Abstract
Objective
Community-acquired pressure ulcers (PrUs) are a frequent cause of hospitalization of Veterans with spinal cord injury (SCI). The Veterans Health Administration (VHA) recommends that SCI annual evaluations include assessment of PrU risk factors, a thorough skin inspection and sharing of recommendations for PrU prevention strategies. We characterized consistency of preventive skin care during annual evaluations for Veterans with SCI as a first step in identifying strategies to more actively promote PrU prevention care in other healthcare encounters.
Design/setting/participants
Retrospective cross-sectional observational design, including review of electronic medical records for 206 Veterans with SCI admitted to 2 VA SCI centers from January-December, 2011.
Outcome measures
Proportion of applicable skin health elements documented (number of applicable elements/skin health elements documented).
Results
Our sample was primarily white (78%) male (96.1%), and mean age = 61 years. 40% of participants’ were hospitalized for PrU treatment, with a mean of 294 days (median = 345 days) from annual evaluation to the index admission. On average, Veterans received an average of 75.5% (IQR 68-86%) of applicable skin health elements. Documentation of applicable skin health elements was significantly higher during inpatient vs. outpatient annual evaluations (mean elements received = 80.3% and 64.3%, respectively, P > 0.001). No significant differences were observed in documentation of skin health elements by Veterans at high vs. low PrU risk.
Conclusion
Additional PrU preventive care in the VHA outpatient setting may increase identification and detection of PrU risk factors and early PrU damage for Veterans with SCI in the community, allowing for earlier intervention.
Keywords: Pressure ulcers, Veterans, Prevention, Spinal cord injury
Introduction
Persons with spinal cord injury (SCI) are at increased risk for pressure ulcers (PrU) throughout their lifetimes due to decreased mobility, lack of sensation and other physiologic changes.1,2,3,4,5 Reported prevalence rates of PrUs in SCI have ranged from 17 to 33% for those residing in the community.2,5,6 High rates of ulcer recurrence also have been reported, ranging from 31% to 79%.7,8,9 Chen et al. found that although PrU risk was relatively stable during the first 10 years following SCI, PrU prevalence was significantly higher at 10–15 years post-SCI.4 Most persons with SCI will have at least one serious PrU during their lifetimes.10 Of the estimated 12,000 new SCIs each year and 270,000 people currently living with SCI in the United States,11 about 12% are Veterans.12 Total annual Veterans Health Administration (VHA) healthcare costs are $100,935 for Veterans with SCI and PrUs vs. $27,914 for those without PrUs (P < .001).10
Improvements in managing SCI have increased life expectancy of Veterans with SCI,13 but longer lifespans also increase the likelihood of PrU development, making prevention even more important. The mean duration of SCI in Veterans is greater than 20 years, thus, age and the burden of co-morbid illnesses may increase their PrU risk.14 PrU prevention relies on identifying and managing individual risk factors, conducting daily skin inspection, redistributing pressure and shear force, assessing and managing nutritional deficits, and providing ongoing education. Beginning during initial rehabilitation following SCI, persons with SCI (and their caregivers) are taught to inspect (e.g. visually with a mirror or by touch) their skin daily to detect PrUs.15 This is difficult to do, however, because PrUs often develop in areas that are difficult to visualize (e.g. sacrum, ischium, ankles, heels), especially for those with limited mobility.15–18
VHA data confirm that PrU development in patients with SCI primarily occurs in the community, with <1% of Veterans hospitalized at VHA SCI Centers developing hospital-acquired PrUs.13 However, virtually all of the data on PrU prevention comes from institutional settings (acute inpatient and/or long term care). Reducing the incidence and improving treatment of PrUs in community-dwelling Veterans with SCI is an important goal for VHA to address.
VHA has long recognized the importance of prevention in maintaining the health and quality of life of Veterans with SCI by providing lifelong care that is often not available in the private sector. Early detection of secondary complications of SCI and/or comorbidities associated with SCI may decrease morbidity and mortality.
People with SCI require specialized follow-up over their lifetime for maximum health, prevention of complications, and long term management of costs (lifetime costs of care are substantially greater than those of the initial rehabilitation).19 Clinical experience suggests that proactive and preventative strategies are preferable to responding to medical emergencies or problems after they occur.20 However, many private insurance providers as well as CMS (Medicare/Medicaid) do not currently reimburse for annual evaluations in people with SCI in the private sector.21 However, VHA does provide preventive care to Veterans with SCI via an annual Comprehensive Preventive Health Evaluation (or annual evaluation).22 The evidence supporting the annual evaluation elements, including those that address PrU prevention, are primarily based on expert consensus, with some notable exceptions (e.g. colorectal cancer screening). There are no nationally accepted CPGs that comprehensively address the skin health elements to be included in an annual health evaluation as part of PrU prevention in SCI.
The annual evaluation for Veterans with SCI focuses on identifying, addressing and/or preventing secondary complications. Annual evaluations can be conducted on an inpatient or an outpatient setting and can take one or more days to complete. The setting in which an annual evaluation is conducted (e.g. inpatient vs. outpatient) also depends on a variety of factors, including acuity and Veteran preference.22 Veterans living at a significant distance from an SCI center are generally admitted to the hospital or receive assistance with lodging during the annual evaluation, depending on their needs.22
The annual evaluation for Veterans with SCI has a very extensive scope (Fig. 1) and includes many preventive health care elements, some of which are specific to SCI (e.g. PrU prevention and skin management), as well as preventive care routinely recommended to the general Veteran population (e.g. cholesterol screening and colonoscopy). To address the high rates of PrU development and recurrence in SCI, VHA recommends that annual evaluations include a comprehensive assessment of PrU risk factors, a review of prevention strategies, a thorough skin inspection, and sharing recommendations for PrU prevention with the Veteran.23
Figure 1.
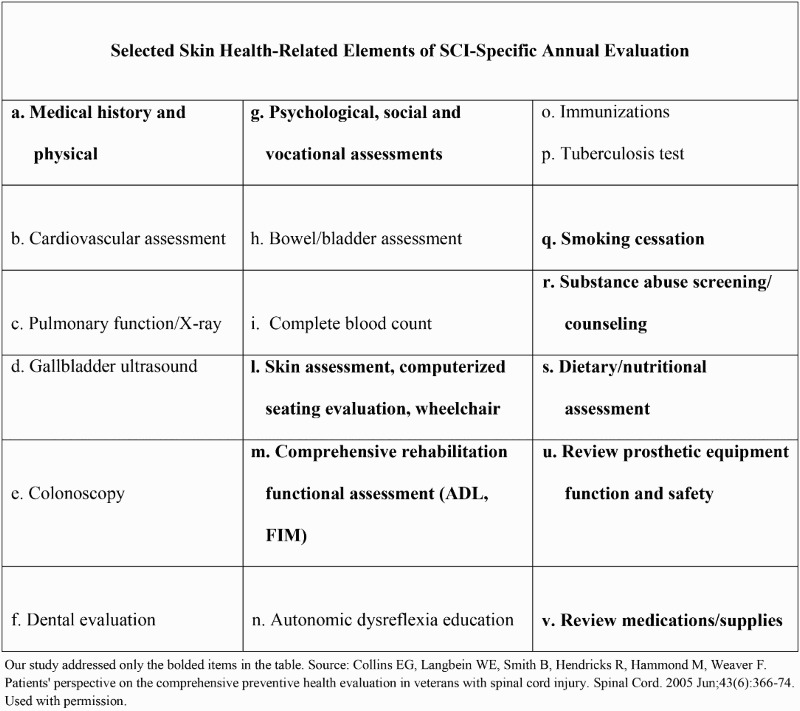
Selected skin health-related elements of SCI-specific annual evaluation.
We focused on annual evaluation components related to promoting skin health using the first edition of the SCI PrU clinical practice guideline (CPG) as the basis for skin health assessment elements.15 The objective of this study was to characterize the consistency of documentation of receipt of skin health assessment elements during annual evaluations as an initial step in addressing prevention of community acquired PrUs among Veterans with SCI. Our research questions included: (1) How many of the PrU CPG recommended skin health elements are documented during annual evaluations; and (2) Was there a difference in skin health elements documented by annual evaluation setting (inpatient vs. outpatient) and by PrU risk?
Methods
The study used a retrospective, cross-sectional observational design. In brief, we defined the skin health elements to include in the study from SCI PrU CPG15 and we presented these skin health elements to a focus group of 6 SCI clinician stakeholders to develop consensus for determining rules related to medical record documentation which would indicate participant receipt of skin health elements. Next, we identified a potential sample and applied the exclusion criteria. We retrospectively reviewed medical records of the sample of participants applying the skin health element documentation rules for individual participants. Finally, we analyzed the data, accounting for individual applicability in analyses.
We obtained a list of all Veterans admitted (n=588) at two of the largest VHA SCI Centers from January 1 – December 31, 2011. For those with multiple admissions, only the first admission (“index admission”) during the study period was retained (n= 386). Electronic medical records were then reviewed retrospectively to identify whether the Veteran received an annual evaluation at a participating SCI center in the 14 months prior to the index admission date. The 14 month window was used to capture annual evaluations done prior to the index admission.
Admissions for the purpose of receiving an annual evaluation were excluded from the sample. In addition, a total of 180 records were excluded for the following reasons: the annual evaluation was conducted >14 months prior to the index admission (n = 58); new SCI (n = 37); first admission ever at the participating VHA SCI Center (n = 23), no record of previous annual evaluation found (n = 17) and those at extremely low PrU risk (American Spinal Injury Association [ASIA] D, n = 45). Our final sample included 206 unique Veterans who were admitted during the study period for any reason except for an annual evaluation, and who received an annual evaluation within 14 months prior to the admission.
Medical record data
Electronic medical records were reviewed to obtain demographic, patient, SCI, and medical information and documentation of skin health elements assessed or received during the annual evaluation.
Patient characteristics included: age, sex, race/ethnicity, marital status, education, employment status and smoking history. SCI characteristics included level and completeness of injury. We also examined overall illness burden using the medical comorbidities on the Charlson index24,25 (e.g. diabetes, chronic obstructive pulmonary disease, tumor, renal disease, peripheral vascular disease, congestive heart failure, myocardial infarction, liver disease, dementia, ulcer, advanced liver disease). In addition we collected data on the setting in which the skin health assessment was completed (inpatient vs. outpatient) and PrU history, and PrU characteristics (if present at the time of the skin health assessment). Previous literature has shown that one of the strongest predictors of future skin breakdown is a previous PrU(s).26,27 Veterans with documentation of an existing PrU during the annual evaluation or history of a PrU within the prior 12 months were classified as “higher” risk in analyses, all others were considered “lower” risk.
Skin health elements
Based on the 2000 SCI PrU CPG, we identified 32 potential skin health elements related to PrU prevention.15 We worked with SCI clinicians at the study sites (n=6) to define for each skin health element: to whom it was applicable and how to determine whether it had been assessed and/or received by participant. Not all skin health elements were applicable to all participants. For example, “documentation of skin integrity” was applicable to all participants, however, only those with a current PrU would have received a “PrU wound assessment” and only those with a stage III/IV PrU might have received a “consultation from a wound care nurse”. Thus the primary outcome is the proportion of applicable skin health elements documented for each participant (i.e. the number of skin health elements documented divided by the number of applicable skin health elements documented for each specific participant).
Each of the 32 skin health elements was reviewed to determine whether it was applicable and/or received. The definition and an example of how each skin health element was defined are presented in Table 1. In addition to reviewing annual evaluation specific electronic progress notes, we also examined History & Physical and admission notes, consults, and/or other progress notes by all SCI providers documented in the electronic medical record during the annual evaluation timeframe. In defining whether a skin health element was assessed during the annual evaluation, explicit documentation of the provider's assessment or action(s) and/or a referral for specialty care in the form of a “consult” was considered the “gold standard.” However, assessment or receipt of many skin health elements was less easily ascertained. We worked with SCI clinicians to create standard definitions and proxy measures for documentation of receipt of skin health elements. For example, documentation of receipt of nutritional assessment was determined by any documentation of nutritional status during the annual evaluation. As there is no mandate for specific documentation of skin health elements during annual evaluations, we accepted provider documentation such as: “denies problems with appetite” in addition to the formal consultations ordered and completed by a registered dietician.
Table 1.
Operationalizing the dependent variables
| Guideline or VA Handbook recommendation | Operationalizing the skin assessment elements | “Gold standard” | Accepted (direct quote from medical record note) |
|---|---|---|---|
| 1. Assessment components | |||
| Describe in detail an existing pressure ulcer: anatomical location and general appearance, size (length, width, depth, and wound area), stage, exudate/ odor, necrosis, undermining, sinus tracts, infection, healing, wound margins/ surrounding tissue. | Assessment of skin integrity | Full body skin assessment documented | “Denies problems with skin” |
| Assessment with measurements for existing ulcers | Assessment of PrUs with measurements | “2 stage III ischial wounds and a stage II left heel wound” | |
| Monitor and assess the pressure ulcer on a consistent, ongoing basis to determine the adequacy of the plan of care. | Documentation of a treatment plan for existing ulcers | Detailed description of PrU treatment plan | “had flap surgery” |
| 2. Inter-disciplinary/specialist consultations for existing PrUs | |||
| An Interprofessional Pressure Ulcer Committee is established and sustained to develop, implement, monitor, and evaluate the Pressure Ulcer Prevention Program; A certified Wound Care Specialist (registered nurse, physician, physical therapist, occupational therapist, physician assistant, or podiatrist) is a member of the Interprofessional Pressure Ulcer Committee; | Consultation made to a wound care specialist, if warranted | Documentation of assessment and plan completed by wound care specialist | “osteomyelitis found” |
| Consultation made to a Podiatrist, if warranted | Documentation of assessment and plan completed by Podiatry | “Refused to follow with ID or Podiatry” | |
| Refer appropriate individuals with complex, deep stage III pressure ulcers (i.e., undermining, tracts) or stage IV pressure ulcers for surgical evaluation. | Consultation made to a plastic surgeon, if warranted | Documentation of assessment and plan by plastic surgeon | “not a good candidate for further surgery” |
| 3. Nutritional assessment and treatment | |||
| Assess nutritional status of all SCI individuals on admission and as needed, based on medical status | Nutritional evaluation or consultation completed | Documentation of assessment and plan completed by Clinical Dietician | “appetite: fair” |
| Implement aggressive nutritional support measures if dietary intake is inadequate or if an individual is nutritionally compromised. | If a nutritional deficit existed, was there an intervention? | Nutritional supplementation ordered | “already receiving Ensure via peg 1-3x a day” |
| 4. Review supplies/medications | |||
| Cleanse pressure ulcers at each dressing change. | Were relevant supplies reviewed/ renewed, if necessary? | Provider discussed with patient/ caregiver dressing changes and ordered supplies | “none needed” |
| Describe medications that can increase PrU risk or complicate management of existing PrUs. | Were relevant medications reviewed/ renewed, if necessary? | Provider and patient reconciled medications, refilled those in need | “resides in nursing home” |
| 5. Assess equipment | |||
| Poor posture, long periods spent on bowel or shower chairs and inadequate offloading from a wheelchair cushion are frequent causes of pressure ulcers. | Assessment of bathroom equipment | PT evaluated shower chair and commode brought to clinic | “pt ambulates without devices” |
| Pressure mapping, seating assessment, and equipment evaluation are vital components of a comprehensive prevention program. | Assessment of transfer equipment | Formal PT evaluation completed of patient's sliding board and lift system | “caregiver uses lift” |
| Assessment ability to change and control body position. | Assessment of patient ability to transfer | Patient's ability to safely transfer was assessed | “dependent in all ADLs” |
| Use pressure-reducing bed support surfaces for individuals who are at risk for or who have pressure ulcers. | Mattress evaluation | Mattress surface quality evaluated | “NH resident” |
| 6. Wheelchair evaluation | |||
| Prescribe wheelchairs and seating systems according to individualized anthropometric, ergonomic, and functional principles. | Wheelchair evaluation | Individualized PT evaluation of wheelchair functioning | “Has a manual wheelchair” |
| Use appropriate wheelchair cushions with all individuals with SCI. | Wheelchair cushion evaluation | Wheelchair cushion evaluated by PT for proper placement and support | “Uses wheelchair but can walk without any aid” |
| Inspect and maintain all wheelchair cushions at regularly scheduled intervals. | Wheelchair pressure mapping evaluation | Patient performed pressure mapping and made recommendations for support surface | “Patient didn't bring chair” |
| 7. Functional assessment | |||
| Assess function whenever a Veteran returns home, or if there is a significant deterioration in the Veteran's functional status, especially mobility. | Functional assessment performed | KT, OT, or PT performed a functional assessment and provided a treatment recommendation or plan | “Followed by KT” |
| 8. Patient education | |||
| Prescribe a power weight-shifting wheelchair system for individuals who are unable to independently perform an effective weight shift. | Counseling on importance of weight shifts | Patient was educated on importance of shifting weight while sitting in wheelchair to prevent skin breakdown | “The pressure ulcer prevention protocol was not needed- patient is not at risk” |
| Use cushions and positioning aids to relieve pressure on pressure ulcers or vulnerable skin areas by elevating them away from the support surface. | Counseling on importance of pressure relief | Patient instructed to perform pressure reliefs every 15 minutes when sitting in wheelchair | “Reminded to avoid pressure on the open area” |
| Develop, display, and use an individualized positioning regimen and repositioning schedule. | Counseling on importance of turning | Education documented on the importance of a turning schedule | “Pt refused to be turned q 2” |
| Teach Veterans and/or designated family members, surrogates, or authorized decision makers how to perform regular (daily) skin inspection…identify and remove the cause of early breakdown…until healed. | Education on what to do if new breakdown or skin worsening | Patient was instructed to call the SCI clinic immediately with any skin breakdown, redness, or worsening appearance of ulcer. | “check the skin daily for any redness” |
| 9. Assess PrU risk factors and co-morbid conditions | |||
| Assess demographic, physical/medical, and psychosocial risk factors associated with pressure ulcer prevention. | Assessment of co-morbid conditions | Co-morbid conditions and patient specific risk factors assessed and addressed | (required—Problem List) |
| Factors that increase risk for development of pressure ulcers: incontinence-bowel and/or bladder; excessive perspiration; and abnormal fluid accumulation (e.g. edema) | Screening for bowel incontinence | Provider and patient discussed bowel care management and addressed any voiding problems | “has bowel care M,W, F” |
| Screening for bladder incontinence | Provider and patient discussed bladder management and addressed any voiding problems | “foley catheter in place” | |
| Screening for excessive sweating or moisture | Sweating and/or moisture issues discussed between patient and provider | “On propantheline” | |
| 10. Assess psycho-social risk factors | |||
| Identify the potential psychosocial impacts of pressure ulcers and immobility and provide referral for therapeutic interventions based upon the individual's characteristics and circumstances. | Psychological assessment performed | Patient received an evaluation by psychiatry with treatment recommendations, if warranted | “History of psychotic disorder” |
| Cognitive assessment performed | Assessment of cognitive status done by provider | “Pt has dementia” | |
| If risk level changes, revise prevention plan to be consistent with the Veteran's current condition. | Assessment of availability and involvement of caregivers or support system | Assessment done on patients ability to function independently at home and support system evaluated | “Maximum resources are in place” |
| If warranted, address issues with the availability and involvement of caregivers or support system | Caregivers trained by staff on how and when to perform patient's ADLs | “Will resume home health services after discharge” | |
| Assessment of social or vocational status | Discussion with patient the need for psychosocial or vocational intervention | “works pretty much full time” | |
| Screened for substance abuse issues | Screened for use of cigarettes/tobacco, alcohol, or illegal substances | “known alcoholic” | |
If no information was present, the skin health element was coded as not having been done.
Statistical analysis
Demographic, patient, SCI, and medical data were analyzed descriptively using frequencies and proportions for categorical variables and mean and standard deviation (SD) for continuous variables. To answer the first research question, we analyzed the data by participant and by skin health element. Receipt of skin health elements were described by frequencies and percent across elements and then percentage of applicable skin health elements received using means and SD by participant. To address the second research question, chi-Square analyses were used to determine whether annual evaluation setting (inpatient vs. outpatient) influenced the receipt of each individual skin health element (when applicable) and Student's t-Test used to determine the effect of annual evaluation setting on the overall mean percentage of skin health elements documented. The same analyses were conducted comparing those at higher risk of PrU development to those who were at lower risk in terms of receipt of each individual skin health element (when applicable) and to determine the effect of PrU risk on overall mean percentage of skin health elements documented. To address the problem of multiple comparisons, we applied a Bonferroni correction. This brought the alpha level required for significance to P=0.001.
All analyses were conducted using SAS 9.3 (SAS Institute Inc., Cary, NC).
Results
Forty percent of the participants’ index admission visits were for PrU treatment. The mean time from annual evaluation to the index admission was 294 days (median = 345 days).
Participants were primarily white (78%) and male (96.1%), with a mean age of 60 years (SD=11.4) (Table 2). About half had tetraplegia (53.4%), ASIA A (44.7%) and an injury duration >20 years (51.5%). Approximately a third (27.2%) of participants were current smokers. The most common comorbidities were diabetes (27.2%), COPD (12.6%) and cancer (6.8%). Half (50.6%) of the participants had a previous history of skin breakdown or actual breakdown at the time of evaluation.
Table 2.
Demographics and clinical characteristics, N=206
| Frequency (%) | |
|---|---|
| Demographic Characteristics | |
| Sex | |
| Female | 8 (3.9) |
| Male | 198 (96.1) |
| Age, mean(sd) | 60.2 (11.4) |
| <50 | 31 (15.0) |
| 50-64 | 114 (55.3) |
| 65+ | 61 (29.6) |
| Race/ethnicity | |
| White | 161 (78.2) |
| Black | 24 (11.7) |
| Other | 12 (5.8) |
| Unknown | 9 (4.4) |
| Marital status | |
| Not married | 106 (51.5) |
| Married | 77 (37.4) |
| Unknown | 23 (11.2) |
| Education | |
| High school or less | 70 (34.0) |
| Any college | 51 (24.8) |
| Other | 11 (5.3) |
| Unknown | 74 (35.9) |
| Employment status | |
| Currently working | 13 (6.3) |
| Not currently working | 132 (64.1) |
| Unknown | 61 (29.6) |
| SCI Characteristics | |
| Level of injury | |
| Tetraplegia | 110 (53.4) |
| Paraplegia | 80 (38.8) |
| Unknown | 16 (7.8) |
| ASIA score | |
| A | 92 (44.7) |
| B | 32 (15.5) |
| C | 24 (11.7) |
| Unknown | 58 (28.2) |
| Duration (years) | |
| Less than10 | 39 (18.9) |
| 10–19 | 40 (19.4) |
| 20 or more | 106 (51.5) |
| Unknown | 21 (10.2) |
| Charlson score, mean (sd) | 1.8 (1.2) |
| Co-Morbid Conditions | |
| Illness burden | |
| Diabetes | 56 (27.2) |
| Chronic obstructive pulmonary disease | 26 (12.6) |
| Tumor | 14 (6.8) |
| Renal disease | 13 (6.3) |
| Peripheral vascular disease | 12 (5.8) |
| Congestive heart failure | 10 (4.9) |
| Myocardial infarction | 9 (4.4) |
| Liver disease | 3 (1.5) |
| Dementia | 2 (1.0) |
| Ulcer | 2 (1.0) |
| Advanced liver disease | 1 (0.5) |
| Pressure ulcer | |
| At annual evaluation | 78 (37.9) |
| At index admission | 74 (35.9) |
| Smoking status | |
| Former/never | 125 (60.7) |
| Current | 56 (27.2) |
| Unknown | 25 (12.1) |
Documentation of skin health elements
Seventy percent (n= 144) of Veteran participants received their annual evaluations in the inpatient setting and 30% received outpatient annual evaluations. Veterans had an average of 75.5% (inter-quartile range [IQR] 68–86%) of the 32 applicable skin health elements documented. Skin health elements documented for greater than 90% of the Veteran participants included: documentation of skin integrity, PrU measurements, PrU treatment plan, wound care consultations, medication reconciliation, assessment of co-morbid conditions, screening for bowel/bladder incontinence, nutritional evaluation and intervention, cognitive or functional assessments, social support assessment and screened for substance abuse (including smoking) (Table 3). No participant had documentation of all applicable skin health elements. Applicable skin health elements that were documented for less than 10% of the applicable Veteran participants included: mattress evaluation (9.4%), screening for sweating/moisture issues (3.9%) and education on skin breakdown procedures (2.1%).
Table 3.
Receipt of skin health elements by setting and PrU Risk (N=206)
| SH Elements | Total N=206 | Outpatient N=62 | Inpatient N=144 | P-Value | Low Risk of PrU N=73 |
High Risk of PrU N=133 |
P-Value |
|---|---|---|---|---|---|---|---|
| Overall completeness, percent received, mean (sd) | 75.5 (11.7) | 64.3 (9.3) | 80.3 (9.0) | <0.001 | 73.2 (12.8) | 76.8 (10.9) | 0.03 |
| Individual elements | N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Medical: wound related | |||||||
| Documentation of skin integrity1 | 206 (100) | 62 (100) | 144 (100) | - | 73 (100) | 133 (100) | 0.13 |
| Documentation of treatment plan for pressure ulcer | 67 (100) | 16 (100) | 51 (100) | 0.61 | - | 67 (100) | - |
| Consult to wound care specialist# | 64 (98.5) | 13 (100) | 51 (98.1) | 0.61 | - | 64 (98.5) | - |
| Documentation of pressure ulcer measurements | 67 (91.8) | 16 (88.9) | 51 (92.7) | 0.61 | - | 67 (91.8) | - |
| Consult to plastic surgeon2 | 21 (67.7) | 1 (33.3) | 20 (71.4) | 0.18 | - | 21 (67.7) | - |
| Consult to podiatrist3 | 3 (60.0) | 1 (50.0) | 2 (66.7) | 0.71 | - | 3 (60.0) | - |
| Educated on skin breakdown procedures | 4 (2.1) | 2 (3.4) | 2 (1.5) | 0.39 | 1 (1.4) | 3 (2.4) | 0.64 |
| Equipment | |||||||
| Wheelchair evaluation | 158 (82.7) | 44 (80.0) | 114 (83.8) | 0.53 | 52 (78.8) | 106 (84.8) | 0.30 |
| Transfer equipment assessed | 145 (78.8) | 49 (92.5) | 96 (73.3) | 0.004 | 55 (82.1) | 90 (76.9) | 0.41 |
| Bathroom equipment assessed | 133 (70.0) | 39 (68.4) | 94 (70.7) | 0.76 | 44 (64.7) | 89 (73.0) | 0.23 |
| Wheelchair cushion evaluation | 112 (57.1) | 23 (41.1) | 89 (63.6) | 0.004 | 32 (47.1) | 80 (62.5) | 0.04 |
| Pressure mapping evaluation2 | 12 (32.4) | 1 (16.7) | 11 (35.5) | 0.37 | - | 12 (32.4) | - |
| Mattress evaluation | 18 (9.4) | 1 (1.7) | 17 (12.9) | 0.01 | 4 (5.6) | 14 (11.6) | 0.17 |
| Function | |||||||
| Functional assessment | 185 (91.1) | 46 (76.7) | 139 (97.2) | <0.001 | 66 (90.4) | 119 (91.5) | 0.79 |
| Assess ability to safely transfer | 171 (85.9) | 44 (75.9) | 127 (90.1) | 0.009 | 61 (87.1) | 110 (85.3) | 0.72 |
| Counseled on PrU reliefs | 150 (73.5) | 16 (26.7) | 134 (93.1) | <0.001 | 49 (68.1) | 101 (76.5) | 0.19 |
| Counseled on weight shifts | 136 (66.0) | 11 (17.7) | 125 (86.8) | <0.001 | 40 (54.8) | 96 (72.2) | 0.01 |
| Counseled on turning | 132 (64.4) | 6 (9.8) | 126 (87.5) | <0.001 | 40 (55.6) | 92 (69.2) | 0.05 |
| Psychosocial | |||||||
| Cognitive assessment* | 203 (99.0) | 61 (98.4) | 142 (99.3) | 0.54 | 72 (100) | 131 (98.5) | 0.30 |
| Support system assessed | 203 (98.5) | 60 (96.8) | 143 (99.3) | 0.16 | 71 (97.3) | 132 (99.2) | 0.26 |
| Screened for substance abuse (smoking, alcohol or drug use) | 192 (94.1) | 56 (90.3) | 136 (95.8) | 0.13 | 64 (90.1) | 128 (96.2) | 0.08 |
| Psychosocial assessment | 171 (89.1) | 39 (75.0) | 132 (94.3) | <0.001 | 61 (89.7) | 110 (88.7) | 0.83 |
| Support system addressed | 21 (87.5) | 5 (100) | 16 (84.2) | 0.34 | 5 (83.3) | 16 (88.9) | 0.72 |
| Social/vocational assessment | 151 (74.4) | 26 (41.9) | 125 (88.7) | <0.001 | 50 (71.4) | 101 (75.9) | 0.48 |
| Medical: non-wound related | |||||||
| Medication reconciliation* | 198 (99.5) | 61 (100) | 137 (99.3) | 0.51 | 71 (100) | 127 (99.2) | 0.46 |
| Co-morbid conditions reviewed* | 205 (99.5) | 61 (98.4) | 144 (100) | 0.13 | 72 (98.6) | 133 (100) | 0.18 |
| Screened for bowel incontinence | 203 (98.5) | 60 (96.8) | 143 (99.3) | 0.16 | 73 (100) | 130 (97.7) | 0.20 |
| Screened for bladder incontinence | 201 (98.0) | 59 (95.2) | 142 (99.3) | 0.05 | 73 (100) | 128 (97.0) | 0.13 |
| Nutritional intervention | 80 (95.2) | 19 (90.5) | 61 (96.8) | 0.24 | 20 (100) | 60 (93.8) | 0.25 |
| Nutritional consult | 186 (94.4) | 49 (87.5) | 137 (97.2) | 0.008 | 69 (98.6) | 117 (92.1) | 0.06 |
| Supplies reviewed and renewed1 | 115 (60.5) | 23 (37.7) | 92 (71.3) | <0.001 | 44 (62.9) | 71 (59.2) | 0.62 |
| Screen sweating/ moisture issues | 8 (3.9) | 3 (4.8) | 5 (3.5) | 0.64 | 3 (4.1) | 5 (3.8) | 0.90 |
1 Routinely addressed for all inpatients, regardless of reason for admission.
2 Eligibility for these SH elements excluded those with stage I/II wounds.
3 Eligibility for this SH element was limited to those with foot ulcers.
* Refers to items that are included on an inpatient nursing template that are done for all inpatients, not just those receiving annual evaluations.
# Limited to those patients with existing stage III/IV PrUs. Patients with stage I/II PrUs would not be routinely seen by a wound care nurse or plastic surgeon.
Bolded items remain significant after Bonferroni correction applied.
Skin health element documentation consistency by setting
Documentation of skin health elements during inpatient annual evaluations was consistently more complete than those in conducted in the outpatient setting (mean applicable skin health elements received = 80.3% and 64.3%, respectively, P > 0.001). Outpatient annual evaluations were less likely to include documentation of consultations with specialists, including functional assessment (76.7% vs. 97.2%); psychosocial assessment (75% vs. 94.3%); social/vocational assessment (41.9% vs. 88.7%); review of supplies (37.7% vs. 71.3%); and counseling on PrU reliefs (26.7% vs. 93.1%), weight shifts (11.7 vs. 86.8%) and turning: (9.8% vs. 87.5%) (P < 0.001 for all).
Outcomes of skin health element documentation by PrU risk group
As shown in Table 3, none of the skin health elements documented were significantly different by PrU risk group.
Discussion
In this sample of 206 Veterans with SCI, documentation of skin health elements as related to PrU preventive care during annual evaluations was relatively high, despite the fact that there are no national VHA performance measures mandating this type of care. Even with relatively high documentation of skin health elements, variability existed in documentation of skin health elements according to setting of the annual evaluation. Veterans with annual evaluations conducted in the outpatient setting had fewer applicable skin health elements documented overall. Although the percentage of applicable skin health elements documented was significantly higher when conducted in the inpatient setting, in no case was all applicable skin health elements documented. Somewhat surprisingly, rates of some important skin health elements that are relatively easy to do were unacceptably low (e.g. wheelchair assessment was done for only 66% of participants).
As shown in Table 3, no significant differences in documentation of skin health elements by high (history of a prior PrU but no current PrU) vs. low PrU risk (no history of a prior PrU and no current PrU) were observed. This underscores the ongoing challenge of how best to focus prevention efforts for both patients and providers.
Medical record documentation is considered a cornerstone of the quality of patient care.28 Accurate documentation in medical records enables continuity of care by detailing clinical assessment(s), treatment(s) and care planning. Documentation also facilitates communication between clinical team members and provides written evidence that can be used to protect the legal interests of the hospital and/or health care provider(s).
Recommendations in the SCI PrU CPG are primarily based on expert consensus, but no guidance is provided regarding their relative importance (i.e. recommendations are not rank-ordered). Some items are directly related to PrU prevention, while others are more indirectly related (e.g. impaired cognitive status may affect an individual's ability to manage their skin). Our analyses treated all items equally, reflecting the state of the science with respect to PrUs generally, not just in SCI.
Focusing on documentation of provision of skin health elements during annual evaluations in SCI allowed assessment of documentation of current annual evaluation practices related to PrU prevention. Our findings suggest that there may be room for improvement in documentation of skin health elements in both the inpatient and especially in outpatient settings. In general, VHA recommends that SCI annual evaluations be conducted in the inpatient setting. However, our data indicate that about a third of annual evaluations are conducted in the outpatient setting. Thus, improving documentation of skin health elements during outpatient annual evaluations could be desirable as well. This is important because most PrUs among Veterans with SCI are community-acquired.13 Any improvement in documentation of skin health elements that stimulates additional PrU preventive care in the outpatient setting has the potential to increase identification and detection of PrU risk factors and early PrU damage in the community environment, allowing for earlier intervention.
During inpatient annual evaluations, some of the skin health elements (i.e. PrU risk assessment, cognitive assessment) are routinely provided as part of the general admission assessment conducted for all patients and are documented using a standard template. Use of a standard template or checklist to assess skin health elements during annual evaluations may improve the documentation of other skin health elements and has the potential to increase assessment of skin health elements. A number of the skin health elements we assessed (e.g. pressure mapping, mattress evaluations, and moisture issues/sweating) are not included in computerized annual evaluation templates at either of the study sites.
Protocols and checklists have been shown to improve patient safety through standardization and communication.23,29 Standardization of practice to improve quality outcomes is a valuable tool to achieve the shared vision for patients and their health care providers.30,31 Standardized approaches have the potential to improve consistency of preventive care, especially in the face of the myriad of mechanical, metabolic, nutritional, behavioral and environmental factors associated with PrUs in SCI. Others have shown use of checklists or standardized approaches can improve care delivery. For example, a 2004 study of 108 hospital intensive care units that implemented a standardized checklist decreased infection rates by 66%.32
As ways to improve PrU prevention in the outpatient setting for Veterans with SCI are examined, there are three sets of players: (1) SCI providers; (2) patients; and (3) caregivers. Many QUERI/QI interventions focus first on modifying provider care delivery behaviors suspected to be influencing patient outcomes, with the long-term goal of improving patient outcomes. By this standard, we identified opportunities to improve the consistency and documentation of skin health elements as part of PrU preventive care during annual evaluations.
The Chronic Care Model (CCM) suggests that health systems must adopt proactive strategies to ensure that guideline recommended care, especially those promoting preventive care, is provided at all health care encounters.33 The CCM emphasizes improvement in patient self-management and the healthcare delivery system to optimize outcomes for those with chronic health conditions.34,35 Improving management of chronic conditions requires health systems to actively implement strategies for embedding active promotion of preventive care into all encounters. This study provides baseline information on preventive care documentation from one provider-patient encounter, the VHA annual evaluation as a first step in identifying strategies for actively promoting PrU prevention care in other provider-patient encounters. The CCM has developed strategies to assist providers in implementing changes to improve care delivery, including flow sheets, visit templates, checklists, reminder tools, and technology to support clinical decision-making.36 Although decision aids are recommended to support continuity of care for those with chronic conditions, to date, checklist use has been primarily focused on relatively short term problems in acute care (e.g. catheter-related blood stream infections in intensive care units).32,37
PrUs in SCI are widely accepted as a complex and multi-factorial problem. Future research should assess whether standardized templates or checklists result in improved documentation, provision of more preventive care and/or improved PrU outcomes. Improving the consistency of documentation of skin health elements of PrU preventative care at the time of annual evaluation, even by a small amount, may be worthwhile when considering the immense cost (>$100,000 annual) per Veteran with SCI and a PrU(s).
Limitations
A major limitation of this study is that it relies on medical record documentation of the skin health elements as evidence of PrU preventive care provided rather than direct observation. We recognize that documentation does not always mean the skin health element was provided.
Although the two participating sites are among the largest VHA SCI centers, the sample size is small and our results may not be generalizable to the other VHA SCI centers. Our results may not apply to the civilian SCI population as comprehensive annual evaluations (like those routinely provided in VHA) are uncommon with SCI, primarily due to lack of reimbursement.
However, the methodology (defining the skin health elements as derived from CPG, developing consensus for determining rules related to documentation indicating receipt of elements with clinician stakeholders, applying the rules to a sample of participants within a given time period, determining applicability for the elements, and accounting for applicability in analyses) and use of such an approach for assessing skin health elements in all provider-patient encounters may be useful outside of the VHA for those interested in this area and those working with civilians with SCI.
We did not observe any significant differences in skin health elements documented by PrU risk group, which may reflect a lack of statistical power.
Veterans with SCI are free to accept or reject provider recommendations of individual skin health elements. Using medical record documentation, it is not possible to know whether a particular skin health element was recommended by the provider but rejected by the Veteran.
Although some studies have documented substantial (>54%) dual (VHA /Medicare) health care utilization,38 we were unable to determine if Veterans received skin health element assessments outside of VHA SCI centers.
Conclusion
Despite the high PrU risk of the SCI population, we found that completeness of documentation of skin health elements for PrU prevention provided as part of annual evaluations varied, with those conducted in the outpatient setting showing less complete documentation of skin health elements than those conducted in the inpatient setting. While the rate of skin health element documentation was higher for persons receiving annual evaluations as inpatients, there was room for improvement. It is possible that a standardized template would help improve the consistency of documentation of skin health elements in both settings. Future research should address whether providers believe that some of the skin health elements should be prioritized over others, whether this approach is more effective at preventing PrUs and how to further implement such an approach in the community setting. Future studies should also address costs of including skin health assessment in patient encounters.
PrU prevention is predicated on the fact that a more thorough assessment will identify potentially modifiable risk factors. However, better identification may not, by itself, result in a decreased PrU incidence. Whether the inconsistences we found are the result of uneven documentation or whether a provider-focused intervention to improve provision of skin health elements would just improve documentation remains unclear. Identifying gaps in documentation of PrU preventive care in SCI is a necessary step to begin to address the problem of community-acquired PrUs in SCI.
Acknowledgment
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Funding Statement
This manuscript was supported by the Department of Veterans Affairs, Health Services Research and Development (LIP # 42-136).
Orcid
Marylou Guihan http://orcid.org/0000-0002-9506-1927
Deirdre Murphy http://orcid.org/0000-0002-3750-0661
Thea J. Rogers http://orcid.org/0000-0003-0221-913X
Ramadevi Parachuri http://orcid.org/0000-0002-1155-0281
Michael SAE Richardson http://orcid.org/0000-0001-8642-897X
Kenneth K. Lee http://orcid.org/0000-0002-9378-673X
Barbara M. Bates-Jensen http://orcid.org/0000-0001-8490-4012
Disclaimer statement
Funding This manuscript was supported by the Department of Veterans Affairs, Health Services Research and Development (LIP # 42-136).
References
- 1.Mawson AR, Biundo JJ, Neville P, Linares HA, Winchester Y, Lopez A. Risk factors for early occurring pressure ulcers following spinal cord injury. Am J Phys Med Rehabil 1988;67:123–7. doi: 10.1097/00002060-198806000-00007 [DOI] [PubMed] [Google Scholar]
- 2.Young JS, Burns PE.. Pressure sores and the spinal cord injured, Part I. SCI Digest 1981;3a:9–25. [Google Scholar]
- 3.Young JS, Burns PE.. Pressure sores and the spinal cord injured, Part II. SCI Digest 1991;b:11–48. [Google Scholar]
- 4.Chen D, Apple DF, Hudson MF, Bode R. Medical complications during acute rehabilitation following spinal cord injury. Arch Phys Med Rehabil 1999;80(11):1397–401. doi: 10.1016/S0003-9993(99)90250-2 [DOI] [PubMed] [Google Scholar]
- 5.Fuhrer MJ, Garber SL, Rintala DH, Clearman R, Hart K. Pressure ulcers in community-resident persons with spinal cord injury: prevalence and risk factors. Arch Phys Med Rehabil 1993;74(11):1172–7. [PubMed] [Google Scholar]
- 6.Carlson CE, King RB, Kirk PM, Temple R, Heinemann A. Incidence and correlates of pressure ulcer development after spinal cord injury. J Rehabil Nurs Res 1992;1:34–40. [Google Scholar]
- 7.Niazi ZB, Salzberg CA, Byrne DW, Viehbeck M. Recurrence of initial pressure ulcer in persons with spinal cord injuries. Adv Wound Care 1997; 10(3):38–42. [PubMed] [Google Scholar]
- 8.Holmes SA, Rintala D, Garber SL, Friedman JD.. Prevention of recurrent pressure ulcers after myocutaneous flap. J Spinal Cord Med 2002;25(Supplement 1),S23. [Google Scholar]
- 9.Goodman CM, Cohen V, Armenta A, Thornby J, Netscher DT. Evaluation of results and treatment variables for pressure ulcers in 48 veteran spinal cord-injured patients. Ann Plast Surg 1999;42(6):665–72. doi: 10.1097/00000637-199906000-00015 [DOI] [PubMed] [Google Scholar]
- 10.Stroupe KT, Manheim LL, Evans CT, Guihan M, Ho CC, Li K,. et al Cost of treating pressure ulcers for veterans with spinal cord injury. Top Spinal Cord Inj Rehabil 2011;16(4):62–73. doi: 10.1310/sci1604-62 [DOI] [Google Scholar]
- 11.Spinal Cord injury facts and figures at a glance. https://www.nscisc.uab.edu/PublicDocuments/nscisc_home/pdf/Facts%202011%20Feb%20Final.pdf.
- 12.SCI QUERI fact sheet, April 2012. http://www.queri.research.va.gov/about/factsheets/sci_factsheet.pdf.
- 13.2008–2009 VA External Peer Review program (EPRP) data.
- 14.SCI QUERI, Department of Veterans Affairs, Quality Enhancement Research Initiative, Strategic Plan, November 2012.
- 15.Consortium for Spinal Cord Medicine Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med 2001; 24(suppl):S40–S101. [DOI] [PubMed] [Google Scholar]
- 16.Priebe MM, Martin M, Wuermser LA, Castillo T, McFarlin J.. The medical management of pressure ulcers. In: Lin VW, Cardenas DD, Cutter NC, et al., editors. Spinal cord medicine: principles and practice. New York: Demos Medical Publishing, Inc; 2003:567–87. [Google Scholar]
- 17.Vasconez LO, Schneider WJ, Jurkiewicz MJ.. Pressure sores. Curr Probl Surg 1977;14(4):1–62. doi: 10.1016/S0011-3840(77)80007-5 [DOI] [PubMed] [Google Scholar]
- 18.Meehan M. National pressure ulcer prevalence survey. Adv Wound Care 1994;7(3):27–37. [PubMed] [Google Scholar]
- 19.Lammertse D.. Maintaining health long-term with spinal cord injury. Top Spinal Cord Inj Rehabil 2015;6(5):15–17. [Google Scholar]
- 20.Guihan M, Bombardier CH.. Potentially modifiable risk factors among veterans with spinal cord injury hospitalized for severe pressure ulcers: a descriptive study. J Spinal Cord Med 2012;35(4):240–50. doi: 10.1179/2045772312Y.0000000016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Special Interest Group on SCI Model System Innovation Toward a model system of post-rehabilitative health care for individuals with SCI. Washington, DC: National Rehabilitation Hospital: National Capital Spinal Cord Injury Model System (NCSCIMS); 2010. http://www.ncscims.org/SCIModelSystemInnovationReport.pdf. [Google Scholar]
- 22.Collins E, Langbein WE, Smith B, Hendricks R, Hammond M, Weaver F.. Patients’ perspective on the comprehensive preventive health evaluation in veterans with spinal cord injury. Spinal Cord 2005;(43):366–74. doi: 10.1038/sj.sc.3101708 [DOI] [PubMed] [Google Scholar]
- 23.VHA Handbook 1176.01. http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=2365.
- 24.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 25.Deyo R, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992;45(6):613–9. doi: 10.1016/0895-4356(92)90133-8 [DOI] [PubMed] [Google Scholar]
- 26.Schryvers OI, Stranc MF, Nance PW. Surgical treatment of pressure ulcers: 20-year experience. Arch Phys Med Rehabil 2000;81(12):1556–62. doi: 10.1053/apmr.2000.17828 [DOI] [PubMed] [Google Scholar]
- 27.Krause J, Broderick L.. Patterns of recurrent pressure ulcers after spinal cord injury: identification of risk and protective factors 5 or more years after onset. Arch Phys Med Rehabil 2004;85(8):1257–64. doi: 10.1016/j.apmr.2003.08.108 [DOI] [PubMed] [Google Scholar]
- 28.Manchikanti L, Singh V, Pampati V, Boswell MV, Benyamin RM, Hirsch JA.. Description of documentation in the management of chronic spinal pain. Pain Physician 2009;12(4):E 199–224. [PubMed] [Google Scholar]
- 29.Pizzi L, Goldbarb N, Nash D.. Crew resource management and its applications in medicine. In: Agency for Healthcare Research and Quality. Making health care safer: a critical analysis of patient safety practices. Evidence Report/Technology Assessment No. 43 Rockville (MD): AHRQ; 2001. p. 505–13. [Google Scholar]
- 30.Grol R. Between evidence-based practice and total quality management: the implementation of cost-effective care. Intl J Qual Health Care 2000;12(4):297–304. doi: 10.1093/intqhc/12.4.297 [DOI] [PubMed] [Google Scholar]
- 31.Berwick DM. A user's manual for the IOM's “Quality Chasm” report. Health Aff(Millwood) 2002;21(3):80–90. [DOI] [PubMed] [Google Scholar]
- 32.Berenholtz SM, et al. Eliminating catheter-related bloodstream infections in the intensive care unit. Crit Care Med 2004;32(10):2014–20. doi: 10.1097/01.CCM.0000142399.70913.2F [DOI] [PubMed] [Google Scholar]
- 33.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Prac 1998; 1(1):2–4. [PubMed] [Google Scholar]
- 34.Wagner EH, Austin BT, Von Korff M.. Organizing Care for Patients with Chronic Illness. Milbank Q. 1996; 74(4):511–44. doi: 10.2307/3350391 [DOI] [PubMed] [Google Scholar]
- 35.Bodenheimer T, Wagner EH, Grumbach K.. Improving primary care for patients with chronic illness. JAMA 2002; 288(14):1775–9. doi: 10.1001/jama.288.14.1775 [DOI] [PubMed] [Google Scholar]
- 36.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract 1998; 1(1):2–4. [PubMed] [Google Scholar]
- 37.Weiser TG, Haynes AB, Lashoher A, Dziekan G, Boorman DJ, Berry WR, Gawande AA.. Perspectives in quality: designing the WHO Surgical Safety Checklist. Int J Qual Health Care 2010;22(5):365–70. doi: 10.1093/intqhc/mzq039 [DOI] [PubMed] [Google Scholar]
- 38.Banerjea R, Findley PA, Smith B, Findley T, Sambamoorthi U.. Co-occurring medical and mental illness and substance use disorders among veteran clinic users with spinal cord injury patients with complexities. Spinal Cord 2009;47(11):789–95. doi: 10.1038/sc.2009.42 [DOI] [PubMed] [Google Scholar]


