Abstract
Context
Previous research studies have confirmed therapeutic physical and psychological benefits of Tai Chi for both the able-bodied and disabled populations. However, given the limited availability of seated Tai Chi, there have not been any studies to date that have examined the effectiveness of seated Tai Chi in individuals with spinal cord disorder (SCD). We designed a customized seated Tai Chi program to meet the need for improved exercise options for individuals with SCD.
Findings
Twenty-six participants were enrolled in a 12-week seated Tai Chi course consisting of weekly sessions. After each Tai Chi session, patients reported improved visual analog scale (VAS) monitoring pain (P) (3.18 v 2.93; P 1.63E-03), emotional sense of well-being (EWB) (2.61 vs 2.04; P 2.86E-07), mental distraction (MD) (3.13 v 2.29; P 9.36E-08), physical sense of well-being (PWB) (2.84 v 2.25; p 7.38E-08), and sense of spiritual connection (SC) (3.28 v 2.50; P 6.46E-08). In our limited follow-up of 9 participants who completed half of the sessions and the long term surveys after the 12-week course, there were no detectable differences in weekly P, EWB, MD, PWB, and SC before each session.
Conclusion and Clinical Relevance
Individuals with SCD demonstrated benefits in pain, emotional sense of well-being, mental distraction, physical sense of well-being, and sense of spiritual connection immediately after seated Tai Chi exercise sessions in our pilot study. More research in a larger population would be needed to study the long-term impact of seated Tai Chi.
Keywords: Spinal cord injury, Exercise, Tai Chi, Quality of life
Introduction
Tai Chi Chuan, which means “supreme ultimate fist,” originated in China more than 300 years ago.1 It is widely promoted as a form of exercise for people of all ages.2 Long-lasting physiological, psychological, and social benefits are believed to accrue through regular practice of Tai Chi, as it has been shown to be effective in many different aspects including sleep,3–5 balance and coordination,6–9 motor skills and physical function.10 Tai Chi can be also of use in improving pain control, quality of life and mental health,11–13 even in patients with physical disability. Practice of Tai Chi in patients with multiple sclerosis improves not only balance, coordination, but also reports of fatigue and depression.14 A review article suggested that Tai Chi can be beneficial for stroke survivors with respect to balance, quality-of-life, and mental health.15 However, in all of these studies, the subjects participated in standing Tai Chi programs.
While Tai Chi is practiced traditionally in a standing position, the positive effects of Tai Chi on mental state and physical health may be attributed not only to the physical movements but due to mind-body techniques such as “body scan techniques” and “focused breathing.”16 In a routine standing Tai Chi class, participants are allowed to sit down if they become uncomfortable and to remain on a chair to continue their exercise;17; participants with physical limitations are often encouraged to imagine and visualize Tai Chi movements and to perform movements. Despite this, many individuals who are wheelchair-users have not been able to participate in standard Tai Chi classes. This may be due to unavailability of seated Tai Chi classes or lack of knowledge that Tai Chi can be practiced from a seated position.
Given the limited availability of seated Tai Chi, there have not been any studies to date that have examined the impact of seated Tai Chi on individuals with spinal cord disorder (SCD). Here, we designed a customized seated Tai Chi program to meet the need for improved exercise options for individuals with SCD who cannot safely practice Tai Chi in a standing position. The purpose of this project was to evaluate the feasibility of a seated Tai Chi Chih program for individuals with SCD who cannot safely participate in a standing Tai Chi exercise program. The primary objective was to investigate the immediate benefits on feelings of wellness, pain management, fatigue, and mood conferred on an individual with SCD who participates in the seated Tai Chi class. The secondary objective was to investigate the long-term effects of practicing Tai Chi for months after the participant completes a Tai Chi course.
Case report
Participants and setting
This project was reviewed and approved by the Research and Human Subjects Review Committee at our county medical center. This case series was of a prospective, interventional, pre- and post-study design in individuals with SCD who cannot safely practice standing Tai Chi movements. The inclusion criteria were: at least 18 years of age, any individual with SCD with sufficient arm movement to be able to participate in the Tai Chi program, medically stable with no pressure sores, and ability to sign an informed consent and HIPAA privacy documents. Exclusion criteria were: inability to tolerate or medically contraindicated to be sitting for more than 2 hours, no working knowledge of English, and pregnancy since the effect of Tai Chi on pregnancy is unknown.
T'ai Chi Chih course
In this study, we used a form of Tai Chi called T'ai Chi Chih (TCC). It is a westernized version of Tai Chi Chuan, which has been designed for use in the elderly and medically compromised populations. TCC takes much less space than with Tai Chi Chuan. While Tai Chi Chuan needs to be taught in person by an instructor, TCC is easier to learn and can be reviewed with a book or videotape. TCC consists of a standardized series of 20 simple, slow, repetitive, relaxed movements. TCC uses “meditation through movement” while incorporating elements of balance, postural alignment, and concentration. There were 20 movements that were taught during a 12-week course. The class met once a week for 90 minutes. The first 10 minutes were used for signing-in, and there was a 10–15 minute break in the middle of each session. In addition, at the beginning of the Tai Chi course, an educational video of the Tai Chi teacher performing the 20 motions of the TCC were provided to every subject, and the subjects were strongly encouraged to practice the TCC movements at home while watching this educational video. At the completion of the 12-week course, participants were given an option of continuing to attend an on-going seated Tai Chi class.
An 11-point visual analog scale (VAS) on pain (P), emotional sense of well-being (EWB), mental distraction (MD), physical sense of well-being (PWB), and sense of spiritual connection (SC) were completed at the end of each weekly session. They were also asked if they have been practicing Tai Chi at home, and if so how often. The subjects were to complete a set of outcome measures on fatigue, pain, and depression at the beginning and the end of the 12-week course of the seated Tai Chi program. The assessment tools included an intake/follow-up demographics form, the Modified Fatigue Impact Scale (MFIS), the Brief Pain Inventory (short form), and the Beck Depression Inventory–II (BDI–II).
Intake/follow-up demographics
The intake form asked basic demographic questions as well as questions concerning diagnosis, cause of injury or disability, duration of injury or disability, the level of injury, and American Spinal Injury Association Impairment Scale (AIS) classification for participants with spinal cord injury. The follow-up assessment form contained questions concerning demographic variables that may have changed. It also asked subjects to rate their satisfaction with a variety of major lifestyle areas such as access to medical care and transportation.
Modified Fatigue Impact Scale (MFIS)
The MFIS is a 21-item self-report instrument that examines the perceived impact of fatigue in three areas: cognitive functioning, physical functioning and psychosocial functioning. All items are scored so that higher scores indicate a greater impact of fatigue on an individual's activities, and the total scores can range from 0–84.
Brief Pain Inventory (short form) (BPI)
This scale assesses the severity of pain and its impact on daily function. Reliability and validity for different disease groups and various cultures has been established.18 A modified version has been used for individuals with mobility impairments in which pain interference in “walking” has been revised to “mobility” and 3 additional items have been added to the interference scale: “self-care,” “recreational activities,” and “social activities.” The severity scale is summed from 0 to 40 and the interference scale is summed from 0 to 100 with higher scores indicating greater severity and interference, respectively. This scale has been used in individuals with SCD.19–21
Beck Depression Inventory–II (BDI–II)
The BDI is a 21-item self-report instrument widely used to determine depressive symptomatology.22 Each item is rated on a scale of “0 – no symptomatology” to “3 – excessive symptomatology.” Item scores are totaled with a minimum score of zero and a maximum score of 63. Levels of depression are assigned by the following rating system: scores of 5–9 are normal; scores of 10–18 indicate mild to moderate depression; scores of 19–29 signify moderate to severe depression; and scores of 30–63 indicate severe depression. Internal consistency for the BDI ranges from 0.60 to 0.74 with a mean of 0.81.23 It is sensitive to changes produced by psychotherapy.24 The BDI–II was created to be consistent with DSM-IV criteria for depression. It has demonstrated also great retest reliability between 0.73 and 0.96 with an internal consistency of 0.9.25 BDI has been used widely in the assessment of depression in SCD.26–28
Statistical method
Changes in the five visual analog subscales at each session were analyzed using the Wilcoxon Signed-Rank tests using R (2.11.1). To track session effects, changes in the five pre session visual analog subscales (P, EWB, MD, PWB, and SC) between first and last session for the 9 participants who completed more than half of the sessions and their long term surveys (MFIS, BDI–II, BPI) were analyzed using the Wilcoxon Signed-Rank tests. MFIS, BDI–II, BPI of the 9 participants at the initial and last session were also compared using the Wilcoxon Signed-Rank tests.
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Twenty-six subjects were enrolled (Table 1). There were 14 males (54%) and 12 females (46%). Average age was 49.8 ± 13.0 years old. Sixteen subjects were tetraplegic, 6 subjects were paraplegic, and 4 subjects had unknown level of injury. Race/ethnicity was as follows: 12 Caucasians, 2 Hispanics, 4 Asians, 2 African-Americans, and 6 unspecified. Average time since injury was 25.1 ± 18.9 years. Seventeen subjects (65%) were wheelchair-users whereas 3 subjects (12%) ambulated as their primary mode of mobility, and 6 subjects (23%) were unspecified. Nine subjects (35%) were considered to have completed the program since they attended at least 50% (greater than six classes out of 12 weeks) of the Tai Chi class and completed their long-term surveys, and the data from these individuals were analyzed.
Table 1.
Demographics of participants
| Age | Sex | Cause of injury | Level of injury | Para/ tetra/ other | AIS | Primary equipment for mobility | Race/ ethnicity | # of sessions | Reason for drop out |
|---|---|---|---|---|---|---|---|---|---|
| 50*^ | M | Falls | C3 | Tetra | None | Hispanic | 12 | ||
| 19*^ | F | Other | C6-C7 | Tetra | B | Manual and power WC | Caucasian | 12 | |
| 61 | M | Sports | C4-C5 | Tetra | C | Power WC | Caucasian | 1 | Other |
| 46*^ | M | Other | C5-C6 | Tetra | A | Power WC | Caucasian | 12 | |
| 42 | F | Vehicular | Para | Manual WC | Caucasian | 1 | Too Busy | ||
| 43*^ | F | Vehicular | C6-C7 | Tetra | Power WC | Asian | 12 | ||
| 41 | F | Other | GBS | Other | Manual WC | Caucasian | 2 | Distance | |
| 64 | F | Vehicular | C6-C7 | Tetra | Power WC | Caucasian | 3 | Distance | |
| 31 | M | Vehicular | T12-L1 | Para | B | Manual WC | Caucasian | 5 | Distance |
| 66*^ | M | Vehicular | T8 | Para | ? | Manual WC | Caucasian | 12 | |
| 37 | F | Tetra | 4 | Other | |||||
| 42* | F | Para | 8 | Too Busy | |||||
| 51*^ | M | Sports | L3–4 | Para | ? | Manual WC, Cane | Hispanic | 11 | Too Busy |
| 54*^ | F | Vehicular | C5-C6 | Tetra | ? | Power WC | Asian | 8 | Other |
| 56 | F | C-5 | Tetra | 3 | Other | ||||
| 51 | M | Tetra | 1 | Other | |||||
| 73*^ | M | Polio | Other | Manual WC | Asian | 12 | |||
| 65* | F | Arthiritis | Other | None | Asian | 12 | |||
| 61* | F | Epidural Abscess | C5 | Tetra | None | African-American | 12 | ||
| 43* | M | Spina bifida | Para | Manual WC | African-American | 11 | Other | ||
| 63 | M | Tetra | 1 | Too Busy | |||||
| 28 | M | Tetra | 1 | Too Busy | |||||
| 55 | M | Vehicular | C6-C7 | Tetra | A | Power WC | Caucasian | 5 | Too Busy |
| 46 | M | Falls | C6 | Tetra | A | Manual and power WC | Caucasian | 1 | Too Busy |
| 63*^ | F | Polio | Other | C | Power WC | Caucasian | 12 | ||
| 44 | M | Falls | C5-C6 | Tetra | A | Power WC | Caucasian | 2 |
* Denotes 13 participants who completed more than 50% of sessions.
∧ Denotes 9 participants who completed more than 50% of sessions and completed long-term surveys (MFIS, BDI–II, or BPI).
GBS = Guillain-Barré syndrome.
Sixteen subjects (60%) dropped out or did not complete the 12-week program for multiple reasons (Fig. 1). Main reason for incompletion was “busy” in five subjects, followed by transportation difficulties and/or distance from the class (3 subjects). One subject had medical reason. One subject developed radicular pain not associated with practicing Tai Chi, but she was unable to sit long enough to continue. One subject, who ambulates, felt uncomfortable practicing Tai Chi among other subjects majority, the of whom were wheelchair-users. Subjects seemed to drop out within several sessions if they chose to not continue.
Figure 1.
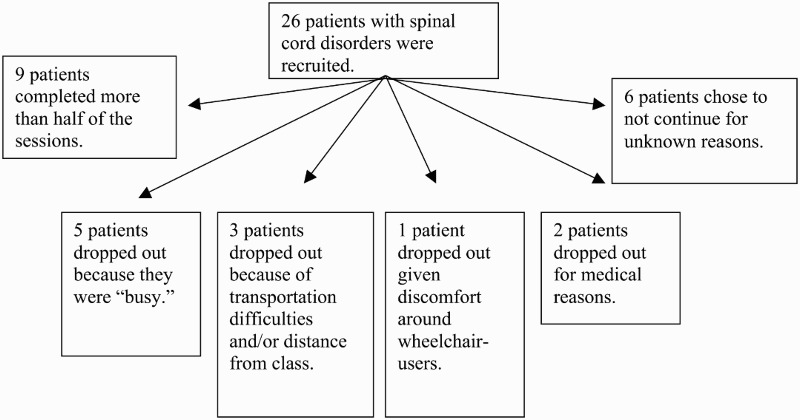
Patient distribution in follow-up.
Patients reported improvement in all five visual analog subscales (P, EWB, MD, PWB, and SC) immediately after the sessions (Table 2). Taking into account data available for all 26 participants, Tai Chi sessions improved VAS P (3.18 v 2.93; P 1.63E-03), EWB (2.61 vs 2.04; P 2.86E-07), MD (3.13 v 2.29; P 9.36E-08), PWB (2.84 v 2.25; P 7.38E-08), and SC (3.28 v 2.50; P 6.46E-08). In our limited follow up of 9 participants who completed half of the sessions and the long-term surveys, there were no detectable differences in the pre session VAS surveys of P, EWB, MD, PWB, and SC between the first and the last sessions (Table 3). There were no detectable changes in the long-term effect surveys of MFIS, BDI–II, BPI between the first and the last sessions (Table 4).
Table 2.
Short term effects of seated Tai Chi
| Pre-session average | Post-session average | Wilcoxon signed rank test | |
|---|---|---|---|
| SP | 3.18 | 2.93 | 1.63E-03 |
| EWB | 2.61 | 2.04 | 2.86E-07 |
| MD | 3.13 | 2.29 | 9.36E-08 |
| PWB | 2.84 | 2.25 | 7.38E-08 |
| SC | 3.28 | 2.50 | 6.46E-08 |
Table 3.
Session effect of seated Tai Chi
| Pre-session on first week | Pre-session on last week | Wilcoxon signed rank test | |
|---|---|---|---|
| SP | 2.33 | 3.00 | 0.63 |
| EWB | 1.78 | 2.56 | 0.22 |
| MD | 1.78 | 3.78 | 0.21 |
| PWB | 3.11 | 2.67 | 0.40 |
| SC | 3.11 | 3.67 | 0.86 |
Table 4.
Long term effects of seated Tai Chi
| Change in outcome measure after more than 6 sessions of Tai Chi | |||
|---|---|---|---|
| Average change | Standard deviation | Wilcoxon signed rank test | |
| Modified Fatigue Impact Scale | 2.00 | 7.57 | 0.50 |
| Brief Pain Inventory | –1.33 | 4.33 | 0.58 |
| Beck Depression Inventory–II | –0.78 | 5.29 | 0.93 |
Discussion
The intended outcome of this project was to prove that seated Tai Chi is well tolerated among the individuals with SCD and that the seated Tai Chi as an exercise program option can help improve quality of life and decrease pain in individuals with SCD. The results of this case series demonstrated that the individuals with SCD who practice seated Tai Chi improved in pain, emotional sense of well-being, mental distraction, physical sense of well-being, and for sense of spiritual connection after these exercise sessions.
The benefits of a regular exercise program in individuals who do not have a disability have been recognized for at least several decades. The substantial physical benefits include, but are not limited to, increased cardiovascular fitness, easier weight control, improved immune function, decreased risk of heart disease, and increased energy. There is also substantial evidence to suggest that significant psychological benefits are obtained as well: decreased dysphoric moods, improved self-esteem, and overall increased Quality of Life (QOL). We hope that seated Tai Chi for an individual with SCD will not only produce the same psychological but also some of the physical benefits as those found in ambulatory persons. For example, several studies have shown that individuals with SCD can show improvements in fitness and that increased fitness has been associated with improved health and function in individuals with SCD. Potential benefits that could specifically improve QOL for individuals with SCD include reduction of secondary impairments such as loss of cardio-respiratory and muscular function, improvements in the ability to perform activities of daily living, and reduction of the increased impairments that come with aging with an SCD. There is an additional benefit that an exercise program may confer on individuals with SCD: by participating in such a program with other persons with SCD, informal peer support and social interactions will probably occur, potentially producing all of the benefits believed to be provided by fostering a sense of community.
Our pilot study could not achieve the follow-up and sample size needed to study the long term effects of seated Tai Chi. We were also more liberal with our inclusion criteria and included individuals with SCDs from a variety of conditions who were both wheelchair users and ambulatory. Our limited follow-up was not able to show an effect of session in most of the variables and also in MFIS, BDI–II, or BPI. This is likely due to the noteworthy dropout rate and the relative short duration of follow-up. In this study, one of the main barriers for completion of the program was transportation. Since the class was held only once a week, some people were unable to participate due to inconvenient time of the class, which is a barrier future studies have to overcome to prevent dropout. Another limitation is that given our study was not blinded, the participants’ self-reported improvement in pain, emotional sense of well-being, mental distraction, physical sense of well-being, and sense of spiritual connection could be secondary to recall bias or the effect of any group setting program that offers social support.
Conclusion
Overall, our pilot showed that seated Tai Chi should be considered as an exercise option for individuals with SCD who cannot participate in standing Tai Chi or other exercises that require them to stand or walk. As an exercise program for individuals with SCD, it is well-tolerated and demonstrated benefits in pain, emotional sense of well-being, mental distraction, physical sense of well-being, and sense of spiritual connection immediately after each session in our small pilot study. Our pilot study was limited by the small sample size and high drop out rate that did not allow us to detect any longer term benefits. More research in a larger population would be needed to study the long-term impact of seated Tai Chi.
Disclaimer statements
Contributors None.
Funding None.
Conflicts of interest All authors declare no conflicts of interests.
Ethics approval None.
References
- 1.Davis B. The Taijiquan classics: an annotated translation. Berkeley, CA: North Atlantic Books; 2004. [Google Scholar]
- 2.Wolf SL, Coogler C, Xu T. Exploring the basis for Tai Chi Chuan as a therapeutic exercise approach. Arch Phys Med Rehabil 1997;78(8):886–92. doi: 10.1016/S0003-9993(97)90206-9 [DOI] [PubMed] [Google Scholar]
- 3.Taylor-Piliae RE, Haskell WL, Stotts NA, Froelicher ES. Improvement in balance, strength, and flexibility after 12 weeks of Tai Chi exercise in ethnic Chinese adults with cardiovascular disease risk factors. Altern Ther Health Med 2006;12(2):50–8. [PubMed] [Google Scholar]
- 4.Lan C, Chen SY, Lai JS, Wong MK. Heart rate responses and oxygen consumption during Tai Chi Chuan practice. Am J Chin Med 2001;90(2–3):403–10. doi: 10.1142/S0192415X01000423 [DOI] [PubMed] [Google Scholar]
- 5.Li F, Fisher KJ, Harmer P, Irbe D, Tearse RG, Weimer C. Tai chi and self-rated quality of sleep and daytime sleepiness in older adults: a randomized controlled trial. J Am Geriatr Soc 2004;52(6):892–900. doi: 10.1111/j.1532-5415.2004.52255.x [DOI] [PubMed] [Google Scholar]
- 6.Fong SM, Ng GY. The effects on sensorimotor performance and balance with Tai Chi training. Arch Phys Med Rehabil 2006;87(1):82–7. doi: 10.1016/j.apmr.2005.09.017 [DOI] [PubMed] [Google Scholar]
- 7.Gatts SK, Woollacott MH. Neural mechanisms underlying balance improvement with short term Tai Chi training. Aging Clin Exp Res 2006;18(1):7–19. doi: 10.1007/BF03324635 [DOI] [PubMed] [Google Scholar]
- 8.Tsang WW, Wong VS, Fu SN, Hui-Chan CW. Tai Chi improves standing balance control under reduced or conflicting sensory conditions. Arch Phys Med Rehabil 2004;85(1):129–137. doi: 10.1016/j.apmr.2003.02.002 [DOI] [PubMed] [Google Scholar]
- 9.Wayne PM, Krebs DE, Wolf SL, Gill-Body KM, Scarborough DM, McGibbon CA, Kaptchuk TJ, Parker SW. Can Tai Chi improve vestibulopathic postural control? Arch Phys Med Rehabil 2004;85(1):142–52. doi: 10.1016/S0003-9993(03)00652-X [DOI] [PubMed] [Google Scholar]
- 10.Qin L, Choy W, Leung K, Au S, Hung W, Dambacher M, Chan K. Beneficial effects of regular Tai Chi exercise on musculoskeletal system. J Bone Miner Metab 2005;23(2):186–90. doi: 10.1007/s00774-004-0559-2 [DOI] [PubMed] [Google Scholar]
- 11.Wang C, Schmid CH, Hibberd PL, Kalish R, Roubenoff R, Rones R, et al. Tai Chi is effective in treating knee osteoarthritis: a randomized controlled trial. Arthritis Rheum 2009;61(11):1545–53. doi: 10.1002/art.24832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones KD, Sherman CA, Mist SD, Carson JW, Bennett RM, Li F. A randomized controlled trial of 8-form Tai Chi improves symptoms and functional mobility in fibromyalgia patients. Clin Rheumatol 2012;31(8):1205–14. doi: 10.1007/s10067-012-1996-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hall A, Maher C, Latimer J, Ferreira M. The effectiveness of Tai Chi for chronic musculoskeletal pain conditions: a systematic review and meta-analysis. Arthritis Care Res 2009;61(6):717–24. doi: 10.1002/art.24515 [DOI] [PubMed] [Google Scholar]
- 14.Burschka JM, Keune PM, Oy UH, Oschmann P, Kuhn P. Mindfulness-based interventions in multiple sclerosis: beneficial effects of Tai Chi on balance, coordination, fatigue and depression. BMC Neurol 2014;14:165. doi: 10.1186/s12883-014-0165-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ding M. Tai Chi for stroke rehabilitation: a focused review. Am J Phys Med Rehabil 2012;91(12):1091–6. doi: 10.1097/PHM.0b013e31826edd21 [DOI] [PubMed] [Google Scholar]
- 16.Ross MC, Bohannon AS, Davis DC, Gurchiek L. The effects of a short-term exercise program on movement, pain, and mood in the elderly. Results of a pilot study. J Holist Nurs 1999;17(2):139–47. doi: 10.1177/089801019901700203 [DOI] [PubMed] [Google Scholar]
- 17.Adler PA, Roberts BL. The use of Tai Chi to improve health in older adults. Orthop Nurs 2006;25(2):122–6. doi: 10.1097/00006416-200603000-00009 [DOI] [PubMed] [Google Scholar]
- 18.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore 1994;2(23):129–38. [PubMed] [Google Scholar]
- 19.Jensen MP, Hoffman AJ, Cardenas DD. Chronic pain in individuals with spinal cord injury: a survey and longitudinal study. Spinal Cord 2005;43(12):704–12. doi: 10.1038/sj.sc.3101777 [DOI] [PubMed] [Google Scholar]
- 20.Stroud MW, Turner JA, Jensen MP, Cardenas DD. Partner responses to pain behaviors are associated with depression and activity interference among persons with chronic pain and spinal cord injury. J Pain 2006;7(2):91–9. doi: 10.1016/j.jpain.2005.08.006 [DOI] [PubMed] [Google Scholar]
- 21.Raichle KA, Osborne TL, Jensen MP, Cardenas D. The reliability and validity of pain interference measures in persons with spinal cord injury. J Pain 2006;7(3):179–86. doi: 10.1016/j.jpain.2005.10.007 [DOI] [PubMed] [Google Scholar]
- 22.Whiteneck GG, Charlifue SW, Frankel HL, Fraser MH, Gardner BP, Gerhart KA, et al. Mortality, morbidity, and psychosocial outcomes of persons spinal cord injured more than 20 years ago. Paraplegia 1992;30(9):617–30. doi: 10.1038/sc.1992.124 [DOI] [PubMed] [Google Scholar]
- 23.Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev 1988;8(1):77–100. doi: 10.1016/0272-7358(88)90050-5 [DOI] [Google Scholar]
- 24.Brent DA, Holder D, Kolko D, Birmaher B, Baugher M, Roth C, et al. A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Arch Gen Psychiatry 1997;54(9):877–85. doi: 10.1001/archpsyc.1997.01830210125017 [DOI] [PubMed] [Google Scholar]
- 25.Wang YP, Gorenstein C, Wang YP, Gorenstein C. Psychometric properties of the Beck Depression Inventory–II: a comprehensive review. Rev Bras Psiquiatr 2013;35(4):416–31. doi: 10.1590/1516-4446-2012-1048 [DOI] [PubMed] [Google Scholar]
- 26.Kennedy P, Rogers BA. Anxiety and depression after spinal cord injury: a longitudinal analysis. Arch Phys Med Rehabil 2000;81(7):932–7. doi: 10.1053/apmr.2000.5580 [DOI] [PubMed] [Google Scholar]
- 27.Judd FK, Stone J, Webber JE, Brown DJ, Burrows GD. Depression following spinal cord injury. A prospective in-patient study. Br J Psychiatry 1989;154:668–71. [DOI] [PubMed] [Google Scholar]
- 28.Craig AR, Hancock K, Dickson H, Chang E. Long-term psychological outcomes in spinal cord injured persons: results of a controlled trial using cognitive behavior therapy. Arch Phys Med Rehabil 1997;78(1):33–8. doi: 10.1016/S0003-9993(97)90006-X [DOI] [PubMed] [Google Scholar]


