Abstract
Context
Clinical decision support systems (CDSSs) can help clinicians assess cardiovascular disease (CVD) risk and manage CVD risk factors by providing tailored assessments and treatment recommendations based on individual patient data. The goal of this systematic review was to examine the effectiveness of CDSSs in improving screening for CVD risk factors, practices for CVD-related preventive care services such as clinical tests and prescribed treatments, and management of CVD risk factors.
Evidence acquisition
An existing systematic review (search period, January 1975–January 2011) of CDSSs for any condition was initially identified. Studies of CDSSs that focused on CVD prevention in that review were combined with studies identified through an updated search (January 2011–October 2012). Data analysis was conducted in 2013.
Evidence synthesis
A total of 45 studies qualified for inclusion in the review. Improvements were seen for recommended screening and other preventive care services completed by clinicians, recommended clinical tests completed by clinicians, and recommended treatments prescribed by clinicians (median increases of 3.8, 4.0, and 2.0 percentage points, respectively). Results were inconsistent for changes in CVD risk factors such as systolic and diastolic blood pressure, total and low-density lipoprotein cholesterol, and hemoglobin A1C levels.
Conclusions
CDSSs are effective in improving clinician practices related to screening and other preventive care services, clinical tests, and treatments. However, more evidence is needed from implementation of CDSSs within the broad context of comprehensive service delivery aimed at reducing CVD risk and CVD-related morbidity and mortality.
Context
Cardiovascular disease (CVD) is the leading cause of death among U.S. adults (approximately 800,000 deaths annually).1 Modifiable risk factors for CVD such as hypertension, hyperlipidemia, diabetes, smoking, obesity, and physical inactivity can be improved with provider-focused strategies such as provider reminders, audit and feedback mechanisms, and educating providers on guidelines.2 Implementation of such strategies could help mitigate the burden of CVD risk factors and advance progress toward achieving objectives outlined in Healthy People 20203 and Million Hearts®.4
The U.S. Preventive Services Task Force (USPSTF)5 and other clinical practice guideline panels6–8 provide evidence-based recommendations for CVD risk factor screening; practices for CVD-related preventive care services (e.g., counseling for diet and physical activity); and management of patients with CVD risk factors. However, barriers such as lack of resources; “clinical inertia” (i.e., clinician failure to initiate or intensify therapy when indicated9); and lack of familiarity with guideline availability impede CVD prevention.10,11 Clinical decision support systems (CDSSs) could play a role in reducing some of these barriers by helping clinicians assess CVD risk and prompting appropriate actions to manage risk factors.
CDSSs are computer-based information systems designed to assist clinicians in implementing clinical guidelines and evidence-based practices at the point of care. CDSSs provide tailored patient assessments and treatment recommendations for clinicians to consider on the basis of individual patient data. Patient information is entered manually or automatically through an electronic health record (EHR) system. CDSSs are often incorporated within EHRs and integrated with other computer-based functions that offer patient care summary reports, feedback on quality indicators, and benchmarking.
CDSSs aimed at preventing CVD include one or more of the following:
tailored reminders to screen for CVD risk factors and CVD-related preventive care, clinical tests, and treatments;
assessments of patients’ risk for developing CVD based on their history, risk factors, and clinical test results;
recommendations for evidence-based treatments to prevent CVD, including intensification of existing treatment regimens;
recommendations for health behavior changes to discuss with patients, such as quitting smoking, increasing physical activity, and reducing excessive salt intake; and
alerts when indicators for CVD risk factors are not at goal.
A recent systematic review by Bright and colleagues12 evaluated the effects of CDSSs on quality of care measures (i.e., clinician practices) and clinical outcomes related to morbidity and mortality for numerous conditions (e.g., cancer screening, immunization, CVD prevention). They analyzed 148 RCTs of CDSSs implemented in clinical settings to aid decision making and found that CDSSs improved healthcare process measures related to performing preventive care services, ordering clinical tests, and prescribing treatments; however, the review found sparse evidence on the effectiveness of CDSSs on clinical outcomes.
The subset of studies from the review of Bright et al.12 that focused on CVD prevention was of specific interest for this Community Guide systematic review, which focused on the potential role of CDSSs in CVD prevention. This review examined the most up-to-date evidence on effectiveness of CDSSs in improving screening for CVD risk factors; clinician practices for CVD-related preventive care services, clinical tests, and treatments; and improvements in CVD risk factors. This review also assessed the applicability of findings for various U.S. populations and settings, as well as considerations for CDSS implementation.
Evidence Acquisition
Detailed systematic review methods used for The Community Guide have been published previously.13,14 For this review, a coordination team was formed, composed of CVD subject matter experts from various agencies, organizations, and academic institutions, together with systematic review methodologists from the Community Guide Branch at CDC. The team worked under the oversight of the independent, unpaid, nonfederal Community Preventive Services Task Force.
Conceptual Approach and Analytic Framework
The coordination team’s conceptual approach to evaluate CDSSs for CVD prevention is depicted in Appendix Figure 1 (available online). CDSSs assist clinicians by providing recommendations for screenings, preventive care services, and treatments, thereby increasing clinician practices such as those recommended by the USPSTF (e.g., screening for high blood pressure and diabetes, smoking-cessation counseling, and use of aspirin).5 Increased uptake of these practices should increase both the number of patients identified with CVD risk factors and clinician knowledge about risk, leading to an increase in appropriate clinical tests ordered and treatments prescribed by clinicians for management of these risk factors in concordance with evidence-based guidelines. Improvements in clinician practices should lead to improved outcomes for hypertension, hyperlipidemia, and diabetes, as well as improved health behaviors and patient satisfaction with care, ultimately leading to reduced morbidity and mortality from CVD and improved health-related quality of life.
Search for Evidence
Existing systematic review
The search for evidence first involved locating existing systematic reviews on this topic. The review of Bright and colleagues,12 accompanied by an Agency for Healthcare Research and Quality (AHRQ) report,15 employed methods comparable to Community Guide standards.13,14 Further, conceptualization of that review was closely aligned with the Community Guide team’s approach. The review identified studies evaluating CDSSs published from January 1975 to January 2011.
Because Bright et al.12 and AHRQ15 examined CDSSs across all health topics, the coordination team considered that evidence a comprehensive source of studies on effectiveness of CDSSs aimed at CVD prevention. Therefore, studies from Bright and colleagues/AHRQ were screened by two Community Guide reviewers independently to identify CDSS studies focused on CVD prevention for inclusion in this review.
Update search
To ensure this review used the most current evidence, an update search was conducted in October 2012 using the Bright et al.12/AHRQ15 search strategy, along with key CVD terms found at www.thecommunityguide.org/cvd/supportingmaterials/SS-CDSS-2013.html.
Inclusion Criteria for Cardiovascular Disease Prevention Studies
In addition to meeting the definition for CDSSs as stated in the reviews of Bright and colleagues12 and AHRQ,15 studies evaluating CDSSs for CVD prevention were included in this Community Guide review if they
were conducted in a high-income country16;
reported at least one primary outcome of interest relevant to identification and management of CVD risk factors;
were focused on study populations in which the majority (≥ 50%) did not have a history of CVD (e.g., myocardial infarction, stroke); and
employed a study design that compared a group receiving CDSS with a usual care group or used an interrupted time series design with at least two measurements before and after CDSS implementation. Usual care is described here as interventions that did not include any new intervention activities (other than minimal activities such as providing brochures or pamphlets). Usual care was whatever routine care was offered at a given primary care site. It is probable that usual care varied across different health systems and settings.
Data Abstraction and Quality Assessment
Each study that met inclusion criteria was abstracted by two reviewers independently. Abstraction was based on a standardized abstraction form (www.thecommunityguide.org/methods/abstractionform.pdf) that included information on study quality, intervention components, participant demographics, and outcomes. Disagreements between reviewers were resolved by team consensus.
Bright et al.12 used AHRQ methods17 to assess threats to validity for included studies. Their quality scoring was applied to the subset of CDSS studies focused on CVD prevention12; similar Community Guide quality scoring methods13,14 were used for studies identified in the update. Threats to validity—such as poor descriptions of the intervention, population, sampling frame, and inclusion/exclusion criteria; poor measurement of exposure or outcome; poor reporting of analytic methods; incomplete data sets; loss to follow-up; or intervention and comparison groups not being comparable at baseline—were used to characterize studies as having good, fair, or limited/poor quality of execution. Studies with limited/poor quality of execution were excluded from analysis.
Primary Outcomes of Interest
Primary outcomes included quality of care outcomes and outcomes related to CVD risk factor management (Appendix Table 1, available online).18–23 Quality of care outcomes measured evidence-based clinician practices as determined by the USPSTF for screening5 and clinical guidelines for management of CVD risk factors.6–8 These practices were categorized as screening and other preventive care services, clinical tests, and prescribed treatments prompted by the CDSS and ordered or completed by the clinician.
Secondary Outcomes
Although CDSSs focused principally on improving clinician practices, distal outcomes focused on improving patient health behavior associated with CVD risk were also reported. Specifically, changes in smoking behavior, diet, physical activity, BMI, and medication adherence were analyzed.
Analysis
Because the focus of this review was on CVD prevention and included RCT and non-RCT study designs, a meta-analysis was not conducted—unlike Bright and colleagues,12 who conducted a meta-analysis from RCT data on all quality of care outcomes. Therefore, descriptive statistics that facilitated simple and concise summaries of study result distribution were used for primary and secondary outcomes.
For each study, absolute percentage point (pct pt) changes were calculated for dichotomous variables for groups receiving clinical decision support compared with usual care. Difference in differences of the mean were calculated for continuous variables for groups receiving clinical decision support compared with usual care (Appendix Table 2, available online).
For the overall summary measure, the median of effect estimates from individual studies and the interquartile interval (IQI) were reported for each primary outcome. Conclusions on the strength of evidence on effectiveness are based on the subset of CVD prevention studies identified from Bright et al.12 and those identified through the update search, taking into account the number of studies, quality of available evidence, consistency of results, and magnitude of effect estimates, per Community Guide standards.
Study and population characteristics, and effect modifiers described previously, were summarized using descriptive statistics.
Evidence Synthesis
Search Yield
The search process from both the Bright and colleagues12/AHRQ15 reviews and the updated search is shown in Appendix Figure 2 (available online). Bright et al. identified a total of 323 studies examining CDSSs across all health topics. Following screening by two independent Community Guide reviewers, a total of 57 articles24–80 representing 50 unique studies of CDSSs for CVD prevention were identified. Of these, 46 studies24–68,80 met inclusion criteria; however, seven studies35,40,49,57,59,62,64 judged to be of limited quality of execution were excluded from analysis. The update search (January 2011 through October 2012) identified 14 articles representing 13 unique studies.81–94 Of these, seven studies81–87 met the inclusion criteria; however, one study86 was judged to be of limited quality and therefore excluded from analysis. From the combined searches, a total of 45 studies24–34,36–39,41–48,50–56,58,60,61,63,65–68,80–85,87 qualified for analysis in this review. Analyses were conducted in 2013.
Study and Intervention Characteristics
Twenty-six studies were from the U.S.,24,25,28,29,31,34,36,39,44,45,47,51–54,56,58,63,65,67,80–82,84,85,87 with the remaining studies conducted in Canada (five studies)41,48,61,66,83; Europe (11 studies)26,27,30,33,37,38,42,46,50,67,68; Australia (two studies)32,60; and New Zealand (one study).43 Most studies implemented CDSSs in outpatient practices; two studies54,55 were in a hospital setting. Nineteen studies25,34,36,39,44,46–48,51,53–55,58,60,61,63,82,84,87 were conducted in practices with an academic affiliation, and three studies25,28,80 took place in Veterans Affairs facilities. Studies focused on screening for CVD risk factors (six studies)36,42,43,48,66,67; hypertension management (seven studies)25,33,37,39,50,51,63; lipid management (six studies)24,27,33,68,81,84; and diabetes management or CVD prevention among a diabetic population (15 studies).26,29,30,38,41,44,45,47,52,58,60,65,82,85,87 Further, 11 studies28,31,32,34,46,53–56,61,80 addressed other disease areas in addition to CVD prevention. Quality limitations assigned to studies were usually attributable to differences in patient demographics between intervention and comparison groups at baseline, possible contamination, and incomplete descriptions of study populations, interventions, and methodology.
CDSS interventions were usually implemented across multiple healthcare sites (median, 7.0 intervention practices per study; IQI=1, 17.5). Median duration of intervention was 12 months (IQI=6, 18.5) and the median number of included clinicians was 24 (IQI=13, 68), with a median of 1,190 total patients (IQI=588, 3545) per study. CDSS users were usually physicians (39 studies),24–26,28,29,31,33,34,36–39,41,43–48,50–56,58,61,63,65–68,81–85,87 followed by nurses (12 studies)24–26,29,36,41,45,47,50,61,63,84; physician assistants (five studies)24,25,31,36,45; and pharmacists (two studies).51,60 Most interventions used locally developed CDSSs (24 studies),24,25,27,28,31,37–39,44–48,51,54,55,58,61,63,65,66,83,85,87 and were integrated within EHRs (29 studies).24,28–30,32–34,37–39,42,43,46,50–52,54–56,63,66–68,80,82–85,87 Decision support was usually delivered to the clinician synchronously during patient visits (38 studies),24–28,30,33,34,36–39,41–44,46,48,51–56,58,60,61,65–68,80–85,87 and CDSS recommendations were usually system-initiated when delivered automatically without a clinician request (37 studies).25–34,36,39,42,44–48,51–54,56,58,60,61,63,65–68,80–85 Most CDSSs were tailored to provide support for chronic disease management (24 studies)24–29,37–39,41,44,45,51,52,58,63,65,80–85,87; pharmacotherapy (17 studies)30,33,46,47,50,52,55,58,60,63,65,66,81,82,84,85,87; preventive care (15 studies)28,31–34,36,42–44,53,54,61,67,68,80; and lab test ordering (13 studies).26,34,36,44,47,52,53,55,82–85,87 Detailed evidence tables are available at www.thecommunityguide.org/cvd/supportingmaterials/SET-CDSS-2013.pdf.
Population Characteristics
Median age of patients was 60.3 years, and slightly more women than men were included (Table 1). From studies that reported race/ethnicity, the median for the proportion of study populations identifying as white was 58.5% (14 studies)24–26,29,36,39,45,48,53–55,81,85,87 and 47.5% for participants identifying as black (nine studies).24,25,29,39,51,53,58,81,87 Few studies reported income level,45 education attainment,31,41,45,51,83 or insurance status.31,36,39,53,83,87
Table 1.
Population Characteristics from Included Studies
| Characteristic | Median (IQI) | Studies reporting characteristic, n (%)a |
|---|---|---|
| Age (years) | 60.3 (50.3–64.4) | 38 (84) |
| Gender (%) | ||
| Male | 45.5 (39.6–50.0) | 35 (78) |
| Female | 54.6 (50.0–60.4) | 35 (78) |
| Race/ethnicity (%) | ||
| White | 58.5 (50.0–94.2) | 14 (32) |
| Black | 47.5 (14.5–79.5) | 9 (21) |
| Hispanic | 5.7 (1.7–21.0) | 5 (11) |
| Other | 2.0 (1.5–2.1) | 7 (16) |
| Income | ||
| Low-income | NA | 1 (2) |
| Education (%) | ||
| Less than high school | 18.0 (NA) | 3 (7) |
| High school diploma | 46.7 (38.1–68.9) | 4 (9) |
| College or university | 36.4 | 2 (5) |
| Insurance status (%) | ||
| Private insurance | 39.5 (29.3–50.8) | 5 (11) |
| Medicare/Medicaid (U.S. studies) | 23.5 (18.0–39.8) | 5 (11) |
| Uninsured | 18.5 (7.7–39.8) | 5 (11) |
Total number of studies (and proportion of total number of included studies) that reported specific demographic characteristics.
IQI, interquartile interval; NA, not available.
Quality of Care Outcomes
Completed or ordered screening and other preventive care services
Figure 1 displays individual effect estimates (with 95% CIs) for absolute change in guideline-based screening and other preventive care services completed or ordered by clinicians from 17 studies24,28,32,33,36,43,48,53,54,61,67,80–83,87,92 comparing CDSSs with usual care. Studies are shown according to the type of completed or ordered screening or preventive care service. The y-axis lists the study author, year of publication, and comparison group values at last follow-up. Effect estimates to the right of zero indicate increases in guideline-based screenings and preventive care services completed or ordered by clinicians when prompted by CDSSs, compared with usual care. There was an overall median increase of 3.8 percentage points (pct pts) (IQI= ‒0.08, +10.6) from 17 studies with 32 outcome measures. Most outcome measures in the favorable direction were statistically significant (p<0.05).28,43,48,53,61,67,82,92 Additionally, five studies41,44,60,68,83 that could not be plotted because of differences in reported outcome measures demonstrated substantial improvements in guideline-based screening and preventive care services.
Figure 1.
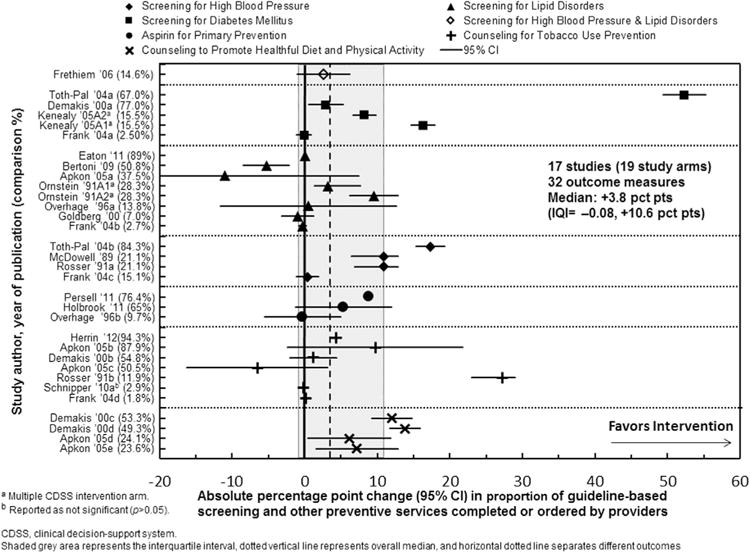
Changes in proportion of guideline-based screening and other preventive care services completed/ordered by providers prompted by a clinical decision support system.
Ordered or completed clinical tests
Figure 2 shows individual effect estimates from seven studies reporting the proportion of guideline-based clinical tests completed or ordered by clinicians. Studies are displayed by the type of clinical test ordered or completed for patients diagnosed with hypertension, hyperlipidemia, or diabetes. Effect estimates to the right of zero favor an increase in guideline-based clinical tests completed or ordered by clinicians when prompted by CDSSs. Seven studies47,52,56,73,82,85,87 with 19 outcome measures reported a median increase of 4.0 pct pts (IQI=0.7, 7.0) in the proportion of guideline-based clinical tests completed or ordered by clinicians when prompted by CDSSs, compared with usual care. Most reported outcome measures were statistically significant (p<0.05).47,52,73,82,85,87 Two additional studies29,83 that could not be included in the analysis demonstrated a substantial increase in guideline-based completed or ordered clinical tests.
Figure 2.
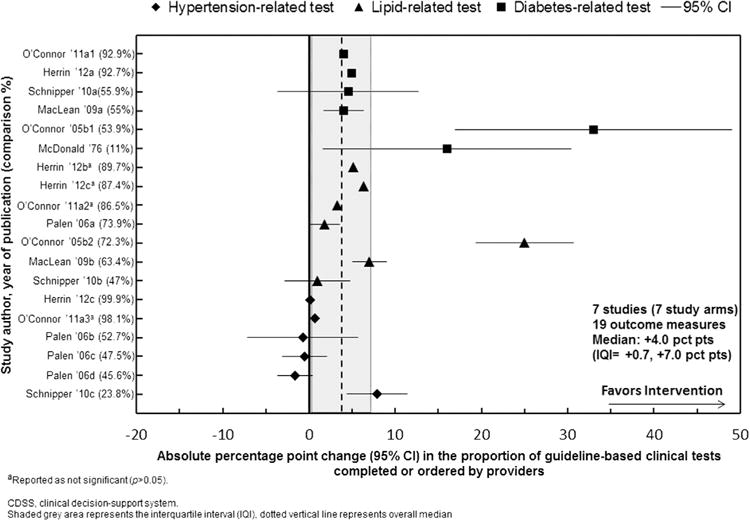
Changes in proportion of guideline-based clinical tests completed/ordered by providers prompted by a clinical decision support system for patients with hypertension, hyperlipidemia, or diabetes.
Prescribed or ordered treatments
Figure 3 displays individual effect estimates of included studies reporting the proportion of guideline-based treatments prescribed or ordered by clinicians when prompted by CDSSs, compared with usual care. Effect estimates are displayed by type of prescribed or ordered treatment medication. In 11 studies24,30,33,39,47,51,54,63,66,82,87 with 20 outcome measures, the overall median increase was 2.0 pct pts (IQI= −0.75, +8.55). Most reported individual outcome measures were statistically significant (p<0.05).30,33,39,47,66,82,87 Additionally, six studies27,46,50,58,65,68 with 11 study arms, not plotted because of differences in the way outcomes were analyzed, showed mixed results for this outcome; five study arms reported favorable results, five study arms reported unfavorable results, and one study arm reported no change in treatments prescribed by providers.
Figure 3.
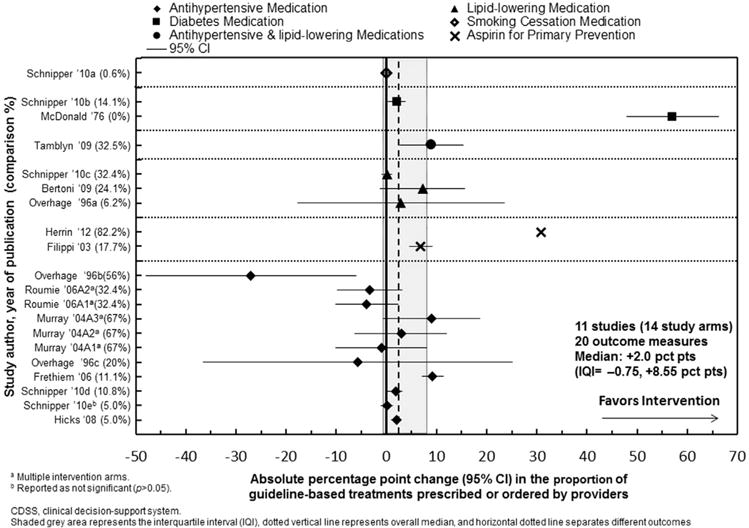
Changes in proportion of guideline-based treatment completed or ordered by providers when prompted by a clinical decision support system.
Cardiovascular Disease Risk Factor Outcomes
Appendix Table 3 (available online) displays results for CVD risk factors, specifically blood pressure, lipid, and diabetes outcomes. Findings were inconsistent in 15 studies25,33,38,39,41,45,50,51,58,63,65,71,82,83,85 reporting blood pressure outcomes, 13 studies27,33,38,41,45,58,65,71,81–83,85,92 reporting lipid outcomes, and 12 studies29,38,41,45,52,58,65,82–85,92 reporting diabetes outcomes.
Morbidity, Mortality, and Patient-Centered Outcomes
For morbidity, five studies reported no significant changes for outcomes related to emergency department visits,51 hospitalizations,45,63 and CVD events.42,83 One study63 with two intervention study arms reported on mortality and found that he group in which providers received education on hypertension guidelines plus CDSS alerts had lower mortality (by 1.90 pct pts) compared with provider education alone. The second intervention study arm, in which providers received education on guidelines plus CDSS alerts, and patients received educational material on hypertension self-management, reduced mortality by 1.60 pct pts.
For patient-centered outcomes, one study reported health-related quality of life. Murray et al.51 found that patients treated by physicians who received evidence-based treatment recommendations via CDSSs for hypertension generally had better health-related quality of life as measured by the Short Form–36 subscales95 compared with patients managed by pharmacists receiving these hypertension reminders or usual care (p>0.05). However, no clinically relevant differences were found for quality of life assessments using the Bulpitt and Fletcher subscales.96
Health Behavior Change Outcomes
Six studies26,38,41,65,82,83 reported changes in smoking status among patients. The proportion of non-smokers in the CDSS intervention arms increased by a median of 2.3 pct pts (IQI=0.1, 3.4) compared with usual care. Another five studies37,38,41,45,83 reported minimal changes in BMI (median reduction, −0.10). Few studies reported changes in physical activity,41,45,83 diet,45,83 and medication adherence,63 and summary measures were not calculated.
Clinical Decision Support Systems Combined With Other Interventions
A small proportion of studies examined CDSSs in combination with other interventions to provide a multicomponent approach to overcome barriers at the patient, provider, or organizational level. Five studies29,39,51,52,83 examined CDSSs implemented with team-based care, an organizational, systems-level intervention where primary care providers and patients work together with other providers, primarily pharmacists and nurses, to improve the efficiency of healthcare delivery and self-management support for patients. Two studies41,53 implemented CDSSs along with generic patient reminders. For screening and preventive care services and clinical testing, these multicomponent studies found larger increases compared with the overall effect estimates for CDSSs, but for prescribed treatments, their effect estimates were similar to the overall estimate for CDSSs (Appendix Table 4, available online).
Applicability of Findings
Findings from this review are applicable to the U.S. healthcare system, especially among large outpatient primary care settings. Most CDSSs in the included studies were developed locally by healthcare systems in concert with providers. CDSSs were added to preexisting EHRs in approximately one third of studies. In most studies, CDSSs were designed to offer recommendations to providers without user requests for information, and most were designed to deliver decision support as part of clinical workflow. Few studies reported whether providers were required to respond to CDSS recommendations.
Information on race/ethnicity was reported only in one third of studies, and data on SES were limited. In most study populations, patients had one diagnosed risk factor among diabetes, hypertension, and hyperlipidemia. However, findings are likely applicable to diverse population groups with comorbid CVD risk factors.
Additional Benefits and Potential Harms
CDSSs can serve as tools to enhance the effectiveness of organizational, system-level interventions such as team-based care and the patient-centered medical home. No harms to patients from CDSSs were identified in studies in the review or in the broader literature.
Conclusion
Summary of Findings
Based on Community Guide rules of evidence,13 there is sufficient evidence that CDSSs are effective in improving screening for CVD risk factors and clinician practices for CVD-related preventive care services, clinical tests, and treatments. In general, studies that combined CDSSs with other interventions found larger improvements. Findings for CVD risk factor outcomes are inconsistent, and meaningful conclusions cannot be drawn. Few studies reported on health behavior change, morbidity, mortality, health-related quality of life, and patient satisfaction with care; therefore, conclusions could not be reached. Economic information on CDSS implementation was sparse.97
Limitations
Although Bright and colleagues12 conducted a formal meta-analysis, this was not considered for the present review primarily because of heterogeneity in study designs. Bright et al. only analyzed data from RCTs, whereas this review took a more inclusive approach and analyzed data from RCTs and quasi-experimental and observational study designs. Hence, descriptive statistics were used to summarize findings for this review, as well as applicability and generalizability of results to various U.S. populations and settings. Second, visual inspection of funnel plots investigating the relationship between effect size and sample size suggest potential publication bias for quality of care outcomes; this may be due to CDSS studies that resulted in positive outcomes having a greater likelihood of being published. Finally, a subgroup analysis based on effect modifiers was not conducted because of substantial heterogeneity with the factors and features incorporated within each CDSS; delivery formats of the systems; and focus of the CDSS (e.g., disease management, pharmacotherapy, preventive care).
Evidence Gaps
Overall, most studies did not collect data on the impact of CDSSs on CVD risk factor outcomes, morbidity, or mortality. Most available evidence is from studies on the effectiveness of CDSSs when implemented alone in the healthcare system rather than as part of a coordinated service delivery. Thus, more evidence is needed about implementation of a CDSS as one part of a comprehensive service delivery system designed to improve outcomes for CVD risk factors and to reduce CVD.
Evidence is also needed on longer-term evaluations of CDSSs. These evaluations might account for issues associated with the initial integration of CDSSs with care workflow. More studies are needed to assess the effectiveness of CDSSs for other providers, such as nurses and pharmacists. Additional assessments on the impact of CDSSs in reducing health disparities and improving patient satisfaction with care are needed.
Discussion
This Community Guide systematic review examined the effectiveness of CDSSs to prevent CVD and provided the basis for the Community Preventive Services Task Force recommendation on use of CDSSs to improve quality of care outcomes for clinician practices related to CVD prevention.98 Findings from this review are consistent with those found in the review of Bright and colleagues,12 which examined the effect of CDSSs on multiple disease conditions. Another review by Souza et al.99 also found CDSSs to be effective for improving CVD-specific quality of care outcomes; moreover, a CDSS review by Montgomery and colleagues100 found a favorable effect on quality of care for hypertension management. More recently, a systematic review that focused on “meaningful use” regulations, by Jones et al.,101 found robust evidence supporting the broad use of CDSSs; however, information on implementation was sparse.
Healthcare systems are shifting to comprehensive, interoperable, point of care–based computer systems that provide patient-specific decisions instantaneously. Also, with patients demanding instant access to their medical records, and healthcare systems seeking new ways to improve productivity, efficiency, safety, and cost savings, health information technology and CDSSs represent a shift in how providers and patients will interact moving forward. Although CDSSs are tools that aid clinicians in adhering to guidelines, more research is needed on their impact on patient outcomes. This review suggests that current CDSSs hold promise to improve quality of care outcomes but could be supplemented with more-intensive health system–level interventions—such as team-based care and provider performance feedback mechanisms—to reduce CVD risk.
Bright and colleagues12 conducted meta-regression analysis in their review and found six key features of successful CDSSs:
use of a computer-based generation of decision support instead of manual processes;
promoting action rather than inaction;
providing research evidence to justify assessments and recommendations;
engaging local users during system development;
linking with electronic patient charts to support workflow integration; and
providing decision support results to patients as well as providers.
Additionally, three features of successful systems previously identified by Kawamoto et al.102 were confirmed by Bright and colleagues12:
automatic provision of decision support as part of workflow;
provision of decision support at the time and location of decision making; and
providing recommendations rather than assessments alone.
As shown in Appendix Table 5 (available online), the present review identified four features likely to be associated with positive process of care outcomes:
provision of support as a part of clinician workflow;
provision of recommendations rather than assessments alone;
provision of decision support at the time and location of patient contact; and
integration with charting order entry system to support workflow integration.
In 2009, the U.S. government enacted the Health Information Technology for Economic and Clinical Health (HITECH) Act103 to provide incentives for rapid implementation and adoption of EHRs for clinicians and hospitals. Through the “meaningful use” regulations in the HITECH Act, hospitals and eligible professionals must implement and adopt clinical decision support rules as a component of “certified” office EHR systems, in order to qualify for payment incentives.104 The HITECH Act authorized incentive payments totaling $27 billion over 10 years for eligible professionals to collect a maximum of $44,000 and $63,750 in Medicare and Medicaid payments, respectively.105
Future research should investigate CDSS interventions in practice-based settings to better understand barriers encountered by implementers and challenges posed by generic, mass-produced EHR software not tailored to practices’ needs. Additionally, current “meaningful use” and implementation standards should be further evaluated. The effectiveness of CDSS interventions from this review is applicable to the U.S. healthcare system, outpatient primary care settings, and patients with multiple CVD risk factors. Implementers may need to adapt systems to meet their specific needs to improve outcomes for patients.
Supplementary Material
Acknowledgments
The authors acknowledge Michael Schooley and the Division for Heart Disease and Stroke Prevention, CDC, for their support at every step of the review. Gillian Sanders (Duke Evidence-Based Practice Center), Lynne T. Braun (Rush University College of Nursing), and Ninad Mishra (National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, CDC) provided guidance during the initial conceptualization. Randy Elder, Kate W. Harris, Kristen Folsom, and Onnalee Gomez (all from the Community Guide Branch, CDC) provided input at various stages of the review and the development of the manuscript.
With great sadness, the authors note the untimely passing of David B. Callahan earlier this year. We greatly valued his insight and contribution to this review.
Points of view are those of the authors and the Community Preventive Services Task Force and do not necessarily represent those of CDC.
The work of Gibril Njie and Ramona Finnie was supported with funds from the Oak Ridge Institute for Scientific Education.
Appendix: Supplementary data
Supplementary data associated with this article can be found at, http://dx.doi.org/10.1016/j.amepre.2015.04.006.
Footnotes
Author affiliations are shown at the time the research was conducted.
References
- 1.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–e245. doi: 10.1161/CIR.0b013e31828124ad. http://dx.doi.org/10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walsh JME, Sundaram V, McDonald K, Owens DK, Goldstein MK. Implementing effective hypertension quality improvement strategies: barriers and potential solutions. J Clin Hypertens. 2008;10(4):311–316. doi: 10.1111/j.1751-7176.2008.07425.x. http://dx.doi.org/10.1111/j.1751-7176.2008.07425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Healthy People 2020. Heart disease and stroke. www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=21.
- 4.USDHHS. Million Hearts: the initiative. www.millionhearts.hhs.gov/aboutmh/overview.html.
- 5.U.S. Preventive Services Task Force. Recommendations for primary care practice. www.uspreventiveservicestaskforce.org/Page/Name/recommendations. Accessed May 26 2015.
- 6.American Diabetes Association. Standards of medical care in diabetes —2013. Diabetes Care. 2013;36(suppl 1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. [PubMed] [Google Scholar]
- 8.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. http://dx.doi.org/10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 9.Phillips LS, Branch JWT, Cook CB, et al. Clinical inertia. Ann Intern Med. 2001;135(9):825–834. doi: 10.7326/0003-4819-135-9-200111060-00012. http://dx.doi.org/10.7326/0003-4819-135-9-200111060-00012. [DOI] [PubMed] [Google Scholar]
- 10.Baiardini I, Braido F, Bonini M, Compalati E, Canonica GW. Why do doctors and patients not follow guidelines? Curr Opin Allergy Clin Immunol. 2009;9(3):228–233. doi: 10.1097/ACI.0b013e32832b4651. http://dx.doi.org/10.1097/ACI.0b013e32832b4651. [DOI] [PubMed] [Google Scholar]
- 11.Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282(15):1458–1465. doi: 10.1001/jama.282.15.1458. http://dx.doi.org/10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 12.Bright TJ, Wong A, Dhurjati R, et al. Effect of clinical decisionsupport systems: a systematic review. Ann Intern Med. 2012;157(1):29–43. doi: 10.7326/0003-4819-157-1-201207030-00450. http://dx.doi.org/10.7326/0003-4819-157-1-201207030-00450. [DOI] [PubMed] [Google Scholar]
- 13.Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based Guide to Community Preventive Services—methods. Am J Prev Med. 2000;18(1S):35–43. doi: 10.1016/s0749-3797(99)00119-1. [DOI] [PubMed] [Google Scholar]
- 14.Zaza S, Wright-De Agüero LK, Briss PA, et al. Data collection instrument and procedure for systematic reviews in the Guide to Community Preventive Services. Am J Prev Med. 2000;18(1 suppl):44–74. doi: 10.1016/s0749-3797(99)00122-1. [DOI] [PubMed] [Google Scholar]
- 15.Agency for Healthcare Research and Quality. Enabling health care decision making through clinical decision making. 2012 www.ahrq.gov/research/findings/evidence-based-reports/er203-abstract.html.
- 16.The World Bank. Country and lending groups. 2012 www.data.worldbank.org/about/country-classifications/country-and-lending-groups.
- 17.Slutsky J, Atkins D, Chang S, Sharp BA. AHRQ series paper 1: comparing medical interventions: AHRQ and the effective healthcare program. J Clin Epidemiol. 2010;63(5):481–483. doi: 10.1016/j.jclinepi.2008.06.009. http://dx.doi.org/10.1016/j.jclinepi.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 18.U.S. Preventive Services Task Force. Screening for high blood pressure in adults. 2007 www.uspreventiveservicestaskforce.org/uspstf/uspshype.htm.
- 19.U.S. Preventive Services Task Force. Screening for lipid disorders in adults. 2008 www.uspreventiveservicestaskforce.org/uspstf/uspschol.htm.
- 20.U.S. Preventive Services Task Force. Screening for type 2 diabetes mellitus in adults. 2008 www.uspreventiveservicestaskforce.org/uspstf/uspsdiab.htm.
- 21.U.S. Preventive Services Task Force. Counseling and interventions to prevent tobacco use and tobacco-caused disease in adults and pregnant women. 2009 www.uspreventiveservicestaskforce.org/Page/Topic/recommendation-summary/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions.
- 22.U.S. Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease. 2009 www.uspreventiveservicestaskforce.org/uspstf/uspsasmi.htm.
- 23.Grundy SM, Cleeman JI, Bairey Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. J Am Coll Cardiol. 2004;44(3):720–732. doi: 10.1016/j.jacc.2004.07.001. http://dx.doi.org/10.1016/j.jacc.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 24.Bertoni AG, Bonds DE, Chen H, et al. Impact of a multifaceted intervention on cholesterol management in primary care practices: guideline adherence for heart health randomized trial. Arch Intern Med. 2009;169(7):678–686. doi: 10.1001/archinternmed.2009.44. http://dx.doi.org/10.1001/archinternmed.2009.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bosworth HB, Olsen MK, Dudley T, et al. Patient education and provider decision support to control blood pressure in primary care: a cluster randomized trial. Am Heart J. 2009;157(3):450–456. doi: 10.1016/j.ahj.2008.11.003. http://dx.doi.org/10.1016/j.ahj.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 26.Cleveringa FG, Gorter KJ, van den Donk M, Rutten GE. Combined task delegation, computerized decision support, and feedback improve cardiovascular risk for type 2 diabetic patients: a cluster randomized trial in primary care. Diabetes Care. 2008;31(12):2273–2275. doi: 10.2337/dc08-0312. http://dx.doi.org/10.2337/dc08-0312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cobos A, Vilaseca J, Asenjo C. Cost effectiveness of a clinical decision support system based on the recommendations of the European Society of Cardiology and other societies for the management of hypercholesterolemia: report of a cluster-randomized trial. Dis Manag Health Out. 2005;13(6):421–432. http://dx.doi.org/10.2165/00115677-200513060-00007. [Google Scholar]
- 28.Demakis JG, Beauchamp C, Cull WL, et al. Improving residents’ compliance with standards of ambulatory care: results from the VA cooperative study on computerized reminders. JAMA. 2000;284(11):1411–1416. doi: 10.1001/jama.284.11.1411. http://dx.doi.org/10.1001/jama.284.11.1411. [DOI] [PubMed] [Google Scholar]
- 29.Dorr DA, Wilcox A, Donnelly SM, Burns L, Clayton PD. Impact of generalist care managers on patients with diabetes. Health Serv Res. 2005;40(5, pt 1):1400–1421. doi: 10.1111/j.1475-6773.2005.00423.x. http://dx.doi.org/10.1111/j.1475-6773.2005.00423.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Filippi A, Sabatini A, Badioli L, et al. Effects of an automated electronic reminder in changing the antiplatelet drug-prescribing behavior among Italian general practitioners in diabetic patients: an intervention trial. Diabetes Care. 2003;26(5):1497–1500. doi: 10.2337/diacare.26.5.1497. http://dx.doi.org/10.2337/diacare.26.5.1497. [DOI] [PubMed] [Google Scholar]
- 31.Frame PS, Zimmer JG, Werth PL, Hall WJ, Eberly SW. Computer-based vs manual health maintenance tracking. A controlled trial. Arch Fam Med. 1994;3(7):581–588. doi: 10.1001/archfami.3.7.581. http://dx.doi.org/10.1001/archfami.3.7.581. [DOI] [PubMed] [Google Scholar]
- 32.Frank O, Litt J, Beilby J. Opportunistic electronic reminders. improving performance of preventive care in general practice. Aust Fam Physician. 2004;33(1–2):87–90. [PubMed] [Google Scholar]
- 33.Fretheim A, Oxman AD, Havelsrud K, Treweek S, Kristoffersen DT, Bjorndal A. Rational Prescribing in Primary Care (RaPP): a cluster randomized trial of a tailored intervention. PLoS Med. 2006;3(6):e134. doi: 10.1371/journal.pmed.0030134. http://dx.doi.org/10.1371/journal.pmed.0030134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gill JM, Chen YX, Glutting JJ, Diamond JJ, Lieberman MI. Impact of decision support in electronic medical records on lipid management in primary care. Popul Health Manag. 2009;12(5):221–226. doi: 10.1089/pop.2009.0003. http://dx.doi.org/10.1089/pop.2009.0003. [DOI] [PubMed] [Google Scholar]
- 35.Gill JM, Ewen E, Nsereko M. Impact of an electronic medical record on quality of care in a primary care office. Del Med J. 2001;73(5):187–194. [PubMed] [Google Scholar]
- 36.Goldberg HI, Neighbor WE, Cheadle AD, Ramsey SD, Diehr P, Gore E. A controlled time-series trial of clinical reminders: using computerized firm systems to make quality improvement research a routine part of mainstream practice. Health Serv Res. 2000;34(7):1519–1534. [PMC free article] [PubMed] [Google Scholar]
- 37.Hetlevik I, Holmen J, Kruger O. Implementing clinical guidelines in the treatment of hypertension in general practice. Evaluation of patient outcome related to implementation of a computer-based clinical decision support system. Scand J Prim Health Care. 1999;17(1):35–40. doi: 10.1080/028134399750002872. http://dx.doi.org/10.1080/028134399750002872. [DOI] [PubMed] [Google Scholar]
- 38.Hetlevik I, Holmen J, Kruger O, Kristensen P, Iversen H, Furuseth K. Implementing clinical guidelines in the treatment of diabetes mellitus in general practice. Evaluation of effort, process, and patient outcome related to implementation of a computer-based decision support system. Int J Technol Assess Health Care. 2000;16(1):210–227. doi: 10.1017/s0266462300161185. http://dx.doi.org/10.1017/S0266462300161185. [DOI] [PubMed] [Google Scholar]
- 39.Hicks LS, Sequist TD, Ayanian JZ, et al. Impact of computerized decision support on blood pressure management and control: a randomized controlled trial. J Gen Intern Med. 2008;23(4):429–441. doi: 10.1007/s11606-007-0403-1. http://dx.doi.org/10.1007/s11606-007-0403-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hobbs FD, Delaney BC, Carson A, Kenkre JE. A prospective controlled trial of computerized decision support for lipid management in primary care. Fam Pract. 1996;13(2):133–137. doi: 10.1093/fampra/13.2.133. http://dx.doi.org/10.1093/fampra/13.2.133. [DOI] [PubMed] [Google Scholar]
- 41.Holbrook A, Thabane L, Keshavjee K, et al. Individualized electronic decision support and reminders to improve diabetes care in the community: COMPETE II randomized trial. CMAJ. 2009;181(1–2):37–44. doi: 10.1503/cmaj.081272. http://dx.doi.org/10.1503/cmaj.081272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Holt TA, Thorogood M, Griffiths F, Munday S, Friede T, Stables D. Automated electronic reminders to facilitate primary cardiovascular disease prevention: randomised controlled trial. Br J Gen Pract. 2010;60(573):e137–e143. doi: 10.3399/bjgp10X483904. http://dx.doi.org/10.3399/bjgp10X483904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kenealy T, Arroll B, Petrie KJ. Patients and computers as reminders to screen for diabetes in family practice. Randomized-controlled trial. J Gen Intern Med. 2005;20(10):916–921. doi: 10.1111/j.1525-1497.2005.0197.x. http://dx.doi.org/10.1111/j.1525-1497.2005.0197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lobach DF, Hammond WE. Development and evaluation of a computer-assisted management protocol (CAMP): improved compliance with care guidelines for diabetes mellitus. Proc Annu Symp Comput Appl Med Care. 1994:787–791. [PMC free article] [PubMed] [Google Scholar]
- 45.Maclean CD, Gagnon M, Callas P, Littenberg B. The Vermont Diabetes Information System: a cluster randomized trial of a population based decision support system. J Gen Intern Med. 2009;24(12):1303–1310. doi: 10.1007/s11606-009-1147-x. http://dx.doi.org/10.1007/s11606-009-1147-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Martens JD, van der Weijden T, Severens JL, et al. The effect of computer reminders on GPs’ prescribing behaviour: a cluster-randomised trial. Int J Med Inform. 2007;76(suppl 3):S403–S416. doi: 10.1016/j.ijmedinf.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 47.Mc Donald CJ. Use of a computer to detect and respond to clinical events: its effect on clinician behavior. Ann Intern Med. 1976;84(2):162–167. doi: 10.7326/0003-4819-84-2-162. http://dx.doi.org/10.7326/0003-4819-84-2-162. [DOI] [PubMed] [Google Scholar]
- 48.McDowell I, Newell C, Rosser W. A randomized trial of computerized reminders for blood pressure screening in primary care. Med Care. 1989;27(3):297–305. doi: 10.1097/00005650-198903000-00008. http://dx.doi.org/10.1097/00005650-198903000-00008. [DOI] [PubMed] [Google Scholar]
- 49.McLaughlin D, Hayes JR, Kelleher K. Office-based interventions for recognizing abnormal pediatric blood pressures. Clin Pediatr (Phila) 2010;49(4):355–362. doi: 10.1177/0009922809339844. http://dx.doi.org/10.1177/0009922809339844. [DOI] [PubMed] [Google Scholar]
- 50.Montgomery AA, Fahey T, Peters TJ, MacIntosh C, Sharp DJ. Evaluation of computer based clinical decision support system and risk chart for management of hypertension in primary care: randomised controlled trial. BMJ. 2000;320(7236):686–690. doi: 10.1136/bmj.320.7236.686. http://dx.doi.org/10.1136/bmj.320.7236.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Murray MD, Harris LE, Overhage JM, et al. Failure of computerized treatment suggestions to improve health outcomes of outpatients with uncomplicated hypertension: results of a randomized controlled trial. Pharmacotherapy. 2004;24(3):324–337. doi: 10.1592/phco.24.4.324.33173. http://dx.doi.org/10.1592/phco.24.4.324.33173. [DOI] [PubMed] [Google Scholar]
- 52.O’Connor PJ, Crain AL, Rush WA, Sperl-Hillen JM, Gutenkauf JJ, Duncan JE. Impact of an electronic medical record on diabetes quality of care. Ann Fam Med. 2005;3(4):300–306. doi: 10.1370/afm.327. http://dx.doi.org/10.1370/afm.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ornstein SM, Garr DR, Jenkins RG, Rust PF, Arnon A. Computer-generated physician and patient reminders: tools to improve population adherence to selected preventive services. J Fam Pract. 1991;32(1):82–90. [PubMed] [Google Scholar]
- 54.Overhage JM, Tierney WM, McDonald CJ. Computer reminders to implement preventive care guidelines for hospitalized patients. Arch Intern Med. 1996;156(14):1551–1556. http://dx.doi.org/10.1001/archinte.1996.00440130095010. [PubMed] [Google Scholar]
- 55.Overhage JM, Tierney WM, Zhou XH, McDonald CJ. A randomized trial of “corollary orders” to prevent errors of omission. J Am Med Inform Assoc. 1997;4(5):364–375. doi: 10.1136/jamia.1997.0040364. http://dx.doi.org/10.1136/jamia.1997.0040364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Palen TE, Raebel M, Lyons E, Magid DM. Evaluation of laboratory monitoring alerts within a computerized physician order entry system for medication orders. Am J Manag Care. 2006;12(7):389–395. [PubMed] [Google Scholar]
- 57.Peterson KA, Radosevich DM, O’Connor PJ, et al. Improving diabetes care in practice: findings from the TRANSLATE trial. Diabetes Care. 2008;31(12):2238–2243. doi: 10.2337/dc08-2034. http://dx.doi.org/10.2337/dc08-2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Phillips LS, Ziemer DC, Doyle JP, et al. An endocrinologist-supported intervention aimed at providers improves diabetes management in a primary care site: improving primary care of African Americans with diabetes (IPCAAD) 7. Diabetes Care. 2005;28(10):2352–2360. doi: 10.2337/diacare.28.10.2352. http://dx.doi.org/10.2337/diacare.28.10.2352. [DOI] [PubMed] [Google Scholar]
- 59.Price M. Can hand-held computers improve adherence to guidelines? A (Palm) pilot study of family doctors in British Columbia. Can Fam Physician. 2005;51:1506–1507. [PMC free article] [PubMed] [Google Scholar]
- 60.Reeve JF, Tenni PC, Peterson GM. An electronic prompt in dispensing software to promote clinical interventions by community pharmacists: a randomized controlled trial. Br J Clin Pharmacol. 2008;65(3):377–385. doi: 10.1111/j.1365-2125.2007.03012.x. http://dx.doi.org/10.1111/j.1365-2125.2007.03012.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rosser WW, McDowell I, Newell C. Use of reminders for preventive procedures in family medicine. CMAJ. 1991;145(7):807–814. [PMC free article] [PubMed] [Google Scholar]
- 62.Rossi RA, Every NR. A computerized intervention to decrease the use of calcium channel blockers in hypertension. J Gen Intern Med. 1997;12(11):672–678. doi: 10.1046/j.1525-1497.1997.07140.x. http://dx.doi.org/10.1046/j.1525-1497.1997.07140.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Roumie CL, Elasy TA, Greevy R, et al. Improving blood pressure control through provider education, provider alerts, and patient education: a cluster randomized trial. Ann Intern Med. 2006;145(3):165–175. doi: 10.7326/0003-4819-145-3-200608010-00004. http://dx.doi.org/10.7326/0003-4819-145-3-200608010-00004. [DOI] [PubMed] [Google Scholar]
- 64.Sequist TD, Gandhi TK, Karson AS, et al. A randomized trial of electronic clinical reminders to improve quality of care for diabetes and coronary artery disease. J Am Med Inform Assoc. 2005;12(4):431–437. doi: 10.1197/jamia.M1788. http://dx.doi.org/10.1197/jamia.M1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Smith SA, Shah ND, Bryant SC, et al. Chronic care model and shared care in diabetes: randomized trial of an electronic decision support system. Mayo Clin Proc. 2008;83(7):747–757. doi: 10.4065/83.7.747. http://dx.doi.org/10.4065/83.7.747. [DOI] [PubMed] [Google Scholar]
- 66.Tamblyn R, Reidel K, Huang A, et al. Increasing the detection and response to adherence problems with cardiovascular medication in primary care through computerized drug management systems: a randomized controlled trial. Med Decis Making. 2010;30(2):176–188. doi: 10.1177/0272989X09342752. http://dx.doi.org/10.1177/0272989X09342752. [DOI] [PubMed] [Google Scholar]
- 67.Toth-Pal E, Nilsson GH, Furhoff AK. Clinical effect of computer generated physician reminders in health screening in primary health care—a controlled clinical trial of preventive services among the elderly. Int J Med Inform. 2004;73(9–10):695–703. doi: 10.1016/j.ijmedinf.2004.05.007. http://dx.doi.org/10.1016/j.ijmedinf.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 68.van Wyk JT, van Wijk MA, Sturkenboom MC, Mosseveld M, Moorman PW, van der Lei J. Electronic alerts versus on-demand decision support to improve dyslipidemia treatment: a cluster randomized controlled trial. Circulation. 2008;117(3):371–378. doi: 10.1161/CIRCULATIONAHA.107.697201. http://dx.doi.org/10.1161/CIRCULATIONAHA.107.697201. [DOI] [PubMed] [Google Scholar]
- 69.Bosworth HB, Olsen MK, Goldstein MK, et al. The Veterans’ Study to Improve the Control of Hypertension (V-STITCH): design and methodology. Contemp Clin Trials. 2005;26(2):155–168. doi: 10.1016/j.cct.2004.12.006. http://dx.doi.org/10.1016/j.cct.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 70.Fretheim A, Aaserud M, Oxman AD. Rational prescribing in primary care (RaPP): economic evaluation of an intervention to improve professional practice. PLoS Med. 2006;3(6):e216. doi: 10.1371/journal.pmed.0030216. http://dx.doi.org/10.1371/journal.pmed.0030216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hetlevik I, Holmen J, Kruger O, Kristensen P, Iversen H. Implementing clinical guidelines in the treatment of hypertension in general practice. Blood Press. 1998;7(5–6):270–276. doi: 10.1080/080370598437114. http://dx.doi.org/10.1080/080370598437114. [DOI] [PubMed] [Google Scholar]
- 72.Holt TA, Thorogood M, Griffiths F, Munday S. Protocol for the “E-Nudge Trial”: a randomised controlled trial of electronic feedback to reduce the cardiovascular risk of individuals in general practice [ISRCTN64828380] Trials. 2006;7:11. doi: 10.1186/1745-6215-7-11. http://dx.doi.org/10.1186/1745-6215-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Khan S, Maclean CD, Littenberg B. The effect of the Vermont Diabetes Information System on inpatient and emergency room use: results from a randomized trial. Health Outcomes Res Med. 2010;1(1):e61–e66. doi: 10.1016/j.ehrm.2010.03.002. http://dx.doi.org/10.1016/j.ehrm.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Martens JD, van der Aa A, Panis B, van der Weijden T, Winkens RA, Severens JL. Design and evaluation of a computer reminder system to improve prescribing behaviour of GPs. Stud Health Technol Inform. 2006;124:617–623. [PubMed] [Google Scholar]
- 75.Ziemer DC, Doyle JP, Barnes CS, et al. An intervention to overcome clinical inertia and improve diabetes mellitus control in a primary care setting: Improving Primary Care of African Americans with Diabetes (IPCAAD) 8. Arch Intern Med. 2006;166(5):507–513. doi: 10.1001/archinte.166.5.507. http://dx.doi.org/10.1001/archinte.166.5.507. [DOI] [PubMed] [Google Scholar]
- 76.Bassa A, del Val M, Cobos A, et al. Impact of a clinical decision support system on the management of patients with hypercholesterolemia in the primary healthcare setting. Dis Manag Health Out. 2005;13(1):65–72. http://dx.doi.org/10.2165/00115677-200513010-00007. [Google Scholar]
- 77.Cleveringa FG, Gorter KJ, van den Donk M, Pijman PL, Rutten GE. Task delegation and computerized decision support reduce coronary heart disease risk factors in type 2 diabetes patients in primary care. Diabetes Technol Ther. 2007;9(5):473–481. doi: 10.1089/dia.2007.0210. http://dx.doi.org/10.1089/dia.2007.0210. [DOI] [PubMed] [Google Scholar]
- 78.Feldstein AC, Perrin NA, Unitan R, et al. Effect of a patient panel-support tool on care delivery. Am J Manag Care. 2010;16(10):e256–e266. [PubMed] [Google Scholar]
- 79.Guerra YS, Das K, Antonopoulos P, et al. Computerized physician order entry-based hyperglycemia inpatient protocol and glycemic outcomes: the CPOE-HIP study. Endocr Pract. 2010;16(3):389–397. doi: 10.4158/EP09223.OR. http://dx.doi.org/10.4158/EP09223.OR. [DOI] [PubMed] [Google Scholar]
- 80.Apkon M, Mattera JA, Lin Z, et al. A randomized outpatient trial of a decision-support information technology tool. Arch Intern Med. 2005;165(20):2388–2394. doi: 10.1001/archinte.165.20.2388. http://dx.doi.org/10.1001/archinte.165.20.2388. [DOI] [PubMed] [Google Scholar]
- 81.Eaton CB, Parker DR, Borkan J, et al. Translating cholesterol guidelines into primary care practice: a multimodal cluster randomized trial. Ann Fam Med. 2011;9(6):528–537. doi: 10.1370/afm.1297. http://dx.doi.org/10.1370/afm.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Herrin J, da Graca B, Nicewander D, et al. The effectiveness of implementing an electronic health record on diabetes care and outcomes. Health Serv Res. 2012;47(4):1522–1540. doi: 10.1111/j.1475-6773.2011.01370.x. http://dx.doi.org/10.1111/j.1475-6773.2011.01370.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Holbrook A, Pullenayegum E, Thabane L, et al. Shared electronic vascular risk decision support in primary care: Computerization of Medical Practices for the Enhancement of Therapeutic Effectiveness (COMPETE III) randomized trial. Arch Intern Med. 2011;171(19):1736–1744. doi: 10.1001/archinternmed.2011.471. http://dx.doi.org/10.1001/archinternmed.2011.471. [DOI] [PubMed] [Google Scholar]
- 84.Kelly E, Wasser T, Fraga JD, Scheirer JJ, Alweis RL. Impact of an EMR clinical decision support tool on lipid management. J Clin Outcomes Manag. 2011;18(12):551. [Google Scholar]
- 85.O’Connor PJ, Sperl-Hillen JAM, Rush WA, et al. Impact of electronic health record clinical decision support on diabetes care: a randomized trial. Ann Fam Med. 2011;9(1):12–21. doi: 10.1370/afm.1196. http://dx.doi.org/10.1370/afm.1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rodbard HW, Schnell O, Unger J, et al. Use of an automated decision support tool optimizes clinicians’ ability to interpret and appropriately respond to structured self-monitoring of blood glucose data. Diabetes Care. 2012;35(4):693–698. doi: 10.2337/dc11-1351. http://dx.doi.org/10.2337/dc11-1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Schnipper JL, Linder JA, Palchuk MB, et al. Effects of documentation-based decision support on chronic disease management. Am J Manag Care. 2010;16(12 suppl HIT):SP72–SP81. [PubMed] [Google Scholar]
- 88.Jean-Jacques M, Persell SD, Thompson JA, Hasnain-Wynia R, Baker DW. Changes in disparities following the implementation of a health information technology-supported quality improvement initiative. J Gen Intern Med. 2012;27(1):71–77. doi: 10.1007/s11606-011-1842-2. http://dx.doi.org/10.1007/s11606-011-1842-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.El-Kareh RE, Gandhi TK, Poon EG, et al. Actionable reminders did not improve performance over passive reminders for overdue tests in the primary care setting. J Am Med Inform Assoc. 2011;18(2):160–163. doi: 10.1136/jamia.2010.003152. http://dx.doi.org/10.1136/jamia.2010.003152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Munoz M, Pronovost P, Dintzis J, et al. Implementing and evaluating a multicomponent inpatient diabetes management program: putting research into practice. Jt Comm J Qual Patient Saf. 2012;38(5):195–206. doi: 10.1016/s1553-7250(12)38025-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Nemeth LS, Ornstein SM, Jenkins RG, Wessell AM, Nietert PJ. Implementing and evaluating electronic standing orders in primary care practice: a PPRNet study. J Am Board Fam Med. 2012;25(5):594–604. doi: 10.3122/jabfm.2012.05.110214. http://dx.doi.org/10.3122/jabfm.2012.05.110214. [DOI] [PubMed] [Google Scholar]
- 92.Persell SD, Kaiser D, Dolan NC, et al. Changes in performance after implementation of a multifaceted electronic-health-record-based quality improvement system. Med Care. 2011;49(2):117–125. doi: 10.1097/MLR.0b013e318202913d. http://dx.doi.org/10.1097/MLR.0b013e318202913d. [DOI] [PubMed] [Google Scholar]
- 93.Shelley D, Tseng TY, Matthews AG, et al. Technology-driven intervention to improve hypertension outcomes in community health centers. Am J Manag Care. 2011;17(12 Spec No):SP103–SP110. [PubMed] [Google Scholar]
- 94.Shih SC, McCullough CM, Wang JJ, Singer J, Parsons AS. Health information systems in small practices improving the delivery of clinical preventive services. Am J Prev Med. 2011;41(6):603–609. doi: 10.1016/j.amepre.2011.07.024. http://dx.doi.org/10.1016/j.amepre.2011.07.024. [DOI] [PubMed] [Google Scholar]
- 95.Charles D, Furukawa M, Hufstader M. Electronic Health Record Systems and Intent to Attest to Meaningful Use Among Non-Federal Acute Care Hospitals in the United States: 2008–2011. Washington DC: Feb, 2012. (ONC Data Brief, no 1). [Google Scholar]
- 96.Bulpitt CJ, Fletcher AE. The measurement of quality of life in hypertensive patients: a practical approach. Br J Clin Pharmacol. 1990;30(3):353–364. doi: 10.1111/j.1365-2125.1990.tb03784.x. http://dx.doi.org/10.1111/j.1365-2125.1990.tb03784.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Community Preventive Services Task Force. Cardiovascular disease prevention and control: clinical decision-support systems (CDSS) Task Force finding and rationale statement. 2013 www.thecommunityguide.org/cvd/RRCDSS.html.
- 98.Community Preventive Services Task Force. Clinical decision-support systems recommended to prevent cardiovascular disease. Am J Prev Med. 2015;49(5):796–799. doi: 10.1016/j.amepre.2015.03.041. [DOI] [PubMed] [Google Scholar]
- 99.Souza NM, Sebaldt RJ, Mackay JA, et al. Computerized clinical decision support systems for primary preventive care: a decision-maker-researcher partnership systematic review of effects on process of care and patient outcomes. Implement Sci. 2011;6:87. doi: 10.1186/1748-5908-6-87. http://dx.doi.org/10.1186/1748-5908-6-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Montgomery AA, Fahey T. A systematic review of the use of computers in the management of hypertension. J Epidemiol Commun Health. 1998;52(8):520–525. doi: 10.1136/jech.52.8.520. http://dx.doi.org/10.1136/jech.52.8.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jones SS, Rudin RS, Perry T, Shekelle PG. Health information technology: an updated systematic review with a focus on meaningful use. Ann Intern Med. 2014;160(1):48–54. doi: 10.7326/M13-1531. http://dx.doi.org/10.7326/M13-1531. [DOI] [PubMed] [Google Scholar]
- 102.Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005;330(7494):765. doi: 10.1136/bmj.38398.500764.8F. http://dx.doi.org/10.1136/bmj.38398.500764.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Office of the National Coordinator for Health Information Technology. Certification and EHR incentives. www.healthit.gov/policy-researchers-implementers/hitech-act.
- 104.Centers for Medicare & Medicaid Services. EHR incentive programs. www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html.
- 105.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501–504. doi: 10.1056/NEJMp1006114. http://dx.doi.org/10.1056/NEJMp1006114. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


