilated loops of large bowel.
CT scan abdomen/pelvis with intravenous contrast:
On initial evaluation, it was reported as dilated loops of large bowel, maximum diameter 11 cm with a transition point in the sigmoid colon with collapsed small bowel figure 5.
Figure 5.
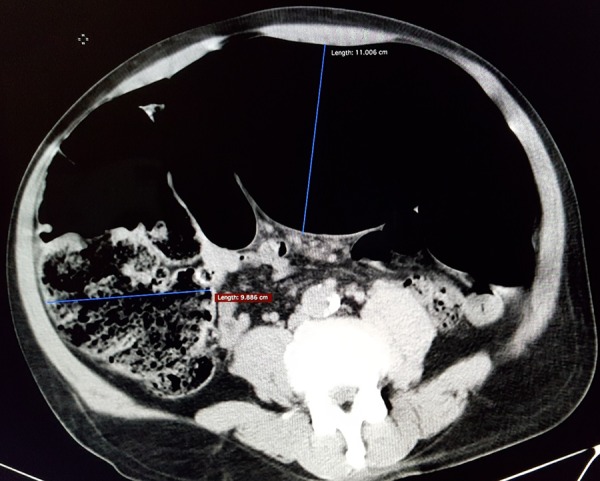
CT scan abdomen showing dilated large bowel, maximum transverse diameter 11 cm with collapsed small bowel.
However, on retrospective review (postsurgical intervention): CT scan demonstrated a sigmoid volvulus with an identifiable whirl sign figures 6 and 7.
Figure 6.

Scout CT film showing dilated large bowel and sigmoid volvulus.
Figure 7.
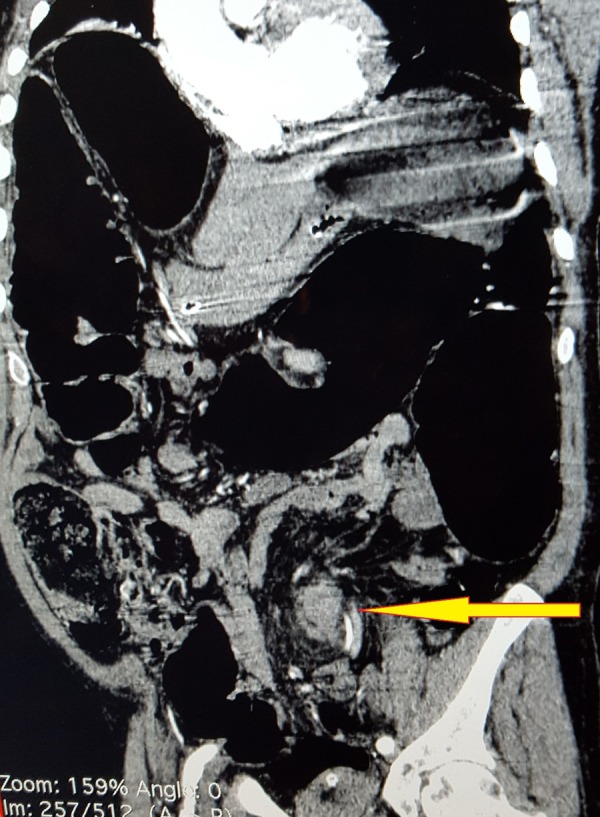
CT scan abdomen demonstrating whirl sign indicative of sigmoid volvulus.
A caecal volvulus was not appreciated on this scan.
Differential diagnosis
Diagnosis was large bowel obstruction secondary to a tumour.
Treatment
After a period of resuscitation, the patient was taken for emergency exploratory laparotomy. Findings include markedly dilated large bowel with a sigmoid volvulus and caecal volvulus. The sigmoid colon was twisted in a clockwise manner and the caecum was twisted in an anticlockwise manner, figures 8 and 9. A long and redundant sigmoid colon was noted with an associated long mesentry. Figure 10 Scattered diverticulae were seen throughout the large bowel with no masses or additional pathology noted. Although the bowel was dilated, there were no serosal tears appreciated and the large bowel appeared viable. The small bowel was collapsed and there were no gross abnormalities noted.
Figure 8.
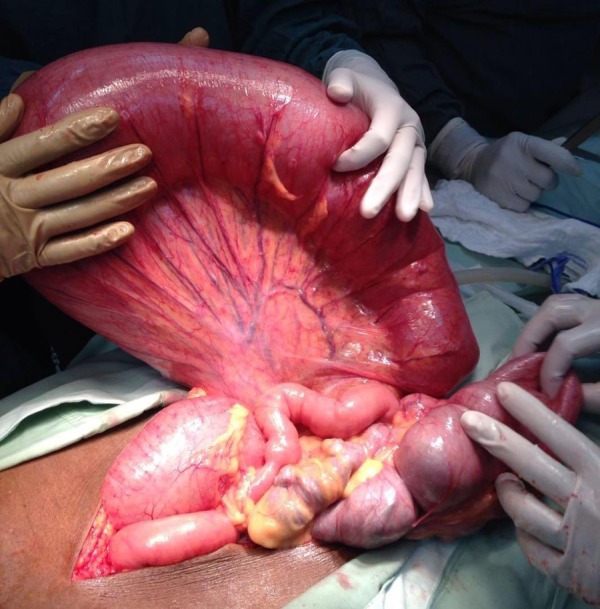
Intraoperative photograph showing sigmoid volvulus.
Figure 9.
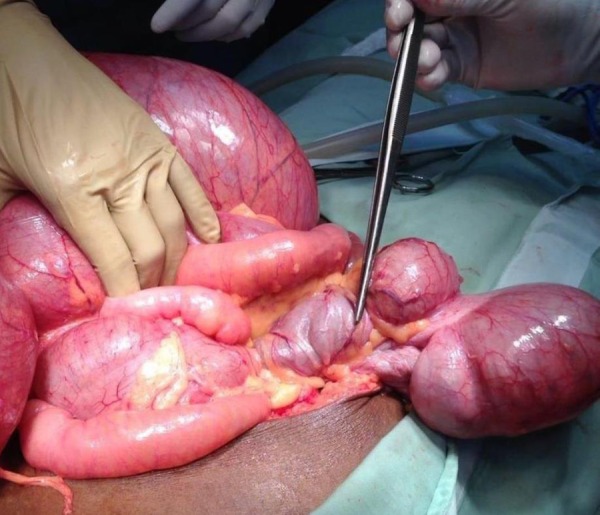
Intraoperative photograph demonstrating the point of twisting for the caecal volvulus.
Figure 10.

Colectomy specimen.
A subtotal colectomy was performed with a side-to-side ileorectal stapled anastomosis.
Outcome and follow-up
The postoperative period was uneventful and the patient was discharged 7 days postoperation. He represented to our hospital with symptoms of intestinal obstruction and on day 2 of admission, it was noted that there was a foul smelling discharge on the inferior aspect of the laparotomy scar with associated peritonism on abdominal examination. An enterocutaneous fistula was suspected and the decision for definitive surgical management was made. On operation he was found to have a breakdown of the anastomosis and extensive adhesions. An end ileostomy was fashioned after extensive adhesiolysis and through abdominal washout.
Discussion
Colonic volvulus is an axial twist of a portion of the colon along its mesentry. The word volvulus is derived from the Latin term volvere which means to twist. This twisting will result in either a complete or partial obstruction of the bowel with associated arterial and venous compromise. As a result, quick and accurate diagnosis is required to expedite treatment for this potentially fatal condition.
Volvulus itself is an unusual cause of intestinal obstruction accounting for ∼5% of cases of gastrointestinal obstruction and 10–15% of large bowel obstruction.1 The most common locations for colonic volvulus are the sigmoid colon (75%), caecum (15%), transverse colon (3%) and splenic flexure (2%).1–3
Having a synchronous volvulus of multiple portions of the bowel is an exceedingly rare occurrence. To the best of our knowledge, our case is the third case in the English literature reporting simultaneous volvulus of the sigmoid colon and the caecum and the fourth case worldwide.4–6 Of note is that synchronous twisting or multiple twisting of the gastrointestinal tract have been reported earlier. Recently, Islam et al7 reported simultaneous torsion of both the splenic flexure and caecum, the only reported entity in the English literature to date. Similarly, Chittal et al8 reported a case of gallbladder and sigmoid colon volvulus. Lianos et al2 reported a case of volvulus of the sigmoid and transverse colon. In addition, Elsharif et al3 reported a case of triple volvulus involving the stomach, caecum and sigmoid colon in a patient with partial situs inversus.
The usual patient who presents with volvulus is described as an elderly, institutionalised individual with a history of chronic constipation and often on psychotropic medication. Other possible associations that have been cited include previous abdominal surgery with subsequent adhesional bands, laxative use and diuretics.9–12 In a younger patient group, volvulus is associated with disorders of abnormal colonic motility or causes of megacolon notably Hirschprung disease and Chaga's disease.13–16
Notably, there has been association with Chilaiditi syndrome and colonic volvulus. Chilaiditi syndrome is defined as a colonic interposition between the liver and the right hemidiaphragm, first described in 1910 by Demitrius Chilaiditi.17 When this sign is associated with symptoms such as abdominal pain, vomiting or respiratory depression, just to name a few, it is called Chilaiditi syndrome. There are reports of Chilaiditi syndrome being associated with volvulus of the caecum, transverse colon and the splenic flexure of the colon.18–21
Many theories have been proposed to explain colonic torsion. Chronic constipation is thought to cause mesenteric stretching which predisposes to torsion. Having a long mesentry as well as surgical division or congenital absence of the gastrocolic, phrenocolic or splenocolic ligaments have all been suggested as possible risk factors.5 9–12 We suspect that having a long mesentery and a redundant sigmoid colon along with the history of chronic constipation predisposed our patient to have a double volvulus.
The diagnosis of this condition is usually made at laparotomy despite a thorough history, examination and appropriate radiological investigations.4–7 Simple X-rays may show large bowel obstruction with typical features of sigmoid or caecal volvulus absent as one entity may alter the appearance of the other. Similarly, with CT imaging the diagnosis may be missed due to the rarity of the condition or the mass effect of one volvulus on the other.7 In our case, the diagnosis was missed radiologically; however, on retrospective review, only a sigmoid volvulus could be positively identified on CT imaging.
The treatment of double volvulus depends on the viability of the bowel, the presence of concomitant pathologies and haemodynamic stability of the patient. For necrotic bowel, resection is mandatory with either primary anastomosis or subsequent ostomy formation. For a viable bowel, the treatment is controversial. Examination of the bowel is necessary to rule out coexisting pathologies such as carcinoma or a megacolon. Of note, Chung et al22 stated that the presence of a megacolon is a significant predictor of recurrence. In the presence of a megacolon, the incidence rate of recurrent volvulus can be as high as 82%.23
If the option of resection is chosen, the decision between performing an ostomy versus primary anastomosis must be made. The advantages of performing a primary anastomosis are obvious as there are several drawbacks associated with a colostomy which include:
Increases psychological stress and financial strain on the patient in addition to the associated complications associated with an ostomy;24 25
Restoration of intestinal continuity involves another operation with its associated morbidity and mortality;26
In cases of diverticulitis, up to 1/3 of patients do not have reversal of the ostomy.26
Prior to performing a primary anastomosis, several factors should be considered before it is deemed safe. As summarised in guidelines by the association of Coloproctology of Great Britain and Ireland there are several risk factors associated with increased risk of anastomotic leak. Known preoperative considerations that placed our patient at a greater risk included male gender, age >60 and emergency surgery. There were no identifiable intraoperative considerations that placed our patient at increased risk as the operation time was <4 hours with very minimal contamination while our patient remained haemodynamically stable throughout. The anastomosis was fashioned without tension and there was good vascularity noted.
Our patient had viable bowel and it was decided to perform a subtotal colectomy and ileorectal anastomosis to decrease the risk of recurrence which would mean a second operation in an elderly man with multiple comorbidities. The decision to perform an anastomosis was made due to low intraoperative risk factors for an anastomotic leak and to spare the patient the additional morbidity of having to manage an ostomy in a setting of poor social support. This decision, however, resulted in the complication of an enterocutaneous fistula secondary to anastomotic break down. Definitive surgical management was chosen over conservative management of this enterocutaneous fistula due to the presence of peritonism on examination.
Ultimately, the treatment lies with the managing surgical team after considering of all factors in order to achieve the best outcome for the patient.
Learning points.
Synchronous volvulus of the sigmoid colon and caecum is a rare cause of large bowel obstruction.
Classic radiological appearances of each volvulus may not be appreciated as one may distort the other due to mass effect.
Early surgical intervention is necessary to decrease morbidity and mortality.
Footnotes
Contributors: SI and DH have contributed significantly in drafting, organising, literature review, writing and critical analyses of the case report. VB and DD have contributed in writing and critical analyses of the case report. All authors have approved the final manuscript for publication.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Halabi WJ, Jafari MD, Kang CY et al. Colonic volvulus in the United States: trends, outcomes, and predictors of mortality. Ann Surg 2014;259:293–301. 10.1097/SLA.0b013e31828c88ac [DOI] [PubMed] [Google Scholar]
- 2.Lianos G, Ignatiadou E, Lianou E et al. Simultaneous volvulus of the transverse and sigmoid colon: case report. G Chir 2012;33:324–6. [PubMed] [Google Scholar]
- 3.Elsharif M, Basu I, Phillips D. A case of triple volvulus. Ann R Coll Surg Engl 2012;94:e62–4. 10.1308/003588412X13171221500781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh G, Gupta SK, Gupta S. Simultaneous occurrence of sigmoid and cecal volvulus. Dis Colon Rectum 1985;28:115–16. 10.1007/BF02552660 [DOI] [PubMed] [Google Scholar]
- 5.Moore JH, Cintron JR, Duarte B et al. Synchronous cecal and sigmoid volvulus. Report of a case. Dis Colon Rectum 1992;35:803–5. 10.1007/BF02050333 [DOI] [PubMed] [Google Scholar]
- 6.Berg AK, Perdawood SK. [Synchronous sigmoideum and caecum volvulus]. Ugeskr Laeg 2015;177:V04150346. [PubMed] [Google Scholar]
- 7.Islam S, Hosein D, Harnarayan P et al. Synchronous volvulus of splenic flexure and caecum: a very rare cause of large bowel obstruction. BMJ Case Rep 2016:▪▪▪ 10.1136/bcr-2015-213029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chittal R, Harris D, Patel A et al. An interesting rare case of double volvulus. BMJ Case Reports 2011:▪▪▪ 10.1136/bcr.10.2010.3464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenthal MJ, Marshall CE. Sigmoid volvulus in association with parkinsonism. Report of four cases. J Am Geriatr Soc 1987;35:683 10.1111/j.1532-5415.1987.tb04346.x [DOI] [PubMed] [Google Scholar]
- 10.Mangiante EC, Croce MA, Fabian TC et al. Sigmoid volvulus. A four-decade experience. Am Surg 1989;55:41–4. [PubMed] [Google Scholar]
- 11.Baker DM, Wardrop PJ, Burrell H et al. The management of acute sigmoid volvulus in Nottingham. J R Coll Surg Edinb 1994;39:304. [PubMed] [Google Scholar]
- 12.Oren D, Atamanalp SS, Aydinli B et al. An algorithm for the management of sigmoid colon volvulus and the safety of primary resection: experience with 827 cases. Dis Colon Rectum 2007;50:489 10.1007/s10350-006-0821-x [DOI] [PubMed] [Google Scholar]
- 13.Krupsky S, Halevy A, Orda R. Sigmoid volvulus in adolescence. J Clin Gastroenterol 1987;9:467 10.1097/00004836-198708000-00023 [DOI] [PubMed] [Google Scholar]
- 14.Mellor MF, Drake DG. Colonic volvulus in children: value of barium enema for diagnosis and treatment in 14 children. AJR Am J Roentgenol 1994;162:1157 10.2214/ajr.162.5.8166002 [DOI] [PubMed] [Google Scholar]
- 15.Atamanalp SS, Yildirgan MI, Başoğlu M et al. Sigmoid colon volvulus in children: review of 19 cases. Pediatr Surg Int 2004;20:492 10.1007/s00383-004-1222-7 [DOI] [PubMed] [Google Scholar]
- 16.Ton MN, Ruzal-Shapiro C, Stolar C et al. Recurrent sigmoid volvulus in a sixteen-year-old boy: case report and review of the literature. J Pediatr Surg 2004;39:1434 10.1016/j.jpedsurg.2004.05.021 [DOI] [PubMed] [Google Scholar]
- 17.Chilaiditi D. Zur frage der hepatoptose und ptose intramuscular allgemeinen intramuscular anschluss an drei fälle von temporärer, partieller leberverlagerung. Fortschritte auf dem Gebiete der Röntgenstrahlen 1910;16:173–208. [Google Scholar]
- 18.Plorde JJ, Raker EJ. Transverse colon volvulus and associated Chilaiditi's syndrome: case report and literature review. Am J Gastroenterol 1996;91:2613–16. [PubMed] [Google Scholar]
- 19.Havenstrite KA, Harris JA, Rivera DE. Splenic flexure volvulus in association with Chilaiditi syndrome: report of a case. Am Surg 1999;65:874–6. [PubMed] [Google Scholar]
- 20.Ansari H, Lay J. Chilaiditi syndrome and associated caecal volvulus. ANZ J Surg 2011;81:484–5. 10.1111/j.1445-2197.2011.05758.x [DOI] [PubMed] [Google Scholar]
- 21.Nofuentes C, Mella M, Soliveres E et al. Transverse colon volvulus and Chilaiditi syndrome: an exceptional association. Am Surg 2011;77:E244–5. [PubMed] [Google Scholar]
- 22.Chung YF, EU KW, Nyam DC et al. Minimizing recurrence after sigmoid volvulus. Br J Surg 1999;86:231–3. 10.1046/j.1365-2168.1999.01034.x [DOI] [PubMed] [Google Scholar]
- 23.Morrissey TB, Deitch EA. Recurrence of sigmoid volvulus after surgical intervention. Am Surg 1994;60:329–31. [PubMed] [Google Scholar]
- 24.Devin H, Seetahal S, Dilip D. Acute complicated diverticulitis: evolving management strategies. In: Dawson B, ed.. Diverticular disease and diverticulitis: symptoms, treatment options and long term health outcomes. New York: Nova Biomedical, 2016:67–86. [Google Scholar]
- 25.Dabirian A, Yaghmaei F, Rassouli M et al. Quality of life in ostomy patients: a qualitative study. Patient Prefer Adherence 2010;5:1–5. 10.2147/PPA.S14508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Belmonte C, Klas JV, Perez JJ et al. The Hartmann procedure. First choice or last resort in diverticular disease? Arch Surg 1996;131:612–15. [DOI] [PubMed] [Google Scholar]


