Abstract
Radiopaque lesions of the jawbones are frequently encountered in dental radiographs. A variety of conditions such as chronic inflammation, soft tissue calcifications, fibrosseous lesions, odontogenic tumors, and bone neoplasms can manifest as radiopaque lesions on the jawbones. These radiopaque lesions are often difficult to distinguish from each other, hence making the formulation of differential diagnosis challenging. A thorough patient's history and clinical examination supplemented by appropriate investigations will enable the clinician in narrowing down the differential diagnosis and to identify the condition accurately. Presented here is a case of the large radiopaque lesion on posterior mandible surrounded by lytic areas in a 20-year-old male patient.
KEY WORDS: Fibro-osseous lesion, mandible, odontome, ossifying fibroma, radiopaque lesions
Radiopaque lesions of jaws are frequently encountered in the practice of diagnostic oral and maxillofacial radiology. Various normal anatomic landmarks in the maxillofacial region, as well as numerous pathologies, however may produce these radiopacities. The spectrum of pathologies is diverse and includes a variety of conditions. The differential diagnosis of a radiopacity in jawbones has to be made considering local and generalized manifestations.
Case Report
A 20-year-old male patient came to Department of Oral Medicine and Radiology, Rajah Muthiah Dental College and Hospital with a complaint of swelling in the left lower jaw, since 6 months. Patient revealed that the swelling gradually increased in size to attain the present status. It has become symptomatic for the past 10 days with the onset of a mild, intermittent and nonradiating type of pain. His medical, dental, and family histories were not contributory.
Extraoral examination revealed facial asymmetry due to a well-defined, swelling over the left body of the mandible [Figure 1]. It measures approximately 4 cm × 3 cm in size and is roughly oval in shape. It extended superiorly to the level of ala-tragal line and inferiorly extending 1 cm beyond lower border of the body of the mandible. Medially it extends 2 cm from the corner of the mouth and laterally to the posterior border of the ramus of the mandible. On palpation, the swelling was tender, hard in consistency, immobile and skin over the swelling is pinchable. Regional lymphadenopathy was not evident.
Figure 1.

A well-defined swelling in the left body of the mandible
Intra-oral examination revealed single well-defined swelling with bicortical expansion extending anteroposteriorly from 36 to retromolar area [Figure 2]. On palpation, the swelling was tender, hard in consistency and immobile. There was no pus discharge or any secondary changes. Third molars in all the four quadrants were clinically absent. Teeth in the region were normal and showed no evidence of displacement of 36 and 37.
Figure 2.
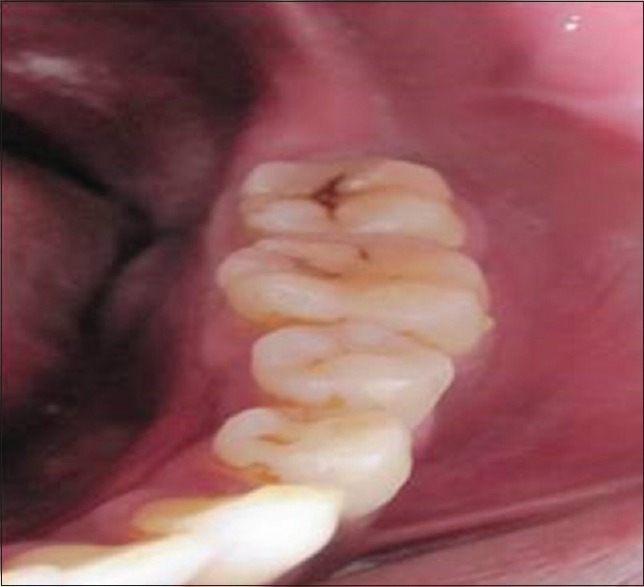
Intraoral view reveals a bicortical expansion
A painless, well defined, slow growing, bony hard swelling, with bicortical expansion located in the posterior aspect of the mandible, apparently not related to the neighboring teeth is suggestive of a bony neoplastic swelling and was provisionally diagnosed as ossifying fibroma (OF).
Investigations performed were intraoral radiographs, orthopantomogram and computed tomography (CT). Intraoral periapical radiograph in relation to 36 region showed a radiopaque mass surrounded by a radiolucent area [Figure 3]. Periodontal ligament (PDL) is seen to be continuous, and lamina dura was found intact. Root resorption or tooth displacement was not evident. An occlusal view revealed a uniform bicortical expansion which was further confirmed on CT examination [Figure 4].
Figure 3.
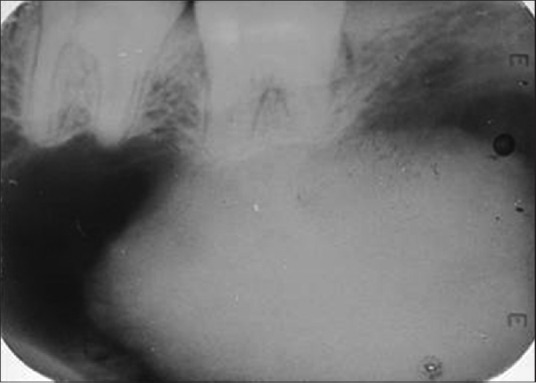
Intraoral periapical showed a radiopaque mass surrounded by a radiolucent area
Figure 4.

Occlusal view revealed bicortical expansion
Panoramic radiograph showed a well-defined radiopaque lesion measuring 4 cm × 3 cm in diameter surrounded by a radiolucent area [Figure 5]. There was inferior cortical bowing and thinning.
Figure 5.
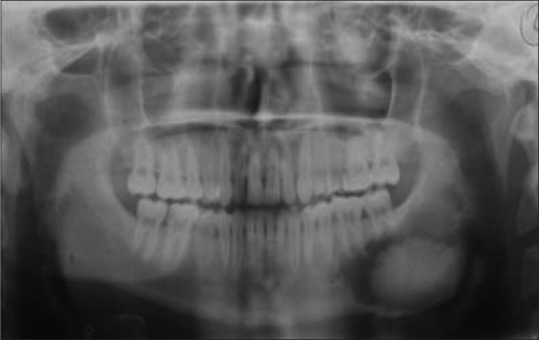
Orthopantomogram shows a lesion in left posterior mandible
The CT scan in axial and coronal sections showed an oval hyperdense mass with central attenuation of 1358 HU [Figure 6a and b]. Periphery was surrounded by a uniform hypodense area with 14 HU. In coronal sections, the mandibular canal was evident on the superiolateral aspect of the mass, suggesting a tumor of nonodontogenic origin [Figure 6a].
Figure 6.

(a) Axial and (b) coronal section of computed tomography reveals a hyperdense mass surrounded by a hypodense mass
Surgical excision of the mass was done under general anesthesia by placing submandibular incision. After excision, the bony wall of the cavity was curetted thoroughly to ensure that no remnants of the lesion were left out. The osseous specimen was submitted for histopathological examination.
Histopathologically, the tissue section revealed stromal tissue containing acellular fibrous connective tissue with numerous spindle fibroblasts. It also showed globular masses of cementum-like calcifications. The final diagnosis was given as OF. The patient is under regular follow-up with no signs recurrence.
Discussion
Fibro-osseous lesions are characterized by the replacement of bone by cellular fibrous tissue containing foci of mineralization that vary in amount and appearance. According to the 2005 edition of WHO classification for odontogenic tumors, fibro-osseous lesions were divided into two categories, osseous neoplasm, and nonneoplastic bone lesions; cementifying OF being included in the former category. However, the term “cementifying ossifying fibroma” was reduced to OF in this edition of WHO classification.[1]
OF is a well demarcated benign fibro-osseous tumor composed of metaplastic bone, fibrous tissue and varying amounts of osteoid. It arises from the periodontal membrane, which contains multipotential cells that are capable of forming cementum, lamellar bone, and fibrous tissue.[2] Pimenta et al. reported association of a new tumor suppressor gene (HRPT2) mutation with OF and suggested that these lesions could arise as a result of haploinsufficiency of the precursor gene.[3]
OF is divided into conventional and juvenile clinicopathologic types. Conventional variant is usually slow growing, expansile, painless with the possibility of root resorption and displacement,[4] this is not seen in our case. Juvenile type, although benign presents as an aggressive neoplasm with invasion into the adjacent bones and bears a tendency to recur. It is commonly seen in young children and adults.[5]
The pathological nature is not clearly understood. The proximity to the PDL has led to a presumption that cemento-ossifying fibroma (COFs) originate in the PDL with the potential for both osseous and cemental differentiation.[6] OF generally occurs in young and middle-aged adults and has a marked predilection for females. It commonly occurs in the mandible with 75% cases in the ramus region and 25% in the posterior mandibular region. Clinically, OF usually presents as a round or ovoid, expansile, painless, and slow-growing well-demarcated lesion in jaws.[2] In 20% of cases, pain and numbness are noted.
Radiographically, early lesions are small and radiolucent. As they mature, they will appear as a mixed lesion with the radiolucent and radiopaque components. Completely mature lesions are predominantly radiopaque. OF expands slowly and centrifugally, creating a well-defined circular or oval shaped mass, usually with sclerotic borders. The degree of ossification is variable, and they may have a “ground glass” or mixed, radiographic appearance depending on the maturity of the lesion. Other findings such as displacement of teeth, root resorption, expansion, and thinning out of the cortex are also reported.[1,4,7] The case presented in this report had an extensive radiopaque mass, surrounded by a well-circumscribed radiolucent zone.
Langlais et al. in 1985 proposed six variations in the radiographic appearance.[4]
They are:
Unilocular radiolucency containing radiopaque foci without root divergence/displacement
Well delineated unilocular radiolucency
Radiolucency with central opacifications with root divergence/displacement
Massive expansile lesions
Multilocular radiolucency with or without root resorption
Unilocular radiolucency interposed between divergent/resorbed roots.
On CT sections mature lesions exhibit as a well-defined hyperdense mass with a density of 1000–1500 HU, as reported in our case. Early OF will present as a well-defined hypodense lesion. Thinning or perforation of cortex will also be evident.
Considering the history, clinical and radiographic presentations, differential diagnosis included for our case was OF, cystic odontome, ameloblastic fibro-odontoma, and fibrous dysplasia (FD).
Occasionally large odontomas are associated with the development of cystic lesions (dentigerous cyst). Most cases are diagnosed in the second decade of life, and are seen in the posterior mandible. Radiographically, it usually presents as a radiopaque mass surrounded by thin radiolucent space.[8] This mimics our case.
Dentigerous cyst arises in relation to the crown of an unerupted tooth, mainly mandibular third molar by the expansion of its follicular space. It is common in the second decade of life. Radiographically, it shows a radiolucent area around an unerupted crown with a well – defined sclerotic margin.
Ameloblastic fibro-odontoma is a benign, slow-growing and expansile odontogenic tumor that consists of both odontogenic epithelium and ectomesenchyme proliferation. It occurs predominantly in the posterior mandible. Radiographically, it is seen as a well-circumscribed, expansile radiolucency generally containing either a solitary/multiple radiopaque mass representing the odontome portion of the lesion.
FD is a fibro-osseous lesion, in which normal bone is replaced with fibro-osseous tissue. Most cases are diagnosed in the second decade of life and mostly seen in the maxilla. Radiographically it usually presents as a diffuse mixed lesion in the late stage. Displacement of inferior alveolar canal superiorly, considered to be pathognomonic and was not seen in our radiographs.[5]
Radiographically OF can resemble FD. However, the boundaries of an OF are usually well defined, and these lesions occasionally have a soft tissue capsule and corticated borders, whereas FD usually blends in with surrounding bone.[9] A key feature that distinguishes OF from FD is that the pattern of mineralization varies from place to place, whereas in FD, the pattern tends to be uniform throughout the lesion.[10]
The other differential diagnosis of mature OF includes focal cemento-osseous dysplasia, extrafollicular calcifying epithelial odontogenic tumor and low-grade osteosarcoma. Completely radiopaque mature lesions can even resemble an osteoma.
Histopathology section shows a cellular fibrous tissue containing spindled fibroblasts, often with a storiform appearance. There may be irregular thin trabeculae of woven bone, sometimes rimmed by osteoblasts. Spherical or cementum-like calcifications or irregular globular masses are also seen.[10]
OF is usually treated by conservative surgical enucleation and recurrence is rare. Mandibular OFs usually “shell out” easily during surgery, but maxillary lesions are more difficult to remove completely.
Conclusion
Fibro-osseous pathologies of the jaw bones and a group of confusing terminologies go hand-in-hand. To the oral diagnosticians, their clinical, radiological, and histological variability adds to the dilemma. Therefore, the need is to correlate clinical, radiographic, and histopathologic data to arrive at a specific diagnosis. Early and prompt diagnosis of the fibro-osseous lesion can reduce the effects of co-morbidity associated with these lesions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Liu Y, Wang H, You M, Yang Z, Miao J, Shimizutani K, et al. Ossifying fibromas of the jaw bone: 20 cases. Dentomaxillofac Radiol. 2010;39:57–63. doi: 10.1259/dmfr/96330046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mintz S, Velez I. Central ossifying fibroma: An analysis of 20 cases and review of the literature. Quintessence Int. 2007;38:221–7. [PubMed] [Google Scholar]
- 3.Pimenta FJ, Gontijo Silveira LF, Tavares GC, Silva AC, Perdigão PF, Castro WH, et al. HRPT2 gene alterations in ossifying fibroma of the jaws. Oral Oncol. 2006;42:735–9. doi: 10.1016/j.oraloncology.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 4.Langlais RP, Langland OE, Nortje CJ. Textbook of Diagnostic Imaging of the Jaws. 1st ed. Philadelphia: Williams and Wilkins; 1995. Periapical radiopacities; pp. 551–8. [Google Scholar]
- 5.MacDonald-Jankowski DS. Fibro-osseous lesions of the face and jaws. Clin Radiol. 2004;59:11–25. doi: 10.1016/j.crad.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Reichart PA, Philipsen HP. Textbook of Odontogenic Tumors & Allied Lesions. London: Quintessence Publishing Co. Ltd; 2004. Ossifying fibroma; p. 273. [Google Scholar]
- 7.Sarwar HG, Jindal MK, Ahmad SS. Cemento-ossifying fibroma – A rare case. J Indian Soc Pedod Prev Dent. 2008;26:128–31. doi: 10.4103/0970-4388.43195. [DOI] [PubMed] [Google Scholar]
- 8.Sales MA, Cavalcanti MG. Complex odontoma associated with dentigerous cyst in maxillary sinus: Case report and computed tomography features. Dentomaxillofac Radiol. 2009;38:48–52. doi: 10.1259/dmfr/95388644. [DOI] [PubMed] [Google Scholar]
- 9.White SC, Pharoah MJ. Oral Radiology: Priniciples and Interpretation. 6th ed. St. Louis: Mosby Publishers; 2004. [Google Scholar]
- 10.Speight PM, Roman C. Maxillofacial fibro-osseous lesions. Curr Diagn Pathol. 2006;12:1–10. [Google Scholar]


