Abstract
Background
Child delivery in a health facility is important to reduce maternal mortality. Bypassing nearby birthing facility to deliver at a hospital is common in developing countries including Nepal. Very little is known about the extent and determinants of bypassing the birthing centres in Nepal. This study measures the status of bypassing, characteristics of bypassers and their reasons for bypassing.
Methods
A community-based cross-sectional study was carried out in six rural village development committees of Chitwan district of Nepal. Structured interviews were conducted with 263 mothers who had given birth at a health facility and whose nearest facility was a birthing centre. Descriptive statistics, univariate and multivariable logistic regression analysis were performed.
Results
More than half of the mothers had bypassed the nearer birthing centres to deliver at hospital. Living in plain area [aOR: 2.467; 95 % CI: 1.005–6.058], higher wealth index [aOR: 4.981; 95 % CI: 2.482–9.999], advantaged caste/ethnicity [aOR: 2.172; 95 % CI: 1.153–4.089], older age [aOR: 2.222; 95 % CI: 1.050–4.703] and first birth [aOR: 2.032; 95 % CI: 1.060–3.894] were associated with higher likelihood of bypassing. Among the reasons of bypassing as reported by the bypassers, lack of operation, video x-ray, and blood test facilities were the most common ones, followed by the lack of medicines/drugs and equipment, lack of skilled service provider, and inadequate physical facilities, among others.
Conclusions
Quality of service at the birthing centres needs to be given a high consideration to increase their use as well as to ensure an equitable access to the quality care by all.
Electronic supplementary material
The online version of this article (doi:10.1186/s12913-016-1848-x) contains supplementary material, which is available to authorized users.
Keywords: Bypassing, Birthing centre, Rural area, Nepal, Equitable access, Quality service
Background
Among the 289,000 maternal deaths that happen worldwide, 99 % occur in developing countries [1]. Although maternal mortality ratio (MMR) has declined in Nepal, it still stands at the second highest level among the South Asian countries [1]. Availability, access, and utilization of safe motherhood service along with the quality of the service are important in reducing the maternal deaths [2]. In particular, availability of birthing facilities is one of the critical strategies to reduce maternal mortality in developing countries [3].
Globally health centres led by midwives that provide basic emergency obstetric care serve as the ‘first level contact of care’ for childbirth close to the settings women live in and the birthing culture and rituals of the community. Referring complicated cases to hospital for comprehensive emergency obstetric care saves mothers and newborns lives [4–6]. Birthing centres should be staffed by midwives trained to manage normal pregnancies, child birth and the postnatal period, and to identify, manage and refer mother and newborn if complications arise [7].
Government of Nepal has been promoting expansion of birthing centres in a phase-wise manner in health facility of rural areas where access to health service is difficult for women [8]. The birthing centres are being attached to health posts and health centres of rural areas. At least two midwives are posted at a centre to provide the service for 24-hours [9]. However, referral system is not instituted properly in Nepal [10].
Utilization of the health services differs largely between the people of advantaged (Brahman/Chhetri and advantaged Janjati) and disadvantaged caste/ethnicity (disadvantaged Janjati and Dalits), with the latter one having less access to health services due to their poorer socio-economic development [11]. Similarly, among the three ecological zones of Nepal (Fig. 1), utilization of the childbirth service is lower in hill and mountain than in plain [12] due to difficulty in reaching to health facility owing to lack of transportation and difficult topography.
Fig. 1.
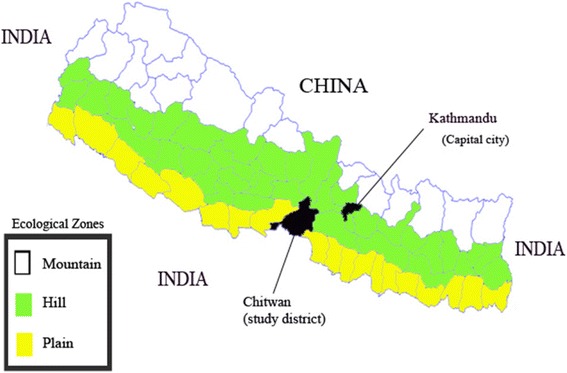
Ecological zones of Nepal and study district (Chitwan)
Despite the delivery service being free, a significant amount of out-of-pocket expenses incur accessing delivery service at a health facility, particularly in transportation, medicines, medical tests and X-rays, staying in maternity waiting homes and supplies [13]. Though the service at private health facility would cost more on drugs, tests and treatment [14], in Nepal accessing the service of private institutions for childbirth increased from 1.3 % in 1996 to 10.4 % in 2011 [15]. However, nearly three quarters (73.65 %) of the health facility deliveries happen in the government sector with only 20.28 % in private sector [16].
Rural areas in developing countries have usually health facilities with poorer quality service [17, 18]. Bypassing primary health care facilities takes place to get better quality service of hospital in terms of competency of service provider, availability of drugs and equipments, and quality of care [13]. A significant number of people tend to bypass the nearest health facilities to access the service including birthing facility of a hospital at a further distance [19–23].
A very limited information is available on bypassing birthing centres in Nepal [24]. Therefore, this study examines the status of bypassing birthing centre, characteristics of the women who bypass, and their reasons of bypassing.
Methods
Study setting
Chitwan district has a total population of 579,948 with 66 % rural population. People with various caste/ethnicity reside in the district including Brahman, Chhetri, Tharu, Tamang, Magar, Gurung, Newar, Chepang, Kami, Magar, Kumal, Darai, Sarki, Musalman, etc. More than three quarters (77 %) of population have upto five years schooling [25]. Although Chitwan is considered a plain district, some of its parts are hilly (Fig. 1). At the time of data collection, the district was divided into two municipalities and 36 village development committees (VDCs), with nine hill and the rest of the others plain VDCs. Recently, some VDCs have been merged to make other new municipalities. All municipalities and VDCs of the district are connected with roads except one hill VDC.
Though there are several private hospitals and nursing homes in the district [25], the major three referral hospitals comprise of one governmental and two teaching hospitals located in the district headquarter. The rural areas have been served by the 18 birthing centres at health posts and primary health care centres [25]. In this study, six rural VDCs were selected on the basis of lower percentage of health facility delivery than the average of the district. Then all eligible women of six randomly selected wards out of nine from each of the selected VDCs were included. The details of sampling process has been explained somewhere else [26].
Study design, study participants and sample size
A community-based cross-sectional study was carried out including 673 women who had given birth during April 21, 2012 and April 20, 2013 in the selected study areas. Among these, for 490 women birthing centre was the nearest birthing facility, while it was a hospital for the remaining 183 women. This study was limited to 263 women whose nearest birthing facility was a birthing centre and had given birth at a health facility. Of the 263 women, 119 gave birth at the nearest birthing centre, whereas 144 bypassed and went to a hospital (Fig. 2).
Fig. 2.
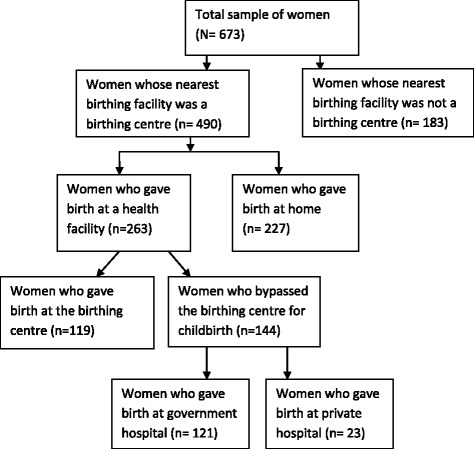
Selection of study participants
Data collection
First a list of mothers who had given birth during the study period was prepared from the records of female community health volunteers (FCHVs). Records of mothers were cross-checked from both pregnancy and delivery registers maintained by the FCHVs under community-based newborn care program [10]. Additionally, inquiry was made in the communities for any other potential missed cases of birth.
Data collection was done between April 26, 2013 and June 30, 2013. Face-to-face interviews were conducted using structured questionnaire (Additional file 1) making household visits. Nepal Health Research Council granted ethical approval to the study (registration number 21/2012). The purpose of the study was explained and informed consent from the participants or from their mother-in-law/husband/other guardian for those who were below the legal age was obtained before the data collection. Voluntary participation of the participants was ensured throughout the study by advising them that they had the right to refuse to participate or to withdraw their participation at any time without prejudice. Personal identifiers were removed from the datasets before analysis. Students of Bachelor of Public Health and Masters of Sociology with previous experience of data collection were recruited as data enumerators. They were provided with orientation on the data collection and involved in pretesting of the questionnaire [27].
Statistical analysis
Outcome variable, i.e., bypasser status, has been categorized as bypassers and non-bypassers. Bypassers are women who bypassed the nearest birthing centre and delivered at hospital (coded 1), while non-bypassers are those who gave birth at the nearest birthing centre (coded 0). Eight independent variables have been included in the study. Place of residence: The place of residence of the women was categorized into ‘hill’ and ‘plain’ area. Caste/Ethnicity: The caste/ethnicity has been categorized as ‘advantaged’ and ‘disadvantaged’ caste/ethnicity. The advantaged group includes the upper caste (Brahman/Chhetri) and advantaged Janjati (Newar and Gurung). The disadvantaged caste/ethnicity includes the disadvantaged Janjati and lower caste (Dalits) [11, 28]. Educational status: The number of schooling year has been categorized as ‘no schooling’ and ‘primary (upto grade five) and above’. Wealth index: A relative wealth index was constructed by principal component analysis based on the household ownership of assets [29]. The women were categorized into two groups- with ‘lower’ and ‘higher’ wealth index. Age: The completed age in years at the time of childbirth has been categorized into ‘15–24 years’ and ‘25 or more years’. Birth order: The order of the recent birth has been categorized as ‘1st’ and ‘2nd or more’. Complication during delivery: Experience of complication during the recent childbirth has been categorized as ‘yes’ if the women experienced complication and ‘no’ if the women did not experience complication. Antenatal care (ANC): It is the number of ANC visit a woman had during the recent pregnancy. It has been categorized as ‘<4’ and ‘4 or more’.
Data entry was done in Epi data version 3.1 [30] and data analysis was carried out in Statistical Package for the Social Sciences version 16.0 [31]. Descriptive statistics was used to identify the distribution of bypassers and non-bypassers across different independent variables. Logistic regression analysis was used [32] for univariate and multivariable analysis. The multivariable logistic regression analysis was performed including all the independent variables simultaneously in a model.
Results
Status of bypassing
Among the 263 women whose nearest birthing facility was a birthing centre and had health facility delivery, 119 (45 %) gave birth in the birthing centre, while 144 (55 %) bypassed and went to a hospital at a further distance for the birth. Among the bypassers, a large majority (84 %) went to government hospital, while the remaining 16 % went to a private hospital.
Characteristics of women associated with bypassing
Table 1 shows the distribution of characteristics of women by the status of bypassing. Nearly two third of women (63 %) living in plain area bypassed, while it was only 21 % among women residing in hill. Nearly three quarters of women from advantaged caste/ethnicity bypassed in comparison to 44 % among disadvantaged caste/ethnicity. Similarly, about three quarters of women with higher wealth index bypassed compared to only 23 % of those with lower wealth index. The likelihood of bypassing was higher among women with more education. A slightly higher percentage of women with age 25 and more years bypassed than the women in the age group 15–24 years. A higher proportion of women having four or more ANC visit bypassed the nearest birthing facility compared to the women having less than four ANC visits (62 % versus 40 %). A larger proportion of women both with first parity and experiencing complication during birth bypassed than the women with two or more births and having no complication respectively.
Table 1.
Distribution of characteristics of women by the status of bypassing
| Characteristics | Status of bypassing | ||
|---|---|---|---|
| Not Bypass | Bypass | Total | |
| Place of residence | |||
| Plain | 78 (37) | 133 (63) | 211 |
| Hill | 41 (79) | 11 (21) | 52 |
| Caste/ethnicity | |||
| Disadvantaged | 91 (56) | 76 (44) | 167 |
| Advantaged | 28 (29) | 68 (71) | 96 |
| Wealth index | |||
| Lower | 69 (78) | 20 (22) | 89 |
| Higher | 50 (29) | 124 (71) | 174 |
| Educational status | |||
| No schooling | 34 (71) | 14 (29) | 48 |
| Primary and above | 85 (40) | 130 (61) | 215 |
| Age group | |||
| 15–24 years | 88 (48) | 97 (52) | 185 |
| 25 and more years | 31 (40) | 47 (60) | 78 |
| Birth order | |||
| 1st | 54 (39) | 84 (61) | 138 |
| 2nd and more | 65 (52) | 60 (48) | 125 |
| ANC number | |||
| < 4 | 53 (60) | 38 (40) | 91 |
| 4 or more | 66 (38) | 106 (62) | 172 |
| Experience of complications during delivery | |||
| No | 105 (48) | 114 (52) | 219 |
| Yes | 14 (32) | 30 (68) | 44 |
Table 2 depicts that in univariate logistic regression analysis five variables, namely, living in plain area, advantaged caste/ethnicity, higher wealth index, first birth and less than 4 ANC visits were found to be statistically significantly associated with the higher odds of bypassing. Likewise, the multivariable analysis also showed five variables having statistically significant associations with bypassing. However, frequency of ANC visit lost its significance, while age of the women appeared to have an association. The women living in plain were more than 2 times [Adjusted odds ratio (aOR): 2.467; 95 % CI: 1.005–6.058] more likely to bypass than women in hill. Similarly, bypassing was more than 2 times [aOR: 2.172; 95 % CI: 1.153–4.089] higher also among women from advantaged caste/ethnicity compared to disadvantaged ones. Women with higher wealth index had about 5 times [aOR: 4.981; 95 % CI: 2.482–9.999] higher odds of bypassing. Likewise, the women with age group 25 and more years and giving first birth had also more than 2 times [aOR: 2.222; 95 % CI: 1.050–4.703 and [aOR: 2.032; 95 % CI: 1.060–3.894] greater likelihood of bypassing compared to younger women and for higher birth order respectively.
Table 2.
Factors associated with bypassing
| Variables | Unadjusted OR (95 % CI) | P-value (Crude) | Adjusted OR (95 % CI) | P-value (adjusted) |
|---|---|---|---|---|
| Place of residence | ||||
| Plain | 6.355 (3.088–13.081) | <0.001 | 2.467 (1.005–6.058) | 0.049 |
| Hill | 1.00 | 1.00 | ||
| Caste/ethnicity | ||||
| Disadvantaged | 1.00 | 1.00 | ||
| Advantaged | 3.714 (1.882–7.330) | <0.001 | 2.172 (1.153–4.089) | 0.016 |
| Wealth index | ||||
| Lower | 1.00 | 1.00 | ||
| Higher | 8.556 (4.713–15.532) | <0.001 | 4.981 (2.482–9.999) | <0.001 |
| Educational status | ||||
| No schooling | 1.00 | 1.00 | ||
| Primary and above | 1.468 (0.666–3.236) | 0.341 | 2.152 (0.921–5.029) | 0.077 |
| Age group | ||||
| 15–24 years | 1.00 | 1.00 | ||
| 25 and more years | 1.375 (0.804–2.354) | 0.245 | 2.222 (1.050–4.703) | 0.037 |
| Birth order | ||||
| 1st | 1.685 (1.033–2.750) | 0.037 | 2.032 (1.060–3.894) | 0.033 |
| 2nd and more | 1.00 | 1.00 | ||
| ANC number | ||||
| < 4 | 2.240 (1.335–3.759) | 0.002 | 0.908 (0.487–1.695) | 0.762 |
| 4 or more | 1.00 | 1.00 | ||
| Experience of complications during delivery | ||||
| No | 1.00 | 1.00 | ||
| Yes | 1.974 (0.992–3.925) | 0.053 | 1.621 (0.846–3.107) | 0.146 |
| Nagelkerke R Square | 0.360 | |||
| Hosmer and Lemeshow Test | 0.411 | |||
Bold font indicates statistical significance with p < 0.05
The Hosmer and Lemeshow test result shows that the data fit into the model well [33].
Reasons of bypassing
Lack of operation /video x-ray/blood test facility at the nearest birthing centres was the most common reason (59 %) for bypassing, followed by lack of necessary equipments/drugs (43 %), lack of skilled health worker (42 %), inadequate physical facilities (36 %), low confidence in service provider (25 %), etc. (Table 3).
Table 3.
Reasons of bypassing reported by bypassers (multiple response analysis)
| Reasons of bypassing | Frequency (n = 144) | Percentage |
|---|---|---|
| Lack of operation/video x-ray/blood test facility | 78 | 59 |
| Lack of necessary drugs/equipments | 57 | 43 |
| Lack of skilled health worker | 56 | 42 |
| Inadequate physical facilities | 48 | 36 |
| Low confidence of health worker | 33 | 25 |
| Service provider not available | 2 | 1.5 |
| Othersa | 3 | 2.3 |
| Don’t know | 3 | 2.3 |
aOn Saturday health post is closed/No knowledge of service/not open for 24 h
Discussion
Status of bypassing
The study found that though birthing centres were closer, more than half (55 %) of the women bypassed the centres and gave birth at a hospital. The bypassing status in the current study is higher than in rural Tanzania [23] where 42.2 % of women who had health facility delivery had bypassed the nearest birthing facility. Similarly, another study of rural Tanzania showed 41.8 % women bypassing the birthing service of the local primary care clinic [21]. The figure of bypassing in the current study is, however, lower than that of the previous study in Nepal which found 70.2 % of women having health facility delivery had bypassed birthing centres [24]. People generally tend to bypass the closer health facilities in favour of those with better quality of service. In a study in Nepal women rated birthing centres lowest in terms of adequacy of medical equipment and competency of health personnel compared to both public and private hospitals [34]. More wealthy and those having intrapartum complications were more likely to bypass the nearest birthing facility. Availability of operating facility, adequacy of medical supplies and equipment and competent health staff at the hospital were mentioned as the reasons of bypassing nearest birthing centres and choosing hospital to give birth [22].
Factors associated with bypassing
Women living in plain area had higher odds of bypassing the nearer birthing centre than the women residing in hill. It could be because of the difficulty in travelling due to lack of roads and transportation in the hills.
In the current study women from advantaged caste/ethnicity were more likely to bypass compared to women from disadvantaged caste/ethnicity. A previous study in Nepal found no association of caste/ethnicity with bypassing [24]. The reason could lie in the types of caste/ethnicity and categorization of the variable. Unlike the previous study, the caste/ethnicity in the current study has been classified into only two categories, i.e., advantaged and disadvantaged. Barker et al also mentioned that access to safe motherhood services is largely influenced by caste/ethnicity [9].
Wealthier women were about five times more likely to bypass the birthing centre. Similar results were found in the previous studies in Nepal [24] and Tanzania [21]. Around a quarter of families in low- and middle-income countries have to borrow or/and sell their assets to pay for health care. Poorer families have to undergo more hardships [13, 35] which would make it difficult for them to access health services at a further distance due to costs related particularly to travelling further and staying at health facility.
Educational status of the women showed no effect on bypassing. This is consistent with the findings of a study in rural Tanzania where there was no association between bypassing and women having no schooling and some schooling [23].
Older women tended to bypass more than the younger ones. Similar results were observed in the previous study of Nepal where women aged 25 or more years had more than four times higher odds of bypassing than the younger women [24]. Likewise, in rural Tanzania 35 or more age group was associated with higher likelihood of bypassing than younger age [23]. Similarly, in Ghana a higher proportion of patients aged above 38 years had bypassed nearer health facility than the younger ones [36].
Bypassing was more common for first birth than the second or thereafter birth. Similar trends were observed in the previous studies of Nepal [24] and Tanzania [21].
Frequency of ANC visits showed no effect on bypassing. There are mixed results in the body of literature regarding the association between ANC visits and bypassing [22, 23]. Similarly, experience of complication during delivery was not associated with bypassing in the current study. The qualitative study carried out before the current study had found that the women who bypassed the nearest birthing centre had directly visited the farther hospital without having any complication. Similarly, in Ghana among the patients visiting an urban hospital 63% had bypassed local facility without experiencing any complication [36]. Having visited the hospital before was about three times more associated with bypassing the local facility. In the current study settings, the birthing centres had recently been in operation for only about two years preceding the survey. Access to health service depends not only on the distance from the home of a person but also upon the quality of health facilities [17]. As mentioned by Parkhurst et al the women might have bypassed the birthing centres due to the popularity of the hospitals they sought care and also because distance was not a problem to them due to the availability of the transportation facility in most of the study areas [37].
Reasons of bypassing
In the current study, the most common reasons for bypassing were lack of operation /video x-ray/blood test facilities, lack of adequate drugs and equipment, and incompetent health worker at the nearer birthing centre. Consistent results were found in other studies conducted in rural Tanzania [19] and Nepal [24]. The study of Tanzania found lack of diagnostic facilities as the major reason, followed by lack of drugs, among others, whereas in the study of Nepal lack of operation facility was the most common reason followed by inadequate drugs and equipment, incompetent staff, etc. Similarly, unavailability of health worker was mentioned by a small percentage of women in all the three studies. The lack of confidence in health workers at birthing centres in this study could be due to lack of cadres appropriately trained as skilled birth attendants, as well as inadequate equipments.
The study has some potential limitations as well as strengths. A major limitation of the study is that bypassing by preference is not distinguished from referral by heath workers for women identified during pregnancy to be at higher risk of birthing complications (e.g. due to primigravida, grand multipara, pre-eclampsia, foetal distress, anaemia, previous history of complications etc.). This could partly explain some of the observed associations between bypassing and age and birth order. However, another study in Nepal found that 98 % of women attending referral hospitals bypass nearer birthing centres by preference [38], and this cannot explain the inequalities observed by caste and wealth groups. Secondly, since the study areas were selected on the basis of lower percentage of institutional delivery compared to the other VDCs of the district, the results may not be generalizable in all contexts. Nevertheless, the study provides information of the settings that are in priority with respect to equity in accessing quality service. Thirdly, there was a possibility of recall bias, however, limiting the study period to one year and most of the variables being socio-demographic characteristics of the women reduced the likelihood of the bias in the study. Lastly, other potential predictors were not included in the study, such as complications during pregnancy, previous pregnancies and birth, and actual quality of care at birthing centres.
Conclusions
More than half of the women had bypassed the nearest birthing centre to give birth at a higher-level hospital with better quality of birthing service. Birthing centres have generally less competent health workers, inadequate drugs and equipment, poorer infrastructure and lack diagnostic facilities. Women residing in plain area, with higher wealth index, from advantaged caste/ethnicity, older women and giving first birth had higher likelihood of bypassing. It indicates inequity among women in accessing quality birthing service. Improvement in the quality of the service of rural birthing centres would ensure equitable access to the quality service by also women from hill, poorer, disadvantaged castes groups, younger women and women giving birth for second or more time. Improvement in the quality of the service at the local birthing centres would also reduce bypassing which would subsequently reduce financial burden to the family associated with travelling further among bypassers as well because people’s willingness to go further does not mean they are able to pay for the expenses [39].
Acknowledgements
Heartfelt thanks are to four supervisors- Maria Delius, Eva A Rehfuess, Mahesh Kumar Maskey and Rainald Fischer, as well as to Dr. Shyam Thapa, Dr. Prem B. Bhandari and Dr. Deepak Paudel who advised and guided in the whole PhD study of which the current one is a part.
Funding
The study was funded with the award received for the study from Farrar Foundation, UK. The funding body did not have role in study design, collection, analysis and interpretation of data or writing the manuscript.
Availability of data and materials
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
Authors’ contributions
RS designed the study, managed field work, analyzed data, and wrote the manuscript.
Competing interests
The author declares that he/she has no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Ethical approval to the study was provided from Nepal Health Research Council (registration number 21/2012). The purpose of the study was explained and informed consent from the participants or from their mother-in-law/husband/other guardian for those who were below the legal age was obtained before the data collection. Voluntary participation of the participants was ensured throughout the study by advising them that they had the right to refuse to participate or to withdraw their participation at any time without prejudice. Personal identifiers were removed from the datasets before analysis.
Abbreviations
- ANC
Antenatal care
- aOR
Adjusted odds ratio
- FCHV
Female Community Health Volunteer
- MMR
Maternal mortality ratio
- VDC
Village Development Committee
Additional file
Survey tool used for interview with respondents. (DOCX 23 kb)
References
- 1.WHO . Trends in Maternal Mortality: 1990 to 2013: Estimates by WHO, UNICEF, UNFPA, the World Bank and the United Nations Population Division. Geneva: World Health Organization; 2014. [Google Scholar]
- 2.CBS . Population Monograph of Nepal (Population Dynamics) Kathmandu: Government of Nepal, National Planning Commission Secretariat, Central Bureau of Statistics; 2014. [Google Scholar]
- 3.Koblinsky MA. Reducing Maternal Mortality: Learning from Bolivia, China, Egypt, Honduras, Indonesia, Jamaica, and Zimbabwe. Washington, D.C: World Bank Publications; 2003.
- 4.Koblinsky M, et al. Going to scale with professional skilled care. Lancet. 2006;368(9544):1377–1386. doi: 10.1016/S0140-6736(06)69382-3. [DOI] [PubMed] [Google Scholar]
- 5.WHO . The World health report 2005 : make every mother and child count. Geneva: World Health Organization; 2005. [DOI] [PubMed] [Google Scholar]
- 6.Campbell OM, Graham WJ. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368(9543):1284–1299. doi: 10.1016/S0140-6736(06)69381-1. [DOI] [PubMed] [Google Scholar]
- 7.[Nepal] M. National Policy on Skilled Birth Attendants. 2006. Ministry of Health and Population, Government of Nepal: Kathmandu
- 8.FHD . National Safe Motherhood and Newborn Health Long-Term Plan (2006-2017) Kathmandu, Nepal: Family Health Division, Ministry of Health and Population, Government of Nepal; 2006. [Google Scholar]
- 9.Barker CE, et al. Support to the Safe Motherhood Programme in Nepal: an integrated approach. Reprod HealthMatters. 2007;15(30):81–90. doi: 10.1016/S0968-8080(07)30331-5. [DOI] [PubMed] [Google Scholar]
- 10.MOHP . Annual Report 2012/2013. Kathmandu: Department of Health Services, Ministry of Health and Population, Government of Nepal; 2014. [Google Scholar]
- 11.World Bank D . Unequal citizens: gender, caste and ethnic exclusion in Nepal- Executive Summary. Kathmandu, Nepal: The World Bank and DFID; 2006. [Google Scholar]
- 12.Tripathi V, Singh R. Ecological and socio-demographic differences in maternal care services in Nepal. PeerJ. 2015;3:e1215. doi: 10.7717/peerj.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kruk ME, et al. User fee exemptions are not enough: out‐of‐pocket payments for ‘free’delivery services in rural Tanzania. Tropical Med Int Health. 2008;13(12):1442–1451. doi: 10.1111/j.1365-3156.2008.02173.x. [DOI] [PubMed] [Google Scholar]
- 14.Basu S, et al. Comparative performance of private and public healthcare systems in low- and middle-income countries: a systematic review. PLoS Med. 2012;9(6):e1001244. doi: 10.1371/journal.pmed.1001244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hotchkiss DR, Godha D, Do M. Expansion in the private sector provision of institutional delivery services and horizontal equity: evidence from Nepal and Bangladesh. Health Policy Plan. 2014;29(Suppl 1):i12–i19. doi: 10.1093/heapol/czt062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MOHP . Nepal Demographic and Health Survey 2011. Kathmandu, Nepal: Ministry of Health and Population, New Era, ICF International; 2012. [Google Scholar]
- 17.Klemick H, Leonard KL, Masatu MC. Defining access to health care: evidence on the importance of quality and distance in rural Tanzania. Am J Agric Econ. 2009;91(2):347–358. doi: 10.1111/j.1467-8276.2009.01252.x. [DOI] [Google Scholar]
- 18.Leonard KL, Masatu MC. Variations in the quality of care accessible to rural communities in Tanzania. Health Aff (Millwood) 2007;26(3):w380–w392. doi: 10.1377/hlthaff.26.3.w380. [DOI] [PubMed] [Google Scholar]
- 19.Kahabuka C, et al. Why caretakers bypass Primary Health Care facilities for child care - a case from rural Tanzania. BMC Health Serv Res. 2011;11:315. doi: 10.1186/1472-6963-11-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Akin JS, Hutchinson P. Health-care facility choice and the phenomenon of bypassing. Health Policy Plan. 1999;14(2):135–151. doi: 10.1093/heapol/14.2.135. [DOI] [PubMed] [Google Scholar]
- 21.Kruk ME, et al. Bypassing primary care clinics for childbirth: a cross-sectional study in the Pwani region, United Republic of Tanzania. Bull World Health Organ. 2014;92(4):246–253. doi: 10.2471/BLT.13.126417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karkee R, Lee AH, Binns CW. Bypassing birth centres for childbirth: an analysis of data from a community-based prospective cohort study in Nepal. Health Policy Plan. 2015;30(1):1–7. doi: 10.1093/heapol/czt090. [DOI] [PubMed] [Google Scholar]
- 23.Kruk ME, et al. Bypassing primary care facilities for childbirth: a population-based study in rural Tanzania. Health Policy Plan. 2009;24(4):279–288. doi: 10.1093/heapol/czp011. [DOI] [PubMed] [Google Scholar]
- 24.Karkee R, Lee AH, Binns CW. Bypassing birth centres for childbirth: an analysis of data from a community-based prospective cohort study in Nepal. Health Policy Plan. 2013;30(1):1–7. doi: 10.1093/heapol/czt090. [DOI] [PubMed] [Google Scholar]
- 25.CBS . District Profile of Chitwan. Chitwan: Government of Nepal, National Planning Commission Secretariat, Central Bureau of Statistics, Statistics Office, Chitwan; 2014. [Google Scholar]
- 26.Shah R, et al. Factors affecting institutional delivery in rural Chitwan district of Nepal: a community-based cross-sectional study. BMC Pregnancy Childbirth. 2015;15:27. doi: 10.1186/s12884-015-0454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Teijlingen E, Hundley V. Pilot studies in family planning and reproductive health care. J Family Plan Repro Health Care. 2014;31(3):219–221. doi: 10.1783/1471189054483735. [DOI] [PubMed] [Google Scholar]
- 28.Pandey JP, Dhakal MR, Karki S, Poudel P, Pradhan MS. Maternal and Child Health in Nepal: The Effects of Caste, Ethnicity, and Regional Identity: Further analysis of the 2011 Nepal Demographic and Health Survey. Calverton, Maryland, USA: Nepal Ministry of Health and Population, New ERA, and ICF International; 2013. [Google Scholar]
- 29.Filmer D, Pritchett LH. Estimating wealth effects without expenditure Data—Or tears: An application to educational enrollments in states of india*. Demography. 2001;38(1):115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 30.Lauritsen JM, Bruus M. EpiData Entry. A comprehensive tool for validated entry and documentation of data. Odense Denmark: The EpiData Association; 2008. [Google Scholar]
- 31.Norusis M. SPSS 16.0 statistical procedures companion. Upper Saddle River, NJ, USA: Prentice Hall Press; 2008.
- 32.Peng C-YJ, Lee KL, Ingersoll GM. An introduction to logistic regression analysis and reporting. J Educ Res. 2002;96(1):3–14. doi: 10.1080/00220670209598786. [DOI] [Google Scholar]
- 33.Bewick V, Cheek L, Ball J. Statistics review 14: Logistic regression. Crit Care. 2005;9(1):112–118. doi: 10.1186/cc3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karkee R, Lee AH, Pokharel PK. Women’s perception of quality of maternity services: a longitudinal survey in Nepal. BMC pregnancy childbirth. 2014;14(1):45. doi: 10.1186/1471-2393-14-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kruk ME, Goldmann E, Galea S. Borrowing and selling to pay for health care in low- and middle-income countries. Health Aff (Millwood) 2009;28(4):1056–1066. doi: 10.1377/hlthaff.28.4.1056. [DOI] [PubMed] [Google Scholar]
- 36.Yaffee AQ, et al. Bypassing proximal health care facilities for acute care: a survey of patients in a Ghanaian Accident and Emergency Centre. Trop Med Int Health. 2012;17(6):775–781. doi: 10.1111/j.1365-3156.2012.02984.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Parkhurst JO, Ssengooba F. Assessing access barriers to maternal health care: measuring bypassing to identify health centre needs in rural Uganda. Health Policy Plan. 2009;24(5):377–384. doi: 10.1093/heapol/czp023. [DOI] [PubMed] [Google Scholar]
- 38.FHD/NHSSP . Responding to Increased Demand for Institutional Childbirths at Referral Hospitals in Nepal: Situational Analysis and Emerging Options. Kathmandu: Family Health Division, Department of Health Services, Ministry of Health and Population [Nepal]/Nepal Health Sector Support Programme; 2013. [Google Scholar]
- 39.McIntyre D, et al. What are the economic consequences for households of illness and of paying for health care in low-and middle-income country contexts? Soc Sci Med. 2006;62(4):858–865. doi: 10.1016/j.socscimed.2005.07.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.


