Abstract
Background
Students’ health and school absenteeism affect educational level, with adverse effects on their future health. This interdependence is reflected in medical absenteeism. In the Netherlands, a public health intervention has been developed to address medical absenteeism in pre-vocational secondary education. This study aims to investigate the effectiveness of this intervention on students’ medical absenteeism, compared to “medical absenteeism policy as usual”.
Methods
A quasi-experimental design with an intervention group (493 students) and a control group (445 students) was applied. Multilevel analysis was used to study differences in the development of the level of a student’s medical absence over time (after 3 and 12 months).
Results
In the intervention group, the level of absenteeism decreased from 8.5 days reported sick in 12 school weeks to 5.7 days after 3 months, and to 4.9 days after 12 months. The number of absence periods fell from 3.9 in 12 school weeks to 2.5 after 3 months, and to 2.2 after 12 months. In the control group, the absence days initially decreased from 9.9 days reported sick in 12 school weeks to 8.4 days after 3 months, after which an increase to 8.9 days was measured. The number of absence periods initially decreased from 4.5 in 12 school weeks to 3.5, after which an increase to 3.7 was measured. The number of absence days per period remained about the same in both groups.
Conclusions
The study provides first indications for the intervention to be effective for Dutch pre-vocational secondary students with increased medical absence rates. The intervention, which consists of personalised management of medical absenteeism by systematic identification of students with extensive medical absenteeism and consistent referral to youth health care physicians, appears to reduce the absence rates more effectively than “medical absenteeism policy as usual”. The effectiveness of the intervention is shown primarily by a decrease in the number of periods reported sick.
Keywords: School absenteeism, Medical absenteeism, Preventive youth health care, Intervention research, Health inequalities, Pre-vocational secondary education
Background
School absenteeism may lead to a lower level of education or even school dropout [1–4]. Low educational level and school dropout are both strongly associated with an increased risk of social failure and delinquency [5–9], increased risk behaviour (e.g. smoking, obesity, lack of exercise) [10, 11], a higher prevalence of mental problems and chronic health issues [12–15], and higher mortality rates [16–21]. Tackling school absenteeism can reduce socio-economic health inequalities by optimising children’s educational opportunities and future prospects.
Literature frequently distinguishes between unexcused and excused school absenteeism. Unexcused absenteeism is truancy, not attending school without permission. Excused absence means not attending lessons with permission because of familial or personal reasons, with sickness reporting, also called medical absenteeism, as a major reason. Prevalence rates on school absenteeism as reported in literature are not directly comparable internationally, due to inconsistent use of parameters for school absenteeism. Nowadays, figures at the national level show that medical absenteeism occurs approximately twice as often as truancy [22–24]. In the Netherlands in 2002 medical absenteeism was more prevalent in pre-vocational secondary education than in the other two tracks in secondary education (senior general secondary education and pre-university education): 4 v. 3.7 and 3.4 % [25]. See Appendix for a description of the Dutch educational system [26]. No more recent valid figures on absenteeism are available. Because of the strict enforcement of measures against truancy in recent years and on the basis of current international figures, it is conceivable that in the Netherlands also, the medical absence rate has increased meanwhile compared to truancy.
Research on medical absenteeism shows that it is caused not only by medical problems [2, 27], but also by a low threshold for reporting sick, by risk behaviour, or stress-related physical complaints [2, 22]. The latter may have more complex causes such as psychological, family, or social problems [2]. Students attending Dutch pre-vocational secondary education are less positive about their health, have a poorer lifestyle and more psychosomatic complaints [28, 29], and more often demonstrate behavioural problems [30], which may explain their higher medical absenteeism. Moreover, these students have difficulties planning their studies [31]. Consequently, they experience problems in catching up after once having fallen behind because of missing course material. When dropping out, these students cannot fall back on a lower level of education. This explains why dropout rates are the highest in pre-vocational secondary education. On average three quarters of the new early school-leavers that are registered each year come from lower pre-vocational secondary education [32].
Until now, the only programmes for reducing school absenteeism developed and applied relate to unexcused absence and school refusal behaviour [2]. It was recommendable to develop interventions for addressing medical absenteeism, especially for pre-vocational secondary students, because of its increased prevalence and risk of dropout. In the Netherlands, medical absenteeism from secondary school depends solely on parental sick reporting and the authority to decide how to deal with it lies with the schools. This so-called “medical absenteeism policy as usual” is not defined. Dutch secondary schools have their own care system and their own way of handling sick reports. The Youth Health Care department of the Regional Public Health Service West Brabant (a region in the southwest of the Netherlands with a population density of 375 people per square kilometre) developed the MASS intervention [33] (see Table 1) in collaboration with the educational sector. It was assumed student’s absence rate to be reduced by providing personalised care, support, and guidance addressing these multiple causes. By applying the MASS intervention, students with increased medical absence rates (i.e. four periods in 12 school weeks, or more than six consecutive days) are identified by the school, and are then referred to youth health care physicians (YHCPs). Besides initial medical assessments, the YHCP also perform biopsychological evaluation of the absence in order to identify specific needs of the student. In addition, the physician, together with student, parents and school, designs a management plan based on guidelines for care, counseling, and educational adaptation. This plan describes what is needed to improve the student’s health and well-being and to maximise the participation in school activities, thus protecting the student against underachievement and dropout from education. Recently, Hawkrigg and Payne presented a more or less similar practical approach to prolonged school non-attendance [34]. The MASS-criterion “four periods in 12 school weeks” was chosen because practice shows that the study outcomes of students are adversely affected not only by the length, but also by the frequency of (short-term) absences, therefore both presenting similar risks. The MASS-criterion “more than six consecutive days” was chosen to exclude students with uncomplicated influenza illness, because uncomplicated influenza illness typically resolves after 3–7 days for the majority of persons [35]. The MASS intervention was included in a survey on European real-life interventions that aim to reduce socio-economic health inequalities [36].
Table 1.
Description of the Dutch intervention ‘Medical Advice for Sick-reported Students’, abbreviated as MASS
| The MASS intervention consists of an integrated approach in a public health setting. MASS provides a clear framework in which schools, in direct collaboration with youth health care physicians (YHCPs), are able to reach students and their parents, discuss aspects of the student’s medical absence, and design and monitor a management plan that aims to optimise students’ health and maximise students’ participation in school activities. In summary, the aim of the MASS intervention is to limit the absenteeism by arranging appropriate care, educational adjustments and adequate support for students and parents. A systematic routine is followed. |
| Step 1 School’s policy: |
| The school communicates with students and parents about the new policy in case of absenteeism because of medical reasons. |
| Step 2 Referral to the YHCP: |
| Students with extensive medical absence are identified by school by using well-defined threshold criteria: reported sick four times in 12 school weeks or more than six consecutive school days (MASS-criteria). Meeting the criteria always leads to a referral to the YHCP for student and parents. |
| Step 3 Consultation of student and parents with the YHCP: |
| During the interview and medical assessment YHCPs look for biological, psychological and social factors that contribute to the students’ medical absenteeism. The YHCP identifies whether there is a specific somatic or psychiatric diagnosis to account for the absence. If the diagnosis is clear the focus will be on optimising the (adherence to) treatment. In cases of frequent physical complaints and psychosocial problems with no clear medical diagnosis, the YHCP considers diagnostics, and looks for family and school related factors, as well as health risk behaviours and lifestyle aspects that contribute to the physical complaints and psychosocial problems. If needed, the YHCP refers to a medical specialist or a psychosocial support network. A management plan is then designed together with student, parents and school, and with curative professionals, if applicable. This plan includes agreements on cure, care and school attendance. |
| Step 4 Monitoring the management plan: |
| School and YHCP monitor the execution of the management plan. |
To the best of our knowledge, the effectiveness of an intervention for addressing extensive medical absenteeism has not been investigated before. The objective of the current study is to evaluate the effects of the MASS intervention in pre-vocational secondary education: is there a decline in students’ level of medical absenteeism following systematic identification and consistent referral to the YHCP of students with extensive medical absenteeism, compared to a situation in which this specific approach is absent?
Methods
Setting
The study was conducted in the Netherlands, West Brabant region. In school year 2011–2012, the MASS intervention had been applied by seven out of all 21 schools for pre-vocational secondary education. To implement the intervention, schools had to release their own financial resources to pay for the consultation with the YHCPs. All these seven schools were asked to participate in the study as an intervention school. In 2014, within the group of the 14 remaining schools, seven schools were asked to participate in the study as a control school, by providing anonymised absence data of their students retrospectively. This was done to avoid influence of their ‘medical absenteeism policy as usual’ during the study period. A condition for participation in the study as a control school was that the MASS intervention still had not been applied in the school year 2012–2013. The selection of the control schools was determined by school characteristics, that had to match as much as possible with those of the intervention schools. The characteristics of the schools are described in Table 2.
Table 2.
The characteristics of the intervention and control schools
| School | School characteristics | |||
|---|---|---|---|---|
| Urbanisationa | Fields of education | Size of the schoolb | ||
| Intervention schools | School 1 | predominantly rural region | General lower secondary education Social care | medium-sized |
| School 2 | predominantly urban region | General lower secondary education Economics Technology |
medium-sized | |
| School 3 | predominantly urban region | Economics Social care Technology |
medium-sized | |
| School 4 | predominantly urban region | General lower secondary education Economics Technology |
large | |
| School 5 | urban region | General lower secondary education Agriculture | medium-sized | |
| School 6 | urban region | General lower secondary education | medium-sized | |
| School 7 | urban region | General lower secondary education Economics | large | |
| Control schools | School 8 | urban region | General lower secondary education Sports | medium-sized |
| School 9 | predominantly urban region | General lower secondary education Economics Technology |
large | |
| School 10 | predominantly rural region | General lower secondary education Social care Technology |
medium-sized | |
| School 11 | predominantly rural region | General lower secondary education Agriculture | large | |
| School 12 | predominantly urban region | General lower secondary education Agriculture | medium-sized | |
| School 13 | predominantly urban region | General lower secondary education Economics Social care Technology |
small | |
| School 14 | rural region | Economics Social care Technology |
medium-sized | |
aUrbanisation: rural (<200 inhabitants per square kilometre), predominantly rural region (200–500 inhabitants per square kilometre), predominantly urban region (500–1000 inhabitants per square kilometre) and urban (>1000 inhabitants per square kilometre)
bSize of the school: small (<250 students), medium-sized (250–750 students) and large (>750 students)
For both groups a prerequisite for participation in the study was a digitised and highly qualified absence registration system. All seven intervention schools and seven control schools eventually participated.
Study design and population
Due to the active role of schools in the intervention, as explained above, random assignment of schools to “intervention or control schools” was not an option. Therefore the study had a quasi-experimental design. The intervention group consisted of students who were attending one of the intervention schools, had been identified by the school as having extensive medical absence according to the MASS-criteria, and had been referred to the YHCP during school year 2011–2012. The control group consisted of students who were attending one of the control schools, and who were identified retrospectively in the absence data as having extensive medical absence according to the MASS criteria.
Data collection procedure and outcome measurements
In order to determine the level of medical absence, the school absence registration over the school years 2011–2012 and 2012–2013 was used. All school absence registration systems work by teachers who check per lesson and digitally record the students being present or absent. Partial absences such as going home during the day because of sickness were counted as full-day absences. When still reported sick after autumn, spring, and Christmas breaks, absences counted for new sickness reporting. Due to the shifting of summer holidays, the irregular school hours during the first school week and the examination weeks at the end of the school year, the level of medical absence was calculated only between September 1 and June 9. When the measurement period was (partly) outside this period, the absence rate was recorded as “missing”.
The level of a student’s medical absence was measured as the number of absence periods and absence days reporting sick during the 12 school weeks prior to the three measurement points. To ensure the accuracy of the measurements, to maintain the class conditions for the student the same as much as possible, and to reduce missings (for example as a result of the student moving to another school), a measurement period of 12 school weeks was chosen so that the effects at 12 school weeks’ time could consequently be measured as much as possible in the same school year. For the intervention group, the first measurement point (T0) was the consultation moment with the YHCP. At the end of the consultation written informed consent was obtained from students and parents to participate in the study. For the control group, the first measurement point (T0) was at two pre-defined points in time: December 1 or March 9. These points in time were chosen to avoid missing data in the 12 school weeks’ measurements periods. The data of a student with an extensive absence rate at both points in time were included in December 1. After 3 months (T1) and 12 months (T2) the measurement was repeated. In accordance with the Dutch public health act [37], collection of data to perform anonymous group comparisons does not require prior informed consent.
Statistical analysis
Pearson’s chi-squared tests (for categorical variables) and Student’s t-test (for continuous variables) were used to determine differences in socio-demographic variables between the intervention group and the control group.
Due to the hierarchical structure of the data, with the repeated measurements on medical absenteeism (first level) nested within students (second level) nested within schools (third level), multilevel analysis (linear mixed models in SPSS, version 19.0) [38] was applied for studying differences between the intervention group and the control group in the development of the level of medical absence over time. The intra class correlations [39] were calculated at school and student level. Intervention, time and the interaction between intervention and time were added as fixed factors to the model. Schools and students were defined as random effects.
Results
The intervention group consisted of 493 students (12 % of the total school population of 4159 students) and the control group consisted of 445 students (14 % of the total school population 3153 students). The total study group, including both intervention and control groups, consisted of 938 students, of whom 40 % were male and 60 % female. As shown in Table 3, there is a statistically significant difference between the two groups in gender, age, absence rate in periods, and absence rate in days. The intervention group had a lower proportion of females, a somewhat higher average age, and a lower absence rate in terms of both periods and days (initial values). There was no significant difference in the average number of days per period between the groups.
Table 3.
The selected demographic characteristics and the initial values of medical absenteeism of the intervention and control groups
| Intervention group (493) | Control group (445) | Statistical values | |
|---|---|---|---|
| Gender, % female | 55.8* | 64.3 | χ 2 = 7.01**, df = 1 |
| Age in years, mean (SD) | 14.54 (1.32) | 14.32 (1.28) | t = 2.49* |
| Absence rate in periods per 12 school weeks, mean (SD) | 3.91 (1.62)** | 4.50 (1.16) | t = −6.20** |
| Absence rate in days per 12 school weeks, mean (SD) | 8.40 (5.39)* | 9.92 (5.39) | t = −4.27** |
| Number of days per period | 2.29 (1.53) | 2.39 (1.67) | t = −0.95 |
* p ≤ 0.05; ** p ≤ 0.01
In the intervention group, 170 students (35 %) had been referred to the YHCP before December 1, 226 students (46 %) between December 1 and March 9, and 97 students (20 %) after March 9. In the control group, 335 students (75 %) were included on December 1, and 110 students (25 %) on March 9. Of all students, in 58 % (52 % intervention students and 64 % control students) there was information about all three measurement points. Multilevel analysis showed a statistically significant effect of time on the absence rate in periods (F = 196.0; p ≤ 0.01), and a significant interaction effect (F = 18.4; p ≤ 0.01) in favour of the intervention group. Figure 1 shows that in the intervention group the number of absence periods decreased over time: from 3.9 (95 % CI:3.8–4.1) to 2.5 (95 % CI:2.3–2.6) and finally to 2.2 (95 % CI:2.0–2.4) times reported sick in 12 school weeks. In the control group, the number of absence periods initially decreased from 4.5 (95 % CI:4.3–4.7) to 3.5 (95 % CI:3.3–3.6), after which an increase to 3.7 (95 % CI:3.5–3.9) was measured.
Fig. 1.
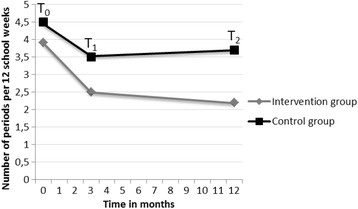
The progress of the absenteeism in number of periods
With respect to the absence rate in total number of days, there was a significant effect of time (F = 56.5; p ≤ 0.01) and a significant interaction effect (F = 11.5; p ≤ 0.01). Again the intervention group scored better than the control group. Figure 2 shows that in the intervention group the total number of absence days in the 12 week period decreased over time: from 8.5 (95 % CI: 7.9–9.1) to 5.7 (95 % CI: 5.0–6.2) to 4.9 (95 % CI: 4.2–5.6) days reported sick. In the control group, the number of absence days initially decreased from 9.9 (95 % CI: 9.3–10.5) to 8.4 (95 % CI: 7.9–9.0) days, after which an increase to 8.9 (95 % CI: 8.2–9.6) was measured.
Fig. 2.
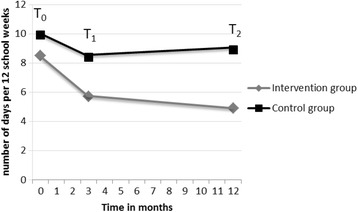
The progress of the absenteeism in number of days. Because of the application of a multilevel model for this part of the analysis, the initial value of 8.5 days differs from the initial value in Table 3
With respect to the number of days per period, there was no significant effect of time (F = 1.0; p > 0.05) and no significant interaction effect (F = 1.3; p > 0.05). Figure 3 shows that in the intervention group the number of days per period remained the same over time: 2.3 (95 % CI: 2.1–2.6) at T0,2.3 (95 % CI: 2.1–2.7) at T1, and 2.3 (95 % CI: 1.9–2.6) at T2. In the control group, the number of days per period increased initially from 2.4 (95 % CI: 2.2–2.6) to 2.7 (95 % CI: 2.4–2.9) days, after which a decrease to 2.5 (95 % CI: 2.3–2.8) was measured.
Fig. 3.
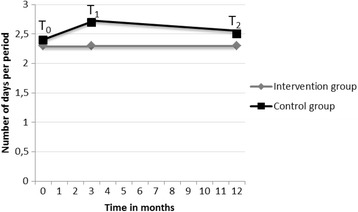
The progress of the absenteeism in number of days per period
A gender effect was found on the absence rate in periods (F = 8.1; p ≤ 0.01), indicating that, in general, girls had a somewhat higher absence rate (3.4) than boys (3.2). For the total number of days no statistically significant difference was found between boys and girls (F = 3.3; p > 0.05). For age no differences were found according to the absence rate in periods (F = 2.0; p > 0.05) and total number of days (F = 0.7; p > 0.05). In addition, no interaction effects were found of gender and time and of age and time on absence rate. The part of the variance that could be attributed to differences between schools was 7 % for the number of absence periods and 12 % for the number of absence days. The part of the variance that could be attributed to the students within schools was 23 % for the number of absence periods and 35 % for the number of absence days.
Discussion
To the best of our knowledge, this was the first study of an intervention for addressing medical absenteeism in which schools and YHCPs collaborated intensively. The objective was to investigate the effects of MASS on students’ medical absenteeism in pre-vocational secondary schools, compared to a situation in which MASS was not applied.
The proportion of students having a high absent rate (four periods in 12 school weeks or more than six consecutive days) was 0.12 within the intervention schools versus a proportion of 0.14 within the control schools. This difference in proportion might be explained by an effect of the intervention at school level: increased awareness of and more attention to sickness reporting may within the school community result in a decrease in medical absenteeism. Moreover, under-identification of intervention students cannot be ruled out. The statistically significant difference between the two study groups related to gender (56 % of the intervention students and 64 % of the control students was male) suggests that schools may be less inclined to refer female students to the YHCP. A statistically significant difference in age between the two groups was also found. However, the actual difference was only 0.22 years (about 2½ months), which seems irrelevant in practice. Since there seemed to be no influence of gender and age on absence over time, probably this selection in the intervention group did not influence our results. The fact that there were more missing data in the intervention group can be explained by the different ways of inclusion between the control and intervention group. However, additional analyses showed no differences in the baseline measurement (as well in days as in periods) between the students with complete data and those with a missing on one of the measurement points.
Although the absence rate of all intervention and control students met one of the MASS-criteria, there were significant differences in the baseline measurements between both groups. This might be due to the way the data was obtained. In the intervention group, the baseline measurement was the consultation moment with the YHCP. The lower baseline absence rate in the intervention group might be explained by the attention and awareness generated by MASS during the time needed to actually meet the YHCP. In the control group, the data for the baseline measurement was close to the moment of meeting one of the criteria and was collected retrospectively. Meanwhile, in the control group there was no systematic attention, as in MASS, in case of an extensive absence rate. Consequently, it is conceivable that a part of the effect of MASS has already been measured at the baseline measurement and therefore cannot generate an effect anymore at follow-up measurements.
The study showed a decrease in the number of absence periods and absence days per 12 school weeks in both groups and in both measurements. The effects were significantly stronger in the intervention group. Regarding the initial decrease after 3 months in both groups, there are three possible interpretations. First, the decrease could (partly) be explained by “regression-to-the-mean” since only students with the highest rates of absenteeism were included in this study. However, the effect measured in the control group is less strong, therefore “regression-to-the-mean” cannot be sustained as the only explanation for the decline. Secondly, the influence of seasonality should be considered because (data of the) students were included at different times: 75.3 % of the intervention students were included before December 1, compared to 34.6 % of the control students. The influence of influenza is almost negligible because, in the Netherlands, in 2011–2012, the prevalence of influenza was extremely low [40]. Paediatric diseases, however, like gastroenteritis, functional complaints and asthma, must be taken into account as they have peaks from November till March [41]. Therefore, the first follow-up measurement in the control group has occurred more often in the peak season. This could explain the lesser decline at the first follow-up measurement in the control group. Thirdly, another reason for the rapid decline of absenteeism in the intervention group after 3 months may be due to the MASS intervention, which generated attention and care.
Regarding the effects after 12 months, it should be noticed that this follow-up measurement took place in the same period as the baseline measurement in both groups. There are two possible interpretations for the different outcomes in both groups. First, seasonality should be considered again. It is likely that seasonal influences of the pediatric diseases have had the same impact on both measurements. However, taking into account that there was a severe flu epidemic in the Netherlands, in 2012–2013, from January to March [40], this could have adversely affected the second follow-up measurement in the intervention group as the measurement was more often during the flu-peak. A difference between the second follow-up measurements can therefore partly be explained by the flu for the benefit of the control group. Secondly, the long-term effect after 12 months may be an effect of MASS. Regarding the number of days per period, no significant effects were found. Our findings are in line with a study of the 12-months effectiveness of an intervention called “SHARP-at work” for reducing recurrent sickness absence in workers with common mental disorders [42]. Arends et al. demonstrated that the intervention had especially an effect on the incidence of recurrent sickness absence.
It is likely that the results can be generalised to a national level. Although a statistically significant part of the variance could be attributed to the school level (7–12 %) the greatest effects were found at the individual student level (25–35 %). The effects that can be expected on other educational levels are uncertain and subject to future research. Strengths of the study are the large sample size and the intervention being rooted in Dutch health care and educational systems. It remains unclear to what extent these results can be generalised internationally, since both public health care and school systems differ substantially across countries.
Medical absence rate was chosen as the central outcome measurement in this study because the absence itself is related to a lower level of education and even school dropout. Consequently, this study provides no definite answers which factors are responsible for the decrease in absence rates that were found in this study. A combination of systematic, and thereby improved, identification of students with extensive medical absenteeism, the school paying more attention to students’ medical absenteeism, and referral to the YHCP, makes students feel that they and their absenteeism are not ignored but taken seriously. This can result in a raised threshold for reporting sick in future because students cannot avoid attention. The decrease in medical absenteeism can also be attributed to the intervention of the YHCP, resulting in more personalised and adequate treatment, care or support: after analysing the great variability of underlying reasons for the absenteeism [43], appropriate care, educational adjustments and adequate support could be arranged by schools and YHCPs in a sustainable manner. As a consequence, students possibly experience fewer (health-related) problems and/or find better ways to deal with their problems. Interventions are already available to handle with absence in cases of specific diseases and problems experienced by the student [2]. Our study showed a relatively high effect at the students’ level. For future research it is recommended to investigate these individual variations: to what extent could the differences in absence trajectories over time be explained by students’ characteristics such as coping behaviour, their social context such as family and peers, the underlying diseases and problems, and to the possible contributions of school, YHCP and health care characteristics. A multicentre prospective study in which intervention and control condition are located in different regions is recommended to further investigate the role of the school and their considerations in referring to the YHCP, to study the effects of the intervention on the care and support initiated by school and health care, and on the satisfaction of students and parents with care and support, and on students’ well-being and health.
Conclusions
The study provides first indications of the added value of personalised management of medical absenteeism, i.e. systematic identification of students with extensive medical absenteeism and consistent referral to the YHCP, compared to “medical absenteeism policy as usual”. The effectiveness of the intervention is demonstrated primarily by a decrease in the number of periods reported sick. MASS seems to be a promising tool in the public health setting for addressing medical absenteeism among students.
Acknowledgements
The authors would like to thank all students and youth health care physicians who participated in this study, and to Winke Swinkels who participated in the data collection.
Funding
This study was funded by ZonMw, the Dutch Organization for Health Research and Development.
Availability of supporting data
The study data is stored by the Faculty of Social and Behavioural Sciences, Tranzo, Tilburg University in The Netherlands following the Institution’s data management policies. Data can be released by researchers in research collaboration based on permission from the steering committee of the study.
Authors’ contributions
All authors contributed to the study design. YV participated in data collection and coordinated the study. JM supported the analysis of this study. All authors contributed to the interpretation of the data. YV drafted the manuscript, the co-authors critically revised the manuscript. All authors have read and approved the final version of this manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The research protocol was approved by the Medical Ethics Committee of the University Hospital Maastricht and Maastricht University (Dossier number 11-4-070.6/ivb). Written informed consent was obtained from students and parents to participate in the study.
Appendix
Box 1 Description of the Dutch educational system.
| The Dutch general educational system is structured as follows (following the International Standard Classification of Education ISCED) [26]: at the age of 12, after primary education, students can choose between three tracks of education, each aiming at a different educational level in secondary school. They can go to pre-vocational secondary education (VMBO: ISCED 2), which is the lowest level, takes 4 years and prepares for intermediate vocational education (MBO: ISCED 3C). The second track in Dutch secondary education is senior general secondary education (HAVO), which takes 5 years and prepares for higher vocational education (HBO). The third track is pre-university education (VWO), which takes 6 years and prepares for studies at university level (academic bachelors and masters). Students can arrange their educational pathways in many ways, by going up or down levels. The levels relate to the degree of complexity of the content of the programme. In addition to general education, in the Netherlands there is also ‘special needs education’, in which the content of the educational programmes designed can be adapted to students’ specific needs. |
Contributor Information
Yvonne T. M. Vanneste, Phone: +31 (0)76-5282000, Phone: +31 (0)6-10540159, Email: y.vanneste@ggdwestbrabant.nl
Jolanda J. P. Mathijssen, Phone: +31 (0)13-4669111, Email: J.J.P.Mathijssen@uvt.nl
Ien A. M. van de Goor, Phone: +31 (0)13-4669111, Email: L.vandeGoor@uvt.nl
Carin M. C. Rots – de Vries, Phone: +31 (0)76-5282000, Email: c.rots@ggdwestbrabant.nl
Frans J. M. Feron, Phone: +31 (0)43-3882262, Phone: +31 (0)6-46892525, Email: f.feron@maastrichtuniversity.nl
References
- 1.Eckstein Z, Wolpin KI. Why youths drop out of high school: the impact of preferences, opportunities, and abilities. Econ Soc. 1999;67(6):1295–1339. [Google Scholar]
- 2.Kearney CA. School absenteeism and school refusal behavior in youth: a contemporary review. Clin Psychol Rev. 2008;28:451–471. doi: 10.1016/j.cpr.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 3.Christenson SL, Thurlow ML. School dropouts: prevention considerations, interventions, and challenges. Am Psychol Society. 2004;13(1):36–39. [Google Scholar]
- 4.Rumberger RW. Why students drop out of school and what can be done. Dropouts in America: how severe is the problem? What do we know about intervention and prevention? Harvard University. 2001;1–45. http://civilrightsproject.ucla.edu/research/k-12-education/school-dropouts/why-students-drop-out-of-school-and-what-can-be-done/rumberger-why-students-dropout-2001.pdf. Accessed 7 Jan 2015
- 5.Traag T, Marie O, Velden Rvd. Risicofactoren voor voortijdig schoolverlaten en jeugdcriminaliteit [Risk factors for school dropout and juvenile delinquency]. http://www.cbs.nl/NR/rdonlyres/131FADA3-2E22-4E51-9A91-6BB53E1E0895/0/2010k2b15p55art.pdf. 2010;55–60. Accessed 26 Feb 2015
- 6.Beckers ITT, Traag T. Met een startkwalificatie betere kansen op de arbeidsmarkt. Sociaaleconomische trends [Better opportunities in the labour market with a basic qualification. Socioeconomic Trends]. The Hague: Statistics, The Netherlands, 2005: 23–28. http://www.cbs.nl/NR/rdonlyres/31B62F76-21E2-40C8-86AB-230589D4F9EA/0/2007k3v4p23art.pdf. Accessed 26 Feb 2015
- 7.Junger-Tas J. Diploma’s en goed gedrag II: Preventie van antisociaal gedrag in het onderwijs [Diplomas and good behaviour II: Prevention of antisocial behavior in education]. The Hague: Dutch Ministry of Justice. 2002; http://onderwijsdatabank.nl/23998/diplomas-en-goed-gedrag-ii/. Accessed 7 Jan 2015.
- 8.Ross CE, Wu C-L. The links between education and health. Am Sociol Rev. 1995;60(5):719. doi: 10.2307/2096319. [DOI] [Google Scholar]
- 9.Galobardes B, Lynch J, Smith GD. Measuring socioeconomic position in health research. Br Med Bull. 2007;81–82:21–37. doi: 10.1093/bmb/ldm001. [DOI] [PubMed] [Google Scholar]
- 10.Droomers M, Schrijvers CTM, Mheen DVD, Mackenbach JP. Educational differences in leisure-time physical inactivity: a descriptive and explanatory study. Soc Sci Med. 1998;47(11):1665–1676. doi: 10.1016/S0277-9536(98)00272-X. [DOI] [PubMed] [Google Scholar]
- 11.Droomers M, Schrijvers CTM, Stronks K, Mheen DVD, Mackenbach JP. Educational differences in excessive alcohol consumption: the role of psychosocial and material stressors. Prev Med. 1999;29(1):1–10. doi: 10.1006/pmed.1999.0496. [DOI] [PubMed] [Google Scholar]
- 12.Thrane Christer C. Explaining educational-related inequalities in health: mediation and moderator models. Soc Sci Med. 2006;62(2):467–478. doi: 10.1016/j.socscimed.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 13.Dahlgren G, Europe WHOWROf. European strategies for tackling social inequities in health: levelling up: WHO Regional Office for Europe; 2006. http://www.euro.who.int/__data/assets/pdf_file/0018/103824/E89384.pdf. Accessed 7 Jan 2015
- 14.Mackenbach JP. Health inequalities: Europe in profile. Tackling health inequalities: governing for health. Rotterdam: European Commission, 2006. http://www.who.int/social_determinants/resources/european_inequalities.pdf Accessed 7 Jan 2015
- 15.Havas J, Bosma H, Spreeuwenberg C, Feron FJ. Mental health problems of Dutch adolescents: the association with adolescents’ and their parents’ educational level. Eur J Public Health. 2009;20(3):258–264. doi: 10.1093/eurpub/ckp172. [DOI] [PubMed] [Google Scholar]
- 16.Kulhánová I, Hoffmann R, Eikemo TA, Menvielle G, Mackenbach JP. Educational inequalities in mortality by cause of death: first national data for the Netherlands. Int J Public Health. 2014;59(5):687–696. doi: 10.1007/s00038-014-0576-4. [DOI] [PubMed] [Google Scholar]
- 17.Bosma H, Mheen DHVD, Borsboom GJJM, Mackenbach JP. Neighborhood socioeconomic status and all-cause mortality. Am J Epidemiol. 2001;153(4):363–371. doi: 10.1093/aje/153.4.363. [DOI] [PubMed] [Google Scholar]
- 18.Huisman M, Kunst AE, Bopp M, Borgan JK, Borrell C, Costa G, et al. Educational inequalities in cause-specific mortality in middle-aged and older men and women in eight western European populations. Lancet. 2005;365(9458):493–500. doi: 10.1016/S0140-6736(05)70273-7. [DOI] [PubMed] [Google Scholar]
- 19.Gathmann C, Jürges H, Reinhold S. Compulsory schooling reforms, education and mortality in twentieth century Europe. Soc Sci Med. 2015;127:74–82. doi: 10.1016/j.socscimed.2014.01.037. [DOI] [PubMed] [Google Scholar]
- 20.Lager ACJ, Torssander J. Causal effect of education on mortality in a quasi-experiment on 1.2 million Swedes. Proc Natl Acad Sci U S A. 2012;109(22):8461–8467. doi: 10.1073/pnas.1105839109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mackenbach JP, Stirbu I, Roskam AJ, Schapp M, Menvielle G, Leinsalu M, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008;358(23):2468–2481. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- 22.Eaton DK, Brener N, Kann LK. Associations of health risk behaviors with school absenteeism. Does having permission for the absence make a difference? J Sch Health. 2008;78(4):223–229. doi: 10.1111/j.1746-1561.2008.00290.x. [DOI] [PubMed] [Google Scholar]
- 23.Scottish Executive National Statistics. Results of pupil attendance and absence for session 2006/7. Edinburgh: The Scottish Government, Statistics. http://www.scotland.gov.uk/Publications/2013/12/4199/17. 2007. Accessed 7 Jan 2015
- 24.Lenzen CFG, Jentzsch A, Kaess M, Parzer P, Carli V, Wasserman D, et al. Schulabsentismus in Deutschland - die Prävalenz von entschuldigten und unentschuldigten Fehlzeiten und ihre Korrelation mit emotionalen und Verhaltensauffälligkeiten [School absenteeism in Germany: prevalence of excused and unexcused absenteeism and its correlation with emotional and behavioural problems] Prax Kinderpsychol Kinderpsychiatr. 2013;62(8):570–582. doi: 10.13109/prkk.2013.62.8.570. [DOI] [PubMed] [Google Scholar]
- 25.NIPO het marktonderzoeksinstituut. Rapport: Schoolverzuim in het Voortgezet Onderwijs [Report on school absenteeism in secondary school]. Amsterdam, 2002. Available at: http://www.tns-nipo.com/pages/persvannipo/pdf/schoolverzuim03.pdf. Accessed 7 Jan 2015.
- 26.UNESCO Institute for Statistics, Canada. ISCED Fields of Education and Training 2013 (ISCED-F 2013). United Nations International Family of Economic and Social Classifications. Manual on the International Standard Classification of Education (ISCED). Re-edition. ©UNESCO-UIS Montreal, Canada. 2014. http://www.uis.unesco.org/Education/Pages/international-standard-classification-of-education.aspx. doi:http://dx.doi.org/10.15220/978-92-9189-150-4-en Accessed 22 Sep 2015
- 27.Jones R, Hoare P, Elton R, Dunhille Z, Scharpe M. Frequent medical absences in secondary school students: survey and case–control study. Arch Dis Child. 2009;94:763–767. doi: 10.1136/adc.2008.140962. [DOI] [PubMed] [Google Scholar]
- 28.Looze Md, Dorsselaer Sv, Roos Sd, Verdurmen J, Stevens G, Gommans R, et al. Gezondheid, welzijn en opvoeding van jongeren in Nederland [Health, well-being and upbringing of young people in the Netherlands]. Utrecht: Trimbos Instituut, 2014. ISBN: 978-90-5335-914-3. http://dspace.library.uu.nl/bitstream/handle/1874/305481/09.pdf?sequence=1: HBSC. Accessed 7 Jan 2015.
- 29.Schrijvers C, Schoemaker CG. Spelen met gezondheid: leefstijl en psychische gezondheid van de Nederlandse jeugd [Playing with health: lifestyle and mental health of the Dutch youth]. Bilthoven: RIVM, 2008. http://hdl.handle.net/10029/262070. Accessed 7 Jan 2015.
- 30.Groeneveld MJ, Steensel KMv, Herben B, et al. Kenmerkend vmbo: een vergelijkend onderzoek naar de kenmerken van vmbo-leerlingen en de ‘generatie Einstein’. [Characteristics pre-vocational secondary education: a comparative study of the characteristics of pre-vocational secondary students and the ‘Einstein generation’]. Hilversum: Hiteq, 2008, http://www.hiteq.org/Hiteq/Downloads/Publicaties%20geheel/Kenmerkend%20vmbo.pdf. Accessed 7 Jan 2015.
- 31.Neut Ivd, Teurlings C, Kools, Q. Inspelen op leergedrag van vmbo-leerlingen [Responding to learning behaviour of pre-vocational secondary students]. http://www.aanvalopschooluitval.nl/userfiles/file/CPB_rapport.pdf Tilburg: IVA., 2005. Accessed 7 Jan 2015
- 32.Traag T, Velden RKWvd. Early school-leaving in the Netherlands. The role of student-, family- and school factors for early school-leaving in lower secondary education. Research Centre for Education and the Labour Market. http://arnop.unimaas.nl/show.cgi?fid=10250 Accessed 29 Mar 2015
- 33.Vanneste YTM, Rots-de Vries MC, Goor LAMVD, Feron FJM. Medische Advisering van de Ziek gemelde Leerling. Ontwikkeling van een interventie [Medical Advice for Students reported Sick. Development of an intervention] TSG. 2012;90(7):412–419. doi: 10.1007/s12508-012-0145-2. [DOI] [Google Scholar]
- 34.Hawkrigg S, Payne DN. Prolonged school non-attendance in adolescence: a practical approach. Arch Dis Child. 2014;99:954–957. doi: 10.1136/archdischild-2013-304595. [DOI] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. [Prevention and Control of Influenza]. MMWR 2008;57(No. RR-7):[5]. http://www.cdc.gov/flu/professionals/acip/clinical.htm Accessed 26 Jan 2016
- 36.Daponte A, Bernal M, Bolívar J, Mateo I, Salmi L-R, Barsanti S, et al. Criteria for implementing interventions to reduce health inequalities in primary care settings in European regions. Eur J Pub Health. 2014;24(6):979–989. doi: 10.1093/eurpub/cku044. [DOI] [PubMed] [Google Scholar]
- 37.Dutch public health law. http://www.wetten.overheid.nl. Accessed 26 Jan 2016
- 38.Twisk JWR. Applied multilevel analysis: a practical guide for medical researchers. Cambridge University Press. 2006
- 39.Shek DTL, Ma CMS. Longitudinal data analyses using linear mixed models in SPSS: concepts, procedures and illustrations. Sci World J. 2011;11:42–76. doi: 10.1100/tsw.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Institute for Public Health and the Environment. http://www.rivm.nl/Onderwerpen/G/Griep Accessed 26 Jan 2016
- 41.Schrijver TV, Brand PLP, Bekhof J. Seasonal variation of diseases in children: a 6-year prospective cohort study in a general hospital. Eur J Pedatrics. 2015 doi: 10.1007/s00431-015-2653-y. [DOI] [PubMed] [Google Scholar]
- 42.Arends I, van der Klink JJL, van Rhenen W, de Boer MR, Bültmann U. Prevention of recurrent sickness absence in workers with common mental disorders: results of a cluster-randomised controlled trial. Occup Environ Med. 2014;71:21–29. doi: 10.1136/oemed-2013-101412. [DOI] [PubMed] [Google Scholar]
- 43.Vanneste YTM, Mathijssen JJP, van de Goor LAM, Rots-de Vries MC, Feron FJM. Extensive medical absenteeism among secondary school students: an observational study on their health condition from a biopsychosocial perspective. Open J Prev Med. 2015;5:111–121. doi: 10.4236/ojpm.2015.53013. [DOI] [Google Scholar]


