Abstract
Aims and Objectives:
Obtaining root coverage has become an important part of periodontal therapy. The aims of this studyare to evaluate the clinical efficacy of acellular dermal matrix graft in the coverage of denuded roots and also to examine the change in the width of keratinized gingiva.
Materials and Methods:
A total of 20 sites with more than or equal to 2 mm of recession depth were taken into the study, for treatment with acellular dermal matrix graft. The clinical parameters such as recession depth, recession width, width of keratinized gingiva, probing pocket depth (PD), and clinical attachment level (CAL) were measured at the baseline, 8th week, and at the end of the study (16th week). The defects were treated with a coronally positioned pedicle graft combined with acellular dermal matrix graft.
Results:
Out of 20 sites treated with acellular dermal matrix graft, seven sites showed complete root coverage (100%), and the mean root coverage obtained was 73.39%. There was a statistically significant reduction in recession depth, recession width, and probing PD. There was also a statistically significant increase in width of keratinized gingiva and also gain in CAL. The postoperative results were both clinically and statistically significant (P < 0.0001).
Conclusion:
The results of this study were esthetically acceptable to the patients and clinically acceptable in all cases. From this study, it may be concluded that acellular dermal matrix graft is an excellent substitute for autogenous graft in coverage of denuded roots.
KEY WORDS: Acellular dermal matrix graft, recession, root coverage
Gingival recession is defined as the exposure of root surfaces due to the apical migration of the gingival margin.[1] The search for the perfect root coverage technique has taken many differing approaches. While several mucogingival surgical procedures have been proved successful and predictable, commonly used in day to day practice are pedicle soft tissue graft and free soft tissue graft procedures. It has been reported that with excellent esthetics, predictability, and genetic predisposition, sub-epithelial connective tissue graft is considered as the gold standard in grafting procedures. Since they are harvested from the palate, an additional surgery is needed, which will be painful during healing and the amount of donor material that was necessary limited the number of teeth that could be treated with a single surgery.
These limitations led to search of alternate methods for root coverage. Klingsberg[2] used preserved sclera for the coverage of denuded roots. Schoo and Coppes[3] and Bartolucci[4] tried duramater and obtained gain in the width of attached gingiva and coverage of denuded roots. The usage of allogenic freeze-dried skin (FDS) graft for mucogingival problems and as a substitute for gingival autografts was reported in 1977. In the early 1980’s, Mishkin et al.[5] reported the first case on the histologic study of FDS allograft in oral cavity.
Since these grafts contained antigens that could cause an immune or inflammatory response and also scarring while healing, acellular dermal matrix graft (ALLODERM®) has been introduced as a substitute for soft tissue grafts. Hence, there is an abundant supply of graft material without resorting to palatal donor site. Alloderm is obtained by processing the dermis of the human donors, where the cells are removed, thereby removing away the source of disease transmission and immunogenic reaction. This leads to a structurally intact connective tissue matrix composed of Type I collagen, which acts as a scaffold to allow ingrowth and replacement by host tissues. Because of this integrity there is no inflammatory response. Because of these factors, this graft is considered as biocompatible and safe over the previously tried FDS allograft. Alloderm has been successfully used in burn surgery, since 1992 and used in periodontal plastic surgery since 1994. Silverstein and Callan[6] had demonstrated ALLODERM to be as effective as free gingival graft in mucogingival surgeries. ALLODERM grafts represent a significant advancement in tissue processing that facilitates effective tissue regeneration and augmentation.
The present study aims to determine the clinical effectiveness of acellular dermal matrix in coverage of gingival recession (Class I and II).
Materials and Methods
The patients for this study were selected from the Department of Periodontics, CSI College of Dental Sciences and Research, Madurai, who complained of receded gingiva.
Inclusion criteria
Patients within the age group of 25–50 years
Recession depth more than or equal to 2 mm
Normal alignment of teeth in the arch
Radiographic evidence of sufficient interdental bone
Patients who can maintain good oral hygiene
Patients with no systemic disease
No abnormal frenal attachments
Patients who had not undergone periodontal surgery within 12 months.
Exclusion criteria
Root surface restoration
Root caries that would require restoration
Smoking
Autoimmune disorders
Allergic to any drugs.
Presurgical treatment and records
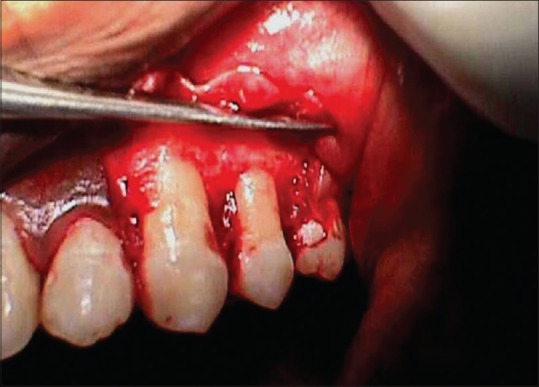
At the baseline, the gingival recession [Figure 1] was evaluated using the following clinical parameters: (1) Recession depth (D) from the cementoenamel junction (CEJ) to the gingival margin. (2) Recession width (W) measured at the widest point (it is the distance between the mesial gingival margin and the distal gingival margin of the tooth).[7] (3) Width of the keratinized gingiva. (4) Probing pocket depth (PD). (5) Clinical attachment level (CAL).
Figure 1.

Preoperative view
All the measurements were made with a William's periodontal probe (Hu-Friedy) with markings 1, 2, 3, 5, 7, 8, 9, and 10. The reference points for all these measurements were CEJ. Measurements were taken to the nearest 0.5 mm. Recession depth and recession width were recorded during the follow-up visits at the end of 2nd and 8th postsurgical week. At the end of the study (16th week), all the abovementioned parameters were recorded. Preoperative and postoperative clinical photographs were taken. All patients underwent the initial phase of treatment, i.e., thorough scaling and root planing. Any trauma from occlusion was eliminated.
Surgical technique
Preparation of the recipient bed
The surgical area was prepared with adequate anesthesia using 2% lignocaine HCl containing 1:2,00,000 epinephrine. A coronally advanced flap procedure was performed in all patients. The flap was extended well-beyond the mucogingival junction, so that it would not exhibit any tension when pulled coronally beyond CEJ [Figure 2]. Following flap elevation, the root surfaces were planed thoroughly. Periodontal probe was used to measure the appropriate length and width of the graft needed.
Figure 2.
After flap reflection
Alloderm: Rehydration and application
The foil bag was opened at the notch, and the peel pouch containing alloderm was removed. The peel pouch was opened, and the alloderm was aseptically transferred with a sterile tweezer. A sufficient dimension of the graft was cut. The alloderm was trimmed to cover and extend at least 3–4 mm on the surrounding bone. Before use, the alloderm with the attached backing was placed in a dish, which was filled with at least 50 ml of rehydration fluid (saline).
When the backing peels off, it was removed and discarded. Then the alloderm was aseptically transferred to the second dish, which contained 50ml of rehydration fluid (saline) as that of first dish [Figure 3]. Alloderm was completely submerged and allowed to soak for 5 min. Thus, alloderm was fully rehydrated and was ready for the application on the recipient bed.
Figure 3.

Hydrated alloderm
Orientation of the alloderm
Alloderm has a basement membrane side and a connective tissue side. The correct orientation was determined by the following:
Dermal or connective tissue side
Readily absorbs blood
More shiny or reflective
More slippery.
Basement membrane side
Does not readily absorb blood
More dull and/or nonreflective
More rough by touch.
In this study, the connective tissue side/dermal side of the acellular dermal graft was placed toward the defect, and the basement membrane side was placed away from the defect [Figure 4].
Figure 4.

Placement of Alloderm
Coronal placement of the pedicle graft
After the placement of the graft, it was secured with 5–0 vicryl sutures. The pedicle was then coronally positioned to completely cover the acellular dermal matrix graft and secured with 4–0 black silk [Figure 5].[8]
Figure 5.

Flap coronally sutured with alloderm
Postoperative instructions
A periodontal dressing was applied [Figure 6]. Postoperative instructions, antibiotics, and analgesics were prescribed. Patients were given handouts of postoperative instructions to be followed. Patients were recalled after 10 days for suture and periodontal dressing removal. The surgical sites were evaluated postoperatively at 2nd, 8th, and 16th week. Clinical measurements were recorded and statistically analyzed.
Figure 6.

Coe pak placed
Results and Statistical Analysis
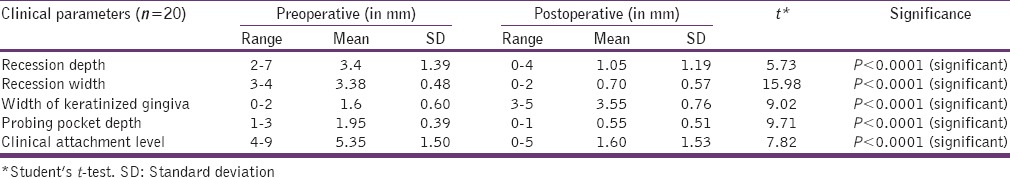
In this study, a total of twenty sites with gingival recession ranging from 2 mm to 7 mm were treated with acellular dermal graft, combined with coronally positioned flap. Out of twenty sites treated with acellular dermal graft, 19 teeth were anterior teeth, and one tooth was maxillary first premolar. To minimize variation in surgical technique, all the procedures were completed by one surgeon and were followed for a period of 16 weeks. The following parameters were recorded: (1) Recession depth, (2) recession width, (3) width of keratinized gingiva, (4) probing depth, (5) CAL. The pre- and post-operative readings of the five parameters were recorded, and the percentages of root coverage for all twenty sites were calculated and tabulated [Table 1]. Statistical evaluation of the results was carried out using paired comparison design (Student's t-test).
Table 1.
Effect of surgical procedure using acellular dermal matrix graft on clinical parameters
Discussion
The outcome of any root coverage procedure is influenced by many factors, such as the oral hygiene maintenance, pretreatment defect size and location. Each of the soft tissue grafting procedures has their own advantages and drawbacks. Of the various techniques used, sub-epithelial connective tissue graft is considered as the gold standard in the treatment for coverage of denuded roots.
Acellular dermal matrix graft is a skin allograft, developed and marketed by Life Cell Inc., Texas, USA. It was developed to act as a substitute for connective tissue grafts in the treatment of burn patients. It eliminates the need for donor site and offers unlimited tissue availability. It is totally nonimmunogenic and safe. Clinically, it acts as much like an autologous connective tissue graft, and hence, it is very easy to trim, adapt, and suture. The purpose of this study was to investigate the possibility of using acellular dermal matrix graft (ALLODERM) as a substitute for autogenous connective tissue grafts in root coverage when combined with a coronally advanced flap.
In this study, the root preparation was limited to mechanical scaling and root planing to avoid any possible influence of the acid on the healing of acellular dermal matrix. However, a study done by Harris[7] treated the root surfaces with tetracycline HCl (125 mg/ml) and obtained higher root coverage of 96.2% with the connective tissue and 95.8% with the acellular dermal matrix grafts.
In this study, the connective tissue side/dermal side of the acellular dermal graft is placed toward the defect (tooth), and the basement membrane side was placed away from the defect.
A total of twenty sites with gingival recession ranging from 2 mm to 7 mm were treated with acellular dermal matrix graft combined with coronally positioned flap. The patients were followed for up to 16 weeks. The following parameters were recorded at the baseline, 8th week, and 16th week: Recession depth, recession width, width of keratinized gingiva, probing PD, CAL.
The processing of the acellular dermal graft retains the basement membrane, thus creating two distinct surfaces of acellular dermal matrix, a basement membrane side and a connective tissue side. It is recommended for gingival augmentation, the basement membrane side is placed away from the bone, and the connective tissue side is placed in such a way that it rests on the bed. Harris[9] in his case report noted that the healing dynamics of root coverage and gingival augmentation are different. Hence, he suggested placing the membrane in the reverse manner, i.e., the basement membrane side of the acellular dermal matrix graft be placed toward the defects. Henderson et al.[10] suggested that success with the acellular dermal matrix graft is highly dependent on proper orientation of the graft and suggested placement of connective tissue side toward the tooth. Aichelmann-Reidy et al.[11] suggested that high predictable and effective root coverage can be obtained when the connective tissue side is placed toward root surface and the basement membrane surface is placed toward the flap. Henderson et al.[12] showed that the orientation of the material did not affect the treatment outcome.
In this study, mean recession depth decreased from baseline to 8th week, i.e. from 3.4 mm to 0.9 mm. However, at the end of the study (16th week), recession depth increased to 1.05 mm. The mean difference in recession depth from the baseline to 16th week was 2.35 mm, which is statistically significant. The mean root coverage of 2.35 mm obtained in this study is well within the results obtained by Harris,[13] Henderson et al.,[10] and Novaes et al.[14]
The mean recession width decreased from 3.38 mm to 0.55 mm at the end of 8th week, but this increased to 0.7 mm at the end of the study (16th week). The mean difference in recession width from baseline to 16th week was 2.68 mm, which is statistically significant and is consistent with the study done by Aichelmann-Reidy et al.[11]
Several surgical procedures have been proposed and practiced to increase the width and thickness of keratinized gingival tissue to assist proper plaque control and prevent further recession of the gingival margin. In this study, there is an increase in width of keratinized gingiva from the baseline to 8th week, i.e. 1.6 mm to 3.7 mm. This increase in width of keratinized gingiva at the end of 8th week decreased to 3.55 mm at the end of the study (16th week). However, the mean gain in width of keratinized gingiva at the end of the 16th week is 1.95 mm, which is statistically significant and correlates well with the study done by Aichelmann-Reidy et al.[11] This significant gain in the width of keratinized tissue is worth noting.
In this study, the mean probing depth decreased from baseline to 8th week, i.e. 1.95 mm to 0.1 mm. However, at the end of the study (16th week), the probing depth increased to 0.55 mm. The mean decrease in probing depth from baseline to 16th week is 1.40 mm, which is statistically significant. The results obtained in this study are consistent with the study done by Tal et al.[15] Clinically, it was difficult to probe the sulcus with no bleeding on probing. This shows a healthy attachment of the graft to the recipient sites. To identify the type of attachment, the grafted tooth should be extracted, which was beyond the scope of this study.
Also in this study, there is a gain in mean CAL from baseline to 8th week (5.35 mm to 1 mm). However, there is a decrease in CAL to 1.6 mm at the end of the study (16th week). However, the mean gain in CAL at end of 16th week was 3.75 mm, which is statistically significant. Thus, the gain in mean CAL in this study correlated well with the results obtained in the studies done by Aichelmann-Reidy et al.[11] and Harris.[13]
Here, in this study, modifications of surgical technique were done in two patients. In one of the patients, a laterally displaced flap with acellular dermal graft was used to cover the recession defect and in another patient, the acellular dermal graft was used like a free gingival graft. At the end of the study, there was decrease in the recession depth in both the patients.
In this clinical study, the mean root coverage obtained is 73.39% with the acellular dermal graft. This coverage of denuded roots is statistically significant, when compared with the preoperative results. Thus, the percentage of root coverage obtained in this study is found to be well within the limits of studies done by Aichelmann-Reidy et al.[11] who obtained root the coverage of 65.9%, and Harris (2002)[13] who gained root coverage of 87% at the end of 18 months. In this study, acellular dermal graft is well-tolerated by the host periodontal tissue. Seven out of twenty sites showed complete coverage (100%), with 10 teeth showing more than or equal to 50 percentage of coverage. Complete root coverage was obtained in 35% of sites, and it correlated well-above with the study by Paolantonio et al.[16] who observed complete root coverage in only 26.6% of sites treated with acellular dermal matrix graft.
In one of the patients treated, the graft was placed as free gingival graft, and we attained only a 2 mm gain in recession depth coverage, i.e., 33.33% of coverage. In another patient, who attained a similar 33.33% of coverage, there was loose sutures and dislodgement of the periodontal dressing. While attempting for another dressing, the graft was dislodged, thus leading to recession in that site. In one more patient, while suturing the graft, the needle nicked the overlying flap thereby leading to tearing of the flap. In this patient, there was coverage, but it was only about 42.57%.
In rest of the patients who did not attain complete coverage, the maintenance of the site was fair to poor, in spite of giving oral hygiene instructions at each appointment, thus leading to reduced root coverage.
Tal et al.[15] suggested that acellular dermal graft might also act as a barrier equivalent to selective cell repopulation membranes, thus encouraging periodontal regeneration. The mean root coverage of 73.39% observed with acellular dermal graft in the present study falls within the range of 52% to 90%[17] mean root coverage reported with guided-tissue regeneration.
Acellular dermal matrix graft may act as substitute for free connective tissue graft. Studies by Harris[9] and Reidy et al. (1998)[11] showed the efficacy of acellular dermal matrix graft equivalent to the connective tissue graft in obtaining root coverage. Haeri and Parsell[18] compared the use of acellular dermal matrix graft to an autogenous gingival graft for gingival augmentation. They found no statistical significance in recession reduction, clinical attachment gain, and probing PD reduction when acellular dermal graft was compared with autogenous gingival graft.
Studies by Bouchard et al.,[19] Borghetti and Louise,[20] Wennström[21] on connective tissue grafts, claim that with the use of connective tissue graft, about 52% to 98% coverage of the initial recession can be obtained. The result from this study, i.e., the percentage of root coverage of 73.39% is well within the results obtained with the use of connective tissue graft.
Acellular dermal matrix allograft yielded better color and tissue blended well into the adjacent tissues [Figure 7]. This is because the acellular dermal matrix allograft is mostly incorporated into the tissue and finally remodeled. Alloderm can be identified by the presence of elastin fibers, which is characteristic of acellular dermal matrix graft and skin. Therefore, we can consider elastin as marker for alloderm. Thus, acellular dermal matrix graft may be used as a substitute for autogenous connective tissue graft. The results obtained with the acellular dermal graft shows that the surgical procedures with acellular dermal graft have a definite therapeutic utility in the clinical practice.
Figure 7.

Postoperative view after 16 week
Conclusion
Within the limitations of this study, it can be concluded that acellular dermal graft is viable, highly safe with biologically acceptable qualities, which can substitute soft tissue grafts that can be used for the treatment of gingival recession. The root coverage obtained improved the esthetics and met with the expectations and demands of the patients and also the treating surgeon. There was a statistically significant coverage obtained with acellular dermal graft [73.39%] and showed widening of the keratinized gingiva. Acellular dermal graft used in this study was well-tolerated by gingival tissues and had no adverse effects on treated and adjacent nontreated sites.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.American Academy of Periodontology; Glossary of periodontal terms. (4th ed) 2001:44. [Google Scholar]
- 2.Klingsberg J. Preserved sclera in periodontal surgery. J Periodontol. 1972;43:634–9. doi: 10.1902/jop.1972.43.10.634. [DOI] [PubMed] [Google Scholar]
- 3.Schoo WH, Coppes L. Use of palatal mucosa and lyophilized dura mater to create attached gingiva. J Clin Periodontol. 1976;3:166–72. doi: 10.1111/j.1600-051x.1976.tb01864.x. [DOI] [PubMed] [Google Scholar]
- 4.Bartolucci EG. A clinical evaluation of freeze-dried homologous dura mater as a periodontal free graft material.Study in humans. J Periodontol. 1981;52:354–61. doi: 10.1902/jop.1981.52.7.354. [DOI] [PubMed] [Google Scholar]
- 5.Mishkin DJ, Shelley LR, Jr, Neville BW. Histologic study of a freeze-dried skin allograft in a human. A case report. J Periodontol. 1983;54:534–7. doi: 10.1902/jop.1983.54.9.534. [DOI] [PubMed] [Google Scholar]
- 6.Silverstein LH, Callan DP. An Acellular dermal matrix allograft substitute for palatal donor tissue. J Postgrad Dent Ser. 1996;3:14–21. [Google Scholar]
- 7.Harris RJ. A comparative study of root coverage obtained with an acellular dermal matrix versus a connective tissue graft: Results of 107 recession defects in 50 consecutively treated patients. Int J Periodontics Restorative Dent. 2000;20:51–9. [PubMed] [Google Scholar]
- 8.Bernimoulin JP, Lusher B. Coronal repositioned periodontal flap. J Clin Periodontol. 1975;2:1–13. doi: 10.1111/j.1600-051x.1975.tb01721.x. [DOI] [PubMed] [Google Scholar]
- 9.Harris RJ. Root coverage with a connective tissue with partial thickness double pedicle graft and an acellular dermal matrix graft: A clinical and histological evaluation of a case report. J Periodontol. 1998;69:1305–11. doi: 10.1902/jop.1998.69.11.1305. [DOI] [PubMed] [Google Scholar]
- 10.Henderson RD, Drisko CH, Greenwell H. Root coverage using Alloderm acellular dermal graft material. J Contemp Dent Pract. 1999;1:24–30. [PubMed] [Google Scholar]
- 11.Aichelmann-Reidy ME, Yukna RA, Evans GH, Nasr HF, Mayer ET. Clinical evaluation of acellular allograft dermis for the treatment of human gingival recession. J Periodontol. 2001;72:998–1005. doi: 10.1902/jop.2001.72.8.998. [DOI] [PubMed] [Google Scholar]
- 12.Henderson RD, Greenwell H, Drisko C, Regennitter FJ, Lamb JW, Mehlbauer MJ. Predictable multiple site root coverage using an acellular dermal matrix allograft. J Periodontol. 2001;72:571–82. doi: 10.1902/jop.2001.72.5.571. [DOI] [PubMed] [Google Scholar]
- 13.Harris RJ. Cellular dermal matrix used for root coverage: 18-month follow-up observation. Int J Periodontics Restorative Dent. 2002;22:156–63. [PubMed] [Google Scholar]
- 14.Novaes AB, Jr, Grisi DC, Molina GO, Souza SL, Taba M, Jr, Grisi MF. Comparative 6-month clinical study of a subepithelial connective tissue graft and acellular dermal matrix graft for the treatment of gingival recession. J Periodontol. 2001;72:1477–84. doi: 10.1902/jop.2001.72.11.1477. [DOI] [PubMed] [Google Scholar]
- 15.Tal H, Moses O, Zohar R, Meir H, Nemcovsky C. Root coverage of advanced gingival recession: A comparative study between acellular dermal matrix allograft and subepithelial connective tissue grafts. J Periodontol. 2002;73:1405–11. doi: 10.1902/jop.2002.73.12.1405. [DOI] [PubMed] [Google Scholar]
- 16.Paolantonio M, Dolci M, Esposito P, D’Archivio D, Lisanti L, Di Luccio A, et al. Subpedicle acellular dermal matrix graft and autogenous connective tissue graft in the treatment of gingival recessions: A comparative 1-year clinical study. J Periodontol. 2002;73:1299–307. doi: 10.1902/jop.2002.73.11.1299. [DOI] [PubMed] [Google Scholar]
- 17.De Sanctis M, Zucchelli G. Guided tissue regeneration with a resorbable barrier membrane (Vicryl) for the management of buccal recession: A case report. Int J Periodontics Restorative Dent. 1996;16:435–41. [PubMed] [Google Scholar]
- 18.Haeri A, Parsell D. Creeping attachment: Autogenous graft vs dermal matrix allograft. Compend Contin Educ Dent. 2000;21:725–9. [PubMed] [Google Scholar]
- 19.Bouchard P, Etienne D, Ouhayoun JP, Nilvéus R. Subepithelial connective tissue grafts in the treatment of gingival recessions.A comparative study of 2 procedures. J Periodontol. 1994;65:929–36. doi: 10.1902/jop.1994.65.10.929. [DOI] [PubMed] [Google Scholar]
- 20.Borghetti A, Louise F. Controlled clinical evaluation of the subpedicle connective tissue graft for the coverage of gingival recession. J Periodontol. 1994;65:1107–12. doi: 10.1902/jop.1994.65.12.1107. [DOI] [PubMed] [Google Scholar]
- 21.Wennström JL. Mucogingival therapy. Ann Periodontol. 1996;1:671–701. doi: 10.1902/annals.1996.1.1.671. [DOI] [PubMed] [Google Scholar]


