Abstract
Introduction:
Several commercially available luting agents are used to cement the dental restorations such as intra-coronal, extra-coronal, and fixed partial dentures. Tensile bond strength (TBS) and accurate marginal fit are the essential factors to determine the good clinical results in fixed prosthesis. The retentivity of the luting cements is assessed by their adhesive capacity over the tooth surface and metal surface. Generally, the adhesive ability has been evaluated with in vitro testing, with tensile bond tests. The failure of fixed prosthesis may be happened as a result of incomplete seating during cementation. Most research on cementation of crowns relates seating failure to the thickness of the cement film.
Materials and Methods:
The study is divided into four groups with 10 samples for each of the luting cement taken up for testing TBS and four groups with 5 samples for each luting agent chosen for assessing marginal fit. The results were tabulated and statistically analyzed.
Results:
In this in vitro study, the TBS of luting cements, and marginal fit in relation to luting cements were tested by using appropriate testing devices. The TBS of cement is measured using universal testing machine, and the results are tabulated. The marginal gap that exists between the margin of the cast metal crown, and the finish line is measured using travelling microscope before and after cementation. The difference between these two values gives the discrepancy that is due to the film thickness of cement used for luting the restoration.
Summary and Conclusion:
The TBS value of zinc phosphate cement and glass ionomer cement were found to be almost same. The chemical adhesiveness of the glass ionomer with calcium ions of enamel and dentin may be the attributed reason (ionic bonding). In this study, the polycarboxylate is the one that showed low TBS, and it may be attributed to the weakness of the cement due to reduced film thickness, though this cement has a chemical bonding nature. The observation of results of marginal fit in this study is the increased gap found in zinc phosphate cement followed by resin cement, zinc polycarboxylate, and glass ionomer cement. It is agreeable to estimate the marginal fit of the restoration, which could be affected by the film thickness of the luting cement along with other factors.
KEY WORDS: Crown retentivity, dental cements, marginal discrepancy, microleakage
The complete veneer restorations as an individual restoration or a component of fixed partial prosthesis play a vital role in the field of prosthetic dentistry. The clinical success of fixed prosthesis also depends upon the luting agent and the proper cementation procedure. Dental cement must be used as a barrier against microbial leakage, sealing the interface between the tooth and restoration and holding them together through some form of surface attachment.[1] This attachment may be mechanical, chemical, or combination of both.[2]
Zinc phosphate cement has been the most widely used luting agent,[3] in spite of its some well-documented disadvantages, including high solubility in saliva, lack of chemical bonding, and low setting pH. Polycarboxylate cement set by a fast acid-base reaction.[1] After hardening, polycarboxylate cements exhibit significantly greater plastic deformation and is not well suited for use in regions of high masticatory stress or in the cementation of long span prosthesis.[4] The strongest clinical merit of this cement is its biocompatibility with the dental pulp.
Glass ionomer cements adhere to tooth structure by formation of ionic bonds at the tooth-cement interfaces. They exhibit higher compressive strength than zinc phosphate cement.[5,6] The major shortcoming of this cement is its susceptibility to water and saliva, if exposed, during the initial setting period.
Resin cements invited the attention of dental professionals due to their excellent bonding ability.[7] Composition of resin cement is filled BIS-GMA resin and other methacrylates.[8] They polymerise through chemically initiated mechanisms, photo polymerization or combination of both. The ability to adhere to multiple substrates, high strength, insolubility in the oral environment, and shade matching potential have made resin cements the adhesive of choice for esthetic type restorations and specifically recommended for luting base metal resin-bonded fixed partial dentures (”Maryland” type).[9]
Aims and Objectives
To evaluate and compare the retentive ability of different luting cements used in fixed Prosthodontics.
To evaluate and compare the marginal adaptation of cast metal restoration in relation to different luting cements.
Materials and Methods
This study was performed to evaluate the tensile bond strength (TBS) and marginal fit of cast metal restoration[10] in relation to four different types of luting agents in use,[11] namely (1) Zinc phosphate - Harvard, Dental Gmbh, Berlin, (2) Zinc polycarboxylate - Heraeus Kulzer FmbH and Co., Hanau, Germany, (3) Glass ionomer GC Fuji 1 radio opaque luting agent, GC, Corp., Tokyo, Japan, (4) Resin cement - multilink, Ivoclar Vivadent, Italy).
Sixty samples were prepared totally for the proposed study and ten samples were allotted for each luting agent to test the TBS (Group I). Similarly five samples were allotted for each luting agent to test marginal fit (Group II).
Preparation of sample
Sixty recently extracted caries free maxillary first premolar teeth of approximately similar sizes were selected, cleaned, and stored in distilled water. The teeth were mounted in the auto polymerizing acrylic resin block measuring 1 cm × 1 cm × 4 cm. The teeth were embedded in the acrylic block 2 mm below the cement enamel junction.
Tooth preparation
The mounted teeth were prepared following the principles of tooth preparation. All the dimensions were predetermined to achieve the standardization of the preparation. Flat occlusal reduction, 6° convergences axially, chamfer finish line, height of the crown is 5 mm, buccolingual width is 5 mm, and mesiodistal width is 4 mm.
Impression making and die fabrication
Impressions of prepared teeth were made with polyvinyl siloxane impression material (virtual putty and light body regular set, ivoclar vivadent, AG, FL 9494 Schaen/Liechtenstein) by double impression technique. Cast was poured with Type IV dental stone (Heraeus Kulzer, FmBh and Co., Hanau, Germany).
Preparation of wax pattern and casting
After applying die spacer, wax pattern was fabricated in a usual manner. A sprue of 2 cm length was attached to enhance the retention of cast crown in the acrylic resin block. Patterns were invested and cast with Nickel – chromium alloy (CB-80, Dentsply/Sankin). Castings were devested and sandblasted with 50 µ aluminum oxide. After verifying the fit, they were finished and polished.
Grouping the samples
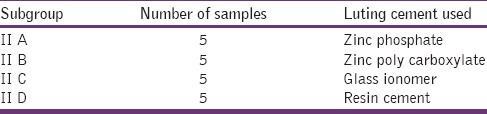
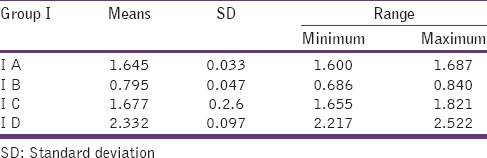
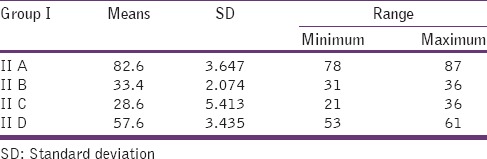
Ten samples were allotted to each luting agent in Group I, and totally forty samples were prepared [Table 1]. Five samples were allotted to each luting agent in Group II and totally twenty samples were prepared [Table 2].
Table 1.
Group I: Used to test tensile bond strength
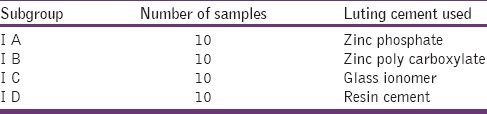
Table 2.
Group II: Used to test the marginal fit
Testing procedure
Group I samples were luted with corresponding cements according to manufacturer's instructions.
Group II samples were evaluated under traveling microscope and the marginal gap that exists between the metal margin and finish line was measured. Then, all the samples were luted with corresponding cements under standard conditions according to manufacturer's instructions.
After cementation, samples were soaked in distilled water for 48 h at 36°C.[7]
Measuring tensile strength
In Universal Testing Machine (Lloyd's Universal Testing Machine), one end of the sample was held at one arm and the other end to the other arm [Figure 1]. The load applied was in the speed of 0.5 mm/min. The tensile load at which the crown detached from the prepared tooth was measured. Using this load value and measured surface area of tooth, the TBS was calculated.
Figure 1.
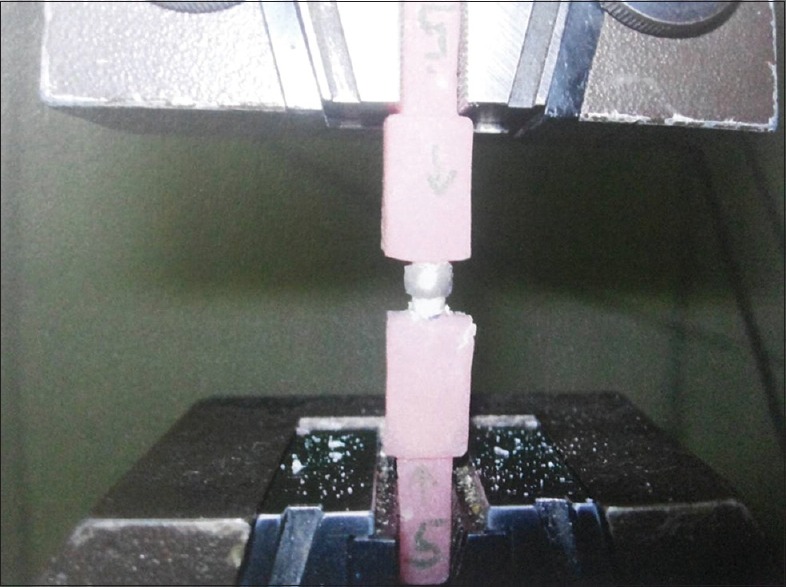
Testing tensile bond strength using universal testing machine
Measuring the marginal fit
The samples were focused under the eyepiece of traveling microscope [Figure 2].[12] The distance from finish line and metal margin was measured, which gives marginal gap value after cementation.[13]
Figure 2.
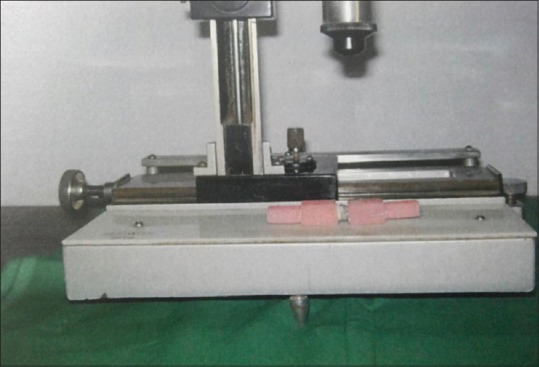
Measuring marginal gap using traveling microscope
Results
In this in vitro study, the TBS of luting cements, and marginal fit in relation to luting cements were tested by using appropriate testing devices. The results of the tests were obtained and calculated and analyzed.
Tensile bond strength
In this study, the TBS of cement is measured using universal testing machine and the results are tabulated. The testing machine gives the value of the force to pull (in newtons), which is converted to KgF by using the following formula:
N/10.2 = KgF (1)
After converting to kg units, the TBS is measured using the formula:
TBS (kg/cm2) = Load (kg)/surface area (cm2) (2)
The kg/cm2 is converted to Mpa using the formula:
Tensile strength (MPa) = Tensile strength (kg/cm2) × 0.09807 (3)
Where 0.09807 is a constant for the conversion.
Substituting all the values, the TBS is calculated, and the results are tabulated [Table 3].
Table 3.
Tensile bond strength: Means and standard deviations of four different types of luting agents
Marginal gap
The marginal gap that exists between the margin of the cast metal crown and the finish line is measured before and after cementation. The difference between these two values gives the discrepancy that is due to the film thickness of cement used for luting the restoration. The values were measured and the results tabulated [Table 4].
Table 4.
Marginal gap: Means and standard deviations of four different types of luting agents
The results were analyzed using two statistical analysis tests:
One-way ANOVA test – to compare between groups [Tables 5 and 6]
Hukey – honest significant difference test– to assess the significant difference between and within groups [Tables 7 and 8].
Table 5.
Analysis of variance Groups I A to I D
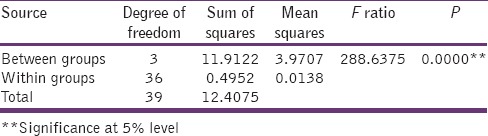
Table 6.
Analysis of variance Groups II A to II D
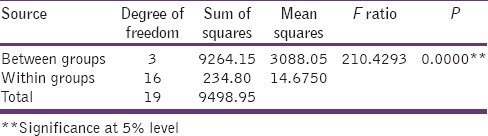
Table 7.
Tukey: Honest significant difference test Groups I A to I D
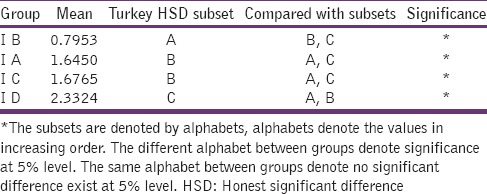
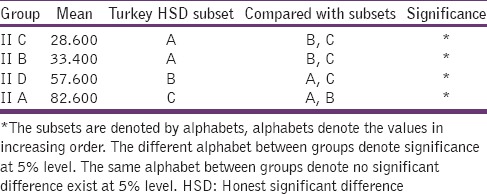
Table 8.
Tukey: Honest significant difference test Groups II A to II D
Interpretation of Results
Tensile bond strength
One-way ANOVA test
Table 3 shows the means and standard deviations of TBS values of Group I. Group I D shows the highest value of 2.332 and Group I B shows the lowest value of 0.795.
Null hypothesis
The Tensile Bond Strength values of Group IA –ID are equal. Since the P value is less than 0.001, the assumed null hypothesis is rejected and so there exists a significant difference between the bond strength of cements.
Tukey – Honest Significant Difference test
In this test, the subsets are denoted by alphabets. The alphabets used to denote the value in increasing order. This means, the different alphabets between groups denote significance at 5% level.
Hence, this study implies that the resin cement has the highest TBS when compared with other cements, when the zinc poly carboxylate cement has the least strength.
Marginal fit
One-way ANOVA test
The null hypothesis
the marginal gap difference values of Group II A – II D are equal. Since P value is <0.001, null hypothesis is rejected and shows that there exists a significant difference between groups. Hence, by comparing the marginal gap due to luting cements, there exists a significant difference between groups.
Tukey – Honest Significant Difference test
This study implies that zinc poly carboxylate and glass ionomer cement have the least film thickness, whereas the zinc phosphate has the highest film thickness.
Discussion
The retentivity of cast metal restorations depends upon many factors such as clinical crown length, buccolingual dimension, taper of the preparation, morphology of tooth, and the cement used to fix the restoration. In this study, the retentivity and the marginal fit of cast crown is assessed by testing TBS using different types of luting agents that are readily available.
The four commercially available luting agents[14] used in this study are as follows: Zinc phosphate cement, zinc polycarboxylate cement, glass ionomer cement, and resin cement. According to ADA specification number 8,[15] Type I materials with film thickness <25 µm are “designed for the accurate seating of precision appliances and for other uses.” The materials included in this group are glass ionomer, zinc phosphate, and poly carboxylate. ADA Type II can have maximal film thickness of 40 µm. These are “recommended for all uses except the cementing of precision appliances.” The materials in this group are resins and glass ionomer resinous hybrids.
In this study, it is found that the film thickness of resin cement is increased, and it could be attributed to the factors which influence the film thickness of luting material such as substrate that the material tested against, the size or shape of filler particles, viscosity of unset material and its rate of set.
Dellabona and van noort 1998 to Nayakar et al.[2] stated that the shear tests were the most efficient to find out the cohesive resistance of the material, whereas tensile tests were appropriate to estimate the adhesion at the interface. Moreover, shear tests are strongly influenced by mechanical properties. The purpose of this study is to evaluate the adhesive capacity of the luting material rather than the stress produced during function; hence, a tensile bond test is performed. Zidan and Ferguson[16] that the taper of crowns had significant effect on retention. The samples are prepared of uniform dimensions with taper of 6°. The highest values for retentivity are measured with 6° taper. The configuration of finish line of the preparation affects the width of the band of cement exposed to oral fluids. Shoulder finish lines exposed more amount of cementing agent at the cervical margin, which also influences the fit of the restoration. Gavelis et al.[17] describes when chamfer finishing margin is used, the exposure of cementing agent decreases according to its inclination.
Pilo[18] said “to fulfill the requirements for an ideal restoration, this must be made to fit the prepared tooth intimately.” The difficult process is the excess cement trapped between the restoration and occlusal surface of tooth to be allowed to escape to achieve proper fit of the restoration. Most research on cementation of crowns relates seating failure to the thickness of cement film.
White et al.[19] assessed the microleakage of various luting systems. They found out that polycarboxylate exhibited microleakage at casting/cement interface, tooth/cement interface, and within the cement layer. In any stressed situation, the weakest link breaks first and thus polycarboxylate shows minimal strength. According to White, the film thickness of zinc phosphate cement was found to be more as compared to other luting cements. This high value of zinc phosphate cement may be attributed to the increased viscosity of cement. In relation to film thickness, the hydrostatic pressure was also increased along with film thickness.[20] Thus, it was concluded that internal pressure plays an appreciable role in preventing the complete seating of the cast crown.
The result of this in vitro study shows that zinc phosphate and glass ionomer cements exhibit almost similar values 1.64 MPa and 1.67 MPa, respectively. Resin cement is found to be the strongest one with the value of 2.33 MPa, and the zinc polycarboxylate was the least one with 0.79 MPa. The highest value of resin cement is quiet understandable because of its bonding ability to tooth structure and metal surface. This could be attributed to the chemical nature of the cement to achieve micromechanical bonding,[21] which is not observed in other luting agents selected for this study.
The TBS value of zinc phosphate cement and glass ionomer cement was found to be almost same. The chemical adhesiveness of the glass ionomer with calcium ions of enamel and dentin may be the attributed reason (ionic bonding). In this study, the polycarboxylate is the one that showed low TBS, and it may be attributed to the weakness of the cement due to reduced film thickness, though this cement has a chemical bonding nature.
Although the film thickness of zinc phosphate is found to be high when compared to other cements, despite its lack of chemical bonding with tooth structure, this cement exhibits fairly good TBS. This appreciable bond strength of zinc phosphate cement could be attributed to other mechanical properties of this cement with mechanical retention to tooth and metal surface. The friction grip is the one which is very much useful in retaining the restoration intact and this tensofrictional retention is facilitated by this zinc phosphate cement due to its enhanced mechanical properties.
The observation of results of marginal fit in this study are the increased gap found in zinc phosphate cement followed by resin cement, zinc polycarboxylate, and glass ionomer cement. It is agreeable to estimate the marginal fit of the restoration, which could be affected by the film thickness of the luting cement along with other factors. Despite increased marginal gap, the zinc phosphate cement exhibit fairly good TBS because of its mechanical properties. Resin cement is the next one to expose more marginal gap but lesser than zinc phosphate. Even though, the marginal fit is not so perfect, this cement exhibits high TBS as compared to other cements. This better result may be attributed to its chemistry with micromechanical retention.
Future studies have to be conducted with a model that closely resembles the oral environment and simulates the functional movements of the mandible. Laboratory tests play an important role to determine physical and chemical characteristics of the materials used. The results of the study should be related to the clinical situation to enable the dental professionals to go for clinical evaluations of these materials.
Summary and Conclusion
The strength of the cement joint is the function of the quality of the bond and other mechanical properties of the cements. This study was performed to evaluate the TBS and marginal fit of different types of luting cements used in clinical practice. From the observation of results of this study, it was found that failure of cemented restorations may be attributed to fracture of the cement, microleakage that can result from poor cementation technique and poor casting fit and weak cements.
Within the limitation of this in vitro study, the following conclusions are made:
Zinc phosphate cement and glass ionomer cement exhibited almost similar values as far as tensile test is concerned. Resin cement had shown comparatively a high value than other cement included in this lists
Zinc polycarboxylate cement, though found to have least TBS, it possess good marginal fit when compared with other luting agents
Zinc phosphate had comparable TBS, but due to its increased film thickness, marginal fit discrepancy was found to be higher
Glass ionomer cement had better TBS and low film thickness, with its adhesive ability makes it a good luting agent
TBS of resin cement was found to be superior when compared to other luting agents, despite of its increased film thickness next to zinc phosphate cement.
When observing the results of the study, we conclude that the resin cement has higher bond strength and better marginal fit, when compared to other luting agents.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Dr. C. Thulasingam, professor and HOD, Department of Prosthodontics, Tamil Nadu Government Dental College.
References
- 1.Nayakar RP, Patil NP, Lekha K. Comparative evaluation of bond strengths of different core materials with various luting agents used for cast crown restorations.J Indian Prosthodont Soc. 2012 Sep;12(3):168–74. doi: 10.1007/s13191-012-0127-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fonseca RG, Dos Santos Cruz CA, Adabo GL, Vaz LG. Comparison of the tensile bond strengths of cast metal crowns luted with resin cements. J Oral Rehab. 2004;31(11):1080–4. doi: 10.1111/j.1365-2842.2004.01345.x. [DOI] [PubMed] [Google Scholar]
- 3.Zidan O, Ferguson GC. The retention of complete crowns prepared with three different tapers and luted with four different cements. J Prosthet Dent. 2003;89(6):565–71. doi: 10.1016/s0022-3913(03)00182-3. [DOI] [PubMed] [Google Scholar]
- 4.Diaz Arnold, Vargas MA, Haselton DR. Current status of luting agents for fixed prosthodontics. J Prosthet Dent. 1999;81:135–41. doi: 10.1016/s0022-3913(99)70240-4. [DOI] [PubMed] [Google Scholar]
- 5.Strang R, Whitters CJ, Brown D, Clarke RL, Curtis RV, Hatton PV, Ireland AJ, et al. Dental Materials: 1996 literature review Part 2. J Dent. 1998;26(4):273–91. doi: 10.1016/s0300-5712(97)00064-x. [DOI] [PubMed] [Google Scholar]
- 6.Craig RG. Restorative Dental Materials. 10th ed. St. Louis: CV Mosby; 1997. pp. 17–84. 201. [Google Scholar]
- 7.Mojan P, Kaltio R, Feduik D, Hawbolt EB, MacEntee MI. Short term contamination of luting cements by water and saliva. Dent Mater. 1996;12:83–7. doi: 10.1016/S0109-5641(96)80073-X. [DOI] [PubMed] [Google Scholar]
- 8.Wu JC, Wilson PR. Review. Resin luting cements for full coverage restorations. Aust Prosthodont J. 1994;8:55–63. [PubMed] [Google Scholar]
- 9.White SN, Yu Z. Compressive and diametral tensile strengths of current adhesive luting agents. J Prosthet Dent. 1993;69(6):568–72. doi: 10.1016/0022-3913(93)90283-t. [DOI] [PubMed] [Google Scholar]
- 10.White SN, Zhokun Yu. Film thickness of new adhesive luting agents. J Prosthet Dent. 1992;67:782–5. doi: 10.1016/0022-3913(92)90582-u. [DOI] [PubMed] [Google Scholar]
- 11.Gorodovsky S, Zidan O. Retentive strength, disintegration and marginal quality of luting cements. J Prosthet Dent. 1992;68(2):269–74. doi: 10.1016/0022-3913(92)90328-8. [DOI] [PubMed] [Google Scholar]
- 12.Vahidi F, Egloff ET, Panno FV. Evaluation of marginal adaptation of all-ceramic crowns and metal ceramic crowns. J Prosthet Dent. 1991;66(4):426–31. doi: 10.1016/0022-3913(91)90499-m. [DOI] [PubMed] [Google Scholar]
- 13.Tregaskes JN, Wohlford JM. Tensile strength of three bonding agents for resin-bonded prostheses. J Prosthet Dent. 1989;62(1):14–7. doi: 10.1016/0022-3913(89)90038-3. [DOI] [PubMed] [Google Scholar]
- 14.White SN, Sorenson JN, Kang SK. Microleakage of new crown and fixed partial denture luting agents. J Prosthet Dent. 1992;67:156–61. doi: 10.1016/0022-3913(92)90447-i. [DOI] [PubMed] [Google Scholar]
- 15.Moody CR, DeWald JP, Ferracane JL. Comparative study of luting agents with composite resin cores. J Prosthet Dent. 1989;62(5):527–9. doi: 10.1016/0022-3913(89)90072-3. [DOI] [PubMed] [Google Scholar]
- 16.Davis SH, Kelly JR, Campbell SD. Use of an elastomeric material to improve the occlusal and marginal seal of cast restorations. J Prosthet Dent. 1989;62(3):288–91. doi: 10.1016/0022-3913(89)90334-x. [DOI] [PubMed] [Google Scholar]
- 17.Abbate MF, Tjan AH, FoxWM Comparison of the marginal fit of various ceramic crown systems. J Prosthet Dent. 1989;61(5):527–31. doi: 10.1016/0022-3913(89)90270-9. [DOI] [PubMed] [Google Scholar]
- 18.Pilo R, Cardash HS, Baharow H. Incomplete seating of cement crowns: a literature review. J Prosthet Dent. 1988;59(4):429–33. doi: 10.1016/0022-3913(88)90037-6. [DOI] [PubMed] [Google Scholar]
- 19.Assif D, Antopolski B, Helft M, Kadde I. Comparison of methods of clinical evaluation of the marginal fit of complete cast gold crowns. J Prosthet Dent. 1985;54(1):20–4. doi: 10.1016/s0022-3913(85)80062-7. [DOI] [PubMed] [Google Scholar]
- 20.Smith DC. Dental Cements: Current status and future prospects. Dent Clin North Am. 1983;6:763–92. [PubMed] [Google Scholar]
- 21.Gavelis JR, Morency JD, Riley ED, Sozio RB. The effect of various finish line preparations on the marginal seal and occlusal seat of full crown preparations. J Prosthet Dent. 1981;45(2):138–45. doi: 10.1016/0022-3913(81)90330-9. [DOI] [PubMed] [Google Scholar]


